Oocyte Transfer and Gamete Intrafallopian Transfer in The Mare
Diunggah oleh
Laura Margarita Gonzalez HilarionDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Oocyte Transfer and Gamete Intrafallopian Transfer in The Mare
Diunggah oleh
Laura Margarita Gonzalez HilarionHak Cipta:
Format Tersedia
Animal Reproduction Science 8283 (2004) 617624
Oocyte transfer and gamete intrafallopian transfer in the mare
E.M. Carnevale
Department of Biomedical Sciences, Colorado State University, Fort Collins, CO 80523, USA
Abstract Methods for the collection and transfer of equine oocytes have been developed, and uses of these techniques have resulted in new clinical and research possibilities. Because oocyte transfer avoids reproductive problems associated with the oviduct, uterus, and cervix, pregnancies can be produced from many mares that cannot carry a pregnancy or produce embryos. Oocytes for clinical transfers are usually collected from preovulatory follicles and cultured for a short interval or transferred directly into a recipients oviduct. For oocyte transfer, the recipient is inseminated within the uterus. A large number (1109 to 2109 ) of motile sperms are preferred for inseminations. In contrast, sperm and oocyte are transferred into the oviduct during gamete intrafallopian transfer (GIFT). Therefore, a lower number (1105 to 2105 ) of sperm can be used. Potentially, GIFT could be used in situations where sperm numbers are limited. Use of oocyte transfer and GIFT in clinical and research settings will aid us in understanding the interactions between oocyte, sperm, and oviduct in the equine. 2004 Published by Elsevier B.V.
Keywords: Equine; Oocyte; Assisted reproduction; Oocyte transfer; GIFT
1. Introduction During oocyte transfer, a donors oocyte is placed in a recipients oviduct, and the recipient is inseminated within the uterus. When sperm are placed within the oviduct with the oocyte, the procedure is called gamete intrafallopian transfer (GIFT). For oocyte transfer and GIFT, fertilization and development of the embryo and fetus occur within the recipient. Technologies to collect and transfer oocytes have provided new methods to study the interaction of oocyte, sperm, and oviduct for research purposes. Oocyte transfer has also been used as a clinical procedure for subfertile mares that cannot provide viable embryos for transfer because of reproductive failure associated with abnormalities of ovulation, oviduct function, uterine health, or cervical function. GIFT has the potential to be used for subfertile
Tel.: +1-970-491-8626; fax: +1-970-491-7005. E-mail address: emc@colostate.edu (E.M. Carnevale).
0378-4320/$ see front matter 2004 Published by Elsevier B.V. doi:10.1016/j.anireprosci.2004.04.002
618
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
stallions with low sperm production because a low number of sperm are placed within the oviduct. Development of procedures for the collection and transfer of oocytes has resulted in new clinical and research possibilities for the equine. 2. Clinical use of oocyte transfer The rst foal was born after an oocyte transfer in the late 1980s (McKinnon et al., 1988). However, the procedure was not efcient. Fifteen oocytes were transferred into inseminated recipients oviduct, three oviductal embryos were collected, two pregnancies were established, and one foal (1/15, 7%) was born. The rst report of a high success rate with oocyte transfer was in 1995 (Carnevale and Ginther, 1995). At that time, the transfer of oocytes from young donor mares into inseminated recipients resulted in an embryo development rate of 92% (11/12). The procedure was not used for commercial transfers until the late 1990s (Hinrichs et al., 2000a; Carnevale et al., 2001b). Oocyte transfer has since been proven to be a useful method to obtain offspring from mares with various reproductive problems that prevent successful pregnancy or embryo donation (Carnevale et al., 2001b). Reproductive problems include ovulatory failure, uterine infections, cervical tears, and undiagnosed anomalies. For older mares and during the autumn months, the incidence of ovulatory failure is increased (Carnevale et al., 1994; Carnevale, 1998). Some mares, especially older mares, appear to repeatedly fail to ovulate. These mares have been used as successful oocyte donors, if oocytes are collected before deleterious changes occur within the follicle (Carnevale et al., 2001b). Oviductal abnormalities are difcult to diagnose; however, results of studies have suggested that sperm selection and collection of the oocyte by the oviduct can be impaired in some mares (Carnevale et al., 1993; Scott et al., 1995). Oviductal masses have been described in the oviducts of mares (Tsutsumi et al., 1979; Liu et al., 1990). The potential of oviductal masses to affect fertility is not known. While oviductal pathology may be uncommon and is difcult to diagnose, uterine pathology is commonly diagnosed in mares. Treatment of uterine infections can be expensive and unsuccessful for some mares, resulting in their failure as embryo donors. Other pathology, such as cervical lacerations, cervical or uterine adhesions, or urine pooling, will affect a mares potential as an embryo donor. However in many of these cases, oocyte transfer provides a viable method to obtain offspring. One major factor, affecting success of oocyte transfer, is age of the donor. Pregnancy rates after transfer of oocytes from young mares are better than those for oocytes from old mares. When oocytes were collected from the follicles of young mares (610 years) and old mares (2026 years) and transferred into the oviducts of young recipients (37 years), signicantly more oocytes from young than old donors developed into embryonic vesicles (11/12, 92% versus 8/26, 31%) (Carnevale and Ginther, 1995). More morphological anomalies were observed in oocytes from old than young mares when evaluated with light and electron microscopy (Carnevale et al., 1999b). When donors for clinical transfers were old, pregnancies were obtained; however, more transfers were required to produce a viable pregnancy when oocytes were collected from old versus young donors. During a breeding season, pregnancies were established for three of four donors 16 years after only one transfer. In contrast, a pregnancy was established for only one of six donors 20 years after
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
619
one transfer, and a pregnancy was not obtained for one old donor after repeated transfers. Between two and four transfers were required to establish pregnancies in the other old mares (Carnevale et al., 2001b). Pregnancy rates for commercial transfers, using older donors and semen of variable quality, ranged from 27 to 40% per transfer (Carnevale et al., 2001b,c). In contrast, experimental transfers done under similar conditions using oocytes from young mares and fertile stallions resulted in pregnancy rates between 54 and 83% per transfer (Carnevale et al., 2001c). However, one or more pregnancies were obtained for at least 80% of the oocyte donors during the breeding season in a clinical program, with donors in the program having long (mean of 7 years) histories of reproductive failure in breeding and embryo transfer programs (Carnevale et al., 2001b).
