SJMC - xi-nCP&HTP - Impaired Skin Integrity
Diunggah oleh
Joy CompetenteDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
SJMC - xi-nCP&HTP - Impaired Skin Integrity
Diunggah oleh
Joy CompetenteHak Cipta:
Format Tersedia
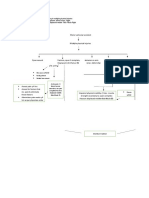
XI.
NURSING CARE PLAN AND HEALTH TEACHING PLAN
NURSING CARE PLAN (1)
NURSING DIAGNOSIS CUES Impaired Skin Integrity related to decubitus ulcer stage I and IV as manifested by destruction of skin layers Subjective(by the relative) nakahiga lang sya lagi sa bahay nanunuod ng t.v. o kaya nakikinig ng radyo. dati ang lalakilaki talaga nung sugat nya sa likod tapos may mga itim-itim pa, mas maayos na nga yung sugat nya sa likod ngayon kaysa dati. ANALYSIS The skin is a barrier to infectious agents; however, any break in the skin can readily serve as a portal of entry putting the individual at risk for potential infections. (Fundamentals of Nursing by Kozier, et.al., 7th edition ,page 633) GOAL / OBJECTIVES GOAL After 8 days of nursing intervention, the client will be able to display timely healing pressure sores without complications. OBJECTIVES After 8 days of nursing interventions, patients stage I decubitus ulcer will not have any increase in redness or any skin tears and patients stage IV decubitus ulcer wound will decreased in size and minimize presence of wound. NURSING INTERVENTIONS Independent RATIONALE EVALUATION
Periodically
remeasure wound and observe for complications
To monitor progress Wounds were
of wound healing
remeasured and observed for complications.
Assess skin. Note the skin color, turgor, and sensation. Describe and measure the decubitus ulcer and wounds and observe changes.
Establishes
comparative baseline providing opportunity for timely intervention.
The skin was
assessed. The skin color, turgor and sensations were noted. Observed changes, measured, and described the patients decubitus ulcer and wounds
Objective Presence of decubitus ulcer stage I in left scapula 4 cm in diameter and stage IV in sacrum 9 cm in diameter Physical immobilization
Reposition the
patient every 2 hours and avoid repositioning the patient on site of the decubitus ulcer
Repositioning improves blood circulation and reduces pressure on bony prominences.
The patient was repositioned every 2 hours, avoiding the patients site of decubitus ulcer
Monitor temperature
An increase in
Temperature
was monitored
temperature can be a sign of infection.
Localized erythema around the decubitus ulcer Hemiplegia Hemiparesis Facial Grimace of pain
Assess patient's nutritional status.
Inadequate
Inter-dependent Keep the area clean and dry, carefully dress wounds, prevent infection and stimulate circulation to the surrounding areas
nutritional intake places individuals at risk for skin breakdown and compromises healing.
Patient's nutritional status was assessed.
Keeping the area clean and dry will prevent harbor of pathogenic microorganisms thus prevents further infection.
Area kept clean and dry with wound dressing applied carefully. Prevented infection and stimulated circulation to the surrounding areas. Wet and wrinkled linens were removed
Remove wet/wrinkled linens promptly
Moisture potentiates skin breakdown
Instruct patient to
avoid scratching the decubitus ulcer. Scratching may lead to skin breakdown which may result to lesion or wound.
Instructed patient to avoid scratching the decubitus ulcer.
Dependent
Administer topical medications as prescribed.
