Complete%20 Drug%20 List
Diunggah oleh
Tr-I-LifeDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Complete%20 Drug%20 List
Diunggah oleh
Tr-I-LifeHak Cipta:
Format Tersedia
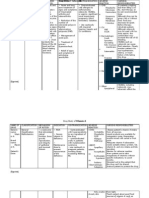
Medications (Include oxygen, IV fluids, saline flushes, and prn medications): Name: Dose, Route Drug Dosage Indications
for Use in Generic/Trade and Times Classification Calculations this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Abacavir/Ziagen
antiretrovirals nucleoside reverse transcriptase inhibitors
Abarelix/Plenaxis
antineoplastics gnrh antagonist
Abatacept/Orencia
antirheumatics fusion proteins
Abciximab/ReoPro
antiplatelet agents glycoprotein iib iiia inhibitors
Acamprosate calcium/ Campral
alcohol abuse therapy adjuncts gamma aminobutyric acid gaba analogues
Assess patient for signs of hypersensitivity reactions; change in severity of HIV symptoms and for symptoms of opportunistic infections throughout therapy. Observe patient for at least 30 min following injection for immediate-onset systemic allergic reactions. Measure serum total testosterone concentrations just prior to administration on Day 29. Assess range of motion, degree of swelling, pain in affected joints, infusionrelated reaction, signs of allergic reaction, latent tuberculosis with a tuberculin skin test, and health status at each session. Assess patient for bleeding at all potential bleeding sites; hypersensitivity reaction or anaphylaxis; mental status changes; nose and mouth mucous membranes, and examine urine, stool and emesis for presence of blood frequently throughout therapy. Check the sheath insertion site and distal pulses of affected leg(s) frequently while femoral artery sheath is in place and for 6 hr after femoral artery sheath is removed. Assess for signs of alcohol withdrawal at initiation of therapy.
headache, insomnia, MI, hepatotoxicity, diarrhea, nausea, vomiting, anorexia, rashes, lactic acidosis, hypersensitivity reactions
dizziness, fatigue, headache, sleep disturbances, peripheral edema, constipation, diarrhea, nausea, dysuria, urinary frequency, hot flushes, breast enlargement/nipple tenderness, back pain headache, dizziness, hypersensictivity reactions including anaphylaxis, infections, infusion-related events,
abnormal thinking, dizziness, headache, hypotension, atrial fibrillation/flutter, bradycardia, complete AV block, supraventricular tachycardia, vascular disorder, chest pain, peripheral edema, bleeding, thrombocytopenia, allergic reactions including anaphylaxis
abnormal thinking, anxiety, depression, drowsiness, headache, abnormal vision, cough, dyspnea, pharyngitis, rhinitis, palpitations, peripheral edema, syncope, vasodilation, abdominal pain, anorexia, constipation, diarrhea, flatulence, appetite, nausea, taste perversion, vomiting, libido,
1
Rev. 08/21/08
Acarbose/Precose
antidiabetics alpha glucosidase inhibitors
Acebutolol/ Sectral
antiarrhythmics (class II) antihypertensives beta blockers
Observe patient for signs and symptoms of hypoglycemia when taking concurrently with other oral hypoglycemic agents. Monitor blood pressure, ECG, and pulse; intake and output ratios and daily weights. Assess routinely for signs and symptoms of CHF.
erectile dysfunction, rash, weight gain, arthralgia, back pain, mylagia, tremor abdominal pain, diarrhea, flatulence, transaminases.
Acetaminophen/
antipyretics nonopioid analgesics
Acetazolamide/ AKZol, Dazamide, Diamox, Diamox Sequels, Storzolamide
anticonvulsants antiglaucoma agents diuretics ocular hypotensive agent carbonic anhydrase inhibitors
Acetohexamide/ Dymelor
antidiabetics sulfonylureas
Assess overall health status and alcohol usage before administering acetaminophen. Assess type, location, and intensity prior to and 3060 min following administration. Assess fever; note presence of associated signs. Assess for allergy to sulfonamides, eye discomfort or decrease in visual acuity, neurologic status, and decrease in severity of symptoms throughout prolonged therapy. Serum electrolytes, complete blood counts, and platelet counts should be evaluated initially. Observe patient for signs and symptoms of hypoglycemic reactions, and allergy to sulfonamides throughout therapy.
fatigue, weakness, anxiety, depression, dizziness, drowsiness, insomnia, memory loss, nervousness, nightmares, blurred vision, stuffy nose, bronchospasm, wheezing, bradycardia, CHF, pulmonary edema, hypotension, peripheral vasoconstriction, constipation, diarrhea, nausea, vomiting, erectile dysfunction, diminished libido, urinary frequency, rashes, hyperglycemia, hypoglycemia, arthralgia, joint pain, druginduced lupus syndrome. Hepatic renal failure, hepatotoxicity, renal failure, neutropenia, pancytopenia, leucopenia, rash, urticaria
Depression, tiredness, weakness, anorexia, metallic taste, nausea, StevensJohnson Syndrome, hyperchloremic acidosis, aplastic anemia, hemolytic anemia, leucopenia, weight loss, paresthesias, allergic reactions including anaphylaxis. Dizziness, headache, anorexia, cholestatic jaundice, constipation, diarrhea, epigastric fullness, heartburn, photosensitivity, hypoglycemia, aplastic anemia, agranulocytosis, hemolytic anemia, leukopenia, pancytopenia. Headache, anxiety, depression, malaise, nervousness, tremulousness, palpitations, superficial phlebitis of the lower
Acetohydroxamic acid/ AHA, Lithostat
anti-infectives (adjunct) urease inhibitors
Assess patient for signs and symptoms of urinary tract infection throughout therapy.
2
Rev. 08/21/08
Acetylcysteine/ Acetadote, Mucomyst, Mucosil
Antidotes (for acetaminophen toxicity) mucolytic
Acitretin/ Soriatane
antipsoriatics retinoids
Assess type, amount, and time of acetaminophen ingestion. Assess plasma acetaminophen levels. Monitor AST, ALT, and bilirubin levels along with prothrombin time every 24 hr for 96 hr in patients with plasma acetaminophen levels indicating potential hepatotoxicity. Monitor cardiac and renal function, serum glucose, and electrolytes. Assess respiratory function and color, amount, and consistency of secretions. Assess skin lesions before and periodically during therapy. Monitor liver function (AST, ALT, and LDH) every 12 wk until stable and periodically thereafter as indicated. Assess neurologic status; administer only if patient is alert. Inquire as to the type of drug or poison and time of ingestion. Monitor blood pressure, pulse, respiratory and neurologic status, and urine output as indicated by toxicity of agent(s). Chronic use may impair absorption of essential nutrients. This may result in decreased mineral or electrolyte levels Assess lesions before and daily during therapy. Monitor neurologic status in patients with herpes encephalitis. Monitor BUN, serum creatinine, and CCr before and during therapy. Assess pain and range of motion; signs of infection; injection site reactions; latex allergy; signs of anaphylaxis; and latent tuberculosis with a tuberculin skin test prior to initiation of therapy.
extremities, alopecia, rash, anorexia, nausea, vomiting, anemia, hemolytic anemia. Drowsiness, vasodilation, rhinorrhea, bronchospasm, bronchial/tracheal irritation, chest tightness, increased secretions, nausea, vomiting, stomatitis, pruritus, rash, urticaria, clamminess, allergic reactions (primarily with IV), including anaphylaxis, angioedema, chills, fever.
Activated charcoal/ Acta-Char Liquid-A, Actidose-Aqua, CharcoAid 2000, Insta-Char, InstaChar Aqueous Suspension, Liqui-Char, SuperChar Aqueous
antidotes adsorbents
Rigors, dry eyes, irritation, hepatotoxicity, pancreatitis, alopecia, dry skin, nail disorder, peeling, pruritis, rash, hematuria, hyperlipidemia, arthralgia, hyperostosis, cheilitis, paresthesia, epistaxis. black stools, constipation, diarrhea, vomiting.
Acyclovir/Zovirax
antivirals purine analogues
Seizures, dizziness, headache, diarrhea, nausea, vomiting, renal failure, unusual sweating, Stevens-Johnson syndrome, thrombotic thrombocytopenic pupura/hemolytic uremic syndrome, pain, phlebitis. Headache, hypertension, abdominal pain, nausea, hematuria, rash, neutropenia, thrombocytopenia, injection site reactions, hypercholesterolemia, hyperlipidemia, back pain, allergic reactions including
Adalimumab/ Humira
antirheumatics dmards monoclonal antibodies
3
Rev. 08/21/08
anaphylaxis, infections. Adefovir/ Hepsera antivirals nucleotides May cause lactic acidosis and severe hepatomegaly with steatosis. Monitor patient for signs of increased serum lactate levels, elevated liver enzymes, liver enlargement on palpation. Monitor viral load and CD4 cell count regularly during therapy in patients with HIV infectionMonitor liver function tests and hepatitis B virus levels throughout and following therapy. Monitor heart rate frequently (every 1530 sec) and ECG continuously during therapy. Monitor blood pressure and respiratory status during therapy. Headache, cough, pharyngitis, sinusitis, dyspepsia, HEPATOMEGALY WITH STEATOSIS, abdominal pain, diarrhea, flatulence, increased liver enzymes, nausea, vomiting, hematuria, nephrotoxicity, pruritus, rash, lactic acidosis, weakness, fever, HIV resistance.
Adenosine/Adenocard, Adenoscan
antiarrhythmics
Agalsidase beta/ Fabrazyme
replacement enzyme enzymes
Assess for infusion reactions, and cardiac function during treatment in patients with previously compromised cardiac function
Alatrofloxacin/Trovan IV
anti-infectives fluoroquinolones
Assess patient for infection, signs and symptoms of anaphylaxis during therapy. Monitor liver function tests and pancreatic tests in patients who develop symptoms consistent with hepatitis and/or pancreatitis.
Albendazole/ Albenza
antihelmintics
Ophthalmic examinations should be performed before therapy to determine presence of retinal lesions. Monitor liver function tests before start of each treatment and at least every
Apprehension, dizziness, headache, head pressure, light-headedness, blurred vision, throat tightness, shortness of breath, chest pressure, hyperventilation, facial flushing, transient arrhythmias, chest pain, hypotension, palpitations, metallic taste, nausea, burning sensation, facial flushing, sweating, neck and back pain, numbness, tingling, heaviness in arms, pressure sensation in groin. Anxiety, depression, dizziness, headache, bronchospasm, edema, cardiomegaly, hypotension, hypertension, dyspepsia, nausea, testicular pain, pallor, skeletal pain, arthrosis, infusion reactions, rigors, fever. Seizures, dizziness, drowsiness, headache, insomnia, hepatoxicity, pseudomembranous colitis, abdominal pain, diarrhea, nausea, altered taste, interstitial cystitis, vaginitis, photosensitivity, rash, hypersensitivity reactions including Stevens-Johnson syndrome, and anaphylaxis. Headache, dizziness/ vertigo, increased intracranial pressure, abnormal liver function tests, abdominal pain, nausea/vomiting, reversible alopecia, granulocytopenia, agranulocytosis, pancytopenia,
4
Rev. 08/21/08
Albumin (human)/ Albuminar, Albutein, Buminate, normal human serum albumin, Plasbumin
volume expanders blood products colloids
Albuterol/Airet, Proventil, Proventil HFA, salbutamol, Ventolin, Ventolin HFA, Ventolin rotacaps
bronchodilators adrenergics
2 weeks during treatment. Monitor WBC count before each 28-day cycle and every 2 weeks during each 28day cycle. Monitor vital signs, CVP, and intake and output; signs of vascular overload; increased bleeding after administration caused by increased blood pressure and circulating blood volume throughout therapy. Monitor serum sodium levels. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; paradoxical bronchospasm before administration and during peak of medication.
meningeal signs, fever.
Headache, pulmonary edema, fluid overload, hypertension, hypotension, tachycardia, increased salivation, nausea, vomiting, rash, urticaria, back pain, chills, fever, flushing.
Alclometasone topical/ Aclovate
anti inflammatories steroidal corticosteroids
Aldesleukin/interleuki n2, IL-2, Proleukin
antineoplastics interleukins
Assess affected skin before and daily during therapy. Note degree of inflammation and pruritus. May cause increased serum and urine glucose concentrations if significant absorption occurs. Adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in longterm therapy. Monitor ECG continuously during infusion. Monitor vital signs at least daily; development of capillary leak syndrome; respiratory status and pulse oximetry; weight daily; changes in mental status; signs of infection; signs of anemia; nutrition and bowel status; skin daily for rash or blisters on skin throughout therapy. Monitor CBC, differential, platelet count, blood chemistries including electrolytes, and renal and hepatic function prior to and daily throughout therapy.
Nervousness, restlessness, tremor, headache, insomnia (Pedi: occurs more frequently in young children than adults), hyperactivity in children, chest pain, palpitations, angina, arrhythmias, hypertension, nausea, vomiting, hyperglycemia, hypokalemia, tremor. Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression.
Apnea, respiratory failure, dyspnea, pulmonary congestion, pulmonary edema, CHF, cardiac arrest, MI, stroke, arrhythmias, hypotension, tachycardia, bowel perforation, diarrhea, jaundice, nausea, stomatitis, vomiting, ascites, hepatomegaly, oliguria/anuria, proteinuria, dysuria, hematuria, renal failure, exfoliative dermatitis, pruritus, acidosis, hypocalcemia, hypokalemia, hypomagnesemia, hypophosphatemia, alkalosis, anemia, coagulation disorders, leukopenia, thrombocytopenia, leukocytosis, capillary leak
5
Rev. 08/21/08
syndrome, chills, fever. Alefacept/ Amevive antipsoriatics immunosuppressan ts fusion proteins rDNA Assess skin lesions; signs and symptoms of infection; allergic reactions; signs and symptoms of hepatic impairment before and during therapy. Monitor CD4 and T lymphocyte count before initiating and weekly during therapy. Monitor for infusion reactions. Obtain CBC and platelet counts weekly during therapy and more frequently if worsening anemia, neutropenia, or thrombocytopenia is observed. Dizziness, chills, pruritis, fatty liver, hepatitis, increase in liver enzymes, liver failure, nausea, lymphopenia, injection site reactions, myalgia, pharyngitis, cough, hypersensitivity reactions (angioedema, urticaria), immunosuppression, infection, malignancies. Depression, dizziness, drowsiness, fatigue, headache, weakness, bronchospasm, cough, dyspnea, hypertension, hypotension, tachycardia, abdominal pain, anorexia, constipation, stomatitis, rash, sweating, edema, neutropenia, pancytopenia/ marrow hypoplasia, anemia, lymphopenia, thrombocytopenia, back pain, skeletal pain, infusion-related events, infection, sepsis. Headache, blurred vision, conjunctivitis, eye pain/inflammation, atrial fibrillation, abdominal distention, abdominal pain, acid regurgitation, constipation, diarrhea, dyspepsia, dysphagia, esophageal ulcer, flatulence, gastritis, nausea, taste perversion, vomiting, erythema, photosensitivity, rash, musculoskeletal pain, osteonecrosis. Dizziness, sleepiness, blurred vision, apnea, respiratory depression, bradycardia, hypotension, tachycardia, arrhythmias, hypertension, nausea, vomiting, thoracic muscle rigidity, skeletal muscle rigidity. Dizziness, fatigue, headache, bronchitis, sinusitis, pharyngitis, postural hypotension, abdominal pain, constipation, dyspepsia, nausea, erectile dysfunction. Bradycardia, tachycardia, respiratory distress failure, cough, oxygen saturation,
Alemtuzumab/ Campath
antineoplastics monoclonal antibodies
Alendronate/ Fosamax
bone resorption inhibitors biphosphonates
Assess patients for low bone mass and symptoms of Paget's disease before and periodically during therapy. Assess serum calcium and alkaline phosphatase before and periodically during therapy.
Alfentanil/ Alfenta
analgesic adjuncts opioid analgesics opioid agonists
Alfuzosin/ Uroxatral
urinary tract antispasmodics peripherally acting antiadrenergics
Alglucosidase/ Myozyme
replacement enzyme
Assess vital signs, especially respiratory status and ECG, frequently during and following administration. Symptoms of toxicity include respiratory depression, hypotension, arrhythmias, bradycardia, and asystole. Assess patient for symptoms of benign prostatic hyperplasia; orthostatic reaction and syncope; BP; and pulse before and periodically during therapy. Observe for signs and symptoms of anaphylaxis; infusion-related reactions;
6
Rev. 08/21/08
and cardiorespiratory status continuously during therapy. Monitor liver enzymes prior to and periodically during therapy.
Aliskiren/ Tekturna
antihypertensives renin inhibitors
Alitretinoin/ Panretin
antineoplastics retinoids antigout agents antihyperuricemics xanthine oxidase inhibitors
Allopurinol/ Alloprim, Lopurin, Zyloprim
Almotriptan/ Axert
vascular headache suppressants five ht1 agonists
Aloe/ Aloe vera, cape, Zanzibar, socotrine, curacao
laxatives
Alosetron/ Lotronex
anti irritable bowel syndrome agents five ht3 antagonists
Monitor blood pressure and pulse frequently during initial dose adjustment and periodically during therapy. Assess skin lesions and dermal toxicities throughout therapy. Monitor intake and output ratios; rash or more severe hypersensitivity reactions; joint pain and swelling; blood glucose in patients receiving oral hypoglycemic agents. Monitor hematologic, renal, and liver function tests before and periodically during therapy, especially during the first few months. Assess pain location, character, intensity, and duration and associated symptoms (photophobia, phonophobia, nausea, vomiting) during migraine attack. Perform baseline skin assessment prior to applying aloe to minor wounds, burns, and abrasions. Assess for abdominal distention, presence of bowel sounds, and usual pattern of elimination; color, consistency, and amount of stool produced; inflammation, drainage, pain, warmth, and/or pruritus. Monitor patient for signs of constipation or ischemic colitis (new or worsening abdominal pain, bloody diarrhea, blood in stool) throughout therapy. Assess for signs of neuropsychiatric disorders; signs of infection; cardiovascular disorders; signs of colitis; development
tachypnea, diarrhea, reflux, vomiting, constipation, flushing, rash, dermatitis, urticaria, anemia, allergic reactions including anaphylaxis, infustion reactions, fever. Cough, abdominal pain, diarrhea (in females and elderly), dyspepsia, reflux, angioedema. Pain, pruritus, rash, edema, exfoliative, dermatitis, paresthesia. Hypotension, flushing, hypertension, bradycardia, and heart failure (reported with IV administration), drowsiness, diarrhea, hepatitis, nausea, vomiting, renal failure, hematuria, rash (discontinue drug at first sign of rash), urticaria, bone marrow depression, hypersensitivity reactions. Drowsiness, headache, coronary artery vasospasm, MI, myocardial ischemia, ventricular fibrillation, ventricular tachycardia, dry mouth, nausea, paresthesia. Contact dermatitis, skin irritation, hypokalemia, dehydration, cramping, diarrhea, laxative dependence (chronic use), red-colored urine.
Alpha Interferons/ Pegasys, Intron A, Pegintron, Alferon N
immune modifiers interferons
Acute ischemic colitis, toxic megacolon, constipation, abdominal discomfort, abdominal distention, flatulence, nausea, GI viral infections, hemorrhoids, regurgitation or reflux. Neuropsychiatric disorders, confusion, depression, dizziness, fatigue, headache, insomnia, irritability, anxiety, blurred vision, nose bleeds,
7
Rev. 08/21/08
of flu-like syndrome; bone marrow depression; pulmonary status; signs of thyroid dysfunction; and number, size, and character of lesions prior to and throughout therapy. Monitor for CBC and differential prior to and periodically during therapy.
Alpha1-proteinase inhibitor, Human/alpha1antitrypsin, Aralast, Prolastin, Zemaira
pulmonary replacement enzyme inhibitor enzyme inhibitors
Alprazolam/ Niravam, Xanax, Xanax XR
antianxiety agents benzodiazepines
Alprostadil (intracavernosal, intraurethral)/ Caverject, Edex, MUSE
erectile dysfunction agents prostaglandins
Monitor respiratory status; fever, chills, and dizziness; signs of fluid overload prior to and weekly during therapy. Monitor serum alpha1-proteinase inhibitor levels to determine response to therapy. Assess degree and manifestations of anxiety and mental status; drowsiness, lightheadedness, and dizziness; CNS effects and risk of falls prior to and periodically during therapy. Monitor CBC and liver and renal function periodically during longterm therapy. Monitor for hypotension during in-clinic dosing.
rhinitis, ischemic disorders, arrhythmias, chest pain, edema, colitis, pancreatitis, anorexia, abdominal pain, diarrhea, dry mouth, nausea, taste disorder, vomiting, weight loss, drug-induced hepatitis, flatulence, alopecia, dry skin, pruritus, rash, sweating, leucopenia, thrombocytopenia, anemia, hemolytic anemia, arthralgia, myalgia, cough, dyspnea, autoimmune disorders, infectious disorders, chills, fever, flu-like syndrome. Dizziness, headache, transient in liver enzymes, transient leukocytosis, cough, respiratory tract infection, sore throat, delayed fever.
Dizziness, drowsiness, lethargy, confusion, hangover, headache, mental depression, paradoxical excitation, blurred vision, constipation, diarrhea, nausea, vomiting, weight gain, rashes, physical dependence, psychological dependence, tolerance.
Alprostadil (systemic)/ Prostaglandin E1, Prostin VR Pediatric
ductus arteriosus patency adjuncts prostaglandins
Monitor temperature, respiratory rate, pulse, blood pressure, and ECG; respiratory status and heart sounds; facial or arm flushing; signs of bleeding during therapy. Monitor arterial blood gases before and periodically throughout therapy.
Dizziness, headache, hypertension, hypotension, penile pain, penile edema, penile fibrosis, penile rashes, priapism, back pain, cough, bleeding, ecchymosis (injection), hematomas (injection), irritation. Seizures, cerebral bleeding, irritability, jitteriness, lethargy, apnea, altered respiratory rate (slow and fast), hypercapnia, respiratory depression, wheezing, arrhythmia, bradycardia, edema, heart block, heart failure, hypotension, tachycardia, diarrhea, gastric regurgitation, hyperbilirubinemia, peritonitis, anuria, hematuria, flushing, hypokalemia, disseminated intravascular coagulation,
8
Rev. 08/21/08
Alteplase/ Activase, Cathflo Activase, tissue plasminogen activator, t-PA
thrombolytics plasminogen activators
Altretamine/ Hexalen, hexamethylmelamine
antineoplastics
Aluminum hydroxide/ AlternaGEL, Alu-Cap, Aluminet, Alu-Tab, Amphojel, Basalgel, Dialume
antiulcer agents hypophosphatemics antacids phosphate binders
Alvimopan/ Entereg
gastric stimulant opioid antagonists
Amantadine/ Symmetrel
antiparkinson agents antivirals
Ambrisentan/ Letairis
antihypertensives endothelin receptor antagonists
Monitor vital signs, including temperature, continuously for myocardial infarction and at least every 4 hr during therapy for other indications. Assess patient carefully for bleeding every 15 min during the 1st hr of therapy, every 1530 min during the next 8 hr, and at least every 4 hr for the duration of therapy. Assess patient for hypersensitivity reaction; neurologic status throughout therapy. Monitor ECG continuously. Monitor for bone marrow depression and signs of neurotoxicity including CNS effects throughout therapy. Monitor CBC and platelets prior to each course of therapy, monthly, and as clinically indicated. Assess location, duration, character, and precipitating factors of gastric pain. Monitor serum phosphate and calcium levels periodically during chronic use of aluminum hydroxide. Assess bowel sounds and frequency, quantity, and consistency of stools periodically during therapy. Monitor blood pressure; drug-induced orthostatic hypotension; vital signs and mental status; CHF; appearance of a diffuse red mottling of the skin; intake and output; akinesia, rigidity, tremors, and gait disturbances; respiratory status and temperature before and throughout therapy. Assess patient for signs and symptoms of primary pulmonary hypertension; peripheral edema during therapy. Monitor liver chemistries prior to initiation
anemia, bleeding, thrombocytopenia, hypoglycemia, neck hyperextension, stiffness, fever, hypothermia, sepsis. Intracranial hemorrhage, epistaxis, gingival bleeding, bronchospasm, hemoptysis, reperfusion arrhythmias, hypotension, recurrent ischemia/thromboembolism, GI bleeding, nausea, retroperitoneal bleeding, vomiting, GU tract bleeding, ecchymoses, flushing, urticaria, bleeding, hemorrhage at injection site, phlebitis at injection site, musculoskeletal pain, allergic reactions including anaphylaxis, fever. Seizures, fatigue, nausea, vomiting, anorexia, hepatic toxicity, gonadal suppression, renal toxicity, alopecia, pruritus, skin rash, gonadal suppression, anemia, leukopenia, thrombocytopenia, peripheral neuropathy. Constipation, hypophosphatemia.
Constipation, dyspepsia, flatulence, hypokalemia, urinary retention, anemia, back pain. Ataxia, dizziness, insomnia, anxiety, confusion, depression, drowsiness, psychosis, seizures, nausea, vomiting, anorexia, constipation, blurred vision, dry mouth, dyspnea, hypotension, CHF, edema, urinary retention, mottling, livedo reticularis, rashes, leukopenia, neutropenia.
Headache, hepatotoxicity, fluid retention, hemoglobin, sperm count.
9
Rev. 08/21/08
Amcinonide/ Cyclocort
anti inflammatories steroidal corticosteroids
of therapy and at least every month thereafter. Assess affected skin before and daily during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected. Monitor blood pressure before and every 5 min during infusion; fluid status; signs and symptoms of anaphylaxis; dry mouth and mouth sores during therapy. Monitor serum calcium concentrations before and periodically during therapy. Assess patient for infection; Evaluate eighth cranial nerve function by audiometry; intake and output and daily weight; and signs of superinfection before and throughout therapy. Monitor renal function by urinalysis, specific gravity, BUN, creatinine, and CCr before and throughout therapy. Monitor intake and output ratios and daily weight; signs and symptoms of hypokalemia throughout therapy. Monitor BUN, serum creatinine, and electrolytes before and periodically throughout therapy. Monitor blood pressure, pulse, and respiratory status; overt bleeding every 1530 min; neurologic status; intake and output ratios; and thromboembolic complications during therapy. Monitor platelet count and clotting factors prior to and periodically throughout therapy in patients with systemic fibrinolysis. Monitor patient for changes in signs of Cushing's
Amifostine/ Ethyol
cytoprotective agents
Amikacin/ Amikin
anti-infectives aminoglycosides
Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression. Dizziness, somnolence, sneezing, hypotension, hiccups, nausea, vomiting, flushing, hypocalcemia, allergic reactions including anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis, toxoderma, erythema multiforma, exfoliative dermatitis, chills. Vertigo, ototoxicity (vestibular and cochlear), nephrotoxicity, enhanced neuromuscular blockade, apnea, hypersensitivity reactions.
