Or Write Up 52611
Diunggah oleh
babydumplingsDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Or Write Up 52611
Diunggah oleh
babydumplingsHak Cipta:
Format Tersedia
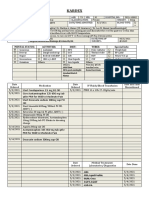
OR WRITE-UP Pts. Profile: Mr.
Romulo Aban Corpus ,male, age 63, from 216 new site bakakeng , baguio city, came in for surgery. The procedure to be performed is mastectomy. His surgeon is Dr. Pablo Candelario ; anesthesiologist is Dr. Noel Delizo. His operation started at 7:55am and ended at around 9:00am , it went well without any complications and not causing any distress for the patient.
Pathophysiology
BREAST CANCER
Etiology/ Cause cancer is a general name given to a large group of dieases characterized by: a)uncontrolled growth and spread of abnormal cells b) proliferation (rapid reproduction by cell division) c) metastasis (spread or transfer of cancer cells from one organ or part to another) -cause is unkown: predisposing factors include family history, high fat diet, -low level ionizing radiation (more common in women than in men)
clinical manifestations -a non tender lump, usually in an upper outer quadrant -axillary lymph adenopathy (late) -fixed nodular breast mass (late) -discharge -edema of the arm
Diagnosis: -mammography -needle biopsy -surgical biopsy
Treatment : -mastectomy - lumpectomy -radiation therapy -chemotherapy including cyclophosphamide
Anatomy of the organ involved
Reconstructive surgery
After having a mastectomy (or some breast-conserving surgeries), a woman may want to consider having the breast mound rebuilt; this is called breast reconstruction. These procedures are not done to treat cancer but to restore the breast's appearance after surgery. If you are going to have breast surgery and are thinking about having reconstruction, it is important to consult with a plastic surgeon who is an expert in breast reconstruction before your surgery.
Decisions about the type of reconstruction and when it will be done depend on each woman's medical situation and personal preferences. You may have a choice between having your breast reconstructed at the same time as the mastectomy (immediate reconstruction) or at a later time (delayed reconstruction). There are several types of reconstructive surgery. Some use saline (salt water) or silicone implants, while others use tissues from other parts of your body (autologous tissue reconstruction). For a discussion of the different reconstruction options, see our document, Breast Reconstruction After Mastectomy. You may also find it helpful to talk with a woman who has had the type of reconstruction you might be considering. Our Reach to Recovery volunteers can help you with this.
Discussion of the procedure
For many, the thought of surgery can be frightening. But with a better understanding of what to expect before, during, and after the operation, many fears can be relieved. Before surgery: The common biopsy procedures let you find out if you have breast cancer within a few days of your biopsy, but the extent of the breast cancer will not be known until after imaging tests and the surgery for local treatment are done. Usually, you meet with your surgeon a few days before the operation to discuss the procedure. This is a good time to ask specific questions about the surgery and review potential risks. Be sure you understand what the extent of the surgery is likely to be and what you should expect afterward. If you are thinking about breast reconstruction, ask about this as well. You will be asked to sign a consent form, giving the doctor permission to perform the surgery. Take your time and review the form carefully to be certain that you understand what you are signing. Sometimes, doctors send material for you to review in advance of your appointment, so you will have plenty of time to read it and won't feel rushed. You may also be asked to give consent for researchers to use any tissue or blood that is not needed for diagnostic purposes. Although this may not be of direct use to you, it may be very helpful to women in the future. You may be asked to donate blood before some operations, such as a mastectomy combined with natural tissue reconstruction, if the doctors think a transfusion might be needed. You might feel more secure knowing that if a transfusion is needed, you will receive your own blood. If you do not receive your own blood, it is important to know that in the United States, blood transfusion from another person is nearly as safe as receiving your own blood. Ask your doctor about your possible need for a blood transfusion. Your doctor will review your medical records and ask you about any medicines you are taking. This is to be sure that you are not taking anything that might interfere with the surgery. For example, if you are taking