Prescribed medications administered
To protect the wound and the surrounding tissues
HEALTH TEACHING PLAN (1)
LEARNING OBJECTIVES Goal (this plan is directed to the clients relative due to the clients inability to comprehend) After 8 days of nursing intervention, the client will be able to display timely healing pressure sores without complications. Objectives After 8 days of nursing interventions, patients stage I decubitus ulcer will not have any increase in redness or any skin tears and patients stage IV decubitus ulcer wound will decreased in size and minimize presence of wound. Bedsores, more accurately called pressure sores or pressure ulcers, are areas of damaged skin and tissue that develop when sustained pressure cuts off circulation to vulnerable parts of your body, especially the skin on your buttocks, hips and heels. Without adequate blood flow, the affected tissue dies. Stage I. A pressure sore begins as a persistent area of red skin that may itch or hurt and feel warm and spongy or firm to the touch. In blacks, Hispanics and other people with darker skin, the mark may appear to have a blue or purple cast, or look flaky or ashen. Stage I wounds are superficial and go away shortly after the pressure is relieved. Stage II. At this stage, some skin loss has already occurred either in the outermost layer of skin (the epidermis), the skin's deeper layer (the dermis), or in both. The wound is now an open sore that looks like a blister or an abrasion, and the surrounding tissues may show red or purple discoloration. Stage III. By the time a pressure ulcer reaches this stage, the damage has extended to the tissue below the skin, creating a deep, crater-like wound. Stage IV. This is the most serious and Develop therapeutic nurse-client relationship. Promotes trust, provides atmosphere in which client is most successful when conducted in a positive, nonjudgmen tal atmosphere Time: 30minutes Venue: ward Resources: visual aids The client was able to display timely healing pressure sore without complications LEARNING CONTENT METHOD/ STRATEDY RATIONALE TIME / VENUE / RESOURCES EVALUATION
Discussion and oral return demonstration
advanced stage. A large-scale loss of skin occurs, along with damage to underlying muscle, bone, and even supporting structures such as tendons and joints. f you've been immobilized, bedsores can be caused by: Sustained pressure. When your skin and the underlying tissues are trapped between bone and a surface such as a wheelchair or bed, blood flow is restricted. This deprives tissue of oxygen and other nutrients, and irreversible damage and tissue death can occur. This tends to happen in areas that aren't well padded with muscle or fat and that lie just over a bone, such as your spine, tailbone (coccyx), shoulder blades, hips, heels and elbows.
In some cases, the pressure that cuts off circulation comes from unlikely sources: the rivets and thick seams in jeans, crumbs in your bed, wrinkled clothing or sheets, a chair whose tilt is slightly off even perspiration, which can soften skin, making it more vulnerable to injury. Friction. Frequent shifts in position are the key to preventing pressure sores. Yet the friction that occurs when you simply turn from side to side can damage your skin, making it more susceptible to pressure sores. Shear. This occurs when your skin moves in one direction, and the
underlying bone moves in another. Sliding down in a bed or chair or raising the head of your bed more than 30 degrees is especially likely to cause shearing, which stretches and tears cell walls and tiny blood vessels. Especially affected are areas such as your tailbone where skin is already thin and fragile. In the early stages (1 and 2) of bedsores, the area may heal with relief of pressure and by applying care to the affected skin. A good diet will aid skin healing, especially by taking in enough vitamin C and zinc, which are available as supplements. For effective skin care: If the skin is not broken, gently wash the area with a mild soap and water. Clean open sores on the skin with salt water (saline, which can be made by boiling 1 quart of water with 1 teaspoon of salt for 5 minutes and kept cooled in a sterile container). Apply a thin layer of petroleum jelly (Vaseline) and then cover with a soft gauze dressing.
Be sure to keep urine and stool away from affected areas. To relieve pressure: Change positions often (every 15 minutes in a chair and every 2 hours in a bed). Use special soft materials or supports (pads, cushions, and mattresses) to reduce pressure against the skin. The first step in treating a sore at any stage is relieving the pressure that caused it. You can reduce pressure by:
Changing positions often. Carefully follow your schedule for turning and repositioning approximately every 15 minutes if you're in a wheelchair and at least once every two hours when you're in bed. If you're unable to change position on your own, a family member or other caregiver must be able to help. Using sheepskin or other padding over the wound can help prevent friction when you move. Using support surfaces. These are special cushions, pads, mattresses and beds that relieve pressure on an existing sore and help protect vulnerable areas from further breakdown.
The most effective support depends on many factors, including your level of mobility, your body build and the severity of your wound. No one support surface is appropriate for all people or all situations. In general, protective padding such as sheepskin isn't thick enough to reduce pressure, but it's helpful for separating parts of your body and preventing friction damage. You can use a variety of foam, air-filled or water-filled devices to cushion a wheelchair, but avoid using pillows and rubber rings, which actually cause compression. For your mattress, doctors often suggest lowair-loss beds or air-fluidized beds. Low-air-loss beds use inflatable pillows for support, whereas air-fluidized beds suspend you on an air-permeable mattress that contains millions of silicone-coated beads.
