Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy
Diunggah oleh
Louise BravoDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy
Diunggah oleh
Louise BravoHak Cipta:
Format Tersedia
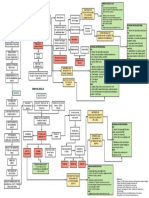
Total abdominal hysterectomy bilateral salpingo oophorectomy (TAHBSO) is the removal of entire uterus, the ovaries, fallopian tubes
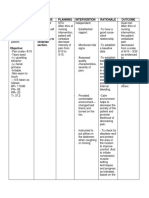
and the cervix. TAHBSO is usually performed in the case of uterine and cervical cancer. This is the most common kind of hysterectomy. Removal of the ovaries eliminates the main source of the hormone estrogen, so menopause occurs immediately. Post-operative nursing care for patients who underwent TAHBSO would include: 1. Determines patient s immediate response to surgical intervention. 2. Monitor patient s physiologic status. 3. Assess patient s pain level and administers appropriate pain relief measures. 4. Maintains patient s safety(airway, circulation, prevention of injury) 5. Administer medication, fluid and blood component therapy, if prescribed. 6. Assess patient s readiness for transfer to in hospital unit or for discharge home based on institutional policy. This post includes several nursing care plans for post-TAHBSO patients. 1. Acute Pain 2. Hypothermia 3. Hyperthermia 4. Anxiety 5. Fatigue 6. Sexual Dysfunction 7. Risk for Infection 8. Risk for Deficient Fluid Volume
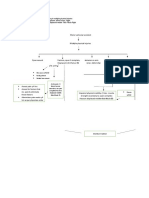
Exploratory laparotomy, total abdominal hysterectomy, bilateral salpingooophorectomy, right and left pelvic lymphadenectomy, common iliac lymphadenectomy, and endometrial cancer staging procedure.
PREOPERATIVE DIAGNOSIS: Endometrial cancer. POSTOPERATIVE DIAGNOSIS: Same.
OPERATION PERFORMED: Exploratory laparotomy, total abdominal hysterectomy, bilateral salpingo-oophorectomy, right and left pelvic lymphadenectomy, common iliac lymphadenectomy, and endometrial cancer
staging procedure. ANESTHESIA: General, endotracheal tube. SPECIMENS: Pelvic washings for cytology, uterus with attached tubes and ovaries, right and left pelvic lymph nodes, para-aortic nodes. INDICATIONS FOR PROCEDURE: The patient recently presented with postmenopausal bleeding and was found to have a Grade II endometrial carcinoma on biopsy. She was counseled to undergo staging laparotomy. FINDINGS: Examination under anesthesia revealed a small uterus with no nodularity. During the laparotomy, the uterus was small, mobile, and did not show any evidence of extrauterine spread of disease. Other abdominal viscera, including the diaphragm, liver, spleen, omentum, small and large bowel, and peritoneal surfaces, were palpably normal. There was no evidence of residual neoplasm after removal of the uterus. The uterus itself showed no serosal abnormalities and the tubes and ovaries were unremarkable in appearance. PROCEDURE: The patient was brought to the Operating Room with an IV in place. Anesthesia was induced, after which she was examined, prepped and draped. A vertical midline incision was made and fascia was divided. The peritoneum was entered without difficulty and washings were obtained. The abdomen was explored with findings as noted. A Bookwalter retractor was placed and bowel was packed. Clamps were placed on the broad ligament for traction. The retroperitoneal spaces were opened by incising lateral and parallel to the infundibulopelvic ligament. The round ligaments were isolated, divided, and ligated. The peritoneum overlying the vesicouterine fold was incised to mobilize the