aspirin, arthritis medicine, or a blood-thinning drug (like coumadin), you may be asked to stop taking the drug about a week or 2 before the surgery. Be sure you tell your doctor about everything you take, including vitamins and herbal supplements. Usually, you will be told not to eat or drink anything for 8 to 12 hours before the surgery, especially if you are going to have general anesthesia (will be asleep during surgery). You will also meet with the anesthesiologist or nurse anesthetist, the health professional who will be giving you the anesthesia during your surgery. The type of anesthesia used depends largely on the kind of surgery being done and your medical history. Surgery: Depending on the likely extent of your surgery, you may be offered the choice of an outpatient procedure (where you go home the same day) or you may be admitted to the hospital. General anesthesia is usually given whenever the surgery involves a mastectomy or an axillary node dissection, and is most often used during breast-conserving surgery as well. You will have
an IV (intravenous) line put in (usually in a vein in your arm), which the medical team will use to give medicines that may be needed during the surgery. Usually you will be hooked up to an electrocardiogram (EKG) machine and have a blood pressure cuff on your arm, so your heart rhythm and blood pressure can be checked during the surgery. The length of the operation depends on the type of surgery being done. For example, a mastectomy with axillary lymph node dissection will usually take from 2 to 3 hours. After your surgery, you will be taken to the recovery room, where you will stay until you are awake and your condition
After surgery: How long you stay in the hospital depends on the type of surgery being done, your overall state of health and whether you have any other medical problems, how well you do during the surgery, and how you feel after the surgery. Decisions about the length of your stay should be made by you and your doctor and not dictated by what your insurance will pay, but it is important to check your insurance coverage before surgery.
An incision in the shape of an ellipse. OVERVIEW OF MRM PROCEDURE: 1.) An incision in the shape of an ellipse is made. (Incisions are made to avoid visibility in a low neckline dress or bathing suit.) 2.) The surgeon removes the minimum amount of skin and tissue so that remaining healthy tissue can be used for possible reconstruction. 3.) Skin flaps are made carefully and as thinly as possible to maximize removal of diseased breast tissues. 4.) The skin over a neighboring muscle (pectoralis major fascia) is removed, after which the surgeon focuses in the armpit (axilla, axillary) region. 5.) In this region, the surgeon carefully identifies vital anatomical structures such as blood vessels (veins, arteries) and nerves.
(Accidental injury to specific nerves like the medial pectoral neurovascular bundle will result in destruction of the muscles that this surgery attempts to preserve, such as the pectoralis major muscle.) 6.) In the armpit region, the surgeon carefully protects the vital structures while removing cancerous tissues. 7.) After the surgeon completes the mastectomy, two plastic tubes each about the width of a pen are gently sewn into place to draw off fluids. The ends of these drains are attached to a pocket-sized suction device. Nursing responsibility: Monitoring of the drains and drainage until the drains are removed 8.) After axillary surgery, breast reconstruction can be performed, if desired by the patient. Normal results If no complications develop, the surgical area should completely heal within three to four weeks. In general, women having a mastectomy and/or axillary lymph node dissection stay in the hospital for 1 or 2 nights and then go home. However, some women may be placed in a 23hour, short-stay observation unit before going home. Less involved operations such as lumpectomy and sentinel lymph node biopsy are usually done in an outpatient surgery center, and an overnight stay in the hospital is usually not needed. You may have a dressing (bandage) over the surgery site that may wrap snugly around your chest. You may have one or more drains (plastic or rubber tubes) coming out from the breast or underarm area to remove blood and lymph fluid that collects during the healing process. Your health care team will teach you how to care for the drains, which may include emptying and measuring the fluid and identifying problems the doctor or nurse needs to know about. Most drains stay in place for 1 or 2 weeks. When drainage has decreased to about 30 cc (1 fluid ounce) each day, the drain will usually be removed. Most doctors will want you to start moving your arm soon after surgery so that it won't get stiff.