Other nonsurgical treatments of pressure sores include: Cleaning. It's essential to keep wounds clean to prevent infection. A stage I wound can be gently washed with water and mild soap, but open sores should be cleaned with a saltwater (saline) solution each time the dressing is changed. Avoid antiseptics such as hydrogen peroxide and iodine, which can damage sensitive tissue and delay healing.
Controlling incontinence as far as possible is crucial to helping sores heal. If you're experiencing bladder or bowel problems, you may be helped by lifestyle changes, behavioral programs, incontinence pads or medications. Removal of damaged tissue (debridement). To heal properly, wounds need to be free of damaged, dead or infected tissue. This can be accomplished in several ways the best approach depends on your overall condition, the type of wound and your treatment goals.
One approach is surgical debridement, a procedure that involves using a scalpel or other instrument to remove dead tissue. Surgical debridement is quick and effective, but it can be painful. For that reason, your doctor may use one or more nonsurgical approaches. These include removing devitalized tissue with a high-pressure irrigation device (mechanical debridement), allowing your body's own enzymes to break
down dead tissue (autolytic debridement), or applying topical debriding enzymes (enzymatic debridement). Dressings. A variety of dressings are used to help protect wounds and speed healing the type usually depends on the stage and severity of the wound. The basic approach, however, is to keep the wound moist and the skin surrounding it dry. Stage I sores may not need any covering, but stage II lesions are usually treated with hydrocolloids, or transparent semipermeable dressings that retain moisture and encourage skin cell growth. Other types of dressings may be more beneficial for weeping wounds or those with surface debris. Contaminated sores may also be treated with a topical antibiotic cream. Hydrotherapy. Whirlpool baths can aid healing by keeping skin clean and naturally removing dead or contaminated tissue. Oral antibiotics. If your pressure sores appear infected, your doctor may prescribe oral antibiotics. Healthy diet. Eating a nutritionally rich diet with adequate calories and protein and a full range of vitamins and minerals especially vitamin C and zinc may improve wound healing. Being well nourished also protects the integrity of your skin and guards against breakdown. If you're at risk of or recovering from a pressure sore, your doctor may prescribe vitamin C and zinc supplements.
Muscle spasm relief. This is essential for both preventing and treating pressure sores. To help alleviate spasticity, your doctor may recommend skeletal muscle relaxants that block nerve reflexes in your spine or in the muscle cells themselves.
Position changes Changing your position frequently and consistently is crucial to preventing bedsores. It takes just a few hours of immobility for a pressure sore to begin to form. For that reason, experts advise shifting position about every 15 minutes that you're in a wheelchair and at least once every two hours, even during the night, if you spend most of your time in bed. If you can't move on your own, a family member or caregiver must be available to help you. A physical therapist can advise you on the best ways to position yourself in bed, but here are some general guidelines: Avoid lying directly on your hipbones. On your side, lie at a 30degree angle. Support your legs correctly. When lying on your back, place a foam pad or pillow not a doughnut-shaped cushion under your legs from the middle of your calf to your ankle. Avoid placing a support directly behind your knee it can severely restrict blood flow. Keep your knees and ankles from touching. Use small pillows or pads.
Avoid raising the head of the bed more than 30 degrees. A higher incline makes it more likely that you'll slide down, putting you at risk of friction and shearing injuries. If the bed needs to be higher when you eat, place pillows or foam wedges at your hips and shoulders to help maintain alignment. Use a pressure-reducing mattress or bed. You have many options, including foam, air, gel or water mattresses. Because these can vary widely in price and effectiveness, talk to your doctor about the best choice for you. For some people, a low-air-loss mattress may provide enough support. But more expensive and technologically sophisticated beds may be needed for people who have recurring pressure sores or who are at very high risk.
