2011 07 Microbiology-Mycobacterium Skin Infection
Diunggah oleh
dtimtimanJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
2011 07 Microbiology-Mycobacterium Skin Infection
Diunggah oleh
dtimtimanHak Cipta:
Format Tersedia
Transcriptionist: Bunny Fril Editor: in Chief Pages: 5
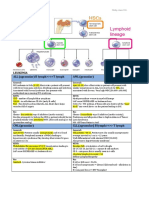
Outline: I. Mycobacterium Leprae a. History b. Diagnostic Features c. Epidemiology d. Clinical Manifestation e. Types f. Lepromin test g. Laboratory Diagnosis h. Treatment i. Prevention and Control II. Mycobacterium Marinum a. Diagnostic Features b. Clinical Manifestations c. Clinical Diagnosis d. Treatment III. Mycobacterium Ulcerans a. Diagnostic Features b. Epidemiology c. Clinical Manifestations d. Treatment
Take note: nasal scrapings contain a very high number of the organisms because they prefer to stay in the cooler part of the body, and the nasal septum temp is lower than any other part of the body.
I. MYCOBACTERIUM LEPRAE A. History Discovered in 1873 by G.A. Hansen Causes Hansens Disease or Leprosy (no effective therapy until 1940) In Spain: Lepers- Legally dead, a social stigma (marker for isolation) B. Diagnostic Features An obligate Intracellular parasites that needs a host to replicate Prefers to attack Macrophages and Schwann cells Acid-fast staining straight or slightly curved rods, arranged singly, in parallel bundles or globular masses Red Stain (seen in smears) Gram Variable - more gram(+) than gram(-) not really useful for identification Regularly found in scrapings from the skin or mucous membrane (nasal septum- has lower temp. Bacilli from ground tissue nasal scrapings: 1. Inoculated into footpads of mice--> development of local granulomatous lesions with limited bacterial multiplication 2. Inoculated into armadillos development of extensive lepromatous/leprosy
Bacilli are often found within endothelial cells of blood vessels or in mononuclear cells Humans and Nine-banded armadillos are the only known natural hosts Has mycolic acid which gives it a thin waxy coating Mycolic acid- large fatty acid; dense, large lipid outer capsule outside the cell wall (phenolic glycolipid 1 or PGL-1) which has served as the antigen for serologic test for leprosy CANNOT be grown in cell-free media or tissue culture Grows best at below 37C in humans and mice (predilection for cooler areas of body) Grows luxuriously in cold blooded armadillos Gram(+) bacillus under Ziehl-Neelsen staining method
Fig.1: A tissue section: Red- mycobacterium acid-fast
C. Epidemiology -estimated 6 million with leprosy (3 million untreated) - Endemic: Asia (greatest number cases), Africa, Latin America, and Pacific - Associated with: poverty, rural residence, armadillo contact (N. America) - Transmission is due to overcrowding and poor hygiene - Modes of Transmission: 1. Majority - nasal droplet infection 2. Skin-to-skin contact - not the general route because organisms are not found histologically in the epidermis nor the dermis 3. Contact with lepromatous leprosy patients (shedding of organisms in nasal secretions or ulcer exudates)
SY 2011-2012
1
Subject: Microbiology Topic: Mycobacterial Skin Infections Lecturer: Dr. Teresa Barzaga MD Date of Lecture: 07-20-2011