Mastectomy
Mastectomy is surgery to remove the entire breast. All of the breast tissue is removed, sometimes along with other nearby tissues. Simple mastectomy: In this procedure, also called total mastectomy, the surgeon removes the entire breast, including the nipple, but does not remove underarm lymph nodes or muscle tissue from beneath the breast. Sometimes this is done for both breasts (a double mastectomy), especially when it is done as preventive surgery in women at very high risk for breast cancer. Most women, if they are hospitalized, can go home the next day. Skin-sparing mastectomy: For some women considering immediate reconstruction, a skinsparing mastectomy can be done. In this procedure, most of the skin over the breast (other than the nipple and areola) is left intact. This can work as well as a simple mastectomy. The amount of breast tissue removed is the same as with a simple mastectomy. This approach is only used when immediate breast reconstruction is planned. It may not be suitable for larger tumors or those that are close to the skin. Implants or tissue from other parts of the body are used to reconstruct the breast. This approach has not been used for as long as the more standard type of mastectomy, but many women prefer it because it offers the advantage of less scar tissue and a reconstructed breast that seems more natural. A variation of the skin-sparing mastectomy is the nipple-sparing mastectomy. This procedure is more often an option for women who have a small early stage cancer near the outer part of the breast, with no signs of cancer in the skin or near the nipple. In this procedure, the breast tissue is removed, but the breast skin and nipple are left in place. This is followed by breast reconstruction. The surgeon often removes the breast tissue beneath the nipple (and areola) during the procedure, to check for cancer cells. If cancer is found in this tissue, the nipple is involved with cancer and must be removed. Even when no cancer is found under the nipple, some doctors give the nipple tissue a dose of radiation during or after the surgery to try and reduce the risk of the cancer coming back. There are still some problems with nipple-sparing surgeries. Afterward, the nipple does not have a good blood supply, so sometimes it can wither away or become deformed. Because the nerves are also cut, there is little or no feeling left in the nipple. In women with larger breasts, the nipple may look out of place after the breast is reconstructed. As a result, many doctors feel that this surgery is best done in women with small to medium sized breasts. This procedure leaves less visible scars, but if it isn't done properly, it can leave behind more breast tissue than other forms of mastectomy. This could result in a higher risk of cancer developing in than for a skin-sparing or simple mastectomy. This was a problem in the past, but improvements in
technique have helped make this surgery safer. Still, many experts consider nipple-sparing procedures too risky to be a standard treatment of breast cancer. Modified radical mastectomy: This procedure is a simple mastectomy plus removal of axillary (underarm) lymph nodes. Surgery to remove these lymph nodes is discussed in further detail later in this section. Radical mastectomy: In this extensive operation, the surgeon removes the entire breast, axillary lymph nodes, and the pectoral (chest wall) muscles under the breast. This surgery was once very common, but it was found that a modified radical mastectomy was just as effective. This meant that the disfigurement and side effects of a radical mastectomy were not needed, so these surgeries are rarely done now. This operation may still be done for large tumors that are growing into the pectoral muscles under the breast. Possible side effects: Aside from post-surgical pain and the obvious change in the shape of the breast(s), possible side effects of mastectomy include wound infection, hematoma (buildup of blood in the wound), and seroma (buildup of clear fluid in the wound). If axillary lymph nodes are also removed, other side effects may occur (see the section, "Axillary lymph node dissection").
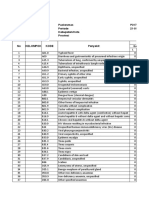
Instruments Used
A Deaver retractor (manual) is used to retract deep abdominal or chest incisions. Available in various widths.
A Richardson retractor (manual) is used to retract deep abdominal or chest incisions
Cutting and Dissecting Instruments
Are sharp and are used to cut body tissue or surgical supplies.
7 handle with 15 blade (deep knife) - Used to cut deep, delicate tissue. 3 handle with 10 blade (inside knife) Used to cut superficial tissue. 4 handle with 20 blade (skin knife) - Used to cut skin.
Straight Mayo scissors - Used to cut suture and supplies. Also known as: Suture scissors.
Curved Mayo scissors - Used to cut heavy tissue (fascia, muscle, uterus, and breast). Available in regular and long sizes.
Metzenbaum scissors (A) - Used to cut delicate tissue. Available in regular and long sizes.
Clamping and Occluding Instruments
Are used to compress blood vessels or hollow organs for hemostasis or to prevent spillage of contents. A hemostat is used to clamp blood vessels or tag sutures. Its jaws may be straight or curved. Other names: crile, snap or stat.
A mosquito is used to clamp small blood vessels. Its jaws may be straight or curved.