Anda mungkin juga menyukai
- CPG AbortionDokumen40 halamanCPG AbortionKatharine Nerva75% (12)
- Professional Adjustment and Nursing Care Management Practice Exam Answer KeyDokumen20 halamanProfessional Adjustment and Nursing Care Management Practice Exam Answer Keystuffednurse93% (41)
- Emj Cases : Questions For Case 1Dokumen8 halamanEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- 500-Bed Hospital General Specification and Design ConceptDokumen5 halaman500-Bed Hospital General Specification and Design ConceptShahnawaz ShaikhBelum ada peringkat
- 3011-1 - NCP & Drug Study - AMCDokumen5 halaman3011-1 - NCP & Drug Study - AMCAngie MandeoyaBelum ada peringkat
- Lonzaga Assessment PDFDokumen7 halamanLonzaga Assessment PDFNiño Naryana Luke PanchoBelum ada peringkat
- Management of A Patient With Acute Abdominal Pain - College of Surgeons of Sri Lanka 2007 PDFDokumen30 halamanManagement of A Patient With Acute Abdominal Pain - College of Surgeons of Sri Lanka 2007 PDFRevalitha PutriBelum ada peringkat
- Treating Tetanus with InterventionDokumen2 halamanTreating Tetanus with InterventionChristopher John Aguelo100% (3)
- NCP Readiness RevisionDokumen3 halamanNCP Readiness RevisionimnasBelum ada peringkat
- Nursing Care Plan for Diabetic Patient with DehydrationDokumen2 halamanNursing Care Plan for Diabetic Patient with DehydrationRodolfo Bong SemaneroBelum ada peringkat
- Motor Vehicle Accident Leads to Multiple Fracture InjuriesDokumen2 halamanMotor Vehicle Accident Leads to Multiple Fracture Injuriesjunifer laynoBelum ada peringkat
- NCP Skin IntegrityDokumen3 halamanNCP Skin IntegrityAlfie Ayro50% (2)
- NCP For Ruptured AppendicitisDokumen2 halamanNCP For Ruptured AppendicitisJansen Arquilita RiveraBelum ada peringkat
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDokumen11 halamanNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDa NicaBelum ada peringkat
- Nursing care plan for patient with meningiomaDokumen3 halamanNursing care plan for patient with meningiomaShaira TillahBelum ada peringkat
- Cues Objectives Interventions Rationale Evaluation: Nursing Care PlanDokumen1 halamanCues Objectives Interventions Rationale Evaluation: Nursing Care Planaprilrosehibaya100% (1)
- ImmobilityDokumen1 halamanImmobilitymicopoliBelum ada peringkat
- Nursing Care Plan for Post-Surgical PainDokumen3 halamanNursing Care Plan for Post-Surgical PainAngelgodess Athena-envyBelum ada peringkat
- Assessing and Treating Post-Operative HypothermiaDokumen2 halamanAssessing and Treating Post-Operative HypothermiaJayrelle D. SafranBelum ada peringkat
- NCP Acute Pain Related To Presence of Postoperative Surgical IncisionDokumen2 halamanNCP Acute Pain Related To Presence of Postoperative Surgical IncisionPebbles PangilinanBelum ada peringkat
- Impaired Physical MobilityDokumen3 halamanImpaired Physical MobilityCharmaine ChuaBelum ada peringkat
- Nursing Cues for Managing Osteosarcoma PainDokumen2 halamanNursing Cues for Managing Osteosarcoma Painkasandra dawn BerisoBelum ada peringkat
- NCP Impaired SkinDokumen2 halamanNCP Impaired Skinarjay2306_obcq100% (1)
- FractureDokumen4 halamanFractureRaveen mayiBelum ada peringkat
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDokumen4 halamanCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDokumen1 halamanNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyBelum ada peringkat
- NCPDokumen10 halamanNCPNefre Dayap DarrocaBelum ada peringkat
- NCP (Fatigue)Dokumen3 halamanNCP (Fatigue)Edrick SilvaBelum ada peringkat
- Head Nurse: General ObjectiveDokumen10 halamanHead Nurse: General Objectiveeihjay-bravo-8041Belum ada peringkat
