Congenital Malformations of Nose and Sinuses
Diunggah oleh
Dr. T. BalasubramanianJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Congenital Malformations of Nose and Sinuses
Diunggah oleh
Dr. T. BalasubramanianHak Cipta:
Format Tersedia
Congenital malformations of nose and paranasal sinuses.
By
Dr T Balasubramanian
Otolaryngology online
Congential malformations of nose and paranasal sinuses
Introduction: Congenital malformations of nose and paranasal sinuses are rare manifestations involving disordered development involving the origin of the aerodigestive tract. These children present with cosmetic malformations, life threatening acute airway obstruction and feeding difficulties. For better understanding of the developmental anamolies of the nose they can be classified according to the involvement of specific anatomical zones. They include: 1. Errors at the anterior neuropore 2. Errors of the central midface 3. Errors of the bucconasal membrane Embryology of nose and paranasal sinuses: Developmentally nose and paranasal sinuses are interlinked. They are always considered together developmentally. Developmentally the various sinuses may follow different calenders, their orgin is the same. Development of head and neck along with face, nose and paranasal sinuses takes place simultaneously in a short window span. At the end of 4th week of development branchial arches, branchial pouches and primitive gut makes their appearance. That is when the embryo gets its first identifiable head and face with an orifice in its middle known as the stomodeum. The stomodeum (primitive mouth) is surrounded by mandibular and maxillary prominences bilaterally. These prominences are derivatives of first arch. This arch will give rise to all vascular and neural supply of this area. The stomodeum is limited superiorly by the presence of frontonasal eminence and inferiorly by the mandibular arch. The frontonasal process inferiorly differentiates into two projections known as Nasal Placodes. These nasal placodes will be ultimately invaded by growing ectoderm and mesenchyme. These structures later fuse to become the nasal cavity and primitive choana, separated from the stomodeum by the oronasal membrane. The primitive choana forms the point of development of posterior pharyngeal wall and the various paranasal sinuses. The oronasal membrane is fully formed by the end of 5th week of development. It gives rise to the floor of the nose (palate develops from this membrane).
Figure showing development of nose and pns The continuing growth of embryo brings both the nasal placodes and the maxillary processes together in midline to form the maxilla and the beginning of the external nose. The frontonasal prominence gives rise to inferior mesodermic projection which goes on to form the nasal septum dividing the nose into two cavities. Simultaneously the skull and facial bones also develop. The skeletal system develops from mesoderm. Each cranial bone is formed by a series of bone spicules that grow from the centre towards the periphery. At birth all the cranial bones are separated by layers of connective tissue which later fuses and ossifies in the postnatal period. At about 25 28 weeks of gestation, three medially directed projections arise from the lateral wall of the nose. This serves as the beginning of the development of paranasal sinuses. Between these projections small lateral diverticula invaginate into the primitive choana to eventually form the meati of the nose. The medial projections arising from the lateral wall of the nose forms the following structures: 1. The anterior projection forms the agger nasi 2. The inferior (maxilloturbinate) projection forms the inferior turbinate and maxillary sinus 3. The superior projection (ethmoidoturbinate) forms the superior turbinate, middle turbinate, ethmoidal air cells and their corresponding drainage channels. The middle meatus develops between the inferior and middle meatus.
Figure showing infundibulum, and meati of nose developing The middle meatus invaginates laterally to form the embryonic infundibulum and uncinate process. During the 13th week of development the embryonic infundibulum grows superiorly to form the frontal recess area. Development of frontal sinus: The frontal sinus may develop as a direct continuation of embryonic infundibulum and frontal recess superiorly during the 16th week. It can also develop by upward migration of anterior ethmoidal air cells to penetrate the inferior aspect of the frontal bone between its outer and inner tables. Pneumatization of frontal bone is a very slow process. The frontal sinus
infact remains as a small blind sac within the frontal bone till the child is about 2 years of age, then secondary pneumatization begins. From the age of 2 till the child becomes 9 years old secondary pneumatization of frontal bone proceeds. When the child reaches the age of 9, the development of the frontal sinus has reached completion. Sometimes frontal sinus may be asymmetrical / aplastic as well.
Figure showing development and enlargement of frontal sinus. The numbers indicate the size of frontal sinus at that corresponding age. The embryonic infundibulum may also invade the mesenchyme in the maxillary process forming the primitive maxillary sinus. Pneumatization of maxillary sinus is faster than that of frontal sinus. Pneumatization occurs at the expense of erupting upper dentition. Abnormalities of maxillary pneumatization is associated with anomalies of upper dentition. Developmental errors involving the anterior neuropore: Anterior neuropore corresponds to the opening of the embryonic neural tube in the anterior portion of the Prosencephalon. This opening closes on day 25 of embryogenesis giving rise to lamina terminalis of the brain. Complete failure of closure of anterior neuropore will lead to anencephaly. This anterior neuropore presists medial to the optic recesses in the third week of life. Around this opening the skull base gives rise to frontal, ethmoidal and nasal bones. This opening narrows down and forms the foramen caecum in the anterior skull base. This area corresponds to the apex of pernasal space. The foramen caecum forms a defect at the anterior skull base at the apex of prenasal space, where the cribriform plate condenses ultimately. This foramen ultimately closes by
fusing with the fonticulous frontalis which is a fontanelle between the inferior aspect of the frontal bones and the developing nasal bones. During the 3rd 8th week of development a projection of dura extends through the foramen caecum traverses the prenasal space and apposes with the ectoderm at the tip of the nasal bones. As the foramen caecum closes, the dural diverticulum detaches from the overlying ectoderm and retracts into the cranium. During this process sometimes irrevocably attached ectoderm could be pulled postero superiorly towards or into the foramen caecum giving rise to dermoid cyst, fistula or sinus. Sometimes faulty closure / premature closure of foramen caecum may lead to persistence of neural tissue inside the nasal cavity. This could cause : 1. Glioma Isolated heterotropic glial tissue 2. Menigocele / Encephalocele Patent central nervous system communication Encephaloceles can occur in a paramedian position as Nasoethmoidal encephalocele. Encephaloceles can occur laterally through a medial orbital wall defect causing a naso orbital encephalocele. Basal encephaloceles herniate posterior to the cribriform plate. Embryological errors may occur above the nasal bones at the level of fonticulus frontalis. Intracranial contents may herniate via the fonticulus frontalis which persists till about the 8th week. Abnormal closure of fonticulus may cause nasofrontal meningoceles, encephaloceles or gliomas.
