Quicktime and A Tiff (Uncompressed) Decompressor Are Needed To See This Picture
Diunggah oleh
clubstarDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Quicktime and A Tiff (Uncompressed) Decompressor Are Needed To See This Picture
Diunggah oleh
clubstarHak Cipta:
Format Tersedia
This gross liver shows numerous pale nodules of metastatic cancer.
It is not possible here to say from which organ these secondary growths came. |<img src=/f/livercancer.png>|
QuickTime and a TIFF (Uncompressed) decompressor are needed to see this picture.
IMDEPSAASIAC: Identify: This gross liver shows numerous pale nodules of metastatic cancer. It is not possible here to say from which organ these secondary growths came. Morphology: -Nodules: Massive Single focus or variable sized-multifoci, or diffuse (entire liver). -Hepatocytes arranged in cords or nests around the masses/densities. -Bile may be found in cytoplasm and in pseudocanalicula between cells. Disease: Hepatic carcinoma. Etiology (main): **Repeated cell damage in liver** Alcohol, Hep B virus, Hep C Virus, Hemochromatosis, Aflatoxin (hepatocarcinogen from plants). Or metastasis from other organs: stomach, intestine, colon, etc. Primary tumors are associated with repeated cell death and regeneration which leads to pathogenesis. Pathogenic mechanism: **KEY: REPEATED Cell death and regeneration with carcinogens=Carcinoma of liver.** Repated cell death-->HCC. Accumulations of mutations during continuous cycles of cell division may transform some hepatocytes. HBV DNA causes genomic instability--> deletions, translocations, duplications. X-proteins (from HBV) disrupts normal growth control-->activation of proto-oncogenes and disruption of cell cycles control. Also antiaptotic. HBV proteins also bind and inactivate tumor suppressor gene TP53.
Structural changes (specific, gross, and micro): **KEY: NODULES, Nest+Cords.** Primary liver carcinomas (which are almost all HCC) may appear as (1) a unifocal, massive tumor; (2) a multifocal malignancy, made of widely dstributed nodules of variable size; or (3) a diffusely infiltrative cancer, permeating widely and sometimes involving the entire liver. Sometimes snake-like masses may invade the portal vein, vena cava, and eventually the right heart.
QuickTime and a TIFF (Uncompressed) decompressor are needed to see this picture.
Extra:Histology is quite variable, ranging from well-differentiated lesions (arranged in cords or small nests) to poorly differentiated lesions, often made up of large multinucleate anaplastic giant cells. The fibrolamellar subtype (associated with young adults:20-40 yrs) is associated with a better prognosis for survival, possibly because it is not associated with cirrhosis and is more likely to be resectable. For this type, histologically, is composed of well-differentiaed polygonal cells arranged in nests or cords, separated by parallel lamellae of dense collagen bundles. The presence of intracellular bile or staining for AFP may be helpful in distinguishing HCC from other hepatic malignancies (eg, cholangiocarcinoma). |<img src=/f/livernest.png>| Are there any other sites of involvement in the body? Metastases may develop in the lung, portal vein, periportal nodes, bones, or brain Are there any other diseases where similar changes can be seen? Signs / Symptoms: Jaundice, ascites, hepatomegaly, alcoholic stigmata, asterixis, pedal edema, periumbilical collateral veins, enlarged hemorrhoidal veins, variceal bleeding, cachexia, right upper quandrant pain (uncommon).