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDokumen2 halamanTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestBelum ada peringkat
- NCP Self Care DeficitDokumen3 halamanNCP Self Care DeficitLeizel ApolonioBelum ada peringkat
- Drug Study Domperidone CompressDokumen1 halamanDrug Study Domperidone CompressAngelica TolledoBelum ada peringkat
- Post-Op Wrist Pain ManagementDokumen13 halamanPost-Op Wrist Pain ManagementJay Jay JayyiBelum ada peringkat
- NCP Knowledge DeficitDokumen2 halamanNCP Knowledge DeficitPrincess Faniega SugatonBelum ada peringkat
- Nursing Care Plan for Acute Pain ManagementDokumen3 halamanNursing Care Plan for Acute Pain ManagementSheene Lysethea Sioteco AguilosBelum ada peringkat
- Saint Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingDokumen4 halamanSaint Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingimnasBelum ada peringkat
- NCP - ERDokumen5 halamanNCP - ERAnnelore ArcayBelum ada peringkat
- Risk for Infection Nursing Care PlanDokumen2 halamanRisk for Infection Nursing Care PlanKarl-Ren LacanilaoBelum ada peringkat
- Impaired Tissue Integrity BurnDokumen1 halamanImpaired Tissue Integrity BurntabaloveBelum ada peringkat
- NCP & Drug Study (Tondo Med)Dokumen5 halamanNCP & Drug Study (Tondo Med)Kevin_Remollo_2431Belum ada peringkat
- Nursing Care Plan for Bronchial Asthma PatientDokumen3 halamanNursing Care Plan for Bronchial Asthma PatientissaiahnicolleBelum ada peringkat
- NCP - Acute PainDokumen2 halamanNCP - Acute PainsAm_300% (1)
- Mechanism, Indications, Contraindications and Adverse Effects of TramadolDokumen5 halamanMechanism, Indications, Contraindications and Adverse Effects of TramadolDenise EspinosaBelum ada peringkat
- Impaired Physical Mobility...Dokumen3 halamanImpaired Physical Mobility...Christy BerryBelum ada peringkat
- Dynastat: What Is in This LeafletDokumen4 halamanDynastat: What Is in This LeafletBenj GilbuenaBelum ada peringkat
- Resource Unit On Common Drugs (LRDR Rotation)Dokumen37 halamanResource Unit On Common Drugs (LRDR Rotation)kiamoiBelum ada peringkat
- NCP Acute PainDokumen3 halamanNCP Acute PainNathalie kate petallarBelum ada peringkat
- NCP Acute PainDokumen3 halamanNCP Acute Painmanoelsterg50% (2)
- E. Nursing DiagnosisDokumen2 halamanE. Nursing DiagnosisAle SandraBelum ada peringkat
- HEALTH-TEACHING (Safety)Dokumen3 halamanHEALTH-TEACHING (Safety)Asterlyn ConiendoBelum ada peringkat
- Nursing Care Plans for Pain Management and Self-CareDokumen15 halamanNursing Care Plans for Pain Management and Self-CareKarl Vincent Soso100% (1)
- GENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANDokumen4 halamanGENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANFran LanBelum ada peringkat
- FdarDokumen1 halamanFdarRoxas Cedrick100% (1)
- Acute Pain NCPDokumen1 halamanAcute Pain NCPJed AvesBelum ada peringkat
- DP Discharge Plan@@@@@@@@Dokumen6 halamanDP Discharge Plan@@@@@@@@Maemae SumalinogBelum ada peringkat
- Discharge Care Plan ChecklistDokumen2 halamanDischarge Care Plan ChecklistLaurinda Angelica Dimaiwat PrestadoBelum ada peringkat
- LortabDokumen1 halamanLortabSheri490Belum ada peringkat
- Acute Pain Prioritization After HysterectomyDokumen2 halamanAcute Pain Prioritization After HysterectomyRuth Lea Cabrera100% (1)
- ASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoDokumen1 halamanASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoCherie MayBelum ada peringkat
- Aaa Gastrectomy NCP FinalDokumen13 halamanAaa Gastrectomy NCP Finallexzaf100% (1)
- Nursing Care Plan: Our Lady of Fatima University College of Nursing Antipolo CampusDokumen2 halamanNursing Care Plan: Our Lady of Fatima University College of Nursing Antipolo CampusJhevilin RMBelum ada peringkat