Amiloride/ Midamor
diuretics potassium sparing diuretics
Dizziness, headache, arrhythmias, constipation, nausea, vomiting, hyperkalemia, hyponatremia, muscle cramps, allergic reactions.
Aminocaproic acid/ Amicar, epsilon aminocaproic acid
hemostatic agents fibrinolysis inhibitors
Dizziness, malaise, nasal stuffiness, tinnitus, arrhythmias, hypotension (IV only), anorexia, bloating, cramping, diarrhea, nausea, diuresis, renal failure, myopathy.
Aminoglutethimide/ Cytadren
antineoplastics adrenal
Drowsiness, dizziness, headache, weakness,
10
Rev. 08/21/08
suppressants aromatase inhibitors
Aminolevulinic acid/ Levulan Kerastick Aminophylline/ Truphylline
photosensitizers
bronchodilators xanthines
Amiodarone/Cordaron e, Pacerone
antiarrhythmics (class III)
syndrome; blood pressure with patient recumbent and upright; CNS side effects; measles-like rash and fever; and during periods of stress throughout therapy. Monitor serum acid phosphatase concentrations periodically throughout therapy in patients with prostatic carcinoma. Assess skin lesions prior to and periodically during therapy. Assess blood pressure, pulse, respiratory status; intake and output ratios for an increase in diuresis or fluid overload; chest pain and ECG changes; and pulmonary function tests before and periodically during therapy. Monitor ABGs, acid-base, and fluid and electrolyte balance in patients receiving parenteral therapy or whenever required by patient's condition. Monitor drug levels routinely. Monitor ECG continuously; signs of pulmonary toxicity; signs and symptoms of ARDS; neurotoxicity; Ophthalmic exams; and thyroid dysfunction during initial and throughout therapy. Monitor liver and thyroid functions; and AST, ALT, and alkaline phosphatase at regular intervals before and periodically throughout therapy.
hypotension, tachycardia, anorexia, nausea, hepatitis, vomiting, measles-like rash, pruritus, urticaria, adrenal insufficiency, hirsutism in women, hypothyroidism, masculinization in women, agranulocytosis, leukopenia, neutropenia, thrombocytopenia, myalgia, fever. Burning, edema, pruritus, stinging, oozing, scaling, ulceration. Seizures, anxiety, headache, insomnia, irritability, arrhythmias, tachycardia, angina, palpitations, rash, nausea, vomiting, anorexia, tremor.
Amitriptyline/ Elavil
antidepressants tricyclic antidepressants
Assess fasting glucose and cholesterol levels in overweight/obese individuals; obtain weight and BMI initially and periodically; blood pressure and pulse; mental status; intensity, quality, and location of pain throughout therapy. Assess leukocyte
Dizziness, fatigue, malaise, corneal microdeposits, adult respiratory distress syndrome (ARDS), pulmonary fibrosis, pulmonary toxicity, CHF, worsening of arrhythmias, bradycardia, hypotension, liver function abnormalities, anorexia, constipation, nausea, vomiting, toxic epidermal necrolysis, photosensitivity, hypothyroidism, hyperthyroidism, ataxia, involuntary movement, paresthesia, peripheral neuropathy, poor coordination, tremor. Lethargy, sedation, blurred vision, dry eyes, dry mouth, arrhythmias, hypotension, ECG changes, constipation, hepatitis, paralytic ileus, increased appetite, weight gain, urinary retention, libido, photosensitivity, changes in blood glucose, gynecomastia, blood
11
Rev. 08/21/08
Amlodipine/ Norvasc
antihypertensives calcium channel blockers
Ammonium chloride
electrolyte modifiers acidifying agents
Amobarbital/ Amytal
sedative/hypnotics barbiturates
Amoxapine/ Asendin
antidepressants
and differential blood counts, liver function, and serum glucose before and periodically during therapy. Monitor blood pressure and pulse; intake and output ratios and daily weight; CHF; location, duration, intensity, and precipitating factors of patient's anginal pain before and periodically during therapy. Assess patient for signs of metabolic alkalosis; signs of hepatic function impairment; especially in patients with uremia, cirrhosis, or hepatitis. Monitor serum bicarbonate levels to determine dose. Monitor patient for symptoms of ammonia toxicity. Monitor respiratory status, pulse, and blood pressure frequently; and sleep patterns before and periodically throughout therapy. Monitor mental status; suicidal tendencies; BP and pulse; onset of extrapyramidal side effects; tardive dyskinesia; and development of neuroleptic malignant syndrome before and during initial therapy. Monitor CBC and differential during chronic therapy. In chronic therapy, periodically monitor hepatic and renal function. Assess for infection; anaphylaxis; and bowel function beginning of and throughout therapy.
dyscrasias.
Headache, dizziness, fatigue, peripheral edema, angina, bradycardia, hypotension, palpitations, gingival hyperplasia, nausea, flushing.
Coma, confusion, drowsiness, headache, seizure, rash, hypokalemia, gastric irritation, nausea, vomiting, metabolic acidosis, pain/irritation at IV site, ammonia toxicity, twitching, hyperventilation.
Amoxicillin/ Amoxil, DisperMox, Moxatag, Trimox, Wymox
anti-infectives antiulcer agents aminopenicillins
Amoxicillin/clavulanat e// Augmentin, Augmentin ES, Augmentin XR
anti-infectives aminopenicillins beta lactamase inhibitors
Assess for infection; anaphylaxis; and bowel function beginning of and throughout therapy.
Drowsiness, bronchospasm (IV ONLY), laryngospasm (IV ONLY), angioedema, hypersensitivity reactions including Stevens-Johnson syndrome, fever. Neuroleptic malignant syndrome, fatigue, sedation, extrapyramidal reactions, tardive dyskinesia, blurred vision, dry eyes, dry mouth, arrhythmias, hypotension, ECG changes, constipation, increased appetite, weight gain, paralytic ileus, testicular swelling, urinary retention, photosensitivity, rash, gynecomastia, sexual dysfunction, blood dyscrasias, fever. Seizures, pseudomembranous colitis, diarrhea, nausea, vomiting, elevated liver enzymes, rashes, urticaria, blood dyscrasias, allergic reactions including anaphylaxis, serum sickness, superinfection. Seizures, urticaria, rashes, pseudomembranous colitis, nausea, diarrhea, hepatic dysfunction, vomiting, vaginal candidiasis, blood dyscrasias, allergic reactions including anaphylaxis, serum sickness,
12
Rev. 08/21/08
superinfection. Amoxapine/ Asendin antidepressants Monitor mental status, suicidal tendencies, blood pressure and pulse, onset of extrapyramidal side effects, tardive dyskinesia, and development of neuroleptic malignant syndrome before and during therapy. Monitor CBC and differential during chronic therapy. In chronic therapy, periodically monitor hepatic and renal function. Neuroleptic malignant syndrome, fatigue, sedation, extrapyramidal reactions, tardive dyskinesia, blurred vision, dry eyes, dry mouth, arrhythmias, hypotension, ECG changes, constipation, increased appetite, weight gain, paralytic ileus, testicular swelling, urinary retention, photosensitivity, rash, gynecomastia, sexual dysfunction, blood dyscrasias, fever. Hyperactivity, insomnia, restlessness, tremor, behavioral disturbances, dizziness, hallucinations, headache, mania, irritability, thought disorder, palpitations, tachycardia, cardiomyopathy, hypertension, hypotension, anorexia, constipation, cramps, diarrhea, dry mouth, metallic taste, nausea, vomiting, erectile dysfunction, increased libido, urticaria, growth inhibition, psychological dependence. anxiety, confusion, headache, insomnia, dyspnea, hypoxia, wheezing, chest pain, hypotension, tachycardia, edema, hypertension, diarrhea, hyperbilirubinemia, liver enzyme elevation, nausea, vomiting, abdominal pain, nephrotoxicity, hematuria, hyperglycemia, hypocalcemia , hypokalemia, hypomagnesemia, anemia, leukopenia, thrombocytopenia, pruritis, rashes, phlebitis, arthralgia, myalgia, chills, fever, acute infusion reactions, hypersensitivity reactions Seizures, pseudomembranous colitis, diarrhea, nausea, vomiting, rashes, urticaria, blood dyscrasias, allergic reactions including anaphylaxis, serum sickness, superinfection.
Amphetamine mixtures/ Amphetamine Salt, Adderall, Adderall XR
central nervous system stimulants
Monitor blood pressure, pulse, and respiration; behavior change; weight biweekly; and frequency of narcoleptic episodes before and periodically during therapy. Assess attention span, impulse control, motor and vocal tics, and interactions with others in children with ADHDs.
Amphotericin B deoxycholate / Amphotec, Abelcet, AmBisome
antifungals
Ampicillin/Marcillin, Omnipen, Penbritin, Principen, Polycillin, Totacillin
anti-infectives aminopenicillins
Assess injection site frequently for thrombophlebitis or leakage; vital signs every 15 min during test dose and every 30 min for 24 hr after administration; intake and output and weigh daily; monitor patient closely during test dose and the first 12 hr of each dose for fever, chills, headache, anorexia, nausea, or vomiting. Monitor CBC, BUN and serum creatinine, and potassium and magnesium levels daily. Assess patient for infection; anaphylaxis; and skin for "ampicillin rash," a nonallergic, dull red, macular or maculopapular, mildly pruritic rash at beginning of and throughout therapy.
13
Rev. 08/21/08
Ampicillin/sulbactam// Unasyn
anti-infectives aminopenicillins beta lactamase inhibitors
Assess patient for infection and anaphylaxis at beginning of and throughout therapy.
Amprenavir/Ageneras e
antiretrovirals protease inhibitors
Amyl nitrite
antianginals antidotes nitrates
Assess patient for change in severity of HIV symptoms; symptoms of opportunistic infections; allergy to sulfonamides; and skin reactions throughout therapy. Monitor viral load and CD4 cell count regularly during therapy. Assess heart rate and blood pressure; location, duration, intensity, and cause of chest pains; signs of cyanide poisoning; and heart rate before and periodically throughout therapy and administration. Monitor blood pressure, cardiovascular status, signs and symptoms of interstitial lung diseases during therapy. Monitor platelet count every 2 days during first wk of therapy and weekly until maintenance dose is reached.
Seizures, diarrhea, nausea, pseudomembranous colitis, vomiting, rashes, urticaria, blood dyscrasias, pain at IM site, pain at IV site, allergic reactions including anaphylaxis, serum sickness, superinfection, elevated liver enzymes. Depression/mood disorder, diarrhea, nausea, taste disorders, vomiting, rash, hyperglycemia, hyperlipidemia, redistribution/accumulation of body fat.
Anagrelide/ Agrylin
platelet reducing agent
Anakinra/ Kineret
antirheumatics (DMARD) interleukin antagonists
Anastrazole/ Arimidex
antineoplastics aromatase inhibitors
Assess patient's range of motion and degree of swelling and pain in affected joints; signs and symptoms of infection; and hypersensitivity reactions before and periodically during therapy. Monitor neutrophil count prior to and during therapy, then monthly for 3 mo and quarterly thereafter for up to 1 yr. Assess patient for pain and other side effects periodically during therapy.
Headache, restlessness, dizziness, fainting, weakness, intraocular pressure, shortness of breath, hypotension, tachycardia, flushing, cyanosis of lips, fingernails, or palms, nausea, methemoglobinemia, hemolytic anemia. Seizures, dizziness, headache, eosinophilic pneumonia, interstitial pneumonitis, pulmonary fibrosis, pulmonary hypertension, dyspnea, cardiomegaly, cardiomyopathy, cerebrovascular accident, complete heart block, congestive heart failure, MI, chest pain, edema, palpitations, GI bleeding, pancreatitis, abdominal pain, diarrhea, flatulence, renal failure, weakness. Headache, diarrhea, nausea, neutropenia, injection site reactions, infections, hypersensitivity reactions (rare).
Headache, weakness, dizziness, pharyngitis, dyspnea, increased cough,
14
Rev. 08/21/08
Anidulafungin/ Eraxis
antifungals echinocandins
Assess infected area and monitor cultures before and periodically during therapy. Assess type, location, and intensity of pain prior to and 1 hr following IV administration; level of consciousness, blood pressure, pulse, and respirations; and bowel function before and periodically during therapy. Assess the frequency and nature of the cough, lung sounds, and amount and type of sputum produced; epigastric or abdominal pain; and weight gain associated with sodium and water retention during therapy. Monitor vital signs, including temperature, continuously for myocardial infarction; bleeding every 15 min during the 1st hr of therapy, every 1530 min during the next 8 hr, and at least every 4 hr; hypersensitivity reaction; inquire about recent streptococcal infection; and neurologic status; ECG continuously; intensity, character, location, and radiation of chest pain; heart sounds and breath sounds throughout therapy. Hematocrit, hemoglobin, platelet count, fibrin/fibrin degradation product (FDP/fdp) titer, fibrinogen concentration, prothrombin time, thrombin time, and activated partial thromboplastin time may be
Anileridine/ Leritine
opioid analgesics opioid agonists
Anise (Anisi fructus)/ anise seed, sweet cumin
expectorant
peripheral edema, nausea, abdominal pain, anorexia, constipation, diarrhea, dry mouth, vomiting, pelvic pain, vaginal bleeding, vaginal dryness, rash, including mucocutaneous disorders, sweating, weight gain, back pain, bone pain, paresthesia, angioedema, urticaria, anaphylaxis, hot flashes, pain. Dyspnea, hypotension, diarrhea, liver enzymes, flushing, rash, urticaria, hypokalemia. Dizziness, euphoria, excitement, nervousness, restlessness, disturbed vision, respiratory depression, constipation, dry mouth, nausea, vomiting, flushing, itching, sweating, physical dependence, psychological dependence, tolerance. Seizures (toxic amounts of essential oil), nausea, vomiting, Pulmonary edema, allergic reactions.
Anistreplase/ anisoylated plasminogen streptokinase activator complex, APSAC,
thrombolytics plasminogen activators
Intracranial hemorrhage, epistaxis, gingival bleeding, bronchospasm, hemoptysis, reperfusion arrhythmias, hypotension, recurrent ischemia/thromboembolism, GI bleeding, hepatotoxicity, nausea, retroperitoneal bleeding, vomiting, GU tract bleeding, ecchymoses, flushing, urticaria, bleeding, hemorrhage at injection site, phlebitis at injection site, musculoskeletal pain, allergic reactions including anaphylaxis, fever.
15
Rev. 08/21/08
Anthrax vaccine (absorbed)/ BioThrax
vaccines/immunizin g agents
Antihemophilic factor/ Advate, AHF, Alphanate, Bioclate, factor VIII, Helixate FS, Helixate NexGen, Humate-P, HYATE:C, Koate-DVI, Kogenate, Kogenate FS, Monoclate-P, Recombinate, ReFacto
hemostatic agents blood products
evaluated before and frequently during therapy. Prior to administration, assess patient's immunization history for possible vaccine sensitivities and/or previous vaccinerelated adverse reactions to determine if vaccine is contraindicated; illness (fever); history of latex sensitivity; adverse reactions throughout series of vaccinations. Monitor blood pressure, pulse, and respirations; renewed bleeding every 15 30 min; intake and output ratios; note color of urine; allergic reaction. Monitor plasma factor VIII levels.
Headache, anorexia, nausea, vomiting, local reactions, myalgia, respiratory difficulty, allergic reactions including anaphylaxis, fever, malaise.
Aprepitant/ Emend
antiemetics neurokinin antagonists
Apomorphine/ Apokyn
antiparkinson agents dopamine agonists
Assess nausea, vomiting, appetite, bowel sounds, and abdominal pain; hydration, nutritional status, and intake and output prior to and following administration. Monitor clotting status closely during the 2 wk period, especially at 710 days, following aprepitant therapy in patients on chronic warfarin therapy. Assess for nausea and vomiting; blood pressure standing and lying during dose titration. Orthostatic hypotension may occur any time during therapy but occurs more frequently during initial therapy or with a dose increase.
Headache, lethargy, loss of consciousness, sedation, visual disturbances, chest tightness, hypotension, tachycardia, nausea, vomiting, flushing, urticaria, intravascular hemolysis, postoperative hemorrhage, back pain, paresthesia, allergic reactions, hepatitis B, C, D, or HIV virus infection, chills, fever, jaundice, rigor. Dizziness, fatigue, weakness, diarrhea, hiccups.
Aprotinin/ Trasylol
hemostatic agents proteinase inhibitors
Monitor patient for development of allergic reactions during therapy. Usually causes elevations in partial thromboplastin time (PTT) and activated clotting
Dizziness, hallucinations, somnolence, confusion, sudden drowsiness, headache, rhinorrhea, cardiac arrest, chest pain, hypotension, angina, CHF, QTc prolongation, nausea, vomiting, priapism, pallor, flushing, sweating, injection site pain, arthralgia, back pain, limb pain, aggravation of Parkinson's disease, dyskinesia, yawning. Renal tubular necrosis, phlebitis, hypersensitivity reactions including anaphylaxis (incidence increases with repeated use).
16
Rev. 08/21/08
time (ACT). Arbutamine/ GenESA diagnostic agents cardiac stress agents Monitor heart rate before and after the procedure until heart rate and blood pressure have returned to acceptable levels. Anxiety, dizziness, fatigue, headache, dyspnea, arrhythmias, angina, hypotension, palpitations, vasodilation, altered taste, dry mouth, flushing, sweating, transient hypokalemia, tremors, hypoesthesia, paresthesia. Dizziness, headache, insomnia, edema, constipation, nausea, reversible increase in liver enzymes, vomiting, urinary retention, ecchymoses, pruritus, rash, urticaria, bleeding, anemia, thrombocytopenia, erythema at injection site, hematoma, irritation, pain, fever.
Ardeparin/ Normiflo
anticoagulants antithrombotics
Arformoterol/ Brovana
bronchodilators adrenergics
Assess patient for signs of bleeding and hemorrhage; evidence of additional or increased thrombosis; hypersensitivity reactions; and epidural catheters frequently for signs and symptoms of neurologic impairment. Observe injection sites for hematomas, ecchymosis, or inflammation. Monitor CBC, platelet count, and stools for occult blood periodically throughout therapy. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; paradoxical bronchospasm before administration and during peak of medication.
Argatroban/ Argatroban
anticoagulants thrombin inhibitors
Aripiprazole/ Abilify
antipsychotics mood stabilizers dihydrocarbostyril
Monitor for signs of anaphylaxis and vital signs periodically during therapy. Monitor aPTT prior to initiation of continuous infusion, 2 hours after initiation of therapy, and periodically during therapy to confirm aPTT is within desired therapeutic range. Assess hemoglobin, hematocrit, and platelet count prior to, and periodically during, argatroban therapy. Assess patient's mental status; weight and BMI; BP, pulse, and respiratory rate; akathisia; extrapyramidal side effects; tardive dyskinesia; and development of neuroleptic malignant syndrome. Obtain fasting blood glucose and
Headache, insomnia, nervousness, weakness, paradoxical bronchospasm, ECG changes, tachycardia, vomiting, rash, hypokalemia, leukocytosis, cramps, tremor, hypersensitivity reactions including anaphylaxis, fever. Hypotens, diarrhea, nausea, vomiting, bleeding, allergic reactions including anaphylaxis, fever.
drowsiness, extrapyramidal reactions, constipation, tremor, neuroleptic malignant syndrome, bradycardia, chest pain, edema, hypertension, orthostatic hypotension, tachycardia, blurred vision, conjunctivitis, ear pain, anorexia, salivation, nausea,
17
Rev. 08/21/08
cholesterol levels initially and periodically during therapy.
Armodafinil/ Nuvigil
central nervous system stimulants
Observe and document wakefulness and frequency of narcoleptic episodes. Monitor blood pressure periodically during therapy.
Arnica/ leopard's bane, mountain tobacco, mountain snuff, wolf's bane Arsenic trioxide/ Trisenox
anti-infectives
antineoplastics heavy metals
Inspect skin for breaks prior to application; and after application, assess the affected area for signs of allergic response. Assess patient for APL differentiation syndrome; ECG prior to initiation of therapy and weekly or more frequently for clinically unstable patients during induction or consolidation phase; and vital signs periodically throughout therapy. Monitor electrolyte, hematologic, and coagulation profiles at least twice weekly and more frequently for clinically unstable patients during induction phase and at least weekly during consolidation phase.
Ascorbic acid/Ascorbicap, Cebid, Cecon, Cecore500, Cemill, Cenolate, Cetane, Cevalin, CeviBid, Flavorcee, MegaC/A Plus, Ortho/CS, Sunkist Asparaginase/ Elspar
vitamins water soluble vitamins
Assess for signs of vitamin C deficiency before and during therapy.
vomiting, weight loss, hyperglycemia, anemia, fatigue, hostility, insomnia, lightheadedness, manic reactions, confusion Dizziness, headache, insomnia, anxiety , psychiatric reactions, blood pressure, nausea, dry mouth, StevensJohnson syndrome, rash, multi-organ hypersensitivity, allergic reactions including anaphylactoid reactions and angioedema. Edematous dermatitis with pustules (chronic treatment of damaged skin), eczema (prolonged use), local allergic reactions. Fatigue, headache, insomnia, weakness, hypoxia, dyspnea, pleural effusion, QT prolongation, complete AV block, atrial arrhythmias, abdominal pain, constipation, increase liver enzymes, renal failure, dermatitis, hyperglycemia, hypoglycemia, acidosis, hypocalcemia, hyperkalemia, hypokalemia, hypomagnesemia, neutropenia, APL differentiation syndrome, disseminated intravascular coagulation, thrombocytopenia, hyperleukocytosis, anemia, leukocytosis, back pain, arthralgia, bone pain, neck pain, limb pain, myalgia, allergic reactions, fever, infection/sepsis. Drowsiness, fatigue, headache, insomnia, cramps, diarrhea, heartburn, nausea, vomiting, kidney stones, flushing, deep vein thrombosis, hemolysis, sickle cell crisis, pain at subcut or IM sites. Seizures, agitation, coma, confusion, depression, dizziness, fatigue, hallucinations, headache, irritability, somnolence, nausea, vomiting, anorexia, cramps, hepatotoxicity,
antineoplastics enzymes
Monitor vital signs; intake and output; hypersensitivity reaction; nausea, vomiting, and appetite; weigh weekly; and neurologic status before and frequently during therapy. Monitor CBC and
18
Rev. 08/21/08
blood glucose before and periodically throughout therapy.
Aspirin/acetylsalicylic Acid,
antipyretics nonopioid analgesics salicylates
Atazanavir/ Reyataz
antiretrovirals protease inhibitors
Atenolol/ Tenormin
antianginals antihypertensives beta blockers
Assess pain and limitation of movement; note type, location, and intensity before and at the peak after administration. Assess fever and note associated signs. Monitor hepatic function before antirheumatic therapy. Monitor for the onset of tinnitus, headache, hyperventilation, agitation, mental confusion, lethargy, diarrhea, and sweating. Assess for change in severity of HIV symptoms and for symptoms of opportunistic infections throughout therapy. Assess for rash which can occur within initial 8 wk of therapy. Usually resolves within 2 weeks without altering therapy. Monitor viral load and CD4 cell count regularly during therapy. Monitor blood pressure, ECG, and pulse; intake and output ratios and daily weights; and CHF frequently during dosage adjustment period and periodically throughout therapy.
pancreatitis, weight loss, rashes, urticaria, hyperglycemia, coagulation abnormalities, transient bone marrow depression, hyperammonemia, hyperuricemia, hypersensitivity reactions including anayphylaxis. Tinnitus, GI bleeding, dyspepsia, epigastric distress, nausea, abdominal pain, anorexia, hepatotoxicity, vomiting, anemia, hemolysis, rash, urticaria, allergic reactions including anaphylaxis and laryngeal edema.
Headache, depression, dizziness, insomnia, PR interval, heart block, nausea, abdominal pain, bilirubin, cholelithiasis, diarrhea, jaundice, vomiting, transaminases, rash. Hyperglycemia, fat redistribution, myalgia, fever.
Atomoxetine/Strattera
agents for attention deficit disorder selective norepinephrine reuptake inhibitors
Assess attention span, impulse control, and interactions with others. Monitor blood pressure and pulse; growth, body height,
Fatigue, weakness, anxiety, depression, dizziness, drowsiness, insomnia, memory loss, mental status changes, nervousness, nightmares, blurred vision, stuffy nose, bronchospasm, wheezing, bradycardia, CHF, pulmonary edema, hypotension, peripheral vasoconstriction, constipation, diarrhea, liver function abnormalities, nausea, vomiting, erectile dysfunction, decreased libido, urinary frequency, rashes, hyperglycemia, hypoglycemia, arthralgia, back pain, joint pain, drug-induced lupus syndrome. Suicidal thoughts, dizziness, fatigue, mood swings, behavioral disturbances, hallucinations, mania, thought disorder, Adultsinsomnia,
19
Rev. 08/21/08
and weight in children; signs of liver injury; and behavior change during therapy.
Atorvastatin/ Lipitor
lipid-lowering agents hmg coa reductase inhibitors
Atovaquone/ Mepron
Antiprotozoals
Atracurium/ Tracrium
neuromuscular blocking agents nondepolarizing
Atropine/ Atro-Pen
antiarrhythmics anticholinergics antimuscarinics
Obtain a diet history, especially with regard to fat consumption. Evaluate serum cholesterol and triglyceride levels before initiating, after 24 wk of therapy, and periodically thereafter. Monitor liver function tests, including AST, prior to, at 12 wk after initiation of therapy, or after dose elevation, and then every 6 mo. If patient develops muscle tenderness during therapy, CPK levels should be monitored. Assess patient for signs of PCP at beginning of and throughout therapy. Monitor hematologic and hepatic functions. Assess respiratory status continuously; ECG, heart rate, and blood pressure; residual muscle weakness and respiratory distress throughout therapy. Neuromuscular response should be monitored with a peripheral nerve stimulator intraoperatively. Assess vital signs and ECG tracings; intake and output ratios in elderly or surgical patients; abdominal distention and auscultate for bowel sounds during therapy.
hypertension, orthostatic hypotension, tachycardia, dyspepsia, severe liver injury (rare), nausea, vomiting, Adultsdry mouth, constipation, rash, urticaria, Adultsdysmenorrhea, ejaculatory problems, libido, erectile dysfunction, urinary hesitation, urinary retention, decreased appetite, weight/growth loss, allergic reactions including angioneurotic edema. Dizziness, headache, insomnia, weakness, rhinitis, bronchitis, chest pain, peripheral edema, abdominal cramps, constipation, diarrhea, flatus, heartburn, altered taste, drug-induced hepatitis, dyspepsia, elevated liver enzymes, nausea, pancreatitis, erectile dysfunction, rashes, pruritus, rhabdomyolysis, arthralgia, arthritis, myalgia, myositis, hypersensitivity reaction including angioneurotic edema. Headache, insomnia, cough, diarrhea, nausea, vomiting, rash, fever.
