Peptic Ucler Disease
Diunggah oleh
Pro fatherDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Peptic Ucler Disease
Diunggah oleh
Pro fatherHak Cipta:
Format Tersedia
1) Protection of the Stomach:
Living stomach is protected in 5 ways from harsh acidic and enzymatic environment it creates: 1) Mucous coat: - thick, highly alkaline mucus resists the actions of acids & enzymes. 2) Epithelial cell replacement: - Stomach epithelial cells live only 3-6 days - are then sloughed off into the chyme & digested with food - replaced as rapidly by cells division in gastric pits. 3) Tight Junctions: - Epithelial cells joined by tight junctions - Prevent gastric juice from seeping between them & digesting the connective tissue of lamina propria and beyond. 4) Bicarbonate secretions: - Produced by epithelial cells in stomach & duodenum - Creates neutral PH environment into boundary zone of adherent mucus 5) Prostaglandin synthesis: - Stimulated by stretching of stomach, and is produced by mucous cells. - Favours production of bicarbonates and mucous & inhibit acid secretion by parietal cells.
2) Peptic Ulcer Disease (PUD): Gastritis inflammation of stomach Can lead to a peptic ulcer pepsin + HCL erode stomach wall. Occur commonly in duodenum Occasionally in oesophagus If untreated they can perforate the organ: Cause fatal haemorrhage or peritonitis Most fatalities occur in people over 65 No evidence between peptic ulcer and stress:
Stress-Related Ulcers. Stress ulcers are ulcers of the stomach or duodenum that occur in
the context of a profound illness or trauma requiring intensive care. The etiology of stressrelated ulcers differs somewhat from that of other peptic ulcers, involving acid and mucosal ischemia. Because of limitations on the oral administration of drugs in many patients with stress-related ulcers, intravenous H2-receptor antagonists have been used extensively to reduce the incidence of GI hemorrhage due to stress ulcers. Now that intravenous preparations of proton pump inhibitors are available, it is likely that they will prove to be equally beneficial. However, there is some concern over the risk of pneumonia secondary to gastric colonization by bacteria in an alkaline milieu. In this setting, sucralfate appears to provide reasonable prophylaxis against bleeding without increasing the risk of aspiration pneumonia. This approach also appears to provide reasonable prophylaxis against bleeding, but is less convenient (Cook et al., 1998).
Hypersecretion of acid and pepsin -- sometimes involved Most involve acid-resistant gram (-) bacterium, Helicobacter Pylori Invades mucosa of stomach & duodenum Opens the way to chemical damage to tissues Risk factors: smoking; aspirin usage + other NSAIDS NSAIDS, supress synthesis of prostaglandins o Normally stimulate secretion of protective mucus + acidreducing bicarbonate o Aspirin is an acid that directly irritates gastric mucosa
Gross appearance: a) Clean, sharply demarcated and slightly elevated around the edges b) Most gastric ulcers are benign o Small percentage maybe malignant c) Duodenal ulcers are never malignant d) Four layers in sequence are noted in histologic sections of ulcers: 1- Necrotic debris 2- Inflammation with a predominance of neutrophils 3- Granulation tissue (repair tissue) 4- Fibrosis
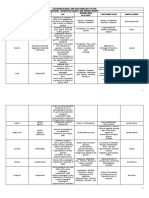
3) Comparison between Gastric Ulcers and Doudenal Ulcers: Feature Percentage of ulcer cases Epidemiology Gastric Ulcers 25% Male-female ratio 1.5 to 2:1 Smoking does not cause PUD but delays healing Duodenal Ulcers 75% Male-female ratio 3:1 Women are most affected at or after menopause. Increased risk in cirrhosis, Chronic Obstructive Pulmonary Disease, renal failure, hyperparathyroidism 80% of cases Defective mucosal barrier due to H. pylori Mucosal ischemia (reduced PGE), bile reflux, delayed gastric emptying
Helicobacter pylori Pathogenesis
90-95% of cases Defective mucosal barrier due to H. pylori
Increased acid production (increased parietal cell mass)
Basal Acid Output and Maximal Acid Output normal to decreased Location Single ulcer on lesser curvature of antrum (same gastric cancer location) Bleeding (most commonly in left gastric artery) Perforation
Complications
Clinical findings Diagnosis
Burning epigastric pain soon after eating Endoscopy; biopsy for gastric ulcers is a must for malignancy check-up.
