CT Ins Dept - BullHC70
Diunggah oleh
cerbone0Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CT Ins Dept - BullHC70
Diunggah oleh
cerbone0Hak Cipta:
Format Tersedia
STATE OF CONNECTICUT
INSURANCE DEPARTMENT
BULLETIN HC-70 AUGUST 1, 2008
TO:
ALL INSURANCE COMPANIES, FRATERNAL BENEFIT SOCIETIES, HOSPITAL SERVICE CORPORATIONS, MEDICAL SERVICE CORPORATIONS AND HEALTH CARE CENTERS THAT DELIVER OR ISSUE INDIVIDUAL AND GROUP HEALTH INSURANCE POLICIES IN CONNECTICUT
RE:
NOTICE PURSUANT TO CONNECTICUT GENERAL STATUTE 38a-477a OF NEW OR MODIFIED BENEFITS REQUIRED TO BE PROVIDED
The legislature enacted several new laws that impact group and individual health insurance policies delivered or issued for delivery in Connecticut. All entities are reminded that all policy forms are subject to prior approval. Policies are reviewed in the order of date received by the Insurance Department. For policy forms that are already approved, you are asked to file an endorsement or amendatory rider to be attached to the approved policy in order to expedite the review process. Entities should file a red lined version as well as two clean copies along with a postage paid envelope of sufficient size to receive a stamped copy. In addition, for new benefits on policies that require rates be filed, a rate filing should be made at the same time as the form filing even if there is no adjustment to the rates. Since some mandates are required to be added to existing policies prior to renewal, carriers should file forms and rates as early as possible to meet any contractual notice requirements.
PA 08-125 An Act Concerning Benefits for Inpatient Treatment of Serious Mental or Nervous Conditions This act expands the benefits payable under a group health insurance policy for treatment received in a residential treatment facility by eliminating a three-day hospital stay prerequisite. It requires benefits to be payable when upon assessment by a physician, psychiatrist, psychologist or clinical social worker, the individual cannot be appropriately, safely or effectively treated in an acute care, partial hospitalization, intensive outpatient or outpatient setting. This bill also extends the benefits to adults. This change is effective for new and existing policies and certificates beginning on January 1, 2009. (C.G.S.38a-514(k))
PA 08-132 An Act Requiring Insurance Coverage for Autism Spectrum Disorder Therapies This act requires all group and individual health insurance policies providing coverage of the type specified in subdivisions (1), (2), (4), (11) and (12) of section 38a-469 of the general statutes that are delivered, issued for delivery, renewed, amended or continued on or after
www.ct.gov/cid P.O. Box 816 Hartford, CT 06142-0816 An Equal Opportunity Employer
January 1, 2009 provide coverage for physical therapy, speech therapy and occupational therapy services for the treatment of autism spectrum disorders as set forth in the most recent edition of the American Psychiatric Associations Diagnostic and Statistical Manual of Mental Disorders, to the extent such services are a covered benefit for other diseases and conditions under such policies.