MRI scan showing dermoid cyst with sinus in the dorsum of the nose
Encephaloceles: An encephalocele is defined as an extracranial herniation of cranial contents through a defect in the skull. If the encephalocele includes only the meninges it is termed as a Menigocele. If an encephalocele includes brain and meninges it is termed as Menigoencephalocele. Types of encephaloceles: 1. Occipital 2. Sincipital 3. Basal Sincipital encephaloceles are the most commonest. This accounts for nearly 25% of all encephaloceles. Sincipital encephaloceles are further classified according to their location into: Nasofrontal encephalocele
Nasoethmoidal encephalocele Nasoorbital encephalocele Nasofrontal encephaloceles: These encephaloceles present as glabellar masses. These masses cause telecanthus and inferior displacement of nasal bones. The bony defect lies between the orbits and inbetween the nasal and frontal bones. Nasoethmoidal encephaloceles: Usually presents as dorsal nasal masses causing superior displacement of nasal bones and inferior displacement of alar cartilages. These masses traverse via the foramen caecum deep to the nasal bones and becomes superficial at the cephalic end of upper lateral cartilage. Further expansion takes place superficial to the upper lateral cartilage. Naso-orbital encephaloceles: Usually manifest as orbital masses causing proptosis and visual disturbances. These masses pass through foramen caecum deep to the frontal and nasal bones and enters the orbit via a defect in the medial orbital wall. Clinically all these lesions: 1. Expands while the child is crying 2. Expands while the child is straining 3. Expands when the jugular vein is compressed 4. Appears as pulsatile bluish compressible lesions 5. Transillumination + Basal encephaloceles: Are less common when compared to that of Sincipital type. These masses arise between cribriform plate and superior orbital tissue / posterior clinoid fissure manifesting as an intranasal mass. These encephaloceles don't manifest until late childhood. They classically cause nasal obstruction and rhinorrhoea.
Types of basal encephaloceles include: 1. Transethmoidal 2. Sphenoethmoidal 3. Trans-sphenoidal 4. Spheno-orbital Transethmoidal type: Is the most common of basal encephaloceles. They present with: 1. Nasal obstruction 2. Hypertelorism
3. Broadening of nasal vault 4. Unilateral nasal mass. These masses pass via the defect at the level of cribriform plate into the superior meatus. It usually presents medial to the middle turbinate. In addition to its transillumination, reducibility and positive cough reflex this position plays a vital role in the diagnosis. Sphenoethmoidal type: This again presents with nasal obstruction, hypertelorism, broadening of nasal vault and unilateral nasal mass. In this type the mass pass into the nasal cavity via the bony defect between posterior ethmoid air cells and sphenoid. Trans-sphenoidal type: This presents as a naso pharyngeal mass causing bilateral nasal obstruction. This condition is usually associated with a cleft palate. Spheno orbital type: In this type the mass passes through superior orbital fissure and exits via inferior orbital fissure into the sphenopalatine fossa. It causes unilateral exophthalmos, diplopia and other visual defects. Histopathology: Histopathologically all encephaloceles have: 1. a glial component 2. Astrocytes surrounded by collagen 3. Submucous glands 4. Calcification 5. Nasal septal cartilage 6. Presence of ependymal tissue is consistent with that of encephalocele. This feature helps in the differentiation between encephaloceles and gliomas.
Role of imaging: CT / MRI helps in deleniating encephaloceles. Helps in ruling out associated anamolies like agenesis of corpus callosum and hydrocephalus. CT scan invariably clearly outlines the bony cartilagenous defects. MRI helps in differentiating meningoceles and meningoencephaloceles. Contrast CT and saggital reconstruction of images helps in identifying intracranial extension. Management of encephaloceles:
Once an encephalocele is diagnosed then it should be managed surgically. These lesions are surgically managed best during the first few months of life. This is important in order to minimize the risk of meningitis and cosmetic deformity. Early surgery also makes identification of intracranial extension easier and hence it can be removed in toto and the defect can be closed completely with complete repair of the dural defect. Small lesions with small skull base defects can be managed endoscopically, while larger lesions require a combined approach of craniotomy and nasal endoscopy. The skull defect should be reconstructed using pericranial flap or full thickness calvarial bone graft. Gliomas: These are heterotopic glial tissue without patent CSF communication with the subarachnoid space. It should however be borne in mind that nearly 5 20 % of gliomas retain fibour communication with the brain contents. Gliomas commonly occur in males. Types of gliomas: 1. Extranasal 2. Intranasal 3. Combined Among these three types the extranasal type is the commonest to be followed by intranasal and combined varieties. Extranasal gliomas: These are firm non compressible masses occuring commonly at the glabella. Sometimes they may occur along the side of the nose i.e. Along the nasomaxillary suture line.
Diagram representing extranasal glioma
Intranasal gliomas: This type of glioma presents as polypoidal pale masses protruding from the nasal cavity. They arise commonly from the lateral nasal wall close to the middle turbinate. On rare occasions they could arise also from the nasal septum. Combined gliomas: They have both intranasal and extranasal components. Features of nasal gliomas: 1. These gliomas can rarely extend into orbit, frontal sinus, oral cavity and nasopharynx 2. Since there is no patent CSF communication these gliomas don't change in size when the child is crying 3. They do not transilluminate
Imaging: Both CT and MRI should be performed as they both complement each other. CT scan helps to assess the bony anatomy of the skull base accurately. On the other hand MRI helps in the accurate assessment of soft tissue. It also helps to delineate any communication with the intracranial structure with clarity.
