Lecture 2
Diunggah oleh
InactiveAccountDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Lecture 2
Diunggah oleh
InactiveAccountHak Cipta:
Format Tersedia
Lecture 2 Assignment-Textbook Chapter 14 (Blood)
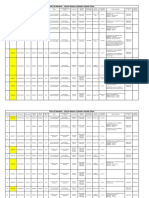
Chapter Assessments (p.5550-551) 14.1 Introduction 1. Major functions of blood include d. a. Nutrient, hormone, oxygen, and waste transport b. Helping maintain stability of interstitial fluid c. Heat distribution d. All of the above 2. Formed elements in blood are red blood cells, white blood cells, and platelets. 3. Define hematocrit, and explain how it is determined. (523) hematocrit: the percentage by volume of red blood cells in a sample of whole blood. If a blood-filled capillary tube is centrifuged, the red cells pack in the lower portion and the percentage of red cells (hematocrit) can be determined. 4. The liquid portion of the blood is called plasma. 14.2 Blood Cells 6. Describe a red blood cell. Biconcave discs with shapes that provide increased surface area and place their cell membranes close to internal structures. RBCs contain hemoglobin, which combines loosely with oxygen. The mature form lacks nuclei and other organelles, but contains enzymes needed for energy-releasing processes. 7. Contrast oxyhemoglobin and deoxyhemoglobin. When hemoglobin combines with oxygen, the resulting oxyhemoglobin is bright red; when the oxygen is released, the resulting deoxyhemoglobin is darker. Blood rich in deoxyhemoglobin may appear bluish when it is viewed through blood vessel walls. 8. Explain the significance of red blood cell counts. Red blood cell count is related to the oxygencarrying capacity of the blood and is used in diagnosing and evaluating the courses of diseases. 10. Define erythropoietin, and explain its function. Its a kidney hormone that promotes red blood cell formation; EPO. A negative feedback mechanism involving erythropoietin from the kidneys and liver controls rate of RBC production. Erythropoietin is released in response to low oxygen levels. 11. Explain how vitamin B12 and folic acid deficiencies affect RBC production. These vitamins are required for DNA synthesis, so they are necessary for the growth and division of all cells. Cell division is rapid in hematopoietic tissue, so this tissue is especially vulnerable to deficiency of either of these vitamins. 12. List two sources of iron that can be used for the synthesis of hemoglobin. Absorbed from small intestine; conserved during RBC destruction and made available for reuse. 13. Distinguish between biliverdin and bilirubin. They are pigments, released from the heme portion, excreted in bile; pigments produced from hemoglobin breakdown. Biliverdin becomes a greenish pigment when heme further decomposes into iron and when its converted to an orange pigment, its called bilirubin.
Lecture 2 Assignment-Textbook Chapter 14 (Blood)
14. Distinguish between granulocytes and agranulocytes. Granulocytes are leukocytes with granular cytoplasm. They include neutrophils, eosinophils, and basophils. Those without cytoplasmic granules are called agranulocytes and includes monocytes and lymphocytes. 15. Name five types of leukocytes, and list the major functions of each type. Component Function Neutrophil Phagocytizes small particles Eosinophil Kills parasites and moderates allergic reactions Basophil Releases heparin and histamine Monocyte Phagocytizes large particles Lymphocyte Helps control blood loss from broken vessels 16. Explain the significance of WBC counts as aids to diagnosing diseases. The number of WBCs may change in abnormal conditions such as infections, emotional disturbances, or excessive loss of body fluids. 17. Blood platelets are fragments of megakaryocytes that function in red bone marrow. 14.3 Blood Plasma 18. The most abundant component of plasma is d. water. 19. Name three types of plasma proteins, and indicate the function of each type. Albumins Help maintain the osmotic pressure of plasma Globulins Provide immunity (antibodies) and transport lipids and fat-soluble vitamins Fibrinogen Functions in blood clotting 20. Name the gases and nutrients in plasma.