Bronchospasm, hypotension tachycardia skin flushing, allergic reactions including anaphylaxis.
Attapulgite/Children's Kaopectate, Fowler's Anti-Diarrhea Tablets,
antidiarrheals adsorbents
Assess the frequency and consistency of stools and bowel sounds before and
Drowsiness, confusion, hyperpyrexia, blurred vision, cycloplegia, photophobia, dry eyes, mydriasis, tachycardia, palpitations, arrhythmias, dry mouth, constipation, impaired GI motility, urinary hesitancy, retention, impotency, tachypnea, pulmonary edema, flushing, decreased sweating. Constipation
20
Rev. 08/21/08
Fowler's attapulgite oral suspension, Kaopectate, Kaopectate Extra Strength Auranofin/ Ridaura
throughout course of therapy. Assess fluid and electrolyte balance and skin turgor for dehydration. antirheumatics (DMARDs) gold compounds Assess patient's range of motion and degree of swelling and pain in affected joints before and periodically throughout therapy. Assess patient's range of motion and degree of swelling and pain in affected joints before and periodically throughout therapy. Peripheral neuropathy, conjunctivitis, corneal gold deposition, proteinuria,, hematuria, bronchitis, pulmonary fibrosis, pneumonitis, bradycardia, GI bleeding, abdominal pain, cramping, diarrhea, gingivitis, glossitis, metallic taste, stomatitis, anorexia, difficulty swallowing, liver enzymes, dyspepsia, flatulence, nausea, vomiting, dermatitis, rash, alopecia, urticaria, photosensitivity reactions, pruritus, agranulocytosis, aplastic anemia, thrombocytopenia, anemia, eosinophilia, leucopenia, allergic reactions including anaphylaxis, angioedema. Dizziness, headache, neuropathy, syncope, corneal gold deposition, corneal ulcerations, pneumonitis, bradycardia, abdominal pain, cramping, diarrhea, metallic taste, stomatitis, anorexia, difficulty swallowing, druginduced hepatitis, dyspepsia, flatulence, nausea, vomiting, dermatitis, rash, photosensitivity reactions, pruritus, agranulocytosis, aplastic anemia, thrombocytopenia, eosinophilia, leucopenia, allergic reactions including anaphylaxis, angioneurotic edema, nitritoid reactions. Fatigue, hepatotoxicity, constipation, diarrhea, nausea, vomiting, nephrotoxicity, renal tubular acidosis, ecchymosis, hypokalemia, anemia, neutropenia, thrombocytopenia, injection site erythema, allergic reactions including anaphylaxis, fever. Dizziness, sedation, tinnitus, thickened bronchial secretions, hypertension, epigastric
Aurothioglucose/Solga nol
antirheumatics (DMARDs) gold compounds
Assess patient's range of motion and degree of swelling and pain in affected joints before and periodically throughout therapy. Monitor patient for nitritoid reaction that may occur immediately to 10 min after injection. Monitor renal, hepatic, and hematologic function and urinalysis before and periodically during therapy. Monitor CBC and platelets before every other injection or every 24 wk.
Azacitidine/ Vidaza
antineoplastics nucleoside analogues
Azatadine/ Optimine
allergy, cold and cough remedies antihistamines
Monitor for bone marrow depression; bleeding; nausea and vomiting; fatigue, dyspnea, and orthostatic hypotension; and signs of anaphylaxis during therapy. Monitor CBC with differential and platelet count prior to each dosing cycle. Assess allergy symptoms; lung sounds and character of bronchial secretions prior
21
Rev. 08/21/08
to and periodically throughout therapy.
Azathioprine/ Azasan, Imuran
immunosuppressan ts purine antagonists
Azelastine/ Astelin
allergy, cold and cough remedies antihistamines
Assess for infection: vital signs, sputum, urine, stool, WBC; intake and output and daily weight; range of motion; degree of swelling, pain, and strength in affected joints; and ability to perform activities of daily living before and periodically during therapy. Monitor renal, hepatic, and hematologic functions before beginning therapy, weekly during the 1st mo, bimonthly for the next 23 mo, and monthly thereafter. Assess allergy symptoms, lung sounds and character of bronchial secretions before and periodically throughout therapy.
distress, vomiting, early menses, urinary hesitancy, urinary retention, sweating, anemia, thrombocytopenia. Retinopathy, pulmonary edema, anorexia, hepatotoxicity, nausea, vomiting, diarrhea, mucositis, pancreatitis, alopecia, rash, anemia, leukopenia, pancytopenia, thrombocytopenia, arthralgia, serum sickness, chills, fever, Raynaud's phenomenon, retinopathy.
Azithromycin/ Zmax, Zithromax
agents atypical mycobacterium anti-infectives macrolides
Assess patient for infection; signs and symptoms of anaphylaxis beginning of and throughout therapy.
Aztreonam/ Azactam
anti-infectives monobactams
Assess patient for infection; determine previous use of and reactions to penicillins and cephalosporins; signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Drowsiness, dizziness, dysesthesia, fatigue, headache, epistaxis, nasal burning, pharyngitis, sinusitis, sneezing, bitter taste, dry mouth, nausea, weight gain, myalgia. Dizziness, seizures, drowsiness, fatigue, headache, chest pain, hypotension, palpitations, QT prolongation (rare), pseudomembranous colitis, abdominal pain, diarrhea, nausea, cholestatic jaundice, elevated liver enzymes, dyspepsia, flatulence, melena, oral candidiasis, nephritis, vaginitis, anemia, leukopenia, thrombocytopenia, photosensitivity, StevensJohnson syndrome, rashes, ototoxicity, hyperkalemia, angioedema. Seizures, pseudomembranous colitis, altered taste, diarrhea, nausea, vomiting, rash, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
Assess muscle spasticity before and periodically
be to
Common Side Effects
Baclofen
Anti-spasticity agents
Dizziness, drowsiness, fatigue, weakness, nausea.
22
Rev. 08/21/08
Balsalazide
gastrointestinal anti-inflammatories
Basiliximab
immunosuppressan ts
during therapy. Observe patient for drowsiness, dizziness, or ataxia. May be alleviated by a change in dose. Assess abdominal pain and frequency, quantity, and consistency of stools at the beginning of and throughout therapy. Assess patient for allergy to Salicylates. May cause elevated AST, ALT, serum alkaline phosphatase, gamma glutamyl transpepsidase (GGT), LDH, and bilirubin. Monitor for signs of anaphylactic or hypersensitivity reactions and infection prior to and during therapy.
Hepatotoxicity, abdominal pain, diarrhea.
Beclomethasone
Anti-inflammatories steroidal corticosteroids
Monitor respiratory status and lung sounds. Pulmonary function tests may be assessed periodically during and for several months following a transfer from systemic to inhalation corticosteroids. Assess patients changing from systemic corticosteroids to inhalation corticosteroids for signs of adrenal insufficiency; and withdrawal symptoms during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic therapy. Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing.
Heart failure, hypersensitivity reactions including anaphylaxis, dizziness, headache, insomnia, weakness, coughing, edema, hypertension, abdominal pain, constipation, diarrhea, dyspepsia, moniliasis, nausea, vomiting, acne, wound complications, hyperglycemia, hypoglycemia, acidosis, hypercholesterolemia, hyperkalemia, hyperuricemia, hypocalcemia, hypokalemia, hypophosphatemia, back pain, leg pain, tremor, infection, weight gain. Headache, cataracts, dysphonia, oropharyngeal fungal infections, pharyngitis, rhinitis, sinusitis, bronchospasm, cough, wheezing, adrenal suppression, decreased growth (children), back pain.
Beclomethasone (nasal)
anti inflammatories steroidal corticosteroids
Dizziness, headache, epistaxis, nasal irritation, nasal stuffiness, rhinorrhea, sneezing, tearing eyes,
23
Rev. 08/21/08
Patients on long-term therapy should have periodic otolaryngologic examinations to monitor nasal mucosa and passages for infection or ulceration. Growth rate in children receiving chronic therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic therapy. Benazepril/Lotensin antihypertensives ace inhibitors Monitor BP, pulse, and signs of angioedema. Monitor renal function.
nausea, adrenal suppression (increased dose, long-term therapy only), decreased growth (children).
Bendamustine
anti-neoplastics
Benzocaine
anesthetics local
topical
Benzonatate/ Tessalon
allergy, cold and cough remedies antitussives (local anesthetic)
Monitor for bone marrow depression, bleeding, symptoms of infusion reactions, tumor lysis syndrome, skin reactions, intake and output, appetite, and nutritional intake, nausea and vomiting prior to and throughout therapy. Monitor CBC with differential and platelet count before and during therapy. Monitor blood chemistry, especially serum potassium and uric acid before and periodically during therapy. Assess type, location, and intensity of pain before and a few minutes after administration of anesthetic. Assess integrity of involved skin and mucous membranes before and periodically throughout course of therapy. Assess frequency and nature of cough, lung sounds, and amount and type of sputum produced.
Dizziness, drowsiness, fatigue, headache, cough, hypotension, nausea, impaired renal function, rashes, hyperkalemia, and angioedema. Fatigue, weakness, cough, nausea, vomiting, diarrhea, skin reactions, anemia, leucopenia, neutropenia, thrombocytopenia, hyperuricemia, tumor lysis syndrome, allergic reactions including anaphylaxis, fever, infusion reactions.
Allergic reactions including anaphylaxis. Mucosal usedecreased or absent gag reflex. Topical useburning, edema, irritation, stinging, tenderness, urticaria.
Benztropine
anti-parkinson agents
Assess parkinsonian and extrapyramidal symptoms; bowel function; constipation, abdominal
Headache, mild dizziness, sedation, burning sensation in eyes, nasal congestion, constipation, GI upset, nausea, pruritus, skin eruptions, chest numbness, chilly sensation, hypersensitivity reactions. Confusion, depression, dizziness, hallucinations, headache, sedation, weakness, blurred vision, dry
24
Rev. 08/21/08
Beractant
anti rds agents pulmonary surfactants
Betamethasone (systemic)
Anti-inflammatories steroidal corticosteroids
pain, distention, or absence of bowel sounds; intake and output ratios; urinary retention; and patients with mental illness before and throughout therapy. Monitor pulse and blood pressure closely and maintain bedrest for 1 hr after administration. Monitor ECG, heart rate, color, chest expansion, facial expression, transcutaneous oxygen saturation, and endotracheal tube patency continuously during dosing. Continuous bedside monitoring should continue for at least 30 min after dosing. Monitor ABGs frequently to prevent hyperoxia or hypocarbia. Assess patient for signs of adrenal insufficiency, intake and output ratios and daily weights, peripheral edema, steady weight gain, rales/crackles, or dyspnea before and periodically throughout therapy. Monitor serum electrolytes and glucose. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal axis suppression in systemic and chronic topical therapy. Assess affected skin before and daily during therapy. Note degree of inflammation and pruritus. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected. Monitor blood pressure, ECG, and pulse, intake and output ratios and daily weights, signs and symptoms of congestive heart failure, frequency and characteristics of angina before and periodically during therapy.
eyes, mydriasis, arrhythmias, hypotension, palpitations, tachycardia, constipation, dry mouth, ileus, nausea, hesitancy, urinary retention, decreased sweating.
Oxygen desaturation and transient bradycardia.
Betamethasone (topical)
Anti-inflammatories steroidal corticosteroids
Betaxolol
antihypertensives beta blockers
Depression, euphoria, hypertension, peptic ulceration, anorexia, nausea, vomiting, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, fluid retention, hypokalemia, hypokalemic alkalosis, thromboembolism, thrombophlebitis, weight gain, weight loss, muscle wasting, osteoporosis, aseptic necrosis of joints, muscle pain, cushingoid appearance, increased susceptibility to infection. Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression Fatigue, weakness, erectile dysfunction, bradycardia, CHF, pulmonary edema, anxiety, depression, back pain, joint pain, dizziness, constipation, diarrhea, liver function abnormalities, drug-induced lupus syndrome, rashes, insomnia, wheezing.
25
Rev. 08/21/08
Bethanechol
urinary tract stimulant cholinergics
Bevacizumab
antineoplastics monoclonal antibodies
Monitor blood pressure, pulse, and respirations before administering and for at least 1 hr after subcut administration. Monitor intake and output ratios. Palpate abdomen for bladder distention. Assess for signs of GI perforation, fistula formation, wound dehiscence, signs of hemorrhage, signs of CHF, thromboembolic events, infusion reactions, and signs of RPLS before and during therapy. Monitor BP every 23 wk during therapy. Monitor serial urinalysis for proteinuria during therapy. Assess patient for adverse GI effects. Diarrhea is the most common cause of discontinuation of therapy. Monitor serum prostatespecific antigen (PSA) periodically to determine response to therapy. Monitor liver function tests before and periodically during therapy. Monitor intraocular pressure in patients with a history of increased intraocular pressure or who are using prostaglandin analogs for intraocular pressure reduction concurrently. Assess parkinsonian and extrapyramidal symptoms; bowel function; intake and output ratios and assess patient for urinary retention; pulse and blood pressure; and mental illness are at risk of developing exaggerated symptoms of their disorder during therapy. Assess patient for abdominal distention, presence of bowel sounds, and normal pattern of bowel function; color, consistency, and amount of stool produced Assess the frequency and consistency of stools and
Bicalutamide
antineoplastics antiandrogens
Headache, miosis, urgency, lacrimation, bronchospasm, heart block, flushing, sweating, vomiting, syncope/cardiac arrest, bradycardia, abdominal discomfort, diarrhea, nausea, salivation. Reversible posterior leukoencephalopathy syndrome (RPLS), arterial thromboembolic events, CHF, hypertension, hypotension, hemoptysis, nongastrointestinal fistulas, nasal septum perforation, GI perforation, nephrotic syndrome, proteinuria, bleeding, wound dehiscence, impaired wound healing, infusion reactions. Weakness, constipation, diarrhea, nausea, nocturia, urinary tract infections, alopecia, rashes, sweating, breast pain, gynecomastia, anemia, hyperglycemia, weight loss, back pain, pelvic pain, bone pain, paresthesia, generalized pain, hot flashes, flu-like syndrome, infection. Conjunctival hyperemia, eye pruritus, hyperpigmentation of eyelids, macular edema, permanent pigmentation of the iris.
Bimatoprost (lash, ophthalmic)
hair regrowth stimulants prostaglandins
Biperiden/ Akineton
antiparkinson agents anticholinergics
Confusion, depression, dizziness, hallucinations, headache, sedation, weakness, blurred vision, dry eyes, mydriasis, arrhythmias, hypotension, palpitations, tachycardia, constipation, dry mouth, ileus, nausea, hesitancy, urinary retention, decreased sweating. abdominal cramps, nausea,
Bisacodyl
stimulant laxatives; laxative
Bismuth subsalicylate/ Bismatrol, Bismed,
antidiarrheals antiulcer agents
Constipation, gray-black stools, impaction (infants,
26
Rev. 08/21/08
Kaopectate, Kapectolin, Kao-Tin, K-Pek, Peptic Relief, Pepto-Bismol, Pink Bismuth
adsorbents
Bisoprolol
antihypertensives beta blockers
bowel sounds before and throughout course of therapy. Assess fluid and electrolyte balance and skin turgor for dehydration. Assess for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate. Monitor blood pressure, ECG, and pulse, intake and output ratios and daily weights, for signs and symptoms of CHF frequently during dosage adjustment period and periodically throughout therapy. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; paradoxical bronchospasm before administration and during peak of medication. Observe patient for drug tolerance and rebound bronchospasm. Symptoms of overdose include persistent agitation, chest pain or discomfort, decreased blood pressure, dizziness, hyperglycemia, hypokalemia, seizures, tachyarrhythmias, persistent trembling, and vomiting. Assess for bleeding and vital signs before, during, and throughout therapy. Assess hemoglobin, hematocrit, and platelet count prior to bivalirudin therapy and periodically during therapy. Monitor ACT periodically in patients with renal dysfunction. Assess frequency and severity of menopausal symptoms; blood pressure; nausea and vomiting; history of seizures, liver disease, and alcohol intake; irregular periods for pregnancy prior to taking this drug because large doses of black cohosh may induce a miscarriage. Assess for fever and chills. May occur 36 hr after
debilitated patients).
Bitolterol/ Tornalate
bronchodilators adrenergics
Fatigue, weakness, bradycardia, CHF, pulmonary edema, erectile dysfunction, decreased libido, urinary frequency, rashes, hyperglycemia, hypoglycemia, arthralgia, back pain, joint pain, drug-induced lupus syndrome. Nervousness, restlessness, tremor, headache, insomnia, light-headedness, paradoxical bronchospasm, chest pain, palpatations, tachycardia, arrhythmias, hypertension, nausea, vomiting, hyperglycemia, hypokalemia, tremor.
Bivalirudin
anticoagulants thrombin inhibitors
Headache, anxiety, insomnia, nervousness, hypotension, bradycardia, hypertension, nausea, abdominal pain, dyspepsia, vomiting, bleeding, injection site pain, back pain, pain, fever, pelvic pain.
Black cohosh
Seizures, headache, dizziness, GI upset, rash, weight gain, cramping.
Bleomycin
antineoplastics antitumor
Aggressive behavior, disorientation, weakness,
27
Rev. 08/21/08
antibiotics
Bortezomib
anti-neoplastics proteasome inhibitors
Bosentan
Vasodilators endothelin receptor antagonists
administration and last 412 hr. Monitor vital signs, anaphylactic and idiosyncratic reactions, respiratory status for dyspnea and rales/crackles, nausea, vomiting, and appetite, and weigh weekly before and frequently during therapy. Monitor CBC before and periodically during therapy. Monitor baseline and periodic renal and hepatic function. Monitor vital signs frequently, GI adverse effects, signs and symptoms of tumor lysis syndrome before and during therapy. Monitor CBC and platelet count frequently during therapy. Monitor blood glucose levels closely in patients taking oral hypoglycemic agents; may require adjustment of antidiabetic agent dose Assess for signs and symptoms of primary pulmonary hypertension prior to and periodically during therapy. Monitor serum AST, ALT, and bilirubin prior to and monthly during treatment. If AST and ALT are >3 and <=5 times the upper limit of normal, confirm level with a second test. If confirmed, reduce dose or interrupt therapy and monitor AST and ALT every 2 wk. Once AST and ALT return to normal levels, reintroduce therapy at starting dose and recheck AST and ALT levels within 3 days. If AST and ALT levels are >8 times the upper limit of normal if clinical symptoms of liver injury occur, or if bilirubin levels are >= 2 times the upper limit of normal, discontinue therapy permanently. Monitor hemoglobin and hematocrit levels 1 and 3 mo after initiation of therapy and
pulmonary fibrosis, pneumonitis, hypotension, peripheral vasoconstriction, anorexia, nausea, stomatitis, vomiting, hyperpigmentation, mucocutaneous toxicity, alopecia, erythema, rashes, urticaria, vesiculation, anemia, leukopenia, thrombocytopenia, pain at tumor site, phlebitis at IV site, weight loss, anaphylactoid reactions, chills, fever. Fatigue, malaise, weakness, dizziness, syncope, blurred vision, diplopia, hypotension, CHF, pneumonia, anorexia, constipation, diarrhea, nausea, vomiting, bleeding, anemia, neutropenia, thrombocytopenia, peripheral neuropathy, fever, tumor lysis syndrome.
Headache, fatigue, nasopharyngitis, edema, hypotension, palpitations, hepatotoxicity, dyspepsia, flushing, pruritus, anemia.
28
Rev. 08/21/08
every 3 mo thereafter. Botulism immune globulin/BabyBIG vaccines/immunizin g agents immune globulins Monitor vital signs continuously during infusion. Monitor urine output and signs of aseptic meningitis syndrome (AMS) during therapy. Assess allergy symptoms, lung sounds and character of bronchial secretions; symptoms of allergic transfusion reaction or anaphylaxis; sweating, hypotension, dizziness, drowsiness, or hypersensitivity reactions before and periodically during therapy. Assess patient for allergy to ergot derivatives. Monitor blood pressure, restlessness or desire to keep moving, rigidity, tremors, pill rolling, masklike face, shuffling gait, muscle spasms, twisting motions, difficulty speaking or swallowing, loss of balance control, fever, respiratory distress, tachycardia, convulsions, diaphoresis, hypertension, hypotension, pallor, tiredness before and throughout therapy. Physical examination including ring size, heel pad thickness, and soft-tissue volume should be assessed throughout therapy. Measure serum prolactin concentrations and anterior pituitary function before female infertility therapy. Monitor serum growth hormone and insulin-like growth factor (IGF-I) concentrations periodically during acromegaly therapy. Measure serum prolactin concentrations monthly during initial therapy and twice yearly during maintenance therapy to determine effectiveness of hyperprolactinemia therapy. Monitor respiratory status and lung sounds. Pulmonary Rash and infusion reactions.
Brompheniramine/ Bromfenac, Dimetapp Allergy, Nasahist B
allergy, cold and cough remedies antihistamines
Drowsiness, sedation, dizziness, excitation (in children), blurred vision, hypertension, arrhythmias, hypotension, palpitations, dry mouth, constipation, obstruction, retention, urinary hesitancy, sweating, hypersensitivity reaction (IV use). Dizziness, confusion, drowsiness, hallucinations, headache, insomnia, nightmares, burning eyes, nasal stuffiness, visual disturbances, effusions, pulmonary infiltrates, MI, hypotension, nausea, abdominal pain, anorexia, dry mouth, metallic taste, vomiting, urticaria, leg cramps, digital vasospasm (acromegaly only).
Bromocriptine
anti-parkinson agents dopamine agonists
Budesonide
anti inflammatories steroidal
Headache, rash, otitis media, dysphonia, epistaxis,
29
Rev. 08/21/08
corticosteroids
Budesonide (nasal)
anti inflammatories steroidal corticosteroids
Budesonide (oral)
gastroinestinal anti inflammatories corticosteroids
function tests may be assessed periodically during and for several months following a transfer from systemic to inhalation corticosteroids. Assess patients changing from systemic corticosteroids to inhalation corticosteroids for signs of adrenal insufficiency during initial therapy and periods of stress. Monitor for withdrawal symptoms during withdrawal from oral corticosteroids. Monitor growth rates in children receiving chronic therapy. Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing. Patients on long-term therapy should have periodic otolaryngologic examinations to monitor nasal mucosa and passages for infection or ulceration. Monitor growth rate in children receiving chronic therapy. Assess signs of Crohn's disease (diarrhea, crampy abdominal pain, fever, bleeding from rectum) during therapy.
oropharyngeal fungal infections, pharyngitis, rhinitis, sinusitis, bronchospasm, cough, abdominal pain, diarrhea, dyspepsia, gastroenteritis, nausea, vomiting, adrenal suppression (high dose, long-term therapy only), decreased growth (children), weight gain, back pain, flu-like syndrome.
Epistaxis, nasal burning, nasal irritation, nasopharyngeal fungal infection, pharyngitis, sneezing, dry mouth, dyspepsia, adrenal suppression (increased dose, long-term therapy only), decreased growth (children), bronchospasm, cough.
Bumetanide
diuretics loop diuretics
Assess fluid status, blood pressure and pulse, tinnitus and hearing loss, allergy to sulfonamides before and during therapy. Monitor daily weight, intake and output ratios, amount and location of edema, lung sounds, skin turgor, and mucous membranes. Assess patients receiving digoxin for anorexia, nausea, vomiting, muscle cramps, paresthesia, and confusion risk of digoxin toxicity due to potassium-depleting effect of diuretic. Diuretic
Headache, easy bruising, acne, nausea, eczema, flushing, increased sweating, striae, adrenal suppression, hypokalemia, leukocytosis, weight gain, hyperkinesia, paresthesia, tremor, back pain, cramps, increased arthritis, myalgia, infection, cushingoid appearance, flu-like syndrome. Dizziness, encephalopathy, headache, hearing loss, tinnitus, hypotension, diarrhea, dry mouth, nausea, vomiting, excessive urination, photosensitivity, pruritis, rash, hyperglycemia, hyperuricemia, dehydration, hypocalcemia, hypochloremia, hypokalemia, hypomagnesemia, hyponatremia, hypovolemia, metabolic alkalosis, arthralgia, muscle cramps, myalgia, increased BUN.
30
Rev. 08/21/08
Bupivacaine
epidural local anesthetics anesthetics topical local
use is associated with increased risk for falls in older adults. Monitor electrolytes, renal and hepatic function, serum glucose, and uric acid levels before and periodically during therapy. Assess for systemic toxicity, BP, HR, and respiratory rate continuously while patient is receiving this medication. Monitor for return of sensation after procedure.
Buprenorphine
opioid analgesics opioid agonists antagonists
Bupropion
antidepressants smoking deterrents aminoketones
Busulfan/ Busulfex, Myleran
antineoplastics alkylating agents
Assess type, location, and intensity of pain before and 1 hr after IM and 5 min (peak) after IV administration. Assess level of consciousness, blood pressure, pulse, and respirations, previous analgesic history, signs and symptoms of opioid withdrawal before and during therapy. Monitor liver function tests prior to and periodically during therapy for opioid dependence. Monitor mood changes, mental status and mood changes during initial few months of therapy and during dose changes. Monitor hepatic and renal function closely in patients with kidney or liver impairment to prevent serum and tissue bupropion concentrations. Monitor for bone marrow depression; bleeding; signs of infection; fatigue, dyspnea, and orthostatic hypotension; intake and output ratios and daily weights; symptoms of gout; pulmonary fibrosis periodically during and after therapy. Monitor CBC with differential and platelet count before and weekly during therapy.
Seizures, anxiety, dizziness, headache, irritability, blurred vision, tinnitus, cardiovascular collapse, arrhythmias, bradycardia, hypotension, nausea, vomiting, urinary retention, pruritus, metabolic acidosis, circumoral tingling/ numbness, tremor, allergic reactions, fever. Confusion, dysphoria, hallucinations, sedation, dizziness, euphoria, floating feeling, headache, unusual dreams, blurred vision, diplopia, miosis (high doses), respiratory depression, hypertension, hypotension, palpitations, nausea, constipation, dry mouth, ileus, vomiting, urinary retention, sweating, clammy feeling, physical dependence, psychological dependence, tolerance. Seizures, suicidal thoughts, agitation, headache, insomnia, mania, psychoses, dry mouth, nausea, vomiting, change in appetite, weight gain, weight loss, photosensitivity, hyperglycemia, hypoglycemia, syndrome of inappropriate ADH secretion, tremor.
Seizures, cerebral hemorrhage/ coma, anxiety, confusion, depression, dizziness, headache, weakness, epistaxis, pharyngitis, pulmonary fibrosis, cardiac tamponade, chest pain, hypotension, tachycardia, thrombosis, abdominal enlargement, anorexia, constipation, diarrhea, dry mouth, hematemesis, nausea, rectal discomfort, vomiting, oliguria,
31
Rev. 08/21/08
Butalbital, acetaminophen
nonopioid analgesics (combination with barbiturate) barbiturates
Assess type, location, and intensity of pain before and 60 min following administration. Prolonged use may lead to physical and psychological dependence and tolerance.