Histology: Histologic examination of gliomas show dysplastic glial cells and fibrovascular tissue. Ependymal tissues are never found in gliomas. It is this feature that helps in the distinguition between glioma and encephalocele. Management: Successful management of glioma is only by surgical removal of the mass in full. Surgery should be performed using multidiciplinary approach as early as possible / feasible. Delay can lead to distortion of nasal bones or may even predispose to infection. Surgical access should be planned by keeping cosmesis in mind. Nasal dermoid: These are frontonasal inclusion cysts / tracts caused by embroyological errors localized to the anterior neuropore. Dermoids are the most common congenital midline masses. Most of these dermoids occur sporadically with a slight male preponderance. Nasal dermoids can be associated with the following congenital anamolies: 1. aural atresia 2. pinna deformity 3. mental retardation 4. hydrocephalus 5. branchial arch anamolies 6. cleft lip and palate 7. hypertelorism 8. hemifacial microsomia Clinical features of nasal dermoid: Usually manifests as midline pit / mass. Commonly a dimple could be seen near the rhinion and is associated with a widened nasal bridge. In its ture spectrum this disease the following manifestations can occur anywhere along the embryonic line from the nasal tip to the cranial space. Lesions can be a mass lesion / cyst / sinuses / fistula. Mass lesion when present will be firm, lobulated and non compressible. It will always be assoicated with a sinus opening with intermittent discharge of caseous material. Hair may also be present within the cyst in some of these patients. Recurrent meningitis with typical skin flora indicate the presence of an intact intracranial tract. Nasal dermoids do not enlarge when the child is crying. It also doesn't transilluminate.
Congenital dermoids contain ectodermal and mesodermal elements, where as a teratoma contains elements of all three germ layers. Imaging:
CT scans with intravenous contrast 3 mm cuts are recommended to differentiate dermoid from the surrounding nasal mucosa. It also helps to define the bony anatomy of the skull base. MRI helps in the diagnosis by its excellent soft tissue resolution. Contrast MRI differentiates dermoid which is non enhancing from that of enhancing hemangiomas and teratomas. It should be noted that in neonates the crista galli does'nt contain fat and hence any enhancing mass seen in this area in a neonate on T1weighted MRI suggests intracranial dermoid.
Coronal CT scan image showing bifid cristagalli with enlarged foramen caecum Management: Nasal dermoids are best managed by complete surgical removal of the lesion. Aspiration, incision and drainage and curettage have been found to have high recurrence rates. Assessment of intracranial extension is vital before deciding the optimal surgical approach. If extracranial approach is to be used then the following criteria should be fullfilled. They include: 1. Excellent access to midline structures 2. Access to skull base 3. Adequate exposure for reconstruction of dorsum of nose 4. The scar produced should be an acceptable one Among the various extra cranial approaches external rhinoplasty approach provides the best exposure and cosmetic result. For lesions extending into the intracranial cavity a multidisiplinary approach is preferred in collaboration with a neurosurgeon.
Midface developmental errors
The following events occur in a synchronised manner. They include: 1. Development of nasal pits and their development into choana 2. Fusion of palatal shelves 3. Growth of nasal septum and soft palate 4. Development of lateral nasal wall and primitive sinuses For normal development of nose and paranasal sinuses these changes should take place with complete precision. This development begins between 4-12 weeks of intrauterine life. It is during this period the neural crest cells begin to migrate form their origin in the dorsal neural folds. They migrate around the developing eyes to form the first and second branchial arch derived facial prominences. These prominences surround the developing mouth i.e. Stomodeum. The stomodeum is surrounded by frontonasal process superiorly, maxillary process laterally and mandibular process inferiorly. Nasal placodes begin to develop as two small thickenings in the fronto nasal process. It begins to burrow forming nasal pits. The development of nasal pits is followed by development of three prominences. They are two lateral nasal prominences and one medial nasal prominence.
Diagram illustrating development of nose
Development of nasolacrimal duct is intricately linked to the development of nose. It begins its development as ectodermal thickening which gets buried in the mesoderm of the nasal pits between
the lateral nasal prominence and the maxillary process. Canalization of this ectodermal thickening takes place from superior to inferior post natally. The lateral and medial nasal prominences interacts with the developing maxillary process forming the philtrum and a portion of the medial part of upper lip. The lateral portion of the upper lip is developed from the maxillary process. Errors in the development of mid face can be a cause for a large number of congenital anamolies involving the nose. Arhinia: This is a congenital absence of nose due to: 1. Abnormal migration of neural crest cells 2. Failure of fusion between medial and lateral nasal processes 3. Overgrowth and premature fusion of medial nasal process 4. Lack of resorption of nasal epithelial plugs Polyrhinia: As the name suggests this congenital malformation features multiple nose like tags in the mid face. This condition usually results from incomplete development of frontonasal process. This causes separation of the developing lateral portions of the nose. The medial nasal process and nasal septum follows the development script and are thereby duplicated causing a double nose. Proboscis lateralis: This anamoly is caused due to mesodermal proliferation disorders. These disorders involving mesodermal proliferation usually occurs in the fronto nasal and maxillary process close to the nasal pit area. Since there is no mesoderm in that area support for epidermis is lost. Epidermal sequestration in this area causes a tube like structure to be formed arisng from the fronto nasal region. Naso lacrimal duct is also not formed in these patients. Naso lacrimal duct cysts: This can occur independent of Proboscis lateralis. This is caused by failure of nasolacrimal ectodermal tract to canalize post nasally. This usually results in naso lacrimal duct cysts in patients who are otherwise normal. Midline / paramedian fusion errors: Fusion errors in the midline / paramedian zones cause midfacial clefting. Clefting may be isolated to the midface, or could be part of cephalic clefting (Robert's syndrome). Fusion errors involving the medial nasal process and the medial aspect of maxillary process produces cleft lip deformity with its accompanying congenital nasal abnormality. Deficiency in the development of primary palate and bony overgrowth of nasal process of maxilla causes congenital nasal pyriform aperture stenosis. Holoprocencephaly: This term was used by DeMayer to describe midline facial cleft anamolies and brain anamolies. This is due to the inability of embryonic forebrain to cleave sagittally into cerebral hemispheres. Arhinia (total absence of nose) could be part of this Holoprocencephaly spectrum. This abnormality is really rare with only about 30 cases being reported in literature so far. This condition
is usually associated with genetic disorders such as trisomy 10, 13 and 21. Features of arhinia: 1. Absence of external nose and nasal airways 2. Hypoplasia of maxilla 3. Small high arched palate 4. Hypertelorism These children have respiratory distress and cyanosis associated with feeding. This is rare in older children as they are able to gobble up food inbetween breaths. They even have anosmia. In addition these children may manifest with hypoplastic orbits. Voice is characteristically hypernasal. Management usually focusses on improvement of nutritional status of the patient. Cleft palate feeder can be made use of during initial stages, if it fails then feeding gastrostomy will have to be resorted to. Prosthetic nose can be used till the child is old enough for definitive surgical repair. Dacryocystorhinostomy will have to be performed as an adjunct procedure to prevent recurrent conjunctivitis caused due to absence of nasolacrimal ducts.