3. Oocyte collection Most oocytes that are transferred for clinical or research purposes are collected from preovulatory follicles. Therefore, oocyte maturation occurs in vivo; and the in vitro effects of follicle selection and oocyte maturation are minimized. Oocyte collections are scheduled based on the time of administration of hCG or a GnRH analog to the donor. The criteria that are used for hCG or GnRH administration are: (i) a follicle >35 mm in diameter, (ii) relaxed cervical and uterine tone, and (iii) uterine edema or estrous behavior for at least 2 days. In our laboratory, oocytes are collected from preovulatory follicles between 24 and 36 h after the administration of hCG (15002500 IU, i.v.) to the donor or between 14 and 0 h before anticipated ovulation, respectively. Oocytes are probably collected at metaphase I or II (Bezard et al., 1997). Oocytes have been collected from the follicles of mares using laparotomies (Vogelsang et al., 1986), colpotomies (Hinrichs and Kenney, 1987), ank punctures (Vogelsang et al., 1983; Palmer et al., 1986), and ultrasound-guided follicular aspirations (Bruck et al., 1992; Carnevale and Ginther, 1993; Cook et al., 1993). Flank or ultrasound-guided punctures are the most common methods of oocyte collection. Oocyte collection by ank puncture is done by manual palpation without the aid of an ultrasound machine. The technique requires that a trocar be placed through the ank musculature, ipsilateral to the preovulatory follicle and at the approximate position of the ovary. The ovary is manipulated per rectum, so that the preovulatory follicle is positioned against the end of the cannula. A needle (1215 gauge) is placed through the cannula and into the follicular antrum, and the follicular uid and oocyte are removed by gentle suction and lavage of the follicle. An ultrasound machine is used to view the procedure during transvaginal, ultrasoundguided follicular aspirations. A linear, curvilinear, or sector transducer can be used. The transducer is placed in a casing containing a needle guide and positioned within the anterior vagina, lateral to the posterior cervix and ipsilateral to the ovary containing the preovulatory follicle. Transrectal manipulations are used to position the ovary against the ultrasound transducer and needle guide. A needle (12-gauge, double lumen) is advanced within the needle guide until it punctures the vaginal and follicular walls. Follicular uid is aspirated from the follicle using a pump set at 150 mm Hg or large syringes. After removal of follicular uid, the lumen can be lavaged with between 50 and 100 ml of media, typically modied
620
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
Dulbeccos phosphate-buffered solution or an embryo ush solution containing a serum source and heparin (10 IU/ml) to prevent coagulation. Oocyte recovery rates will vary with experience of the clinician. During the last 3 years in our laboratory, collection rates of oocytes from commercial donors were 98% (331/339) per cycle and 76% (331/434) per follicle (Carnevale et al., 2003a). Media and equipment for handling the oocyte are maintained at 3839 C. Because the oocyte is surrounded by expanding cumulus cells, the cumulus oocyte complex is usually large (>1 mm), translucent, and easy to identify under a stereomicroscope. Critical evaluation of the oocyte is difcult because of the surrounding cells.
4. Oocyte culture Oocytes collected 36 h after hCG administration to the donor are ready for immediate transfer into a recipients oviduct. Oocytes collected 24 h after administration to the donor are often cultured in vitro for between 12 and 16 h before transfer. Tissue Culture Medium 199 with additions of 10% fetal calf serum, 0.2 mM pyruvate, and 50 g/ml gentamicin has been established as an acceptable medium for culture of the maturing oocyte (Carnevale and Ginther, 1995; Hinrichs et al., 1998). Oocytes have been cultured at 38.239 C in atmospheres of 5 or 6% CO2 and air. Time of oocyte collection (24h versus 36 h after administration of hCG to donors) did not affect pregnancy rates (Hinrichs et al., 2000b).
