Gestational Hypertension
Diunggah oleh
Jason Jimmy Lee PillayDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Gestational Hypertension
Diunggah oleh
Jason Jimmy Lee PillayHak Cipta:
Format Tersedia
Gestational hypertension
Defined as a sustained of blood pressure to 140/90 mmHg or more on at least two occasion 4 or more hours apart beyond the 20th week of pregnancy or during the first 24 hours after delivery in a previously normotensive woman Associated with higher risk for pre-eclampsia hypertensive disorders in pregnancy are among the leading causes of maternal mortality, along with thromboembolism, hemorrhage and nonobstetric injuries. Between 1991 and 1999, pregnancy-induced hypertension caused 15.7% of maternal deaths in the United States Criteria o Absence of evidence of underlying cause of hypertension o Unassociated with other evidence of preeclampsia o Not associated with hemoconcentration ,thrombocytopenia, raised uric acid level
To confirm diagnosis do a glucose challenge : pt is given 50g of glucose then after 1 h we ,measure the concentration : if >140 mg/dl we do a oral 3h glucose test but if < 140 mg/dl its normal
Essential hypertension in pregnancy Its also a common disorder in pregnancy Criteria of diagnosis o Rise of blood pressure to 140/90mmHg or more prior to 20 weeks of pregnancy o Cardiac enlargement on ECG o Medical disorder present This kind of hypertension can lead to chronic placental insufficiency that leads to retarded fetus , when blood pressure exceeds 160/100mmHg the perinatal loss doubles and may complicate with pre-eclampsia Management o Aim of treatment : stabilize blood pressure below 160/100mmHg, prevent superimposition of pre-eclampsia, monitor the maternal and fetal well being o Antihypertensive drugs given but with care to avoid placental insufficiency . o If hypertension is uncontrollable pregnancy is continued till 37 weeks and induction of labour is made
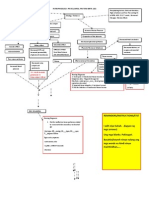
Differential diagnosis
Pre-eclampsia Primigravida After 20 weeks of pregnancy Proteinuria None Thromobocytopenia Pre-eclampsia Pre-pregnant hypertension Essential hypertension Multipara Before 20 weeks of pregnancy Negative findings Silver wiring , hypertensive retinopathy Chronic nephritis Variable Presence of cast and albumin with low specific gravity Albuminuric retinopathy , cotton wool patches & flame hemorrhages High urea & creatinine History of lesion on renal
Parity Onset of hypertension Urine Eye changes Specific blood values Past history
Eclampsia Eclampsia, which is considered a complication of severe preeclampsia, is commonly defined as new onset of grand mal seizure activity and/or unexplained coma during pregnancy or postpartum in a woman with signs or symptoms of preeclampsia It typically occurs during or after the 20th week of gestation or in the postpartum period. Nonetheless, eclampsia in the absence of hypertension with proteinuria has been demonstrated to occur in 38% of cases reported in the United Kingdom. Similarly, hypertension was absent in 16% of cases reviewed in the United States. The clinical manifestations of maternal preeclampsia are hypertension and proteinuria with or without coexisting systemic abnormalities involving the kidneys, liver, or blood. There is also a fetal manifestation of preeclampsia involving fetal growth restriction, reduced amniotic fluid, and abnormal fetal oxygenation. HELLP syndrome is a severe form of preeclampsia and involves hemolytic anemia, elevated liver function tests (LFTs), and low platelet count. Most cases of eclampsia present in the third trimester of pregnancy, with about 80% of eclamptic seizures occurring intrapartum or within the first 48 hours following delivery. Rare cases have been reported before 20 weeks' gestation or as late as 23 days postpartum. Other than early detection of preeclampsia, no reliable test or symptom complex predicts the development of eclampsia. Course of eclamptic seizures o Eclampsia manifests as 1 seizure or more, with each seizure generally lasting 6075 seconds. The patients face initially may become distorted, with protrusion of the eyes, and foaming at the mouth may occur. Respiration ceases for the duration of the seizure. o Eclamptic seizures may be divided into 2 phases. Phase 1 lasts 15-20 seconds and begins with facial twitching. The body becomes rigid, leading to generalized muscular contractions. o Phase 2 lasts about 60 seconds. It starts in the jaw, moves to the muscles of the face and eyelids, and then spreads throughout the body. The muscles begin alternating between contracting and relaxing in rapid sequence. o A coma or period of unconsciousness, lasting for a variable period, follows phase 2. After the coma phase, the patient may regain some consciousness, and she may become combative and very agitated. However, the patient will have no recollection of the seizure.
