Surgical Options For People With Type 2 Diabetes
Diunggah oleh
joseneves1987Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Surgical Options For People With Type 2 Diabetes
Diunggah oleh
joseneves1987Hak Cipta:
Format Tersedia
Surgical options for people with type 2 diabetes: a Review of Current and emerging therapies
David C.W. Lau MD PhD FRCPC
Departments of Medicine, Biochemistry and Molecular Biology Julia McFarlane Diabetes Research Centre Diabetes and Endocrine Research Group University of Calgary Calgary, Alberta
iNtroduCtioN
The obesity epidemic continues to escalate the global prevalence of type 2 diabetes (1). Currently, 258 million people worldwide live with diabetes, and 90 to 95% of them have type 2 diabetes. By 2030, the figure is estimated to exceed 438 million (2). In Canada, >2 million adults are affected by diabetes; indeed, every 10 minutes another Canadian will be diagnosed with the disease. The personal and economic costs of diabetes are staggering; if left unchecked, the financial burden of diabetes is estimated to be $16.9 billion by 2020, which will surely bankrupt the healthcare system (3). Diabetes has truly become the tsunami of chronic diseases (2).
iabetes is a progressive disease. The hallmark metabolic abnormality of diabetes is hyperglycemia, which is known to be associated with substantive increases in morbidity and mortality. Achieving normal or near-normal glycemic control is associated with a powerful reduction in microvascular complications in both type 1 and type 2 diabetes (4). Intensive glycemic control has been shown to reduce cardiovascular (CV) complications in type 1 diabetes (5); unfortunately, several large clinical trials have failed to demonstrate similar benefits of intensive glycemic control on cardiovascular disease (CVD) outcomes in people with type 2 diabetes (6). Nonetheless, glycemic control remains a major focus of type 2 diabetes management, together with intensive management of coexisting CV risk factors. While lifestyle modification and regular physical activity continue to be the cornerstones of treatment, a majority of people fail to achieve glycemic targets and pharmacotherapy is often required, especially as the disease progresses. Rapid advances in our knowledge of the pathophysiology of type 2 diabetes have led to the development of novel therapies, with the hope of achieving better glycemic control. The availability of novel antidiabetic
medications has provided more options and choices to customize therapeutic approaches to specific patients. An alternative innovative approach is bariatric surgery, which results in sustained body weight loss and significant improvement in obesity-related comorbidities, most notably diabetes. By using a case-based approach to the management of hyperglycemia, this article will assist healthcare providers in navigating through the various treatment options to select the most appropriate interventions for their patients with type 2 diabetes who struggle with obesity. You saw Daniel in the office shortly after his annual medical examination and counselled him regarding weight loss to improve his glycemic and metabolic control. You advised him to follow the recommendations of the Canadian Diabetes Association (CDA) clinical practice guidelines: increase his physical activity level to 30 minutes daily at least 5 days per week and decrease food portion sizes that would amount to a decrease of ~350 kcal per day (7,8). Lifestyle modification has broad benefits that extend beyond improvement of glycemic and metabolic control (7-9). You also discussed with him the need for additional pharmacotherapy to reduce his glycated hemoglobin (A1C) to 7.0%.
Canadian Diabetes / Le Diabte au Canada
autumn 2010
CAsE studY: dANiEL
Patient history and presentation
5 6-year-old truck driver with type 2 diabetes for 5 years L ongstanding history of obesity (since his early 20s) Married and lives a sedentary lifestyle Medication: metformin 1000 mg BID Body mass index (BMI): 38.1 kg/m2 Waist circumference: 121 cm Blood pressure (BP): 135/85 mm Hg Heart bpm rate: 80 P hysical examination: unremarkable, other than abdominal obesity N o history or evidence of microvascular or macrovascular complications L aboratory values: fasting plasma glucose (FPG) 8.0 mmol/L; glycated hemoglobin (A1C) 7.8% F asting lipid profile: total cholesterol 5.3 mmol/L; triglycerides 1.9 mmol/L; high-density lipoprotein cholesterol (HDL-C) 1.0 mmol/L; low-density lipoprotein cholesterol (LDL-C) 3.9 mmol/L No microalbuminuria
Editor-in-Chief Danile Pacaud MD FRCPC Calgary, Alberta Associate Editors Sarah Capes MD MSc FRCPC Victoria, British Columbia J. Robin Conway MD Smiths Falls, Ontario Sara Meltzer MD FRCPC Montreal, Quebec Managing Editor Susan Ball Design Comet art + design Publications Coordinator Ryan Moffat Translation Claude Filteau
Lynn Nabata MA RD CDE Victoria, British Columbia Diana Sherifali RN PhD CDE Hamilton, Ontario
The Canadian Diabetes Association has a careers site especially for you! Job opportunities within the diabetes community, including positions for nurses, educators and healthcare specialists, are available for your review today. Visit diabetes.ca/careers and find the right job for you.
Canadian Diabetes/le Diabte au Canada is published by the Canadian Diabetes Association. All articles published in Canadian Diabetes are the sole opinions of the authors and are not necessarily endorsed by the Canadian Diabetes Association. Copyright Canadian Diabetes Association, 2010; all rights reserved. Reproduction of this publication in whole or in part is prohibited without the written consent of the Publisher. Change of address notices to: Canadian Diabetes Association 1400-522 University Avenue Toronto, Ontario M5G 2R5 Canada Post Publication agreement number 40063447. ISSN0841-9388 Research and clinical experience are continually adding to medical knowledge of diagnosis, treatments and drug therapies. When authors refer to drug therapies, indications and/or dosage schedules, reference to product monograph and prescribing information is suggested to assure use of these products in accordance with the manufacturers recommendations. Reference in some articles to products by their trademark names without the trademark designation is not to be interpreted that the products or tradenames or trademarks are in the public domain.