Investigations (confirmation / gauge extent): **KEY: Raised AFP (sensitive, but not specific).** Expect total bilirubin, aspartate aminotransferase (AST), alkaline phosphatase, albumin, and prothrombin time to show results consistent with cirrhosis. Alpha-fetoprotein (AFP) is elevated in 75% of cases. Biopsy, imaging. Are there any other diseases you have studied where such tests can be positive? Increased AFP is associated with 90% of patients with HCC, but it has low specificity, because modestly elevated levels are also encountered in cirrhosis, massive liver necrosis, chronic hepatitis, normal pregnancy, fetal distress or death, fetal neural tube defects (anencephaly, spina bifida), and gonadal germ cell tumors. Very high levels are found almost exclusively in HCC. Course of disease progress (complications, monitoring, outcome): Overall prognosis for survival depends on the extent of cirrhosis and tumor stage, which then determine the appropriate treatment. HCC tends to remail confied to the liver until late in the course, when it may spread to lymph nodes, lungs, bones, adrenal glands, and other sites. Patients able to undergo a curative resection have a median survival of as long as 4 years; patients who present when they are too ill to be treated have a median survival of 3 months. Extra: A primary malignancy of the hepatocyte that generally leads to death within 6 months of onset. HCC frequently arises in the setting of cirrhosis, appearing 20-50 years following initial insult to the liver. However, 25% of patients have no history or risk factors for the development of cirrhosis. The extent of hepatic dysfunction limits treatment options, and patients usually die of liver failure. Highlight 3 important points: 1. Median survival is 7 months 2. Death from: profound cachexia, GI or esophageal bleeding, liver failure with hepatic coma, tumor rupture with fatal hemorrhage. 3. Only hope for cure is surgical resection of smaller tumors. But still have a recurrence rate of greater than 60% at 5 years. 4. Control: Vaccine against HBV. 5. Pronounced male preponderance of HCC worldwide (3:1 to 8:1). Blacks>whites. Vignette: 50 year old alcoholic male showed up to the ER complaining of unexplained weight loss, weakness, enlarged liver, and a slight pain on his right upper quadrant. Later that night, he woke up and threw up a lot of blood and died within minutes. Questions: 1. How do you distinguish primary liver cancer from metastasis in a gross specimen? Primary liver cancer presents as a unifocal nodule, whereas metastasis presents as multiple nodules.
2. What are the common sites of metastasis for cancers? What is the most important factor that determines the site for metastasis? The lungs and liver are common predilection sites for metastases; they are the circulatory sieves which have a tendency to accumulate neoplastic cells. 3. Which are the likely primary sites to produce metastasis in liver? Any area which drains into the hepatic portal system is a likely primary site: the stomach, intestines, colon, bones, etc 3. What is alpha fetoprotein? Alpha fetoprotein is a fetal antigen (i.e. expressed by embryonic tissue) and is a type of tumor marker. Alpha fetoprotein is elevated in cancer, and although it is not diagnostic, it can be useful in establishing a baseline of comparison for subsequent treatment modalities. Elevated levels are associated with hepatocellular carcinoma or embryonic cell carcinoma.
Anda mungkin juga menyukai
- 3rd Stage Liver Diseases (2) - HMUDokumen31 halaman3rd Stage Liver Diseases (2) - HMUjwan ahmedBelum ada peringkat
- hepatoCA 2Dokumen9 halamanhepatoCA 2Al VlaovicBelum ada peringkat