o A period of hyperventilation occurs after the tonic-clonic seizure. This compensates for the respiratory and lactic acidosis that develops during the apneic phase. Pathophysiology of Eclampsia o Inhibition of uterovascular development Many uterovascular changes occur when a woman is pregnant. It is believed that these changes are due to the interaction between fetal and maternal allografts and result in systemic and local vascular changes. It has been shown that in patients with eclampsia, the development of uteroplacental arteries is hindered. o Hindrance of cerebral blood flow regulation It is believed that in eclampsia there is abnormal cerebral blood flow in the setting of extreme hypertension. The regulation of cerebral perfusion is inhibited, vessels become dilated with increased permeability, and cerebral edema occurs, resulting in ischemia and encephalopathy. In extreme hypertension, normal compensatory vasoconstriction may become defective.
o Endothelial dysfunction Factors associated with endothelial dysfunction have been shown to be increased in the systemic circulation of women suffering from eclampsia. These include the following
Cellular fibronectin Von Willebrand factor Cell adhesion molecules (ie, P-selectin, vascular endothelial adhesion molecule-1 [VCAM-1] Intercellular adhesion molecule-1 [ICAM-1]) Cytokines (ie, interleukin-6 [IL-6]) Tumor necrosis factor- [TNF-] o In addition, it is believed that antiangiogenic factors, such as placental protein fms-like tyrosine kinase 1 (sFlt-1) and activin A, antagonize vascular endothelial growth factor (VEGF). Elevated levels of these proteins cause a reduction of VEGF and induce systemic and local endothelial cell dysfunction. Clinical picture o Eclampsia convulsion is divided to 4 stage Premonitory stage : pt is unconscious with twitching of muscle of face ,limbs, this stage last for 30 sec Tonic stage : body goes into tonic spasm , respiration cease and tongue protrude between teeth , stage last for 30 sec Clonic stage : all voluntary muscle contract and relax , tongue bitting may occur, stage last for 1-4 min Coma
If the fits are multiple, occurring at varying interval it is calles status eclampticus Complication of maternal o Tongue injuries o Edema o Pneumonia
o Embolism o Left ventricular failure o Renal failure o DVT o Shock , sepsis, psychosis Management o General First aid Oxygen administration Hemodynamic stabilization Arrest convulsion o Specific Anticonvulsant and sedative regime MgSO4 Antihypertensive drugs : hydralzine, labetalol ,CCB Status eclampticus : thiopentone 2.0g in 20ml of 5% dextrose IV
Fits controlled Baby mature : o Termination of pregnancy should be done if cervix favourable and there is no contradication of vaginal delivery o Oxytoxin drip may achieved o If cervix unfavourable C-section is prefer Baby premature o Drag pregnancy till 37 week , fetal monitored constantly
Fits uncontrolled Termination of pregnancy Assess the responds to have delivery , c-section if unfavourable
Chronic hypertension
Defined as presence of hypertension of any cause antedating or before 20th weeks of pregnancy and its presence beyond 42 days after delivery Chronic hypertension is a primary disorder in 90-95% of cases and may be either essential (90%) or secondary to some identifiable underlying disorder, such as renal parenchymal disease (eg, polycystic kidneys, glomerular or interstitial disease), renal vascular disease (eg, renal artery stenosis, fibromuscular dysplasia), endocrine disorders (eg, adrenocorticosteroid or mineralocorticoid excess, pheochromocytoma, hyperthyroidism or hypothyroidism, growth hormone excess, hyperparathyroidism), coarctation of the aorta, or oral contraceptive use. About 20-25% of women with chronic hypertension develop preeclampsia during pregnancy.
