Neonates Chest RX
Diunggah oleh
Uri MoraDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Neonates Chest RX
Diunggah oleh
Uri MoraHak Cipta:
Format Tersedia
Current Paediatrics (2003) 13, 460 -- 468
2003 Elsevier Ltd. All rights reserved. c doi:10.1016/S0957-5839(03)00080 - 0
Radiology of the chest in neonates
Susan J. Morris
Consultant Radiologist, University Hospital of Wales, Heath Park, Cardiff, UK
KEYWORDS neonatal chest; radiology
Summary The unique diseases encountered in the neonate, their small size, fragile nature and increased susceptibility to the damaging effects of radiation all combine to make their imaging both challenging and interesting for the radiologist and radiographer. All radiation exposures must be justif|ed. Meticulous attention to detail is a prerequisite to performing a good chest x-ray in young infants, requiring dedicated staff and equipment. Low dose techniques and adequate lead protection must always be employed. A knowledge of the normal radiological anatomy in the neonate are essential for correct interpretation of the f|lms, as well as the appearance and evolution of the disease processes which occur in this age group. Ateam approach with good communication between obstetricians, paediatric surgeons, neonatologists and radiologists is vital as interpretation of the images is dependent on many clinical and technical factors. Different imaging modalities are available each with specif|c uses, risks and limitations, knowledge of which is necessary for their appropriate use. An overview of many of the common abnormalities seen in the chest in the newborn period is described and illustrated.
2003 Elsevier Ltd. All rights reserved. c
PRACTICE POINTS
*
* * * *
Assess technical factors of the f|lm f|rst (name,side markers, exposure, rotation, inspiratory effort, motion artifact) Compare with previous f|lms if available Check position of lines, tubes and drains Systematic approach in looking at f|lm Pertinent clinical history which may be helpful including prenatal history and scan f|ndings Discuss with radiologist the need for further imaging (US, CT, MRI)
ricians, paediatric surgeons, neonatologists and radiologists is vital as interpretation of the images is dependent on many clinical and technical factors. Different imaging modalities are available, and knowledge of their specif|c uses, risks and limitations is necessary for their appropriate use. An overview of many of the common abnormalities seen in the chest in the newborn period is described and illustrated in this paper.
RADIATION RISK
Irradiation of radiosensitive bone marrow, present in most bones at birth, increases the risks of induced leukaemia and genetic effects.1 Unnecessary or repeated exposures, poor technique and lack of lead protection increase the risk, so meticulous care must be taken to minimize radiation while still providing diagnostic images. Alternative modes of imaging that do not use ionizing radiation should be considered wherever possible. Computed tomography (CT) and magnetic resonance imaging (MRI) pose particular diff|culties in the neonate; the latter requiring highly specialized anaesthetists and dedicated equipment. The radiology department is not the ideal environment for sick infants.
INTRODUCTION
The unique diseases encountered in the neonate, their small size, fragile nature and increased susceptibility to the damaging effects of radiation combine to make their imaging both challenging and interesting. A team approach with good communication between obstetCorrespondence to: SJM.Tel.: +44 (0) 2920 74 4887; fax: +44 (0) 2920 74 3069
RADIOLOGYOF THE CHEST IN NEONATES
461
TECHNICAL FACTORS IN PERFORMING A CHEST X-RA Y
The plain chest x-ray is still the most frequently requested radiological examination on the neonatal unit. It requires a core group of staff responsible for performing the examination and ensuring, through audit, that acceptable image quality is maintained. The use of a high-speed f|lm/screen system with a mobile x-ray unit with a powerful high-frequency or constant potential generator is recommended.2 A short exposure time, high KV-low MAS technique is employed and the exposure factors must be recorded on the f|lm. Tight collimation is essential, and lead shielding should be placed on the baby and incubator. Unnecessary lines and tubing should be removed from the chest area, and the infant should be immobilized by holding the arms flexed either side of the head. The mandible must not obscure the upper chest, and the f|eld of view must include the cervical trachea as its upper limit and T12/L1 vertebral bodies as the lower limit. Errors in interpretation may occur due to poor technique. A f|lm taken in expiration may cause the lungs to appear consolidated. Rotated f|lms produce an increased lucency on one side, and line positions appear misplaced. A lordotic f|lm alters the appearance of the heart contour and the apparent position of the endotracheal tube (ETT). The recent increased use of digital imaging and storage systems has many benef|ts on the neonatal unit; previous f|lms are instantly available and the image can be manipulated to optimize viewing even in poorly exposed f|lms, resulting in fewer repeat exposures.