Daniel heard from his friend that bariatric surgery is a new option for the treatment of type 2 diabetes, and wondered if he might be a candidate. Before answering his question, you reviewed with him the targets for glycemic and metabolic control, as well as current and emerging pharmacotherapies for type 2 diabetes.
GLYCEMiC CoNtroL ANd CV CoMPLiCAtioNs
Epidemiological analyses from the United Kingdom Prospective Diabetes Study (UKPDS) suggest that each 1% in A1C lowering is associated with a 30% reduction in microvascular complications. Clinical trial data regarding the benefits of glucose lowering and macrovascular disease remain controversial. In 2008, results from 3 large glucose-lowering studies (Action to Control Cardiovascular Risk in Diabetes [ACCORD], Action in Diabetes and Vascular Disease [ADVANCE] and Veterans Affairs Diabetes Trial [VADT]) failed to demonstrate reductions in CV events with improved glycemic control (6,10-12). A recent meta-analysis of 5 large glucose-lowering trials indicated that a 0.9% reduction in A1C resulted in a 15% reduction in coronary artery disease risk (13). Furthermore, the UKPDS 10-year follow-up study concluded that intensive glycemic control in the sulfonylureainsulin group early in the disease resulted in a sustained legacy effect in reducing death from any cause (9%), microvascular disease (24%) and risk of myocardial infarction (15%) (14). Significant risk reductions also
persisted in the metformin-treated group: death from any cause (27%), any diabetes-related endpoint (21%) and risk of myocardial infarction (33%) (14). Thus, it is clear that glucose lowering is beneficial in reducing microvascular and macrovascular complications in people with type 2 diabetes. Optimal glycemic control in the early phase of the disease appears to be associated with longterm benefits on CVD risk, the so-called legacy effect. According to the 2008 CDA clinical practice guidelines, the glycemic targets recommended for most people with type 1 or type 2 diabetes are: fasting plasma glucose (FPG) 4.07.0 mmol/L; 2-hour postprandial PG 5.010.0 mmol/L; and A1C 7.0% (15).
PhArMACothErAPY For tYPE 2 diABEtEs
Metformin is recommended as first-line therapy when lifestyle measures fail to achieve glycemic targets (4). In Daniels case, metformin monotherapy was inadequate so combination therapy should be considered, along with reinforcements of lifestyle modification (4). With respect to pharmacotherapy, an oral antidiabetic agent from any of the 5 available classes can be added to metformin therapy (Table 1). Unfortunately, the CDA clinical practice guidelines do not provide specific guidance on the choice of add-on oral agents. You carefully reviewed with Daniel the advantages and
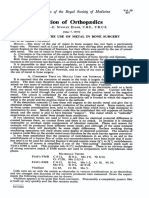
Table 1. Summary of glucose-lowering interventions for the treatment of type 2 diabetes
Interventions
Lifestyle modification Biguanide Sulfonylureas
Generic name (alphabetical order)
Metformin Chlorpropamide Gliclazide Glimepiride Glyburide Nateglinide Repaglinide Pioglitazone Rosiglitazone
A1C g (%)
1.02.0 1.02.0 1.02.0
Advantages
Broad benefits Weight neutral Rapid effect
Disadvantages
Insufficient for most within first few years following diagnosis GI side effects, contraindicated with renal insufficiency (eGFR <30 mL/min) Weight gain, hypoglycemia (especially with glyburide or chlorpropamide), lack of long-term durability (secondary failure) Weight gain, TID dosing, hypoglycemia, expensive
References
7-9 4,44 4,44
Meglitinides TZDs
0.51.5 0.52.0
Rapid effect
4,44 4,21,44
Improved lipid profile, Slow onset, fluid retention, weight gain, potential decrease in CHF, bone fractures, expensive, potential MI (pioglitazone) increase in MI (rosiglitazone) Frequent GI side effects, TID dosing GI side effects (orlistat), contraindicated in CVD (sibutramine), expensive
Alpha-glucosidase Acarbose inhibitor Weight loss agents DPP-4 inhibitors Orlistat Sibutramine Saxagliptin Sitagliptin Liraglutide Detemir Glargine NPH
0.50.75 Weight neutral 0.50.75 Weight loss, no hypoglycemia
4,18,44 4,17 4,24
0.50.75 Weight neutral, Expensive, long-term safety not no hypoglycemia, OD, established no dose titration 0.51.5 1.53.5 Weight loss, no hypoglycemia, OD Rapid effect, no dose limit, improved lipid profile Injection, expensive, long-term safety not established Hypoglycemia, weight gain, injections, expensive (basal analogues) OD = once daily TID = three times daily TZD = thiazolidinedione
GLP-1 receptor agonist Insulin
4,24,25 4
CHF = congestive heart failure CVD = cardiovascular disease DPP-4 = dipeptidyl peptidase-4 eGFR = estimated glomerular filtration rate
GI = gastrointestinal GLP-1 = glucagon-like peptide-1 MI = myocardial infarction NPH = neutral protamine Hagedorn
disadvantages of the 5 classes of oral agents. The choice of antidiabetic agent should be predicated on its efficacy, safety, tolerability and cost. The efficacy of all antidiabetic agents is dependent on the baseline A1C values, e.g. a majority of the agents would reduce A1C by ~11.5% at a baseline A1C of 8.0%. The 2 exceptions to this caveat are alpha-glucosidase inhibitors and anti-obesity agents, where the expected A1C reduction is 0.50.75% (16,17). Alpha-glucosidase inhibitors reduce the digestion and absorption of carbohydrates and are effective agents in lowering postprandial hyperglycemia. Acarbose is the only oral agent in the Canadian-led Study to Prevent Non-Insulin-Dependent Diabetes Mellitus (STOP-NIDDM) that has been shown to reduce CV events in people with impaired glucose tolerance who subsequently developed type 2 diabetes (16,18). It is a nonsystemic and safe medication that is particularly useful in the early stages of diabetes. Unfortunately, it is used sparingly in North America, primarily because of its gastrointestinal mode of action, which can cause flatulence and gastrointestinal upset.