Chronic hypertension occurs in up to 22% of women of childbearing age, with the prevalence varying according to age, race, and body mass index (BMI). Population-based data indicate that approximately 1% of pregnancies are complicated by chronic hypertension, 5-6% by gestational hypertension (without proteinuria), and 1-2% by preeclampsia. Risk o Age > 40 o Duration of hypertension >15 years o Level of BP >160/110mmHg o Presence of any medical disorder o Presence of thrombophillia
Anda mungkin juga menyukai
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- EclampsiaDokumen47 halamanEclampsiarranindyaprabasaryBelum ada peringkat
- Gestational HypertensionDokumen6 halamanGestational HypertensionDimitrisSoulisBelum ada peringkat
- Gestational HypertensionDokumen72 halamanGestational HypertensionYn El100% (1)
- Neonatal Jaundice: Zilpa, AMODokumen44 halamanNeonatal Jaundice: Zilpa, AMOmarco luenaBelum ada peringkat
- Post Abortion CareDokumen35 halamanPost Abortion CareNatukunda DianahBelum ada peringkat
- Puerperium:: Psychological DisordersDokumen5 halamanPuerperium:: Psychological DisordersManisha ThakurBelum ada peringkat
- Prenatal Substance Dependence AbuseDokumen13 halamanPrenatal Substance Dependence Abusenursereview100% (2)
- PROM Care PlanDokumen2 halamanPROM Care PlanMariagmzBelum ada peringkat
- Meconium Aspiration Syndrome (MAS)Dokumen12 halamanMeconium Aspiration Syndrome (MAS)Angela AmaoBelum ada peringkat
- Birth Asphyxia: by Anne E. Odaro MCM/2017/69852Dokumen26 halamanBirth Asphyxia: by Anne E. Odaro MCM/2017/69852ElvisBelum ada peringkat
- Incompetent CervixDokumen29 halamanIncompetent CervixCyrelle Jen TorresBelum ada peringkat
- Pregnancy Induced HypertensionDokumen52 halamanPregnancy Induced HypertensionJoy GloryBelum ada peringkat
- Uterine ProlapseDokumen11 halamanUterine ProlapseMelDred Cajes BolandoBelum ada peringkat
- Pathophysiology of PihDokumen3 halamanPathophysiology of PihMargueretti Delos ReyesBelum ada peringkat
- Postpartum HemorrhageDokumen2 halamanPostpartum HemorrhageAr'nyj Pabualan ZaballeroBelum ada peringkat
- Pre EclampsiaDokumen8 halamanPre EclampsiaJamie Agbannawag100% (1)
- Ectopic Pregnancy - OMDokumen9 halamanEctopic Pregnancy - OMrheindBelum ada peringkat
- Convulsive Disorders in ChildrenDokumen44 halamanConvulsive Disorders in ChildrenMurugesanBelum ada peringkat
- IUFDDokumen2 halamanIUFDnurseon0% (1)
- DEFINITION: Abortion Is The Expulsion or Extraction From Its MotherDokumen10 halamanDEFINITION: Abortion Is The Expulsion or Extraction From Its MothermOHAN.SBelum ada peringkat
- Hyperemesis GravidarumDokumen36 halamanHyperemesis GravidarumjanissBelum ada peringkat
- Ectopic PregnancyDokumen4 halamanEctopic PregnancyJovie Anne BorjaBelum ada peringkat
- Shoulder DystociaDokumen22 halamanShoulder Dystociaamulan_aBelum ada peringkat
- EpisiotomyDokumen18 halamanEpisiotomyAnnapurna DangetiBelum ada peringkat
- Abnormal Progress in Labor (Precipitous Labor and Birth & Retraction Rings)Dokumen34 halamanAbnormal Progress in Labor (Precipitous Labor and Birth & Retraction Rings)Ana100% (3)
- Incompetent CervixDokumen5 halamanIncompetent CervixNaidin Catherine De Guzman-Alcala100% (1)
- Nursing Care of The High Risk NewbornDokumen7 halamanNursing Care of The High Risk NewbornAbigail MangaoangBelum ada peringkat
- Nursing Care Plan For HysterectomyDokumen17 halamanNursing Care Plan For HysterectomySuresh kumarBelum ada peringkat
- Abruptio PlacentaDokumen60 halamanAbruptio PlacentaSindhu JojoBelum ada peringkat
- Neonatal Hypoglycemia APNECDokumen26 halamanNeonatal Hypoglycemia APNECyumicheongBelum ada peringkat
- Case Study Missed Miscarriage Dilation and CurettageDokumen48 halamanCase Study Missed Miscarriage Dilation and CurettageEsther Ellise AbundoBelum ada peringkat