Grasping and Holding Instruments
Are used to hold tissue, drapes or sponges. An Allis is used to grasp tissue. Available in short and long sizes. A "Judd-Allis" holds intestinal tissue; a "heavy allis" holds breast tissue.
A Babcock is used to grasp delicate tissue (intestine, fallopian tube, ovary). Available in short and long sizes.
A Kocher is used to grasp heavy tissue. May also be used as a clamp. The jaws may be straight or curved. Other names: Ochsner.
DeBakey forceps are used to grasp delicate tissue, particularly in cardiovascular surgery
towel clips- for securing and holding towels in place.
Thumb forceps are used to grasp tough tissue (fascia, breast). Forceps may either have many teeth or a single tooth. Single tooth forceps are also called "rat tooth forceps."
Mayo-Hegar needle holders are used to hold needles when suturing. They may also be placed in the sewing category
Nipple-Sparing Mastectomy
Nipple-sparing mastectomy (NSM) has now entered the mainstream for both the treatment and prevention of breast cancer. It is not however, the standard of care for either. NSM in the past was known as subcutaneous mastectomy. In the 1970's, subcutaneous mastectomy was occasionally performed for fibrocystic disease, breast cancer prevention and less frequently for cancer. By the 1980's, reports of cancer occurring in the residual breast tissue led the procedure into disfavor. It was not until the last several years that this procedure was essentially reborn as nipple-sparing mastectomy. In examining the studies of subcutaneous mastectomy done in prior decades it was apparent that there were several problems that led to relatively poor results. Most importantly, most subcutaneous mastectomies of the 1970's were performed with a focus on cosmetics and less concern about removing a maximum amount of breast tissue. In many instances breast tissue was left behind intentionally to improve cosmetic results and to prevent necrosis (death) of the nipple. NSM is now usually performed by a surgical oncologist, breast surgeon or general surgeon with a focus on maximizing breast tissue removal, while still attempting to maximize the cosmetic outcome. The term "nipple-sparing mastectomy" now refers to a more radical removal of breast tissue than was carried out during the subcutaneous mastectomy era. There has never been a comparative study that compares nipple-sparing mastectomy with standard or standard skin-sparing mastectomy. A skin-sparing mastectomy preserves the breast skin but does not preserve the nipple. There are large series of skin-sparing mastectomies (SSM) that have been studied suggesting that results are likely similar to standard mastectomy techniques. However, as in NSM, no randomized comparative studies comparing SSM with standard mastectomy techniques have been carried out. At this time, there are no large studies of NSM followed for sufficient time to verify its ultimate safety. Because there are no studies to draw upon,
surrogate information must be used to make a judgment as to its appropriate use.
Pre OP Nipple-sparing mastectomy for cancer
Post OP
Without comparative studies, investigators have focused on the risk of finding occult (not diagnosable by examination or imaging studies) cancer cells in the nipple in women undergoing mastectomy for cancer. There have in fact been at least 13 studies which have looked at the incidence of occult nipple involvement by carefully examining the nipple under the microscope after its removal for cancer. Each study has slightly different results but there is some general agreement as to what factors lead to an increase in risk of occult nipple involvement. 1. Proximity of the cancer to the nipple: The closer the cancer is to the nipple the more likely cancer cells will be found in the nipple. Most investigators agree that at least 2 cm (a bit less than an inch) should separate the cancer from the nipple. Some investigators think that a 4cm distance is safer and utilize this distance in their recommendations. 2. Tumor size: As tumors increase in size, whether invasive or non-invasive (DCIS), the incidence of occult nipple involvement increases. Investigators differ on whether 3 or 4 cm should be the cutoff. 3. Lymph node involvement: A definite risk factor but not as significant as (1) or (2). 4. Multicentricity (cancer in more than one breast quadrant): This factor was not examined by all studies but was significant in those where it was studied. Nipple-sparing mastectomy for risk-reduction (prophylactic) Women undergo risk-reduction mastectomy for a variety of reasons including: 1. Test positive for a mutation in the BRCA 1/2 genes. 