PA 08-147 An Act Making Changes to the Insurance Statutes All individual health policies providing coverage of the type specified in subdivisions (1), (2), (4), (6), (10), (11) and (12) of section 38a-469 of the general statutes delivered, issued for delivery, amended or renewed in this state on or after January 1, 2009, shall provide that coverage for a child shall terminate no earlier than the policy anniversary date on or after whichever of the following occurs first, the date on which the child: marries; ceases to be a resident of the state; becomes covered under a group health plan through dependents own employment; or attains the age of twenty six. The residency requirement shall not apply to dependent children under nineteen years of age or full-time students attending an accredited institution of higher learning. (C.G.S. 38a-497) All group health insurance policies providing coverage of the type specified in subdivisions (1), (2), (3), (4), (11) and (12) of section 38a-469, shall provide the option for a child to continue coverage for the longer of the following periods: At the end of the month following the month in which the child marries; ceases to be a resident of the state; becomes covered under a group health plan through dependents own employment; or attains the age of twenty six. The residency requirement shall not apply to dependent children under nineteen years of age or fulltime students attending an accredited institution of higher learning. This applies to new and existing policies on and after January 1, 2009. (C.G.S. 38a-554) The Department is issuing a separate Bulletin containing more detail and Questions and Answers on the new rules for termination of coverage for children under PA 08-147. Effective October 1, 2008, this act defines limited coverage to be a policy providing coverage of the type specified in subdivisions (1), (2), (4), (11) and (12) of section 38a-469 of the general statutes that contains an annual maximum benefit of less than one hundred thousand dollars or fixed dollar benefits of less than twenty thousand dollars on any core services. For the purpose of this section core services means medical, surgical and hospital services, including inpatient and outpatient physician, laboratory and imaging services. (C.G.S. 38a-482b and 38a-513d)
Please contact the Insurance Department Life and Health Division at ctinsdept.lifehealth@ct.gov with any questions about the Public Acts in this notice.
Thomas R. Sullivan Insurance Commissioner
Anda mungkin juga menyukai
- The Secret of The House WTDokumen22 halamanThe Secret of The House WTPetr -50% (2)
- DHHS Guidance On External Review For Group Health Plans and Health Insurance IssuersDokumen16 halamanDHHS Guidance On External Review For Group Health Plans and Health Insurance IssuersJeff ReifmanBelum ada peringkat
- The Ultimate Safari (A Short Story)Dokumen20 halamanThe Ultimate Safari (A Short Story)David AlcasidBelum ada peringkat
- Social Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionDari EverandSocial Security / Medicare Handbook for Federal Employees and Retirees: All-New 4th EditionBelum ada peringkat
- Physician Group Employed 1Dokumen10 halamanPhysician Group Employed 1Abhay TandonBelum ada peringkat
- Mufon Ufo JournalDokumen21 halamanMufon Ufo JournalSAB78Belum ada peringkat
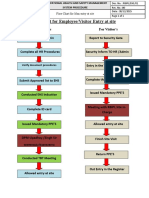
- fLOW CHART FOR WORKER'S ENTRYDokumen2 halamanfLOW CHART FOR WORKER'S ENTRYshamshad ahamedBelum ada peringkat