- Placenta Abruptio: Maneja, Jan Michael B. BSN 223Dokumen6 halamanPlacenta Abruptio: Maneja, Jan Michael B. BSN 223JiraGonzales100% (1)
- Hyperemesis GravidarumDokumen31 halamanHyperemesis GravidarumFeregrine VerayoBelum ada peringkat
- Heart Disease in PregnancyDokumen5 halamanHeart Disease in PregnancyAngeliqueBelum ada peringkat
- Mechanism of LaborDokumen12 halamanMechanism of LaborSaidatul Safarah Md HassanBelum ada peringkat
- Abnormal Uterine BleedingDokumen19 halamanAbnormal Uterine BleedingDelphy Varghese100% (1)
- Case StudyDokumen5 halamanCase StudyJui Perano100% (2)
- The Incompetent Cervix 2Dokumen30 halamanThe Incompetent Cervix 2api-3705046100% (3)
- Case Presentation Hyperemesis Gravidarum Maricar Abonado Midwifery IIDokumen27 halamanCase Presentation Hyperemesis Gravidarum Maricar Abonado Midwifery IIMaricar Crescini AbonadoBelum ada peringkat
- Postpartal Diabetes MellitusDokumen7 halamanPostpartal Diabetes Mellitusnursereview100% (3)
- Neonatal SepsisDokumen44 halamanNeonatal SepsisIsabel Barredo Del MundoBelum ada peringkat
- PolyhydramniosDokumen2 halamanPolyhydramniosNathaniel RemandabanBelum ada peringkat
- Φ PathophysiologyDokumen4 halamanΦ PathophysiologyMariah AshooriyanBelum ada peringkat
- RH Incompatibility HandoutDokumen4 halamanRH Incompatibility HandoutMaricar Sanson FelicianoBelum ada peringkat
- Cervical Incompetence 1Dokumen5 halamanCervical Incompetence 1api-3705046100% (1)
- Hyperemesis GravidarumDokumen16 halamanHyperemesis GravidarumBabi PanggangBelum ada peringkat
- 1retinal DetachmentDokumen5 halaman1retinal Detachmentsunny_jr_Belum ada peringkat
- Puerperal SepsisDokumen4 halamanPuerperal SepsisSonali NayakBelum ada peringkat
- The PartographDokumen65 halamanThe PartographAmyAgustinBelum ada peringkat
- Prematurity and PostmaturityDokumen34 halamanPrematurity and PostmaturityAngelo MolinaBelum ada peringkat
- Polyhydraminos and OligohydraminosDokumen11 halamanPolyhydraminos and OligohydraminosMelissa Catherine ChinBelum ada peringkat
- Management Placenta PreviaDokumen24 halamanManagement Placenta PreviaMuhammad RifaldiBelum ada peringkat
- Assesment and Monitoring During 2nd Stage of LabourDokumen11 halamanAssesment and Monitoring During 2nd Stage of LabourPragati BholeBelum ada peringkat
- Unit I: Maternal and Child Health Nursing Practice 1Dokumen10 halamanUnit I: Maternal and Child Health Nursing Practice 1Gresha GamaBelum ada peringkat
- Care PlanDokumen4 halamanCare PlangopscharanBelum ada peringkat
- CPD, Dystocia, Fetal Distress OutputDokumen8 halamanCPD, Dystocia, Fetal Distress OutputJohn Dave AbranBelum ada peringkat
- Assessment in PregnancyDokumen15 halamanAssessment in PregnancyAna75% (4)
- Hypertension in PregnancyDokumen78 halamanHypertension in PregnancyNidhi PalBelum ada peringkat
- Hypertensive Disorders of Pregnancy PDFDokumen9 halamanHypertensive Disorders of Pregnancy PDFMohammed AbdBelum ada peringkat
- Role of Family Planning in Responsible Parent HoodDokumen40 halamanRole of Family Planning in Responsible Parent HoodJason Jimmy Lee PillayBelum ada peringkat
- Physical and Psychosocial Impacts of Pregnancy On Adolescents and Their Coping Strategies A Descriptive Study in Kuala Lumpur Malaysia PDFDokumen9 halamanPhysical and Psychosocial Impacts of Pregnancy On Adolescents and Their Coping Strategies A Descriptive Study in Kuala Lumpur Malaysia PDFJason Jimmy Lee PillayBelum ada peringkat
- Physical and Psychosocial Impacts of Pregnancy On Adolescents and Their Coping Strategies A Descriptive Study in Kuala Lumpur Malaysia PDFDokumen9 halamanPhysical and Psychosocial Impacts of Pregnancy On Adolescents and Their Coping Strategies A Descriptive Study in Kuala Lumpur Malaysia PDFJason Jimmy Lee PillayBelum ada peringkat