2. Strong family history of breast cancer without a positive genetic test. 3. Women undergoing mastectomy for cancer and wish to reduce their risk in the opposite breast. The issue in performing NSM for risk reduction centers around the milk ducts which exist in the nipple and the understandable concern that these ducts might serve as a source of new breast cancers. There are little in the way of actual studies which can support or deny that cancers actually arise in the ducts of the nipple. However, if one looks in the scientific literature, it will be difficult to find any studies which deal specifically with the risk of forming cancers in the nipple. (We are not speaking here about Paget's disease, which is cancer that has spread to the nipple from an underlying site in the breast.) Because cancers originating in the nipple have not been reported in the cancer literature, it seems reasonable to conclude that cancer originating in the nipple is rare or at the least, unusual. The low risk of nipple cancers may be at least partially explained by examining the actual anatomic origin of breast cancer. From very scholarly studies carried out in the 1970's, it has been discovered that virtually all breast cancers begin not in the large milk ducts similar to the ones found in the nipple but in the small microscopic ducts and milk-producing areas of the breast (lobules). A study publish by our group in 2008 in the Annals of Surgical Oncology examined this very question. We studied the nipple anatomy in patients undergoing mastectomy in which the nipple was removed. Our
study found that the small ducts and lobules in which breast cancer arises were rare in the nipple. In the very few cases in which lobules were found, there were few in number and found only at the junction of the nipple with the underlying breast tissue and not near the tip of the nipple. From this study it seemed reasonable to conclude that because the anatomic structures needed to form a breast cancer were rare in the nipple, that cancer originating in the nipple should also be rare.
Technical Issues Surgical complications related to nipple-sparing surgery are not unusual. The ability to get oxygen to the remaining breast skin is related to blood supply. The blood supply to the nipple and areola is particularly tenuous following NSM. Necrosis (tissue death) of the nipple-areola has been noted in virtually all reported series. It appears to vary from a high near 20% to a low of 2-3%. Many factors likely account for the differences including experience of the surgical team, choice of incision, breast size (increase risk in larger breasts) and on how effectively breast tissue is removed from behind the nipple and areola. In some circumstances, necrosis can occur to only the most superficial layers of the skin and complete healing usually occurs within a few weeks. Some surgeons feel the need to intentionally retain breast tissue behind the nipple and areola while others feel that nothing short of an attempt to remove all visible breast tissue is appropriate. It should be noted however, that intentionally retaining breast tissue behind the nipple could be problematic particularly in patients carrying a BRCA 1/2 genetic mutation. Patients electing to undergo NSM should also note that in almost all instances, the nipple will have little to no sensation. It is not unusual for some patients note a return of sensation to the breast skin but few report a return of anything but the most minimal sensation in the nipple.
Conclusion Nipple-sparing mastectomy is currently being performed at high-volume breast centers throughout the country. It would be fair to say that it is still investigational. However, we do believe that it is a procedure that warrants serious consideration when mastectomy is needed to treat cancer or desired for risk reduction. In the cancer setting, strict selection criteria should be followed at all times (as outlined above) in order to minimize the risk of recurrent cancer in the nipple. Cancers greater than 2cm from the nipple, less than 4cm in size can be considered. Axillary node status and multicentricity should be considered on a case-by-case basis. In the risk reduction setting, it is our feeling that there is minimal risk to retaining the nipple as long as great care is taken to remove all visible breast tissue from beneath the nipple. Coring of the nipple (removing tissue from within the nipple itself) should be considered in appropriate cases.