gases
nutrients
oxygen
simple sugars
carbon dioxide
amino acids
nitrogen
lipids
22. The most abundant plasma electrolytes are sodium and chloride.
Lecture 2 Assignment-Textbook Chapter 14 (Blood)
23. Name several plasma electrolytes. They include ions of sodium, potassium, calcium, magnesium, chloride, bicarbonate, phosphate, and sulfate. 14.4 Homostasis 24. Homostasis is the term for stoppage of bleeding. 25. Explain how blood vessel spasm is stimulated following an injury. Smooth muscles in the walls of smaller blood vessels reflexly contracts following injury. Platelets release serotonin that stimulates vasoconstriction and helps maintain blood vessel spasm. 26. Platelets adhering to form a plug may control blood loss from a small break, but a larger break may require a blood clot to halt bleeding. 27. Name a vitamin required for blood clotting. Vitamin K 28. Distinguish between fibrinogen and fibrin. Fibrin is insoluble, fibrous protein formed from fibrinogen during blood coagulation. Fibrinogen is plasma protein converted into fibrin during blood coagulation. 29. Describe the major steps leading to the formation of a blood clot.
platelets adhere to each other, to end of broken vessel, and to exposed collagen
break in vessel wall
blood escaping through break
platelets plug helps control blood loss
31. Describe a positive feedback system that operates during blood clotting. Once a blood clot begins to form, it promotes additional clotting, because thrombin also acts directly on blood clotting factors other than fibrinogen, causing prothrombin to form still more thrombin. 32. Define serum. Fluid portion of coagulated blood. Its essentially plasma minus all of its fibrinogen and most other clotting factors. 33. Distinguish between a thrombus and an embolus. A thrombus is a blood clot abnormally forming in a vessel. An embolus is a clot that dislodges, or a fragment of a clot that breaks loose and is carried away by the flow of blood. 34. Explain how a blood clot may be removed naturally from a blood vessel. Platelets associated with a blood clot also release platelet-derived growth factor (PDGF), which stimulates smooth muscle cells and fibroblasts to repair damaged blood vessel walls. Fibroblasts invade a clot, forming CT throughout. Protein-splitting enzymes may eventually destroy a clot. 35. Describe how blood coagulation may be prevented. The smooth inner lining of blood vessels discourages the accumulation of platelets. As a clot forms, fibrin adsorbs thrombin and prevents the reaction from spreading. Antithrombin interferes with the action of excess thrombin. Some cells secrete heparin, an anticoagulant.
Lecture 2 Assignment-Textbook Chapter 14 (Blood)
14.5 Blood Groups and Transfusions 36. Distinguish between an antigen and an antibody. Antigens are chemical that stimulates B lymphocytes to produce antibodies. Antibodies are proteins (immunoglobulin) that B cells of the immune system produce in response to a nonself antigen; it reacts with antigen. 37. Explain the basis of ABO blood types. Its based on the presence (or ansence) of two major antigens on RBC membranes-antigen A and antigen B. 38. Indicate the blood type (both ABO and Rh) of the individual: A, Rh-positive 39. What blood type(s) could safely receive blood from this individual (#38)? A, Rh positive and AB, Rh positive 40. What blood type(s) could this individual (#38) safely receive? A Rh-positive A Rh-negative O Rh negative [packed cells] O Rh positive [packed cells] 41. Explain why a person with blood type AB is sometimes called a universal recipient. AB individuals can receive blood of any type because they lack anti-A and anti-B antibodies. 42. Explain why a person with blood type O is sometimes called a universal donor. Type O blood lacks antigens A and B. This type could be transfused into persons with blood of any other type. 43. Distinguish between Rh-positive and Rh-negative blood. Rh antigens are present on the RBC membranes of Rh positive blood; they are absent in Rh negative blood. 44. Describe how a person may become sensitized to Rh-positive blood. By receiving a transfusion. 45. Describe erythroblastosis fetalis, and explain how this condition may develop. The hemolytic disease of the newborn. If a woman who has already developed anti-Rh antibodies becomes pregnant with a second Rh-positive fetus, these anti-Rh antibodies, called hemolysins, cross the placental membrane and destroy the fetal red cells. Critical Thinking (p.551) 2. Erythropoietin is available as a drug. Why would athletes abuse it? EPO increases the carrying capacity of oxygen in the blood, thereby increasing the stamina of the athlete. 4. How would you explain to a patient with leukemia, who has a greatly elevated WBC count, the importance of avoiding bacterial infections? In leukemia, the WBC formed are immature and remain undifferentiated. They have no or little ability to phagocytize bacteria or produce antibodies to combat infection. 5. Hypochromic (iron-deficiency) anemia is common among aging persons admitted to hospitals for other conditions. What environmental and sociological factors might promote this type form of anemia? Not being financially stable as in food being too expensive (meat, seafood and vegetables are high in iron but cost too much). Lack of mobility, to go one place to another and lack of dentures.