- Flow Chart For Suspected Ebola Patient To EdDokumen1 halamanFlow Chart For Suspected Ebola Patient To EdJason Jimmy Lee PillayBelum ada peringkat
- Upper GI BleedingDokumen10 halamanUpper GI BleedingJason Jimmy Lee PillayBelum ada peringkat
- Placenta CirculationDokumen11 halamanPlacenta CirculationJason Jimmy Lee PillayBelum ada peringkat
- Failure To Thrive With NotesDokumen45 halamanFailure To Thrive With NotesJason Jimmy Lee PillayBelum ada peringkat
- Syllabus - MBBSDokumen167 halamanSyllabus - MBBStariqayubBelum ada peringkat
- Smiley Face ChartDokumen2 halamanSmiley Face ChartJason Jimmy Lee PillayBelum ada peringkat
- ESL Text 1& 2Dokumen3 halamanESL Text 1& 2Jason Jimmy Lee PillayBelum ada peringkat
- Ventilation Cheat SheetDokumen1 halamanVentilation Cheat Sheetlizzy59683% (6)
- Diazoxide 50mg Tab DCC SummeryDokumen1 halamanDiazoxide 50mg Tab DCC SummeryarifpharmjuBelum ada peringkat
- Diabetic Emergencies PDFDokumen20 halamanDiabetic Emergencies PDFhenry leonardo gaona pinedaBelum ada peringkat
- Health Is WealthDokumen1 halamanHealth Is Wealthriana safrianiBelum ada peringkat
- DAFTAR PUSTAKA HydrocephalusDokumen2 halamanDAFTAR PUSTAKA HydrocephalusRahma darisBelum ada peringkat
- 559 FullDokumen12 halaman559 FullAmatystBelum ada peringkat
- Case Study Colorectal CancerDokumen23 halamanCase Study Colorectal CancerLeogalvez BedanoBelum ada peringkat
- Sesi 15-Making Your Hospital Baby FriendlyDokumen47 halamanSesi 15-Making Your Hospital Baby FriendlySiti HajarBelum ada peringkat
- Normal Puerperium PDFDokumen22 halamanNormal Puerperium PDFwawa3385100% (1)
- The History of PsychiatryDokumen12 halamanThe History of PsychiatryMarkoff Chaney100% (1)
- Dry Eye Disease After Refractive SurgeryDokumen6 halamanDry Eye Disease After Refractive SurgeryCastiglianoBelum ada peringkat
- Jameson Chassin-Operative StrategyDokumen566 halamanJameson Chassin-Operative StrategyMaria Alexandra100% (3)
- Endocrine SystemDokumen35 halamanEndocrine SystemLinkBelum ada peringkat
- MEAL (Psychiatric Nursing 2)Dokumen4 halamanMEAL (Psychiatric Nursing 2)Yucef Bahian-AbangBelum ada peringkat
- 1026 FullDokumen5 halaman1026 FullMuhammad Yufimar Rizza FadilahBelum ada peringkat
- Veneracion NCP 1Dokumen2 halamanVeneracion NCP 1Romm JacobBelum ada peringkat
- URiSCAN Optima - Operating Manual - ENGrev10Dokumen28 halamanURiSCAN Optima - Operating Manual - ENGrev10Jony MaiaBelum ada peringkat
- Bsped Dka Guidelines 2020Dokumen23 halamanBsped Dka Guidelines 2020drsaleemBelum ada peringkat
- Diarrhea in ChildrenDokumen42 halamanDiarrhea in ChildrenIPNATC NEPALBelum ada peringkat
- Tool For Bundling CalculationDokumen1 halamanTool For Bundling CalculationGladdy CabrezaBelum ada peringkat
- Project Biology 11Dokumen15 halamanProject Biology 11ABHISHEK SinghBelum ada peringkat
- VapingDokumen2 halamanVapingGlenn Maneja VillaBelum ada peringkat
- DR - Iniesta ReportDokumen97 halamanDR - Iniesta ReportRaceRadioBelum ada peringkat
- IDEXX CBC Chem ExplainedDokumen38 halamanIDEXX CBC Chem Explainedmmatthew74Belum ada peringkat
- Augmentin Tablet Pi Ipi13 SiDokumen11 halamanAugmentin Tablet Pi Ipi13 Siاسد راجBelum ada peringkat
- UNIT 4 and UNIT 5 ISDokumen9 halamanUNIT 4 and UNIT 5 ISMarinelle TumanguilBelum ada peringkat
- TMJ SlidesDokumen113 halamanTMJ SlidesRah Ma GhassanBelum ada peringkat
- U.S. Patent 9,301,519, Entitled, Systems and Methods For Ex Vivo Organ Care, To Hassanein Et Al., Issued Apr. 5, 2016.Dokumen106 halamanU.S. Patent 9,301,519, Entitled, Systems and Methods For Ex Vivo Organ Care, To Hassanein Et Al., Issued Apr. 5, 2016.Anonymous a7S1qyXBelum ada peringkat
- HbA1c OdtDokumen2 halamanHbA1c OdtAhmed AssafBelum ada peringkat
- Es I Algorithm PosterDokumen2 halamanEs I Algorithm Posterkusdiyah ningrumBelum ada peringkat