Butenafine
anti-fungal (topical)
Butoconazole
anti-fungal (vaginal)
Butorphanol
opioid analgesics opioid agonists antagonists
Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate sensitization and warrant discontinuation of medication. Assess type, location, and intensity of pain before and 3060 min after IM, 5 min after IV, and 6090 min after intranasal administration. Assess blood pressure, pulse, and respirations before and periodically during administration. Assess previous analgesic history.
itching, rashes, sterility, hypokalemia, hypomagnesemia, hypophosphatemia, bone marrow depression, inflammation/pain at injection site, hyperglycemia, arthralgia, myalgia, allergic reactions, chills, fever, infection. Drowsiness, confusion, delirium, depression, dizziness, excitation, headache (with chronic use), irritability, lethargy, nervousness, numbness, tingling, earache, nasal congestion, tinnitus, respiratory depression, tachycardia, constipation, dry mouth, dysphagia, flatulence, heartburn, dermatitis, pruritis, rash, sweating, leg pain, muscle weakness, fever, physical dependence, psychological dependence, tolerance. Burning, itching, local hypersensitivity reactions, redness, stinging.
Itching, pelvic pain, soreness, swelling, vulvovaginal burning.
Confusion, dysphoria, hallucinations, sedation, euphoria, floating feeling, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypertension, hypotension, palpitations, nausea, constipation, dry mouth, ileus, vomiting, urinary retention, sweating, clammy feeling, physical dependence, psychological dependence, tolerance.
32
Rev. 08/21/08
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
C1 inhibitor (human)/ Cinryze
antiangioedema agents proteinase inhibitors
Cabergoline/ Dostinex
Anti hyperprolactinemic dopamine agonists
Assess for signs and symptoms of hypersensitivity reactions during or after injection. Monitor patients with known risk factors for thrombotic events. Monitor blood pressure, ECG, parkinsons disease symptoms. Serum prolactin concentrations.
Headache, rash, hypersensitivity reactions including anaphylaxis.
Caffeine citrate/ Cafcit
central nervous system stimulants respiratory stimulants
Calcipotriene/ Dovonex
antipsoriatics synthetic vitamin d3 analogues
Assess respiratory status and signs of necrotizing enterocolitis frequently throughout therapy. Monitor serum caffeine levels before and periodically during therapy in infants previously treated with theophylline or in infants whose mothers consumed caffeine before delivery. Monitor serum glucose levels. Assess skin before and periodically during therapy. Monitor serum calcium concentrations.
Dizziness, headache, depression, drowsiness, fatigue, nervousness, vertigo, weakness, pulmonary fibrosis, pleural effusion, abnormal vision, valvular disorders, postural hypotension, hot flashes, constipation, nausea, abdominal pain, dyspepsia, vomiting, dysmenorrheal, breast pain, paresthesia. Insomnia, irritability, jitteriness, restlessness, tachycardia, necrotizing enterocolitis, feeding intolerance, gastritis, GI bleeding, increased urine output, dry skin, rash, skin breakdown, hypoglycemia, hyperglycemia, muscle tremors, twitches.
Calcitonin (rdna)/ Fortical
hypocalcemics hormones
Observe patient for signs of hypersensitivity and hypocalcemic tetany. Assess nasal mucosa, septum, turbinates, and mucosal blood vessels. Monitor serum calcium and alkaline phosphatase.
Calcitonin (salmon)/ Miacalcin
hypocalcemics hormones
Observe patient for signs of hypersensitivity and hypocalcemic tetany. Assess nasal mucosa, septum, turbinates, and mucosal blood vessels. Monitor serum calcium and alkaline
Burning, itching, skin irritation, dry skin, erythema, peeling, rash, worsening/spreading of psoriatic lesions, hypercalcemia. Nasal onlyheadaches, rhinitis, epistaxis, nasal irritation, arthralgia, back pain. IM, subcutnausea, vomiting, urinary frequency. Rashes, injection site reactions, allergic reactions including anaphylaxis, facial flushing, swelling. Nasal onlyheadaches, rhinitis, epistaxis, nasal irritation, arthralgia, back pain. IM, subcutnausea, vomiting, urinary frequency. Rashes, injection site
33
Rev. 08/21/08
phosphatase.
Calcitriol/ 1,25 Dihydroxycholecalcifer ol, Calcijex, Rocaltrol
vitamins fat soluble vitamins
Assess patient for bone pain and weakness, height and weight, evidence of hypocalcemia. Serum calcium and phosphorus concentrations should be drawn twice weekly during initial therapy.
Calcium acetate/PhosLo
mineral electrolyte replacements supplements
Calcium carbonate/ Alka-Mints, Amitone, BioCal, Calcarb, CalciChew, Calciday, Calcilac, Calci-Mix, CalPlus, Caltrate, Chooz, Dicarbosil, Equilet, Gencalc, Liqui-Cal, Liquid Cal-600, Maalox Antacid Caplets, Mallamint, NephroCalci, Os-Cal, Oysco, Oyst-Cal, Oystercal, Rolaids Calcium Rich, Surpass, Surpass Extra Strength, Titralac, Tums, Tums E-X Calcium chloride
mineral electrolyte replacements supplements
Observe patient closely for symptoms of hypocalcemia. Assess patient for nausea, vomiting, anorexia, thirst, severe constipation, paralytic ileus, and bradycardia. Observe patient closely for symptoms of hypocalcemia, heartburn, indigestion, and abdominal pain. Monitor patient on digitalis glycosides for signs of toxicity. Monitor serum calcium or ionized calcium, chloride, sodium, potassium, magnesium, albumin, and parathyroid hormone (PTH) concentrations before and periodically during therapy.
reactions, allergic reactions including anaphylaxis, facial flushing, swelling. Headache, somnolence, weakness, conjunctivitis, photophobia, rhinorrhea, arrhythmias, hypertension, abdominal pain, anorexia, constipation, dry mouth, liver function test elevation, metallic taste, nausea, pancreatitis, polydipsia, vomiting, weight loss, albuminuria, azotemia, decreased libido, nocturia, polyuria, pruritus, hypercalcemia, pain at injection site, hyperthermia, bone pain, metastatic calcification, muscle pain, allergic reactions (pruritis, rash, urticaria). Headache, tingling. arrhythmias, bradycardia. constipation, nausea, vomiting calculi, hypercalciuria. phlebitis (IV only).
Headache, tingling, arrhythmias, bradycardia, constipation, nausea, vomiting, calculi, hypercalciuria.
mineral electrolyte replacements supplements
Observe patient closely for symptoms of hypocalcemia, blood pressure, pulse, and ECG, IV site for patency. Monitor patient on digitalis glycosides for signs of toxicity. Monitor serum calcium or ionized calcium, chloride, sodium, potassium,
Headache, tingling, syncope, cardiac arrest, arrhythmias, bradycardia, constipation, nausea, vomiting, calculi, hypercalciuria, phlebitis.
34
Rev. 08/21/08
Calcium citrate/ CalCitrate 250, Citrical, Citrical Liquitab
mineral electrolyte replacements supplements
Calcium glubionate
mineral electrolyte replacements supplements
Calcium gluconate/ Kalcinate
mineral electrolyte replacements supplements
Calcium lactate/ CalLac
mineral electrolyte replacements supplements
Candesartan/ Atacand
antihypertensives angiotensin ii receptor antagonists
magnesium, albumin, and parathyroid hormone (PTH) concentrations. Observe patient closely for symptoms of hypocalcemia and digitalis glycosides for signs of toxicity before and during therapy. Monitor serum calcium or ionized calcium, chloride, sodium, potassium, magnesium, albumin, and parathyroid hormone (PTH) concentrations before and periodically during therapy for treatment of hypocalcemia. Observe patient closely for symptoms of hypocalcemia. Monitor patient on digitalis glycosides for signs of toxicity. Monitor serum calcium or ionized calcium, chloride, sodium, potassium, magnesium, albumin, and parathyroid hormone (PTH) concentrations. Observe patient closely for symptoms of hypocalcemia, blood pressure, pulse, and ECG, IV site for patency. Monitor patient on digitalis glycosides for signs of toxicity. Observe patient closely for symptoms of hypocalcemia. Monitor patient on digitalis glycosides for signs of toxicity. Assess blood pressure (lying, sitting, standing) and pulse, signs of angioedema, daily weight and assess patient routinely for resolution of fluid overload. Assess mucous membranes, number and consistency of stools, and frequency of vomiting, signs of infection, symptoms of toxicity, and hand-and-foot syndrome. Monitor hepatic, renal, and hematologic function. Monitor PT or INR frequently.
Headache, tingling, arrhythmias, bradycardia, constipation, nausea, vomiting, calculi, hypercalciuria.
Headache, tingling, arrhythmias, bradycardia, constipation, nausea, vomiting, calculi, hypercalciuria.
Headache, tingling, syncope, cardiac arrest, arrhythmias, bradycardia, constipation, nausea, vomiting, calculi, hypercalciuria, phlebitis.
Capecitabine/ Xeloda
antineoplastics antimetabolites
Headache, tingling, arrhythmias, bradycardia, constipation, nausea, vomiting, calculi, hypercalciuria. Dizziness, fatigue, headache, hypotension, chest pain, edema, hyperkalemia, abdominal pain, diarrhea, nausea, impaired renal function, arthralgia, back pain, angioedema. Fatigue, headache, dizziness, insomnia, eye irritation, epistaxis, rhinorrhea, edema, chest pain, diarrhea, necrotizing enterocolitis, abdominal pain, anorexia, constipation, dysgeusia, hyperbilirubinemia, nausea, stomatitis, vomiting, dyspepsia, xerostomia, dermatitis, hand-and-foot syndrome, nail disorder,
35
Rev. 08/21/08
Capsaicin/ Capsin, Capzasin-P, Dolorac, No Pain-HP, Pain Doctor, Pain-X, R-Gel, RidaPainHP, Zostrix, Zostrix-HP Captopril/Capoten
nonopioid analgesics (topical)
Assess pain intensity and location before and periodically throughout therapy.
alopecia, erythema, rashes, dehydration, anemia, leukopenia, arthralgia, myalgia, thrombocytopenia, peripheral neuropathy, cough, dyspnea, fever. Cough and transient burning.
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor weight and assess patient routinely for resolution of fluid overload.
Carbamazepine/ Carbatrol, Epitol, Equetro, Tegretol, Tegretol-XR, Teril
anticonvulsants mood stabilizers
Assess for facial pain, seizures, mental status, and changes in skin condition before and periodically during therapy. Monitor CBC, including platelet count, reticulocyte count, and serum iron, Liver function tests, urinalysis, and BUN, serum ionized calcium levels, ECG and serum electrolytes weekly during the first 2 mo and yearly thereafter for evidence of potentially fatal blood cell abnormalities.
Carbidopa/levodopa// Parcopa, Sinemet, Sinemet CR
antiparkinson agents dopamine agonists
Assess parkinsonian symptoms, blood pressure and pulse frequently during therapy. Monitor hepatic and renal function and CBC periodically in patients on long-term therapy.
dizziness, fatigue, headache, insomnia, cough, hypotension, chest pain, palpitations, tachycardia, taste disturbances, abdominal pain, anorexia, constipation, diarrhea, nausea, vomiting, proteinuria, impaired renal function, angioedema, rashes, pruritis, hyperkalemia, agranulocytosis, neutropenia, fever. Ataxia, drowsiness, fatigue, psychosis, sedation, suicidal behavior or ideation, vertigo, blurred vision, nystagmus, corneal opacities, pneumonitis, CHF, edema, hypertension, hypotension, syncope, hepatitis, pancreatitis, weight gain, hesitancy, urinary retention, chills, photosensitivity, rashes, stevens-johnson syndrome, toxic epidermal necrolysis, urticaria, syndrome of inappropriate antidiuretic hormone (SIADH), fever, hyponatremia, aplastic anemia, agranulocytosis, thrombocytopenia, eosinophilia, leucopenia, lymphadenopathy, elevated liver enzymes, multi-organ hypersensitivity reactions, hepatic failure (rare). Involuntary movements, anxiety, dizziness, hallucinations, memory loss, psychiatric problems, blurred vision, mydriasis, nausea, vomiting, anorexia, dry mouth, hepatotoxicity, melanoma, hemolytic anemia, leucopenia, darkening of urine
36
Rev. 08/21/08
or sweat. Carboplatin/ Paraplatin antineoplastics alkylating agents Assess for nausea and vomiting; bleeding; neurotoxicity; bone marrow depression; signs of anaphylaxis; and signs of infection. Monitor CBC, differential, and clotting studies before and weekly during therapy. Weakness, ototoxicity, abdominal pain, nausea, vomiting, hypocalcemia, hypokalemia, anemia, hypomagnesemia, hyponatremia, leucopenia, peripheral neuropathy, thrombocytopenia, hyperuricemia, hypersensitivity reactions including anaphylactic-like reactions. dizziness, headache. wheezing, diarrhea, nausea, vomiting, abdominal pain, cramps, uterine rupture, flushing, fever, chills, shivering.
Carboprost/ Hemabate
abortifacients oxytocics prostaglandins
Carisoprodol/ Soma, Vanadom
skeletal muscle relaxants (centrally acting)
Assess for nausea, vomiting, and diarrhea; amount and type of vaginal discharge; temperature, pulse, and BP; frequency, duration, and force of contractions and uterine resting tone. Auscultate breath sounds. Assess patient for pain, muscle stiffness, and range of motion before and periodically throughout therapy.
Carmustine/ BCNU, BiCNU, Gliadel
antineoplastics alkylating agents
Carteolol/ Cartrol
antianginals antihypertensives beta blockers
Monitor vital signs; bone marrow depression; bleeding; respiratory status; intake and output, appetite, and nutritional intake before and frequently during therapy. Monitor CBC with differential and platelet count before and throughout therapy. Monitor blood pressure and pulse, intake and output ratios and daily weight, evidence of fluid overload, angina, and signs of overdose before and during therapy.
Dizziness, drowsiness, agitation, ataxia, depression, headache, insomnia, irritability, syncope, asthma attacks, hypotension, tachycardia, epigastric distress, hiccups, nausea, vomiting, flushing, rashes, eosinophilia, leucopenia, anaphylactic shock, fever, psychological dependence, severe idiosyncratic reaction. Pulmonary fibrosis, pulmonary infiltrates, hepatotoxicity, nausea, vomiting, anorexia, diarrhea, esophagitis, renal failure, alopecia, leucopenia, thrombocytopenia, anemia, pain at IV site.
Fatigue, weakness, anxiety, depression, dizziness, CHF, drowsiness, insomnia, memory loss, mental status changes, nightmares, blurred vision, dry eyes, nasal stuffiness, rashes, bronchospasm, wheezing, bradycardia, pulmonary edema, orthostatic hypotension, peripheral vasoconstriction, itching, constipation, diarrhea, nausea, erectile dysfunction, decreased libido, hyperglycemia,
37
Rev. 08/21/08
Carvedilol/ Coreg, Coreg CR
antihypertensives beta blockers
Monitor blood pressure and pulse frequently during dose adjustment period and periodically during therapy. Monitor intake and output ratios and daily weight, evidence of fluid overload, signs of overdose, orthostatic hypotension before and during therapy.
Caspofungin/ Cancidas
antifungals (systemic) echinocandins
Cefaclor/ Raniclor
anti-infectives second generation cephalosporins
Assess patient for signs and symptoms of fungal infections, and signs of anaphylaxis prior to and periodically during therapy. Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefadroxil/ Duricef
anti-infectives first generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefazolin/ Ancef, Kefzol
anti-infectives first generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefdinir/ Omnicef
anti-infectives third generation
Assess patient for infection, signs and symptoms of
hypoglycemia, arthralgia, back pain, muscle cramps, paresthesia, drug-induced lupus syndrome. Dizziness, fatigue, weakness, anxiety, depression, drowsiness, insomnia, memory loss, mental status changes, nervousness, nightmares, blurred vision, dry eyes, nasal stuffiness, back pain, bronchospasm, wheezing, bradycardia, CHF, pulmonary edema, diarrhea, constipation, nausea, erectile dysfunction, decreased libido, itching, rashes, hyperglycemia, hypoglycemia, arthralgia, muscle cramps, paresthesia, drug-induced lupus syndrome. Headache, diarrhea, nausea, vomiting, flushing, venous irritation at injection site, allergic reactions including anaphylaxis, fever. Seizures (very high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, rashes, urticaria, agranulocytosis, bleeding, eosinophilia, hemolytic anemia, neutropenia, allergic reactions including anaphylaxis and serum sickness, superinfection. Seizures (very high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, dyspepsia, rashes, pruritis, urticaria, agranulocytosis, thrombocytopenia, allergic reactions including anaphylaxis and serum sickness, superinfection. Seizures (high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, cramps, rash, pruritis, urticaria, Stevens-Johnson syndrome, leukopenia, neutropenia, thrombocytopenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis and serum sickness, superinfection. Seizures, headache, rash, pseudomembranous colitis,
38
Rev. 08/21/08
cephalosporins
anaphylaxis at beginning of and throughout therapy.
Cefditoren/ Spectracef
anti-infectives third generation cephalosporins
Assess patient for infection, bowel function, signs and symptoms of anaphylaxis at beginning of and throughout therapy. Monitor prothrombin time and assess patient for bleeding daily in high-risk patients.
Cefepime/ Maxipime
anti-infectives fourth generation cephalosporins
Assess patient for infection, bowel function, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefixime/ Suprax
anti-infectives third generation cephalosporins
Assess patient for infection, bowel function, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefoperazone/ Cefobid
anti-infectives third generation cephalosporins
Cefotaxime/ Claforan
anti-infectives third generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy. Monitor prothrombin time and assess patient for bleeding daily in high-risk patients. Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
diarrhea, vomiting, abdominal pain, nausea, vaginal moniliasis, vaginitis, pruritus, allergic reactions including anaphylaxis. Seizures (high doses), pseudomembranous colitis, headache, diarrhea, abdominal pain, dyspepsia, nausea, vomiting, hematuria, vaginal moniliasis, bleeding, eosinophilia, hemolytic anemia, lymphocytosis, neutropenia, thrombocytosis, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses in patients with renal impairment), neutropenia, pseudomembranous colitis, encephalopathy, headache, diarrhea, nausea, vomiting, rashes, pruritis, urticaria, bleeding, eosinophilia, hemolytic anemia, fever, thrombocytopenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, cramps, rashes, urticaria, bleeding, blood dyscrasias, hemolytic anemia, allergic reactions including anaphylaxis and serum sickness, superinfection. Seizures (high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, rashes, urticaria, bleeding, eosinophilia, neutropenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Seizures (high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, rashes, pruritis, urticaria, agranulocytosis, bleeding, eosinophilia, hemolytic anemia, neutropenia, thrombocytopenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection.
39
Rev. 08/21/08
Cefotetan/ Cefotan
anti-infectives second generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy. Monitor prothrombin time and assess patient for bleeding daily in high-risk patients.
Cefoxitin/ Mefoxin
anti-infectives second generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefpodoxime/ Banan, Vantin
anti-infectives third generation cephalosporins
Assess patient for infection, bowel function, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cefprozil/ Cefzil
anti-infectives second generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Ceftazidime/ Fortaz, Tazicef
anti-infectives third generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Ceftibuten/ Cedax
anti-infectives third generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Seizures (high doses), pseudomembranous colitis, diarrhea, nausea, rashes, urticaria, bleeding, eosinophilia, hemolytic anemia, leukopenia, thrombocytopenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Seizures (high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, rashes, urticaria, bleeding, eosinophilia, hemolytic anemia, leukopenia, thrombocytopenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), headache, abdominal pain, pseudomembranous colitis, diarrhea, nausea, vomiting, rashes, urticaria, vaginal moniliasis, bleeding, blood dyscrasias, hemolytic anemia, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), dizziness, urticaria, pseudomembranous colitis, abdominal pain, diarrhea, nausea, vomiting, rashes, eosinophilia, hemolytic anemia, leucopenia, vaginitis, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses in patients with renal impairment), dizziness, headache, abdominal pain, pseudomembranous colitis, diarrhea, dyspepsia, nausea, vomiting, rashes, urticaria, bleeding, fever, eosinophilia, hemolytic anemia, leukopenia, thrombocytopenia, thrombocytosis allergic reactions including anaphylaxis, superinfection. Seizures (very high doses in patients with renal impairment), dizziness, headache, abdominal pain, pseudomembranous colitis, diarrhea, dyspepsia, nausea, vomiting, rashes, urticaria,
40
Rev. 08/21/08
Ceftizoxime/ Cefizox
anti-infectives third generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Ceftriaxone/ Rocephin
anti-infectives third generation cephalosporins
Assess patient for infection, bowel function, signs and symptoms of anaphylaxis at beginning of and throughout therapy. Assess newborns for jaundice and hyperbilirubinemia.
Cefuroxime/ Ceftin, Zinacef
anti-infectives second generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Celecoxib/ Celebrex
antirheumatics nonsteroidal anti inflammatory agents cox 2 inhibitors
Assess range of motion, degree of swelling, and pain in affected joints before and periodically throughout therapy.
Cephalexin/ Keflex
anti-infectives first generation cephalosporins
Assess patient for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
Cephradine/ Velosef
anti-infectives first generation
Assess patient for infection, signs and symptoms of
bleeding, eosinophilia, hemolytic anemia, leukopenia, thrombocytopenia, thrombocytosis allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, pruritis, rashes, urticaria, bleeding, eosinophilia, hemolytic anemia, fever, leukopenia, neutropenia, thrombocytopenia, thrombocytosis, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), pseudomembranous colitis, diarrhea, cholelithiasis, sludging in the gallbladder, rashes, urticaria, bleeding, eosinophilia, hemolytic anemia, leukopenia, thrombocytosis, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, cramps, rashes, urticaria, diaper dermatitis, eosinophilia, hemolytic anemia, leucopenia, bleeding, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis, superinfection. Dizziness, headache, insomnia, edema, GI bleeding, abdominal pain, diarrhea, dyspepsia, flatulence, nausea, exfoliative dermatitis, stevensjohnson syndrome, toxic epidermal necrolysis, rash. Seizures (very high doses), pseudomembranous colitis, diarrhea, nausea, vomiting, abdominal pain, rashes, urticaria, eosinophilia, hemolytic anemia, thrombocytopenia, neutropenia, allergic reactions including anaphylaxis, superinfection. Seizures (very high doses), pseudomembranous colitis,
41
Rev. 08/21/08
cephalosporins
anaphylaxis at beginning of and throughout therapy.
Certolizumab pegol/ Cimzia
gastroinestinal anti inflammatories tumor necrosis factor blockers
Assess abdominal pain, stools, signs of infection, signs of hypersensitivity reactions prior to and during therapy. Assess allergy symptoms, lung sounds and character of bronchial secretions before and periodically during therapy. Assess for infusion reaction (rapid onset of airway obstruction [bronchospasm, stridor, hoarseness], urticaria, hypotension) for at least 1 hr following infusion. Assess for onset or worsening of pulmonary symptoms. Assess for dermatologic toxicities. Monitor serum electrolytes periodically during and for at least 8 wks following infusion.
Cetirizine/ Zyrtec
Cetuximab/ Erbitux
allergy, cold and cough remedies antihistamines piperazines peripherally selective antineoplastics monoclonal antibodies
diarrhea, nausea, vomiting, cramps, rashes, pruritis, urticaria, eosinophilia, leukopenia, neutropenia, allergic reactions including anaphylaxis and serum sickness, superinfection. Skin reactions (rarely severe), hematologic reactions, arthralgia, allergic reactions including anaphylaxis, infections, lupus-like syndrome. Dizziness, drowsiness (significant with doses > 10 mg/day), fatigue, pharyngitis, dry mouth.
Cevimeline/ Evoxac
Chamomile (Matricaria chamomilla, Anthemis nobilis)
xerostomia therapy adjuncts cholinergics muscarinic agonists sialagogues gastroinestinal anti inflammatories sedative/hypnotics
Assess patient for dry mouth prior to and periodically during therapy.
Chloral hydrate/ Aquachloral
sedative/hypnotics
Assess patient for abdominal distention and auscultate for bowel sounds. Evaluate sleep pattern and anxiety level prior to initiation. Note size, location and character of affected skin prior to and after topical application. Assess mental status, LOC, sleep pattern before and periodically throughout therapy.
Malaise, depression, headache, insomnia, conjunctivitis, dyspnea, cough, interstitial lung disease, pulmonary embolism, abdominal pain, constipation, diarrhea, nausea, vomiting, anorexia, stomatitis, renal failure, acneform dermatitis, alopecia, nail disorder, pruritus, skin desquamation, dehydration, hypomagnesemia, peripheral edema, anemia, leucopenia, back pain, weight loss, infusion reactions, fever, desquamation of mucosal epithelium. Coughing, rhinitis, visual disturbances, nausea, diarrhea, excessive salivation, excessive sweating, hot flashes. Contact dermatitis, allergic reactions including anaphylaxis.
Excess sedation, rashes, disorientation, dizziness, hangover, headache, incoordination, irritability, paradoxical excitation (children), respiratory depression, diarrhea, nausea, vomiting, flatulence, tolerance,
42
Rev. 08/21/08
Chlorambucil/Leukera n
antineoplastics immunosuppressan ts alkylating agents
Chloramphenicol/ Chloromycetin
anti-infectives
Monitor for bone marrow depression; bleeding; intake and output ratios and daily weights; fatigue, dyspnea, and orthostatic hypotension; and symptoms of gout during therapy. Monitor CBC and differential before and weekly during course of therapy. Monitor liver function tests, BUN, serum creatinine, and uric acid before and periodically during course of therapy. Assess patient for infection, signs of bone marrow depression, and gray syndrome at beginning of and throughout therapy. CBC should be monitored every 2 days throughout therapy.
physical or psychological dependence. Pulmonary fibrosis, nausea, stomatitis (rare), vomiting, decreased sperm count, sterility, alopecia (rare), dermatitis, rash, leucopenia, anemia, thrombocytopenia, hyperuricemia, allergic reactions, risk of second malignancy.
Chlordiazepoxide/ Libritabs, Librium
antianxiety agents sedative/hypnotics benzodiazepines
Chloroquine/Aralen
antimalarials antirheumatics (DMARDs)
Assess for anxiety and level of sedation, mental status, blood pressure, heart rate, and respiratory rate, tremors, agitation, delirium, and hallucinations prior to and periodically during therapy. CBC and liver function tests evaluated periodically. Assess deep tendon reflexes periodically to determine muscle weakness. Assess degree of joint pain and limitation of motion monthly. Monitor CBC periodically throughout therapy.