Lecture 2 Assignment-Textbook Chapter 14 (Blood)
6. Why do patients with liver diseases commonly develop blood clotting problems? Because its the liver that manufactures the clotting factors.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- всё необходимое для изучения английского языкаDokumen9 halamanвсё необходимое для изучения английского языкаNikita Chernyak100% (1)
- Unit 1 EssayDokumen5 halamanUnit 1 EssayInactiveAccountBelum ada peringkat
- MYCAA Spouse Education and Training PlanDokumen3 halamanMYCAA Spouse Education and Training PlanInactiveAccountBelum ada peringkat
- Med-Surg II Pretest Keywords and ComplicationsDokumen4 halamanMed-Surg II Pretest Keywords and ComplicationsInactiveAccountBelum ada peringkat
- Vocab1 4Dokumen14 halamanVocab1 4InactiveAccountBelum ada peringkat
- Lecture 9Dokumen4 halamanLecture 9InactiveAccountBelum ada peringkat
- Soci1306 Exam 2Dokumen15 halamanSoci1306 Exam 2InactiveAccountBelum ada peringkat
- TN16 18Dokumen17 halamanTN16 18InactiveAccountBelum ada peringkat
- Terminology Notebook-Ch. 22-24: Chapter 22 Reproductive Systems Understanding Words p830 Andr-Contra - CrurDokumen15 halamanTerminology Notebook-Ch. 22-24: Chapter 22 Reproductive Systems Understanding Words p830 Andr-Contra - CrurInactiveAccountBelum ada peringkat
- Terminology Notebook-Ch. 19-21: Chapter 19 Respiratory System Understanding Words p735Dokumen10 halamanTerminology Notebook-Ch. 19-21: Chapter 19 Respiratory System Understanding Words p735InactiveAccountBelum ada peringkat
- PretestDokumen9 halamanPretestInactiveAccountBelum ada peringkat
- Study Guide 9-12Dokumen7 halamanStudy Guide 9-12InactiveAccountBelum ada peringkat
- Lecture 8Dokumen4 halamanLecture 8InactiveAccountBelum ada peringkat
- TN1Dokumen13 halamanTN1InactiveAccountBelum ada peringkat
- Socio 1306 Exam 1Dokumen28 halamanSocio 1306 Exam 1InactiveAccountBelum ada peringkat
- Prefix ExamDokumen8 halamanPrefix ExamInactiveAccountBelum ada peringkat
- Nature NurtureDokumen1 halamanNature NurtureInactiveAccountBelum ada peringkat
- Lecture 4Dokumen4 halamanLecture 4InactiveAccountBelum ada peringkat
- Lecture 7Dokumen4 halamanLecture 7InactiveAccountBelum ada peringkat
- Lecture 5Dokumen3 halamanLecture 5InactiveAccountBelum ada peringkat
- Lecture 12Dokumen3 halamanLecture 12InactiveAccountBelum ada peringkat
- Mycaa Educ Plan SampleDokumen5 halamanMycaa Educ Plan SampleInactiveAccountBelum ada peringkat
- Lecture 6Dokumen4 halamanLecture 6InactiveAccountBelum ada peringkat
- Lecture 10Dokumen3 halamanLecture 10InactiveAccountBelum ada peringkat
- Lecture 1Dokumen7 halamanLecture 1InactiveAccountBelum ada peringkat
- Lecture 3Dokumen4 halamanLecture 3InactiveAccountBelum ada peringkat
- Lecture 11Dokumen2 halamanLecture 11InactiveAccountBelum ada peringkat
- Lab 8Dokumen15 halamanLab 8InactiveAccountBelum ada peringkat
- Lab 5Dokumen15 halamanLab 5InactiveAccountBelum ada peringkat
- Lab 7Dokumen6 halamanLab 7InactiveAccountBelum ada peringkat
- Contact and Profile of Anam ShahidDokumen1 halamanContact and Profile of Anam ShahidSchengen Travel & TourismBelum ada peringkat
- PLC Networking with Profibus and TCP/IP for Industrial ControlDokumen12 halamanPLC Networking with Profibus and TCP/IP for Industrial Controltolasa lamessaBelum ada peringkat