- Colorectal Carcinoma: Colorectal Carcinoma (CRC) Is The Most Common Cancer of The Gastrointestinal Tract and TheDokumen14 halamanColorectal Carcinoma: Colorectal Carcinoma (CRC) Is The Most Common Cancer of The Gastrointestinal Tract and TheYTBelum ada peringkat
- CholangiocarcinomaDokumen7 halamanCholangiocarcinomailovedaneBelum ada peringkat
- Histopathology of Hepatocellular CarcinomaDokumen11 halamanHistopathology of Hepatocellular CarcinomaCindy Sabina FaleandraBelum ada peringkat
- Rare Liver Cancer: Fibrolamellar Hepatocellular CarcinomaDokumen46 halamanRare Liver Cancer: Fibrolamellar Hepatocellular CarcinomaStephanie NuñezBelum ada peringkat
- LIVER CANCER CAUSES, SYMPTOMS & TREATMENTDokumen21 halamanLIVER CANCER CAUSES, SYMPTOMS & TREATMENTMusaBelum ada peringkat
- Liver TumorsDokumen12 halamanLiver Tumorskiemdinhit7Belum ada peringkat
- Liver Tumor Types and TreatmentsDokumen39 halamanLiver Tumor Types and Treatmentsinstagram googleBelum ada peringkat
- Colorectal CancerDokumen6 halamanColorectal CancerAshiniBelum ada peringkat
- Carcinoma of Renal Pelvis and UreterDokumen27 halamanCarcinoma of Renal Pelvis and UreterIsaac MwangiBelum ada peringkat
- AlsnlasnfDokumen13 halamanAlsnlasnfDina A. ŠabićBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen23 halamanNIH Public Access: Author ManuscriptkinemasBelum ada peringkat
- Renal Cell CarcinomaDokumen15 halamanRenal Cell Carcinomadger11Belum ada peringkat
- Renal Tumors RCC Renal Cells Carcinoma Renal Adenocarcinoma HypernephromaDokumen5 halamanRenal Tumors RCC Renal Cells Carcinoma Renal Adenocarcinoma HypernephromaMohamed Al-zichrawyBelum ada peringkat
- Pathophysiology, Clinical Presentation, and Management of CC (2008)Dokumen24 halamanPathophysiology, Clinical Presentation, and Management of CC (2008)Miguel RamírezBelum ada peringkat
- Cholangiocarcinoma - Radiology Reference Article - RadiopaediaDokumen5 halamanCholangiocarcinoma - Radiology Reference Article - RadiopaediaWill SmithBelum ada peringkat
- Hemicolectomy GuideDokumen5 halamanHemicolectomy GuideMuhammad MalikBelum ada peringkat
- TJW Bladder CancerDokumen35 halamanTJW Bladder CancerShariq ShaBelum ada peringkat
- Liver CancerDokumen44 halamanLiver CancerJoyce Ann CumlatBelum ada peringkat
- Prof - Amer Eltwati Ben Irhuma Consultant Surgeon Sebha Medical CollegeDokumen79 halamanProf - Amer Eltwati Ben Irhuma Consultant Surgeon Sebha Medical Collegeckyew64100% (1)
- Bladder Cancer 1Dokumen31 halamanBladder Cancer 1Anas HamadBelum ada peringkat
- Malignant Liver Tumours OxfordDokumen7 halamanMalignant Liver Tumours OxfordJose Tomás MooreBelum ada peringkat
- Ajdabya University Medical College - Colorectal Cancer Signs, Risks and ManagementDokumen81 halamanAjdabya University Medical College - Colorectal Cancer Signs, Risks and Managementckyew64Belum ada peringkat
- Hepatocellular Carcinoma: Hepatocellular Carcinoma (HCC, Also Called Malignant Hepatoma) Is The MostDokumen10 halamanHepatocellular Carcinoma: Hepatocellular Carcinoma (HCC, Also Called Malignant Hepatoma) Is The MostNurul An NisaBelum ada peringkat
- Germ Cell TumoursDokumen32 halamanGerm Cell Tumoursapi-3705046Belum ada peringkat
- The Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PADokumen19 halamanThe Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PAAnonymous D29e00Belum ada peringkat
- Genitourinary Tract Tumors Including Renal Tumors: Pre-ReadingDokumen31 halamanGenitourinary Tract Tumors Including Renal Tumors: Pre-Readingmus zaharaBelum ada peringkat
- शल्यतन्त्र Paper II, Part BDokumen79 halamanशल्यतन्त्र Paper II, Part BAnil DasBelum ada peringkat