4. Insect vectorsbed bugs and mosquitoes in areas of leprosaria community harbor M. Leprae 5. Transmitted by soil: a.) M. Leprae specific PGL-1 has been found in soil b.)Leprosy is primarily a rural and not an urban disease c.) Direct dermal inoculation such as in tattoo parlors has been associated with disease transmission Incubation period: minimum of 2-3 years; can be as long as 40 years Long Incubation period: M. Leprae multiplies very slowly (doubling every 14 days in mice) The number of bacilli harbored by lepromatous patient on initial diagnosis if far greater than that of any human bacterial disease D. Clinical Manifestations Largely confined to the skin, Upper respiratory tract, testes, and peripheral nerves Most serous sequelae: small nerve fibers are functionally impaired (loss og touch, pain, hot and cold sensation- result of topism for peripheral nerves) E. Major Types CATEGORY Course Skin lesions Acid Fast Organisms (AFB) in skin Nerve Involvement Lepromin skin test Cellmediated immunity Skin infiltrates TUBERCULOID LEPROMATOUS Nonprogressive; benign Macular Few Severe, sudden, asymmetric Positive Intact Helper T-cell Progressive; malignant Nodular Abundant
Fig.2: Tuberculoid leprosy
Fig.3 Tuberculoid type of leprosy
Fig. 4 Leonine Facies- Lepromatous Leprosy
Slow symmetric Negative Deficient Suppressor TCells
Fig. 5 Leonine Fascie- lepromatous type of leprosy
F. Lepromin Test - Intradermal skin test using heat killed human or armadillo derived M. Leprae - Not diagnostic - Test lacks specificity
- Can be induced in normal healthy individuals by vaccination with BCG G. Laboratory Diagnosis 1. Demonstration of AFB (acid-fast bacilli) in smears of: a. Nasal scrapings b. Skin lesions c. Ear lobes- lower temp; organisms can be taken from here 2. Tissue sections 3. Biopsy of Skin or thickened nerve 4. Culture in footpads of mice
Fig.6 Section of the skin, showing abundant organisms (acid-fast bacilli)
- Slow growing - Grow optimally at low temp. (32C) - Shares other antigens with other mycobacteria - Inhibits water and marine organism - Incubation period: 2-3 weeks - Infection follows: o After minor trauma in infected swimming pools, aquariums or natural bodies of water o Trauma from fish spines or nips by crustaceans *Infection is common among fish handlers and swimmers - Disease almost always confined to superficial cooler body tissues, most often on the extremities - Typical presentation: Single inflammatory nodule that is seen in the elbows, knees or on the feet of swimmers, or hands of fish handlers begin as small papulesenlarges acquire a blue purple hue suppuration progress to ulceration Take note: lesions are called swimming pool granulomas or fish-tank granulomas B. Diagnosis 1. Culture of skin lesions (definitive diagnosis) Organisms grow best at 30C35C 2. Histologic exam Presence of granuloma + clinical history (suggestive of the diagnosis) *most strains are resistant to IMH, para-amino-salicylic acid and streptomycin C. Treatment *most strains are resistant to INH, PAS and SM 1. good results with Rifampicin and EMB 2. Tetracyclines 3. TMP- SMX
Fig. 7 Section of the Skin, Acid fast bacilli, underneath the dermis
H. Treatment - Sulfones - Rifampicin - Clofazimine *take note: treatment should be continued until skin smears become negative I. Prevention and Control 1. Identification and treatment of case 2. Children of presumably contagious parents has rendered them noninfectious
---------------------------------------------------------------II. MYCOBACTERIUM MARINUM A. Diagnostic Features - From salt water dead fish - Can cause tuberculosis
Fig. 8