5. Oocyte transfer Cyclic and noncyclic mares have been used as oocyte recipients. When cyclic mares are used, recipients are synchronized with the donor, and the recipients own oocyte is removed by aspiration to prevent its fertilization. Noncyclic mares or mares with reduced follicular activity can be used as oocyte recipients, eliminating the need to remove the recipients oocyte. Synchronization is obtained by the administration of exogenous hormones. During the spring, anestrus and early transitional mares were used as recipients (Carnevale et al., 1999a; Carnevale et al., 2001b). During the breeding season, a high dose of a GnRH agonist (4.2 mg, deslorelin acetate) (Carnevale et al., 2001a) or a period of progesterone and estrogen (150 mg P4 and 10 mg E2 ) daily for up to 10 days followed by withdrawal (Hinrichs et al., 2000a) were used to reduce follicular development. Estradiol (25 mg daily for 37 days) was administered before insemination and oocyte transfer, and progesterone (150200 mg daily) was administered after transfer. Exogenous progesterone or progestin was required to maintain pregnancies (Carnevale et al., 2001b). Pregnancy rates after commercial transfers were similar for cyclic and noncyclic recipients (8/15, 53% and 37/93, 39%) (Carnevale et al., 2001c). Oocyte transfers are performed through standing ank laparotomies with surgical procedures similar to previously described methods for surgical embryo transfer (Squires and Seidel, 1995). After the peritoneum is punctured, the ovary is located and gently exteriorized through the incision. The oocyte is loaded into a re-polished, glass pipette with a
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
621
small volume of medium (<0.05 ml), and gently deposited within the oviduct through the infundibular os. The equine oocyte retains high fertility for approximately 12 h after a natural ovulation (Ginther, 1992). Therefore, recipients are inseminated before or directly after oocyte transfer. Pregnancies have occurred when recipients were inseminated only before (Scott et al., 2001; Maclellan et al., 2002) or after (Carnevale et al., 2000) transfer of oocytes. For most experimental transfers, recipients were inseminated approximately 12 h before and 2 h after transfer with a total of 2 109 motile sperms (Carnevale et al., 2001c). In a recent study (Carnevale et al., 2002), oocyte recipients were inseminated with semen from different stallions before and after transfer. Embryonic vesicles were collected from recipients uteri on day 16 and submitted for parentage testing. Signicantly, more transferred oocytes were fertilized by semen inseminated before versus after transfer (29/31 versus 2/31). Therefore, insemination before transfer was adequate when using semen from fertile stallions.
6. Transfer of oocytes matured in vitro In vitro fertilization and embryo culture are not very successful for the equine. Therefore, oocyte transfer has been used to determine the ability of oocytes, matured in vitro, to undergo fertilization and embryo development. In a study by Scott et al. (2001), oocytes were collected from small, diestrus follicles and from preovulatory follicles. Oocytes, collected from small follicles, were matured in vitro for 3638 h before transfer, while oocytes collected from preovulatory follicles were transferred immediately into a recipients oviduct. Embryo development rates after transfers were signicantly lower for oocytes matured in vitro versus in vivo, 9% versus 82%, respectively. Hinrichs et al. (2002) transferred multiple oocytes, matured in vitro, into the oviducts of recipient mares. Fertilization rates of nondegenerate oocytes were high, but of 87 recovered oocytes/embryos, only 16 had cleaved to 2 cells (18%). Results of the studies suggest that oocyte transfer can be used to evaluate fertilization and developmental competence of oocytes matured in vitro. Oocyte transfer has also been used for the transfer of oocytes collected from the ovaries of valuable mares that have been euthanized, or that have died. This procedure was initially attempted in 1999 (Carnevale et al., 2001b), but the rst foal, from ovaries transported across the country, was not produced until 2002 (Carnevale et al., 2003b). During the past 3 years in our laboratory, oocytes have been collected and transferred from the ovaries of 21 mares, with three healthy foals born and four ongoing, late-term pregnancies. 7. Gamete intrafallopian transfer (GIFT) Gamete intrafallopian transfer involves transfer of sperm, in addition to an oocyte, into a recipients oviduct. For oocyte transfer, intrauterine inseminations of high numbers of sperm are desirable (Carnevale et al., 2001c). However, for GIFT, substantially lower numbers of sperm can be used because the sperms are placed directly into the oviduct. Because low numbers of sperm are used and because sperms are placed near the site of fertilization,
622
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
GIFT could theoretically be used to produce pregnancies from subfertile stallions, frozen semen, and sex-sorted sperm. The rst successful GIFT in the horse was achieved in 1998 (Carnevale et al., 1999a). Since that time, GIFT has been attempted with fresh, frozen, and cooled sperm. Typically, a density gradient has been used to select a population of sperms with a high percentage of motility, and to minimize debris and seminal plasma. Between 2 and 5 105 motile sperms are pulled into a transfer pipette containing the oocyte and placed into the oviduct of a recipient mare. Using fresh semen and young oocyte donors, embryo development rates after GIFT ranged from 27 to 82% (Carnevale et al., 2000; Coutinho da Silva et al., 2001). In comparison to results using fresh semen, semen that has been cooled or frozen for GIFT was less successful in establishing pregnancies. Recent studies in our laboratory using cooled and frozen semen for GIFT resulted in pregnancy rates of 25 and 8%, respectively (Coutinho da Silva et al., 2002). Projects are ongoing to investigate the causes of limited success.