- Case Studies On Industrial Accidents - 2Dokumen84 halamanCase Studies On Industrial Accidents - 2Parth N Bhatt100% (2)
- 10059-DC-K-01-A Design BasisDokumen34 halaman10059-DC-K-01-A Design BasisAnonymous RvIgDUBelum ada peringkat
- Farid Jafarov ENG Project FinanceDokumen27 halamanFarid Jafarov ENG Project FinanceSky walkingBelum ada peringkat
- No Balance Billing PolicyDokumen6 halamanNo Balance Billing PolicyRhyne Amante YpulongBelum ada peringkat
- Alternate Mekton Zeta Weapon CreationDokumen7 halamanAlternate Mekton Zeta Weapon CreationJavi BuenoBelum ada peringkat
- Philippine Health Insurance vs. Chinese GenDokumen8 halamanPhilippine Health Insurance vs. Chinese GenFlorz GelarzBelum ada peringkat
- Abstract - Tropen Tag 2011 PDFDokumen634 halamanAbstract - Tropen Tag 2011 PDFzmoghesBelum ada peringkat
- Spec BoilerDokumen9 halamanSpec BoilerAchmad MakmuriBelum ada peringkat
- Executed Michigan SB 248, 2011 PA 142 (Sept. 20, 2011)Dokumen6 halamanExecuted Michigan SB 248, 2011 PA 142 (Sept. 20, 2011)Paul MastersBelum ada peringkat
- Species Diversity in Lentic and Lotic Systems of Lake Tamblyn and The Mcintyre RiverDokumen21 halamanSpecies Diversity in Lentic and Lotic Systems of Lake Tamblyn and The Mcintyre Riverapi-393048315Belum ada peringkat
- State of Connecticut: Insurance DepartmentDokumen2 halamanState of Connecticut: Insurance Departmentapi-27631527Belum ada peringkat
- Bill NoDokumen28 halamanBill NoRob PortBelum ada peringkat
- May 2012 PIP FAQDokumen9 halamanMay 2012 PIP FAQinfo6272Belum ada peringkat
- Terms Conditions Provider Relief 20 BDokumen11 halamanTerms Conditions Provider Relief 20 BRanal QurbanovBelum ada peringkat
- Terms Conditions Phase 2 General Distribution Relief FundDokumen10 halamanTerms Conditions Phase 2 General Distribution Relief FundRanal Qurbanov100% (1)
- Summary of The No Surprises Act (H.R. 133, P.L. 116-260)Dokumen26 halamanSummary of The No Surprises Act (H.R. 133, P.L. 116-260)Neil StreetBelum ada peringkat
- BackgroundDokumen27 halamanBackgroundrun2fast4meBelum ada peringkat
- The Affordable Care Act: Universal and Continuous CoverageDokumen16 halamanThe Affordable Care Act: Universal and Continuous CoverageIndiana Family to FamilyBelum ada peringkat
- UT Insurance Act DraftDokumen3 halamanUT Insurance Act DraftjbrecaldeBelum ada peringkat
- Health System Reform Short SummaryDokumen11 halamanHealth System Reform Short SummarySteve LevineBelum ada peringkat
- Be It Enacted by The People of The State of Illinois, Represented in The General AssemblyDokumen39 halamanBe It Enacted by The People of The State of Illinois, Represented in The General AssemblyAnn DwyerBelum ada peringkat
- Ab - 97 - Health Care ServicesDokumen133 halamanAb - 97 - Health Care ServicesCalWonkBelum ada peringkat
- HospitalAgreement LADokumen48 halamanHospitalAgreement LARi OzBelum ada peringkat
- Easy Health Premium Plan SummaryDokumen13 halamanEasy Health Premium Plan Summaryama2amalBelum ada peringkat
- Aetna Hmo 20 GeorgiaDokumen94 halamanAetna Hmo 20 Georgiabill_w85081Belum ada peringkat
- Tennessee Child Support Guidelines RulesDokumen69 halamanTennessee Child Support Guidelines RulesburritoiceBelum ada peringkat
- Eo 87600 1 22Dokumen4 halamanEo 87600 1 22Kaylee SteinBelum ada peringkat
- Nami 3803 North Fairfax Drive, Suite 100 Arlington, VA 22203-1701 (703) 524-7600Dokumen4 halamanNami 3803 North Fairfax Drive, Suite 100 Arlington, VA 22203-1701 (703) 524-7600Jasmine Elisa BeltranBelum ada peringkat
- Entitlement To BenefitsDokumen10 halamanEntitlement To BenefitsMimi KasukaBelum ada peringkat