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Dokumen20 halamanSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizBelum ada peringkat
- Decubetic Ulcer (Bed Sores)Dokumen22 halamanDecubetic Ulcer (Bed Sores)Jerry ZahidBelum ada peringkat
- Pressure Ulcers: by Mr. M. Shivanandha ReddyDokumen35 halamanPressure Ulcers: by Mr. M. Shivanandha ReddyDr Ali100% (2)
- Pressure Sore or Decubitus Ulcer or Bed SoreDokumen20 halamanPressure Sore or Decubitus Ulcer or Bed SorePrecious BlessingBelum ada peringkat
- ReferatDokumen35 halamanReferatYuni AurraBelum ada peringkat
- TMC Cadi Press Release RFID Baby TaggingDokumen4 halamanTMC Cadi Press Release RFID Baby TaggingmeboniteerBelum ada peringkat
- Nurs Fpx 4010 Assessment 3 Interdisciplinary Plan ProposalDokumen5 halamanNurs Fpx 4010 Assessment 3 Interdisciplinary Plan Proposalfarwaamjad771Belum ada peringkat
- Scientists Study The Benefits of Worms - NewselaDokumen3 halamanScientists Study The Benefits of Worms - NewselaMr WarnockBelum ada peringkat
- Unit 1 - Ways Informatics Transforming Health CareDokumen22 halamanUnit 1 - Ways Informatics Transforming Health CareRaquel MonsalveBelum ada peringkat
- Hyperkalemia Approach AND Management: Dr. Renuka RayanaDokumen38 halamanHyperkalemia Approach AND Management: Dr. Renuka RayanaSap ModulesBelum ada peringkat
- Case Study FIXDokumen66 halamanCase Study FIXPatrick Kelvian100% (1)
- Comparing Cognitive Screening Tools MMSE and SLUMSDokumen7 halamanComparing Cognitive Screening Tools MMSE and SLUMSseftri Puji ABelum ada peringkat
- Vertical Control of Overbite in Mixed Dentition by Trainer SystemDokumen7 halamanVertical Control of Overbite in Mixed Dentition by Trainer SystemJUAN FONSECABelum ada peringkat
- Diabetic Ketoacidosis Protocol PICU Oct 2010 2Dokumen9 halamanDiabetic Ketoacidosis Protocol PICU Oct 2010 2Vidini Kusuma AjiBelum ada peringkat
- Resme Rahul GuptaDokumen5 halamanResme Rahul Guptarahul guptaBelum ada peringkat
- Homoeopathic Perspective of Thyroid DisordersDokumen20 halamanHomoeopathic Perspective of Thyroid DisordersSaurav AroraBelum ada peringkat
- Salivary Gland DisordersDokumen50 halamanSalivary Gland DisordersghazyBelum ada peringkat
- Mariam Burchuladze: Group 7 / Reflection EssayDokumen1 halamanMariam Burchuladze: Group 7 / Reflection EssayMariam BurchuladzeBelum ada peringkat
- Subq and Im InjectionsDokumen2 halamanSubq and Im Injectionsapi-242267470Belum ada peringkat
- Physical Assessment:: Area Technique Norms Findings Analysis and Interpretation A. SkullDokumen15 halamanPhysical Assessment:: Area Technique Norms Findings Analysis and Interpretation A. SkullRoseben SomidoBelum ada peringkat
- Artificial OrgansDokumen7 halamanArtificial OrgansFranziska WagnerBelum ada peringkat
- Icd 10 Chapter XviiiDokumen2 halamanIcd 10 Chapter Xviiifebi novrizalBelum ada peringkat
- Internal Medicine Write Up 1Dokumen16 halamanInternal Medicine Write Up 1Ariff MahdzubBelum ada peringkat
- ICS Factsheet 6 (JW) July 2016Dokumen3 halamanICS Factsheet 6 (JW) July 2016José Ignacio YánezBelum ada peringkat
- Thyroid CytologyDokumen36 halamanThyroid CytologyNaglaa RamadanBelum ada peringkat
- Six Sigma Green BeltDokumen57 halamanSix Sigma Green BeltRavi ValiyaBelum ada peringkat
- Sarnat 1976Dokumen10 halamanSarnat 1976João Paulo RaposoBelum ada peringkat
- Annotated Bib - JasmineDokumen3 halamanAnnotated Bib - JasminejasreadingitBelum ada peringkat
- Dental Chair Positions GuideDokumen35 halamanDental Chair Positions GuideFaye Nervanna Alecha Alferez100% (1)