The choice of antidiabetic agent should be predicated on its efficacy, safety, tolerability and cost.
Among the insulin secretagogues, sulfonylurea agents are widely prescribed because of their efficacy and low cost. Gliclazide and glimepiride are preferred to glyburide, as they are associated with less hypoglycemia and subsequent weight gain, and history of CVD (19). Meglitinides are short-acting insulin secretagogues that are also associated with less hypoglycemia and weight gain. Their disadvantages include more frequent administration with meals, cost and lack of formulary coverage in some provinces. Thiazolidinediones (TZDs) are insulin-sensitizing agents that lower fasting and postprandial hyperglycemia. TZDs are peroxisome proliferator-activator receptor agonists and potent inducers of preadipocyte differentiation. TZDs also augment insulin sensitivity, at least partly through stimulation of adiponectin expression and secretion by adipocytes and formation of new adipocytes that are more insulin sensitive. Hence, TZDs improve insulin sensitivity while paradoxically inducing an increase in body fat mass and
redistribution of fat from the visceral to subcutaneous depots. The glucose-lowering efficacy of TZDs is comparable to that of metformin and insulin secretagogues. Importantly, data from A Diabetes Outcome Progression Trial (ADOPT) suggested that the TZD rosiglitazone was superior to metformin and glyburide for long-term glycemic control (20). Rosiglitazone and pioglitazone are the approved TZDs in Canada and have similar efficacies. Their adverse side effects include weight gain, fluid retention, congestive heart failure and non-vertebral fractures in women. Recent studies raised controversies on the association of rosiglitazone, but not pioglitazone, with increased CV events (21). While awaiting definitive answers on the CV effects associated with long-term use of rosiglitazone or pioglitazone in the multicentre Thiazolidinedione Intervention with Vitamin D Evaluation (TIDE) trial, clinicians have the option of either discontinuing rosiglitazone or switching patients to pioglitazone, which has not been plagued by controversy, in the treatment of type 2 diabetes. Newer agents recommended by the CDA clinical practice guidelines as second-line therapy fall in the class of incretins, which are a group of gastrointestinal hormones that stimulate insulin secretion following meals (4,22,23). The 2 main endogenous incretin hormones are glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP). Both incretins are inactivated by the enzyme dipeptidyl peptidase-4 (DPP4). People with type 2 diabetes appear to have reduced incretin response to meals, which may explain in part the decreased insulin secretion and responsiveness. Saxagliptin and sitagliptin are both DPP-4 inhibitors that stimulate insulin release following a meal by prolonging the effects of endogenous incretins through enzyme inhibition (4,23,24). They also inhibit glucagon release from the pancreatic alpha cells. DPP-4 inhibitors lower glucose in a glucosedependent manner and therefore do not cause hypoglycemia and are weight neutral. A combination formulation of sitagliptin and metformin is also available as a once- or twice-daily regimen. Both DPP-4 inhibitors have few side effects and are well-tolerated. Their long-term safety and side effects remain to be determined. The first incretin mimetic approved in Canada is liraglutide, an injectable GLP-1 receptor agonist (24). By raising the plasma GLP-1 to pharmacological levels, several additional physiological effects of incretins become evident. First, the central effect of appetite suppression, along with delayed gastric emptying, can lead to sustained weight loss. Second, a more potent glucoselowering effect has been documented in the head-to-head Liraglutide Effect and Action in Diabetes 3 (LEAD-3) clinical trial
comparing liraglutide with sitagliptin (25). Third, preservation of beta cells have been observed in rodent models of diabetes, which has undoubtedly heightened interest in the use of this class of drugs in the hope of changing the natural history of type 2 diabetes, which is associated with progressive beta-cell failure. Data from the UKPDS suggested that by the time the diagnosis of diabetes is made, 50% of beta-cell function is already lost (26). Incretins not only preserve but also augment beta-cell mass, which is an important consideration as a disease-modifying therapy. Nausea and gastrointestinal upset are the more common side effects reported with GLP-1 analogues. A few cases of pancreatitis have been reported with the use of exenatide, another GLP-1 analogue that has been approved in the US for over 5 years. C-cell hyperplasia has been observed in rodents in preclinical trials; however, whether this occurs in humans will require close monitoring over the long-term. Once-weekly injectable GLP-1 analogues are currently under development and will soon be available (24). Unlike TZDs, the incretin class of medications does not appear to be associated with CV safety concerns. Indeed, saxagliptin is the first antidiabetic agent to be approved by the United States (US) Food and Drug Administration following the development of new guidance on the CV safety issue related to antidiabetic agents. Nonetheless, the long-term safety data and side effects of incretins are being investigated in 2 ongoing randomized controlled studies: Trial Evaluating Cardiovascular Outcomes With Sitagliptin (TECOS) and Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus (SAVOR-TIMI). The high cost of oral DPP-4 inhibitors and injectable incretin mimetics (~$8/day) may preclude more widespread use of this new class of drugs.