- AdenocarcinomaDokumen6 halamanAdenocarcinoma6tsqs5bcs4Belum ada peringkat
- Structural/functional Properties of The BladderDokumen67 halamanStructural/functional Properties of The BladderMinda TilahunBelum ada peringkat
- Liver CancerDokumen44 halamanLiver CancerEjay Jacob Ricamara50% (2)
- 4 IntestineDokumen15 halaman4 IntestinemyarjddbzBelum ada peringkat
- Benign Lesions of The OvaryDokumen7 halamanBenign Lesions of The Ovaryredhasalah665Belum ada peringkat
- $12. Urinary Tract Infections 2015Dokumen39 halaman$12. Urinary Tract Infections 2015Sindhu BabuBelum ada peringkat
- Malignant Liver Tumors Undergrad 6th Year Students SharaanDokumen56 halamanMalignant Liver Tumors Undergrad 6th Year Students SharaanMohamed AhmedBelum ada peringkat
- Practice Essentials: Signs and SymptomsDokumen6 halamanPractice Essentials: Signs and SymptomsekaBelum ada peringkat
- Jordanian Surgical Society - PPT LastDokumen166 halamanJordanian Surgical Society - PPT LastNessreen Jamal100% (1)
- Fibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleDokumen3 halamanFibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleIKIKIKIKIKI999999Belum ada peringkat
- Benign and Malignant Lesion of Lower GIDokumen45 halamanBenign and Malignant Lesion of Lower GIAhmad Alzu3beBelum ada peringkat
- Pathology Lab Guidebook 2019 CH 17 Hepatobiliary SystemDokumen11 halamanPathology Lab Guidebook 2019 CH 17 Hepatobiliary System6460801016Belum ada peringkat
- COLORECTAL CANCER FINAL PPT To Be PresentedDokumen53 halamanCOLORECTAL CANCER FINAL PPT To Be Presentedamanuel100% (1)
- Pertanyaan Referat CA SigmoidDokumen9 halamanPertanyaan Referat CA SigmoidBelladinaMMBelum ada peringkat
- Gallbladder Carcinoma: Anatomy, Risk Factors, Staging and TreatmentDokumen29 halamanGallbladder Carcinoma: Anatomy, Risk Factors, Staging and TreatmentRashmiBelum ada peringkat
- Carcinoma Gall BladderDokumen25 halamanCarcinoma Gall Bladderrajan kumarBelum ada peringkat
- Hematuria in AdultsDokumen9 halamanHematuria in AdultsTheddyon BhenlieBelum ada peringkat
- Guide to evaluating hematuria in adultsDokumen9 halamanGuide to evaluating hematuria in adultsTheddyon BhenlieBelum ada peringkat
- Zinoide To Indicate The Carcinoma-Like Appearance and The PreDokumen4 halamanZinoide To Indicate The Carcinoma-Like Appearance and The PreKarim SupanovaBelum ada peringkat
- Liver Cancer Risk Factors, Symptoms, Imaging & StagingDokumen29 halamanLiver Cancer Risk Factors, Symptoms, Imaging & StagingRizky KurniawanBelum ada peringkat
- Colorectal CancerDokumen68 halamanColorectal Cancerjack sawda100% (1)
- Ecr2017 C-1147Dokumen52 halamanEcr2017 C-1147julius yves bagacayBelum ada peringkat
- NEOPLASIADokumen70 halamanNEOPLASIARose de DiosBelum ada peringkat
- 45657Dokumen28 halaman45657zoxpop1980Belum ada peringkat
- Carcinoma of ColonDokumen39 halamanCarcinoma of ColonMuhammad DaniyalBelum ada peringkat
- Definisi, Epidemiologi, Klasifikasi, dan Terapi Karsinoma HepatokelularDokumen37 halamanDefinisi, Epidemiologi, Klasifikasi, dan Terapi Karsinoma HepatokelularkadinfathiaBelum ada peringkat
- CAP Protocol-2016 Thyroid - HighlightedDokumen8 halamanCAP Protocol-2016 Thyroid - Highlightedpath2016Belum ada peringkat
- Squamous Cell Tumors Bile Duct Cancers: PathophysiologyDokumen6 halamanSquamous Cell Tumors Bile Duct Cancers: PathophysiologySiti RahmahBelum ada peringkat
- HCC HarrisonDokumen5 halamanHCC HarrisonJesly CharliesBelum ada peringkat
- Hyper Cortisol Is MDokumen1 halamanHyper Cortisol Is MclubstarBelum ada peringkat
- 2014step3 Sample Items 11032014Dokumen41 halaman2014step3 Sample Items 11032014Christian JaraBelum ada peringkat