- Oracle Learning ManagementDokumen168 halamanOracle Learning ManagementAbhishek Singh TomarBelum ada peringkat
- Ancient Greek Divination by Birthmarks and MolesDokumen8 halamanAncient Greek Divination by Birthmarks and MolessheaniBelum ada peringkat
- Evaluating Sources IB Style: Social 20ib Opvl NotesDokumen7 halamanEvaluating Sources IB Style: Social 20ib Opvl NotesRobert ZhangBelum ada peringkat
- Annamalai International Journal of Business Studies and Research AijbsrDokumen2 halamanAnnamalai International Journal of Business Studies and Research AijbsrNisha NishaBelum ada peringkat
- Good Ethics Is Good BusinessDokumen9 halamanGood Ethics Is Good BusinesssumeetpatnaikBelum ada peringkat
- On The Behavior of Gravitational Force at Small ScalesDokumen6 halamanOn The Behavior of Gravitational Force at Small ScalesMassimiliano VellaBelum ada peringkat
- Pradhan Mantri Gramin Digital Saksharta Abhiyan (PMGDISHA) Digital Literacy Programme For Rural CitizensDokumen2 halamanPradhan Mantri Gramin Digital Saksharta Abhiyan (PMGDISHA) Digital Literacy Programme For Rural Citizenssairam namakkalBelum ada peringkat
- Wasserman Chest 1997Dokumen13 halamanWasserman Chest 1997Filip BreskvarBelum ada peringkat
- Multiple Choice: CH142 Sample Exam 2 QuestionsDokumen12 halamanMultiple Choice: CH142 Sample Exam 2 QuestionsRiky GunawanBelum ada peringkat
- CMC Ready ReckonerxlsxDokumen3 halamanCMC Ready ReckonerxlsxShalaniBelum ada peringkat
- Case StudyDokumen2 halamanCase StudyBunga Larangan73% (11)
- Final Thesis Report YacobDokumen114 halamanFinal Thesis Report YacobAddis GetahunBelum ada peringkat
- 2010 - Impact of Open Spaces On Health & WellbeingDokumen24 halaman2010 - Impact of Open Spaces On Health & WellbeingmonsBelum ada peringkat
- Main Research PaperDokumen11 halamanMain Research PaperBharat DedhiaBelum ada peringkat
- PESO Online Explosives-Returns SystemDokumen1 halamanPESO Online Explosives-Returns Systemgirinandini0% (1)
- LM1011 Global ReverseLogDokumen4 halamanLM1011 Global ReverseLogJustinus HerdianBelum ada peringkat
- Dole-Oshc Tower Crane Inspection ReportDokumen6 halamanDole-Oshc Tower Crane Inspection ReportDaryl HernandezBelum ada peringkat
- April 26, 2019 Strathmore TimesDokumen16 halamanApril 26, 2019 Strathmore TimesStrathmore Times100% (1)
- Attributes and DialogsDokumen29 halamanAttributes and DialogsErdenegombo MunkhbaatarBelum ada peringkat
- Clark DietrichDokumen110 halamanClark Dietrichikirby77Belum ada peringkat
- CIT 3150 Computer Systems ArchitectureDokumen3 halamanCIT 3150 Computer Systems ArchitectureMatheen TabidBelum ada peringkat
- Requesting A Query in Zemanta Using PHPDokumen10 halamanRequesting A Query in Zemanta Using PHPAther SajjadBelum ada peringkat
- Sewage Pumping StationDokumen35 halamanSewage Pumping StationOrchie DavidBelum ada peringkat
- Resume Template & Cover Letter Bu YoDokumen4 halamanResume Template & Cover Letter Bu YoRifqi MuttaqinBelum ada peringkat
- Os PPT-1Dokumen12 halamanOs PPT-1Dhanush MudigereBelum ada peringkat
- PROF ED 10-ACTIVITY #1 (Chapter 1)Dokumen4 halamanPROF ED 10-ACTIVITY #1 (Chapter 1)Nizelle Arevalo100% (1)
- Riddles For KidsDokumen15 halamanRiddles For KidsAmin Reza100% (8)