CordBlood and Heart Damage An 2009)
Diunggah oleh
Suria NitaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CordBlood and Heart Damage An 2009)
Diunggah oleh
Suria NitaHak Cipta:
Format Tersedia
Cell Transplantation, Vol. 18, pp. 855868, 2009 Printed in the USA. All rights reserved.
Copyright 2009 Cognizant Comm. Corp.
0963-6897/09 $90.00 + .00 DOI: 10.3727/096368909X471170 E-ISSN 1555-3892 www.cognizantcommunication.com
Autologous Umbilical Cord Blood Mononuclear Cell Transplantation Preserves Right Ventricular Function in a Novel Model of Chronic Right Ventricular Volume Overload
Can Yerebakan,* Eugen Sandica,* Stephanie Prietz,* Christian Klopsch,* Murat Ugurlucan,* Alexander Kaminski,* Sefer Abdija, Bjorn Lorenzen, Johannes Boltze, Bjorn Nitzsche, Dietmar Egger, Malte Barten,# Dario Furlani,* Nan Ma,* Brigitte Vollmar,** Andreas Liebold,* and Gustav Steinhoff*
*Department of Cardiac Surgery, Medical Faculty, University of Rostock, Rostock, Germany Department of Cardiology, Ruppiner Clinics, Neuruppin, Germany Department of Diagnostic and Interventional Radiology, Medical Faculty, University of Rostock, Rostock, Germany Fraunhofer Institute for Cell Therapy and Immunology, Translational Center of Regenerative Medicine, Leipzig, Germany Vita 34 AG, Leipzig, Germany #Institute for Pathology, Medical Faculty, University of Rostock, Rostock, Germany **Institute for Experimental Surgery, Medical Faculty, University of Rostock, Rostock, Germany
We aimed to evaluate the feasibility and efficacy of autologous umbilical cord blood mononuclear cell (UCMNC) transplantation on right ventricular (RV) function in a novel model of chronic RV volume overload. Four-month-old sheep (n = 20) were randomized into cell (n = 10) and control groups (n = 10). After assessment of baseline RV function by the conductance catheter method, a transannular patch (TAP) was sutured to the right ventricular outflow tract (RVOT). Following infundibulotomy the ring of the pulmonary valve was transected without cardiopulmonary bypass. UCMNC implantation (8.22 6.28 107) in the cell group and medium injection in the control group were performed into the RV myocardium around the TAP. UCMNCs were cultured for 2 weeks after fluorescence-activated cell sorting (FACS) analysis for CD34 antigen. Transthoracic echocardiography (TTE) and computed tomography were performed after 6 weeks and 3 months, respectively. RV function was assessed 3 months postoperatively before the hearts were excised for immunohistological examinations. FACS analysis revealed 1.2 0.22% CD34+ cells within the isolated UCMNCs from which AcLDL+ endothelial cells were cultured in vitro. All animals survived surgery. TTE revealed grade IIIII pulmonary regurgitation in both groups. Pressurevolume loops under dobutamine stress showed significantly improved RV diastolic function in the cell group (dP/dtmin: p = 0.043; Eed: p = 0.009). CD31 staining indicated a significantly enhanced number of microvessels in the region of UCMNC implantation in the cell group (p < 0.001). No adverse tissue changes were observed. TAP augmentation and pulmonary annulus distortion without cardiopulmonary bypass constitutes a valid large animal model mimicking the surgical repair of tetralogy of Fallot. Our results indicate that the chronically volumeoverloaded RV profits from autologous UCMNC implantation by enhanced diastolic properties with a probable underlying mechanism of increased angiogenesis. Key words: Tetralogy of Fallot; Right ventricular dysfunction; Pulmonary insufficiency; Umbilical cord blood; Stem cells
INTRODUCTION Tetralogy of Fallot (TOF) is one of the most common cyanotic congenital heart defects. Surgical repair is inevitable and aims to normalize jeopardized pulmonary blood flow by correcting the abnormal anatomy of the
right ventricular outflow tract (RVOT) caused by anterior and leftward displacement of the infundibular septum. Hence, the closure of ventricular septal defect(s) and the resection of the hypertrophied trabecular muscle bands in the right ventricle (RV) followed by transannular patching is the standard corrective surgery. However,
Received November 3, 2008; final acceptance April 6, 2009. Online prepub date: April 9, 2009. Address correspondence to Can Yerebakan, M.D., Department of Cardiac Surgery, Medical Faculty, University of Rostock, Schillingallee 35, 18057, Rostock, Germany. Tel: +49 494 381 6101; Fax: +49 494 381 6102; E-mail: can.yerebakan@med.uni-rostock.de
855
856
YEREBAKAN ET AL.
additional infundibulectomy with RVOT enlargement performed during the correction may predispose to RVOT aneurysms, akinetic myocardial regions, and pulmonary regurgitation with chronic right ventricular (RV) volume overload. The latter, though well tolerated in the short term, is the most dominant factor contributing to late morbidity and mortality of patients (18). Currently, routine and generous transannular patch type of repair has therefore been abandoned. Rather limited RVOT patching with the preservation of pulmonary valve function, if possible, is the preferred strategy (16). Nevertheless, development of RV dysfunction in the long term still remains a challenge and requires further animal and human studies to establish protective strategies. To date, however, the literature lacks a valid in vivo experimental model mimicking the postsurgical scenario of TOF patients. Recent discoveries seem to overcome the historical consideration of the heart as a postmitotic organ, and the detection of residing cardiac stem cells able to regenerate damaged myocardium has fueled great attention for cellular cardiomyoplasty (5,7,34,42). Although different stem cells have been used in experimental and clinical settings, the ideal source for stem cell harvesting is still in debate. The ideal source of stem cells should possess properties such as genetic compatibility, pluripotency, and, especially for cardiac therapies, the ability to gain cardiomyocyte traits. Umbilical cord blood (UCB) is known to accommodate a considerable number of multipotent stem/progenitor cells (19,26,29,32,40) and can easily be obtained during birth. Moreover, mononuclear cells isolated from the UCB have been successfully employed in experimental approaches for myocardial repair and regeneration, which can be expanded in vitro and then transplanted (20,21,23,25,30,38). Latest literature provides only a limited number of studies that investigate the effects of stem cells on RV dysfunction (9,46). No experimental approach has been conducted to study the potential of stem cell treatment in case of RV volume overload. Hence, the aim of our experimental design was to evaluate the effects of intramyocardial transplantation of autologous umbilical cord blood mononuclear cells (UCMNCs) on RV function in a novel experimental surgical model of RV volume overload in sheep. MATERIALS AND METHODS Animals All procedures were approved by the local Animal Care Committee of Mecklenburg/Vorpommern in Rostock, Germany. Animals received humane care in compliance with the Principles of Laboratory Animal Care formulated by the National Society for Medical Research and the Guide for the Care and Use of Laboratory Animals