- Prevalent in Australia (median age group 50-66) and Africa (peak age 515) Take note: (worldwide infection) *1st most common: mycobacterium tuberculosis *2nd most common: mycobacterium leprae *3rd most common: mycobacterium ulcerans B. Transmission - not fully understood - linked in contaminated water 1. abraded skin 2. probably via skin trauma (contaminated with water, soil or vegetation) 3. insects play an important role - ONLY mycobacterium to cause disease by the production of TOXINS - Toxins produced are called Mycolactum - lipid molecule, it diffuses at the side of infection and at the surrounding skin to kill the surrounding cells and suppresses the immune response of the patient - lesion begins as a nodule ulcerates over 4-6 weeks Centers of ulcer necrotic without ceasation Organisms are located at the periphery, adjacent to normal tissue C. Treatment Success has been reported with: 1. Local heat, excision and skin grafting 2. Combination of either INHStreptomycin or diaminodiphenylsulfone plus oxytetracycline 3. Combination of SMX, RMP and minocycline Supposed to be red acid-fast bacterium (but the picture given was black and white) ---------------------------------------------------------------III. MYOBACTERIUM ULCERANS A. Diagnostic Features - Slow growing, belongs to a large group of environmental Mycobacteria - Inhabits water where it can colonize aquatic plants, herbivorous animals and aquatic insects - Endemic in countries with tropical rainforest - Causes chronic, painless, cutaneous ulcers (Buruli ulcers- Uganda; Bairnsdale ulcers- Australia) - Prefer cooler temperatures (30C35C) seen at the extensors of the body (hands and feet) - Ulcers: seen in extensor surface of extremities
Fig. 9 lesions on the hand
Lesion seen in the arm with hemorrhage and ulceration
Note the location of the lesion. Mycobacterium likes to stay at cooler temp part of the body
Caused by Mycobacterium ulcerans
____________
___fin_______
____
Luke, I am your Father -Darth Vader ------------------------------------------------------------From BUNNY FRIL: ***HELLO Everyone! Hello Friends and Fiends! (wag ng isa-isahin, saying ung ink!) STUDY WELL!!! And WE ROCK!!! ***first tranx na ginawa namin, kaya pagpasensyahan niyo na ha. ***this tranx were based from the powerpoint, recording, previous tranx and some infos were pulled out from nursery books. *** Lizette! Ikaw na ang may malaking tooooot IKAW NA ! IKAW NA ANG MAY LAHAT!!! From THE CHIEF: ***DISCLAIMER: kapag may mali, please inform the batch agad (thru FB or whatever means). Thank you. AND walang sisihan!!!hahaha hope this tranx will suffice. ***ung pictures, baka malabo kapag xinerox na, nasa FB naman ung powerpoint slides, so check
nalang, pampa-KAPAL at pampadami lang yan actually. Hahaha *** Limtra Boys! Limtra Girls! Limtra boy/girl? mga squatter ng Limtra! At sa mga naka-apak na dun! WE SUCK!!!hahaha BAWAL ANG BOBODOBO!!! MAG-ARAL at ischedule na ang next steak-out!
Anda mungkin juga menyukai
- Anti FungalsDokumen5 halamanAnti FungalskakuBelum ada peringkat
- Pathology Block 2 CandyDokumen44 halamanPathology Block 2 CandyAndleeb ImranBelum ada peringkat
- Skin Structure and Function GuideDokumen10 halamanSkin Structure and Function GuideyassrmarwaBelum ada peringkat
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Dokumen18 halamanPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiBelum ada peringkat
- PATH All TA Reviews Answers and Notes11Dokumen718 halamanPATH All TA Reviews Answers and Notes11Andleeb Imran100% (1)
- CH 2 - Inflammation II Compatibility Mode PDFDokumen19 halamanCH 2 - Inflammation II Compatibility Mode PDFHussam AL-AmirBelum ada peringkat
- PathologyDokumen30 halamanPathologyTenorski baritonBelum ada peringkat
- Abdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsDokumen6 halamanAbdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsMon Ordona De GuzmanBelum ada peringkat
- SYPHYLISDokumen1 halamanSYPHYLISkhadzxBelum ada peringkat
- NephroticDokumen8 halamanNephroticsangheetaBelum ada peringkat