cardiothoracic ratio is not usually helpful although a normal upper limit of approximately 65% can be used. Pulmonary vascular markings taper gradually towards the periphery of the lungs, and air bronchograms are commonly seen in the medial third of the lung bases.3
PROBLEMS IN THE PRE-TERMINFANT
Respiratory distress syndrome
Respiratory distress syndrome is a disease of hypoventilation and a manifestation of pulmonary immaturity and surfactant def|ciency. Surfactant usually coats the alveolae and prevents atalectasis by lowering surface tension. In respiratory distress syndrome, the lungs are poorly compliant with acinar atelectasis, and there is a gradual development of thickening of the interstitium and dilatation of the terminal airways. Radiological abnormalities correlate well with the clinical severity. There is reticulogranular or ground glass opacif|cation, progressive hypo-aeration and air bronchograms (Fig.1). Symptoms and radiological signs progress during the f|rst 6 h of life, and in mild to moderate disease, the granular densities persist for 3--5 days, clearing from peripheral to central and upper to lower lungs. Artif|cial surfactant has contributed to a reduced frequency of pneumothoraces and improved early survival of these infants, although the long-term consequences of bronchopulmonary dysplasia may still occur. Uneven distribution of surfactant can cause patchy areas of increased aeration, radiologically simulating pulmonary interstitial emphysema or meconium aspiration.4
THE NORMAL CHEST
Having f|rst assessed these technical factors, the position of the lines, drains, tubes and catheters should be noted. The ideal location of the ETT tip is 1cm above the carina. The umbilical arterial catheter (UAC) tip should be above the coeliac axis and superior mesenteric arteries, preferably in the lower thoracic aorta.The umbilical venous catheter (UVC) tip should be just above the liver. The normal shape of the chest in the newborn is trapezoid with horizontal ribs.The thymus is prominent but rapidly involutes during the f|rst few days of post-natal life, especially in stressed infants. It is a smooth, usually bilateral quadrilateral shape of soft tissue density. Pulmonary vessels can be seen through it. A notch may be seen at its inferior edge adjacent to the heart, and a saillike projection from the mediastinum and scalloping of the lateral or inferior margins are not uncommon. The assessment of heart size in young infants is diff|cult;
Figure 1 Respiratory distress syndrome.
462
CURRENT PAEDIATRICS
Air block complications of RDS
Decreased lung compliance and high positive pressure ventilation may lead to air leaks from the pulmonary parenchyma, resulting in pneumothorax, pneumomediastinum and even pneumoperitoneum (Fig. 2). If air leaks into the interstitial space and spreads through the lymphatics along the perivascular sheaths, it leads to pulmonary interstitial emphysema. Radiologically, this produces a pattern of small bubbles radiating from the hilum.5 If this becomes extensive, it compresses the airways, reducing gas exchange; if severe, it can even result in cardiac compression. Unlike pneumothorax, pulmonary interstitial emphysema cannot be drained and can result in extensive lung damage.
Bronchopulmonary dysplasia (chronic lung disease of prematurity)
A combination of barotrauma, oxygen toxicity, infection, def|ciency of anti-oxidant defences and altered inflammatory response in the pre-term lung results in bronchopulmonary dysplasia.6 The early radiological appearance is of coarse interstitial densities interspersed with small cystic-like areas. This progresses over weeks to months to generalized hyperinflation with larger cystic areas, atelectasis and f|brosis (Fig. 3). The heart is frequently enlarged due to right ventricular strain and cor pulmonale. Wilson Mikity syndrome produces the same radiological picture but in immature infants who have had minimal ventilatory support.7
Figure 3 Bronchopulmonary dysplasia.
monary haemorrhage. There is a spectrum from a small amount of fresh blood to catastrophic cardiovascular collapse. The chest x-ray f|ndings are non-specif|c, ranging from small areas of opacif|cation to a complete whiteout of one or both lungs.