8. Conclusions The minimal success of in vitro fertilization in the equine has hindered clinical and research investigations. Methods involving transfer and fertilization in vivo, however, have proven valuable. Using oocyte transfer, interactions between oocyte, sperm, and oviduct can be studied, and factors affecting oocyte viability can be determined. Oocyte transfer has also been used to produce offspring from mares that are unsuccessful oocyte donors in clinical practices. Transfer of oocyte and sperm (GIFT) into a recipients oviduct has resulted in high embryo development rates when fresh semen was used. Further development of GIFT could result in its use for cases in which sperm numbers are limited. Findings from oocyte transfer and GIFT will increase our understanding of equine gametes and oviductal function.
Acknowledgements Research in oocyte transfer and GIFT was funded by benefactors of Preservation of Equine Gametes and the Colorado Equine Racing Commission through the Research Council of the College of Veterinary Medicine and Biomedical Sciences at Colorado State University. References
Bezard, J., Mekarska, A., Goudet, G., Duchamp, G., Palmer, E., 1997. Meiotic stage of the preovulatory equine oocyte at collection and competence of immature oocytes for in vitro maturation: effect of interval from induction of ovulation to follicle puncture. Theriogenology 47, 386. Bruck, I., Raun, K., Synnestvedt, B., Greve, T., 1992. Follicle aspiration in the mare using a transvaginal ultrasound-guided technique. Equine Vet. J. 24, 5859. Carnevale, E.M., Ginther, O.J., 1993. Use of a linear ultrasonic transducer for the transvaginal aspiration and transfer of oocytes in the mare. J. Equine Vet. Sci. 13, 331333.
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
623
Carnevale, E.M., Grifn, P.G., Ginther, O.J., 1993. Age-associated subfertility before entry of embryos into the uterus in mares. Equine Vet. J. Suppl. 15, 3135. Carnevale, E.M., Bergfelt, D.R., Ginther, O.J., 1994. Follicular activity and concentrations of FSH and LH associated with senescence in mares. Anim. Reprod. Sci. 35, 231246. Carnevale, E.M., Ginther, O.J., 1995. Defective oocytes as a cause of subfertility in old mares. Biol. Reprod. Mono. 1, 209214. Carnevale, E.M., 1998. Folliculogenesis and ovulation. In: Rantanen, N.W., McKinnon, A.O. (Eds.), Equine Diagnostic Ultrasonography. Williams & Wilkins, Baltimore, pp. 201211. Carnevale, E.M., Alvarenga, M.A., Squires, E.L., Choi, Y.H., 1999a. Use of noncycling mares as recipients for oocyte transfer and GIFT. Proceedings of the Annual Conference Society for Theriogenology, Nashville, TN, pp. 44. Carnevale, E.M., Uson, M., Bozzola, J.J., King, S.S., Schmitt, S.J., Gates, H.D., 1999b. Comparison of ooyctes from young and old mares with light and electron microscopy. Theriogenology 51, 299. Carnevale, E.M., Maclellan, L.M., Coutinho da Silva, M.A., Scott, T.J., Squires, E.L., 2000. Comparison of culture and insemination techniques for equine oocyte transfer. Theriogenology 54, 982987. Carnevale, E.M., Checura, C.H., Coutinho da Silva, M.A., Maclellan, L.J., Squires, E.L., 2001a. Use of deslorelin acetate to suppress follicular activity in mares used as recipients for oocyte transfer. Theriogenology 55, 358. Carnevale, E.M., Squires, E.L., Maclellan, L.J., Alvarenga, M.A., Scott, T.J., 2001b. Use of oocyte transfer in a commercial breeding program for mares with reproductive abnormalities. J. Am. Vet. Med. Assoc. 218, 8791. Carnevale, E.M., Maclellan, L.J., Coutinho da Silva, M.A., Checura, C.M., Scoggin, C.F., Squires, E.L., 2001c. Equine sperm-oocyte interaction: results after intraoviductal and intrauterine inseminations of recipients for oocyte transfer. Anim. Reprod. Sci. 68, 305314. Carnevale, E.M., Coutinho da Silva, M.A., Maclellan, L.J., Neves Neto, J.R., Squires, E.L., 2002. Effects of culture media and time of insemination on oocyte transfer. Theriogenology 58, 759762. Carnevale, E.M., Coutinho da Silva, M.A., Squires, E.L., 2003a. How to collect and transfer oocytes. In: Proceedings of the Annual Convention of the American Association of Equine Practitioners, New Orleans, LA, pp. 293294. Carnevale, E.M., Maclellan, L.J., Coutinho da Silva, M.A., Squires, E.L., 2003b. Pregnancies attained after collection and transfer of oocytes from ovaries of ve euthanatized mares. J. Am. Vet. Med. Assoc. 