ICD 10.0: K29 Condition/Disease: Gastritis Description:: Symptom
Diunggah oleh
vicndubDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
ICD 10.0: K29 Condition/Disease: Gastritis Description:: Symptom
Diunggah oleh
vicndubHak Cipta:
Format Tersedia
ICD 10.
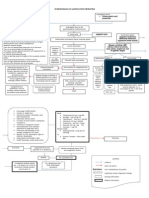
0: K29 Condition/Disease: Gastritis Description: Dyspepsia: Continuous or recurrent upper abdominal pain or discomfort with or without associated symptom (nausea, bloating, regurgitation,etc) Gastritis: Inflammatory changes in the gastric mucosa Peptic ulcer disease: Chronic illness manifested by recurrent ulceration in the stomach and proximal duodenum. Epidemiology: Complications of gastritis include PUD (Peptic ulcer disease) and, rarely, extensive bleeding. PUD accounts for more than 50% of all causes of upper gastrointestinal bleeds in the United States. Approx 10% of US population older than 17 years have peptic ulcer at some time Frequency of PUD is decreasing in the developed world but increasing in developing countries The prevalence of dyspepsia is 25 to 30 percent in the US Male-to-female ratio of gastritis is approximately 1:1 Male-to-female ratio of PUD is approximately 2:1 The mortality rate is low. Sign and symptom: Symptom: Typically present with abdominal pain that has the following characteristics: o Epigastric to left upper quadrant o Frequently described as burning o May radiate to the back o Usually occurs 1-5 hours after meals o May be relieved by food, antacids (duodenal), or vomiting (gastric) o Typically follows a daily pattern specific to patient (episodic and chronic) Bloating, indigestion, eructation, flatulence, and heartburn Anorexia, nausea/vomiting Gastritis may present as bleeding, which is more likely in elderly patients. Sign: Epigastric tenderness is present and usually mild. Dehydration, tachycardia, and electrolyte disturbance (With vomiting) Bowel sounds are normal. Hematemesis melena, pallor, and sign of volume depletion (Hemorrhagic gastritis) Signs of peritonitis or GI bleeding may be manifest. Perform a rectal examination Alarm feature: - Age older than 45-50 years - Weight loss - Dysphagia
Long history of symptom Anemia Persistent anorexia Early satiety Persistent vomiting Gastrointestinal bleeding
Specific diagnostic: - Upper gastrointestinal barium contrast radiography - Endoscopy of upper gastrintestinal tract - H Pylori test (IgG serology, urea breath test, fecal antigent test, rapid urea test) Disposition: - Outpatient - Inpatient : o Acute hemorrhagic or erosive gastritis that present with upper GI tract bleeding, tachycardia and hypotension o Uncontrolled pain or vomiting o Coagulopathy from medication or liver disease Management and tretment: - Diet: Avoid iritating food - IVFD: o Fluid resuscitation on Acute hemorrhagic gastritis o Blood transfusion if low hematocrite - Diagnostic: o CBC, BUN, Creatinin serum, Electrolyte (If suspected GI Bleeding) o Amylase, Lipase for pancreatitis o Urinalysis, asses dehydration o ECG, in elderly patient `Medication: 1. Proton pump inhibitor (PPI), ex: Esomeprazole, 20-40 mg PO qd 2. H2-receptor antagonist (H2RA), ex: Ranitidine 150 mg PO bid or 300 mg PO qhs; not to exceed 300 mg/d, or 50 mg/dose IM/IV q6-8h 3. Antacids (2-4 tsp PO qid prn) or a GI cocktail (30ml antacid + 10-20ml viscous lidocaine) 4. Sucralfate: 1gr, PO, QID 5. In chronic gastritis (Treatment of H Pylori infection): Omeprezole 20mg or lansoprazole 30mg + Clarithromycine 500mg + Amoxycillin 1gr, all taken BID - Monitoring: Sign and symptom When to refer: (Gastroenterologist or Surgeon) - If there is alarm sign - When there is complication (Malignancy, Hemorrhage, Perforation, Obstruction) Recommendation: - Patients should be warned of known or potentially injurious drugs and agents (NSAIDs, Aspirin, Alcohol, Caffeine (eg, coffee, tea, colas))
Refference: Five minutes emergency, Tintinally, eMedicine (Philip Shayne, MD)
Anda mungkin juga menyukai
- Med Surg Test 4 Study GuideDokumen29 halamanMed Surg Test 4 Study GuideJessBelum ada peringkat
- Hematemesis Melena (Upper Gi Bleeding)Dokumen134 halamanHematemesis Melena (Upper Gi Bleeding)Mardoni Efrijon100% (1)
- Initial Assessment Form Specialist OPDDokumen1 halamanInitial Assessment Form Specialist OPDvicndub100% (1)
- Practical Prescriber PDFDokumen515 halamanPractical Prescriber PDFGandhi Lanka100% (2)
- Interpretation of Gastric BiopsyDokumen77 halamanInterpretation of Gastric Biopsyyourinmyheart100% (2)
- Gatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2010Dokumen62 halamanGatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2010Ardi PratamaBelum ada peringkat
- Definition and Etiology: PancreatitisDokumen24 halamanDefinition and Etiology: PancreatitisAliyah Tofani PawelloiBelum ada peringkat
- GASTROENTEROLOGY GUIDE: COMMON CONDITIONSDokumen21 halamanGASTROENTEROLOGY GUIDE: COMMON CONDITIONSmuradkhanBelum ada peringkat
- Peptis Ulcer-Bs TâmDokumen27 halamanPeptis Ulcer-Bs TâmÁnh PhạmBelum ada peringkat
- Liver Nursing NotesDokumen7 halamanLiver Nursing NotesHeather ShantaeBelum ada peringkat
- Pre-Res Case Presentation: Jo Anne N. Ramos, MDDokumen72 halamanPre-Res Case Presentation: Jo Anne N. Ramos, MDKah Mote KyuBelum ada peringkat
- Pancreatitis Definition of TermsDokumen6 halamanPancreatitis Definition of TermsDonna Marie Arguelles AmpaBelum ada peringkat
- Peptic Ulcer DiseaseDokumen54 halamanPeptic Ulcer DiseaseMohammad_Islam87Belum ada peringkat
- PepticDokumen29 halamanPepticMuhammad Irfan JamilBelum ada peringkat
- GIT OverviewDokumen108 halamanGIT OverviewNasser SalahBelum ada peringkat
- PancreatitisDokumen28 halamanPancreatitisFrench Pastolero-ManaloBelum ada peringkat
- Peptic Ulcer Disease: Erwin Budi CahyonoDokumen29 halamanPeptic Ulcer Disease: Erwin Budi Cahyonoshavira nuzulaBelum ada peringkat
- Exocrine Pancreatic and Biliary Disorders and ManagementDokumen77 halamanExocrine Pancreatic and Biliary Disorders and ManagementAnthon Kyle TropezadoBelum ada peringkat
- 1100 Ultrasound of The Acute Abdomen 15 3Dokumen84 halaman1100 Ultrasound of The Acute Abdomen 15 3gp1promo2016Belum ada peringkat
- Everything You Need to Know About Peptic Ulcer DiseaseDokumen29 halamanEverything You Need to Know About Peptic Ulcer Diseasehanizah kurniaBelum ada peringkat
- Acute Gastrointestinal Bleeding GuideDokumen47 halamanAcute Gastrointestinal Bleeding GuideJohn Clements Galiza100% (1)
- Acute & Chronic Pancreatitis GuideDokumen38 halamanAcute & Chronic Pancreatitis GuideAliyah Tofani PawelloiBelum ada peringkat