surGiCAL MANAGEMENt oF tYPE 2 diABEtEs
Is bariatric surgery an increasingly attractive option for the longterm management of obesity, and especially people with obesityrelated medical complications? Bariatric surgery is currently considered for people with a BMI 40 kg/m2 and those with a BMI 35 kg/m2 who have comorbid conditions such as diabetes (27). A recent Canadian Institute of Health Information survey reported a 92% increase in bariatric procedures performed in Canadian hospitals between 20042005 and 20082009, for a total of 2385 procedures (28). Bariatric surgery is available in 8 provinces, with the majority of the procedures performed in Quebec and Ontario (28). The inpatient procedures were performed mainly on women (80%), whose average age was 43 years; the average length of stay in 20082009 was 3.4 days (28). Bariatric surgery procedures can be classified as restrictive, malabsorptive, or combined restrictive and malabsorptive. Four types of bariatric procedures are now available in Canada. Gastric bypass, or Roux-en-Y, is the gold standard procedure, whereby the size of the stomach is reduced to create a smaller pouch that is connected to a small segment of the proximal jejunum. Adjustable gastric banding is a restrictive procedure that involves the placement of an adjustable silicone band around the upper portion of the stomach to reduce its overall size. Vertical sleeve gastrectomy is a relatively new restrictive procedure: the stomach is stapled vertically, thereby removing about 85% of the original stomach area. The most technically challenging procedure is biliopancreatic diversion with duodenal switch, whereby the size of the stomach is reduced to create a sleeve-shaped stomach, which is then anastomosed to 2 segments of the small bowel. The first 3 procedures are mainly performed laparoscopically; consequently, peri- and postoperative complications are reduced drastically.
thE FiNAL Word oN ANtidiABEtiC AGENts
Currently, metformin is the first-line drug for monotherapy in type 2 diabetes, as in Daniels case. Combination therapies with insulin secretagogues, TZDs or incretins are other treatment options that can be considered for Daniel. Sulfonylurea agents have a good safety record and are inexpensive; however, hypoglycemia and weight gain are common side effects. Incretins are an attractive option because they do not cause hypoglycemia. DPP-4 inhibitors are weight neutral, whereas injectable GLP-1 analogues are associated with weight loss, which is highly desirable for people who are struggling with obesity; however, lack of long-term safety data and cost may dampen somewhat the enthusiasm for using incretins as add-on therapy to metformin.
hoW EFFECtiVE is BAriAtriC surGErY iN trEAtiNG diABEtEs?
Bariatric surgery not only results in significant and sustained weight loss, but also leads to dramatic amelioration and even remission of diabetes, improvement in blood pressure (BP) and dyslipidemia and, most notably, reduction in all-cause, CV and cancer mortality (29). A recent systematic review and metaanalysis examined the impact of bariatric surgery on type 2 diabetes. The paper included 621 studies with a total of 135 246 subjects (30). The mean age of subjects was 40.2 years, BMI was 47.9 kg/m2, 80% were women, and 22% had type 2 diabetes (30). Among the 4 surgical procedures included in the analysis,
gastric bypass was the most common (46%), followed by gastric banding (32%), gastroplasty (14%) and biliopancreatic diversion with duodenal switch (8%). A majority of the banding studies were laparoscopic (85%), whereas 60% of the gastric bypass and >80% of gastroplasty and biliopancreatic diversion with duodenal switch procedures were open. The total weight loss was 40.6 kg, or 64% of excess body weight (30). Overall, 78% of people with diabetes had resolution of the clinical manifestations of diabetes at 2 years (30).
ArE ALL surGiCAL ProCEdurEs EQuALLY EFFECtiVE?