222, 6062. Cook, N.L., Squires, E.L., Ray, B.S., Cook, V.M., Jasko, D.J., 1993. Transvaginal ultrasound-guided follicular aspiration of equine oocytes. J. Equine Vet. Sci. 15, 7174. Coutinho da Silva, M.A., Carnevale, E.M., Maclellan, L.J., Preis, K.A., Squires, E.L., 2001. Embryo development rates after oocyte transfer comparing intrauterine or intraoviductal insemination and fresh or frozen semen in mares. Theriogenology 55, 359. Coutinho da Silva, M.A., Carnevale, E.M., Maclellan, L.J., Preis, K.A., Leao, K.M., Squires, E.L., 2002. Use of fresh, cooled and frozen semen during gamete intrafallopian transfer in mares. Theriogenology 58, 763766. Ginther, O.J., 1992. Reproductive Biology of the Mare, second ed. Equiservices, Cross Plains, WI, pp. 299300. Hinrichs, K., Kenney, R.M., 1987. A colpotomy procedure to increase oocyte recovery rates on aspiration of equine preovulatory follicles. Theriogenology 27, 237. Hinrichs, K., Matthews, G.L., Freeman, D.A., Torello, E.M., 1998. Oocyte transfer in mares. J. Am. Vet. Med. Assoc. 212, 982986. Hinrichs, K., Provost, P.J., Torello, E.M., 2000a. Treatments resulting in pregnancy in nonovulating, hormone-treated oocyte recipient mares. Theriogenology 54, 12851293. Hinrichs, K., Betschart, R.W., McCue, P.M., Squires, E.L., 2000b. Effect of time of follicle aspiration on pregnancy rate after oocyte transfer in the mare. J. Reprod. Fertil. Suppl. 56, 493498. Hinrichs, K., Love, C.C., Brinsko, S.P., Choi, Y.H., Varner, D.D., 2002. In vitro fertilization of in vitro-matured equine oocytes: Effect of maturation medium, duration of maturation, and sperm calcium ionophore treatment, and comparison with rates of fertilization in vivo after oocyte transfer. Biol. Reprod. 67, 256262. Liu, I.K.M., Lantz, K.C., Schlafke, S., Bowers, J.M., Enders, A.C. 1990. Clinical observaltions of oviductal masses in the mare In: Proceedings of the Annual Convention of the American Association of Equine Practitioners, Lexington, KY, pp. 4145. Maclellan, L.J., Carnevale, E.M., Coutinho da Silva, M.A., Scoggin, C.F., Bruemmer, J.E., Squires, E.L., 2002. Pregnancies from vitried equine oocytes collected from superstimulated and non-stimulated mares. Theriogenology 58, 911919.
624
E.M. Carnevale / Animal Reproduction Science 8283 (2004) 617624
McKinnon, A.O., Carnevale, E.M., Squires, E.L., Voss, J.L., Seidel Jr., G.E., 1988. Heterogenous and xenogenous fertilization of in vivo matured equine oocytes. J. Equine Vet. Sci. 8, 143147. Palmer, E., Duchamp, G., Bezard, J., Magistrini, M., King, A., Bousquet, D., Betteridge, K., 1986. Recovery of follicular uid and oocytes of mares by non-surgical puncture of the preovulatory follicle. Theriogenology 25, 178. Scott, M.A., Liu, I.K.M., Overstreet, J.W., 1995. Sperm transport to the oviducts: abnormalities and their clinical implications. In: Proceedings of the Annual Convention of the American Association of Equine Practitioners, Lexington, KY, pp. 12. Scott, T.J., Carnevale, E.M., Maclellan, L.J., Scoggin, C.F., Squires, E.L., 2001. Embryo development rates after transfer of oocytes matured in vivo, in vitro, or within oviducts of mares. Theriogenology 55, 705715. Squires, E.L., Seidel, G.E., 1995. Collection and transfer of equine embryos. Animal Reproduction and Biotechnology Laboratory Bulletin 8. Colorado State University, Fort Collins, CO, pp. 2426. Tsutsumi, Y., Suzuki, H., Takeda, T., Terami, Y., 1979. Evidence of the origin of the gelatinous masses in the oviducts of mares. J. Reprod. Fertil. 57, 287290. Vogelsang, M.M., Kreider, J.L., Potter, G.D., 1983. Recovery of pre-ovulatory equine oocytes by follicular aspiration. In: Proceedings of the 8th Equine Nutrition and Pysiology Symposium, Lexington, KY, pp. 285288. Vogelsang, M.M., Kraemer, D.C., Bowen, M.J., Potter, G.D., 1986. Recovery of equine follicular oocytes by surgical and non-surgical techniques. Theriogenology 25, 208.