Developmental deficiency of incisive os explains the occurrence of a triangular plate, the narrow inferior portion of the nasal cavity and associated centrally located maxillary mega incisor. Polyrhinia / supernumerary nostril: Double nose / supernumerary nostril are rather very rare anamolies. These anamolies can occur as isolated ones or in combination with pseudohypertelorism. These patients have anterior septal duplication with duplicated nasal passageways and post nasal defects like choanal atresia. Major priority in managing these patients is correction of choanal atresia. Nasal deformity can be corrected by removing the medial portions of each nasal cavity and anastomosing the lateral portions in the midline. This gives rise to a broad flat nose with a depression in the midline. Superneumerary nostrils usually present as small accessory nasal orifices surrounded by redundant soft tissue. These orifices could be seen lateral, medial or superior to the already existing nose. When true fistulous tract is present then discharge from these orifices are common. Proboscis lateralis: This rare congenital disorder manifests as a tubular sleeve of skin attached to the inner canthus of the eye with associated heminasal aplasia on the affected side. This disorder could be caused due to fusion of the maxillary process on the affected side with that of the developing contralateral nasal process. This disorder is usually associated with CNS abnormalities, congenital ocular lesions and archnoid cysts. The various localization points of probscis lateralis lie in the fusion line between the maxillary process and the frontonasal process. These include: 1. Level I : Supramedial canthal area 2. Level II : Medial canthal area 3. Level III : Inframedial canthal area 4. Level IV : Supra nostril area
Diagram illustrating the various levels of proboscis lateralis Treatment of this condition should be delayed till the facial growth is complete. Restenosis is common even after surgical reconstruction and periodical dilatations are necessary. Craniofacial clefts: These disorders are rather rare. This disorder is characterised by: 1. Ocular hypertelorism 2. Broad nasal root 3. Lack of nasal tip 4. Median clefting of nose / lip / palate Nasal deformities associated with cleft lip: Cleft lip deformities are rather common. Complete cleft lip extends up to the floor of the nose. Where as an incomplete cleft does'nt reach the floor of the nose. Children with bilateral cleft lip have flattened nasal tip and a shortened columella. There may also be associated maxillary hypoplasia with prognathism. Congenital pyriform aperture stenosis: This anamoly is caused by bony overgrowth of nasal process of maxilla and usually manifests during the first few months of life. Stenosis of nose may occur in isolation or may be associated with the presence of central mega incisor and holoprocencephaly spectrum of congenital midline
lesions. Since the pyriform aperture is the narrowest portion of the nasal cavity even small changes involving this area can increase the nasal airway resistance. Upper respiratory infections may compicate the issue by increasing the severity of nasal block. CT scan of nose and paranasal sinuses demonstrate that the cross sectional area of the pyriform aperture, nasal cavity and choana are all reduced. The size of the pyriform aperture can be measured in the CT scan axial cut as the distance between the medial aspects of the maxillae at the level of inferior meatus. This value is about 12 mm in normal controls while it is much less in these patients.
Axial CT scan of nose and sinuses showing areas of narrowing in stenosis of nose Nasolacrimal duct cysts: These are also known as dacryocystoceles. These are rather uncommon abnormalities involving the inferior meatus. These abnormalities cause: 1. Nasal obstruction 2. Respiratory distress 3. Epiphora Usually the nasolacrimal duct begins to canalize from the lacrimal end and proceeds in an inferior direction. In addition to nasal block this condition can cause feeding difficulties in neonates with this condition. The diagnosis of nasolacrimal duct cysts could be made by anterior rhinoscopy / nasal endoscopy. The lesion could be seen as cystic mass in the inferior meatus. CT scan of nose and paranasal sinuses shows the following features: 1. Dilated nasolacrimal duct
2. Intranasal cyst 3. Cystic dilatation of lacrimal sac Surgery is indicated in those infants with acute nasal block and feeding difficulties. The cyst can be marsupialized into the inferior meatus under endoscopic vision. Naso lacrimal duct will have to be probed and stented to prevent recurrence. Developmental errors involving the Bucconasal membrane: During 3rd / 4th weeks of development ectodermal nasal placodes begin to appear in the paramedian area. These are small thickenings in the frontonasal process which begin to burrow forming nasal pits. These pits are the ones that develop into nose and paranasal sinuses. These pits develop into pouches and lie just above the oral and buccal cavity. A membrane Bucconasal membrane separates this pouch from the oral cavity. Failure of this membrane to rupture between the 5th and 6th weeks of development results in choanal atresia. Alternatively it has been suggested that abnormal migration of neural crest cells could result in choanal atresia. When choanal atresia develops the postnasal space fails to communicate with the nasopharynx. In 2/3 of cases this is usually unilateral. It is more common in the right side. In bilateral choanal atresia the child is in acute respiratory distress which improves when the child starts to cry, since it takes in air through the mouth by passing the obstructed choanal airway. Since infants are obligate nasal breathers bilateral choanal atresia should be considered to be an airway emergency. Types of choanal atresia: 1. Bony - 90% 2. Membranous - 10% This atretic plate of bone / membrane are generally situated just in front of the posterior end of nasal septum. The congenital choanal atresia should not be considered as an isolated plate of bone but as one component of a skull base anomaly developing between the 4th and 12th weeks of gestation. Theories of development of choanal atresia: 1. Persistence of a buccopharyngeal membrane from the foregut. 2. Persistence of the nasobuccal membrane of Hochstetter - most commonly accepted theory. 3. The abnormal persistence or location of mesodermal adhesions in the choanal region. 4. A misdirection of mesodermal flow secondary to local genetic factors better explains the popular theory of persistent nasobuccal membrane Boundaries of the atretic plate: 1. Superior - Under surface of the body of sphenoid 2. Lateral - Medial pterygoid lamina
3. Medial - vomer 4. Inferior - Horizontal plate of palatine bone
Other anamolies associated with cleft palate include: CHARGE This indicates Coloboma / Heart disease / Atresia of choana / Retarded growth / Genital anamolies. Symptoms: In patients with bilateral choanal atresia, mouth breathing is seen. The patient is unable to clear the nasal cavity of its secretions. There is also associated loss of sensation of smell. Patient's with unilateral atresia has c/o unilateral nasal block associated with thick tenacious secretions which cannot be cleared fully. These patients commonly have foul smelling breath either due to mouth breathing and its attendant drying effects, or due to the inability to clear the nasal cavity of its secretions. These patients also have associated change in voice due to loss of normal nasal intonation i.e. Rhinolalia clausa. The respiratory obstruction is cyclic - as the child falls asleep the mouth closes and a progressive obstruction starting with stridor followed by increased respiratory effort and cyanosis. Either the observer opens the child's mouth or the child cries and the obstruction is cleared. Child with bilateral atresia has difficulty in sucking milk. Clinical examination: 1. Failure to pass a # 6 to 8 French plastic catheter through the nares into the pharynx. (a typical solid feeling will be encountered at the level of the posterior choana approx. 3-3.5 cm from the alar rim). If obstruction is encountered within 1 - 2 cms from the nasal rim it is probably due to traumatic deflection of nasal septum during delivery. If obstruction is due to mucosal oedema it can be shrinked using nasal decongestants like oxymetazoline / xylometazoline. 2. Wisps of cotton may be placed in front of the nasal cavity and the movement of air flow can be ascertained. 3. Placing methylene blue in the nares and not visualizing it within the pharynx.