- +++++great Review Path Notes & Pics+++++Dokumen430 halaman+++++great Review Path Notes & Pics+++++patriciacafBelum ada peringkat
- Pelvis and Perineum Clinical CorrelationDokumen4 halamanPelvis and Perineum Clinical CorrelationKeesha Mariel AlimonBelum ada peringkat
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDokumen5 halamanEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriBelum ada peringkat
- IV Fluid ChartDokumen2 halamanIV Fluid Chartbenny christantoBelum ada peringkat
- Skin and MSK EverythingDokumen31 halamanSkin and MSK EverythingBernard HernandezBelum ada peringkat
- Kidney Physiology (Q & A)Dokumen28 halamanKidney Physiology (Q & A)ramadan100% (1)
- Chronic Inflammatory Dermatoses Inflammatory Blistering DisordersDokumen4 halamanChronic Inflammatory Dermatoses Inflammatory Blistering DisordersspringdingBelum ada peringkat
- Nephrotic Syndrome WikipediaDokumen10 halamanNephrotic Syndrome WikipediaJohn KevlarBelum ada peringkat
- Non-Pathogenic Intestinal Amoebae Cyst MorphologyDokumen2 halamanNon-Pathogenic Intestinal Amoebae Cyst MorphologyCoy NuñezBelum ada peringkat
- Somatosensory Pathways: Primary Sensory and Motor AreasDokumen36 halamanSomatosensory Pathways: Primary Sensory and Motor AreasAnonymous w3vYureBelum ada peringkat
- Microbology of Urinary Track Infection Kel 1Dokumen29 halamanMicrobology of Urinary Track Infection Kel 1Alfred L ToruanBelum ada peringkat
- Most Common Medical Conditions and DiseasesDokumen3 halamanMost Common Medical Conditions and Diseasesazul2233Belum ada peringkat
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDokumen19 halamanNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamBelum ada peringkat
- LOOK! Neuroscience Brainstorm 2010Dokumen32 halamanLOOK! Neuroscience Brainstorm 2010genome12345Belum ada peringkat
- Pulmonary Path PearlsDokumen33 halamanPulmonary Path PearlsCristi Popescu100% (1)
- Renal SyndromeDokumen13 halamanRenal SyndromeAndreas KristianBelum ada peringkat
- Exam 2 Study Guide 2018Dokumen21 halamanExam 2 Study Guide 2018EvanBelum ada peringkat
- 5 Cyto AbnormalDokumen9 halaman5 Cyto AbnormalMerli Ann Joyce CalditoBelum ada peringkat
- Cytogenetics Basics: Chromosomes, Analysis & AbnormalitiesDokumen11 halamanCytogenetics Basics: Chromosomes, Analysis & Abnormalitiesjo_jo_mania100% (1)
- Nephrotic Nephritic SyndromsDokumen4 halamanNephrotic Nephritic SyndromsKimiwari100% (2)
- Disease PDFDokumen6 halamanDisease PDFJohn Christopher LucesBelum ada peringkat
- Cytogenetics Note PDFDokumen14 halamanCytogenetics Note PDFMerjema Bahtanović100% (1)
- Kidney NewDokumen4 halamanKidney NewParth BhayanaBelum ada peringkat
- Gram Positive Cocci: Golden Staff of MosesDokumen8 halamanGram Positive Cocci: Golden Staff of MosesAnna A.Belum ada peringkat
- Actinic Keratosis: (Aka Bowen's Disease)Dokumen5 halamanActinic Keratosis: (Aka Bowen's Disease)fadoBelum ada peringkat
- Chart - WBC DisordersDokumen1 halamanChart - WBC DisordersSamuel RothschildBelum ada peringkat
- AtelectasisDokumen3 halamanAtelectasisLouis FortunatoBelum ada peringkat
- Major Bacterial Genera TableDokumen12 halamanMajor Bacterial Genera TablemojdaBelum ada peringkat
- Goljan Notes on Oxygen Transport and Tissue HypoxiaDokumen5 halamanGoljan Notes on Oxygen Transport and Tissue HypoxiaDaniyal AzmatBelum ada peringkat
- Zanki Respiratory PathologyDokumen15 halamanZanki Respiratory Pathologysmian08100% (1)
- Basic SuturingDokumen17 halamanBasic SuturingWahyu HidayatBelum ada peringkat
- Patho CA - Acute PancreatitisDokumen1 halamanPatho CA - Acute PancreatitisKBelum ada peringkat
- MCB 252 Final Exam Study GuideDokumen62 halamanMCB 252 Final Exam Study GuideJay ZBelum ada peringkat