prepared by the Institute of Laboratory Animal Resources and the US National Institutes of Health. Four-month-old domestic sheep (n = 20) were used. Animals were randomly assigned to two groups as, the cell group (n = 10, mean weight: 41.1 5.2 kg), which received intramyocardial UCMNC implantation, and the control group, which received medium only (n = 10, mean weight: 37.9 4.9 kg). Autologous UCB Collection and Isolation of UCMNCs Collection and cryopreservation of autologous ovine UCB was performed by VITA 34 (Vita 34 AG, Leipzig, Germany). After the collection of the UCB samples, dimethyl sulfoxide was added and the UCB was stored in liquid nitrogen tanks with a temperature of 141C according to standard operating procedures. Mononuclear cells (MNC) were isolated from UCB using the Pancoll (density 1.086 g/ml, PAN-Biothech GmbH, Aidenbach, Germany) density gradient separation technique according to the manufacturers protocol. Thereafter, definite cell count was determined. Total mononuclear cell suspension in IMDM of 1 ml volume was prepared as final product for autologous transplantation on the day of the operation. Flow Cytometry of the Mononuclear Cell Fraction and Cell Cultures From UCMNCs Only for quantification of antigen expression within the isolated mononuclear cell fraction, fluorescence-activated cell sorting (FACS, FACS Scan flow cytometer; Becton Dickinson, San Jose, CA, USA) analysis was performed. Cells were incubated with antibodies against CD34 (CD34 goat polyclonal IgG, Santa Cruz, Santa Cruz, CA, USA). Subsequently, donkey anti-rabbit AlexaFluor 488 or secondary antibody (Invitrogen, Carlsbad, CA, USA) was applied. Samples lacking primary antibody incubation were used as negative controls. After isolation from umbilical cord blood the UCMNC fraction was resuspended in endothelial media (MCDB 131 Medium; Sigma Aldrich) and transferred to a culture flask. After 14 days of cultivation in endothelial media culture, AcLDL (low-density lipoprotein from human plasma, acetylated, Alexa-Fluor 488 conjugated; Molecular Probes) staining was performed according to the manufacturers instruction. These investigations were instituted to define the cell surface markers within the total mononuclear cell suspension, which was isolated from the umbilical cord blood and was delivered intramyocardially. Surgical Procedure Animals were premedicated with an intramuscular injection of 0.10.5 mg/kg xylazin (Rompun 2%, Bayer Vital GmbH, Leverkusen, Germany) and 1020 mg/kg
UCMNC TREATMENT IN CHRONIC RV VOLUME OVERLOAD
857
Ketamin 10% (Bela-Pharm GmbH & Co. KG, Vechta, Germany). After intubation anesthesia was maintained by inhalation of 1.5% to 2.5% isoflurane delivered through a ventilator (Excel 210 SE, Ohnmeda-BOC Group, Madison, WI, USA). Oxygen was added to the respiratory circle with the aim of a peripheral arterial saturation of over 94%. Invasive arterial blood pressure was measured through right femoral artery line, central venous pressure was measured through the right jugular vein, and peripheral arterial saturation was monitored with a pulse oxymeter in a continuous fashion. Creation of Chronic Right Ventricular Volume Overload A novel model for chronic RV volume overload mimicking hemodynamic properties after the correction of TOF was created by transannular patch (TAP) implantation and pulmonary valve distortion in the RVOT (Fig. 1af). For this purpose, a left anterior thoracotomy was performed along the 5th or 6th intercostal space and the RVOT was exposed. A TAP (Gelweave woven vascular prosthesis, Vacutek Ltd., Terumo, Refrewshire, Scotland) was sutured from the infundibulum to the main pulmonary artery reaching approximately 2 cm below and 2 cm above the pulmonary annulus on the RVOT with continuous 5/0 polypropylene (Ethicon, Norderstedt, Germany). Thereafter, an incision in the RVOT was performed through an opening in the patch
and the pulmonary valve ring was transected bluntly with scissors via the infundibulotomy without the need for extracorporal circulation. Experimental Design Each animal underwent two surgeries. During the first operation as described above, a TAP with infundibulotomy and a transsection of the pulmonary valve ring with the aim of creating pulmonary regurgitation were conducted following baseline hemodynamic measurements with conductance catheters. Postprocedural hemodynamic parameters were assessed to validate acute pulmonary regurgitation. Thereafter, 1 ml of UCMNC suspension for the animals of the cell group and 1 ml of medium (10 injections of 0.1 ml) to each control animal were injected intramyocardially into the RV free wall below the inferior border of the transannular patch in two rows with a special self-constructed tuberculin syringe with an epicardial stopper (a shorter 21-gauge needle slided over the original 30-gauge needle) to prevent ventricular perforation and outflow of the cell suspension during injection. All animals received a preoperative single dose of 0.1 mg/kg body weight dexamethasone (Dexa-ratiopharm, Ratiopharm GmbH, Ulm, Germany) intravenously to prevent inflammation induced by multiple intramyocardial injections as described before by Borenstein and collegues (9). Although proliferative effects of dexamethasone on UCMNC have been
Figure 1. Steps of the novel technique for the creation of the pulmonary insufficiency with TAP implantation. (a) Exposure of the RVOT through a left anterior thoracotomy. (b) Preoperative conductance catheter measurements via main pulmonary artery. (c) TAP implantation on the RVOT. (d) Completed TAP on the RVOT. (e) RVOT incision and pulmonary valve ring transsection through an opening on the TAP. (f) Closure of the patch incision after side clamping of the TAP and postoperative conductance catheter measurements. Scale bars: 1 cm.
858
YEREBAKAN ET AL.
described in vitro (24), the single preoperative dose that was instituted in our series in vivo did not target a proliferative response of the administered cells. Echocardiography was performed 6 weeks after the first operation to assess the grade of pulmonary regurgitation. Thirty-two-slice cardiac computed tomography (CT) (Toshiba, Aquilion 32, Toshiba Medical Systems Corp., Tochigi, Japan) was performed for the detection of any adverse tissue formation (e.g., calcification, tumor formation) 1012 weeks postoperatively. The blinded radiologists were asked to indicate any presence and location of possible myocardial calcifications and tissue changes. The second operation was performed 12 weeks after the first operation. Online pressurevolume loop analysis was again conducted for each animal under baseline and dobutamine stress conditions (310 g/kg/min, target heart rate of 200210/min). Analysis of Myocardial Function PressureVolume Loops. A combined pressure volume conductance catheter 5 F (Millar Instruments, Houston, TX, USA) was inserted into the RV through a small stab wound in the pulmonary artery. The conductance catheter was connected to one pressurevolume transducer system for pressure (Millar MPVS 300, EMKA Technologies, Paris, France) and another volume transducer system for volume analysis (Sigma 5 DF, CD Leycom, Zoetermeer, The Netherlands). Transducer systems were linked to the Millar PowerLab data acquisition hardware (Type ITF 16, EMKA Technologies) and real-time signal processing was performed by IOX 1.8.3.20 software (EMKA Technologies). The reference
values for volumetric analysis were obtained in triplicate via the thermodilution method using a Swan-Ganz-catheter (Arrow International Inc., Reading, PA, USA). The mean was saved for offline factor calibration. Parallel conductance was measured by using hypertonic saline (injection of 5 ml of 10% NaCl into the right atrium). Thereafter a 23-mm balloon catheter (Fogarty Occlusion Catheter, 8-22 F, Edward Lifesciences LLC, Irvine, CA, USA) was advanced through the right atrium into the inferior vena cava for standardized preload reduction maneuvers. A series of three caval occlusions of 10 pressurevolume loops was gained during apnea. Maximum pressure (Pmax), end-diastolic pressure (EDP), enddiastolic and end-systolic volume (EDV, ESV), ejection fraction (EF), cardiac output (CO), stroke volume (SV), maximal slope of systolic pressure increment (dP/dtmax), diastolic pressure decrement (dP/dtmin), end-diastolic pressure volume relation (EDPVR), and end-systolic pressure volume relation (ESPVR) slopes (Eed and Ees, respectively), and preload recruitable stroke work (PRSW) were determined. We applied a volume intercept at a fixed pressure within the pressure range [20 mmHg for baseline measurements (V20) and 40 mmHg for dobutamine stress examinations (V40), respectively], thus avoiding the insecurity of a linear extrapolation of ESPVR to zero pressure. Accordingly, for the positioning of the EDPVR, we used a pressure intercept at a fixed volume within the volume range to evade linear extrapolation of EDPVR to zero volume [40 ml for baseline conditions (P40) and 20 ml for dobutamine conditions (P20)] (14). Echocardiography. Transthoracic echocardiography (Vivid, GE Healthcare, Milwaukee, WI, USA) was performed by a cardiologist blinded to the distribution of
Figure 2. Representative FACS plot of CD34+ antigen (A) and subsequent AcLDL+ cells (B) after 14 days of cultivation in endothelial cell medium. Red line: positive, black line: control. M1: gating strategy.