The resolution of diabetes, defined as maintenance of normal FPG 6.0 mmol/L or A1C 6.0%, appeared to be best achieved with procedures that included intestinal bypass. The greatest resolution of diabetes was observed in patients who underwent biliopancreatic diversion with duodenal switch procedures (96%), followed by gastric bypass (80%), gastroplasty (80%) and laparoscopic adjustable gastric banding (57%) (30). The resolution or improvement in diabetes (decreased dosage of diabetes medications or more normal FPG values) appeared to persist for >2 years (Table 2). FPG, A1C, insulin levels, plasma lipid profiles and BP values also improved significantly (30,31). In a retrospective cohort study with a mean follow-up of 7.1 years, cost-specific mortality among the 9949 patients who had undergone Roux-en-Y gastric bypass surgery was decreased by 92% for diabetes (0.4 vs. 3.4 per 10 000 personyears, p=0.005) (32). Another retrospective review of 23 803 morbidly obese patients, 5047 of whom had diabetes, reported an increase in survival rates and decrease in the presence of comorbidities in the surgical group, compared with
the nonsurgical group. The survival benefits occurred as early as 6 months for patients <65 years of age and at 11 months for patients >65 years of age (32). The first randomized trial comparing surgically induced weight loss with conventional therapy for the management of type 2 diabetes was conducted in 60 obese patients (50% men) with a mean age of 47 years, BMI 37 kg/m2 and A1C 7.8% (33). The duration of diabetes was <2 years, however 28 of 30 subjects in the surgical group were using pharmacotherapy. Remission of diabetes (defined as FPG <7.0 mmol/L and A1C <6.2%) was achieved in 22 of 30 (73%) subjects at 2 years following laparoscopic adjustable gastric banding and 4 of 30 (13%) in the conventional therapy group (33). The surgical group lost 21 kg (20%) of body weight, compared with 1.5 kg (1.4%) in the conventional therapy group. Remission was largely dependent on the magnitude of weight loss, as only 12% of patients who lost 10% body weight were in remission at 2 years (Table 3). Conversely, 15% (4 of 26) of subjects who lost >10% body weight did not achieve remission (33). At 2 years, 26 of 30 surgically treated subjects were no longer taking antidiabetic agents. There was also a significant reduction in the use of antihypertensive agents and lipid-lowering medications in the surgical group, but no significant change in the conventional therapy group at 2 years (33).
WhAt ArE thE CELLuLAr MEChANisMs For iMProVEMENt oF diABEtEs FoLLoWiNG surGErY?
The mechanisms by which bariatric surgery induces diabetes remission and the accompanying improvements in medical comorbidities, including dyslipidemia and hypertension,
Table 2. Effect of bariatric surgery on body weight loss and diabetes resolution (adapted from reference 30)
Total
EBWL, % Resolution,* % <2 years, % 2 years, % 64.4 78.1 80.3 74.6
LAGB
46.2 56.7 55.0 58.3
Gastroplasty
55.5 79.7 81.4 77.5
Roux-en-Y bypass
59.7 80.3 81.6 70.9
BPD/DS
63.6 95.1 94.0 95.9
*Percentage of patients with normal FPG and A1C <6.2% A1C = glycated hemoglobin BPD/DS = biliopancreatic diversion with duodenal switch EBWL = estimated body weight loss FPG = fasting plasma glucose LAGB = laparoscopic adjustable gastric banding
Table 3. Effect of bariatric surgery on weight loss and diabetes resolution (adapted from reference 33)
WhAt is thE durABiLitY oF diABEtEs rEMissioN?
Few studies have reported follow-up on the incidence and remission rates of diabetes following bariatric surgery. The prospective, controlled Swedish Obese Subjects (SOS) study reported the longest 15-year follow-up, with a mean of 10.9 years. The SOS study involved 4047 obese subjects, of whom 2010 had undergone bariatric surgery and 2037 had received conventional therapy. Obese subjects who underwent bariatric surgery had significantly lower rates of diabetes incidence (7% vs. 24%) and higher rates of diabetes remission (36% vs. 13%) compared with subjects who received conventional therapy (29). Importantly, bariatric surgery was associated with improvement in quality of life and a significant 24% reduction in overall CV and cancer mortality (29). In a US retrospective cohort study, the adjusted long-term mortality decreased by 40% over 18 years of follow-up (mean, 7.1 years) after Roux-en-Y gastric bypass surgery (32). Christou reported that among patients in the McGill Bariatric Cohort Study who had undergone gastric bypass surgery, the rate of death from any cause decreased by 89% after a mean follow-up of 2.6 years, compared with the rate among control subjects (39). He concluded that the relative risk reduction in mortality in people with massive obesity was proportional to the magnitude of sustained weight loss induced by the various bariatric surgical procedures.
Surgery
Remission,* % (n) Achieving A1C <6.2%, % (n) Medication use, n Weight loss, % (meanSD) Excess weight loss, % Change in BMI (kg/m2) 73 (22/30) 80 (24) 4 209.4 62.5 7.4
Conventional therapy
13 (4/30) 20 (6) 22 1.44.9 4.3 0.5
*Defined as defined FPG <7.0 mmol/L and A1C <6.2% A1C = glycated hemoglobin BMI = body mass index FPG = fasting plasma glucose SD = standard deviation
cannot be attributed to sustained weight loss alone. In most cases, diabetes remission was observed within days to weeks following surgery, before any substantial weight loss had occurred (31,34). Emerging evidence suggests gut hormones play a critical role and that the type of surgical procedure performed may influence these hormones as well as the magnitude of weight loss (31,34). For example, plasma levels of ghrelin, an intestinal hormone that increases hunger and food intake, is decreased following Roux-en-Y gastric bypass surgery (35). This effect is not seen in patients following laparoscopic adjustable gastric banding procedures. Satiety hormones such as PYY and oxyntomodulin, as well as GLP-1, all of which are secreted in the small bowel, are also increased in patients who have undergone Roux-en-Y bypass surgery (35). These changes occur as early as 4 to 6 weeks after surgery, suggesting that the altered anatomy and rapid delivery of nutrients to the distal bowel stimulate their secretion (34-36). The long-term effects of Roux-en-Y bypass surgery on plasma GLP-1 levels and islet function have been investigated in a crosssectional study of 24 women. The GLP-1 response to food intake increased steadily following surgery and did not result in the development of inappropriate insulin secretion or hypoglycemia over time (37). Beta-cell function significantly improved following surgically induced sustained weight loss, and both insulin hypersecretion and insulin resistance were normalized following bariatric surgery (31,35-38).