PINES CITY COLLEGES MAGSAYSAY AVENUE, BAGUIO CITY
(BREAST CANCER) Or write-up
SUBMITTTED BY : CARINO, MARIA CHRISTINA SUBMITTTED TO: MARJORIE ILONEN 5/25/2011
Anda mungkin juga menyukai
- Drug Study-Med WardDokumen2 halamanDrug Study-Med WardErnest Brian FernandezBelum ada peringkat
- Final Case Study - CADDokumen109 halamanFinal Case Study - CADPatricia Marie Buenafe100% (1)
- Discharge Planning EnglishDokumen11 halamanDischarge Planning Englishrahmat hidayatBelum ada peringkat
- Dynastat: What Is in This LeafletDokumen4 halamanDynastat: What Is in This LeafletBenj GilbuenaBelum ada peringkat
- DrugDokumen3 halamanDrugPeace Andong PerochoBelum ada peringkat
- Disaster Preparedness - Leadership and Coordination in Disaster in Health Care System With LectureDokumen29 halamanDisaster Preparedness - Leadership and Coordination in Disaster in Health Care System With LectureArvie ReyesBelum ada peringkat
- Drug StudiesDokumen16 halamanDrug Studiesvitcloud23100% (2)
- 13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsDokumen31 halaman13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsRena SafitriBelum ada peringkat
- AnastrozoleDokumen2 halamanAnastrozoleAnonymous FgT04krgymBelum ada peringkat
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDokumen4 halamanTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestBelum ada peringkat
- LFDDokumen3 halamanLFDVhince Norben PiscoBelum ada peringkat
- NCP OsteosarcomaDokumen6 halamanNCP OsteosarcomaNiksBelum ada peringkat
- LevofloxacinDokumen2 halamanLevofloxacinKatie McPeek100% (3)
- Job Application Letter For NurseDokumen2 halamanJob Application Letter For Nursenur aisyahBelum ada peringkat
- Pathophysiology of Transitional Cell CarcinomaDokumen10 halamanPathophysiology of Transitional Cell CarcinomaJheanAlphonsineT.MeansBelum ada peringkat
- PrednisoloneDokumen2 halamanPrednisoloneKatie McPeekBelum ada peringkat
- Learning Feedback DiaryDokumen10 halamanLearning Feedback DiaryLoids IgnacioBelum ada peringkat
- KetorolacDokumen5 halamanKetorolacMichelle Ann P. NacuaBelum ada peringkat
- NCP Skin IntegrityDokumen3 halamanNCP Skin IntegrityAlfie Ayro50% (2)
- Drug Study Amlodipine & HydrocortisoneDokumen4 halamanDrug Study Amlodipine & HydrocortisoneJohn Kristoffer JisonBelum ada peringkat
- Cefoxitin and Ketorolac Edited!!Dokumen3 halamanCefoxitin and Ketorolac Edited!!Bryan Cruz VisarraBelum ada peringkat
- Discharge Plan Methods InstructionsDokumen5 halamanDischarge Plan Methods InstructionsKirk CabasaBelum ada peringkat
- DexamethasoneDokumen6 halamanDexamethasoneapi-3797941100% (1)
- MannitolDokumen3 halamanMannitolAlexandra AntondyBelum ada peringkat
- NCP MentalDokumen6 halamanNCP MentalMarius Clifford BilledoBelum ada peringkat
- CHNDokumen11 halamanCHNAngelina Janiya NicoleBelum ada peringkat
- Nursing ManagementDokumen19 halamanNursing ManagementAjie ZamBelum ada peringkat
- Electrical Burn PathophysiologyDokumen1 halamanElectrical Burn PathophysiologydanicaBelum ada peringkat
- Cervical Cancer ChemotherapyDokumen6 halamanCervical Cancer ChemotherapyTheeya Quigao0% (1)
- Lui Sh-Colored Lips and Finger Nails Blur Red VisionDokumen1 halamanLui Sh-Colored Lips and Finger Nails Blur Red VisionMagdayao Romamea100% (1)
- Module V ActDokumen3 halamanModule V ActQueencess hayoBelum ada peringkat
- Discharge PlanDokumen4 halamanDischarge PlanVillanueva NiñaBelum ada peringkat
- Bearse Tablet InsertDokumen2 halamanBearse Tablet InsertLeonard ByunBelum ada peringkat