PROBLEMS IN THE TERM INFANT
Pulmonary haemorrhage
Bleeding from the airway, often associated with sudden deterioration in respiratory function, suggests acute pul-
Neonatal pneumonia and persistent pulmonary hypertension of the newborn
Pneumonia in the newborn occurs in approximately 0.2% of live births.8 It may present early with respiratory distress, and clinical features and chest X-ray f|ndings indistinguishable from respiratory distress syndrome due to associated surfactant def|ciency. A history of prolonged rupture of membranes may be present. The most common organisms are group B b-haemolytic streptococcus or coliforms. The chest x-ray f|ndings are non-specif|c. Lobar collapse and consolidation are unusual in neonatal pneumonia, and are more likely to be due to poor ETT positioning. Persistent pulmonary hypertension of the newborn can occur as a consequence of pneumonia, hypoxia, birth asphyxia and sepsis, and is associated with pulmonary hypoplasia. It may also develop without any obvious predisposing cause.9 Failure of the right heart pressure to fall, leads to the ductus arteriosus remaining open and a persistent right to left shunt. The chest x-ray may show evidence of pneumonia, but the lung f|elds may have minimal changes or there may be oligaemia.The echocardiogram is helpful in demonstrating the right to left shunt.
Figure 2 Respiratory distress syndrome with right tension pneumothorax.
RADIOLOGYOF THE CHEST IN NEONATES
463
T ransient tachypnoea of the newborn
Delayed clearing of the amniotic fluid from the lungs during the f|rst few breaths results in wet lungsor transient tachypnoea of the newborn. The infant presents within the f|rst few hours of life with tachypnoea and mild to moderate hypoxia. Predisposing factors include Caesarean section, precipitous delivery, birth asphyxia and maternal diabetes. There is usually a gradual clinical improvement with minimal respiratory support over the subsequent few days.The chest x-ray typically shows normal volume lungs and streaky perihilar markings representing the distended pulmonary veins and lymphatics. There may be small effusions and fluid in the horizontal f|ssure. Clearing starts at about 12 h starting peripherally and from the upper lung f|elds.10
Pleural effusions and chylothorax
Pleural effusions may be part of generalized hydrops, secondary to perinatal infection, or due to abnormal lymphatic drainage of the pleural spaces.5 Chylothorax is the most common cause of a large pleural effusion in the newborn, although the pleural fluid does not become chylous until milk has been ingested (Fig. 5). Increasingly, large effusions are detected pre-natally when they are sometimes drained by thoracentesis or intra-uterine thoraco-amniotic shunt insertion in an attempt to prevent pulmonary hypoplasia. The male to female ratio is 2:1 and most affect the right hemithorax. The majority can be treated with single or repeated thoracocentesis and appropriate feeding with medium-chain triglycerides.
Meconium aspiration syndrome
Meconium staining of amniotic fluid is present in approximately 10 --15% of live births but only 1--1.5% have MAS. The viscid, hyperosmolar substances are aspirated resulting in widespread, patchy, asymmetrical opacities with areas of collapse and hyperinflation from air trapping due to the ball-valve effect of the meconium plugs (Fig. 4). There is a spectrum of severity depending on the quantity of meconium aspirated, and up to 25% develop air block complications of pneumothorax and pneumomediastinum.11 A chemical pneumonitis causes slow resolution of the opacif|cation. Secondary surfactant def|ciency and superimposed pneumonia are common. Survivors may have long-term respiratory failure due to lung damage.