Emerging evidence suggests gut hormones play a critical role and that the type of surgical procedure performed may influence these hormones as well as the magnitude of weight loss.
WhAt ArE thE short- ANd LoNG-tErM surGiCAL CoMPLiCAtioNs?
When performed on appropriate patients at experienced centres, bariatric surgery is associated with relatively low morbidity and mortality. Two systematic reviews demonstrated that overall
operative mortality was 0.28% (0.1% for purely restrictive procedures, 0.5% for gastric bypass and 1.1% for biliopancreatic diversion with duodenal switch) (30,40). Generally, laparoscopic procedures were associated with significantly lower peri- and postoperative complications. Short-term complications and perioperative mortality rates were lowest with laparoscopic adjustable gastric banding, which is also technically less demanding. In addition, operating time was shorter as well as lengths of hospital stay. In experienced surgical centres, the procedure is performed as day surgery and patients are discharged within a few hours. However, long-term complications and reoperation rates were more common with laparoscopic adjustable gastric banding procedures. Port leakage and displacement, band slippage and erosion are common reasons for reoperation. Gall bladder problems and incisional hernias were relatively uncommon long-term complications. Bowel obstruction was the most common long-term complication of gastric bypass surgery (40). Micronutrient vitamin deficiencies are common following bariatric surgery, more so with gastric bypass than with banding procedures, due to malabsorption. Iron deficiency and, less commonly, fat-soluble vitamin deficiencies can also occur. Supplementation with multivitamins is recommended for people who have undergone bariatric surgery. It is important to advise patients that they must modify their nutritional intake following surgery. One of the common adverse effects from restrictive and malabsorptive procedures is dumping syndrome, which can occur in patients who do not change their diets. The rapid delivery of simpler sugars into the small bowel creates an osmotic load, causing adrenergic stimulation and resulting in such vasomotor symptoms as palpitations, confusion or even syncope (31,40). A rare complication associated with Roux-en-Y gastric bypass surgery is postprandial hyperinsulinemic hypoglycemia (41,42). Symptoms include palpitations, anxiety, tremor, diaphoresis and hunger pangs. In severe cases, symptoms of neuroglycopenia (e.g. confusion, seizure and loss of consciousness) can occur. Symptoms usually present 1 to 2 years after surgery, typically after dietary changes and weight loss have been achieved (41,42). Dietary modification, i.e. frequent, small meals low in carbohydrate and glycemic index, with higher protein and saturated fat content, usually results in clinical improvement. Pharmacotherapy with acarbose, somatostatin analogues and diazoxide has met with success in a majority of patients. However, those who do not respond to pharmacological
intervention require partial pancreatectomy to manage the severe symptoms. The cause of hyperinsulinemic hypoglycemia is not well understood, but may be related to elevated incretin hormones, notably GLP-1 (42). Based on currentalbeit largely observationalevidence, Roux-en-Y gastric bypass surgery is associated with greater weight loss, diabetes resolution and improvement, and improvement in other obesity-related comorbidities than laparoscopic adjustable gastric banding (40). Meanwhile, bariatric surgery for type 2 diabetes has received endorsement as a research priority and a potential treatment option by a number of healthcare organizations, including the American Diabetes Association and the European Association for the Study of Diabetes (43).
is BAriAtriC surGErY Cost EFFECtiVE?
The cost of bariatric surgery in Canada varies widely, ranging from $15 000 for laparoscopic adjustable gastric banding to $20 000 25 000 for laparoscopic Roux-en-Y gastric bypass. Laparoscopic adjustable gastric banding is not a medically insurable procedure and its cost is not covered by provincial health insurance plans. Physician follow-up visits and band adjustments are additional costs. While the cost effectiveness of bariatric surgery for diabetes management has not been published, early estimates suggest that it may be more cost effective than conventional therapy, especially in patients who undergo the procedure early in the course of the disease. At the First Canadian Summit on Surgery for Type 2 Diabetes held in Montreal, Quebec, in May 2010, Pierre-Yves Crmieux PhD presented preliminary data on the cost effectiveness of bariatric surgery vs. conventional medical therapy for type 2 diabetes. It was estimated that weight loss surgery will pay for itself after only 2 to 3 years (P-Y Cremieux, oral communication, June 2010).
AdVANtAGEs ANd disAdVANtAGEs oF BAriAtriC surGErY For diABEtEs MANAGEMENt
Sustained weight loss, improvement in diabetes and metabolic control, and greater quality of life are the principal advantages of bariatric surgery for type 2 diabetes management (Table 4). While diabetes remission and improvement rates are high with bariatric surgery, longer-term data on its efficacy and safety, and comparative trials on the various surgical procedures, are still needed. The future for diabetes surgery is promising, and merits further
10
Table 4. Bariatric surgery for type 2 diabetes: Advantages and disadvantages
guidelines for the prevention and management of diabetes in Canada. Pharmacologic management of type 2 diabetes. Can J Diabetes. 2008;32(suppl 1):S53-S61. 5. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653. 6. Skyler JS, Bergenstal R, Bonow RO, et al. Intensive Glycemic Control and the Prevention of Cardiovascular Events: Implications of the ACCORD, ADVANCE, and VA Diabetes Trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Diabetes Care. 2009;32:187-192. 7. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Nutrition therapy. Can J Diabetes. 2008;32(suppl 1):S40-S45. 8. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Physical activity and diabetes. Can J Diabetes. 2008;32(suppl 1): S37-S39. 9. The Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care. 2007;30:1374-1383. 10. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545-2559. 11. ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560-2572. 12. Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2008; 360:129-139. 13. Ray KK, Seshasai SR, Wijesuriya S, et al. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: a meta-analysis of randomised controlled trials. Lancet. 2009;373:1765-1772. 14. Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577-1589. 15. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Targets for glycemic control. Can J Diabetes. 2008;32 (suppl 1):S29-S32.