UCMNC TREATMENT IN CHRONIC RV VOLUME OVERLOAD
859
Table 1. Pressure-Volume Loop Measurements With Comparison of the Right Ventricular Function Between the Cell and Control Groups and Within Each Group for Different Time Points Day 90 After TAPI Dobutamine Stress Control (n = 8) 46.51 3.69 Cell (n = 7) 54.12 5.00
Day 0 Before TAPI Baseline Control (n = 9) 26.87 1.70 n.s. 11.56 1.06 n.s. 415.08 25.21 n.s. 310.11 15.49 n.s. 67.76 6.00 n.s. 18.93 3.66 n.s. 72.74 4.21 n.s. 4273.05 349.60 n.s. 48.90 4.86 n.s. n.a. n.a. 42.65 1.97 3760.21 123.40 75.40 3.41 14.46 2.47 57.12 2.67 329.30 30.95 439.19 35.79 10.08 0.97 Cell (n = 9) 26.82 1.39
Day 0 After TAPI Baseline Control (n = 9) 31.01 1.64 0.008* 15.69 1.33 Cell (n = 9) 29.91 0.97 0.023 12.04 0.86 0.016* 508.26 26.08 0.039 324.42 18.28 0.641 90.24 17.57 0.023 38.86 9.28 0.008 54.64 4.21 0.008 4955.98 1109.70 0.078 51.37 9.58 0.195 n.a.
Day 90 After TAPI Baseline Control (n = 8) Cell (n = 7)
Parameter Pmax (mmHg) p p EDP (mmHg) p p dp/dtmax (mmHg/s) p p dp/dtmin (mmHg/s) p p EDV (ml) p p ESV (ml) p p EF (%) p p CO (ml/min) p p SV (ml) p p PRSW (ml mmHg) p Eed (mmHg/ml) p
30.43 26.86 3.17 2.29 0.383* 0.938 0.278 9.38 0.50 0.055 11.65 2.33 0.148* 0.852
0.235 12.13 9.53 1.72 1.48 1.000 0.279 1512.79 84.81 1881.98 135.06
476.85 43.24 0.039* 331.37 25.33 0.148* 103.89 10.83 0.008* 43.18 7.38 0.008* 58.51 4.35 0.008* 5583.95 651.24 0.023* 60.76 7.07 0.055* n.a.
432.26 326.83 74.95 47.06 0.945* 0.078 0.271 246.14 254.44 28.63 25.32 0.055* 0.078 0.834 47.81 49.87 7.07 6.67 0.055* 0.109 0.837 19.86 18.18 4.84 3.85 0.641* 0.297 0.794 61.56 66.87 4.73 5.10 0.078* 0.156 0.459 2925.27 3102.04 363.41 269.34 0.008* 0.016 0.709 27.97 31.70 2.71 3.08 0.008* 0.031 0.378 16.37 12.41 2.57 1.54 0.224 0.21 0.08 0.731 0.17 0.04
0.033 665.49 44.94 902.89 101.61
0.043 27.94 3.87 31.09 1.69
0.491 9.45 2.78 0.297 69.48 4.85 74.75 4.41 7.87 1.30
0.441 3809.28 340.04 5044.78 444.19
0.094 18.50 1.67 23.28 1.83
0.075 23.83 26.23 2.84 2.69 0.553 0.67 0.10 0.009 0.29 0.07
n.a.
n.a.
n.a.
n.a.
860
YEREBAKAN ET AL.
Table 1. Continued Day 90 After TAPI Dobutamine Stress Control (n = 8) n.a. Cell (n = 7) n.a.
Day 0 Before TAPI Baseline Control (n = 9) n.a. Cell (n = 9) n.a.
Day 0 After TAPI Baseline Control (n = 9) n.a. Cell (n = 9) n.a.
Day 90 After TAPI Baseline Control (n = 8) 5.07 2.16 0.809 n.a. Cell (n = 7) 5.67 1.03 n.a.
Parameter P40 (mmHg) p P20 (mmHg) p Ees (mmHg/ml) p V20 (ml) p V40 (ml) p
n.a.
n.a.
n.a.
n.a.
12.36 7.50 1.69 1.29 0.044 2.78 0.64 0.699 n.a. n.a. 2.48 0.38
n.a.
n.a.
n.a.
n.a.
1.20 0.18 0.228
0.85 0.21
n.a.
n.a.
n.a.
n.a.
27.10 30.93 5.53 4.22 0.600 n.a. n.a.
n.a.
n.a.
n.a.
n.a.
14.62 13.67 3.04 3.89 0.829
Values are presented as mean SEM. n.s.: no significance; Vx, volume intercept for a given pressure of x; Px, pressure intercept for a given volume of x. *Versus control day 0 before transannular patch implantation (TAPI) under baseline conditions. Versus cell day 0 before TAPI under baseline conditions. Control versus cell day 90 after TAPI under baseline conditions. Control versus cell day 90 after TAPI under dobutamine stress conditions.
the groups 6 weeks postoperatively. Parasternal long and short axis views were obtained with both M-mode and two-dimensional echocardiography images. Right ventricular end-diastolic and end-systolic volume (RVEDV, RVESV) as well as right and left ventricular ejection fraction (RVEF, LVEF) were determined. The grade of pulmonary insufficiency was scaled in four categories as grade I (minimal), II (mild), III (moderate), and IV (severe). Morphological and Histological Studies After the measurements in the second surgery hearts were arrested with potassium chloride and rapidly excised. The postmortem RVOT preparations were photographed for macroscopic assessment. Paraffin-embedded 10-m sections of the RVOT from the region of UCMNC transplantation were used for immunohistochemistry. Hematoxylin-eosin, Goldner, and Kossa stainings were applied for histological investigation of the myocardium with regard to morphology of the myocytes, integrity of the myocardium, detection of fibrosis, and calcifications. The area of fibrosis (in m2) was analyzed with com-
puter-assisted planimetry at the region of TAP in eight different sections for each animal with 20 different highpower fields (HPF) of 0.216 mm2 per section. Immunohistochemical staining with CD-31 antibody [PECAM-1(M-20) goat polyclonal IgG; Santa Cruz Biotechnology, CA, USA] followed by donkey anti-goat Alexa-Fluor 568-conjugated secondary antibody (Invitrogen) was performed around the region of the TAP and cell/medium injection for comparison of capillary density between the groups. Sections were then counterstained with DAPI. Four sections of the RV myocardium of each animal along the TAP implantation region and further four sections 1 cm remote from the area of TAP were analyzed using confocal microscopy. Twenty highpower fields (0.216 mm2) in each section were randomly selected, and the number of capillaries in each field was averaged and expressed per mm2. Statistical Analysis Data are presented as mean SE. Statistical analysis was carried out with the SPSS software package (SPSS Inc). For time- and procedural-dependent comparison
UCMNC TREATMENT IN CHRONIC RV VOLUME OVERLOAD
861
between pre- and postoperative RV function within the groups, the Wilcoxon signed-rank test was chosen. For overall comparison between the experimental groups data were subjected to one-way analyses of variance (ANOVA) method that applies post hoc multiple HolmSidak tests, the nonparametric Kruskal-Wallis (failing normality), or post hoc multiple Dunn tests. Values of p < 0.05 were considered statistically significant. RESULTS Experimental Outcome No mortality was registered due to the surgical procedure. Three animals died postoperatively. In the cell group, one animal suffered from severe pneumonia and died on the 11th postoperative day, and the other died during the transport to the CT investigation, probably due to aspiration following premedication. One animal in the control group did not survive late pericardial tamponade in the second postoperative week.