- Medical Marijuana Chronic PainDokumen14 halamanMedical Marijuana Chronic PainDerek VoelkerBelum ada peringkat
- Easy Health Insurance (Family) BrochureDokumen2 halamanEasy Health Insurance (Family) Brochuresahilmehra141Belum ada peringkat
- Healthcare Presentation MaterialDokumen8 halamanHealthcare Presentation MaterialMadhan KraceeBelum ada peringkat
- P ERC Obama Announcement For Transition Relief1Dokumen3 halamanP ERC Obama Announcement For Transition Relief1c62ke40Belum ada peringkat
- Maria T. Vullo Superintendent Andrew M. Cuomo GovernorDokumen9 halamanMaria T. Vullo Superintendent Andrew M. Cuomo GovernorrkarlinBelum ada peringkat
- Portability allows health insurance credits to transfer between insurersDokumen15 halamanPortability allows health insurance credits to transfer between insurersroyjeenaelizabethBelum ada peringkat
- Health Companion 12 - 2011an-02Dokumen2 halamanHealth Companion 12 - 2011an-02sprashant5Belum ada peringkat
- SPD Ra Spd2011Dokumen51 halamanSPD Ra Spd2011Judy RomatelliBelum ada peringkat
- Health Insurance Portability and Accountability ActDokumen5 halamanHealth Insurance Portability and Accountability ActqweasdcasewBelum ada peringkat
- New Dependent Child DefinitionDokumen11 halamanNew Dependent Child DefinitionJoshua MarksBelum ada peringkat
- Chapter 48 P.L. 1999Dokumen4 halamanChapter 48 P.L. 1999RCBelum ada peringkat
- Phase 4 Provider Relief Fund Payment TermsDokumen10 halamanPhase 4 Provider Relief Fund Payment TermsRanal QurbanovBelum ada peringkat
- ALEC Mandated Benefits Review ActDokumen3 halamanALEC Mandated Benefits Review ActALEC WatchBelum ada peringkat
- Glossary of Health Insurance Terms: Benefits For Plan Years Beginning After Sept. 23, 2010Dokumen5 halamanGlossary of Health Insurance Terms: Benefits For Plan Years Beginning After Sept. 23, 2010api-27631527Belum ada peringkat
- 11-08-09 Physician Employment AgreementDokumen21 halaman11-08-09 Physician Employment AgreementTariq Niaz Ahmad, MD100% (1)
- Arrafmap-Factsheet Final 508Dokumen11 halamanArrafmap-Factsheet Final 508New York SenateBelum ada peringkat
- Survivor ShipDokumen31 halamanSurvivor Shipxxjulyxx87Belum ada peringkat
- CST WordDokumen42 halamanCST WordKISHORE STUDIOS OFFICIALBelum ada peringkat
- Maryland Health Care Reform PlanDokumen7 halamanMaryland Health Care Reform PlanEddie O'BrienBelum ada peringkat
- Charter - Health Plan Annual Notice Booklet 2023 - FinalDokumen20 halamanCharter - Health Plan Annual Notice Booklet 2023 - FinalKelle SuttonBelum ada peringkat
- For QuizBEE ReviewerDokumen12 halamanFor QuizBEE ReviewerLeah Moyao-DonatoBelum ada peringkat
- Standard Policy Provisions: 1. DefinitionsDokumen4 halamanStandard Policy Provisions: 1. DefinitionsskvskvskvskvBelum ada peringkat
- Standard Policy Provisions for Aegon Life iTerm PlanDokumen4 halamanStandard Policy Provisions for Aegon Life iTerm PlanskvskvskvskvBelum ada peringkat
- Public Act 095-0958: Previous General AssembliesDokumen6 halamanPublic Act 095-0958: Previous General AssembliesEd ScanlonBelum ada peringkat
- New India Sixty Plus Mediclaim Policy Highlights in 35 CharactersDokumen17 halamanNew India Sixty Plus Mediclaim Policy Highlights in 35 Charactersvishal shahBelum ada peringkat
- 87226TX006Dokumen118 halaman87226TX006James delgadoBelum ada peringkat
- Portability Law SummaryDokumen29 halamanPortability Law SummaryElvin Nobleza PalaoBelum ada peringkat
- Local GW Group Life Terms and Conditions July 09Dokumen3 halamanLocal GW Group Life Terms and Conditions July 09McDonald Bucca TafirenyikaBelum ada peringkat