Anda mungkin juga menyukai
- Handbook of Current and Novel Protocols for the Treatment of InfertilityDari EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanBelum ada peringkat
- Reproductive Technologies in AnimalsDari EverandReproductive Technologies in AnimalsGiorgio PresicceBelum ada peringkat
- Embryo TransferDokumen13 halamanEmbryo TransferGerwyn Gervacio CBelum ada peringkat
- 2023 Clinical Decision Making - Embryo GradingDokumen34 halaman2023 Clinical Decision Making - Embryo GradingPhuong Nguyen100% (1)
- Cattle Embryo Transfer Procedure PDFDokumen135 halamanCattle Embryo Transfer Procedure PDFFadli NugrahaBelum ada peringkat
- Abnormal Fertilization in ARTDokumen33 halamanAbnormal Fertilization in ARTAl Mamun100% (1)
- Sperm Freezing Protocol PDFDokumen2 halamanSperm Freezing Protocol PDFminh3010Belum ada peringkat
- Breeding Soundness Evaluation and Semen Analysis For Predicting Bull FertilityDokumen6 halamanBreeding Soundness Evaluation and Semen Analysis For Predicting Bull FertilityBahlibiBelum ada peringkat
- Hezavehei 2018Dokumen13 halamanHezavehei 2018ermianusBelum ada peringkat
- Artificial Insemination EquineDokumen16 halamanArtificial Insemination EquineSebastián Ordóñez RamírezBelum ada peringkat
- Equine PregnancyDokumen5 halamanEquine PregnancySavannah Simone PetrachenkoBelum ada peringkat
- 1 Ahamd Sarki GumelDokumen11 halaman1 Ahamd Sarki GumelAhmad Mohammed GumelBelum ada peringkat
- Cryopreservation: Anuja Kamath, M.SC Bangalore Assisted Conception CentreDokumen50 halamanCryopreservation: Anuja Kamath, M.SC Bangalore Assisted Conception CentreAl MamunBelum ada peringkat
- IETS 2018 Program Book FinalDokumen68 halamanIETS 2018 Program Book FinalCesar Augusto Camacho RozoBelum ada peringkat
- Lecture 5 Follicular Dynamics in Domestic AnimalsDokumen37 halamanLecture 5 Follicular Dynamics in Domestic AnimalsgnpobsBelum ada peringkat
- Lecture 10 Repeat Breeding in Cattle and BuffaloDokumen37 halamanLecture 10 Repeat Breeding in Cattle and BuffalognpobsBelum ada peringkat
- Lecture 2 Hormones of Reproduction in Domestic AnimalsDokumen78 halamanLecture 2 Hormones of Reproduction in Domestic AnimalsgnpobsBelum ada peringkat
- Lecture 12 Methods For Collection of Semen of Farm Animals - 10Dokumen3 halamanLecture 12 Methods For Collection of Semen of Farm Animals - 10kushal NeupaneBelum ada peringkat
- Lecture 7 Bovine InfertilityDokumen19 halamanLecture 7 Bovine InfertilitygnpobsBelum ada peringkat
- 411 Veterinary GynaecologyDokumen584 halaman411 Veterinary GynaecologyVaidika YadavBelum ada peringkat
- Textbook of Assisted Reproductive Techni PDFDokumen461 halamanTextbook of Assisted Reproductive Techni PDFjessicaBelum ada peringkat
- Intra Uterine Insemination: Dr. Suryakant HayatnagarkarDokumen47 halamanIntra Uterine Insemination: Dr. Suryakant HayatnagarkarSuryakant HayatnagarkarBelum ada peringkat
- Equine Embryo Transfer (VetBooks - Ir)Dokumen183 halamanEquine Embryo Transfer (VetBooks - Ir)felemen29Belum ada peringkat
- Assisted Reproductive Technology (ART) : and ApplicationDokumen38 halamanAssisted Reproductive Technology (ART) : and ApplicationPraluki HerliawanBelum ada peringkat
- 2006 Cryopreservation and Intracytoplasmic Sperm Injection With Bovine Eith Egg Yolk Sigma E0625Dokumen215 halaman2006 Cryopreservation and Intracytoplasmic Sperm Injection With Bovine Eith Egg Yolk Sigma E0625Oriza Savitri AriantieBelum ada peringkat
- CASA Amann2014Dokumen17 halamanCASA Amann2014DavidAlejandroContrerasGuerraBelum ada peringkat
- Factsheet - Livestock - ReproductiveDiseases in Cattle v2Dokumen3 halamanFactsheet - Livestock - ReproductiveDiseases in Cattle v2lenn chandBelum ada peringkat
- Infertility and Candidate Gene Markers For Fertility in Stallions A ReviewDokumen7 halamanInfertility and Candidate Gene Markers For Fertility in Stallions A ReviewBenjamínCamposBelum ada peringkat
- Dynamics of The Mammalian Sperm Plasma Membrane in The Process of FertilizationDokumen39 halamanDynamics of The Mammalian Sperm Plasma Membrane in The Process of FertilizationWachiel ArhamzBelum ada peringkat