Basal Acid Output and Maximal Acid Output both increased Single ulcer on anterior portion of first part of duodenum followed by single ulcer on posterior portion (danger of perforation into pancreas) Bleeding (most commonly in gastroduodenal artery) Perforation (air under diaphragm, pain radiates to left shoulder) Gastric outlet obstruction, pancreatitis Burning epigastric pain 1-3 hours after eating Endoscopy; biopsy is not needed for duodenal ulcer is never malignant.
Treatment
Stop Smoking, alcohol, and NSAIDS. Avoid foods that may cause such symptoms. Eradicate H. Pylori; Use H2 antagonists, PPI, or antacids Surgery Method: anteroctomy or hemigasterectomy for ulcer removal without selective vagetomy.
Stop Smoking, alcohol, and NSAIDS. Avoid foods that may cause such symptoms. Eradicate H. Pylori; use H2 antagonists, PPI, or antacids Surgery Method: selective vagetomy
Anda mungkin juga menyukai
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- CIN & Cervical ScreeningDokumen51 halamanCIN & Cervical ScreeningPro fatherBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Neurological Paraneoplastic Syndromes: An OverviewDokumen13 halamanNeurological Paraneoplastic Syndromes: An OverviewPro father100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Cumming - Otolaryngology - EpistaxisDokumen9 halamanCumming - Otolaryngology - EpistaxisPro fatherBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Heart DefectsDokumen20 halamanHeart DefectsPro fatherBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Cervical CancerDokumen36 halamanCervical CancerPro fatherBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Clinical Case On JaundiceDokumen43 halamanClinical Case On JaundicePro fatherBelum ada peringkat
- Clinical Case DiarrheaDokumen49 halamanClinical Case DiarrheaPro fatherBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Testicular CancerDokumen23 halamanTesticular CancerPro fatherBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Abdominal PainDokumen38 halamanAbdominal PainPro fatherBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Groundhog DayDokumen11 halamanGroundhog DayPro fatherBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Urinary Tract InfectionsDokumen18 halamanUrinary Tract InfectionsPro fatherBelum ada peringkat
- GI Bacterial InfectionsDokumen2 halamanGI Bacterial InfectionsPro fatherBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- ECG LeadsDokumen13 halamanECG LeadsPro fatherBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- FMRIDokumen10 halamanFMRIPro fatherBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Apoptosis & NecrosisDokumen12 halamanApoptosis & NecrosisPro fatherBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Skull DevelopmentDokumen15 halamanSkull DevelopmentPro fatherBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Neuroglia: Non-Neuronal Cells of The Nervous SystemDokumen18 halamanNeuroglia: Non-Neuronal Cells of The Nervous SystemPro fatherBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Billirubin MetabolismDokumen37 halamanBillirubin MetabolismPro father100% (1)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Cholinergic and Noradrenergic Neurons: Key Components of the Diffuse Modulatory SystemDokumen11 halamanCholinergic and Noradrenergic Neurons: Key Components of the Diffuse Modulatory SystemPro fatherBelum ada peringkat
- Heart DefectsDokumen20 halamanHeart DefectsPro fatherBelum ada peringkat
- Biology Curriculum MapDokumen2 halamanBiology Curriculum Mapapi-644434957Belum ada peringkat