bladder. Retroperitoneal spaces were then opened, allowing exposure of pelvic vessels and ureters. The infundibulopelvic ligaments were isolated, divided, and doubly ligated. The uterine artery pedicles were skeletonized, clamped, divided, and suture ligated. Additional pedicles were developed on each side of the cervix, after which tissue was divided and suture ligated. When the base of the cervix was reached, the vagina was cross-clamped and divided, allowing removal of the uterus with attached tubes and ovaries. Angle stitches of o-Vicryl were placed, incorporating the uterosacral ligaments and the vaginal vault was closed with interrupted figureof-eight stitches. The pelvis was irrigated and excellent hemostasis was noted. Retractors were repositioned to allow exposure for lymphadenectomy. Metzenbaum scissors were used to incise lymphatic tissues. Borders of the pelvic node dissection
included the common iliac bifurcation superiorly, the psoas muscle laterally, the cross-over of the deep circumflex iliac vein over the external iliac artery inferiorly, and the anterior division of the hypogastric artery medially. The posterior border of dissection was the obturator nerve, which was carefully identified and preserved bilaterally. Ligaclips were applied where necessary. After the lymphadenectomy was performed bilaterally, excellent hemostasis was noted. Retractors were again repositioned to allow exposure of para-aortic nodes. Lymph node tissue was mobilized, Ligaclips were applied, and the tissue was excised. The pelvis was again irrigated and excellent hemostasis was noted. The bowel was run and no evidence of disease was seen. All packs and retractors were removed and the abdominal wall was closed using a running Smead-Jones closure with #1 permanent monofilament suture. Subcutaneous tissues were irrigated and a Jackson-Pratt drain was placed. Scarpa's fascia was closed with a running stitch and skin was closed with a running subcuticular stitch. The final sponge, needle and instrument counts were correct at the completion of the procedure. The patient was then awakened from her anesthetic and taken to the Post Anesthesia Care Unit in stable condition.
FROM http://www.mtsamples.com/site/pages/sample.asp?type=45Obstetrics%20/%20Gynecology&sample=956-Hysterectomy%20(TAH%20-%20BSO)
Anda mungkin juga menyukai
- Total Abdominal Hysterectomy Bilateral Salpingo OophorectomyDokumen3 halamanTotal Abdominal Hysterectomy Bilateral Salpingo OophorectomyMitch Elle Infante100% (1)
- PRELIMS 219 Q - uPDATEDDokumen8 halamanPRELIMS 219 Q - uPDATEDAloha ItsmeBelum ada peringkat
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDokumen2 halamanTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestBelum ada peringkat
- NCP Episiotomy WoundDokumen3 halamanNCP Episiotomy WoundJP2001Belum ada peringkat
- Nursing Resource Unit Postpartum CareDokumen4 halamanNursing Resource Unit Postpartum Caredee_day_8Belum ada peringkat
- Family Nursing Care Plan: Group A3 - ObDokumen4 halamanFamily Nursing Care Plan: Group A3 - ObErika CadawanBelum ada peringkat
- Benign Prostatic HyperplasiaDokumen6 halamanBenign Prostatic HyperplasiaJE MagbanuaBelum ada peringkat
- NCP and Drug Study For Ob WardDokumen7 halamanNCP and Drug Study For Ob WardAce Fabrigas100% (1)
- LRDR ProceduresDokumen67 halamanLRDR ProceduresJustJ ThingsBelum ada peringkat
- Case Study Final PortraitDokumen11 halamanCase Study Final PortraitZhy CaluzaBelum ada peringkat
- Dela Rosa 2A MCN-Module 05Dokumen2 halamanDela Rosa 2A MCN-Module 05Atsu MiyaBelum ada peringkat