- Cholelithiasis and CholecystitisDokumen28 halamanCholelithiasis and Cholecystitisandreva8Belum ada peringkat
- Lower GI BleedingDokumen40 halamanLower GI BleedingMohammad Firdaus100% (2)
- Uworld GI NotesDokumen17 halamanUworld GI NotesAyodeji SotimehinBelum ada peringkat
- Adult Health Nursing Phase I Thursday 6:00-9:00 PM: Irritable Bowel SyndromeDokumen18 halamanAdult Health Nursing Phase I Thursday 6:00-9:00 PM: Irritable Bowel SyndromeLavinia Malazarte CaballeroBelum ada peringkat
- Upper Gi BleedDokumen43 halamanUpper Gi BleedPreethi GudipalliBelum ada peringkat
- Non Variceal Upper GI Bleeding: Causes, Risk Factors, Diagnosis and ManagementDokumen66 halamanNon Variceal Upper GI Bleeding: Causes, Risk Factors, Diagnosis and ManagementsarangpbBelum ada peringkat
- Pancreatitis: Pancreatitis Is Inflammation of The Pancreas. It Occurs When Pancreatic Enzymes (Especially Trypsin)Dokumen6 halamanPancreatitis: Pancreatitis Is Inflammation of The Pancreas. It Occurs When Pancreatic Enzymes (Especially Trypsin)tianallyBelum ada peringkat
- UgumDokumen50 halamanUgumhailu henockBelum ada peringkat
- Prepared by Inzar Yasin Ammar LabibDokumen47 halamanPrepared by Inzar Yasin Ammar LabibdiaBelum ada peringkat
- Gi BleedingDokumen74 halamanGi Bleedingponcus payBelum ada peringkat
- Examen IM-gastroenterologieDokumen15 halamanExamen IM-gastroenterologieNicola BereholschiBelum ada peringkat
- AscitesDokumen71 halamanAscitessohilaw210Belum ada peringkat
- Gasteroenterology 151 200Dokumen30 halamanGasteroenterology 151 200Ahmed Kh. Abu WardaBelum ada peringkat
- Gastric Outlet Obstruction PathophysiologyDokumen2 halamanGastric Outlet Obstruction PathophysiologyTania Noviza100% (1)
- Liver Cirrhosis: DR - Aryadevi A SDokumen89 halamanLiver Cirrhosis: DR - Aryadevi A SMahesh PethkarBelum ada peringkat
- Acute Pancreatitis SymptomsDokumen12 halamanAcute Pancreatitis SymptomsUthraa SalvatoreBelum ada peringkat
- MDs Discuss Common GI IssuesDokumen111 halamanMDs Discuss Common GI IssuesRenny WidiastutiBelum ada peringkat
- Case 5 - Pancreatitis-1Dokumen4 halamanCase 5 - Pancreatitis-1ngBelum ada peringkat
- Chronic Liver Disease PresentationDokumen202 halamanChronic Liver Disease PresentationMohammadAbdurRahmanBelum ada peringkat
- Upper Gastrointestinal Bleeding 2007Dokumen43 halamanUpper Gastrointestinal Bleeding 2007Matthew ThompsonBelum ada peringkat
- Gastrointestinal System Review PPT 2022 (Autosaved)Dokumen30 halamanGastrointestinal System Review PPT 2022 (Autosaved)LalaBelum ada peringkat
- Hematology Case Stdy 1 FINALEDokumen30 halamanHematology Case Stdy 1 FINALEvinoedhnaidu_rajagopalBelum ada peringkat
- Lecture On Conjugated HyperbilirubinaemiaDokumen38 halamanLecture On Conjugated HyperbilirubinaemiaIgwe SolomonBelum ada peringkat
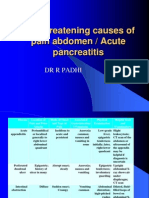
- Life Threatening Causes of Pain Abdomen / Acute PancreatitisDokumen27 halamanLife Threatening Causes of Pain Abdomen / Acute PancreatitisDr. Rajesh Padhi100% (1)
- 2019review Internal Medicine (II)Dokumen65 halaman2019review Internal Medicine (II)Wai Kwong ChiuBelum ada peringkat
- 2007 MAY JUNE 2007 CompleteDokumen68 halaman2007 MAY JUNE 2007 CompleteKay BristolBelum ada peringkat