- Bio SafetyDokumen57 halamanBio SafetySatyaveer SinghBelum ada peringkat
- Prestigi0us BiochemistryDokumen30 halamanPrestigi0us Biochemistrybovey69015Belum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- AABB Billing Guide For Blood Products and Related Services: July 2020 1Dokumen45 halamanAABB Billing Guide For Blood Products and Related Services: July 2020 1Rija KhanBelum ada peringkat
- Letter WritingDokumen17 halamanLetter WritingEmtiaj RahmanBelum ada peringkat
- GASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXDokumen11 halamanGASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXRhealyn LegaspiBelum ada peringkat
- Mitochondrial Cytopathies in Children and AdultsDokumen28 halamanMitochondrial Cytopathies in Children and AdultsmmaitehmdBelum ada peringkat
- Case Scenario: Self-Risk AssessmentDokumen2 halamanCase Scenario: Self-Risk AssessmentAlyanna Alcazar CapateBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- CH 59 Care of Patients With Problems of The Biliary System and PancreasDokumen28 halamanCH 59 Care of Patients With Problems of The Biliary System and Pancreasjrflores1284Belum ada peringkat
- Alex Cox Death 911 Call TranscriptDokumen10 halamanAlex Cox Death 911 Call Transcripttmiller696733% (3)
- Wound Care InstructionsDokumen3 halamanWound Care InstructionsKat TaasinBelum ada peringkat
- Fall 2010 Eco Newsletter, EcoSuperiorDokumen12 halamanFall 2010 Eco Newsletter, EcoSuperiorEco SuperiorBelum ada peringkat
- 2024 - ĐỀ 4Dokumen10 halaman2024 - ĐỀ 4ellypham1357Belum ada peringkat
- Equipo de Contrapulsacion Arrow-KaatDokumen103 halamanEquipo de Contrapulsacion Arrow-KaatCarito HernandezBelum ada peringkat
- Effectiveness of 6 Step Prevention and Control For Dengue Hemorrhagic Fever in Rural Community of ThailandDokumen142 halamanEffectiveness of 6 Step Prevention and Control For Dengue Hemorrhagic Fever in Rural Community of ThailandMendoza Alech ChelaBelum ada peringkat
- GS 101 Advance English SkillsDokumen49 halamanGS 101 Advance English SkillsJomarie Sahhara Grande Turtoga0% (1)
- Atc DDD OlukaDokumen65 halamanAtc DDD Olukarini setyawatiBelum ada peringkat
- Essential Health Services and PlansDokumen4 halamanEssential Health Services and Planszahara mahalBelum ada peringkat
- EHSMS Performance and Incident ReportingDokumen38 halamanEHSMS Performance and Incident ReportingravimanasBelum ada peringkat
- Introduction of PHCDokumen39 halamanIntroduction of PHCIdiris Mohamed100% (1)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Pharmacology ReviewerDokumen21 halamanPharmacology ReviewerCzairalene QuinzonBelum ada peringkat
- Managing Cardiac Patients in the ICUDokumen26 halamanManaging Cardiac Patients in the ICUvamshidh100% (2)
- Emropub 2016 en 19266Dokumen45 halamanEmropub 2016 en 19266jamshaidjiBelum ada peringkat
- Cement CSRDokumen35 halamanCement CSRKasak Gupta100% (1)
- Bannock Awareness: Celebrating Aboriginal Culture Through RecipesDokumen28 halamanBannock Awareness: Celebrating Aboriginal Culture Through RecipesMaggie SedgemoreBelum ada peringkat
- Pneumonia: Causes, Signs, Symptoms and Nursing CareDokumen16 halamanPneumonia: Causes, Signs, Symptoms and Nursing CareMelissa David100% (1)
- Pediatrics ImpDokumen233 halamanPediatrics Impملك عيسى100% (1)
- AllergiesDokumen11 halamanAllergiesAficionadoBelum ada peringkat
- Severe Acute Respiratory Syndrome Coronavirus 2Dokumen31 halamanSevere Acute Respiratory Syndrome Coronavirus 2Ian VillacrusisBelum ada peringkat