- Daily MNGT Plan3Dokumen4 halamanDaily MNGT Plan3Christian Apple Angwas GonzalesBelum ada peringkat
- Nursing Care Plan ColostomyDokumen5 halamanNursing Care Plan ColostomyCarissa Mae Tapec EstradaBelum ada peringkat
- DP Discharge Plan@@@@@@@@Dokumen6 halamanDP Discharge Plan@@@@@@@@Maemae SumalinogBelum ada peringkat
- NCP HemothoraxDokumen3 halamanNCP HemothoraxMichael John F. NatividadBelum ada peringkat
- Nursing Drug StudyDokumen12 halamanNursing Drug StudyJoshkorro Geronimo100% (2)
- MSN CASE STUDY FORMATnew-1Dokumen26 halamanMSN CASE STUDY FORMATnew-1Dinesh BanerjeeBelum ada peringkat
- Pathophysiology AbrasionDokumen3 halamanPathophysiology AbrasionVito VitoBelum ada peringkat
- Activity IntoleranceDokumen1 halamanActivity IntoleranceAndrea Francesca SantosBelum ada peringkat
- NCPDokumen1 halamanNCPEduard C. TaganapBelum ada peringkat
- Altretamine: Drug DosageDokumen16 halamanAltretamine: Drug DosagePrincess CruzBelum ada peringkat
- NCP 1Dokumen6 halamanNCP 1Maedine Urbano-BrionesBelum ada peringkat
- CHNDokumen11 halamanCHNAngelina Janiya NicoleBelum ada peringkat
- Discharge PlanDokumen9 halamanDischarge PlanRheynel NietesBelum ada peringkat
- Common Fears Related To Childbirth and Coping Mechanisms Among Primigravida MothersDokumen42 halamanCommon Fears Related To Childbirth and Coping Mechanisms Among Primigravida MothersSmile Tambanillo100% (1)
- NCP 3Dokumen4 halamanNCP 3bananakyuBelum ada peringkat
- NCP NephrolithiasisDokumen3 halamanNCP NephrolithiasisMANUEL EMERSONBelum ada peringkat
- Case Study: HemorrhoidectomyDokumen19 halamanCase Study: HemorrhoidectomyJoyJoy Tabada CalunsagBelum ada peringkat
- Case (Acute Gastroenteritis) Group 4Dokumen36 halamanCase (Acute Gastroenteritis) Group 4EljhayrosBelum ada peringkat
- MetherginDokumen2 halamanMetherginOtan Cuison100% (1)
- Nursing Care Plan Problem: Difficulty of BreathingDokumen5 halamanNursing Care Plan Problem: Difficulty of BreathingIvan Louise Fajardo ManiquizBelum ada peringkat
- Disaster Management and Nurses RoleDokumen34 halamanDisaster Management and Nurses RoleMebin NinanBelum ada peringkat
- CASE STUDY Acute Pain Related To Laceration 1Dokumen29 halamanCASE STUDY Acute Pain Related To Laceration 1Maria Jessica Dumdum100% (1)
- Normal Spontaneous DeliveryDokumen11 halamanNormal Spontaneous DeliveryAyah GarciaBelum ada peringkat
- Learning Derived (Lysha)Dokumen1 halamanLearning Derived (Lysha)Choy DavidBelum ada peringkat
- Nursing Care Plan D-CDokumen2 halamanNursing Care Plan D-CGian MonillaBelum ada peringkat
- Reflective Journal 1Dokumen4 halamanReflective Journal 1api-365605511Belum ada peringkat
- 3011-1 - NCP & Drug Study - AMCDokumen5 halaman3011-1 - NCP & Drug Study - AMCAngie MandeoyaBelum ada peringkat
- Request Letter For CHNDokumen1 halamanRequest Letter For CHNdusty kawiBelum ada peringkat
- Nursing Diagnosis For AppendicitisDokumen1 halamanNursing Diagnosis For AppendicitisTweenie DalumpinesBelum ada peringkat
- NCP Example Pre EclampsiaDokumen6 halamanNCP Example Pre EclampsiaChristian Joseph OpianaBelum ada peringkat
- Drug Name Dosa Ge Mechanis Mof Action Indicatio N Contraindic Ation Adverse/Side Effects Nursing InterventionsDokumen14 halamanDrug Name Dosa Ge Mechanis Mof Action Indicatio N Contraindic Ation Adverse/Side Effects Nursing InterventionsVin LandichoBelum ada peringkat
- Rationale: This Will Assess Pain LevelDokumen7 halamanRationale: This Will Assess Pain LevelCoreyBelum ada peringkat