Management: In bilateral atresia securing the airway takes the first place. An oral airway may be introduced to tide over the immediate crisis. Intraoral nipple - a large nipple can be modified by having its end cut off and then ties are attached to the nipple and placed around the occiput. This type of airway is called a McGovern nipple and provides an airway through which the baby can breath. A very small feeding tube can then we passed either through another hole in the nipple or along side the nipple for gavage feeding.
This is the preferred method of establishing an oral airway. Role of tracheostomy is highly controversial.
Surgical management: Transnasal approach: (using endoscopes): The surgery is performed under general anesthesia. A self retaining nasal speculum is used to expose the nasal cavity and the atretic plate. If the atresia is membranous in nature a simple perforation of the same under endoscopic guidance would suffice. The nasal cavity is decongested using 4% xylocaine with adrenaline in the concentration of 1 in 10,000 concentration. Under endoscopic guidance a mucosal incision is made and the mucosal flaps are elevated exposing the posterior vomer and lateral pterygoid lamina. A diamond burr on an angled hand piece is used to drill the atretic bony plate. It is perforated at the junction of the hard palate and the vomer. Incidentally this is the thinnest part of the atretic plate. This procedure was first described by Stankiewicz. To improve visualisation the inferior turbinate can be out fractured or even be trimmed. After drilling care is taken to preserve the mucosal flaps. A silastic stent is placed into each nostril passing through the drilled neo choana. This helps in reducing the incidence of restenosis. Stent is kept in place for atleast 6 weeks. Caution: While performing this procedure caution must be taken not to injure the sphenopalatine vessels behind the middle turbinate. Advantages of this procedure: 1. This process is faster and easier 2. Blood loss is minimal 3. Can be performed in children of all ages who do not have associated external nasal deformities 4. Child can be immediately breast fed 5. Child can be discharged on the 3rd day itself Disadvantages: 1. Vision is highly limited especially in the new born 2.Inability to adequately remove enough of the posterior vomerine septal bone and prevent restenosis 3. Longer stenting time 4. Endoscopes do not offer binocular vision 5. Can not be done safely and with good results on patients with multiple nasal and nasopharyngeal anomalies.
Transpalatal approach: This procedure is performed under general anaesthesia. A Dingman-Denhardt mouth gag with the infant tongue blade is used. The palate is injected with 0.5% lidocaine with 1:200,000 epinephrine in the area of the mucosal incision. a Owens type(U-shaped) mucosal incision is made beginning just behind the maxillary tuberosity on one side and then continued medial to the alveolar ridge up to the canine region and then angled back to the nasopalatine foramen. A likewise incision is made on the opposite side and the mucosal flap is elevated taking care not to damage the greater palatine arteries. Mucosa of the nose and nasopharynx is elevated and preserved. Then the palatine bones posterior to the greater palatine foramina, the atresia plates and the posterior vomer are carefully drilled away using a diamond burr. Two 14 or 16 French catheters are passed simultaneously into each nostril to check the patency of the newly created choanea. The preserved mucosa is then used to cover the superior and inferior surfaces of the newly formed choanea and then sutured in place to cover the bone. Stents are left in place for 4 weeks. Advantages: 1. Better visualisation and exposure 2. Both hands are free 3. Less stenting period (a portex endotracheal tube can be cut and used as a stent) 4. Less failure rate Disadvantages: 1. The incisions, which are identical to those for a cleft palate repair, may have a banding effect on maxillary growth due to scar formation. (Therefore, most surgeons prefer to wait to use this approach until some teeth are in occlusion - at approx.12-18 months). 2. Palatal growth can be stunted in 50 % of individuals 3. Increased blood loss 4. Increased risk of development of palatal fistulas post operatively Care of the post op patient: 1. The parents must be taught to maintain the stents with frequent suction and a saline-moistened pipe cleaner or cotton applicator 3 to 6 times per day. 2. Antibiotics and decongestants are prescribed if there is evidence of rhinitis 3. Patients must be followed up regularly till the stents are removed. Mesodermal malformations: Congenital mesodermal derived lesions like hemangioma and lipoblastomas can occur in this area, eventhough it is rare. Germline malformations like teratomas can also occur in this area. Management of cutaneous hemangiomas fall within the realm of plastic surgery. Intranasal hemangiomas: GLUT-1 (glucose isoform 1) positive infantile hemangiomas usually have a prediliction to
embryonic fusion plates on the central face. Deep midface infantile hemangiomas usually cause distortion of nasal mucosa. Non infantile GLUT 1 negative hemangiomas of the nasal cavity are commonly seen in the nasal septum, middle turbinate, inferior turbinate and lateral nasal wall. These non infantile hemanigomas of nose could be lobular capillary hemangiomas and reparative cavernous hemangiomas. These hemangiomas are usually friable, sessile / pedunculated. They usually bleed on touch. Nasopharyngeal teratomas: These are common germ cell tumors of childhood. They are almost invariably benign. These tissues comprises of representative elements from the three embryonic layers (ectoderm, mesoderm and endoderm). They also usually contain tissues foreign to the anatomic site of origin. Nasopharyngeal teratomas can either be sessile / pedunculated and may protrude through the mouth. Anencephaly, hemicrania and palatal fissures are commonly seen in these patients. Congenital nasopharyngeal dermoid can be suspected even while the infant is in uterus. This suspicion should occur in all patients with polyhydramnios. This is usually caused due to impaired swallowing of the fetus due to the presence of a large teratoma protruding into the oral cavity. These lesions can be picked up during routine ultrasound examination. A majority of these masses don't have intracranial extension and hence can be excised completely. Surgical approach varies according to the size of the mass.