Confusion, delirium, depression, headache, blurred vision, optic neuritis, bitter taste (IV only), diarrhea, enterocolitis, glossitis, nausea, stomatitis, vomiting, rashes, urticaria, aplastic anemia, bone marrow depression, neutropenia, angioedema, thrombocytopenia, gray syndrome in newborns, peripheral neuritis, fever. Dizziness, drowsiness, hangover, headache, mental depression, paradoxical excitation, sedation, blurred vision, constipation, diarrhea, nausea, vomiting, weight gain, rashes, pain at IM site, physical/psychological dependence, tolerance. Seizures, delirium, depression, headache, personality changes, psychosis, hearing impairment, retinopathy, alopecia, tinnitus, visual disturbances, vomiting, cardiomyopathy, ECG changes (T-wave abnormalities, QRS prolongation), hypotension, abdominal cramps, anorexia, diarrhea, nausea, dermatoses, skin eruptions, photosensitivity, aplastic anemia, pigmentary changes, pruritus, agranulocytosis, leucopenia, thrombocytopenia, neuromyopathy, peripheral neuritis, weakness. Dizziness, drowsiness, lethargy, weakness,
Chlorothiazide/ Diuril
antihypertensives diuretics
Monitor blood pressure, intake, output, and daily
43
Rev. 08/21/08
thiazide diuretics
weight and assess feet, legs, and sacral area for edema daily. Monitor electrolytes (especially potassium), blood glucose, BUN, serum creatinine, and uric acid levels before and periodically throughout therapy
Chlorpheniramine/Alle rChlor, Allergy, ChloAmine, Chlorate, ChlorTrimeton, ChlorTrimeton Allergy 4 Hour, Chlor-Trimeton Allergy 8 Hour, ChlorTrimeton Allergy 12 Hour, PediaCare Allergy Formula, Phenetron, Telechlor, Teldrin Chlorpromazine/ Thorazine, Thor-Prom
allergy, cold and cough remedies antihistamines
Assess allergy symptoms; pulse and blood pressure; adverse anticholinergic effects; lung sounds and character of bronchial secretions prior to and periodically during therapy.
hypotension, anorexia, cramping, hepatitis, nausea, vomiting, pancreatitis, photosensitivity, rashes, hyperglycemia, hypokalemia, dehydration, hypercalcemia, hypochloremic alkalosis, hypomagnesemia, hyponatremia, blurred vision, hypophosphatemia, hypovolemia, rarely blood dyscrasias, muscle cramps, thrombocytopenia, hyperuricemia, hypercholesterolemia. Drowsiness, dizziness, excitation (in children), blurred vision, hypertension, arrhythmias, hypotension, palpitations, dry mouth, constipation, obstruction, retention, urinary hesitancy.
antiemetics antipsychotics phenothiazines
Chlorpropamide/ Diabinese
antidiabetics sulfonylureas
Assess mental status, weight and BMI, fasting blood glucose and cholesterol levels, symptoms of schizophrenia, blood pressure (sitting, standing, lying), pulse, and respiratory rate, fluid intake and bowel function, onset of akathisia, tardive dyskinesia, development of neuroleptic malignant syndrome, level of anxiety, and pain. CBC, liver function tests, and ocular exams periodically throughout therapy. Observe patient for signs and symptoms of hypoglycemic reactions. Serum glucose and glycosylated hemoglobin, CBC, urine, serum sodium levels and plasma osmolarity periodically throughout therapy
Neuroleptic malignant syndrome, sedation, extrapyramidal reactions, tardive dyskinesia, blurred vision, dry eyes, lens opacities, hypotension ( with IM, IV), tachycardia, constipation, dry mouth, anorexia, hepatitis, ileus, priapism, urinary retention, photosensitivity, pigment changes, rashes, galactorrhea, amenorrhea, agranulocytosis, leucopenia, hyperthermia, allergic reactions.
Anorexia, dizziness, headache, constipation, diarrhea, druginduced hepatitis, increased appetite, nausea, vomiting, photosensitivity, rash, pruritis, urticaria, hypoglycemia, syndrome of inappropriate antidiuretic hormone (SIADH) secretion, hyponatremia, aplastic anemia, agranulocytosis, eosinophilia, hemolytic anemia, leukopenia,
44
Rev. 08/21/08
Chlorthalidone/ Hygroton, Thalitone
antihypertensives diuretics thiazide diuretics
Monitor blood pressure, intake, output, and daily weight and assess feet, legs, and sacral area for edema daily. Monitor electrolytes (especially potassium), blood glucose, BUN, serum creatinine, and uric acid levels before and periodically throughout therapy.
Chlorzoxazone/ EZEDS, Paraflex, Parafon Forte DSC, Relaxazone, Remular, Remular-S, Strifon Forte DSC Cholecalciferol/ DeltaD, vitamin D3 (inactive)
skeletal muscle relaxants (centrally acting)
Assess patient for pain, muscle stiffness, and range of motion before and periodically throughout therapy
vitamins fat soluble vitamins
Assess for symptoms of vitamin deficiency, bone pain and weakness, evidence of hypocalcemia prior to and periodically during therapy. Serum calcium, phosphorus, and alkaline phosphatase should be monitored periodically.
Cholestyramine/ LoCHOLEST, LoCHOLEST Light, Prevalite, Questran, Questran Light
lipid-lowering agents bile acid sequestrants
Choline and magnesium salicylates/ Trilisate
antipyretics nonopioid analgesics salicylates
Assess severity of itching and skin integrity, stools. Obtain a diet history, especially in regard to fat consumption. Serum cholesterol and triglyceride levels should be evaluated before initiating, frequently during first few months and periodically throughout therapy. Assess pain and limitation of movement, fever before and during therapy. Monitor hepatic function and serum salicylate levels.
pancytopenia, thrombocytopenia, disulfiramlike reaction. Dizziness, drowsiness, lethargy, weakness, hypotension, anorexia, cramping, hepatitis, nausea, vomiting, photosensitivity, rashes, hyperglycemia, hypokalemia, dehydration, hypercalcemia, hypochloremic alkalosis, hypomagnesemia, hyponatremia, hypophosphatemia, hypovolemia, blood dyscrasias, hyperuricemia, hypercholesterolemia, muscle cramps, pancreatitis. Dizziness, drowsiness, GI bleeding, constipation, diarrhea, heartburn, nausea, vomiting, allergic dermatitis, agranulocytosis, anemia, allergic reactions including angioedema. Headache, irritability, somnolence, weakness, conjunctivitis, photophobia, arrhythmias, hypertension, anorexia, constipation, dry mouth, liver function test elevation, metallic taste, nausea, pancreatitis, polydipsia, vomiting, weight loss, albuminuria, azotemia, polyuria, pruritus, hypercalcemia, bone pain, muscle pain. Irritation of the tongue, abdominal discomfort, constipation, nausea, fecal impaction, flatulence, hemorrhoids, perianal irritation, steatorrhea, vomiting, irritation, rashes, hyperchloremic acidosis, vitamin A, D, and K deficiency.
Chondroitin/ chondroitin
Nonopioid analgesics
Monitor pain and range of motion, gastric discomfort,
Tinnitus, GI bleeding, dyspepsia, epigastric distress, nausea, abdominal pain, anorexia, hepatotoxicity, vomiting, allergic reactions including anaphylaxis and laryngeal edema. Heartburn, nausea, diarrhea, bleeding (antiplatelet effect),
45
Rev. 08/21/08
Polysulfate, CPS, CDS
Ciclesonide (inhalation)/ Alvesco
antiasthmatics corticosteroids inhalation
Ciclesonide (nasal)/ Omnaris
allergy, cold and cough remedies corticosteroids
Ciclopirox/ Loprox, Penlac
antifungals (topical)
Cidofovir/ Vistide
antivirals
signs of bleeding on an ongoing basis as an indicator of drug efficacy. Monitor respiratory status and lung sounds, signs of adrenal insufficiency, growth rates in children, change in vision or with a history of increased intraocular pressure, glaucoma, or cataracts closely during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic therapy. Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing. Patients on long-term therapy should have periodic otolaryngologic examinations to monitor nasal mucosa and passages for infection or ulceration. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Monitor vision for progression of CMV retinitis, ocular symptoms, intraocular pressure, and visual acuity, vital signs, signs and symptoms of infection periodically. Renal function must be monitored within 48 hr before each dose and throughout therapy. WBC before each dose.
allergic reactions, edema, hair loss. Headache, candida infection of mouth and pharynx, nasal congestion, nasopharyngitis, pharyngolaryngeal pain, cataracts, intraocular pressure, adrenal suppression ( dose, long term therapy), growth (children), arthralgia, back pain, bone mineral density ( dose, long term therapy), extremity pain, worsening of infections.
Headache, ear pain, epistaxis, local stinging, nasopharyngitis, adrenal suppression ( dose, long term therapy only).
burning, itching, local hypersensitivity reactions, redness, stinging. Headache, weakness, decreased intraocular pressure, hearing loss, iritis, ocular hypotony, uveitis, dyspnea, infection, pneumonia, hepatic dysfunction, pancreatitis, abdominal pain, nausea, vomiting, anorexia, chills, diarrhea, renal failure, proteinuria, alopecia, rash, fever, decreased serum bicarbonate, neutropenia, anemia, metabolic acidosis, Headache, dizziness, palpitations, tachycardia, diarrhea. Confusion, dizziness, drowsiness, hallucinations, headache, arrhythmias, constipation, diarrhea, druginduced hepatitis, nausea, decreased sperm count, erectile dysfunction, gynecomastia, pain at IM site,
Cilostazol/ Pletal
Cimetidine/ Tagamet, Tagamet HB
antiplatelet agents platelet aggregation inhibitors antiulcer agents histamine h2 antagonists
Assess patient for intermittent claudication before and periodically during therapy. Assess patient for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate. CBC with differential should be monitored periodically throughout therapy
46
Rev. 08/21/08
Cinacalcet/ Sensipar
hypocalcemics calcimimetic agents
Ciprofloxacin/ Cipro, Cipro XR, Proquin XR
anti-infectives fluoroquinolones
Monitor for signs and symptoms of hypocalcemia during therapy. Monitor serum calcium and phosphorous levels within 1 wk after initiation of therapy or dose adjustment and monthly for patients with hyperparathyroidism or every 2 mo for patients with parathyroid carcinoma once maintenance dose has been established, especially in patients with a history of seizure disorder. Assess for infection, signs and symptoms of anaphylaxis, bowel function, diarrhea, abdominal cramping, fever, and bloody stools at beginning of and throughout therapy.
agranulocytosis, aplastic anemia, anemia, neutropenia, thrombocytopenia, hypersensitivity reactions. Nausea, vomiting, hypocalcemia, adynamic bone disease.
Cisatracurium/ Nimbex
neuromuscular blocking agents nondepolarizing
Cisplatin/ Platinol-AQ
antineoplastics alkylating agents
Citalopram/ Celexa
antidepressants selective serotonin reuptake inhibitors ssris
Assess respiratory status, ECG, heart rate, and blood pressure, infusion site continuously throughout therapy. Monitor vital signs; intake and output and specific gravity; patency of IV site; bone marrow depression; anaphylaxis; ototoxicity and neurotoxicity; and overdose during therapy. Monitor CBC with differential and platelet count before and routinely throughout therapy. Monitor BUN, serum creatinine, and CCr before initiation of therapy and before each course of cisplatin to detect nephrotoxicity. Monitor mood changes and sexual dysfunction during therapy.
Seizures, dizziness, drowsiness, headache, insomniaagitation, confusion, hyperglycemia, pseudomembranous colitis, abdominal pain, diarrhea, abnormal liver enzymes , nausea, vaginitis, photosensitivity, rash, hypoglycemia, eosinophilia, phlebitis at IV site, tendinitis, tendon rupture, peripheral neuropathy, hypersensitivity reactions including anaphylaxis. Bronchospasm, rash, allergic reactions including anaphylaxis.
Seizures, malaise, weakness, ototoxicity, tinnitus, severe nausea, vomiting, diarrhea, hepatotoxicity, nephrotoxicity, sterility, alopecia, hypocalcemia, hypokalemia, hypomagnesemia, leucopenia, thrombocytopenia, anemia, phlebitis at IV site, hyperuricemia, peripheral neuropathy, anaphylactoid reactions.
Apathy, confusion, drowsiness, insomnia, weakness, agitation, amnesia, anxiety, decreased libido, dizziness, fatigue,
47
Rev. 08/21/08
Cladribine/ Leustatin
antineoplastics antimetabolites
Clarithromycin/ Biaxin, Biaxin XL
agents atypical mycobacterium anti-infectives antiulcer agents macrolides allergy, cold and cough remedies antihistamines
Monitor for bone marrow depression, fever, chills, sore throat, and signs of infection, platelet count, bleeding, IV site for phlebitis, intake and output throughout therapy. CD4 Tlymphocyte count and CD8 T-lymphocyte count; renal and hepatic function; serum uric acid concentrations before initiation of therapy and periodically during and after therapy. Monitor hemoglobin, hematocrit, leukocyte, and platelet counts before and periodically throughout therapy, especially during the first 48 wk after treatment. Assess patient for infection, epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate during therapy. Assess allergy symptoms, lung sounds and character of bronchial secretions prior to and periodically throughout therapy.
impaired concentration, increased depression, migraine headache, suicide attempt, abnormal accommodation, cough, postural hypotension, tachycardia, abdominal pain, anorexia, diarrhea, dry mouth, dyspepsia, flatulence, increased saliva, nausea, altered taste, increased appetite, vomiting, amenorrhea, dysmenorrhea, ejaculatory delay, erectile dysfunction, polyuria, increased sweating, photosensitivity, pruritus, rash, decreased weight, increased weight, arthralgia, myalgia. Fatigue, headache, dizziness, insomnia, malaise, weakness, epistaxis, abnormal breath sounds, cough, dyspnea, edema, tachycardia, anorexia, diarrhea, nausea, vomiting, abdominal pain, constipation, rash, erythema, petechiae, pruritis, sweating, neutropenia, anemia, thrombocytopenia, injection site reactions, phlebitis, thrombosis, arthralgia, myalgia, chills, fever, infection, trunk pain.
Clemastine/ Dayhist Allergy, Tavist Allergy
Clevidipine/ Cleviprex
antihypertensives calcium channel blockers
Monitor blood pressure and heart rate during infusion, and until vital signs
Headache, pruritus, rash, Stevens-Johnson syndrome, pseudomembranous colitis, abdominal pain/discomfort, abnormal taste, diarrhea, dyspepsia, nausea. Drowsiness, confusion, dizziness, paradoxical excitation (children), blurred vision, hypertension, arrhythmias, hypotension, palpitations, tachycardia, dry mouth, constipation, nausea, obstruction, vomiting, urinary retention, rash, thick mucus. Headache, CHF, hypotension, rebound hypertension, reflex tachycardia, nausea, vomiting,
48
Rev. 08/21/08
dihydropyridine
Clindamycin/ Cleocin, Cleocin T, ClindaDerm, Clindagel, Clindesse, ClindaMax, Clindets, C/T/S, Evoclin Clobetasol/ Clobex, Temovate, Temovate E
anti-infectives
anti inflammatories steroidal corticosteroids
stabilize. Hypotension and reflex tachycardia may occur with rapid upward titration. Assess for infection, bowel elimination, diarrhea, abdominal cramping, fever, and bloody stools, hypersensitivity before and during therapy. Monitor CBC. Assess affected skin before and daily during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected.
arthralgia.
Dizziness, headache, vertigo, arrhythmias, hypotension, pseudomembranous colitis, diarrhea, bitter taste (IV only), nausea, vomiting, rashes, phlebitis at IV site. Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression (use of occlusive dressings, long-term therapy). Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression (use of occlusive dressings, long-term therapy). Fatigue, pharyngitis, pericardial effusion, tachycardia, edema, diarrhea, hepatic toxicity, nausea, abdominal pain, constipation, mucositis, vomiting, dehydration, neutropenia, anemia, thrombocytopenia, injection site pain, systemic inflammatory response syndrome, tumor lysis syndrome, infections, fever, chills.
Clocortolone/ Cloderm
anti inflammatories steroidal corticosteroids
Assess affected skin before and daily during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected.
Clofarabine/ Clolar
antineoplastics antimetabolites
Clomiphene/ Clomid, Milophene, Serophene
ovulation inducer
Monitor respiratory status and blood pressure during infusion. Monitor for bone marrow depression, bleeding, signs and symptoms of tumor lysis syndrome and cytokine release, nausea and diarrhea before and during therapy. CBC and platelet counts at regular intervals during therapy and more frequently if levels are abnormal. Hepatic and renal function frequently during therapy. Perform a pelvic examination to determine ovarian size and presence of ovarian cysts prior to therapy and before subsequent courses of therapy. Assess patient for abdominal pain throughout therapy. Liver function tests
Headache, blurred vision, floaters, photophobia, scotomata, phosphenes, hot flashes, abdominal pain, bloating, distention, nausea, vomiting, liver enzymes, ovarian cyst formation, ovarian enlargement, breast discomfort, multiple births,
49
Rev. 08/21/08
should be performed prior to course of therapy. Clomipramine/ Anafranil antiobsessive agents tricyclic antidepressants Monitor mental status, blood pressure and pulse, weight and BMI, onset of extrapyramidal parkinsonian side effects before and during initial therapy. Monitor CBC and differential during chronic therapy. Monitor hepatic and renal function.
Clonazepam/Klonopin
Anticonvulsant; benzodiazepines
Clonidine/ Catapres, Catapres-TTS, Duraclon
antihypertensives adrenergics centrally acting
Clopidogrel/ Plavix
antiplatelet agents platelet aggregation inhibitors
Assess degree and manifestations of anxiety and mental status, drowsiness, unsteadiness, and clumsiness prior to and periodically during therapy Monitor intake and output ratios and daily weight, and assess for edema daily, blood pressure and pulse frequently during initial dosage adjustment and periodically throughout therapy. Assess location, character, and intensity of pain prior to, frequently during first few days, and routinely throughout administration. Monitor patient for signs and symptoms of opioid withdrawal. Monitor for fever as potential sign of catheter infection. Assess patient for symptoms of stroke, peripheral vascular disease, signs of thrombotic thrombocytic purpura or MI periodically during therapy. Monitor CBC with differential and platelet count periodically during therapy.
intermenstrual spotting, abnormal menstrual flow, weight gain. Seizures, lethargy, sedation, weakness, aggressive behavior, blurred vision, dry eyes, dry mouth, vestibular disorder, arrhythmias, ECG changes, orthostatic hypotension, constipation, nausea, vomiting, weight gain, eructation, male sexual dysfunction, urinary retention, dry skin, photosensitivity, gynecomastia, anemia, muscle weakness, extrapyramidal reactions, hyperthermia. behavioral changes, drowsiness, ataxia
Drowsiness, depression, dizziness, nervousness, nightmares, bradycardia, hypotension (increased with epidural), palpitations, dry mouth, constipation, nausea, vomiting, erectile dysfunction, rash, sweating, sodium retention, weight gain, withdrawal phenomenon.
Clorazepate/ GenXENE, Tranxene, TranxeneSD
anticonvulsants sedative/hypnotics benzodiazepines
Assess for drowsiness, unsteadiness, and clumsiness, anxiety and mental status, alcohol withdrawal, seizures prior to
Depression, dizziness, fatigue, headache, epistaxis, cough, dyspnea, chest pain, edema, hypertension, GI bleeding, abdominal pain, diarrhea, dyspepsia, gastritis, pruritus, purpura, rash, bleeding, neutropenia, thrombotic thrombocytopenic pupura, hypercholesterolemia, arthralgia, back pain, fever, hypersensitivity reactions. Dizziness, drowsiness, lethargy, hangover, headache, mental depression, slurred speech, ataxia, paradoxical excitation, blurred vision,
50
Rev. 08/21/08
and periodically during therapy. CBC and liver function tests evaluated periodically.
Clotrimazole (topical)/ Cruex, Lotrimin
antifungals (topical)
Clotrimazole (vaginal)/ Gyne-Lotrimin-3, Mycelex-7 Cloxacillin/ Cloxapen
antifungals (vaginal)
anti-infectives penicillinase resistant penicillins
Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Assess for infection, signs and symptoms of anaphylaxis at beginning of and throughout therapy.
respiratory depression, constipation, diarrhea, nausea, vomiting, weight gain (unusual), rashes, physical dependence, psychological dependence, tolerance. Burning, itching, local hypersensitivity reactions, redness, stinging.
Itching, soreness, vulvovaginal burning.
Clozapine/Clozaril
Antipsychotics
Codeine
allergy, cold and cough remedies antitussives opioid analgesics opioid agonists
Monitor patient's mental status, BP, pulse, weight, BMI, fasting BG and cholesterol levels, signs of myocarditis, onset of akathisia and extrapyramidal side effects, tardive dyskinesia, BMs, development of neuroleptic malignant syndrome Assess blood pressure, pulse, respirations, pain, bowel function, cough before and periodically during administration.
Seizures, diarrhea, epigastric distress, nausea, vomiting, eosinophilia, pseudomembranous colitis, interstitial nephritis, rash, urticaria, leucopenia, allergic reactions including anaphylaxis and serum sickness, superinfection. Neuroleptic malignant syndrome, seizures, dizziness, sedation, myocarditis, hypotension, tachycardia constipation, agranulocytosis, leukopenia
Colchicine
antigout agents
Assess patient for toxicity, joints for pain, mobility, and edema, intake and output ratios before and during therapy. During initiation of therapy, monitor for drug response every 12 hr. In patients receiving prolonged therapy, monitor baseline and periodic CBC; report
Confusion, sedation, dysphoria, euphoria, floating feeling, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, nausea, vomiting, urinary retention, flushing, sweating, physical dependence, psychological dependence, tolerance. Diarrhea, nausea, vomiting, abdominal pain, anuria, hematuria, renal damage, alopecia, agranulocytosis, aplastic anemia, leukopenia, thrombocytopenia, phlebitis at IV site, peripheral neuritis.
51
Rev. 08/21/08
significant in values. Colesevelam/ Welchol lipid-lowering agents bile acid sequestrants Obtain a diet history, especially in regard to fat consumption. Monitor serum total cholesterol, LDL, and triglyceride levels before initiating, and periodically during therapy. Assess severity of itching and skin integrity. Obtain a diet history, especially in regard to fat consumption. Assess frequency, amount, and consistency of stools. Serum cholesterol and triglyceride levels should be evaluated before initiating, frequently during first few months and periodically throughout therapy. Assess skin surface prior to application of this herb and at least daily during use. Assess area for signs of infection such as redness, swelling or drainage at least daily during use. Assess response to therapy by evaluating adjacent wound for size, color and drainage at least daily. Constipation, dyspepsia.
Colestipol/ Colestid
lipid-lowering agents bile acid sequestrants
Irritation of the tongue, abdominal discomfort, constipation, nausea, fecal impaction, flatulence, hemorrhoids, perianal irritation, steatorrhea, vomiting, irritation, rashes, hyperchloremic acidosis, vitamin A, D, and K deficiency.
Comfrey/ Ass ear, black root, blackwort, bruisewort, Consolidae radix, consound, gum plant, healing herb, knitback, knitbone, salsify, slippery root, Symphitum officinale, Symphitum radix, wallwort
none assigned
Concentrated oral gel/ Gelclair Conivaptan/ Vaprisol
oral protectants
electrolyte modifiers vasopressin antagonists
Assess mouth ulcers and severity of pain prior to and periodically during therapy. Monitor injection site and neurologic status during administration. Monitor vital signs frequently during therapy. Monitor serum sodium concentration frequently during therapy. Monitor blood pressure and daily weight periodically during therapy. Assess waking and sleeping electroencephalograms periodically in patients treated for infantile myoclonic seizures. Monitor CBC, serum calcium, electrolytes, phosphorus, serum fasting and postprandial glucose, and
Headache, apathy, lassitude, gastroenteritis, abdominal pain, decreased urine output, pulmonary hypertension, pleural effusion, ascites, hepatosplenomegaly, jaundice, hepatic cirrhosis and necrosis and death as a result of venoocclusive disease, oral use of comfrey for as little as 5-7 days in a child and 19-45 days in adults have resulted in severe hepatic disease and death. None noted
Corticotrophin/ ACTH80, H.P. Acthar Gel
hormones (adrenocorticotropi c) hormones
Headache, confusion, insomnia, hypertension, hypotension, diarrhea, polyuria, dehydration, hypokalemia, hypomagnesemia, hyponatremia, injections site reactions, fever, thirst. Depression, euphoria, psychoses, cataracts, increased intraocular pressure, CHF, thromboembolism, edema, hypertension, nausea, increased appetite, peptic ulceration, vomiting, weight gain, decreased wound healing, petechiae, acne, ecchymoses, fragility, hirsutism, adrenal suppression, decreased growth
52
Rev. 08/21/08
renal function tests with urinalysis before initiation of therapy.
Cortisone
anti inflammatories steroidal corticosteroids
Assess patient for signs of adrenal insufficiency, intake and output ratios and daily weights, peripheral edema, steady weight gain, rales/crackles, or dyspnea before and periodically throughout therapy. Monitor serum electrolytes and glucose. Guaiac-test stools.
Cosyntropin/ Cortrosyn
diagnostic agents hormones (adrenocorticotropi c) hormones antiasthmatics allergy, cold and cough remedies mast cell stabilizers
Cromolyn/ Intal, Gastrocrom, NasalCrom
Monitor for hypersensitivity response. Plasma cortisol concentrations will be measured before and 30 or 60 min after administration of cosyntropin. Evaluate pulmonary function testing before initiating therapy in asthmatics. Assess lung sounds and respiratory function before and periodically during therapy. Assess for symptoms of rhinitis.
in children, hyperglycemia, menstrual irregularities, hypokalemia, sodium retention, hypocalcemia, metabolic alkalosis, atrophy at IM sites, aseptic necrosis of joints, myopathy, osteoporosis, weakness, cushingoid appearance, increased susceptibility to infections, pancreatitis. Depression, euphoria, headache, increased intracranial pressure (children only), personality changes, psychoses, restlessness, cataracts, increased intraocular pressure, hypertension, peptic ulceration, anorexia, nausea, vomiting, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, hyperglycemia, fluid retention (long-term high doses), hypokalemia, hypokalemic alkalosis, thromboembolism, thrombophlebitis, weight gain, weight loss, muscle wasting, osteoporosis, aseptic necrosis of joints, muscle pain. Hypersensitivity reactions including anaphylaxis.
Cyanocobalamin/ Nascobal, Rubramin PC
antianemics vitamins water soluble vitamins
Assess patient for signs of vitamin B12 deficiency before and periodically during therapy. Monitor plasma folic acid, vitamin B12, and iron levels, hemoglobin, hematocrit, and reticulocyte count before treatment, 1 month after the start of
Dizziness, headache, rash, urticaria, angioedema, nausea, unpleasant taste, allergic reactions including anaphylaxis or worsening of conditions being treated. Intranasalnasal irritation, nasal congestion, sneezing. Inhalationirritation of the throat and trachea, cough, wheezing, bronchospasm. Headache, heart failure, diarrhea, itching, swelling of the body, hypokalemia, thrombocytosis, pulmonary edema, pain at IM site, hypersensitivity reactions including anaphylaxis.