- NCP - Activity Intolerance & Excess Fluid VolumeDokumen2 halamanNCP - Activity Intolerance & Excess Fluid VolumeCindy MariscotesBelum ada peringkat
- NCP2Dokumen2 halamanNCP2Jrose CuerpoBelum ada peringkat
- AB Critical Thinking ExercisesDokumen4 halamanAB Critical Thinking ExercisesAhmad BaolayyanBelum ada peringkat
- Doctors Order LoveDokumen4 halamanDoctors Order LoveAubrey Unique EvangelistaBelum ada peringkat
- Discharge PlanDokumen4 halamanDischarge PlanVillanueva NiñaBelum ada peringkat
- Drug Study ObDokumen6 halamanDrug Study Obednaria100% (1)
- Drug-Study NCPDokumen5 halamanDrug-Study NCPMURILLO, FRANK JOMARI C.Belum ada peringkat
- Nursing Care Plan (Post CS)Dokumen5 halamanNursing Care Plan (Post CS)Tony ReyesBelum ada peringkat
- Retracting and Exposing InstrumentsDokumen3 halamanRetracting and Exposing InstrumentsTherese Manalansan AlvarezBelum ada peringkat
- Gastroschisis & OmphaloceleDokumen1 halamanGastroschisis & OmphaloceleMaecy PasionBelum ada peringkat
- Concept MapDokumen2 halamanConcept Mapjunifer laynoBelum ada peringkat
- Name of The DrugDokumen2 halamanName of The DrugSistine Rose LabajoBelum ada peringkat
- ClubfootDokumen22 halamanClubfootJhong Xyrus100% (3)
- Nifedipine Drug StudyDokumen2 halamanNifedipine Drug StudyMary Shane MoraldeBelum ada peringkat
- Clinical Portrait Pertinent DataDokumen9 halamanClinical Portrait Pertinent DataGermin CesaBelum ada peringkat
- TAHBSODokumen2 halamanTAHBSOarziaBelum ada peringkat
- Total Abdominal Hysterectomy With Bilateral Salpingo Oophorectomy.Dokumen3 halamanTotal Abdominal Hysterectomy With Bilateral Salpingo Oophorectomy.Daywalker PedragozaBelum ada peringkat
- Gynecology Review: Abigail Elsie Dg. Castro, MD, Maed, Fpogs, Fpsuog August 11, 2017Dokumen198 halamanGynecology Review: Abigail Elsie Dg. Castro, MD, Maed, Fpogs, Fpsuog August 11, 2017Jojo Mendoza100% (1)
- On ImmunoGen and Mirvetuximab Soravtansine (IMGN 853), A Subjective Meta-Analysis From A Clinical Trial Based PerspectiveDokumen15 halamanOn ImmunoGen and Mirvetuximab Soravtansine (IMGN 853), A Subjective Meta-Analysis From A Clinical Trial Based PerspectiveDavid Fernandez FerrerBelum ada peringkat
- CancerDokumen81 halamanCancerCodered Review100% (1)
- Evaluation of Ascites and Its Etiology Using Ultrasonography JRD 119 PDFDokumen4 halamanEvaluation of Ascites and Its Etiology Using Ultrasonography JRD 119 PDFEstu Paramadina PratamaBelum ada peringkat
- ARID1A Mutations in Endometriosis-Associated Ovarian: CarcinomasDokumen6 halamanARID1A Mutations in Endometriosis-Associated Ovarian: CarcinomasherryBelum ada peringkat
- 526064MCQDokumen4 halaman526064MCQSREE NITHINBelum ada peringkat
- CLIENTS WITH PROBLEMS IN CELLULAR ABERRATIONS Notes For StudentsDokumen39 halamanCLIENTS WITH PROBLEMS IN CELLULAR ABERRATIONS Notes For StudentsAno NymousBelum ada peringkat
- Cancer - QDokumen7 halamanCancer - QroldanBelum ada peringkat
- (Ebookobgyne - Net) Diagnostic Imaging Gynecology, 2ndDokumen948 halaman(Ebookobgyne - Net) Diagnostic Imaging Gynecology, 2ndJessica Ugalde Mata100% (3)
- Tumor Marker Tests - CancerDokumen4 halamanTumor Marker Tests - CancerMonna Medani LysabellaBelum ada peringkat
- (#5) Benign and Malignant Ovariaan TumorsDokumen35 halaman(#5) Benign and Malignant Ovariaan Tumorsmarina_shawkyBelum ada peringkat
- Uterine Fibroids: Review ArticleDokumen12 halamanUterine Fibroids: Review ArticleDusty SandBelum ada peringkat
- Saso, S.Dokumen8 halamanSaso, S.Azka Syifa AnnisaBelum ada peringkat
- Tumor MarkersDokumen10 halamanTumor MarkersGianna SablanBelum ada peringkat