Congenital abnormalities of lung development
By the third week of gestation, the primitive larynx, trachea and lung buds develop from a ventral diverticulum of the foregut. The oesophagotracheal ridges split the oesophagus from the trachea proceeding from caudal to cranial. By 6 weeks, primitive lung buds are present representing the early bronchial divisions. Anomalous budding results in bronchopulmonary foregut malformations including congenital lobar emphysema (CLE), congenital cystic adenomatoid malformation (CCAM) and pulmonary sequestration. Incomplete splitting of the oesophagotracheal ridge leads to oesophageal atresia with tracheo-oesophageal f|stula (TOF) anomalies.12 By 6 months gestation, 17 generations of branching have occurred. Terminal saccules are present and the number
Figure 4 Meconium aspiration syndrome.
Figure 5 Bilateral chylothorax.
464
CURRENT PAEDIATRICS
increases until birth and beyond. Surfactant-forming pneumocytes appear at approximately 24 weeks gestation.True alveolar development occurs after term for up to 3 years.
Pulmonary agenesis and hypoplasia
Pulmonary growth and development can be affected at different stages of fetal life resulting in hypoplasia or agenesis of one or both lungs.Restricted lung growth occurs due to oligohydramnios as in renal agenesis (Potters syndrome) or infantile polycystic kidneys, or in premature rupture of membranes. The thorax is small and bell-shaped with small-volume lungs. The abdomen appears hugely distended in cystic kidney disease (Fig. 6). Pneumothoraces are common. Unilateral lung agenesis appears as a completely opaque hemithorax with rib crowding and displacement of the mediastinum towards that side (Fig. 7). Associations with lung aplasia are cardiac anomalies, TOF, imperforate anus, renal dysgenesis and vertebral anomalies.13 Space occupying lesions within the thorax (diaphragmatic hernia,CLE,CCAM, effusions) can compress the ipsilateral lung causing hypoplasia.The contralateral lung may also be affected due to mediastinal compression. Many of these conditions are diag-
Figure 7 CTscan of left pulmonary hypoplasia.
Figure 8 Scimitar syndrome.
nosed on pre-natal ultrasound allowing for appropriate counselling and planning of delivery of the infant. Scimitar syndrome (venolobular syndrome) is a form of right lung agenesis or hypoplasia associated with anomalies of pulmonary vessels.14 The anomalous draining vein is seen as a scimitar-shaped density extending inferiorly towards the diaphragm (Fig. 8). It usually drains into the inferior vena cava but may enter the portal vein, hepatic vein or right atrium.The right pulmonary artery may be partly or completely absent. The condition has been associated with pulmonary sequestration, bronchogenic cyst, atrial septal defect and abnormalities of the diaphragm and bony thorax.
Pulmonary sequestration
This is def|ned as an aberrant mass of pulmonary tissue, usually at the left base, that has no normal connection with the bronchial tree or pulmonary arterial system. It possesses a systemic blood supply. It is frequently
Figure 6 Polycystic kidneys with pulmonary hypoplasia.
RADIOLOGYOF THE CHEST IN NEONATES
465
asymptomatic unless suspected from antenatal scans or recurrent chest infections. It may be associated with foregut malformations and CCAM. Systemic feeding vessels are best demonstrated in the fetus or early neonatal period with Doppler ultrasound, or with MRI angiography.15 In the newborn, the chest x-ray may be normal, but with repeated infection, a persisting opacity is seen at the lung base. Air fluid levels may also be seen within infected cavities.
Oesophageal atresia with tracheooesophageal f|stula
This condition may be suspected pre-natally with polyhydramnios and a small fetal stomach, or in the newborn period with choking, cyanosis and coughing during feeds. Failure to pass a nasogastric tube produces the typical chest x-ray with the tube coiled in the upper oesophageal pouch (Fig. 9). Air within distal bowel indicates a distal tracheo-oesophageal f|stulous connection. Approximately 50% of babies with tracheo-oesophageal atresia have associated anomalies of the heart, renal system, spine, limbs and anorectal malformations. Further imaging is required to identify these problems. If an H-type f|stula is suspected, a contrast-tube oesophagogram is performed to outline the f|stulous track. It usually arises anteriorly from the upper trachea near the thoracic inlet and extends cephalad into the oesophagus (Fig.10).16
Figure 10 Barium tube oesophagogram showing H-type tracheo-oesophageal f|stula.