We were able to create standardized acute pulmonary regurgitation in all animals with the novel experimental surgical technique, which was confirmed by conductance catheter measurements (see below). In the cell group a mean number of 8.22 6.28 107 UCMNC was successfully transplanted into the RV myocardium around the area of TAP implantation. In the control group medium was injected in the same way and in the region of RV myocardium. The mean weight of the animals before the second operation was 40.8 3.5 and 39.7 4.3 kg, in the cell and control groups, respectively. FACS and Cell Culture FACS studies revealed 1.2 0.22% CD34+ cells of the total mononuclear cell fraction as the end product after isolation from umbilical cord blood before intramyocardial transfer. After 14 days of cultivation of UCMNC in endothelial cell medium we were able to detect cell cultures showing growth of AcLDL+ endothelial cells (Fig. 2). This finding confirmed the existence of the CD34+ cell fraction within the UCMNCs. Right Ventricular Functional Analysis Table 1 contains the data from the monitored hemodynamics during a follow-up period of 90 days. Prior to valvular injury and TAP implantation, RV catheterization did not reveal any significant difference between animals in both experimental groups. Early Postoperative Right Ventricular Functions at Day 0 Systolic Functions. RVEF following RVOT incision and TAP implantation decreased 20% and 28% in control and cell groups, respectively (both p = 0.008). DP/ dtmax was significantly higher when compared to preoperative values in both groups (control group: 15%, cell group: 16%; both p = 0.039). Right ventricular Pmax increased 15% in the control group (p = 0.008) and 12% in the cell group (p = 0.023) postoperatively. Right ventricular ESV following the surgical procedure was 2.3fold and 2.7-fold increased in control and cell groups (both p = 0.008), confirming the RV volume overload due to pulmonary regurgitation. Although there was a significant 31% increase in CO in the control group (p = 0.023), the 32% increase in UCMNC group hearts did not yield a statistically significant change (p = 0.078). Furthermore, SV was augmented but the differences were not significant in both groups when compared to the preoperative values. RV early postoperative systolic functions were similar in both groups. Diastolic Functions. Right ventricular EDV, the main indicator of ventricular volume load, significantly increased postoperatively in both groups (control group:
Figure 3. (A) Slope of end-diastolic pressure volume relation (Eed) and (B) maximal slope of diastolic pressure decrement (dp/dtmin) after 3 months of follow-up under dobutamine stress conditions in comparison of cell and control groups (n = 7 and n = 8, respectively). *p < 0.05.
862
YEREBAKAN ET AL.
Figure 4. Caval vein occlusions performed 3 months postoperatively reflected the contractility and elasticity of the RV occupying surgical PR. The curves of end-diastolic pressure volume relation (EDPVR, green) and end-systolic pressure volume relation (ESPVR, red) were determined under dobutamine-induced stress conditions. The pressure intercept of EDPVR (P20 at a fixed volume of 20 ml) and its slope significantly reduced under dobutamine stress conditions in the cell group (solid loops) when compared with the control group (dashed loops). *p < 0.05.
53% increase, p = 0.008; and cell group: 58% increase, p = 0.023). Further, EDP was significantly elevated by 36% in control animals (p = 0.016) after surgery, whereas the 19% increase found in the cell group was not found to be significant (p = 0.055). DP/dtmin was not significantly different from preoperative values in both groups. Again, the comparison of postoperative parameters between the groups was outside of significant variance.
Long-Term Right Ventricular Functions at Day 90 Systolic Functions. Under baseline conditions in both groups CO and SV were found to be significantly lower than preoperative levels at day 0 (CO in control group: 32%, p = 0.008; CO in cell group: 18%, p = 0.016; SV control group: 43%, p = 0.008; SV cell group: 26%, p = 0.031). Remaining monitored parameters EF, dP/dtmax, Pmax, and ESV were not significantly different
UCMNC TREATMENT IN CHRONIC RV VOLUME OVERLOAD
863
than the preoperative findings in both groups. However, although the derangement of right ventricular CO and SV seemed stronger in the control group than in the cell group, the comparison of systolic functions in between both groups at day 90 did not expose any significant differences under baseline conditions. Similarly under dobutamine stress conditions CO and SV elevations in cell group compared with the control group were again not statistically significant (CO: 32%, p = 0.094; SV: 26%, p = 0.075). In contrast, pharmacologically induced stress augmented the speed of contraction in the cell group more prominently when compared to the control group (dP/dtmax: 24%, p = 0.033). Diastolic Functions. Catheterization after 90 days follow-up reflected no significant differences in EDP and EDV in both groups under baseline conditions when compared with preoperative findings at day 0. Moreover, both groups revealed moderate decreases in dP/ dtmin that did not reach statistical significance late after RVOT incision and TAP implantation (control group: 21%, p = 0.055; cell group: 23%, p = 0.078). Similar to the systolic evaluations, a comparison of diastolic functions between cell group and control group at day 90 did not uncover significant differences under baseline conditions. Again, dobutamine-induced stress led to significantly greater speed of relaxation in the cell group than in the control group (dP/dtmin: 36%, p = 0.043). ESPVR and EDPVR gained by the occlusion of the vena cava inferior revealed the contractility and elasticity indices of the right heart late after surgical PR induction. Drawing curvilinear ESPVR also causes a source of error (11). However, the adequate quantification of the volume intercept of ESPVR within the pressure range did not reveal significant differences between the experimental groups under baseline (V20) and dobutamine stress (V40) conditions. Likewise, Ees did not vary between the groups. On the contrary, under dobutamine stress conditions EDPVR shifted rightward downward in the cell group compared with the control group. The pressure intercept of EDPVR (P20) and Eed were signifi-
cantly reduced by 39% (p = 0.044) and 57% (p = 0.009), respectively (Figs. 3 and 4). Transthoracic Echocardiography After 6 Weeks Echocardiography revealed pulmonary regurgitation in all operated animals. Table 2 shows the absolute values of RVEDV, RVESV, the comparison of RVEF and LVEF, and pulmonary insufficiency grades in both groups. Pulmonary insufficiency grading confirmed a similar extent of pulmonary valve injury when both study groups are compared (control group: 2.50 0.33; cell group: 2.88 0.30; p = 0.19). Figure 5 provides a visualization of the regurgitant flow in the region of the TAP. Cardiac Computed Tomography No adverse tissue changes were detected via cardiac computed tomography before the second operation. We did not add RV functional volumetric parameters that were gained from the CT because breath-holding episodes needed for quantitative analysis would have exposed the animals to a greater risk for hemodynamic compromise. Therefore, CT data did not reveal representative values for the assessment of RV function. Macroscopic and Microscopic Examinations Macroscopy. All hearts occupied a pulmonary valve annulus defect as expected from echocardiography and cardiac CT. At this region fibrinous, reendothelialized tissue covered the TAP. Further, none of the removed hearts provided evidence for intravascular thrombus or tumor formations in the area of interest. Figure 6A represents typical tissue formations and RV organic shape late after RVOT incision and TAP implantation. The RV sections that were used for microscopic investigations are shown in Figure 6B. Microscopy. The analysis of the area of fibrosis at two different levels did not expose any significant differences between the experimental groups at the area of TAP (control group: 5523.07 653.43 m2, cell group: 6256.99 1143.99 m2, p = 0.575), and 1 cm away from the area of TAP (control group: 3826.16 323.87 m2, cell group: 3306.87 472.88 m2, p = 0.371). On the contrary, capillary density in the cell group was dramatically enhanced at both levels when compared with the control group at the area of TAP (control group: 738.83 10.45 capillaries/mm2, cell group: 846.32 22.71 capillaries/mm2, p < 0.001), and 1 cm away from the area of TAP (control group: 721.76 10.88 capillaries/mm2, 918.88 17.69 capillaries/mm2, p < 0.001) (Fig. 7). Again no adverse tissue changes could be detected using microscopic and macroscopic investigations after 3-month follow-up.