Anda mungkin juga menyukai
- Cholesteatoma, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCholesteatoma, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Big Book Sponsorship - The Twelve Step Program - Big Book Guide - 4-Hour-12-StepsDokumen30 halamanBig Book Sponsorship - The Twelve Step Program - Big Book Guide - 4-Hour-12-StepscafegrBelum ada peringkat
- Owbn Infernalism: Guide To Dark Thaumaturgy: A Sourcebook For One World by NightDokumen35 halamanOwbn Infernalism: Guide To Dark Thaumaturgy: A Sourcebook For One World by NightJuhász ZoltánBelum ada peringkat
- Diseases of Middle Ear CavityDokumen235 halamanDiseases of Middle Ear CavityDr. T. BalasubramanianBelum ada peringkat
- MS ENT Basic Sciences MGR University September 2009 Question Paper With SolutionDokumen36 halamanMS ENT Basic Sciences MGR University September 2009 Question Paper With SolutionDr. T. Balasubramanian67% (3)
- Basic Sinus AnatomyDokumen71 halamanBasic Sinus AnatomyTalal AlanzyBelum ada peringkat
- Larynx Wrote by DR Nassem TalaatDokumen38 halamanLarynx Wrote by DR Nassem TalaatAbouzr Mohammed ElsaidBelum ada peringkat
- Microtia and Congenital Aural AtresiaDokumen20 halamanMicrotia and Congenital Aural Atresiaapi-19500641Belum ada peringkat
- Eprints Complete Installation ManualDokumen77 halamanEprints Complete Installation ManualDr. T. BalasubramanianBelum ada peringkat
- Important Topics in OtologyDokumen94 halamanImportant Topics in OtologyDr. T. Balasubramanian100% (1)
- Anatomy of Orbit - ENT SCHOLARDokumen16 halamanAnatomy of Orbit - ENT SCHOLARDr. T. BalasubramanianBelum ada peringkat
- Coblation in ENTDokumen45 halamanCoblation in ENTDr. T. BalasubramanianBelum ada peringkat
- Coblation in ENTDokumen45 halamanCoblation in ENTDr. T. BalasubramanianBelum ada peringkat
- Recent Advances in OtolaryngologyDokumen305 halamanRecent Advances in OtolaryngologyDr. T. Balasubramanian80% (5)
- ProptosisDokumen20 halamanProptosisDr. T. Balasubramanian100% (1)
- Glomus TumourDokumen50 halamanGlomus TumourPratibha Goswami100% (1)
- Anesthesia For EntDokumen44 halamanAnesthesia For EntDrshoaib KhanBelum ada peringkat
- RhinitisDokumen23 halamanRhinitisDr. T. BalasubramanianBelum ada peringkat
- SurgeryDokumen606 halamanSurgeryDr. T. Balasubramanian100% (1)
- Ana PnsDokumen15 halamanAna PnsDr. T. BalasubramanianBelum ada peringkat
- Conser LaryngectomyDokumen32 halamanConser LaryngectomyDr. T. Balasubramanian100% (4)
- Nasal Topical TherapeuticsDokumen13 halamanNasal Topical TherapeuticsDr. T. BalasubramanianBelum ada peringkat
- Nasal BleedDokumen32 halamanNasal BleedDr. T. Balasubramanian100% (1)
- Functional Endoscopic Sinus Surgery (Fess) (3) JDokumen20 halamanFunctional Endoscopic Sinus Surgery (Fess) (3) JJulianthy SuentoBelum ada peringkat
- Nasal Septal PerforationDokumen13 halamanNasal Septal PerforationDr. T. Balasubramanian75% (4)
- Clinicals ENTDokumen70 halamanClinicals ENTMarrow Pg42Belum ada peringkat
- Rhinosporidiosis Still An EnigmaDokumen12 halamanRhinosporidiosis Still An EnigmaDr. T. BalasubramanianBelum ada peringkat
- Nasal Stents Are They Really Useful ?Dokumen9 halamanNasal Stents Are They Really Useful ?Dr. T. BalasubramanianBelum ada peringkat
- Ac PolypDokumen8 halamanAc PolypDr. T. BalasubramanianBelum ada peringkat
- Otolaryngology PG Guide BookDokumen75 halamanOtolaryngology PG Guide BookDr. T. Balasubramanian100% (5)
- Endoscopic OtologyDokumen142 halamanEndoscopic OtologyDr. T. Balasubramanian100% (2)
- SialendosDokumen18 halamanSialendosDr. T. Balasubramanian50% (2)
- Endoscopic Anatomy of Nose and PNS FinalDokumen98 halamanEndoscopic Anatomy of Nose and PNS FinalRahul Kurkure100% (2)
- Use of Coblation Technology in OtolaryngologyDokumen70 halamanUse of Coblation Technology in OtolaryngologyDr. T. BalasubramanianBelum ada peringkat
- Use of Coblation Technology in OtolaryngologyDokumen70 halamanUse of Coblation Technology in OtolaryngologyDr. T. BalasubramanianBelum ada peringkat
- CSF RhinorrhoeaDokumen12 halamanCSF RhinorrhoeaSuprit Sn100% (5)
- Pest Control Risk Assessment Indoor and OutdoorDokumen72 halamanPest Control Risk Assessment Indoor and OutdoorarmkarthickBelum ada peringkat
- Congenital Craniofacial MalformationsDokumen79 halamanCongenital Craniofacial MalformationsDr. T. BalasubramanianBelum ada peringkat
- Mastoidectomy Various TypesDokumen33 halamanMastoidectomy Various TypesDr. T. BalasubramanianBelum ada peringkat
- Mastoidectomy Various TypesDokumen33 halamanMastoidectomy Various TypesDr. T. BalasubramanianBelum ada peringkat
- Viral Exanthems: Sahara Tuazan AbonawasDokumen75 halamanViral Exanthems: Sahara Tuazan AbonawasMarlon Cenabre Turaja100% (1)
- Role of Imaging in RhinologyDokumen223 halamanRole of Imaging in RhinologyDr. T. Balasubramanian100% (2)
- Facial Nerve and Its DisordersDokumen66 halamanFacial Nerve and Its DisordersDr. T. BalasubramanianBelum ada peringkat