- Chemotherapy For Gynecologic CancerDokumen69 halamanChemotherapy For Gynecologic CancerBEREKET100% (1)
- Fibroid With PregnancyDokumen5 halamanFibroid With PregnancyvaishaliBelum ada peringkat
- Cancer Trials Unit BrochureDokumen57 halamanCancer Trials Unit Brochuredavesmart1025Belum ada peringkat
- ESMO 5 Advanced Breast CancerDokumen27 halamanESMO 5 Advanced Breast CancerAlex DelgadoBelum ada peringkat
- ASE Presentation: DR - Ramesh Sharma Department of Obstetrics and Gynaecology. IOM, TU Teaching HospitalDokumen58 halamanASE Presentation: DR - Ramesh Sharma Department of Obstetrics and Gynaecology. IOM, TU Teaching HospitalNinaBelum ada peringkat
- Recall January 2018-2Dokumen38 halamanRecall January 2018-2Umme Habiba GilaniBelum ada peringkat
- Grade9 STE Con.-Chem. Q4 Module-3 Wk4 ADMDokumen20 halamanGrade9 STE Con.-Chem. Q4 Module-3 Wk4 ADMChelzy Catabas67% (3)
- Dermoid CystDokumen8 halamanDermoid CystMohamed Hazem ElfollBelum ada peringkat
- All India Institute of Medical Sciences Nagpur Department of Obstetrics and GynecologyDokumen19 halamanAll India Institute of Medical Sciences Nagpur Department of Obstetrics and GynecologySugan GavaskarBelum ada peringkat
- Section A Multiple Choice Questions Gynaecology: Prepared by Da Roux Barrett Class of 2014Dokumen13 halamanSection A Multiple Choice Questions Gynaecology: Prepared by Da Roux Barrett Class of 2014Sheldon FerronBelum ada peringkat
- Ong Cases Final-1Dokumen49 halamanOng Cases Final-1Cedric KyekyeBelum ada peringkat
- Soal MCQ USU 2009Dokumen19 halamanSoal MCQ USU 2009SuzetteBelum ada peringkat
- Iq2wjqjhfkkby1lyhkyd5z3iDokumen2 halamanIq2wjqjhfkkby1lyhkyd5z3iSubham RajputBelum ada peringkat
- Early Detection and Cancer PreventionDokumen18 halamanEarly Detection and Cancer PreventionFred YangBelum ada peringkat
- Gynaecological Diseases in PregnancyDokumen76 halamanGynaecological Diseases in PregnancyKarishma Shroff67% (9)
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 4 dari 5 bintang4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDari EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDPenilaian: 5 dari 5 bintang5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Dari EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Penilaian: 5 dari 5 bintang5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDari EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisPenilaian: 4 dari 5 bintang4/5 (1)
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerDari EverandGut: the new and revised Sunday Times bestsellerPenilaian: 4 dari 5 bintang4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDari EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsPenilaian: 4.5 dari 5 bintang4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDari EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryPenilaian: 4 dari 5 bintang4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDari EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDari EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningPenilaian: 4 dari 5 bintang4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Dari EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Penilaian: 4 dari 5 bintang4/5 (378)
- To Explain the World: The Discovery of Modern ScienceDari EverandTo Explain the World: The Discovery of Modern SciencePenilaian: 3.5 dari 5 bintang3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlDari EverandThe Marshmallow Test: Mastering Self-ControlPenilaian: 4.5 dari 5 bintang4.5/5 (58)