- Certificate of Prior Health CoverageDokumen2 halamanCertificate of Prior Health CoverageElias EgoziBelum ada peringkat
- PORTABILITY LAW - OdtDokumen1 halamanPORTABILITY LAW - OdtKla AlvarezBelum ada peringkat
- Motion Picture Health Plan Appeals - NoticeDokumen6 halamanMotion Picture Health Plan Appeals - Noticeravip3366Belum ada peringkat
- Key Features of The Affordable Care Act by YearDokumen8 halamanKey Features of The Affordable Care Act by YearGabriel NguyenBelum ada peringkat
- General Insurance Policy SummaryDokumen9 halamanGeneral Insurance Policy SummarysriheroBelum ada peringkat
- Health Care Reform Act: Critical Tax and Insurance RamificationsDari EverandHealth Care Reform Act: Critical Tax and Insurance RamificationsBelum ada peringkat
- Solids Level Measurement Application Guide en 78224 PDFDokumen144 halamanSolids Level Measurement Application Guide en 78224 PDFwalcalBelum ada peringkat
- Roadblocks Overcome Cruise PurchaseTITLE Top 15 Cruise Hesitations Answered TITLE How to Convince People Cruises Worth CostDokumen4 halamanRoadblocks Overcome Cruise PurchaseTITLE Top 15 Cruise Hesitations Answered TITLE How to Convince People Cruises Worth CostJanel Castillo Balbiran33% (3)
- 2 English Course BDokumen8 halaman2 English Course BAnjana27Belum ada peringkat
- Jounce Therapeutics Company Events and Start DatesDokumen48 halamanJounce Therapeutics Company Events and Start DatesEquity NestBelum ada peringkat
- LH 11 180 190 220 230 270 280 390 400 Breaker Safety & Operating InstructionsDokumen304 halamanLH 11 180 190 220 230 270 280 390 400 Breaker Safety & Operating InstructionshadensandorBelum ada peringkat
- Vaginal Examinations in Labour GuidelineDokumen2 halamanVaginal Examinations in Labour GuidelinePooneethawathi Santran100% (1)
- Chennai's 9 sewage treatment plants process 486 MLDDokumen5 halamanChennai's 9 sewage treatment plants process 486 MLDmoni_john_1Belum ada peringkat
- Failures of Gabion Walls: Ganesh C. Chikute, Ishwar P. SonarDokumen7 halamanFailures of Gabion Walls: Ganesh C. Chikute, Ishwar P. SonarnavigareeBelum ada peringkat
- Schneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFDokumen3 halamanSchneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFAnonymous dH3DIEtzBelum ada peringkat
- Heat Exchanger Sodium SilicateDokumen2 halamanHeat Exchanger Sodium SilicateChristopher BrownBelum ada peringkat
- Junayed - 19 39800 1Dokumen11 halamanJunayed - 19 39800 1gurujeeBelum ada peringkat
- FB77 Fish HatcheriesDokumen6 halamanFB77 Fish HatcheriesFlorida Fish and Wildlife Conservation CommissionBelum ada peringkat
- Funds Flow Statement ExplainedDokumen76 halamanFunds Flow Statement Explainedthella deva prasad0% (1)
- Critical Criminal Justice IssuesDokumen132 halamanCritical Criminal Justice IssuesAnnamarella Amurao CardinezBelum ada peringkat
- Reach Out and Read Georgia Selected For AJC Peachtree Road Race Charity Partner ProgramDokumen2 halamanReach Out and Read Georgia Selected For AJC Peachtree Road Race Charity Partner ProgramPR.comBelum ada peringkat
- Universal Basic IncomeDokumen31 halamanUniversal Basic IncomeumairahmedbaigBelum ada peringkat
- Impact of Energy Consumption On The EnvironmentDokumen9 halamanImpact of Energy Consumption On The Environmentadawiyah sofiBelum ada peringkat
- Medpet Pigeon ProductsDokumen54 halamanMedpet Pigeon ProductsJay Casem67% (3)
- Aço X6NiCrTiMoVB25!15!2 - 1.4980 Austenitic SteelDokumen2 halamanAço X6NiCrTiMoVB25!15!2 - 1.4980 Austenitic SteelMoacir MachadoBelum ada peringkat