- MGR Medical University MS ENT Basic Sciences March 2009 Question Paper With SolutionDokumen44 halamanMGR Medical University MS ENT Basic Sciences March 2009 Question Paper With SolutionDr. T. Balasubramanian100% (4)
- Embryology of Inner Ear Recent TrendsDokumen22 halamanEmbryology of Inner Ear Recent TrendsDr. T. BalasubramanianBelum ada peringkat
- Granulomatous Lesions of NoseDokumen15 halamanGranulomatous Lesions of NoseDr. T. Balasubramanian100% (1)
- History of TonsillectomyDokumen9 halamanHistory of TonsillectomyDr. T. Balasubramanian100% (1)
- CholesteatomaDokumen29 halamanCholesteatomawhitelotusoo7Belum ada peringkat
- TympanoplastyDokumen21 halamanTympanoplastyDr. T. BalasubramanianBelum ada peringkat
- Scribus An IntroductionDokumen149 halamanScribus An IntroductionDr. T. BalasubramanianBelum ada peringkat
- Open Monograph Press Installation To FunctioningDokumen40 halamanOpen Monograph Press Installation To FunctioningDr. T. Balasubramanian100% (1)
- Open Monograph Press Installation To FunctioningDokumen40 halamanOpen Monograph Press Installation To FunctioningDr. T. Balasubramanian100% (1)
- Deviated Nose Septum, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandDeviated Nose Septum, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Dlobasic Apr11Dokumen27 halamanDlobasic Apr11Dr. T. BalasubramanianBelum ada peringkat
- Congenital Anomalies of the NoseDokumen53 halamanCongenital Anomalies of the NoseNindya Pratita Heriyono100% (1)
- Trismus An OverviewDokumen13 halamanTrismus An OverviewDr. T. Balasubramanian100% (1)
- Advanced Anatomy of Lateral Nasal Wall - Ent ScholarDokumen7 halamanAdvanced Anatomy of Lateral Nasal Wall - Ent ScholarDr. T. BalasubramanianBelum ada peringkat
- Rhinology SelectionsDokumen186 halamanRhinology SelectionsDr. T. Balasubramanian100% (2)
- Clinical Examination Techniques in Otology Edition IIDokumen43 halamanClinical Examination Techniques in Otology Edition IIDr. T. Balasubramanian100% (2)
- Paraph ImagingDokumen20 halamanParaph ImagingDr. T. Balasubramanian67% (3)
- Maxillary Carcinoma, Nasal Cavity and Paranasal Sinus Malignancy PDFDokumen18 halamanMaxillary Carcinoma, Nasal Cavity and Paranasal Sinus Malignancy PDFSuprit Sn100% (2)
- CP TumorsDokumen21 halamanCP TumorsDr. T. Balasubramanian100% (4)
- Voice Rehabilitation Following Total LaryngectomyDokumen32 halamanVoice Rehabilitation Following Total LaryngectomyDr. T. BalasubramanianBelum ada peringkat
- Tracheal Stenosis and Its ManagementDokumen29 halamanTracheal Stenosis and Its ManagementDr. T. Balasubramanian100% (1)
- MGRUniv UGMar07Dokumen32 halamanMGRUniv UGMar07Dr. T. BalasubramanianBelum ada peringkat
- Vertical Partial Laryngectomy An AtlasDokumen14 halamanVertical Partial Laryngectomy An AtlasDr. T. Balasubramanian100% (2)
- Otalgia by DrtbaluDokumen13 halamanOtalgia by DrtbaluDr. T. Balasubramanian100% (2)
- Approaches To The SphenoidDokumen8 halamanApproaches To The SphenoidSuprit Sn100% (1)
- Eprints From Below Upwards The Manual That Was MissedDokumen58 halamanEprints From Below Upwards The Manual That Was MissedDr. T. Balasubramanian100% (1)
- Instruments in OtolaryngologyDokumen35 halamanInstruments in OtolaryngologyDr. T. BalasubramanianBelum ada peringkat
- Mandibular SwingDokumen12 halamanMandibular SwingDr. T. Balasubramanian100% (4)
- Kriya For Balancing The ChakrasDokumen5 halamanKriya For Balancing The ChakrasFedra Fox Cubeddu100% (2)
- Logan Turner's Diseases of the Nose, Throat and EarDari EverandLogan Turner's Diseases of the Nose, Throat and EarPenilaian: 4 dari 5 bintang4/5 (2)
- Role of X-Rays in RhinologyDokumen18 halamanRole of X-Rays in RhinologyDr. T. BalasubramanianBelum ada peringkat
- Orbital Disorders: DR T BalasubramanianDokumen19 halamanOrbital Disorders: DR T BalasubramanianDr. T. BalasubramanianBelum ada peringkat
- Radio Logical Anatomy of Frontal SinusDokumen9 halamanRadio Logical Anatomy of Frontal SinusDr. T. BalasubramanianBelum ada peringkat
- Child Development Mannualfinal-SinhalaDokumen250 halamanChild Development Mannualfinal-SinhalaAshhara FazalBelum ada peringkat
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsDari EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsBelum ada peringkat
- Vidian NeurectomyDokumen54 halamanVidian NeurectomyDin PcBelum ada peringkat
- Cholesteatoma Part 9 - Reconstruction of The Mastoid Cavity PDFDokumen4 halamanCholesteatoma Part 9 - Reconstruction of The Mastoid Cavity PDFSuprit SnBelum ada peringkat
- Petrous Apex FinalDokumen53 halamanPetrous Apex Finalpravinxyz100% (1)
- Septoplasty IncisionDokumen11 halamanSeptoplasty Incision이상하Belum ada peringkat
- Mbbs Feb11Dokumen22 halamanMbbs Feb11Dr. T. Balasubramanian100% (2)
- Utmb-Glomus Tumors of The Temporal BoneDokumen11 halamanUtmb-Glomus Tumors of The Temporal BoneAnoop SinghBelum ada peringkat