- General Embryology Lecture 1 and 2 - Day 1-Third WeekDokumen142 halamanGeneral Embryology Lecture 1 and 2 - Day 1-Third WeekSalma LyambilaBelum ada peringkat
- Lecture 18 Camelid Reproduction and InfertilityDokumen50 halamanLecture 18 Camelid Reproduction and InfertilitygnpobsBelum ada peringkat
- Bovine Obstetrics 1Dokumen48 halamanBovine Obstetrics 1Viswanatha ReddyBelum ada peringkat
- CASA Krishnakumar2011Dokumen9 halamanCASA Krishnakumar2011Oriza Savitri AriantieBelum ada peringkat
- Vaginal CytologyDokumen4 halamanVaginal Cytologyابراهيم عبدالله100% (1)
- Art PDFDokumen38 halamanArt PDFLinguumBelum ada peringkat
- Parturition Related Disorders in Sheep and Goat: G.N.PurohitDokumen36 halamanParturition Related Disorders in Sheep and Goat: G.N.PurohitgnpobsBelum ada peringkat
- Reproductive Bio Technologies BuffaloDokumen2 halamanReproductive Bio Technologies Buffalognpobs100% (1)
- Sign of Hyperandrogenism PDFDokumen6 halamanSign of Hyperandrogenism PDFmisbah_mdBelum ada peringkat
- Juyena Et Al-2012-Journal of AndrologyDokumen16 halamanJuyena Et Al-2012-Journal of AndrologyAnamaria Blaga PetreanBelum ada peringkat
- CryopreservationDokumen29 halamanCryopreservationDharmendra KumarBelum ada peringkat
- Database of Cattle Candidate Genes and Genetic MarkersDokumen20 halamanDatabase of Cattle Candidate Genes and Genetic MarkersrohishaakBelum ada peringkat
- Contraceptive ImplantsDokumen17 halamanContraceptive ImplantsKingBee1123Belum ada peringkat
- Newborn Calf ManagmentDokumen17 halamanNewborn Calf ManagmentCarolyn ParsonsBelum ada peringkat
- AI History PDFDokumen11 halamanAI History PDFBlanca FuentesBelum ada peringkat
- Mastitis Treatment Supporting FormulaDokumen17 halamanMastitis Treatment Supporting FormulaPavan Kumar P N100% (1)
- Table 4.1 AFS Classifi Cation System (: The Embryological-Clinical Classifi CationDokumen111 halamanTable 4.1 AFS Classifi Cation System (: The Embryological-Clinical Classifi CationArya Syafaromania RachmaBelum ada peringkat
- Ovarian Ultrasonography and Follow of Estrus in The Bitch and QueenDokumen8 halamanOvarian Ultrasonography and Follow of Estrus in The Bitch and QueenTere GarzónBelum ada peringkat
- Reproductive TechnologiesDokumen347 halamanReproductive TechnologiesMagda SofronBelum ada peringkat
- Reproductive Management of Equine InfertilityDokumen23 halamanReproductive Management of Equine InfertilitygnpobaBelum ada peringkat
- Assisted Reproductive Technology: Shanty Olivia F.JDokumen41 halamanAssisted Reproductive Technology: Shanty Olivia F.Jshanty Olivia jasirwanBelum ada peringkat
- Interpretation of The Semen Analysis and Initial Male Factor ManagementDokumen10 halamanInterpretation of The Semen Analysis and Initial Male Factor ManagementRosangela Mazariegos CastilloBelum ada peringkat
- Implantation and Development of The PlacentaDokumen8 halamanImplantation and Development of The PlacentaZulfi Nur Amrina RosyadaBelum ada peringkat
- Sperm Selection Methods in The 21st Century. Biology of Reproduction.Dokumen19 halamanSperm Selection Methods in The 21st Century. Biology of Reproduction.Karen Lorena MontealegreBelum ada peringkat
- Effect of Post - Milking Teat Dipping On Hygienic Quality of Cows Milk - D. Kučević, M. Plavšić, S. Trivunović, M. Radinović, D. S. KučevićDokumen9 halamanEffect of Post - Milking Teat Dipping On Hygienic Quality of Cows Milk - D. Kučević, M. Plavšić, S. Trivunović, M. Radinović, D. S. KučevićCk_psihBelum ada peringkat
- Unit: 08 Placentation in Mammals: Developmental Biology Cr. Hours: 4 (3+1)Dokumen30 halamanUnit: 08 Placentation in Mammals: Developmental Biology Cr. Hours: 4 (3+1)Task BirdBelum ada peringkat
- Vitrification ManualDokumen46 halamanVitrification Manualjose.antoni3480Belum ada peringkat
- Lecture 8 Uterine Torsion in Domestic AnimalsDokumen19 halamanLecture 8 Uterine Torsion in Domestic AnimalsgnpobsBelum ada peringkat