- Disease Deficient Enzyme Cardinal Clinical Features Glycogen Structure Von Gierke'sDokumen84 halamanDisease Deficient Enzyme Cardinal Clinical Features Glycogen Structure Von Gierke'sclubstar100% (4)
- Torso - Thorax Overview - Cherchi - 1999Dokumen17 halamanTorso - Thorax Overview - Cherchi - 1999clubstarBelum ada peringkat
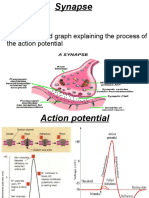
- Synapse Structure and Function ExplainedDokumen11 halamanSynapse Structure and Function ExplainedMuhammad AbdullahBelum ada peringkat
- CRA-W Ra03-04 enDokumen116 halamanCRA-W Ra03-04 enThanh MiBelum ada peringkat
- Therapeutic Cancer VaccinesDokumen19 halamanTherapeutic Cancer VaccinesIrguard AdminBelum ada peringkat
- Introduction To Crop Protection 1Dokumen16 halamanIntroduction To Crop Protection 1Nida Ratilla100% (2)
- REV Micro HSB RemedsDokumen16 halamanREV Micro HSB RemedsPatricia HariramaniBelum ada peringkat
- Photosynthesis WorksheetDokumen2 halamanPhotosynthesis WorksheetYhannai FerronBelum ada peringkat
- BASIC HUMAN NEEDS WordDokumen70 halamanBASIC HUMAN NEEDS WordManju TalluriBelum ada peringkat
- Biology Ia IbdpDokumen10 halamanBiology Ia Ibdpzain ahmedBelum ada peringkat
- Gerard MullinDokumen21 halamanGerard Mullinchocoholic_soph91Belum ada peringkat
- Insulin and Insulin ResistanceDokumen21 halamanInsulin and Insulin ResistanceFisiologiaUFCG100% (1)
- Concepts of BiologyDokumen615 halamanConcepts of BiologyGrant M EsteppBelum ada peringkat
- Super 20 Ch-7 Control & Coordination Class 10 Science (2) YeahhhhhDokumen2 halamanSuper 20 Ch-7 Control & Coordination Class 10 Science (2) Yeahhhhhkamalkandpal4848Belum ada peringkat
- Genetics - Student SampleDokumen13 halamanGenetics - Student SampleMaria Isabel MorandiBelum ada peringkat
- 6 Enzymes and Cellular Regulation-SDokumen5 halaman6 Enzymes and Cellular Regulation-Sapi-502781581Belum ada peringkat
- Chapter 9 Homework PDFDokumen3 halamanChapter 9 Homework PDFRhonda JacobsBelum ada peringkat
- Natural Selection Bird SimulationDokumen6 halamanNatural Selection Bird SimulationSumaira UddinBelum ada peringkat
- Test Review - Cells, Cell Transportation and Communication: Unit ObjectivesDokumen5 halamanTest Review - Cells, Cell Transportation and Communication: Unit ObjectivesCole McFarlandBelum ada peringkat
- Clinical and Microbiology SSIDokumen6 halamanClinical and Microbiology SSIFaozan FikriBelum ada peringkat
- Biological Basis of Sexual OrientationDokumen18 halamanBiological Basis of Sexual OrientationIndira EspitiaBelum ada peringkat
- Genetics Exp 6Dokumen6 halamanGenetics Exp 6Ck WongBelum ada peringkat
- BIOMOLECULES General BiologyDokumen23 halamanBIOMOLECULES General BiologyKurt Russel CarlosBelum ada peringkat
- Fakultas Kedokteran: Kementerian Pendidikan Dan Kebudayaan Universitas Jenderal SoedirmanDokumen1 halamanFakultas Kedokteran: Kementerian Pendidikan Dan Kebudayaan Universitas Jenderal SoedirmanChausarPutraBenagilBelum ada peringkat
- Basic Physiology of The SkinDokumen4 halamanBasic Physiology of The SkinRegina SinagaBelum ada peringkat
- Deaf Mute PaperDokumen11 halamanDeaf Mute PaperneviBelum ada peringkat
- Biology Notebook For All Bio ClassesDokumen392 halamanBiology Notebook For All Bio Classesnikitaanne83% (12)
- Frog Embryo PDFDokumen17 halamanFrog Embryo PDFmicrobeateria100% (1)
- Biology Form 4 Chapter 4.5 EnzymesDokumen11 halamanBiology Form 4 Chapter 4.5 EnzymesSatpal SinghBelum ada peringkat
- Iranian English journals in ScopusDokumen4 halamanIranian English journals in ScopushusseinBelum ada peringkat
- Lysosomes PresentationDokumen53 halamanLysosomes PresentationCaroline Stephenson50% (2)
- Milk Thistle Extract PreparationDokumen13 halamanMilk Thistle Extract PreparationSinisa KusnjirBelum ada peringkat