53
Rev. 08/21/08
Cyclobenzaprine/Flexe ril
Skeletal muscle Relaxants
Cyclophosphamide/ Cytoxan, Neosar
antineoplastics immunosuppressan ts alkylating agents
Cyclosporine/ Neoral, Sandimmune, Gengraf
immunosuppressan ts antirheumatics ( DMARD) polypeptides cyclic
Cyproheptadine/ Periactin, PMSCyproheptadine
allergy, cold and cough remedies antihistamines
Cysteamine/ Cystagon
cystine depleting agent
therapy, and then every 36 months. Assess patient for pain, muscle stiffness, and range of motion before and periodically throughout therapy Monitor blood pressure, pulse, respiratory rate, and temperature; urinary output; bone marrow depression; bleeding; nausea, vomiting, and appetite; weight; cardiac and respiratory status for dyspnea, rales/crackles, weight gain, edema during therapy. Monitor CBC with differential and platelet count; BUN, creatinine, and uric acid; ALT, AST, LDH, and serum bilirubin before and periodically during therapy. Monitor serum creatinine level, intake and output ratios, daily weight, and blood pressure during therapy. Assess for symptoms of organ rejection throughout therapy. Assess pain and limitation of movement prior to and during administration. Prior to initiating therapy, perform a physical exam including blood pressure on 2 occasions to determine baseline. Monitor blood pressure every 2 wk during initial 3 mo, then monthly if stable. Assess for adverse anticholinergic effects, rhinitis, conjunctivitis, hives, food intake and weight, lung sounds and respiratory function prior to and periodically throughout therapy. Assess patient for rash, neurologic status, anorexia, nausea, vomiting, and abdominal pain throughout therapy. Monitor leukocyte cystine levels every 3 mo. Monitor CBC and liver function tests periodically
dizziness, drowsiness, dry mouth
Pulmonary fibrosis, myocardial fibrosis, hypotension, anorexia, nausea, vomiting, hemorrhagic cystitis, hematuria, alopecia, gonadal suppression, syndrome of inappropriate antidiuretic hormone (SIADH), leucopenia, thrombocytopenia, anemia, hyperuricemia, secondary neoplasms.
Seizures, tremor, confusion, flushing, headache, psychiatric problems, hypertension, diarrhea, hepatotoxicity, nausea, vomiting, abdominal discomfort, anorexia, pancreatitis, nephrotoxicity, hirsutism, acne, hyperkalemia, hypomagnesemia, anemia, leukopenia, thrombocytopenia, hyperlipidemia, hyperuricemia, hyperesthesia, paresthesia, gingival hyperplasia, hypersensitivity reactions, infections.
Drowsiness, excitation (increased in children), blurred vision, arrhythmias, hypotension, palpitations, dry mouth, constipation, hesitancy, retention, photosensitivity, rashes, weight gain. Seizures, lethargy, ataxia, confusion, depression, encephalopathy, headache, hallucinations, nightmares, somnolence, hypertension, hearing loss, anorexia, diarrhea, vomiting, abdominal pain, abnormal liver function
54
Rev. 08/21/08
during therapy.
Cytarabine/Ara-C, cytosine arabinoside, Cytosar-U, DepoCyt
antineoplastics antimetabolites
Cytomegalovirus immune Globulin/CMVIG, CytoGam
vaccines/immunizin g agents immune globulins
Monitor for bone marrow depression, bleeding, intake and output ratios and daily weights, symptoms of gout, nutritional status, development of cytarabine or ara-C syndrome, respiratory distress and pulmonary edema, signs of anaphylaxis, Chemical arachnoiditis before and during therapy. Monitor patients receiving IT therapy continuously for the development of neurotoxicity. Monitor CBC with differential and platelet count prior to and frequently during therapy. Monitor renal and hepatic function prior to and routinely during therapy Monitor vital signs prior to, during, and following infusion and before any increases in infusion rate. Monitor patient for adverse reactions throughout therapy.
studies, bad breath, constipation, dyspepsia, rash, urticaria, dehydration, anemia, leucopenia, tremor, fever. CNS dysfunction (high dose), confusion, drowsiness, headache, corneal toxicity (high dose), hemorrhagic conjunctivitis (high dose), pulmonary edema (high dose), edema, nausea, vomiting, hepatitis, hepatotoxicity, severe GI ulceration (high dose), stomatitis, urinary incontinence, alopecia, rash, sterility, anemia, leukopenia, cytarabine syndrome, fever, thrombocytopenia, hyperuricemia. Intrathecal onlychemical arachnoiditis, abnormal gait.
Headache, tremor, anxiety, seizures, pancytopenia, hemolysis, leucopenia, rash, wheezing, dyspnea, pulmonary edema, anuria, hypotension, back pain, thromboembolism, nausea, fever, vomiting, hepatic dysfunction, flushing, oliguria, acute renal failure, muscle cramps, allergic reactions including chills, anaphylaxis.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Dacarbazine/DTICDome
antineoplastics alkylating agents
Monitor vital signs; bone marrow depression; bleeding; IV site; intake and output, appetite, and nutritional intake; and nausea and vomiting prior to and frequently during therapy.
Daclizumab/Zenapax
immunosuppressan ts monoclonal
Assess for fluid overload, signs of anaphylactic or hypersensitivity reactions,
Hepatic necrosis, anorexia, nausea, vomiting, diarrhea, hepatic vein thrombosis, alopecia, facial flushing, photosensitivity, rash, gonadal suppression, anemia, leukopenia, thrombocytopenia, pain at IV site, phlebitis at IV site, tissue necrosis, myalgia, facial paresthesia, anaphylaxis, fever, flu-like syndrome, malaise. dizziness, fatigue, headache, insomnia, pulmonary edema, coughing, dyspnea, chest pain,
55
Rev. 08/21/08
antibodies
infection, vital signs and breath sounds closely. Obtain chest x-ray within 24 hr before beginning therapy.
Dactinomycin/ actinomycin-D, Cosmegen
antineoplastics antitumor antibiotics
Monitor vital signs; bone marrow depression; bleeding; signs of infection during neutropenia; intake and output, appetite, and nutritional intake; nausea and vomiting; and IV site frequently for inflammation or infiltration. Monitor CBC and differential before and periodically during therapy.
Dalteparin/ Fragmin
anticoagulants antithrombotics low molecular weight heparins anticoagulants low molecular weight heparins
Danaparoid/ Orgaran
Danazol/ Danocrine
hormones androgens
Assess for signs of bleeding and hemorrhage. Observe injection sites for hematoma, ecchymosis, or inflammation. Assess patient for signs of bleeding and hemorrhage, bleeding from surgical site, evidence of additional or increased thrombosis, hypersensitivity reactions, epidural catheters frequently for signs and symptoms of neurologic impairment. Observe injection sites for hematomas, ecchymosis, or inflammation Assess patient for endometrial pain, breast pain, tenderness, and nodules, edematous attacks
edema, hypertension ( in children), hypotension, tachycardia, abdominal discomfort, constipation, diarrhea ( in children), dyspepsia, epigastric pain, nausea, pyrosis, vomiting ( in children), dysuria, oliguria, renal tubular necrosis, acne, impaired wound healing, pruritus ( in children), thrombosis, arthralgia, back pain, musculoskeletal pain, tremor, allergic reactions including anaphylaxis, fever ( in children), post-operative pain ( in children), urinary and respiratory tract infection( in children). Lethargy, malaise, anorexia, nausea, stomatitis, vomiting, abdominal pain, ascites, diarrhea, dysphagia, esophagitis, hepatotoxicity, ulceration, acne, alopecia, erythema, hyperpigmentation, skin eruptions, photosensitivity, rash, pharyngitis, hypocalcemia, gonadal suppression, anemia, leukopenia, thrombocytopenia, phlebitis at IV site, myalgia, pneumonitis, fever. Dizziness, reversible increase in liver enzymes, bleeding, thrombocytopenia.
dizziness, headache, insomnia, edema, constipation, nausea, reversible increase in liver enzymes, vomiting, urinary retention, ecchymoses, pruritus, rash, urticaria, bleeding, anemia, thrombocytopenia, erythema at injection site, hematoma, irritation, pain, fever.
emotional lability, deepening of voice, edema, hepatitis (cholestatic jaundice), amenorrhea, clitoral enlargement, testicular atrophy, acne, hirsutism, oiliness, amenorrhea,
56
Rev. 08/21/08
Dang quai/ Angelic sinensis, Chinese Angelica, Dang Gui, Danggui, Dong Qua, Ligustilides, Phytoestrogen, Radix angelicae giganitis, Tang Kuei, Tan Kue Bai Zhi Dantrolene/ Dantrium
None (treats menstrual pain)
Assess pain and menstrual patterns, pregnancy test, history of hormone sensitive cancer, medication profile.
anovulation, decreased breast size (women), decreased libido, weight gain. Photosensitivity, can be carcinogenic and mutagenic.
skeletal muscle relaxants (direct acting)
Assess bowel function, neuromuscular status and muscle spasticity, anesthesia history of all surgical patients. Monitor ECG, vital signs, electrolytes, and urine output continuously when administering IV for malignant hyperthermia. difficulty swallowing and choking during meals on the day of administration.
Dapsone/ Aczone
leprostatic agent
Assess skin for new or toxic dermatologic reactions during therapy. Assess patient for infection and monitor respiratory status at beginning of and throughout therapy. Monitor AST and ALT prior to and periodically during therapy.
Daptomycin/ Cubicin
anti-infectives cyclic lipopeptide antibacterial agents
Assess patient for infection and signs of pseudomembranous colitis (diarrhea, abdominal cramping, fever, and bloody stools)
Darbepoetin/ Aranesp
antianemics hormones rDNA
Monitor blood pressure, symptoms of anemia, allergic reactions, signs of anaphylaxis, dialysis shunts
drowsiness, muscle weakness, confusion, dizziness, headache, insomnia, malaise, nervousness, excessive lacrimation, visual disturbances, pleural effusions, changes in BP, tachycardia, hepatotoxicity, diarrhea, anorexia, cramps, dysphagia, GI bleeding, vomiting, crystalluria, dysuria, frequency, erectile dysfunction, incontinence, nocturia, pruritus, sweating, urticaria, eosinophilia, irritation at IV site, phlebitis, myalgia, chills, drooling, fever. Headache, tonic-clonic movements (topical), vertigo, blurred vision, tinnitus, hepatotoxicity, abdominal pain, nausea, pancreatitis, vomiting, exfoliative dermatitis, Stevens-Johnson syndrome, agranulocytosis, methemoglobinemia, reticulocytosis, hemolytic anemia. Dizziness, dyspnea, hypertension, hypotension, pseudomembranous colitis, constipation, diarrhea, nausea, vomiting, liver function tests, renal failure, pruritus, rash, anemia, injection site reactions, CPK, fever. Seizures, dizziness, fatigue, headache, weakness, cough, dyspnea, bronchitis, CHF, MI, stroke, thrombotic events, edema, hypertension, hypotension, chest pain, abdominal pain, nausea, diarrhea, vomiting, constipation, pruritus, pure red cell aplasia, myalgia,
57
Rev. 08/21/08
Darifenacin/ Enablex
Urinary tract antispasmodic Anticholinergic
Darunavir/ prazista
Antiretroviral Protease inhibitor
Dasatinib/ Sprycel
Antineoplastic Enzyme iinhibitor
Monitor voiding pattern and assess symptoms of overactive bladder (urinary urgency, urinary incontinence, urinary frequency) periodically during therapy. Assess patient for change in severity of HIV symptoms and for symptoms of opportunistic infections. Assess for allergy to sulfonamides. Monitor patient for development of rash. Monitor viral load and CD4 counts regularly. Monitor liver function prior to and periodically during therapy. Monitor for fluid retention. Weigh regularly, and assess for signs of pleural effusion, pericardial effusion, pulmonary edema, ascites. Monitor chest x-ray in patients with symptoms of pleural effusion. Monitor vital sigs. Monitor liver function before and monthly during treatment. Monitor CBC weekly for first 2 months, monthly after that.
arthralgia, back pain, limb pain, fever, allergic reactions, flu-like syndrome, sepsis, mortality and tumor growth Dizziness, blurred vision, constipation, dry mouth, dyspepsia, nausea, heat intolerance.
Hepatotoxicity, constipation, diarrhea, nausea, vomiting, hyperglycemia, body fat redistribution, rash.
Daunorubicin citrate liposome/ daunoXome
Antineoplastics Anthracyclines
Monitor vital signs before/during therapy. Assess patient for back pain, flushing, and chest tightness. Monitor for bone marrow depression. Assess
Seizures, altered affect, anxiety, confusion, depression, drowsiness, insomnia, malaise, syncope, vertigo, conjunctivitis, dry eye, tinnitus, asthma, peneumonitis, CHF, MI, pulmonary edema, QTC prolongation, hypertension, hypotension, palpitations, abdominal pain, altered appetite, dysgeusia, dyspepsia, ileus, mucositis, nausea, vomiting, renal failure, urinary frequency, acne, alopecia, dry skin, flushing, nail disorder, photosensitivity, pigment disorder, rash , sweating, urticaria, gynecomastia, fluid retention, hypocalcemia, bleeding events, anemia, nautropenia, pancrytopenia, thrombocytopenia, hyperuricemia, muscle inflammation/weakness, tremor, infections, palmarolanter erythrodysesthesia, tumor lysis syndrome Fatigue, headache, depression, dizziness, insomnia, malaise, rhinitis, abnormal vision, sinusitis, cardiotoxixity, chest pain, edema, abdominal pain,
58
Rev. 08/21/08
Daunorubicin hydrochloride/ cerubidine
Antiineoplastic Anthracyclines
Decitabine/ Dacogen
Antineolastics
for bleeding and avoid IM injections and taking rectal temps. Apply pressure to venipuncture sites for 10 min. assess for signs of infection. Monitor for increase fatigue, dyspnea, and orthostatic hypotension. Assess IV site frequently for inflammation or infiltration. Monitor intake/output, appetite, and nutritional intake. Assess for nausea and vomiting. Administer an antimetic periodically and adjust diet as tolerated to hlelp maintain fluid and electrolyte balance and nutritional status. Encourage fluid intake of 2000-3000ml/day. Assess patient for evidence of cardiotoxicity which manafests as CHF. Monitor uric acid levels, CBC and differential, hepatic and renal functions before each dose/ course of therapy. Monitor vital signs. Monitor for bone marrow depression. Assess for bleeding and avoid IM injections and taking renal temps. Monitor for lncrease fatigue, dyspnea, and orthostatic hypotension. Apply pressure to venipuncture sties for 10min. assess IV site for inflammation or infiltration. Monitor intake/output, apetite, and nutritional intake. Assess for nausea and voimiting. Administer antiemetic periodically and adjust diet as tolerated to help maintain fluid and electrolyte balance and nutritional status. Encourage fluid intake of 2000-3000ml/day. Assess patient for evidence of cardiotoxicity, which may manifest as CHF. Monitor uric acid, CBC and differential, leukocyte count, liver, and kidney function. Monitor for bone marrow depression. Assess for
anorexia, constipation, diarrhea, nausea, stomatitis, tenesmus, vomiting, red urine, gonadal suppression, alopecia, increased sweating, pruritus, anemia, leucopenia, thrombocytopenia, phlebitis at IV site, hyperuricemia, back pain, arthralgia, myalgia, neuropathy, allergic reactions, chills, fever, flushing, chest tightness, influenza-like symptoms.
Rhinitis, abnormal vision, sinusitis, cardiotoxicity, arrhythmias, nausea, vomiting, esophagitis, hepatotoxicity, stomatitis, red urine, gonadal suppression, alopecia, anemia, leucopenia, thrombocytopenia, phlebitis at IV site, hyperuricemia, chills, fever.
Confusion, fatigue, insomnia, depression, lethargy, blurred
59
Rev. 08/21/08
Deferasirox/ Exjade
Antidotes Chelating agents
Deferoxamine/ desferal
Antidotes Heavy metal antagonists
Delavirdine/ Resciptor
Antiretrovirals Non nucleoside reverse transcriptase inhibitors Antineolastics Cytotoxic proteins
Denileukin diftitox/ Ontak
bleeding and avoid IM injections and taking rectal temps. Apply pressure to venipuncture sites for 10 min. assess for signs go infection during neutropenia. Monitor for increased fatigue, dyspnea, and orthostatic hypotension. Monitor CBC prior to each dosing cycly. Obtain liver chemistries and serum creatinine prior to treatment. Assess hearing and vision prior to and periodically. May cause high frequency hearing loss and visual disturbances. Assess patient for rash during therapy. Measure serum ferritin monthly. Monitor serum creatinine prior to and monthly. Monitor urine protein periodically. In acute poisoning assess time, amount, and type of iron preparation ingested. Monitor signs of iron toxicity. Early (abdominal pain, bloody diarrhea, emesis), late (decreased level of consciousness, shock, metabolic acidosis). Monitor vital signs closely. Watch for anaphylactic reactions. Monitor intake/output and urine color. Monitor serum iron, total iron binding capacity, ferritin levels, and uring iron excretion before and periodically. Monitor liver function and assess damage of iron poisoning. Assess patient for changes in severity of HIV symptoms and for symptoms of opportunistic infections. Monitor viral load and CD4 cell counts. Monitor patient for signs and symptoms of hypersensitivity reaction. Motitor patient for flu-like syndrome. Assess patient for symptoms of vascular leak syndrome. Monitor
vision, cough, atrial fibrillation, pulmonary edema, tachycardia, abdominal pain, constipation, diarrhea, stomatitis, vomiting, abnormal liver function tests, petechiae, rash, edema, hypokalemia, hypomagnesemia, ascites, bleeding, anemia, neutropenia, thrombocytopenia, injection site irritation, hyperglycemia, arthralgia, myalgia, infection, fever lymphadenopathy. Headache, hearing loss, ocular disturbances, cough, diarrhea, nausea, vomiting, abdominal pain, drug-induced hepatitis, increase serum creatinine, skin rash, arthralgia, fever.
Blurred vision, cataracts, ototoxicity, hypotension, tachycardia, abdominal pain, diarrhea, red urine, erythema, flushing, urticaria, induration at injection site, pain at injection site, leg cramps, allergic reactions, fever, shock after rapid IV administartaion.
Fatigue, headache, diarrhea, increased amylase, increased liver enzymes, nausea, vomiting, rash, pruritus, fat redistribution. Dizziness, headache, confusion, insomnia, nervousness, weakness, loss of visual acuity. Loss of color vision, cough, dyspnea, pharyngitis, rhinitis, chest pain, edema, hypotension,
60
Rev. 08/21/08
bowel function and fluid status. Assess patient for rash. Monitor CBC, blood chemistry, liver and renal function, serum albumin.
Desipramine/ Norpramin, pertofrane
Antidepressants Tricyclic antidepressants
Desirudin/ iprivask
Anticoagulants Thrombin inhibitors
Desloratadine/ Clarinex
Allergy, cold and cough remedies Antihistamines piperidines
Desmopressin/ DDAVP, DDAVP Rhinal tube,
Hormones Antidiuretic hormones
Obtain weight and BMI initiatially and periodically throughout therapy. Assess FBS and cholesterol levels for overweight/ obese individuals. Monitor BP and pulse prior to and during therapy. Patients taking high doses or with a history of cardio disease should have ECG monitored prior to and periodically during therapy. Monitor mental status. Assess for suicidal tendencies. Assess intensity, quality, and location of pain. Assess leukocyte and differential blood counts, liver function, and serum glucose periodically. Assess for sings of bleeding. Assess patient for evidence of thrombosis. Monitor patients with epidural catheters frequently for signs of neurological impairment. Observe injection sites for hematomas, ecchymosis, or inflammation. Monitor aPTT daily. Monitor CBC. Assess allergy symptoms. Assess lung sounds and character of bronchial secretions. May cause falsenegative result on allergy skin testing Chronic intranasal use may cause tolerance. Monitor frequency of enuresis.
tachycardia, arrhythmia, hypotension, thrombotic events, rash pruritis, sweating, anorexia, diarrhea, nausea vomiting, constipation ,dyspepsia, dysphagia, increased transaminases, albuminuria, hematuria, hypocalcemia, dehydration, hypokalemia, anemia, leucopenia, thrombocytopenia, injection site reactions, hypoalbuminemia, weight loss, myalgia, arthroalgia, paresthesia, acute hupersensitivity reactions, chills, fever, flu-like syndrome, infection. Drowsiness fatigue, blurred vision, dry eyes, dry mouth, arrhythmias, hypotension, ECG changes, constipation, drug-induced hepatitis, paralytic ileus, increased appetite, weight gain, urinary retention, decreased libido, photosensitivity, changes in blood glucose, gynecomastia, blood dyscrasias.
Nauseas, bleeding, anemia, injection site reactions, wound secretion.
Drowsiness, pharyngitis, dry mouth, allergic reactions including anaphylaxis
Drowsiness, headache, listlessness, nasal congestion, rhinitis, dyspnea,
61
Rev. 08/21/08
DDAVP rhinyle drops, Octostim, Stimate
Desonide/ Desonate, DesOwen, Verdeso,
Anti inflammatories steroidal Corticosteroids
Desoximetasone/ Topicort
Anti inflammatories steroidal corticosteroids
Desvenlafaxine/ Pristiq
Antidepressants Selective serotonin norepinephrine reuptake inhibitor
Monitor urine and plasma osmolality and urine volume. Assess patient for symptoms of dehydration. Weigh patient daily. Monitor plasma factor VIII coagulation, factor VIII antigen, and ristocetin cofactor. Monitor aPTT. Monitor BP and pulse during IV infusion. Monitor intake/output and adjust fluid intake to avoid overhydration. Assess for signs of water intoxication. Assess affected skin before and daily during therapy. Note degree of inflammation and pruritus. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy. Assess affected skin before and daily during therapy. Note degree of inflammation and pruritus. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy. Assess mental status and mood changes. Assess suicidal tendencies. Monitor BP, appetite and nutritional intake. Weight weekly. Assess for serotonin syndrome.
hypertension, hypotension, tachycardia, mild abdominal cramps, nausea, valval pain, flashing, water intoxication/ hyponatremia, phlebitis at IV site.
Allergic contatct dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrochosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection striae, adrenal suppression. Allergic contatct dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrochosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection striae, adrenal suppression. Seizures, anxiety, dizziness, drowsiness, insomnia, headache, increased intraocular lpressure, mydriasis, eosinophilic pneumonia,interstitial lung disease, hypertension, decreased appetite, constipation, nausea, male sexual dysfunction, sweating, hyponatremia, increased risk of bleeding, hypercholesterolemia, hyperlipidemia, serotonin syndrome. Depression, euphoria, hallucinations, headache, increased intracranial pressure (children only), insomnia, personality changes, phychoses, restlessness, cataracts , increased intraocular pressure,
Dexamethasone/ DexPak
Anti inflammatories steroidal
Assess involved systems. Assess for signs of adrenal insufficiency. Monitor intake/output ratios and daily weights. Observe for peripheral edema, steady weight gain, rales/crackels, or dyspnea. Children should
62
Rev. 08/21/08
Dexamethasone (topical)/AerosebDex, Decadron, Decaspray
anti inflammatories steroidal corticosteroids
have periodic evaluations of growth. Monitor for signs of allergic reactions. Monitor ECG. Assess for changes in level of consciousness and headache. Monitor serum electrolyes and glucose. Periodic adrenal function tests. Dexamethasone suppression test: obtain baseline cortisol level; administer dexamethasone at 11 pm and obtain cortisol levels at 8 am the next day. Normal response is a decreased cortisol level Assess affected skin before and daily during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected. Assess patient routinely for epigastric or abdominal pain and for frank or occult blook in stool, emesis, or gastric aspirate. Monitor liver function. Monitor INR and prothrombin time. Assess level of sedation. Monitor ECG and BP continuously. Assess childs attention span, impulse control, and interactions with others. Monitor BP, pulse, and respiration. Obtain a history and physical to assess for cardiac disease. Monitor growth (height and weight) in children. Monitor behavior change. Monitor CBC, differential, and platelet count. Assess extent of cardiomyopathy. Assess site of extavasation for pain, burning, swelling, and redness. Monitor CBC and platelet count. Monitor liver function. Monitor BP,pulse, and respiration. Obtain history
Dexlansoprazole/ Kapidex
Antiulcer agents Proton pump inhibitor
hypertension, edema, peptic ulceration, anorexia, nausea, increased appetitie, vomiting, acne, decreased woundt healing, acchymoses, hirsutism, petechiae, adrenal suppression, hyperglycemia, amenorrhea, hypokalemenia, alkalosis, thromboembolism, thrombophlebitis, weight gain, muscle wasting, osteoporosis, aseptic necrosis of joints, muscle pain, allergic reactions, cushingoid appearance, increased susceptibility to infection Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression. Abdominal pain, diarrhea, flatulence, nausea, vomiting.
Dexmedatomidine/ Precedex
Sedative/ hypnotics
Dexmethylphenidate/ Focalin (XR)
Central nervous system stimulants
Hypoxia, bradycardia, sinus arrest, hypotension, transient hypertension, nauseas, vomiting, anemia, fever. Behavioral disturbances, hallucinations, insomnia, mania, nervousness, thought disorder, visual disturbances, tachycardia, abdominal pain, anorexia, nausea, growth suppression, weight loss, twitching, fever.
Dexrazoxane/ Totect, Zinecard
Cardioprotective agents
Myelosuppression, pain at injection site.
Dextroamphetamine/ Dexedrine,
Central nervous system stimulants
Hyperactivity, insomnia, restlessness, tremor,
63
Rev. 08/21/08
Dextrostate
Amphetamines
and physical exam to assess for cardiac disease. Moniot weight biweekly. Monitor height periodically in children. Assess attention span, impulse control, motor and vocal tics, and interactions with others. Observe and document frequency of narcoleptic eplisodes.