- Adequacy Criteria: ExceptionsDokumen3 halamanAdequacy Criteria: ExceptionsPranayBelum ada peringkat
- Genetic Disorders-Www - Qworld.co - inDokumen13 halamanGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- USMLE Logistic Packet For IMGs-1Dokumen7 halamanUSMLE Logistic Packet For IMGs-1Brian VianaBelum ada peringkat
- 7sgdfgf PDFDokumen438 halaman7sgdfgf PDFPratik JadhavBelum ada peringkat
- University of Santo Tomas: Faculty of Pharmacy - Department of Medical TechnologyDokumen7 halamanUniversity of Santo Tomas: Faculty of Pharmacy - Department of Medical TechnologyWynlor AbarcaBelum ada peringkat
- Chapter 3 Genetic VariationDokumen21 halamanChapter 3 Genetic VariationAbdulkarimBelum ada peringkat
- Benign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDokumen83 halamanBenign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDian Permata PutraBelum ada peringkat
- Leukemia and Lymphoma OverviewDokumen2 halamanLeukemia and Lymphoma OverviewAyeshaArifBelum ada peringkat
- Pathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & ThymusDokumen5 halamanPathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & Thymusangel_sagun_1Belum ada peringkat
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDokumen4 halaman4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaBelum ada peringkat
- VirologyLearnTable 2017-Sketchy PDFDokumen4 halamanVirologyLearnTable 2017-Sketchy PDFdfgbdfgBelum ada peringkat
- Histo Review 2Dokumen13 halamanHisto Review 2Coy NuñezBelum ada peringkat
- Zanki (Complete) + R/medicalschoolanki Microbiology ErrataDokumen70 halamanZanki (Complete) + R/medicalschoolanki Microbiology ErrataedBelum ada peringkat
- Anaerobic Infections in HumansDari EverandAnaerobic Infections in HumansSydney FinegoldPenilaian: 5 dari 5 bintang5/5 (1)
- Pharmacodynamics 2Dokumen8 halamanPharmacodynamics 2Pinay YaunBelum ada peringkat
- 2011 07 Microbiology Skin Diseases1Dokumen8 halaman2011 07 Microbiology Skin Diseases1dtimtimanBelum ada peringkat
- PharmacokineticsDokumen8 halamanPharmacokineticsPinay YaunBelum ada peringkat
- Approach To Patient With Allergic Diseases: Jovilia M. Abong, M.D. FPCP, Fpsaai, MSCDokumen65 halamanApproach To Patient With Allergic Diseases: Jovilia M. Abong, M.D. FPCP, Fpsaai, MSCCristinaConcepcionBelum ada peringkat
- 2011 087 Microbiology Intro To Mycology FinalDokumen7 halaman2011 087 Microbiology Intro To Mycology FinalCristinaConcepcionBelum ada peringkat
- Micro Metab RJDokumen5 halamanMicro Metab RJPinay YaunBelum ada peringkat
- 2011-07 - MIcrobio-Bacteria Skin Infection 2Dokumen10 halaman2011-07 - MIcrobio-Bacteria Skin Infection 2dtimtimanBelum ada peringkat
- Pharma Basic ToxicologyDokumen8 halamanPharma Basic ToxicologyCristinaConcepcionBelum ada peringkat
- 2 - Inflammation and Repair (Edited Ver)Dokumen149 halaman2 - Inflammation and Repair (Edited Ver)CristinaConcepcionBelum ada peringkat
- 2011 07 MICROBIO LAST PAGE of Bacterial Skin Infection 2Dokumen1 halaman2011 07 MICROBIO LAST PAGE of Bacterial Skin Infection 2CristinaConcepcionBelum ada peringkat
- 2011 06 MICRO Intro To VirologyDokumen8 halaman2011 06 MICRO Intro To VirologydtimtimanBelum ada peringkat
- Lect Notes - Bacterial Genetics 2012-2013Dokumen10 halamanLect Notes - Bacterial Genetics 2012-2013CristinaConcepcionBelum ada peringkat
- Experiment 1 in Pharmacology 2012 (Dokumen11 halamanExperiment 1 in Pharmacology 2012 (CristinaConcepcionBelum ada peringkat
- BeneficenceDokumen31 halamanBeneficenceCristinaConcepcion100% (1)
- Cell Injury Lecture TranscriptionDokumen19 halamanCell Injury Lecture TranscriptionCristinaConcepcionBelum ada peringkat