- Gastrointestinal Bleeding Aug 24-1Dokumen82 halamanGastrointestinal Bleeding Aug 24-1xiongmao2389Belum ada peringkat
- Update On The Management of PancreatitisDokumen92 halamanUpdate On The Management of Pancreatitisadamu mohammadBelum ada peringkat
- GI Disorders Problems in Elimiation Absorption DigestionDokumen4 halamanGI Disorders Problems in Elimiation Absorption DigestionMikee PaningbatanBelum ada peringkat
- CLD 2Dokumen5 halamanCLD 2macdominic22Belum ada peringkat
- GERDDokumen15 halamanGERDAhmed EzzatBelum ada peringkat
- Clinical Clerk Seminar Series: Approach To Gi BleedsDokumen11 halamanClinical Clerk Seminar Series: Approach To Gi BleedsAngel_Liboon_388Belum ada peringkat
- Dental Management of Diseases of The Gastrointestinal SystemDokumen61 halamanDental Management of Diseases of The Gastrointestinal SystemkomalgorayaBelum ada peringkat
- Anemia Sec To UGIBDokumen32 halamanAnemia Sec To UGIBJose Fernando Gregana ElpaBelum ada peringkat
- Lower GI Chapter Summary: Constipation, Diarrhea, Appendicitis & MoreDokumen8 halamanLower GI Chapter Summary: Constipation, Diarrhea, Appendicitis & MoreRebeccaBelum ada peringkat
- Dyspepsia: Dr. Kinar Kh. SaeedDokumen25 halamanDyspepsia: Dr. Kinar Kh. SaeedsamiBelum ada peringkat
- Dr. S.P. Hewawasam (MD) Consultant Gastroenterologist/Senior Lecturer in PhysiologyDokumen33 halamanDr. S.P. Hewawasam (MD) Consultant Gastroenterologist/Senior Lecturer in PhysiologyAjung SatriadiBelum ada peringkat
- Obstructive Jaundice 2020Dokumen4 halamanObstructive Jaundice 2020Choden JamyangBelum ada peringkat
- Portal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandPortal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Mandible Fracture Postoperative InstructionsDokumen3 halamanMandible Fracture Postoperative InstructionsvicndubBelum ada peringkat
- D-Dimer AssaysDokumen1 halamanD-Dimer AssaysAlisha AhmadBelum ada peringkat
- Our Services CaptionDokumen1 halamanOur Services CaptionvicndubBelum ada peringkat
- Hong Kong Covering Letter of Lab Report EngDokumen1 halamanHong Kong Covering Letter of Lab Report EngvicndubBelum ada peringkat
- Molecular and Antibody Point-Of-Care Tests To Support The Screening, Diagnosis and Monitoring of COVID-19Dokumen12 halamanMolecular and Antibody Point-Of-Care Tests To Support The Screening, Diagnosis and Monitoring of COVID-19vicndubBelum ada peringkat
- What Is HospitalistDokumen1 halamanWhat Is HospitalistvicndubBelum ada peringkat
- WHO COVID 19 Laboratory 2020.5 Eng PDFDokumen7 halamanWHO COVID 19 Laboratory 2020.5 Eng PDFChicky DressesBelum ada peringkat
- Flow Covid-19 Rapid Test Promo: Examination and Blood Test (RAPID TEST Only) With APDDokumen1 halamanFlow Covid-19 Rapid Test Promo: Examination and Blood Test (RAPID TEST Only) With APDvicndubBelum ada peringkat
- Perbandingan Test Covid - Texas ArticleDokumen4 halamanPerbandingan Test Covid - Texas ArticlePutri SyawalBelum ada peringkat
- Actemra Larutan Injeksi 20 MG, ML (Infus) - Tokilizumab - DKI1135900149A1 - 2020Dokumen53 halamanActemra Larutan Injeksi 20 MG, ML (Infus) - Tokilizumab - DKI1135900149A1 - 2020karindaBelum ada peringkat
- Antigen-Detection in The Diagnosis of Sars-Cov-2 Infection Using Rapid ImmunoassaysDokumen9 halamanAntigen-Detection in The Diagnosis of Sars-Cov-2 Infection Using Rapid ImmunoassaysMuhammadWathoniIkhlasBelum ada peringkat