Advantages
ustained long-term weight S loss >10% ore patients achieve M glycemic and metabolic targets eduction in antidiabetic R medications No hypoglycemia May be cost effective
Disadvantages
urgical complications S (short- and long-term) emission not achieved in R all patients who achieved >10% weight loss Long surgical wait list equires long-term follow-up R ong-term efficacy and safety L data not available
research and attention as a feasible alternative to conventional therapy in some patients with diabetes. Randomized, controlled comparative trials with adequate sample sizes and longer followup periods are also needed to determine the optimal bariatric procedure for diabetes resolution and improvement.
thE FiNAL Word oN dANiELs GLYCEMiC MANAGEMENt
Daniel has had diabetes for 5 years and still has residual beta-cell function that will respond well to either medical or surgical therapies. Lifestyle modification, along with combination therapy with metformin and an incretin agent, are the logical next steps. Insulin therapy can be considered as add-on therapy, should his diabetes progress with worsening glycemic control. The benefits and operative risks of surgery, efficacy of the various procedures, costs, and short- and long-term complications must be explained to Daniel, to ensure he understands that his diabetes may vastly improve but will not be cured. Should he decide on surgery, laparoscopic Roux-en-Y gastric bypass appears to be the optimal procedure in achieving much greater and sustained weight loss than medical therapy, as well as improved metabolic control over the long-term.
rEFErENCEs
1. 2. 3. 4. Lau DCW. Evidence-based Canadian obesity clinical practice guidelines: Relevance to diabetes management. Can J Diabetes. 2007;31:148-152. Lau DCW. Fighting diabetes: The tsunami of noncommunicable diseases. Can J Diabetes. 2009;33:348-349. Lau DCW. The cost of diabetes: A game changer. Can J Diabetes. 2010;34:16-18. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2008 clinical practice
11
16. Chiasson JL, Josse RG, Gomis R, et al. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359:2072-2077. 17. Rucker D, Padwal R, Li SK, et al. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007;335:1194-1199. 18. Chiasson JL, Josse RG, Gomis R, et al. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290: 486-494. 19. Pantalone KM, Kattan MW, Yu C, et al. The risk of overall mortality in patients with type 2 diabetes receiving glipizide, glyburide, or glimepiride monotherapy: a retrospective analysis. Diabetes Care. 2010;33:1224-1229. 20. Kahn SE, Haffner SM, Heise MA, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355:2427-2443. 21. Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007; 356:2457-2471. 22. Buse JB, Rosenstock J, Sesti G, et al. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet. 2009;374:39-47. 23. Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696-1705. 24. Lovshin JA, Drucker DJ. Incretin-based therapies for type 2 diabetes mellitus. Nat Rev Endocrinol. 2009;5:262-269. 25. Pratley RE, Nauck M, Bailey T, et al. Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet. 2010;375:1447-1456. 26. Holman RR. Assessing the potential for alpha-glucosidase inhibitors in prediabetic states. Diabetes Res Clin Pract. 1998;40(suppl):S21-S25. 27. Lau DCW, Douketis JD, Morrison KM, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ. 2007;176:S1-S13. 28. Arkinson J, Ji H, Fallah S, et al. CIHI survey: bariatric surgery in Canada. Healthc Q. 2010;13:14-17. 29. Sjstrm L, Narbro K, Sjstrm CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741-752. 30. Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248-256.
31. Frachetti KJ, Goldfine AB. Bariatric surgery for diabetes management. Curr Opin Endocrinol Diabetes Obes. 2009;16:119-124. 32. Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753-761. 33. Dixon JB, OBrien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299:316-323. 34. Rubino F, Moo TA, Rosen DJ, et al. Diabetes surgery: a new approach to an old disease. Diabetes Care. 2009;32(suppl 2):S368-S372. 35. Korner J, Bessler M, Cirilo LJ, et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90: 359-365. 36. Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244:741-749. 37. Vidal J, Nicolau J, Romero F, et al. Long-term effects of Roux-en-Y gastric bypass surgery on plasma glucagon-like peptide-1 and islet function in morbidly obese subjects. J Clin Endocrinol Metab. 2009; 94:884-891. 38. Camastra S, Manco M, Mari A, et al. Beta-cell function in morbidly obese subjects during free living: long-term effects of weight loss. Diabetes. 2005;54:2382-2389. 39. Christou N. Impact of obesity and bariatric surgery on survival. World J Surg. 2009;33:2022-2027. 40. Tice JA, Karliner L, Walsh J, et al. Gastric banding or bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med. 2008;121:885-893. 41. Service GJ, Thompson GB, Service FJ, et al. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med. 2005;353:249-254. 42. Goldfine A, Mun E, Patti M. Hyperinsulinemic hypoglycemia following gastric bypass surgery for obesity. Curr Opin Endocrinol Diabetes. 2006;13:419-424. 43. Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg. 2010;251:399-405. 44. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. A consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193-203.