Congenital lobar emphsema
This condition is characterized by progressive overdistension of (usually) one lobe. The majority are due to some kind of bronchial obstruction causing a ball-valve effect.The male to female ratio is 2:1and up to 50% have associated anomalies, usually of the cardiovascular system. Upper lobes are most commonly affected, followed by the right middle lobe. On the chest x-ray, there may initially be trapped fluid within the affected lobe, which appears opaque (Fig. 11a). As the fluid re-absorbs, a hyperinflated, hyperlucent lobe produces mediastinal shift and compression of adjacent lung (Fig.11b).CT is helpful in differentiating this condition from cystic lung lesions (Fig. 11c). The abnormal lobe may require surgical resection if symptomatic; however, many cases resolve spontaneously.17
Figure 9 Oesophageal atresia.
466
CURRENT PAEDIATRICS
Foregut malformations
Foregut cysts are anomalies of either foregut or tracheobronchial budding. Bronchogenic cysts are commonly mediastinal, either paratracheal or subcarinal, but are occasionally intrapulmonary. They have no communication with the tracheobronchial tree initially.18 Enteric cysts tend to be in the posterior mediastinum and include oesophageal duplication cysts. They may contain gastric mucosa, and spinal anomalies are associated. Neurenteric cysts have a similar radiological appearance of a posterior mediastinal soft tissue mass; however, vertebral anomalies are more common. MRI is the imaging modality of choice when the spine is involved; otherwise, CT def|nes the extent and relationship of these masses to other structures. CCAM is diagnosed with increasing frequency in the pre-natal period. It is caused by a hamartomatous proliferation of terminal bronchioles. The cysts communicate with the bronchial tree. Histologically, type 1 has cysts of varying sizes, at least one being more than 2 cm (approximately 50%). Type 2 has small uniform cysts of 1--10 mm and is associated with other congenital abnormalities. Type 3, composed of microcysts, has the poorest prognosis and is associated with fetal hydrops.The infant may present early with respiratory distress due to the mass effect and pulmonary hypoplasia. Late presentation due to recurrent infection also occurs.The initial chest x-ray may show mediastinal shift and opacif|cation of the abnormal lung. As fluid is resorbed, the hyperinflated area is hyperlucent with a bubbly appearance of multiple cysts. In many cases, the initial chest x-ray is normal; CTscanning demonstrates the extent of the abnormality and differentiates it from other cystic lung abnormalities (Fig.12).5,19
Figure 11 (a) Rightcongenitallobar emphysema showing mediastinal shift and opacif|cation ofthe abnormallung; (b) Right congenital lobar emphysema after clearing of fetal lung fluid; and (c) CTscan of right middle lobe congenitallobar emphysema.
Figure 12 CT scan of left congenital cystic adenomatoid malformation.
RADIOLOGYOF THE CHEST IN NEONATES
467
Congenital diaphragmatic hernia
Abdominal viscera herniate through the posterior pleuroperitoneal fold into the chest causing compression of the lungs and mediastinal shift; it is most frequent on the left (75%). The diagnosis is often made pre-natally. There is usually severe respiratory distress due to associated pulmonary hypoplasia. The typical chest x-ray shows mediastinal displacement and air-f|lled loops of bowel occupying one hemithorax (Fig. 13).5 Liver, spleen and stomach can all be herniated into the chest. The prognosis correlates closely with the degree of underlying lung hypoplasia.
Chest masses
Congenital cysts and tumours of neurogenic origin (neuroblastoma, ganglioneuroma, neurof|broma) make up most of the mediastinal masses encountered in the neonatal period, comprising 50 -- 60% of all masses. Teratomas and dermoid tumours account for 15--20%. The remainder is made up of thymomas, haemangiomas, cystic hygromas and sarcomas.3 Calcif|cation may be present in neurogenic tumours and teratomas. Compression of local structures with displacement of the trachea and bronchi can cause stridor and lobar collapse. Neuroblastoma can cause rib and vertebral erosion, and intraspinal extension can enlarge intervertebral foramina and cause pedicular flattening and spinal canal widening.Cystic hygromas in the thorax are usually from direct extension from the neck. CT or MRI with its multiplanar imaging ability are the imaging modalities of choice for thoracic tumours.