Table 2. Right and Left Ventricular Function in the Transthoracic Echocardiography 6 Weeks Postoperatively Cell (n = 6) Control (n = 6)
p n.s. n.s. n.s. n.s. n.s.
RVEDV (ml) 26.6 7.0 26.1 9.4 RVESV (ml) 7.2 3.8 9.0 2.6 RVEF (%) 73.9 9.3 62.6 12.0 LVEF (%) 72.7 3.2 60.3 17.7 Pulmonary insufficiency grade 2.9 0.3 2.5 0.3
864
YEREBAKAN ET AL.
Figure 5. Representative echocardiographic image showing pulmonary regurgitant flow 6 weeks after surgery.
DISCUSSION Diseased myocardium has been one of the most attractive targets of novel regenerative approaches in the current era. The delivery of stem cells to the myocardium has successfully been performed in a considerable number of experimental and clinical trials with a resul-
tant improvement of myocardial performance (6,34,35, 42). Unfortunately, congenital cardiac anomalies have widely been estranged from cell-based cardiac regenerative approaches. TOF belongs to the most common cyanotic congenital heart defects. Although surgical correction reveals superior early postoperative results (2), chronic pulmo-
Figure 6. Macroscopic images of the RVOT postmortem 3 months after TAP implantation. (A) Cross-sectional image through the TAP on the RVOT and pulmonary artery (PA) with presentation of successful valvulotomy (*) of the pulmonary valve (PV) and creation of valvular leakage below the TAP. (B) View from the RV side on the RVOT after TAP implantation. Sections were made in the RVOT at the site of the UCMNC implantation for histological studies.
UCMNC TREATMENT IN CHRONIC RV VOLUME OVERLOAD
865
Figure 7. Representative confocal microscopic images from the cell group (A) and from the control group (B) for the presentation capillary density with CD31 staining of the myocardial regions around the transannular patch where the UCMNC (cell group) and medium (control group) injections were instituted [630 magnification, CD31 antibody (green) for endothelial cells, nuclear counterstaining with TO-PRO-3 iodide (Invitrogen, Carlsbad, CA, USA) (blue)].
nary regurgitation with late RV dysfunction mainly determines long-term morbidity and mortality of patients despite advanced surgical techniques (4). Patients are candidates for surgical reintervention due to worsening RV function with a decline in clinical performance, but also malignant ventricular arrhythmias, especially in
those patients with more severe pulmonary regurgitation, may contribute to higher morbidity and mortality in these patients (47). The employment of stem cell therapies in the complementary treatment of congenital heart defects bears major potential for regenerative medicine in addition to surgical therapies (43). UCB is rich in stem/progenitor cells with enhanced potency for angiogenic and myogenic differentiation and superior proliferative characteristics (19,33,36). These cells have already been therapeutic agents in patients suffering from major hematological disorders (45). UCMNCs have also been used experimentally in several different settings for myocardial regeneration. These cells were administered systemically or locally in settings for the treatment of myocardial infarction with improvement in cardiac function, reduction of infarction size and elevation of capillary density (20, 21,30). Recently, immunoselected human UCB CD133+ cells have been reported to possess endothelial and cardiomyogenic properties expressing VE-cadherin, CD146, or muscle proteins such as troponin I and myosin ventricular heavy chains in vitro (8). Very early efforts aiming at an experimental enlargement of the pulmonary or aortic orifices were reported in 1914 by Carrel et al. (12). Our model constitutes a novel experimental model of pulmonary orifice enlargement and pulmonary valve distortion without using extracorporal circulationa first in the literature. To the best of our knowledge, the present study is one of the very first investigations in the field combining myocardial regenerative therapy with autologous UCMNCs, the RV and congenital cardiac surgery in a large animal model. UCMNCs were successfully isolated and transplanted into RV myocardium around the transannular patch and the site of infundibulotomy. Confirming previous studies using human umbilical cord blood, about 1% of the total sheep UCMNCs expressed CD34, which is known to be a marker for hematopoietic stem cells, satellite cells, and endothelial progenitor cells. The content of endothelial progenitor cells in UCMNCs was also supported by the cultures grown in vitro. By applying special endothelial media to the final cell product we were able to show a considerable growth of AcLDL+ endothelial cells that originated from UCMNCs. Early conductance catheter analysis revealed altered ventricular volume parameters and acute stress with an enhancement of systolic properties due to acute pulmonary regurgitation, which corroborates with other reports in the setting of acute volume overload (27,37). Echocardiography after 6 weeks indeed confirmed the success of our experimental strategy by showing pulmonary insufficiency between grades II and III in all operated animals. The visualization and adequate functional quantification of the RV via transthoracic echocardiog-
866
YEREBAKAN ET AL.