- Links For MCQs Vet Gynec & Obst by Prof G.N.purohitDokumen1 halamanLinks For MCQs Vet Gynec & Obst by Prof G.N.purohitgnpobsBelum ada peringkat
- Embryo TransferDokumen47 halamanEmbryo TransferArchael De GuzmanBelum ada peringkat
- Equine Castration AU Vet JournalDokumen7 halamanEquine Castration AU Vet JournalYolandi Lewis StoltzBelum ada peringkat
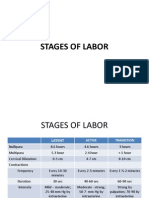
- Stages of LaborDokumen30 halamanStages of LaborPerrilyn Perey100% (1)
- TH THDokumen11 halamanTH THFista Divi AmesiaBelum ada peringkat
- K16 - Pharmacology of Hormonal ContraceptionDokumen51 halamanK16 - Pharmacology of Hormonal Contraceptiondhiyas100% (1)
- Depo ProveraDokumen3 halamanDepo ProveraDivika ShilvanaBelum ada peringkat
- STD Prevention ScriptDokumen3 halamanSTD Prevention ScriptAbimbolaBamigbolaBelum ada peringkat
- Pelvic Inflammatory Disease Cause Infertility: A Condition Requiring Closer AttentionDokumen60 halamanPelvic Inflammatory Disease Cause Infertility: A Condition Requiring Closer AttentionVergina ClaudiaBelum ada peringkat
- The Socio Cultural Factors Affecting The Use of Family Planning Among Rural Women in Gwagwalada Area Council, Fct.Dokumen5 halamanThe Socio Cultural Factors Affecting The Use of Family Planning Among Rural Women in Gwagwalada Area Council, Fct.David SamBelum ada peringkat
- The Waiting Period - Shaykh Fawzan's Fiqh BookDokumen12 halamanThe Waiting Period - Shaykh Fawzan's Fiqh BookNasrin AktherBelum ada peringkat
- MrmbsDokumen7 halamanMrmbsASHBelum ada peringkat
- Sexually Transmitted DiseasesDokumen29 halamanSexually Transmitted DiseasesDha DhaBelum ada peringkat
- Adapted From Family Planning Competency-Based Training: Basic Course HandbookDokumen4 halamanAdapted From Family Planning Competency-Based Training: Basic Course HandbookVanessa EnteroBelum ada peringkat
- M12 Reproductive FertilityDokumen6 halamanM12 Reproductive Fertilityសេន វិចិត្ត Sen VichethBelum ada peringkat
- ANP2001 Female Reproductive System LAB QUIZ PDFDokumen5 halamanANP2001 Female Reproductive System LAB QUIZ PDFJerilee SoCute WattsBelum ada peringkat
- Sales & Distribution Project: Contraceptive Condom DurexDokumen32 halamanSales & Distribution Project: Contraceptive Condom DurexManish NeerajBelum ada peringkat
- In Vitro FertilizationDokumen4 halamanIn Vitro FertilizationFrances Kaye Sta. CruzBelum ada peringkat
- Equine Male Reproductive SystemDokumen6 halamanEquine Male Reproductive SystemSavannah Simone Petrachenko100% (1)
- HDDokumen77 halamanHDAngel RudyBelum ada peringkat
- Reproductive Health BillDokumen3 halamanReproductive Health BillCharmane Barte-MatalaBelum ada peringkat
- Kaylee MyersDokumen5 halamanKaylee Myersapi-410354384Belum ada peringkat
- Responsible Parenthood and Reproductive Health:: Family PlanningDokumen37 halamanResponsible Parenthood and Reproductive Health:: Family PlanningalyssaBelum ada peringkat
- Contraception ReportDokumen16 halamanContraception ReportJino Onij BolandoBelum ada peringkat
- Article - Yoga For WomenDokumen8 halamanArticle - Yoga For WomenDuath Dinen100% (1)
- Annexure 1Dokumen8 halamanAnnexure 1Arumugam KrishnanBelum ada peringkat
- 009obs and Gynae History TakingDokumen13 halaman009obs and Gynae History TakingkbBelum ada peringkat
- Sexually Transmitted InfectionDokumen16 halamanSexually Transmitted InfectionSonam ChaudharyBelum ada peringkat
- MMCDDokumen24 halamanMMCDworksheetbookBelum ada peringkat
- Induction of Labor PDFDokumen8 halamanInduction of Labor PDFGustomo PanantroBelum ada peringkat
- ContraceptionDokumen156 halamanContraceptionLorenn DacpanoBelum ada peringkat
- CDC FACT SHEET: Reported STDs in The United States - 2012 National Data For Chlamydia, Gonorrhea, and SyphilisDokumen3 halamanCDC FACT SHEET: Reported STDs in The United States - 2012 National Data For Chlamydia, Gonorrhea, and Syphilistherepubliq.comBelum ada peringkat
- Post Partum Family Planning/Planification Familiale Du Post - PartumDokumen18 halamanPost Partum Family Planning/Planification Familiale Du Post - PartumJhpiego100% (2)