Figure 14 Osteogenesis imperfecta type II. Multiple Rib fractures and short fractures humeri.
Congenital chest deformities
A number of skeletal dysplasias are associated with a very small thorax with concomitant pulmonary hypoplasia.20 The most severe and more frequently encountered are thanatophoric dysplasia, osteogenesis imperfecta (lethal type) (Fig.14) and asphyxiating thoracic dystrophy ( Jeunes). The radiological features of each syndrome are often diagnostic. Many die in the early neonatal period from lung hypoplasia.
SUMMARY
This review has demonstrated the importance of close liaison of all clinical groups involved in the pre- and postnatal management of these infants who are often critically ill. There may be disorders of many systems and the condition may evolve requiring a frequent review of the imaging and further investigations. A wide variety of radiological tests are available and each must be tailored to the particular clinical circumstance to provide the best information. Highly trained staff and specialized equipment are necessary to minimize the risks while obtaining quality images.
REFERENCES
1. Fletcher EWL, Baum LD, Draper G. The risk of diagnostic radiation in the newborn. Br J Radiol 1986; 59: 165--170. 2. Cook JV, Shah K, Pablot S et al. Guidelines of Best Practice in the X-ray Imaging of Children. Surrey, Ian Allen Printing, 1998. 3. Swischuck LE. Imaging of the Newborn Infant and Young Child, 3rd edn. Baltimore: Williams & Wilkins, 1989. 4. Edwards DK, Hilton SVW, Merrit FA et al. RDS treatment with human surfactant: radiographic ndings. Radiology 1985; 157: 329--344.
Figure 13 Congenitalleft diaphragmatic hernia.
468
CURRENT PAEDIATRICS
5. Gibson AT, Steiner GM. Imaging the neonatal chest. Clin Radiol 1997; 52: 172--186. 6. Moylan FM, Walker AM, Kramer SS et al. The relationship of BPD to the occurrence of alveolar rupture during positive pressure ventilation. Crit Care Med 1978; 6: 140--142. 7. Wilson MG, Mikity VG. A new form of respiratory disease in premature infants. Am J Dis Child. 1960; 99: 489--499. 8. Webber S, Wilkinson AR, Lindsell D et al. Neonatal pneumonia. Arch Dis Child 1990; 65: 207--221. 9. Yu VY. Persistant pulmonary hypertension in the newborn. Early Hum Develop 1993; 33: 163--175. 10. Wesenberg RL, Graven SN, Mc Cabe EB. Radiological ndings in wet-lung disease. Radiology 1971; 98: 69--74. 11. Gooding CA, Gregory GA. Roentgenographic analysis of meconium aspiration of the newborn. Radiology 1971; 100: 131--140. 12. Inselman LS, Mellins RB. Growth and development of the lung. J Pediatr 1987; 98: 1--15. 13. Felson B. Pulmonary agenesis and related anomalies. Semin Roentgenol 1972; 7: 17--30.