raphy is known to be challenging. Therefore, the volumetric parameters gained from the echocardiographic evaluation should receive cautious acceptance. At the end of the 3-month follow-up we were already able to observe an alteration of the RV function, which is one of the main long-term determinants of morbidity and mortality after TOF correction. Even when the derangement for CO and SV seemed more prominent in the control group than in the cell group baseline cardiac function did not differ significantly between the groups. Under dobutamine stress conditions, however, hemodynamic assessment of the cell group uncovered a better systolic function of the RV with significantly enhanced values for dP/dtmax compared to the controls. Szabo et al. conducted an experimental chronic RV volume overload study by creating a femorofemoral arteriovenous shunt in dogs for 3 months (44). The authors observed that the chronic volume overload had no effect on RV contractility whereas the inotropic response to an increased afterload was limited. However, the setting of our experimental approach closely mimics the clinical scenario in that the transannular patch implantation with infundibulectomy was the reason for the volume overloading in the RV. Regional contractile deterioration following the incision in the RVOT may have partly influenced the global systolic performance that was partly preserved in the animals of the cell group. Additionally, the reason for the alteration in systolic function may be dependent on cellular changes in calcium homeostasis and contractile proteins due to chronic volume stress (3). Because systolic function was not preserved by the increase of preload (heterometric autoregulation), the remaining mechanism for better systolic function in the cell group may involve the increase of contractile performance (homeometric autoregulation), which may have been positively influenced by the stem cells. On the other hand, the latter has been reported to be completely absent in chronically volume-overloaded hearts without additional treatment such as stem cells (10). It is known that diastolic dysfunction occurs in stressed human hearts (10,39). The difference in diastolic properties between the groups under dobutamine stress conditions was more exaggerated. Because the slope and position of EDPVR represent relatively independent parameters for the comparison of elasticity of the RV, the rightward downward shift of EDPVR slope and reduced intracavitary pressure load under pharmacologically induced stress mirrored the enhanced elasticity of the RV that received UCMNC treatment. Further, dP/ dtmin under dobutamine stress conditions represented preserved diastolic function in the cell group compared to the controls. The restoration of RV volume and pressure loadings under baseline conditions at 3 months in comparison to the immediate postoperative period in both groups is, however, an interesting feature in our hemo-
dynamic analysis. The evidence for a lasting pulmonary insufficiency of grade IIIII in the echocardiography at 6 weeks and our postmortem macroscopic investigations showing clear signs of pulmonary annular distortion in all animals contradicts the idea of the resolution of the pulmonary incompetence. A possible explanation would be early remodeling or structural adaptation of the RV resisting against spatial dilatation (13). We observed significantly enhanced capillary formation in the cell group, which yielded the possible explanation of better diastolic function achieved by cell transplantation. The detection of endothelial cells in the cultivation of UCMNCs supports the potential role of these cells in the elevation of angiogenesis. This finding indicates potential importance for RV remodeling after infundibulotomy and is in concert with other reports in the literature (21,30). In our study the area of fibrosis did not show any significant difference between the groups. The average area of fibrosis around the TAP was about 2.7% in both groups, which is a low value when compared to the ratio of myocardial fibrosis in settings for myocardial infarction but slightly over the normal ratio of fibrotic tissue in healthy myocardium (1). The route for delivery of UCMNCs seems to be safe and effective at the time of surgery whereas intracoronary delivery has been reported to be unsuitable for the treatment of myocardial infarction in a swine model (31) similarly to intravenous delivery of mesenchymal stem cells in canine model by Freyman and collegues (17). Moreover, the thin myocardium of the RV free wall must be considered prone to perforation. Therefore, we used a special hand-made double stage needle with an epicardial stopper to prevent this eventual complication during the intramyocardial application of UCMNCs. In an experimental study by Borenstein et al. myogenic cell were implanted into the RV myocardium in a setting of pulmonary artery banding and two animals were lost as a result of the several injections that presumably lead to RV edema and failure (9). We did not observe that kind of complication. Not only the number of injections and the amount of injected volume, but also the appropriate instruments used for injection should be carefully determined. Undoubtedly, there are limitations to our study. Firstly, the conductance catheter method for assessment of the RV function has also been questioned in the literature. Nevertheless, it is generally accepted as one of the most accurate methods for differentiated functional analysis (15,22,28,41). Alternatively, magnetic resonance imaging would have provided a detailed assessment of RV function whereas the requirement of sedation and breathholds for qualitative imaging would have exposed animals with RV compromise to a higher risk during the investigation and eventually impaired our outcome by causing a higher rate of mortality. Secondly, the effects
UCMNC TREATMENT IN CHRONIC RV VOLUME OVERLOAD
867
of the implanted cells may originate from neovessel formation in the transplanted heart, although the definitive evidence is missing if the transplanted autologous cells remained in the myocardium after 3 months, even though there is no concern for immunorejection in our autologous setting of UCMNC transplantation. Nevertheless, cell tracking was not applied in our study. Whether the enhanced angiogenesis is a direct effect of the cell implantation or is derived partly by circulating or resident cardiac stem cells remains to be elucidated. In conclusion, the results of our study have proven a novel and unique experimental model mimicking postsurgical scenario of TOF patients in large animals. Autologous, intramyocardial UCMNC transplantation has been found feasible and safe and seems to positively influence the diastolic properties of the RV under chronic volume overload probably through enhanced angiogenesis. However, the strategy of cardiac regeneration with UCMNCs in TOF still requires further detailed investigation before possible introduction into a clinical setting.
ACKNOWLEDGMENTS: We are grateful to Prof. Matthias Peuster from the Department of Pediatric Cardiology of the University of Rostock for his helpful discussion. We thank Ms. Margit Fritsche and Mr. Reinhard Schwarmer for their excel lent technical assistance.
9.
10.
11. 12. 13.
14.
15.
REFEENCES
1. Agata, J.; Chao, L.; Chao, J. Kallikrein gene delivery improves cardiac reserve and attenuates remodeling after myocardial infarction. Hypertension 40:653659; 2002. 2. Alexiou, C.; Mahmoud, H.; Al-Khaddour, A.; Gnanapragasam, J.; Salmon, A. P.; Keeton, B. R.; Monro, J. L. Outcome after repair of tetralogy of Fallot in the first year of life. Ann. Thorac. Surg. 71:494500; 2001. 3. Alvarez, B. V.; Perez, N. G.; Ennis, I. L.; Camilion de Hurtado, M. C.; Cingolani, H. E. Mechanisms underlying the increase in force and Ca(2+) transient that follow stretch of cardiac muscle: A possible explanation of the Anrep effect. Circ. Res. 85:716722; 1999. 4. Ammash, N. M.; Dearani, J. A.; Burkhart, H. M.; Connolly, H. M. Pulmonary regurgitation after tetralogy of Fallot repair: Clinical features, sequelae, and timing of pulmonary valve replacement. Congenit. Heart Dis. 2:386403; 2007. 5. Anversa, P.; Kajstura, J. Ventricular myocytes are not terminally differentiated in the adult mammalian heart. Circ. Res. 83:114; 1998. 6. Assmus, B.; Honold, J.; Schachinger, V.; Britten, M. B.; Fischer-Rasokat, U.; Lehmann, R.; Teupe, C.; Pistorius, K.; Martin, H.; Abolmaali, N. D.; Tonn, T.; Dimmeler, S.; Zeiher, A. M. Transcoronary transplantation of progenitor cells after myocardial infarction. N. Engl. J. Med. 355: 12221232; 2006. 7. Beltrami, A. P.; Barlucchi, L.; Torella, D.; Baker, M.; Limana, F.; Chimenti, S.; Kasahara, H.; Rota, M.; Musso, E.; Urbanek, K.; Leri, A.; Kajstura, J.; Nadal-Ginard, B.; Anversa, P. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell 114:763776; 2003. 8. Bonanno, G.; Mariotti, A.; Procoli, A.; Corallo, M.; Rutella, S.; Pessina, G.; Scambia, G.; Mancuso, S.; Pier16.
17.
18. 19. 20.
21.
22.
23.