- The Most Powerful Natural Antibiotic Ever23Dokumen5 halamanThe Most Powerful Natural Antibiotic Ever23Anonymous WA0ihAS100% (1)
- GIT - Dr. Allam 2021 PDFDokumen47 halamanGIT - Dr. Allam 2021 PDFMohammedBelum ada peringkat
- 6 13Dokumen3 halaman6 13Shawn Gaurav JhaBelum ada peringkat
- Exogenic ReasonsDokumen6 halamanExogenic ReasonsJohn wickBelum ada peringkat
- Diagnosis: Surgical Pathology ReportDokumen2 halamanDiagnosis: Surgical Pathology ReportMHCNSBelum ada peringkat
- Intestinal MetaplasiaDokumen12 halamanIntestinal MetaplasiaarifBelum ada peringkat
- Edited HP I Fri ConfDokumen85 halamanEdited HP I Fri ConfTara Oliveros Dela CruzBelum ada peringkat
- Gastritis An Update in 2020Dokumen17 halamanGastritis An Update in 2020adri20121989Belum ada peringkat
- User Manual - Cem Tech NEW 1cmDokumen21 halamanUser Manual - Cem Tech NEW 1cmBacean Aurel IoanBelum ada peringkat
- General Practitioner - Gastroenterology MCQsDokumen23 halamanGeneral Practitioner - Gastroenterology MCQsAsif NewazBelum ada peringkat
- Upper Gastrointestinal - Esophageal BleedingDokumen15 halamanUpper Gastrointestinal - Esophageal Bleedingmardsz100% (9)
- Ilovepdf MergedDokumen152 halamanIlovepdf MergedHart ElettBelum ada peringkat
- Helicobacter PyloriDokumen3 halamanHelicobacter Pyloriursula_ursulaBelum ada peringkat
- Ms Prelim NewDokumen12 halamanMs Prelim NewJane LaquihonBelum ada peringkat
- Erosive & Hemorrhagic "Gastritis" (Gastropathy)Dokumen7 halamanErosive & Hemorrhagic "Gastritis" (Gastropathy)Rizka KartikasariBelum ada peringkat
- Lp8 - DIgestive System DiseasesDokumen4 halamanLp8 - DIgestive System DiseasesTeacher OliBelum ada peringkat
- GI Agents: Inorganic Pharmacy-IIDokumen28 halamanGI Agents: Inorganic Pharmacy-IIAbdur RaquibBelum ada peringkat
- NCM 103 Metab N EndocrineDokumen148 halamanNCM 103 Metab N EndocrinernrmmanphdBelum ada peringkat
- A Cross-Sectional Study of The Prevalence ofDokumen9 halamanA Cross-Sectional Study of The Prevalence ofKurnia pralisaBelum ada peringkat
- Yoga Sudha Sept 2022Dokumen44 halamanYoga Sudha Sept 2022Parameswaran MBelum ada peringkat
- Gastric Mass Diagnosis and StagingDokumen41 halamanGastric Mass Diagnosis and StagingsparkleBelum ada peringkat
- Alterations in Git Function 2Dokumen35 halamanAlterations in Git Function 2Lloyd The UnicornBelum ada peringkat
- Stomach - GastritisDokumen22 halamanStomach - GastritisaimanBelum ada peringkat
- H2SO4 Cyclohexanone Cyclohexanol Benzoic Acid Hexane Isopropanol H2O NaOH NaHCO3 HCl solubility hazardsDokumen1 halamanH2SO4 Cyclohexanone Cyclohexanol Benzoic Acid Hexane Isopropanol H2O NaOH NaHCO3 HCl solubility hazardsBug AphidBelum ada peringkat
- Gastritis 508Dokumen8 halamanGastritis 508FaichalMartadinataBelum ada peringkat
- A Supplement A Day Keeps The Doctor Away - The Science of Why We Need To Supplement Our Diet (PDFDrive)Dokumen214 halamanA Supplement A Day Keeps The Doctor Away - The Science of Why We Need To Supplement Our Diet (PDFDrive)angelobuffaloBelum ada peringkat
- AshitabaDokumen6 halamanAshitabaBenjie BugarinBelum ada peringkat
- Chronic Gastritis Case StudyDokumen17 halamanChronic Gastritis Case StudyKaren Evangelista50% (4)