14. Gao YA, Burrows PE, Benson LN et al. Scimitar syndrome in infancy. J Am Coll Cardiol 1993; 22: 873--882. 15. Felker RE, Tonkin IL. Imaging of pulmonary sequestration. AJR Am J Roentgenor 1990; 154: 241--249. 16. Benjamin B, Phan T. Diagnosis of H-type tracheo oesophageal stulae. J Pediatr Surgery 1991; 26: 667--671. 17. Kennedy CP, Habibi P, Matthew DJ et al. Lobar emphysema: long term imaging follow up. Radiology 1991; 180: 189--193. 18. Fowler CL, Pokorny WJ, Wagner ML, Kessler MS. Review of bronchopulmonary foregut malformations. J Pediatr Surg 1988; 23: 793--797. 19. SiHig SE, Asay GF. Cystic adenomatoid malformation in the newborn: two case studies and a review of the literature. Respir Care 2000; 45: 1188--1195. 20. Taybi H, Zachman RS. Radiology of Syndromes, Metabolic Disorders and Skeletal Dysplasias, 3rd edn. Chicago: YearBook Medical, 1990.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Prevención NAC y EDA NiñosDokumen13 halamanPrevención NAC y EDA NiñosUri MoraBelum ada peringkat
- Oxygen Therapy CBPGDokumen44 halamanOxygen Therapy CBPGUri Mora100% (2)
- Alergia AlimentariaDokumen16 halamanAlergia AlimentariaUri MoraBelum ada peringkat
- Clinical Predictors of PneumoniaDokumen10 halamanClinical Predictors of PneumoniaUri MoraBelum ada peringkat
- Americanas Neumo PDFDokumen291 halamanAmericanas Neumo PDFUri MoraBelum ada peringkat
- Pulmonary Venoocclusive Disease in ChildhoodDokumen8 halamanPulmonary Venoocclusive Disease in ChildhoodUri MoraBelum ada peringkat
- (Lung Biology in Health and Disease, V. 137) Richard D Bland - Jacqueline J Coalson-Chronic Lung Disease in Early Infancy-Marcel Dekker (2000)Dokumen1.080 halaman(Lung Biology in Health and Disease, V. 137) Richard D Bland - Jacqueline J Coalson-Chronic Lung Disease in Early Infancy-Marcel Dekker (2000)Uri MoraBelum ada peringkat
- Empiema en PediatriaDokumen7 halamanEmpiema en PediatriaUri MoraBelum ada peringkat
- (European Respiratory Monograph) A. Bush, K-H. Carlsen, M.S. Zach-Growing Up With Lung Disease - The Lung in Transition To Adult Life-European Respiratory Society Journals Ltd. (2002)Dokumen111 halaman(European Respiratory Monograph) A. Bush, K-H. Carlsen, M.S. Zach-Growing Up With Lung Disease - The Lung in Transition To Adult Life-European Respiratory Society Journals Ltd. (2002)Uri MoraBelum ada peringkat
- Asthma and Respiratory Physiology Putting Lung Function Into PerspectiveDokumen10 halamanAsthma and Respiratory Physiology Putting Lung Function Into PerspectiveUri MoraBelum ada peringkat
- Recommendation WHODokumen176 halamanRecommendation WHODananjaya JuniorBelum ada peringkat
- Acute Respiratory Distress Syndrome The Berlin DefinitionDokumen8 halamanAcute Respiratory Distress Syndrome The Berlin DefinitionUri MoraBelum ada peringkat
- Measurement of FEF and FEF Does Not Contribute To Clinical Decision MakingDokumen8 halamanMeasurement of FEF and FEF Does Not Contribute To Clinical Decision MakingUri MoraBelum ada peringkat
- LungFunction Ninos Menores 6 Anos 2013Dokumen11 halamanLungFunction Ninos Menores 6 Anos 2013Uri MoraBelum ada peringkat
- Pulmonary Alveolar MicrolithiasisDokumen9 halamanPulmonary Alveolar MicrolithiasisUri MoraBelum ada peringkat
- Acute Kidney Injury - Final Version (08 March 2011)Dokumen59 halamanAcute Kidney Injury - Final Version (08 March 2011)Abdel-hafiz MamounBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Strategic ManagementDokumen46 halamanStrategic ManagementWaseque Uddin Ahmed100% (2)
- Motor Neuron DiseasesDokumen103 halamanMotor Neuron DiseasesJamil AhmadBelum ada peringkat