12
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- PY 5.16: Record Arterial Pulse Tracing Using Finger Plethysmography in A Volunteer or Simulated EnvironmentDokumen6 halamanPY 5.16: Record Arterial Pulse Tracing Using Finger Plethysmography in A Volunteer or Simulated EnvironmentADITYA SARAFBelum ada peringkat
- General Surgery NuggetsDokumen12 halamanGeneral Surgery Nuggetsamna_badar1Belum ada peringkat
- Innovations in Cardiovascular Disease ManagementDokumen183 halamanInnovations in Cardiovascular Disease ManagementGopal Kumar DasBelum ada peringkat
- AIIMS Nursing Officer Question Paper With Key 2019-1Dokumen35 halamanAIIMS Nursing Officer Question Paper With Key 2019-1shubham vermaBelum ada peringkat
- Aetcom 3.5Dokumen4 halamanAetcom 3.5Kondayoor SharadaBelum ada peringkat
- Pathophysiology Total Anterior Circulation Infarction Left Middle Cerebral Artery (TACILMCA)Dokumen2 halamanPathophysiology Total Anterior Circulation Infarction Left Middle Cerebral Artery (TACILMCA)PATHOSHOPPE100% (1)
- E.C.G Machine: by Er.U.Karthik Premkumar, H.O.D - Biomedical Engineering DepartmentDokumen36 halamanE.C.G Machine: by Er.U.Karthik Premkumar, H.O.D - Biomedical Engineering DepartmentAch ThungBelum ada peringkat
- Mandibular SwingDokumen12 halamanMandibular SwingDr. T. Balasubramanian100% (4)
- Preboard Exam Np3 Medical Surgical NursingDokumen19 halamanPreboard Exam Np3 Medical Surgical NursingBhie Bhie100% (1)
- Candidate Guide Trauma Case Fat Embolism SyndromeDokumen10 halamanCandidate Guide Trauma Case Fat Embolism SyndromevidiadityapamoriBelum ada peringkat
- Laparoscopic Drainage of Pancreatic Pseudocysts 1584 9341 11 3 8Dokumen4 halamanLaparoscopic Drainage of Pancreatic Pseudocysts 1584 9341 11 3 8ciuca bogdanBelum ada peringkat
- Core Concepts For Local RN ExamsDokumen16 halamanCore Concepts For Local RN ExamsChantilly Marie VillarinBelum ada peringkat
- Brier Ley 2020Dokumen8 halamanBrier Ley 2020kemoBelum ada peringkat
- HistologyDokumen18 halamanHistologyGlavinorBelum ada peringkat
- Color Atlas of Anterior SegmentDokumen170 halamanColor Atlas of Anterior Segmentxakos16766Belum ada peringkat
- Goniometric Reliability of Shoulder MeasurementsDokumen6 halamanGoniometric Reliability of Shoulder MeasurementssaswepakBelum ada peringkat
- ISUOG Practice Guidelines Updated Performance of 11 14 Week Ultrasound ScanDokumen17 halamanISUOG Practice Guidelines Updated Performance of 11 14 Week Ultrasound ScanhugoBelum ada peringkat
- (2014) Capnography During Cardiopulmonary Resuscitation - Current Evidence and Future DirectionsDokumen10 halaman(2014) Capnography During Cardiopulmonary Resuscitation - Current Evidence and Future DirectionsDominik Chirito PastorBelum ada peringkat
- Introduction To NeuroanatomyDokumen20 halamanIntroduction To NeuroanatomySurjagnee SannyamatBelum ada peringkat
- Definitions Opthalmology MedadDokumen10 halamanDefinitions Opthalmology MedadAhmed MansourBelum ada peringkat
- Pleural EffusionDokumen72 halamanPleural Effusionmaeliszxc kimBelum ada peringkat
- Effect of Fasting Time Before Anesthesia On Complicated Post OperativDokumen6 halamanEffect of Fasting Time Before Anesthesia On Complicated Post OperativsantiBelum ada peringkat
- Labia Minora Reconstruction Using Clitoral Hood Flaps, Wedge Excisions, and YV Advancement FlapsDokumen8 halamanLabia Minora Reconstruction Using Clitoral Hood Flaps, Wedge Excisions, and YV Advancement FlapsHazel Vivian Soliz AlconzBelum ada peringkat
- Pup Letterhead TemplateDokumen17 halamanPup Letterhead TemplateMarange, Marjorie A.Belum ada peringkat
- ACI CPG Care Adult Patients Acute TracheostomyDokumen66 halamanACI CPG Care Adult Patients Acute TracheostomyTùng KimBelum ada peringkat
- Chapter 7Dokumen7 halamanChapter 7Mia Kristhyn Calinawagan SabanalBelum ada peringkat
- 1957 Use of Metal in Bone Surgery ProcrsmedDokumen10 halaman1957 Use of Metal in Bone Surgery ProcrsmedilanBelum ada peringkat
- Benign Paraoxysmal Positional VertigoDokumen3 halamanBenign Paraoxysmal Positional VertigoPrabowoBelum ada peringkat
- Unit 6 Concet of EliminationDokumen32 halamanUnit 6 Concet of EliminationAbdur Rehman100% (1)
- UntitledDokumen2 halamanUntitledAelysa PabloBelum ada peringkat