Dextromethorphan/ Balminil DM, Benylin Adult (and pediatric), broncho-Grippol-DM, Calmylin #1, childrens Hold, Creo-Terpin, Delsym, DexALone, DM syrup, Drixoral Liquid cough caps, Elixsure Childrens cough syrup, Gold, Koffex, little colds cough formula drops, mediquell, Neo-DM, Ornex-DM, PediCare Infants long acting cough drops, pertussin cough suppressant, Protussin CS, Pertussin ES, Robidex, Robitussin cough calmers, Robitussine GoughGels, Robitussin maximum strength cough suppressant, Robitussin Pediatric, sedatuss, simply cough, Sucrets cough control formula, TheraFlu thin strips long acting cough, Triaminic think strips long acting cough, Vicks 44 cough relief, Vicks formula 44
Allergy, cold, and cough remedies Antitussives
Assess frequency and nature of cough, lung sounds, and amount and type of sputum produced.
behavioral disturbances, depression, dizziness, hallucinations, headache, irritability, mania, thought disorder, palpitations, tachycardia, arrhythmias, hypertension, anorexia, constipation, cramps, diarrhea, dry mouth, metallic taste, nausea, vomiting, erectile dysfunction, increased libido, urticaria, physical dependence, psychological dependency. Dizziness, sedation, nausea
64
Rev. 08/21/08
pediatric formula Dextrose/ Glucose, Glutose, Instaglucose, Insulin Reaction caloric sources carbohydrates Assess hydration status of patients receiving IV. Monitor intake/output and electrolyte concentrations. Assess patient for dehydration and edema. Assess nutritional status, function of gastrointestinal tract, and caloric needs. Diabetic patients and patients receiving hypertonic dextrose solution should have serum glucose, potassium, and phosphate monitored regularly. Monitor IV site for phlebitis and infection. Monitor blood pressure, pulse, and respiratory rate prior to therapy. Conduct regular assessment of continued need for treatment. Assess mental status and degree of anxiety. Assess level of sedation. Assess patient routinely for signs and symptoms of congestive heart failure, blood pressure and pulse every 5 min until stable and then hourly, signs of hyperglycemia, blood glucose on diabetic patients Assess integrity of involved skin and mucous membranes, signs of infection or irritation, type, location, and intensity of pain before and a few minutes after administration of anesthetic Assess pain and limitation of movement; note type, location, and intensity before and 3060 min after administration. Assess arthritic pain (note type, location, intensity) and limitation of movement, lesions. Inappropriate insulin secretion, fluid overload, hypokalemia, hypomagnesemia, hypophophatemia, local pain/irritation at IV site, glycosuria, hyperglycemia.
Diazepam/Valium
Benzodiazepines, antianxiety agents, anticonvulsants, sedative/hypnotics, skeletal muscle relaxants
dizziness, drowsiness, lethargy, respiratory depression, depression, hangover, ataxia, slurred speech, headache, paradoxical excitation, rashes, physical dependence, psychological dependence, tolerance. dizziness, headache, hypotension, tachycardia, angina, edema, flushing, hirsutism, hyperglycemia, hyperuricemia, sodium and water retention, nausea, vomiting, constipation, phlebitis at IV site, weakness. Mucosal usedecreased or absent gag reflex. Topical useburning, edema, irritation, stinging, tenderness, urticaria. allergic reactions including anaphylaxis dizziness, headache, hypertension, tinnitus, GI bleeding, abdominal pain, constipation, diarrhea, dyspepsia, flatulence, heartburn, liver enzyme elevation, nausea, vomiting, acute renal failure, hematuria, exfoliative dermatitis, stevensjohnson syndrome, toxic epidermal necrolysis, pruritis, rashes, eczema, photosensitivity, edema, anemia, prolonged bleeding
Diazoxide/Hyperstat, Proglycem
antihypertensives hyperglycemic vasodilators
Dibucaine/ Nupercainal
anesthetics topical local
Diclofenac potassium/ Cataflam
nonopioid analgesics nonsteroidal anti inflammatory agents
65
Rev. 08/21/08
Diclofenac sodium/ Voltaren
nonopioid analgesics nonsteroidal anti inflammatory agents
Assess pain and limitation of movement; note type, location, and intensity before and 3060 min after administration. Assess arthritic pain (note type, location, intensity) and limitation of movement, lesions.
Diclofenac topical/ Solaraze
nonopioid analgesics nonsteroidal anti inflammatory agents
Assess pain and limitation of movement; note type, location, and intensity before and 3060 min after administration. Assess arthritic pain (note type, location, intensity) and limitation of movement, lesions.
Diclofenac (topical patch)/ Flector
nonsteroidal anti inflammatory agents analgesics
Dicloxacillin/ Dycill, Dynapen, Pathocil
anti-infectives penicillinase resistant penicillins
Assess pain and limitation of movement; note type, location, and intensity before and 3060 min after administration. Assess arthritic pain (note type, location, intensity) and limitation of movement, lesions. Assess for infection, signs and symptoms of anaphylaxis
time, allergic reactions including anaphylaxis. Topical onlycontact dermatitis, dry skin, exfoliation. dizziness, headache, hypertension, tinnitus, GI bleeding, abdominal pain, constipation, diarrhea, dyspepsia, flatulence, heartburn, liver enzyme elevation, nausea, vomiting, acute renal failure, hematuria, exfoliative dermatitis, stevensjohnson syndrome, toxic epidermal necrolysis, pruritis, rashes, eczema, photosensitivity, edema, anemia, prolonged bleeding time, allergic reactions including anaphylaxis. Topical onlycontact dermatitis, dry skin, exfoliation. dizziness, headache, hypertension, tinnitus, GI bleeding, abdominal pain, constipation, diarrhea, dyspepsia, flatulence, heartburn, liver enzyme elevation, nausea, vomiting, acute renal failure, hematuria, exfoliative dermatitis, stevensjohnson syndrome, toxic epidermal necrolysis, pruritis, rashes, eczema, photosensitivity, edema, anemia, prolonged bleeding time, allergic reactions including anaphylaxis. Topical onlycontact dermatitis, dry skin, exfoliation. edema, hypertension, GI bleeding, liver enzymes, renal toxicity, stevens-johnson syndrome, toxic epidermal necrolysis, local reactions at treatment site, rash, allergic reactions including anaphylatoid reactions. Seizures, diarrhea, epigastric distress, nausea, vomiting, pseudomembranous colitis, liver enzymes, interstitial nephritis, rash, urticaria, eosinophilia, leucopenia,
66
Rev. 08/21/08
Dicyclomine/ Bentyl
antispasmodics anticholinergics
Assess patient for symptoms of irritable bowel syndrome, abdominal distention and auscultate for bowel sounds, intake and output ratios
Didanosine/ ddI, Dideoxyinosine, Videx, Videx EC
antiretrovirals nucleoside reverse transcriptase inhibitors
Monitor for change in severity of HIV symptoms and for symptoms of opportunistic infection, peripheral neuropathy, symptoms of pancreatitis
Difenoxin/atropine// Motofen
antidiarrheals anticholinergics
Assess the frequency and consistency of stools and bowel sounds, fluid and electrolyte balance and skin turgor for dehydration
Diflorasone/ Florone, Florone E, Psorcon,
anti inflammatories steroidal
Assess affected skin. Note degree of inflammation and
allergic reactions including anaphylaxis and serum sickness, superinfection confusion (increased in geriatric patients), drowsiness, light-headedness (IM only), blurred vision, increased intraocular pressure, palpitations, tachycardia, paralytic ileus, constipation, heartburn, decreased salivation, dry mouth, nausea, vomiting, erectile dysfunction, urinary hesitancy, urinary retention, decreased sweating, decreased lactation, pain/redness at IM site, allergic reactions including anaphylaxis Seizures, headache, dizziness, insomnia, lethargy, pain, weakness, rhinitis, ear pain, epistaxis, optic neuritis, parotid gland enlargement, photophobia, retinal depigmentation, sialoadenitis, cough, asthma, arrhythmias, edema, hypertension, vasodilation, liver failure, pancreatitis, anorexia, diarrhea, liver function abnormalities, nausea, vomiting, abdominal pain, constipation, dry mouth, dyspepsia, flatulence, hepatic steatosis, stomatitis, urinary frequency, alopecia, ecchymoses, rash, fat redistribution, hyperglycemia, granulocytopenia, anemia, bleeding, leucopenia, lactic acidosis, hyperlipidemia, hyperuricemia, weight loss, rhabdomyolysis, arthritis, myalgia, peripheral neuropathy, poor coordination, chills, fever, anaphylactoid reactions. dizziness, confusion, drowsiness, headache, insomnia, nervousness, blurred vision, dry eyes, tachycardia, constipation, dry mouth, epigastric distress, ileus, nausea, vomiting, urinary retention, flushing. allergic contact dermatitis, atrophy, burning, dryness,
67
Rev. 08/21/08
Psorcon E
corticosteroids
pruritus.
Diflunisal/ Dolobid
nonopioid analgesics nonsteroidal anti inflammatory agents salicylic acid derivatives
Assess pain and range of motion, BP, pain (type, location, and intensity) before and 12 hr after administration
Difluprednate (ophthalmic)/ Durezol
ocular agents corticosteroids
Assess affected eye for pain and swelling, intraocular pressure of difluprednate is used more than 10 days
Digoxin/ Digitek, Lanoxicaps, Lanoxin
antiarrhythmics inotropics digitalis glycosides
Digoxin immune Fab/ Digibind, DigiFab Dihydroergotamine/ D.H.E. 45, Migranal
antidotes antibody fragments vascular headache suppressants ergot alkaloids
Diltiazem/ Cardizem, Cardiazem CD, Cardizem
antianginals antiarrhythmics (class IV)
Monitor apical pulse for 1 full min before administering. Monitor blood pressure periodically in patients receiving IV digoxin, ECG throughout IV administration and 6 hours after each dose, peripheral edema, and auscultate lungs for rales/crackles. Observe IV site for redness or infiltration; extravasation can lead to tissue irritation and sloughing Monitor ECG, pulse, blood pressure, and body temperature, signs of CHF Assess frequency, location, duration, and characteristics (pain, nausea, vomiting, visual disturbances) of chronic headaches. During acute attack, assess type, location, and intensity of pain before and 60 min after administration. blood pressure and peripheral pulses, signs of ergotism, nausea and vomiting Monitor blood pressure and pulse, signs of CHF, location, duration, intensity,
edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression dizziness, drowsiness, headache, tinnitus, arrhythmias, in blood pressure, chest pain, edema, GI bleeding, abdominal discomfort, nausea, constipation, diarrhea, dyspepsia, vomiting, renal failure, rash, blood dyscrasias, prolonged bleeding time, allergic reactions including anaphylaxis, chills. intraocular pressure, blepharitis, cataracts, conjunctival hyperemia, corneal edema, delayed healing, eye pain, infections, iritis, photophobia. fatigue, headache, weakness, blurred vision, yellow or green vision, arrhythmias, bradycardia, ECG changes, AV block, S-A block, anorexia, nausea, vomiting, diarrhea, gynecomastia, thrombocytopenia, electrolyte imbalances with acute digoxin toxicity.
re-emergence of atrial fibrillation, re-emergence of CHF, hypokalemia. Dizziness, rhinitis, MI, hypertension, angina pectoris, arterial spasm, intermittent claudication, abdominal pain, nausea, vomiting, altered taste, diarrhea, polydipsia, extremity stiffness, muscle pain, stiff neck, stiff shoulders, leg weakness, numbness or tingling in fingers or toes, fatigue. abnormal dreams, anxiety, confusion, dizziness, drowsiness, headache,
68
Rev. 08/21/08
LA, Cardizem SR, Cartia XT, Dilacor XR, Diltia XT, Nu-Diltiaz, Taztia XT, Tiazac
antihypertensives calcium channel blockers
and precipitating factors of patient's anginal pain, ECG,
Dimenhydrinate/ Calm X, Dimetabs, Dinate, Dramamine, Dramanate, Hydrate, Triptone Caplets
antiemetics antihistamines
Assess nausea, vomiting, bowel sounds, and abdominal pain, intake and output, including emesis, signs of dehydration
Dimercaprol/ British antilewisite, BAL in Oil
antidotes chelating agents
Monitor blood pressure and pulse throughout therapy. Systolic blood pressure may rise, and tachycardia may occur 1530 min after administration. Blood pressure usually returns to normal within 2 hr. intake and output, temperature
Dinoprostone/ Cervidil Vaginal Insert, Prepidil Endocervical Gel, Prostin
cervical ripening agent oxytocics prostaglandins
Monitor frequency, duration, and force of contractions and uterine resting tone. Monitor temperature, pulse,
nervousness, psychiatric disturbances, weakness, blurred vision, disturbed equilibrium, epistaxis, tinnitus, cough, dyspnea, arrhythmias, CHF, peripheral edema, bradycardia, chest pain, hypotension, palpitations, syncope, tachycardia, abnormal liver function studies, anorexia, constipation, diarrhea, dry mouth, dysgeusia, dyspepsia, nausea, vomiting, dysuria, nocturia, polyuria, sexual dysfunction, urinary frequency, dermatitis, erythema multiforme, flushing, increased sweating, photosensitivity, pruritus/urticaria, rash, gynecomastia, hyperglycemia, anemia, leukopenia, thrombocytopenia, weight gain, joint stiffness, muscle cramps, paresthesia, tremor, stevens-johnson syndrome, gingival hyperplasia. drowsiness, dizziness, headache, paradoxical excitation (children), blurred vision, tinnitus, hypotension, palpitations, anorexia, constipation, diarrhea, dry mouth, dysuria, frequency, photosensitivity, pain at IM site. Seizures, headache, nervousness, blepharospasm, unpleasant breath odor, increased blood pressure, tachycardia, abdominal pain, nausea, salivation, vomiting, dysuria, nephrotoxicity, hemolysis (in G6PD-deficient patients), transient leukopenia (increased in children), thrombocytopenia, pain at IM site, sterile abscesses at IM site, muscle ache, paresthesia, burning sensation in lips, mouth, throat, eyes, or penis, feeling of constriction in throat, chest, or hands, fever uterine contractile abnormalities, warm feeling in vagina, back pain, fever. Suppository: headache,
69
Rev. 08/21/08
E Vaginal Suppository
and blood pressure, Auscultate breath sounds, nausea, vomiting, and diarrhea, amount and type of vaginal discharge, symptoms of hemorrhage. Monitor uterine activity, fetal status, and dilation and effacement of cervix allergy, cold and cough remedies antihistamines antitussives Assess for urticaria and for patency of airway; degree of nasal stuffiness, rhinorrhea, and sneezing; movement disorder; sleep patterns; nausea, vomiting, bowel sounds, and abdominal pain; frequency and nature of cough, lung sounds, and amount and type of sputum produced; degree of itching, skin rash, and inflammation during therapy.
Diphenhydramine/Alle rgy Medication, AllerMax, Banophen, Benadryl DyeFree Allergy, Benadryl Allergy, Benadryl, Compoz, Compoz Nighttime Sleep Aid, Diphen AF, Diphen Cough, Diphenhist, Dormin, Genahist, 40 Winks, Hyrexin- 50, Maximum Strength Nytol, Maximum Strength Sleepinal, Midol PM, Miles Nervine, Nighttime Sleep Aid, Nytol, ScotTussin Allergy DM, Siladril, Silphen, Sleep-Eze 3, Sleepwell 2-night, Sominex, Snooze Fast, Sominex, Tusstat, Twilite, Unisom Nighttime Sleep-Aid Diphenoxylate/atropin e// Logen, Lomanate, Lomotil, Lonox
drowsiness, syncope, coughing, dyspnea, wheezing, hypotension, hypertension, diarrhea, nausea, vomiting, uterine rupture, urinary tract infection, uterine hyperstimulation, vaginal/uterine pain, allergic reactions including anaphylaxis, chills, fever. Drowsiness, dizziness, headache, paradoxical excitation (increased in children), blurred vision, tinnitus, hypotension, palpitations, anorexia, dry mouth, constipation, nausea, dysuria, frequency, urinary retention, photosensitivity, chest tightness, thickened bronchial secretions, wheezing, pain at IM site.
antidiarrheals anticholinergics
Assess the frequency and consistency of stools and bowel sounds, fluid and electrolyte balance and skin turgor for dehydration
Dipyridamole/ Dipridacot, Persantine, Persantine IV
antiplatelet agents diagnostic agents (coronary vasodilators) platelet adhesion inhibitors
Monitor blood pressure and pulse. Monitor vital signs during and for 1015 min after infusion. Obtain ECG in at least 1 lead. If severe chest pain or bronchospasm occurs, administer IV aminophylline 50250 mg at a rate of 50100 mg over
dizziness, confusion, drowsiness, headache, insomnia, nervousness, blurred vision, dry eyes, tachycardia, constipation, dry mouth, epigastric distress, ileus, nausea, vomiting, urinary retention, flushing. dizziness, headache, syncope, nausea, diarrhea, GI upset, vomiting, rash. IV onlytransient cerebral ischemia, weakness, bronchospasm, MI, hypotension, arrhythmias, flushing.
70
Rev. 08/21/08
3060 sec. Dirithromycin anti-infectives Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC) at beginning of and throughout course of therapy Monitor blood pressure, pulse, and ECG before and routinely throughout therapy. Check pulse before administering medication Assess patient for recent alcohol use. Monitor liver function tests at baseline, after 1014 days of therapy, and periodically thereafter. Monitor CBC and blood chemistry every 6 months during therapy. Monitor CBC, platelet count, and bleeding time prior to and periodically during therapy; Assess location, duration, and characteristics of seizure activity; Monitor frequency of migraine headaches; Assess mood, ideation, and behavior frequently Monitor blood pressure, heart rate, ECG, pulmonary capillary wedge pressure (PCWP), cardiac output, CVP, and urinary output continuously during the administration. Palpate peripheral pulses and assess appearance of extremities routinely throughout administration. Monitor potassium concentrations during therapy Monitor vital signs before and after administration; Monitor CBC and differential before each treatment Assess skin lesions prior to and periodically throughout therapy Assess for abdominal distention, presence of bowel sounds, and usual pattern of bowel function; Assess color, consistency, dizziness/vertigo, headache, insomnia, abdominal pain, diarrhea, vaginitis, dyspnea
Disopyramide
antiarrhythmics
constipation, dry mouth,urinary hesitancy, urinary retention
Disulfiram/ Antabuse
alcohol abuse therapy adjuncts enzyme inhibitors
Divalproex sodium
anticonvulsants, vascular headach suppressants
Drowsiness, fatigue, headache, psychoses, optic neuritis, hepatic toxicity, metallic/garlic-like taste, erectile dysfunction, acneiform eruptions, allergic dermatitis, peripheral neuritis/neuropathy, polyneuritis. agitation, dizziness, headache, insomnia, sedation, visual disturbances, tremor, abdominal pain, anorexia, anorexia, diarrhea, indigestion, nausea, vomiting
DOBUTamine/ Dobutrex
inotropics adrenergics
Headache, shortness of breath, hypertension, increased heart rate, premature ventricular contractions, angina pectoris, arrhythmias, hypotension, palpitations, nausea, vomiting, phlebitis, hypersensitivity reactions including skin rash, fever, bronchospasm or eosinophilia, nonanginal chest pain. fatigue, weakness, peripheral edema, diarrhea, nausea, stomatitis, vomiting, alopecia, rashes, anemia, thrombocytopenia acne, skin, itching, rash
Docetaxel
antineoplastics
Docosanol/Abreva
antivirals (topical)
Docusate
laxative
Throat irritation. mild cramps rashes
71
Rev. 08/21/08
Docusate calcium
laxative
Docusate sodium/Colace
stool softeners; laxative
Docusate sodium/senna
laxative
Dofetilide
antiarrhythmics
Dolasetron
antiemetics
and amount of stool produced Assess for abdominal distention, presence of bowel sounds, and usual pattern of bowel function; Assess color, consistency, and amount of stool produced Assess patient for abdominal distention, presence of bowel sounds, and normal pattern of bowel function; color, consistency, and amount of stool produced Assess patient for abdominal distention, presence of bowel sounds, and normal pattern of bowel function; color, consistency, and amount of stool produced Creatinine clearance must be calculated for all patients prior to administration and every 3 months during therapy; Assess the patient's medication history including OTC, Rx, and natural/herbal products, with emphasis on those that interact with dofetilide; Monitor ECG, pulse, and blood pressure continuously during initiation of therapy Assess patient for nausea, vomiting, abdominal distention, and bowel sounds before and after administration Administer Mini-Mental Status Exam (MMSE) initially and periodically as a screening tool to rate cognitive functioning; Administer Clock Drawing Test initially and periodically as a screening tool to measure severity of dementia Monitor blood pressure, heart rate, pulse pressure, ECG, pulmonary capillary wedge pressure (PCWP), cardiac output, CVP, and urinary output continuously during administration. Monitor urine output
Throat irritation. mild cramps rashes
Throat irritation. mild cramps rashes
electrolyte imbalances,, dehydration, abdominal cramps, nausea, vomiting, diarrhea, rashes, urine discoloration dizziness, headache, ventricular arrhythmias, chest pain, QT interval prolongation
Donepezil
anti-Alzheimers's agents
headache (increased in cancer patients), dizziness, fatigue, syncope, bradycardia, ECG changes, hypertension, hypotension, tachycardia, diarrhea, dyspepsia. headache, abnormal dreams, depression, diarrhea, nausea
DOPamine/ Intropin
inotropics vasopressors adrenergics
Headache, mydriasis (high dose), dyspnea, arrhythmias, hypotension, angina, ECG change, palpitations, vasoconstriction, nausea, vomiting, piloerection, irritation at IV site.
72
Rev. 08/21/08
Doripenem
anti-infectives
Dornase alfa
cystic fibrosis therapy adjuncts
Doxacurium
neuromuscular blocking agents nondepolarizing
Doxapram
central nervous system stimulants
Doxazosin
antihypertensives
Doxepin
antianxiety agents, antidepressants, antihistamines
frequently throughout administration. Palpate peripheral pulses and assess appearance of extremities routinely during administration. Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC) at beginning of and during therapy; Obtain a history before initiating therapy to determine previous use of and reactions to penicillins, cephalosporins or carbapenems; Obtain specimens for culture and sensitivity before initiating therapy Assess vital signs and respiratory status (lung sounds, respiratory rate, amount and color of sputum, dyspnea) periodically throughout therapy. Incidence of cough, rash, and rhinitis is greater in children under 5 yr Monitor ECG, heart rate, and blood pressure throughout administration; Neuromuscular response should be monitored with a peripheral nerve stimulator intraoperatively; Assess respiratory status continuously throughout therapy Because of narrow margin of safety and indications for use, patient must be monitored constantly when receiving doxapram and until patient is fully alert for 3060 min; Monitor ABGs prior to and every 30 min during therapy; Monitor vital signs, ECG, and hemodynamic parameters Monitor blood pressure and pulse 26 hr after first dose, with each increase in dose, and periodically during therapy Monitor blood pressure and pulse rate prior to and during initial therapy;
headache, pseudomembranous colitis, diarrhea, nausea, liver enzymes.
sore throat, voice alteration, conjunctivitis, hoarseness, rhinitis, chest pain, rash
rash, atracuriumskin flushing, allergic reactions including anaphylaxis
Seizures, apprehension, disorientation, dizziness, headache, gagging, mydriasis, laryngospasm, bronchospasm, cough, dyspnea, hiccups, rebound hypoventilation, tachypnea
dizziness, headache, first-dose orthostatic hypotension, abnormal vision, blurred vision, conjunctivitis, epistaxis fatigue, sedation, blurred vision, hypotension, constipation, dry mouth
73
Rev. 08/21/08
Doxercalciferol
vitamins
DOXOrubicin hydrochloride/ Adriamycin PFS, Adriamycin RDF, Rubex
antineoplastics anthracyclines
DOXOrubicin hydrochloride liposome
antineoplastics
DOXOrubicin, liposomal
antineoplastics anthracyclines
Doxycycline
anti-infectives
Assess weight and BMI initially and throughout treatment; Assess degree and manifestations of anxiety prior to and during therapy; Assess the type, location, and severity of pain prior to and periodically during therapy; Assess pruritic area prior to and periodically during therapy Assess for symptoms of vitamin deficiency prior to and periodically during therapy; Assess patient for bone pain and weakness prior to and during therapy; Serum ionized calcium, phosphorus, and intact PTH concentrations should be monitored prior to initiation of therapy Monitor blood pressure, pulse, respiratory rate, and temperature; bone marrow depression; bleeding; intake and output ratios; signs of cardiac toxicity; and oral mucosa frequently for development of stomatitis before and periodically during therapy. Severe and protracted nausea and vomiting may occur as early as 1 hr after therapy and may last 24 hr. Monitor CBC and differential prior to and periodically during therapy. Monitor CBC and differential prior to and periodically during therapy; Monitor renal (BUN and creatinine) and hepatic (AST, ALT, LDH, and serum bilirubin) function prior to and periodically during therapy Monitor CBC and differential prior to and periodically during therapy; Monitor renal (BUN and creatinine) and hepatic (AST, ALT, LDH, and serum bilirubin) function prior to and periodically during therapy Assess for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC) at beginning of
dizziness, headache, malaise, dyspnea, edema, nausea, vomiting
Recall pneumonitis, cardiomyopathy, ECG changes, diarrhea, esophagitis, nausea, stomatitis, vomiting, red urine, alopecia, photosensitivity, sterility, prepubertal growth failure with temporary gonadal impairment (children only), anemia, leukopenia, thrombocytopenia, phlebitis at IV site, tissue necrosis, hyperuricemia, hypersensitivity reactions.
nausea, anemia, leukopenia, thrombocytopenia, anaphylactoid allergic reactions, acute infusionrelated reactions, fever.
nausea, anemia, leukopenia, thrombocytopenia, anaphylactoid allergic reactions, acute infusionrelated reactions, fever.
Pseudomembranous colitis, diarrhea, nausea, vomiting, photosensitivity
74
Rev. 08/21/08
Dronabinol
antiemetics
Droperidol
sedative/hypnotics
Drotrecogin/ Xigris
activated protein c human anti-infectives
Duloxetine
antidepressants
Dutasteride
benign prostatichyperplasi a bph agents
Dyclonine/ Sucrets Children's Sore Throat, Dyclone, Sucrets Maximum Strength, Vapor Lemon Sucrets
anesthetics topical local
and during therapy; Obtain specimens for culture and sensitivity before initiating therapy Assess nausea, vomiting, appetite, bowel sounds, and abdominal pain prior to and following the administration of this drug; Monitor hydration, nutritional status, and intake and output Assess nausea, vomiting, hydration status, bowel sounds, and abdominal pain prior to and following administration; Monitor blood pressure and heart rate frequently during therapy Assess for signs of bleeding, hemorrhage, and infection. Use PT to monitor coagulation status of patients receiving drotrecogin. Monitor blood pressure before and periodically during therapy; Assess suicidal tendencies in both adults and children, especially in early therapy or during dose changes; Assess mental status Digital rectal examinations should be performed before and periodically during therapy for BPH; Assess patient for symptoms of prostatic hyperplasia Assess integrity of involved skin and mucous membranes, signs of infection or irritation, type, location, and intensity of pain before and a few minutes after administration of anesthetic
anxiety, concentration difficulty, confusion, dizziness, drowsiness, dry mouth
Seizures, extrapyramidal reactions, hypotension, tachycardia
Bleeding
Seizures, suicidal thoughts, fatigue, drowsiness, insomnia, hepatotoxicity, appetite, constipation, dry mouth, nausea,dysuria
decreased libido, ejaculation disorders, erectile dysfunction, rash, urticaria.