- Activity 6 - Drug StudyDokumen14 halamanActivity 6 - Drug StudyAl-Mujib TanogBelum ada peringkat
- Paracetamol - Drug StudyDokumen1 halamanParacetamol - Drug StudyPatricia Reese YutiamcoBelum ada peringkat
- Cefoxitin Drug StudyDokumen1 halamanCefoxitin Drug StudyArthur Christopher CorpuzBelum ada peringkat
- Pathophysiology / Explanation of The ProblemDokumen1 halamanPathophysiology / Explanation of The ProblemArian May MarcosBelum ada peringkat
- Tahbso ArticleDokumen4 halamanTahbso ArticleAlianna Kristine OhBelum ada peringkat
- Kardex: Mental Status: Activities: Diet: Tubes: Special InfoDokumen3 halamanKardex: Mental Status: Activities: Diet: Tubes: Special InfoJanelle Cabida SupnadBelum ada peringkat
- Operating Room WriteDokumen2 halamanOperating Room WritemodiBelum ada peringkat
- Drug Study CefuroximeDokumen2 halamanDrug Study CefuroximeSiafei RabeBelum ada peringkat
- Drug Study - Epidural AnesthesiaDokumen5 halamanDrug Study - Epidural AnesthesiaMarie PotayreBelum ada peringkat
- Cefazolin Sodium AncefDokumen1 halamanCefazolin Sodium AncefKristi WrayBelum ada peringkat
- Chromium Picolinate Drug StudyDokumen1 halamanChromium Picolinate Drug StudyjoellaBelum ada peringkat
- Tissue PerfusionDokumen2 halamanTissue Perfusionnursezey100% (3)
- Drug Study Generic Name (Brand Name) Indication Dosage, Route, Frequency Mechanism of Action Adverse Reaction Contraindication Nursing ResponsibilityDokumen3 halamanDrug Study Generic Name (Brand Name) Indication Dosage, Route, Frequency Mechanism of Action Adverse Reaction Contraindication Nursing ResponsibilityKimm Charmaine RodriguezBelum ada peringkat
- 6 PathophysiologyDokumen2 halaman6 PathophysiologyAJ SnowhiBelum ada peringkat
- Discharge Plan For AppendectomyDokumen1 halamanDischarge Plan For AppendectomyMyra AtuleBelum ada peringkat
- OxytocinDokumen1 halamanOxytocinjhinBelum ada peringkat
- Drug StudyDokumen3 halamanDrug StudyStephannie MirandaBelum ada peringkat
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokumen1 halamanAssessment Diagnosis Planning Intervention Rationale EvaluationFranz RolfBelum ada peringkat
- Drug Study For Cefazolin Drug Data Classificat Ion Mechani SM of Action Indicatio Ns Contraindica Tions Adverse Effect Nursing Responsibil ItiesDokumen2 halamanDrug Study For Cefazolin Drug Data Classificat Ion Mechani SM of Action Indicatio Ns Contraindica Tions Adverse Effect Nursing Responsibil ItiesCarl J.Belum ada peringkat
- Assessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationDokumen3 halamanAssessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationCrissa AngelBelum ada peringkat
- Drug StudyDokumen1 halamanDrug StudycliffordbuenoBelum ada peringkat
- Im Case Study 04Dokumen49 halamanIm Case Study 04Shaine BalverdeBelum ada peringkat
- Tetanus PathoDokumen3 halamanTetanus PathoElisha Gine AndalesBelum ada peringkat
- Mycophenolate Mofetil (Cellcept) and Mycophenolate Sodium (Myfortic)Dokumen3 halamanMycophenolate Mofetil (Cellcept) and Mycophenolate Sodium (Myfortic)Riksan RiksanBelum ada peringkat
- Mastectomy Case StudyDokumen9 halamanMastectomy Case StudyAura Regene AtienzaBelum ada peringkat
- Emergency Laparotomy: Patient Information FactsheetDokumen4 halamanEmergency Laparotomy: Patient Information FactsheetMuhammad RizqiBelum ada peringkat
- Consent Transsphenoidal SurgeryDokumen10 halamanConsent Transsphenoidal SurgeryAbhinav GuptaBelum ada peringkat
- Regional Anesthesia in The Patient Receiving Antithrombotic or Thrombolytic TherapyDokumen64 halamanRegional Anesthesia in The Patient Receiving Antithrombotic or Thrombolytic TherapyAlejandro CespedesBelum ada peringkat