- Facial Pain PDFDokumen4 halamanFacial Pain PDFSuprit SnBelum ada peringkat
- Drtbalu'S Otolaryngology Online: TracheomalaciaDokumen3 halamanDrtbalu'S Otolaryngology Online: TracheomalaciaAnish RajBelum ada peringkat
- Tamil Nadu DR MGR Medical University ENT MBBS Prefinal Feb 2009 Question Paper With SolutionDokumen21 halamanTamil Nadu DR MGR Medical University ENT MBBS Prefinal Feb 2009 Question Paper With SolutionDr. T. BalasubramanianBelum ada peringkat
- OSCE Notes in Otology Surgery by DrtbaluDokumen85 halamanOSCE Notes in Otology Surgery by DrtbaluDrAli JafarBelum ada peringkat
- The Development of The Middle Ear Spaces and Their Surgical SignificanceDokumen15 halamanThe Development of The Middle Ear Spaces and Their Surgical SignificanceDrTarek Mahmoud Abo Kammer100% (2)
- Paranasal Sinus (Repaired) EntDokumen48 halamanParanasal Sinus (Repaired) EntDr-Firas Nayf Al-ThawabiaBelum ada peringkat
- Google Classroom For NoviceDokumen87 halamanGoogle Classroom For NoviceDr. T. BalasubramanianBelum ada peringkat
- Ent Wiki Installation ManualDokumen13 halamanEnt Wiki Installation ManualDr. T. BalasubramanianBelum ada peringkat
- Otolaryngology Online Journal Faciomaxillary Trauma An UpdateDokumen66 halamanOtolaryngology Online Journal Faciomaxillary Trauma An UpdateDr. T. BalasubramanianBelum ada peringkat
- Ent Scholar Volume 2 Issue 1 2013Dokumen100 halamanEnt Scholar Volume 2 Issue 1 2013Dr. T. BalasubramanianBelum ada peringkat
- Otolaryngology Online Journal Faciomaxillary Trauma An UpdateDokumen66 halamanOtolaryngology Online Journal Faciomaxillary Trauma An UpdateDr. T. BalasubramanianBelum ada peringkat
- Entscholar Volume 1 Issue 2Dokumen68 halamanEntscholar Volume 1 Issue 2Dr. T. BalasubramanianBelum ada peringkat
- Hydralazine For Severe PIHDokumen4 halamanHydralazine For Severe PIHYwagar YwagarBelum ada peringkat
- Apotex Pharmachem Product ListDokumen2 halamanApotex Pharmachem Product Listমোঃ এমদাদুল হকBelum ada peringkat
- Raising Dengue Awareness in the PhilippinesDokumen4 halamanRaising Dengue Awareness in the PhilippinesAlyssa Hazza Membrano MayonadoBelum ada peringkat
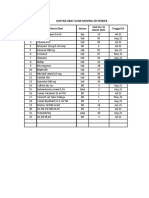
- Daftar Obat Slow Moving Dan Ed Rawat Inap Maret 2021Dokumen8 halamanDaftar Obat Slow Moving Dan Ed Rawat Inap Maret 2021Vima LadipaBelum ada peringkat
- Prothrombin Time Normal RangeDokumen2 halamanProthrombin Time Normal RangeKent AlveBelum ada peringkat
- SVCTDokumen70 halamanSVCTSvct DelhiBelum ada peringkat
- Novo NordiskDokumen2 halamanNovo NordiskSpotlightBelum ada peringkat
- Modified Fluid Wax Impression For A Severely Resorbed Edentulous Mandibular RidgeDokumen4 halamanModified Fluid Wax Impression For A Severely Resorbed Edentulous Mandibular RidgeChepe LemusBelum ada peringkat
- Bio OssDokumen4 halamanBio OssVizi AdrianBelum ada peringkat
- NIH Training On Human SubjectsDokumen73 halamanNIH Training On Human SubjectsDavid Andrés Montoya ArenasBelum ada peringkat
- ResumeDokumen7 halamanResumeRonald Fuéntes EndómaBelum ada peringkat
- Ayushman Bharat - KailashDokumen11 halamanAyushman Bharat - KailashKailash NagarBelum ada peringkat
- Emotional Influences On Food Choice Sensory, Physiological andDokumen9 halamanEmotional Influences On Food Choice Sensory, Physiological andpanda_pandita22Belum ada peringkat
- FISIOGRAFT ENG Set 17 PDFDokumen28 halamanFISIOGRAFT ENG Set 17 PDFmaxBelum ada peringkat
- Integrating Modern Dermatology and AyurvedaDokumen25 halamanIntegrating Modern Dermatology and AyurvedachandusgBelum ada peringkat
- The LungsDokumen6 halamanThe LungsnandaBelum ada peringkat
- Penelitian Pengembangan Minyak Atsiri Sebagai Aromaterapi Dan Potensinya Sebagai Produk Sediaan Farmasi MuchtaridiDokumen9 halamanPenelitian Pengembangan Minyak Atsiri Sebagai Aromaterapi Dan Potensinya Sebagai Produk Sediaan Farmasi MuchtaridiFitria Dewi 'uthie'Belum ada peringkat
- Introduction to Radiographic Imaging InterpretationDokumen17 halamanIntroduction to Radiographic Imaging Interpretationpradep4u21Belum ada peringkat
- Fycompa Efficacy Adjunctive Partial SeizuresDokumen20 halamanFycompa Efficacy Adjunctive Partial SeizuresoneniravBelum ada peringkat
- Class 11 English Snapshots Chapter 7Dokumen2 halamanClass 11 English Snapshots Chapter 7Alpha StarBelum ada peringkat
- Kaloji Narayana Rao University Health Sciences College Allotment ListDokumen79 halamanKaloji Narayana Rao University Health Sciences College Allotment ListVivek GuptaBelum ada peringkat
- Diagnostic Imaging Equipment & Consumables Laser PrintersDokumen5 halamanDiagnostic Imaging Equipment & Consumables Laser Printersnanu_gomezBelum ada peringkat
- ق 4Dokumen36 halamanق 4Zainab HasanBelum ada peringkat
- Model Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20Dokumen1 halamanModel Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20SwarnA TamtaBelum ada peringkat