elli, L. Human cord blood CD133+ cells immunoselected by a clinical-grade apparatus differentiate in vitro into endothelial- and cardiomyocyte-like cells. Transfusion 47: 280289; 2007. Borenstein, N.; Jian, Z.; Fromont, G.; Bruneval, P.; Hekmati, M.; Behr, L.; Laborde, F.; Montarras, D.; Le Bret, E. Noncultured cell transplantation in an ovine model of right ventricular preparation. J. Thorac. Cardiovasc. Surg. 129: 11191127; 2005. Brixius, K.; Reuter, H.; Bloch, W.; Schwinger, R. H. Altered hetero- and homeometric autoregulation in the terminally failing human heart. Eur. J. Heart Fail. 7:2935; 2005. Burkhoff, D.; Sugiura, S.; Yue, D. T.; Sagawa, K. Contractility-dependent curvilinearity of end-systolic pressurevolume relations. Am. J. Physiol. 252:12181227; 1987. Carrel, A. Experimental operations on the orifices of the heart. Ann. Surg. 60:16; 1914. Chaturvedi, R. R.; Shore, D. F.; Lincoln, C.; Mumby, S.; Kemp, M.; Brierly, J.; Petros, A.; Gutteridge, J. M.; Hooper, F; Redington, A. N. Acute right ventricular restrictive physiology after repair of tetralogy of Fallot: Association with myocardial injury and oxidative stress. Circulation 100:15401547; 1999. de Vroomen, M.; Cardozo, R. H.; Steendijk, P.; van Bel, F.; Baan, J. Improved contractile performance of right ventricle in response to increased RV afterload in newborn lamb. Am. J. Physiol. Heart Circ. Physiol. 278:100 105; 2000. Dickstein, M. L.; Yano, O.; Spotnitz, H. M.; Burkhoff, D. Assessment of right ventricular contractile state with the conductance catheter technique in the pig. Cardiovasc. Res. 29:820826; 1995 dUdekem dAcoz, Y.; Pasquet, A.; Lebreux, L.; Ovaert, C.; Mascart, F.; Robert, A.; Rubay, J. E. Does right ventricular outflow tract damage play a role in the genesis of late right ventricular dilatation after tetralogy of Fallot repair? Ann. Thorac. Surg. 76:555561; 2003. Freyman, T.; Polin, G.; Osman, H.; Crary, J.; Lu, M.; Cheng, L.; Palasis, M.; Wilensky, R. L. A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. Eur. Heart J. 27:11141122; 2006. Gregg, D.; Foster, E. Pulmonary insufficiency is the nexus of late complications in tetralogy of Fallot. Curr. Cardiol. Rep. 9:315322; 2007. Harris, D. T.; Rogers, I. Umbilical cord blood: A unique source of pluripotent stem cells for regenerative medicine. Curr. Stem Cell Res. Ther. 2:301309; 2007. Henning, R. J.; Abu-Ali, H.; Balis, J. U.; Morgan, M. B.; Willing, A. E.; Sanberg, P. R. Human umbilical cord blood mononuclear cells for the treatment of acute myocardial infarction. Cell Transplant. 13:729739; 2004. Hirata, Y.; Sata, M.; Motomura, N.; Takanashi, M.; Suematsu, Y.; Ono, M.; Takamoto, S. Human umbilical cord blood cells improve cardiac function after myocardial infarction. Biochem. Biophys. Res. Commun. 327:609 614; 2005. Hon, J. K.; Steendijk, P.; Petrou, M.; Wong, K.; Yacoub, M. H. Influence of clenbuterol treatment during six weeks of chronic right ventricular pressure overload as studied with pressure-volume analysis. J. Thorac. Cardiovasc. Surg. 122:767774; 2001. Hu, C. H.; Wu, G. F.; Wang, X. Q.; Yang, Y. H.; Du, Z. M.; He, X. H.; Xiang, P. Transplanted human umbilical cord blood mononuclear cells improve left ventricular
868
YEREBAKAN ET AL.
24. 25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
function through angiogenesis in myocardial infarction. Chin. Med. J. 119:14991506; 2006 Jager, M.; Bachmann, R.; Scharfstadt, A.; Krauspe, R. Ovine cord blood accommodates multipotent mesenchymal progenitor cells. In Vivo 20:205214; 2006. Kim, B. O.; Tian, H.; Prasongsukarn, K.; Wu, J.; Angoulvant, D.; Wnendt, S.; Muhs, A.; Spitkovsky, D.; Li, R. K. Cell transplantation improves ventricular function after a myocardial infarction: A preclinical study of human unrestricted somatic stem cells in a porcine model. Circulation 112:I96104; 2005. Kogler, G.; Sensken, S.; Airey, J. A.; Trapp, T.; Muschen, M.; Feldhahn, N.; Liedtke, S.; Sorg, R. V.; Fischer, J.; Rosenbaum, C.; Greschat, S.; Knipper, A.; Bender, J.; Degistirici, O.; Gao, J.; Caplan, A. I.; Colletti, E. J.; Almeida-Porada, G.; Muller, H. W.; Zanjani, E.; Wernet, P. A new human somatic stem cell from placental cord blood with intrinsic pluripotent differentiation potential. J. Exp. Med. 200:123135; 2004. Lange, P. E.; Onnasch, D. G.; Bernhard, A.; Heintzen, P. H. Left and right ventricular adaptation to right ventricular overload before and after surgical repair of tetralogy of Fallot. Am. J. Cardiol. 50:786794; 1982 Leeuwenburgh, B. P.; Helbing, W. A.; Steendijk, P.; Schoof, P. H.; Baan, J. Biventricular systolic function in young lambs subject to chronic systemic right ventricular pressure overload. Am. J. Physiol. Heart Circ. Physiol. 281:H26972704; 2001. Lewis, I. D.; Verfaillie, C. M. Multi-lineage expansion potential of primitive hematopoietic progenitors: Superiority of umbilical cord blood compared to mobilized peripheral blood. Exp. Hematol. 28:10871095; 2000. Ma, N.; Stamm, C.; Kaminski, A.; Li, W.; Kleine, H. D.; Muller-Hilke, B.; Zhang, L.; Ladilov, Y.; Egger, D.; Stein hoff, G. Human cord blood cells induce angiogenesis following myocardial infarction in NOD/scid-mice. Cardiovasc. Res. 66:4554; 2005. Moelker, A. D.; Baks, T.; Wever, K. M.; Spitskovsky, D.; Wielopolski, P. A.; van Beusekom, H. M.; van Geuns, R. J.; Wnendt, S.; Duncker, D. J.; van der Giessen, W. J. Intracoronary delivery of umbilical cord blood derived unrestricted somatic stem cells is not suitable to improve LV function after myocardial infarction in swine. J. Mol. Cell. Cardiol. 42:735745; 2007. Nieda, M.; Nicol, A.; Denning-Kendall, P.; Sweetenham, J.; Bradley, B.; Hows, J. Endothelial cell precursors are normal components of human umbilical cord blood. Br. J. Haematol. 98:775777; 1997. Nishiyama, N.; Miyoshi, S.; Hida, N.; Uyama, T.; Okamoto, K.; Ikegami, Y.; Miyado, K.; Segawa, K.; Terai, M.; Sakamoto, M.; Ogawa, S.; Umezawa, A. The significant cardiomyogenic potential of human umbilical cord blood-derived mesenchymal stem cells in vitro. Stem Cells 25:20172024; 2007. Orlic, D.; Kajstura, J.; Chimenti, S.; Jakoniuk, I.; Anderson, S. M.; Li, B.; Pickel, J.; McKay, R.; Nadal-Ginard, B.; Bodine, D. M.; Leri, A.; Anversa, P. Bone marrow cells regenerate infarcted myocardium. Nature 410:701 705; 2001. Perin, E. C.; Dohmann, H. F.; Borojevic, R.; Silva, S. A.;
36.
37.
38.
39. 40. 41.
42.
43. 44.
45. 46.
47.