- NRP HandoutDokumen10 halamanNRP HandoutElisabeth F. OjhaBelum ada peringkat
- Congenital Corneal DisordersDokumen101 halamanCongenital Corneal Disorderseyemd_in_training100% (1)
- Awakenings Video QuestionsDokumen2 halamanAwakenings Video Questionswatevermoron0% (1)
- DysrythmiasDokumen4 halamanDysrythmiasmgmjlm01_881676250100% (1)
- Effective Treatment of ExhibitionismDokumen2 halamanEffective Treatment of Exhibitionismex1617Belum ada peringkat
- The Heart and Soul of Change Getting BetDokumen2 halamanThe Heart and Soul of Change Getting BetLola Al Smith100% (1)
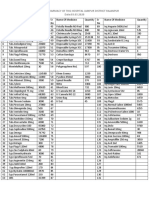
- Good Healthy Eating HabitsDokumen31 halamanGood Healthy Eating HabitsjoseBelum ada peringkat
- Nursing care for prostatectomy patientsDokumen8 halamanNursing care for prostatectomy patientsNicole HerreraBelum ada peringkat
- Kasus 2Dokumen3 halamanKasus 2Amalia RisnaBelum ada peringkat
- IOSRPHRDokumen2 halamanIOSRPHRIOSR Journal of PharmacyBelum ada peringkat
- Dermatofibroma Updated January 2020 - Lay Reviewed January 2020Dokumen3 halamanDermatofibroma Updated January 2020 - Lay Reviewed January 2020Gandhi BossBelum ada peringkat
- Grade 10 Disaster Management Project Pocket Guide On First AidDokumen6 halamanGrade 10 Disaster Management Project Pocket Guide On First AidSweta JainBelum ada peringkat
- Yellow Wallpaper Lit AnalysisDokumen6 halamanYellow Wallpaper Lit Analysisapi-197908942Belum ada peringkat
- Pancreas functions in digestion and glucose metabolismDokumen4 halamanPancreas functions in digestion and glucose metabolismClayton VerBerkmösBelum ada peringkat
- City & Guilds Unit 116: Support The Use of Medication in Social Care SettingsDokumen85 halamanCity & Guilds Unit 116: Support The Use of Medication in Social Care SettingsBex FerridayBelum ada peringkat
- Principles of intra-articular fracture careDokumen31 halamanPrinciples of intra-articular fracture carebaoBelum ada peringkat
- Club FootDokumen47 halamanClub FootSujanaBelum ada peringkat
- December 30, 2015 Tribune-PhonographDokumen15 halamanDecember 30, 2015 Tribune-PhonographcwmediaBelum ada peringkat
- Nutrilab, Inc. v. Schweiker, 547 F. Supp. 880 (N.D. IllDokumen4 halamanNutrilab, Inc. v. Schweiker, 547 F. Supp. 880 (N.D. Illapi-237393155Belum ada peringkat
- Surgical NursingDokumen7 halamanSurgical NursingNick BishopBelum ada peringkat
- Integrative Music TherapyDokumen6 halamanIntegrative Music TherapyAlmudena Sanchiz DiazBelum ada peringkat
- Digital Technology in EndoDokumen91 halamanDigital Technology in Endonandani kumariBelum ada peringkat
- Cognitive Therapy: Past, Present, and Future: Aaron T. BeckDokumen5 halamanCognitive Therapy: Past, Present, and Future: Aaron T. BeckLuisa LageBelum ada peringkat
- Pavlostathi Pharmaceutical Portfolio 1Dokumen3 halamanPavlostathi Pharmaceutical Portfolio 1api-255607190Belum ada peringkat
- Available Medicine at Pharmacy of THQ Hospital Jampur District Rajanpur Date:03.03.2020Dokumen2 halamanAvailable Medicine at Pharmacy of THQ Hospital Jampur District Rajanpur Date:03.03.2020Kashif AhmadBelum ada peringkat
- Joining Bupa GlobalDokumen16 halamanJoining Bupa GlobalMayar RagabBelum ada peringkat
- Comparative Health Information Management 4th Edition Peden Solutions Manual DownloadDokumen15 halamanComparative Health Information Management 4th Edition Peden Solutions Manual DownloadVickie Montejo100% (28)
- Minimal Intervention Dentistry (MID) For Managing Dental CariesDokumen3 halamanMinimal Intervention Dentistry (MID) For Managing Dental CariesatikramadhaniBelum ada peringkat