- Health6q4Dokumen80 halamanHealth6q4Pretpret Arcamo BanlutaBelum ada peringkat
- Lab ManualDokumen4 halamanLab ManualSagar AryalBelum ada peringkat
- Encephalitis ChildDokumen8 halamanEncephalitis ChildJeane SuyantoBelum ada peringkat
- Lower Gastrointestinal Series (Colonoscopy) : Nursing Skills Output (Nso)Dokumen3 halamanLower Gastrointestinal Series (Colonoscopy) : Nursing Skills Output (Nso)Grant Wynn ArnucoBelum ada peringkat
- Laporan Bulanan Lb1: 0-7 HR Baru LDokumen20 halamanLaporan Bulanan Lb1: 0-7 HR Baru LOla SarlinaBelum ada peringkat
- Drugs Name of Heterocyclic CompoundsDokumen4 halamanDrugs Name of Heterocyclic CompoundsNAZIM10728233% (6)
- SP PaperDokumen10 halamanSP Paperapi-506783921Belum ada peringkat
- 1 Revised Food Borne Illness Lecture 1Dokumen5 halaman1 Revised Food Borne Illness Lecture 1Tarequl Islam NishadBelum ada peringkat
- Usmle SuperDokumen239 halamanUsmle SupermaksventileBelum ada peringkat
- Hubungan Ketepatan Penulisan Informasi Diagnosis Dengan Keakuratan Kode Diagnosis Kasus Obstetry Di Rumah Sakit Umi Barokah BoyolaliDokumen5 halamanHubungan Ketepatan Penulisan Informasi Diagnosis Dengan Keakuratan Kode Diagnosis Kasus Obstetry Di Rumah Sakit Umi Barokah BoyolaliirmasariBelum ada peringkat
- Patient'S Bill of Rights: MedsurgDokumen3 halamanPatient'S Bill of Rights: MedsurgIvy VillalobosBelum ada peringkat
- Sephan Eve-In - Intensive - Care - Transport - VentilationDokumen4 halamanSephan Eve-In - Intensive - Care - Transport - VentilationzorgglubBelum ada peringkat
- Proceeding Ilmu KesehatanDokumen183 halamanProceeding Ilmu KesehatanIim Rimba100% (1)
- BFSA-Volume 46-Issue 1 - Page 647-657Dokumen11 halamanBFSA-Volume 46-Issue 1 - Page 647-657mizranitaBelum ada peringkat
- 1 Latifah Jehloh - งานนำเสนอDokumen41 halaman1 Latifah Jehloh - งานนำเสนอAisyahBelum ada peringkat
- Uporaba Metoda Palijativne Skrbi U Djece Implementation of Palliative Care Methods in ChildrenDokumen7 halamanUporaba Metoda Palijativne Skrbi U Djece Implementation of Palliative Care Methods in ChildrenMoonyBelum ada peringkat
- Introduction To BioethicsDokumen33 halamanIntroduction To BioethicsReymart BolagaoBelum ada peringkat
- Pemicu 6 Blok Saraf Dan KejiwaanDokumen44 halamanPemicu 6 Blok Saraf Dan KejiwaanTommy WidjajaBelum ada peringkat
- Roles & Responsibilities of CRADokumen26 halamanRoles & Responsibilities of CRANaresh Kumar RapoluBelum ada peringkat
- StentsDokumen4 halamanStentsChitresh MotwaniBelum ada peringkat
- Week 4 Ethics Decision MakingDokumen59 halamanWeek 4 Ethics Decision Makingmaha abdallahBelum ada peringkat
- Continuing Education Activity: HypospadiasDokumen6 halamanContinuing Education Activity: HypospadiasMaulani Nurlatifah100% (1)
- Oral Lichen PlanusDokumen28 halamanOral Lichen PlanusParul SinghBelum ada peringkat
- Medical Physics and Biomedical EngineeringDokumen743 halamanMedical Physics and Biomedical Engineeringwildoapriza100% (1)
- Evidence-Based Practice Fact SheetDokumen3 halamanEvidence-Based Practice Fact Sheetmohamedwhatever100% (2)
- Version Structures and Functions of Living Organisms 8.L.1.1Dokumen28 halamanVersion Structures and Functions of Living Organisms 8.L.1.1Marianna HernandezBelum ada peringkat
- Pectus Carinatum Pigeon ChestDokumen2 halamanPectus Carinatum Pigeon ChestWulanSyafitriBelum ada peringkat
- The Role of The Gut Microbiota in SepsisDokumen9 halamanThe Role of The Gut Microbiota in SepsisSyahrul HamidBelum ada peringkat