Sousa, A. L.; Mesquita, C. T.; Rossi, M. I.; Carvalho, A. C.; Dutra, H. S.; Dohmann, H. J.; Silva, G. V.; Belem, L.; Vivacqua, R.; Rangel, F. O.; Esparcatte, R.; Geng, Y. J.; Vaughn, W. K.; Assad, J. A.; Mesquita, E. T.; Willerson, J. T. Transendocardial, autologous bone marrow cell transplantation for severe, chronic ischemic heart failure. Circulation 107:22942302; 2003. Prat-Vidal, C.; Roura, S.; Farre, J.; Galvez, C.; Llach, A.; Molina, C. E.; Hove-Madsen, L.; Garcia, J.; Cinca, J.; Bayes-Genis, A. Umbilical cord blood-derived stem cells spontaneously express cardiomyogenic traits. Transplant. Proc. 39:24342437; 2007. Shah, A. S.; Atkins, B. Z.; Hata, J. A.; Tai, O.; Kypson, A. P.; Lilly, R. E.; Koch, W. J.; Glower, D. D. Early effects of right ventricular volume overload on ventricular performance and beta-adrenergic signaling. J. Thorac. Cardiovasc. Surg. 120:342349; 2000. Shpall, E. J.; Quinones, R.; Giller, R.; Zeng, C.; Baron, A. E.; Jones, R. B.; Bearman, S. I.; Nieto, Y.; Freed, B.; Madinger, N.; Hogan, C. J.; Slat-Vasquez, V.; Russell, P.; Blunk, B.; Schissel, D.; Hild, E.; Malcolm, J.; Ward, W.; McNiece, I. K. Transplantation of ex vivo expanded cord blood. Biol. Blood Marrow Transplant. 8:368376; 2002. Sibbald, W. J.; Driedger, A. A. Right ventricular function in acute disease states: Pathophysiologic considerations. Crit. Care Med. 11:339345; 1983. Song, S.; Sanchez-Ramos, J. Preparation of neural progenitors from bone marrow and umbilical cord blood. Methods Mol. Biol. 438:123134; 2008. Stamato, T. M.; Szwarc, R. S.; Benson, L. N. Measurement of right ventricular volume by conductance catheter in closed-chest pigs. Am. J. Physiol. 269:H869876; 1995. Stamm, C.; Westphal, B.; Kleine, H. D.; Petzsch, M.; Kittner, C.; Schumichen, C.; Nienaber, C. A.; Freund, M.; Steinhoff, G. Autologous bone marrow stem cell transplantation for myocardial regeneration after myocardial infarction. Lancet 361:4546; 2003. Steinhoff, G. The regenerating hearthope for children with congenital heart defects. Kinderkrankenschwester 25: 4750; 2006. Szabo, G.; Soos, P.; Bahrle, S.; Radovits, T.; Weigang, E.; Kekesi, V.; Merkely, B.; Hagl, S. Adaptation of the right ventricle to an increased afterload in the chronically volume overloaded heart. Ann. Thorac. Surg. 82:989995; 2006. Tse, W. W.; Zang, S. L.; Bunting, K. D.; Laughlin, M. J. Umbilical cord blood transplantation in adult myeloid leukemia. Bone Marrow Transplant. 41:465472; 2008. Wairiuko, G. M.; Crisostomo, P. R.; Wang, M.; Morrell, E. D.; Meldrum, K. K.; Lillemoe, K. D.; Meldrum, D. R. Stem cells improve right ventricular functional recovery after acute pressure overload and ischemia reperfusion injury. J. Surg. Res. 141:241246; 2007. Zahka, K. G.; Horneffer, P. J.; Rowe, S. A.; Neill, C. A.; Manolio, T. A.; Kidd, L.; Gardner, T. J. Long-term valvular function after total repair of tetralogy of Fallot. Relation to ventricular arrhythmias. Circulation 78:III1419; 1988.
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Kidney HistogenesisDokumen9 halamanKidney HistogenesisKshitija KasturiBelum ada peringkat
- Grade 8 - 4thquarter - BiotechDokumen11 halamanGrade 8 - 4thquarter - BiotechChrista dana ReyesBelum ada peringkat
- Management of Deep Carious LesionsDokumen5 halamanManagement of Deep Carious LesionsEmeka V. ObiBelum ada peringkat
- Hester-Biosciences Karvy 010915 PDFDokumen17 halamanHester-Biosciences Karvy 010915 PDFmannimanojBelum ada peringkat
- Anticoagulant Activity of Paragis Pudadera Et. AlDokumen35 halamanAnticoagulant Activity of Paragis Pudadera Et. Alvanessa piraanBelum ada peringkat
- Challis, Debbie The Archaeology of Race The Eugenic Ideas of FrancisDokumen217 halamanChallis, Debbie The Archaeology of Race The Eugenic Ideas of FrancisSonicoBelum ada peringkat
- IMN1207 McGillActiveProtocolsDokumen11 halamanIMN1207 McGillActiveProtocolsapi-3714923Belum ada peringkat
- DNA - The Double Helix: Chromosomes Are Composed of Genes. A Gene Is A Segment of DNA ThatDokumen4 halamanDNA - The Double Helix: Chromosomes Are Composed of Genes. A Gene Is A Segment of DNA Thatapi-310760045Belum ada peringkat
- Hemostasis, Surgical Bleeding and TransfusionDokumen10 halamanHemostasis, Surgical Bleeding and TransfusionCarl Earvin L. FavoritoBelum ada peringkat
- BISC202 PracticeEXM 1Dokumen7 halamanBISC202 PracticeEXM 1Layomi Dele-DareBelum ada peringkat
- Diagnostic Criteria For The Behavioral Variant FTDDokumen5 halamanDiagnostic Criteria For The Behavioral Variant FTDMusleh AlgarniBelum ada peringkat
- RT-5 Unit 2 QPDokumen7 halamanRT-5 Unit 2 QPbiotecnika_testBelum ada peringkat
- Cystic Fibrosis Foundation: Richmond's Finest 2017Dokumen4 halamanCystic Fibrosis Foundation: Richmond's Finest 2017Richmond MagazineBelum ada peringkat
- Male Reproductive Physiology - UpToDate - 2020Dokumen18 halamanMale Reproductive Physiology - UpToDate - 2020Karaca AzizBelum ada peringkat
- Sample Pages of MBBS Decode (MGR University)Dokumen20 halamanSample Pages of MBBS Decode (MGR University)vkBelum ada peringkat
- Comparative Circulatory SystemDokumen15 halamanComparative Circulatory SystemSmartcool SoBelum ada peringkat
- Adaptive Immunity: Shimelis Teshome (BSC MLS)Dokumen31 halamanAdaptive Immunity: Shimelis Teshome (BSC MLS)Shimelis Teshome AyalnehBelum ada peringkat
- Gene TherapyDokumen29 halamanGene TherapypriyankaBelum ada peringkat
- Clinical Practice Guideline For Management For Rehabilitation of Lower Limb AmputationDokumen55 halamanClinical Practice Guideline For Management For Rehabilitation of Lower Limb Amputationburtyx100% (1)
- Antigen Presenting CellDokumen26 halamanAntigen Presenting CellSurja DasBelum ada peringkat
- Biology of Domestic Animals PDFDokumen371 halamanBiology of Domestic Animals PDFfeketerigo67% (3)
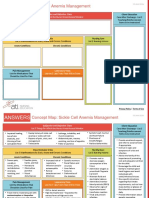
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDokumen2 halamanNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- CMV Quant PCRDokumen82 halamanCMV Quant PCRyousrazeidan1979Belum ada peringkat
- Chapter 18. Mood StabilizersDokumen12 halamanChapter 18. Mood StabilizersAlfen PranataBelum ada peringkat
- The Bull's Eye - May 2011Dokumen13 halamanThe Bull's Eye - May 2011dbhsbullseyeBelum ada peringkat
- Cambridge IGCSE: Biology 0610/22Dokumen16 halamanCambridge IGCSE: Biology 0610/22Aisha YousifBelum ada peringkat
- Antibacterials 2018 PDFDokumen203 halamanAntibacterials 2018 PDFfdfdfdfBelum ada peringkat
- Endocrine System Notes - NCERT BasedDokumen8 halamanEndocrine System Notes - NCERT Basedpallab mukherjeeBelum ada peringkat
- Teratology: Handbook ofDokumen478 halamanTeratology: Handbook ofmaria5basBelum ada peringkat
- Pediatrics in Review 2012 McCavit 195 206Dokumen14 halamanPediatrics in Review 2012 McCavit 195 206cindyBelum ada peringkat