Mucosal usedecreased or absent gag reflex. Topical useburning, edema, irritation, stinging, tenderness, urticaria. allergic reactions including anaphylaxis
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Echinacea
anti-infectives antipyretics
Assess frequency of illness during therapy.
Dizziness, fatigue, headache, somnolence, heartburn, n/v, tingling sensation on tongue, sore throat, heartburn, allergic reaction, abdominal pain, rash, diarrhea, fever
75
Rev. 08/21/08
Econazole (Spectazole) Eculizumab (Soliris)
antifungals (topical) hemostatic agent complement inhibitors
Inspect involved areas of skin Monitor for infusion reaction during administration.
Edentate calcium disodium
antidotes chelating agents
Monitor intake and output and daily weight; LOC before and during therapy.
Efalizumab (Raptiva)
antipsoriatics monoclonal antibodies
Assess for signs of infections before and during therapy.
Efavirenz (Sustiva)
antiretrovirals non-nucleoside reverse transcriptase inhibitors
Assess for rash, CNS and psychiatric symptoms before and during therapy.
Eflornithine (topical) (Vaniqa) Eletriptan (Relpax)
facial hair removers (topical) vascular headache suppressants; five ht1 agonists
Eltrombopag (Promacta)
Emtricitabine (Emtriva)
antithrombocytopenic thrombopoetin receptor agonists antiretroviral; nucleoside reverse transcriptase inhibitors
Assess facial hair before administration. Assess pain location, intensity, character, duration, and associated symptoms before and during therapy. Monitor for unusual bleeding; signs/ symptoms of cataracts before and during therapy. Monitor HIV symptoms before and during therapy.
Burning, itching, local hypersensitivity reactions, redness, stinging Meningococcal infections, headache, back pain, nasopharyngitis, nausea, fatigue, sinusitis, cough, constipation, myalgia, extremity pain, herpes simplex infection, influenza-like illness Nephrotoxicity, headache, n/v, lacrimation, nasal congestion, sneezing, arrhythmia, ECG changes, hypotension, anemia, anorexia, glycosuria, myalgia, proteinuria, hypercalcemia, zinc deficiency, pain at IM site, phlebitis at IV site, fever, arthralgia, numbness, tingling, tremor, chills, excessive thirst Malignancies, serious infections, headache, photosensitivity, worsening of psoriasis, pain, arthritis, toxic epidermal necrolysis, fever, hemolytic anemia, arthralgia, dose reactions, thrombocytopenia, first hypersensitivity reactions, inflammatory/ immune mediated reactions Rash, nausea, fatigue, renal calculi, abnormal dreams, dizziness, drowsiness, headache, insomnia, impaired concentration, nervousness, psychiatric symptomatology, abdominal pain, anorexia, diarrhea, dyspepsia, pruritus, flatulence, hematuria, hypoesthesia, increased sweating Burning, rash, stinging, tingling Dizziness, drowsiness, weakness, chest tightness/ pressure, abdominal pain, dry mouth, dysphagia, nausea, paresthesia Hepatotoxicity, bone marrow changes, development or worsening of cataracts Severe hepatomegaly with steatosis, lactic acidosis, dizziness, rash, headache, diarrhea, insomnia, weakness,
76
Rev. 08/21/08
Enalapril/ Enalaprilat// Vasotec, Vasotec IV
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor weight and assess patient routinely for resolution of fluid overload. Monitor renal function.
Enfuvirtide (Fuzeon)
antiretrovirals fusion inhibitors
Assess for injection site reactions before and during therapy.
Enoxaparin (Lovenox)
anticoagulants antithrombotics low molecular weight heparins
Assess for signs of bleeding and hemorrhage before and during therapy.
Entacapone (Comtan)
antiparkinson agents; catechol omethyltransferase inhibitors
Monitor for diarrhea, assess parkinsonian and EPS symptoms before and during therapy.
Entecavir (Baraclude)
antivirals nucleoside analogues antiasthmatics bronchodilators vasopressors adrenergics
Monitor liver function
Epinephrine/Adrenalin , Ana-Guard, AsthmaHaler Mist, AsthmaNefrin (racepinephrine), EpiPen, microNefrin, Nephron, Primatene, Sus-Phrine, S-2
Assess lung sounds, respiratory pattern, pulse, and blood pressure; pulmonary function tests; ECG; and nasal and sinus congestion before administration and during peak of medication. Symptoms of overdose include persistent agitation, chest pain or discomfort,
abdominal pain, nausea, cough, depression, nightmares, dyspepsia, skin discoloration, vomiting, fat redistribution, neuropathy, paresthesia, arthralgia, myalgia, rhinitis Dizziness, fatigue, headache, vertigo, weakness, cough, hypotension, chest pain, abdominal pain, diarrhea, nausea, vomiting, proteinuria, impaired renal function, rashes, hyperkalemia, dyspnea, angioedema. Fatigue, diarrhea, injection site reactions, nausea, cough, conjunctivitis, pneumonia, sinusitis, abdominal pain, dry mouth, anorexia, pancreatitis, weight loss, myalgia, herpes simplex, limb pain, hypersensitivity reactions, Bleeding, anemia, dizziness, headache, insomnia, urinary retention, edema, reversible increase in liver enzymes, n/v, constipation, ecchymoses, pruritus, hyperkalemia, rash, urticaria, irritation, fever, thrombocytopenia, erythema at injection site, hematoma, pain Neuroleptic malignant syndrome, rhabdomyolysis, dizziness, hallucinations, syncope, diarrhea, pulmonary infiltrates, pleural effusion, pleural thickening, nausea, hypotension, abdominal pain, retroperitoneal fibrosis, brownish-orange discoloration of urine, dyskinesia Hepatomegaly w/steatosis, lactic acidosis, dizziness, rash, fatigue, headache, dyspepsia, nausea Nervousness, restlessness, tremor, headache, insomnia, paradoxical bronchospasm (excessive use of inhalers), angina, arrhythmias, hypertension, tachycardia, nausea, vomiting, hyperglycemia.
77
Rev. 08/21/08
Epirubicin (Ellence)
antineoplastics anthracyclines
decreased blood pressure, dizziness, hyperglycemia, hypokalemia, seizures, tachyarrhythmias, persistent trembling, and vomiting. Monitor CBC, bone marrow depression, ECG before and during therapy.
Eplerenone/ Inspra
antihypertensives aldosterone antagonists
Epoetin
antianemics hormones
Monitor blood pressure periodically during therapy. Monitor serum potassium levels prior to starting therapy, within the first wk, at 1 month following start of therapy or dose adjustmentand periodically thereafter. BP, monitor for symptoms of anemia before and during therapy.
Cardiotoxicity, leucopenia, anaphylaxis, infection, alopecia, n/v, lethargy, anorexia, diarrhea, mucositis, flushing, radiation-recall reaction, itching, rash, photosensitivity, skin/nail hyperpigmentation, gonadal suppression, anema, tissue necrosis, thrombocytopenia, treatment-related leukemia/ myelodysplastic syndromes, injection site reactions, hot flashes, phlebitis at IV site, hyperuricemia Dizziness, fatigue, abnormal liver function tests, abdominal pain, diarrhea, albuminuria, abnormal vaginal bleeding, gynecomastia, hyperkalemia, hypercholesterolemia, hypertriglyceridemia, flu-like symptoms. Seizures, stroke, CHF, thrombotic events, MI, hypertension, headache, transient rashes, restored fertility, resumption of menses, increased mortality and tumor growth. Anxiety, headache, dizziness, tachycardia, hypotension, n/v, chest pain, abdominal pain, diarrhea, flushing, myalgia, jaw pain, hypesthesia/ hyperesthesia/paresthesia, flu-like symptoms, dyspnea, injection site reactions Angioedema, depression, fatigue, hypotension, rhinitis, pharyngitis, hyperkalemia, abdominal pain, impaired renal function, pain Bleeding including GI and intracranial, hematuria, and hematomas, hypotension Pancreatitis, dizziness, headache, malaise, weakness, somnolence, conjunctivitis, photophobia, rhinorrhea, dry mouth, edema, hypertension, dyspnea, arrhythmias, liver
Epoprostenol
vasodilators prostaglandins
Monitor hemodynamic parameters before and during therapy.
Eprosartan (Teveten)
antihypertensives angiotensin ii receptor antagonists antiplatelet agents glycoprotein iib iiia inhibitors fat soluble vitamins
BP (lying, sitting, standing), and pulse before and during therapy.
Eptifibatide (Integrilin) Ergocalciferol (Drisdol, Vitamin D2)
Assess for bleeding before and during therapy. Assess for vitamin deficiency, bone pain and weakness, hypocalcemia before and during therapy.
78
Rev. 08/21/08
Ergonovine (ergometrine, Ergotrate)
oxytocics
BP, pulse, and respirations q 15-30 minutes before and during therapy.
Ergotamine (Ergomar, Ergostat)
vascular headache suppressants; ergot alkaloids
BP, peripheral pulses before and during therapy.
Erlotinib (Tarceva)
antineoplastics enzyme inhibitors
Respiratory status, liver function tests
Ertapenem (Invanz)
anti-infectives carbapenems
Assess for infection before and during therapy.
Erythromyocin oral/ E-mycin
Macrolides, antiinfectives
Assess patient for infection and bowel function
Erythromycin (parenteral) (Erythrocin)
anti-infectives macrolides
Monitor bowel function
Erythromycin topical/ Akne-Mycin, DelMycin, A/T/S, E/Gel, Emgel, Erycette, Erygel, EryMax, Erysol, ETS, Staticin, Theramycin Z, T-Stat
anti-infectives macrolides
Assess patient for prior history of hypersensitivity or allergy to erythromycin
function test elevation, weight loss, anorexia, constipation, metallic taste, n/v, polydypsia, albuminuria, azotemia, bone pain, decreased libido, muscle pain, hyperthermia, nocturia, polyuria, pruritus, metastatic calcification, hypercalcemia n/v, dizziness, headache, chest pain, tinnitus, hypertension, arrhythmias, palpitations, sweating, allergic reactions MI, hypertension, abdominal pain, n/v, dizziness, diarrhea, polydipsia, angina pectoris, stiff shoulders, intermittent claudication, stiff neck, leg weakness, extremity stiffness, fatigue, numbness/tingling in fingers or toes, muscle pain Interstitial lung disease, dyspnea, diarrhea, rash, fatigue, conjunctivitis, corneal ulceration, abdominal pain, cough, n/v, increased liver transaminase, stomatitis, anorexia, dry skin, pruritis Pseudomembranous colitis, seizures, hypersensitivity reactions, headache, n/v, diarrhea, vaginitis, phlebitis at IV site, pain at IM site Ventricular arrhythmias, pseudomembranous colitis, nausea, vomiting, allergic reactions, super infection Pseudomembranous colitis, ventricular arrhythmias, QTC prolongation, phlebitis at IV site, n/v, seizures, druginduced hepatitis, cramping, ototoxicity, hypotension, abdominal pain, infantile hypertrophic pyloric stenosis, superinfection, rashes, druginduced pancreatitis, allergic reactions rashes, pruritis, allergic reactions
79
Rev. 08/21/08
Escitalopram/Lexapro
Esmolol (Brevibloc)
selective serotonin reuptake inhibitors ssris; antidepressant antiarrhythmics beta blockers
Assess for suicidal tendencies, mood changes and level of anxiety, sexual dysfunction during therapy BP, ECG, and pulse, monitor I&Os
insomnia, diarrhea, nausea
Esomeprazole (Nexium) Estazolam (ProSom)
antiulcer agents proton pump inhibitors sedative/hypnotic benzodiazepines
Assess for epigastric or abdominal pain or blood in stool Assess sleep patterns
Estradiol
hormones; estrogens
BP, monitor I&Os
Estramustine/ Emcyt
antineoplastics hormones alkylating agents
Monitor blood pressure; intake and output ratios and weekly weight; and blood glucose closely in diabetic patients throughout therapy. Monitor hematologic and hepatic functions, serum calcium, and phosphorus periodically throughout therapy.
Estrogens (conjugated)
hormones estrogens
BP, monitor I&Os
Fatigue, hypotension, n/v, agitation, confusion, dizziness, drowsiness, weakness, peripheral ischemia, injection site reactions, sweating Headache, abdominal pain, constipation, diarrhea, dry mouth, flatulence, nausea Drowsiness, headache, weakness, abnormal thinking, behavior changes, abnormal dreams, sleep-driving, chest pain, confusion, depression, dizziness, hangover, malaise, nervousness, abdominal pain, pharyngitis, dyspepsia, cold symptoms, nausea, stiffness, lower extremity pain, physical dependence, psychological dependence, hypokinesia, back pain, abnormal coordination, body pain Thromboembolism, MI, headache, edema, intolerance to contact lenses, hypertension, nausea, weight changes, oily skin, erectile dysfunction, amenorrhea, dysmenorrhea, breast tenderness, testicular atrophy, dizziness, lethargy, vomiting, worsening of myopia or astigmatism, anorexia, loss of libido, increased appetite, jaundice, urticaria, leg cramps, breakthrough bleeding, vaginal candidiasis, cervical erosions, pigmentation, hyperglycemia, hypercalcemia, acne, sodium and water retention Insomnia, thromboembolism, edema, hypertension, diarrhea, nausea, anorexia, flatulence, vomiting, bruising, dry skin, pruritis, rashes, decreased libido, gynecomastia, gonadal suppression (azoospermia), hyperglycemia, leukopenia, thrombocytopenia, leg cramps, dyspnea, angioedema, allergic reactions. Thromboembolism, MI, headache, edema,
80
Rev. 08/21/08
Estropipate
hormones; estrogens
BP, monitor I&Os
Eszopiclone (Lunesta)
sedative/hypnotic cyclopyrrolones
Assess sleep patterns; mental status
Etanercept (Enbrel)
antirheumatics (DMARDS), anti tnf agents
Assess ROM, swelling, and pain in affected joints
Ethacrynic acid (Edecrin)
loop diuretics
BP, pulse, daily weight, I&Os
amenorrhea, hypertension, nausea, weight changes, erectile dysfunction, dysmenorrhea, oily skin, breast tenderness, testicular atrophy, acne, breakthrough bleeding, gynecomastia, lethargy, mental depression, dizziness, anorexia, insomnia, increased appetite, jaundice, vomiting, urticaria, cervical erosion, pigmentation, vaginal candidiasis, urticaria, loss of libido, hyperglycemia, hypercalcemia, Na & H2O retention, leg cramps Thromboembolism, MI, headache, edema, amenorrhea, hypertension, nausea, weight changes, erectile dysfunction, dysmenorrhea, oily skin, breast tenderness, testicular atrophy, acne, breakthrough bleeding, gynecomastia, intolerance to conact lenses, lethargy, mental depression, dizziness, anorexia, insomnia, increased appetite, jaundice, vomiting, urticaria, cervical erosion, pigmentation, vaginal candidiasis, urticaria, loss of libido, hyperglycemia, hypercalcemia, Na & H2O retention, leg cramps Abnormal thinking, behavior changes, hallucinations, chest pain, headache, depression, dry mouth, peripheral edema, rash, unpleasant taste, sleepdriving Infections, injection site reactions, upper respiratory tract infection, rhinitis, cough, dizziness, weakness, sinusitis, pharygitis, respiratory disorder, abdominal pain, dyspepsia, rash, pancytopenia, increased risk of malignancies Agranulocytosis, fatigue, dehydration, vertigo, hypochloremia, confusion, hypokalemia, headache, hyponatremia, anorexia, hypomagnesemia, hearing loss, metabolic acidosis, hypovolemia, nervousness, rash, tinnitus, hypotension,
81
Rev. 08/21/08
Ethambutol (Myambutol)
antituberculars
Assess lung sounds, visual function
Ethinyl estradiol/desogestrel (Apri 28, Desogen, Ortho-Cept, Reclipsen, Solia, Kariva, Mircette, Cesia, Cyclessa, Velivet)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethinyl estradiol/drospirenone (Yasmin, Yaz)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethinyl estradiol/ethynodiol (Kelnor 1/35, Zovia 1/35, Zovia 1/50)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium,
abdominal pain, diarrhea, n/v, excessive urination, hematuria, hyperglycemia, hyperuricemia, dry mouth Hepatitis, optic neuritis, confusion, dizziness, headache, hallucination, malaise, fever, abdominal pain, anorexia, n/v, hyperuricemia, joint pain, anaphylactoid reactions, peripheral neuritis, depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema,
82
Rev. 08/21/08
triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethinyl estradiol/etonogestrel (NuvaRing)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethinyl estradiol/levonorgestr el (Alesse-28, Aviane28, Lessina-28, Levlen-28, Levlite-28, Levora-28, Lutera, Nordette-28, Portia28, Sronyx, Enpresse, Tri-Levlen, Triphasil 28, Trivora 28, Lybrel, Seasonale, Seasonique)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethinyl estradiol/norelgestrom in (Ortho Evra)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum
hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change, uterine imbedment/uterine rupture. depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary
83
Rev. 08/21/08
glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethinyl estradiol/norethindron e (Balziva, Brevicon, Femcon Fe, Junel 21 1/20, Junel 21 1.5/20, Junel Fe 1/20, Junel Fe 1.5/30, Loestrin 21 1/20, Loestrin 21 1.5/30, Loestrin Fe 1/20, Loestrin Fe 1.5/30, Microgestin Fe 1/20, Modicon, Necon 0.5/35, Necon 1/35, Norethin 1/35E, Norinyl 1+ 35, Nortrel 0.5/35, Nortrel 1/35, Ortho-Novum 1/35, Ovcon 35, Ovcon 50, Zenchant, Necon 10/11, Ortho-Novum 10/11, Aranelle, Leena, Necon 7/7/7, Nortrel 7/7/7, OrthoNovum 7/7/7, TriNorinyl) Ethinyl estradiol/norgestimate (MonoNessa, OrthoCyclen, Previfem, Sprintec, Ortho TriCyclen, Ortho TriCyclen Lo, Tri-Nessa, Tri-Previfem, TriSprintec)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change.
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change.
84
Rev. 08/21/08
Ethinyl estradiol/norgestrel (Cryselle, Lo/Ovral 28, Low-Ogestrel 28, Ogestrel 28)
contraceptive hormones
Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Ethosuximide (Zarontin)
anticonvulsants
Monitor CBC, hepatic function tests, urinalysis
Etidronate (Didronel)
bone resorption inhibitors; hypocalcemics; biphosphonates
Assess for bone pain, weakness, or loss of function
Etodolac (Lodine, Lodine XL)
antirheumatics; nonopioid analgesics; pyranocarboxylic acid
Assess pain, ROM
depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. Increased frequency of grand mal seizure, stevens-johnson syndrome, ataxia, fatigue, dizziness, drowsiness, myopia, euphoria, headache, irritability, hyperactivity, n/v, psychiatric disturbances, abdominal pain, anorexia, cramping, diarrhea, weight loss, hiccups, vaginal bleeding, rashes, pink/brown discoloration of urine, ataxia, urticaria, agranulocytosis, eosinophilia, leucopenia, pancytopenia, systemic lupus erythematosus Diarrhea, musculoskeletal pain, nausea, loss of taste, metallic taste, nephrotoxicity, rash, microfractures, osteonecrosis (primarily of jaw) Exfoliative dermatitis, stevensjohnson syndrome, toxic epidermal necrolysis, allergic reactions, angioedema, GI bleeding, dyspepsia, depression, malaise, dizziness, drowsiness, asthma, insomnia, nervousness, edema, syncope, weakness, abdominal pain, photophobia, palpitations, tinnitus, hypertension, CHF, constipation, diarrhea, thirst, drug-induced hepatitis, n/v, dry mouth, stomatitis, flatulence, gastritis, dysuria, renal failure, urinary frequency, prolonged bleeding
85
Rev. 08/21/08
Etomidate (Amidate)
general anasthetics; nonbarbiturates
BP, respiratory status, pulse
Etonorgestgrel (implant) (Implanon)
contraceptive hormones; progestins
BP, monitor hepatic function
Etoposide (VePesid, VP-16)
antineoplastics; podophyllotoxin derivatives
BP before and q 15 min. during infusion. Monitor for hypersensitivity reactions
Etoposide phosphate (Etopophos)
antineoplastics; podophyllotixin derivatives
BP before and q 15 min. during infusion Monitor for hypersensitivity reactions
Etravirine (Intelence)
antiretrovirals; non-nucleoside reverse transcriptase inhibitors
Assess for rash, monitor viral load and CD4 cell count
time, ecchymoses, flushing, hyperpigmentation, pruritus, rashes, sweating, anemia, thrombocytopenia, chills, fever Laryngospasm, apnea, transient skeletal muscle movements, arrhythmias, post-operative n/v, hypertension, hypotension, hyperventilation, hypoventilation, transient injection site pain Thromboembolic events, depression, hepatic adenomas, dizziness, emotional lability, headache, leukorrhea, nervousness, hypertension, dysmenorrhea, increased risk of ectopic pregnancy, irregular/ unpredictable menses, ovarian cysts, acne, breast pain, weight gain, implant site reactions, back pain Allergic reactions, anorexia, diarrhea, alopecia, leucopenia, hypotension, thrombocytopenia, anemia, n/v, drowsiness, rash, fatigue, pruritis, abdominal pain, stomatitis, urticaria, sterility, peripheral neuropathy, phlebitis at IV site, fever Allergic reactions, malaise, anorexia, mucositis, alopecia, leukopenia, anemia, thrombocytopenia, n/v, rash, dizziness, hypotension, taste alteration, constipation, fever, diarrhea, urticaria, abdominal pain, pruritis, sterility, phlebitis at IV site MI, Stevens-johnson syndrome, immune reconstitution syndrome, seizures, nausea, rash, anxiety, fatigue, confusion, headache, insomnia, sleep disorders, blurred vision, vertigo, angina pectoris, atrial fibrillation, hypertension, renal failure, abdominal pain, dry mouth, gynecomastia, anema, hyperglycemia, hepatitis, fat redistribution, hyperlipidemia, stomatitis, vomiting, hemolytic anemia, peripheral neuropathy, hemiarthrosis,
86
Rev. 08/21/08
allergic reaction Eucalyptus anti-infectives expectorant Assess frequency and nature of cough Seizures, pulmonary edema (overdose), cyanosis, delirium, drowsiness, diarrhea, epigastric pain, dyspnea, n/v Fatigue, weakness, headache, pneumonitis, cough, dyspnea, anorexia, diarrhea, mucositis, mouth ulcers, nausea, stomatitis, vomiting, dysgeusia, peripheral edema, dry skin, pruritus, rash, anemia, leukopenia, thrombocytopenia, hyperglycemia, hyperlipidemia, hypertriglyceridemia, extremity pain, infections, hypersensitivity reactions including anaphylaxis, fever. Pancreatitis, diarrhea, n/v, dizziness, headache, hyperhyrosis, gastrointestinal reflux, dyspepsia, jitteriness, weakness, decreased appetite, weight loss Cholecystitis, cholelithiasis, hepatic transaminases, nausea, pancreatitis. Rash; angioedema.
Everolimus/ Afinitor
antineoplastics kinase inhibitors
Assess for symptoms of non-infectious pneumonitis; mouth ulcers, stomatitis, or oral mucositis during therapy. Monitor renal function prior to and periodically during therapy.
Exenatide (Byetta)
antidiabetics; incretrin mimetic agents
Monitor serum glucose levels
Ezetimibe/Zetia
cholesterol absorption inhibitors; lipidlowering agent
Obtain a diet history, especially with regard to fat consumption
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
Monitor BP, pulse, and respirations; monitor for renewed or increased bleeding
be to
Common Side Effects
Factor ix (human)
Hemostatic agents blood products clotting factors
Famciclovir Famotidine/ Mylanta AR, Pepcid, Pepcid AC Maximum Strength, Pepcid RPD
antiviral antiulcer agents histamine h2 antagonists
Assess lesions and assess for posthepetic neuralgia Assess for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate. Monitor CBC with differential periodically during therapy. Assess elderly and debilitated patients routinely for confusion.
drowsiness, headache, lethargy, changes in BP, changes in HR, n/v, chills flushing, urticaria, fever, disseminated intravascular coagulation, thrombosis, tingling, dyspnea, risk for transmission of viral hepatitis and HIV virus, hypersensitivity reactions headache, dizziness, fatigue, diarrhea, n/v Confusion, dizziness, drowsiness, hallucinations, headache, arrhythmias, constipation, diarrhea, nausea, decreased sperm count, erectile dysfunction, gynecomastia, agranulocytosis, aplastic anemia, anemia, neutropenia, thrombocytopenia, pain at IM
87
Rev. 08/21/08
site, hypersensivity reactions. Fat emulsion caloric sources Monitor weights every other day. phlebitis at IV site, fever, infection, chest pain, hepatomegaly, jaundice, N&V, pancreatitis, chills, hypertriglyceridemia, hypersensitivity reactions. Intravascular fat accumulation in preterm infants only. liver function abnormalities, nausea, rash, gout flare, arthralgia
Febuxostat
Antigout agent xantine oxidase inhibitor
Felbamate
anticonvulsant
Assess for joint pain and swelling, especially during early therapy. Monitor for signs and symptoms of MI and stroke. Monitor serum uric acid levels prior to, 2 wks after intitiating, and periodically thereafter. Monitor liver function at 2 and 4 months of therapy and periodically thereafter. location, duration, and characteristics of seizure activity
Felodipine
anti-anginals antihypertensive calcium channel blockers
Monitor BP and pulse
Aplastic anemia, acute liver failure, dizziness, drowsiness, n/v, fatigue, headache, insomnia, anorexia, constipation, dyspepsia, anxiety, diplopia, psychological disturbances, pharyngitis, rhinitis, acne, sinusitis, rashes, myalgia, ataxia, flulike syndrome, weight loss. Arrhythmias, CHF, stevensjohnson syndrome, headache, peripheral edema, abnormal dreams, anxiety, confusion, dizziness, drowsiness, chest pain, nervousness, blurred vision, tinnitus, psychiatric disturbances, weakness, disturbed equilibrium, cough, epistaxis, dyspnea, bradycardia, hypotension, palpitations, syncope, n/v, tachycardia, dysuria, dry mouth, nocturia, polyuria, sexual dysfunction, urinary frequency, dermatitis, erythema multiforme, rash, flushing, anemia, increased sweating, photosensitivity, abnormal liver function studies, constipation, diarrhea, dysgeusia, pruritis/ urticaria, dyspepsia, anemia, gynecomastia, leukopenia, hyperglycemia, thrombocytopenia.
88
Rev. 08/21/08
Fennel Fenofibrate
none assigned lipid-lowering agents; fibric acid derivatives
frequency and nature of cough Assess for cholelithiasis
photosensitivity fatigue/weakness, rash, headache, arrhythmias, pancreatitis, urticaria, rhabdomyolysis, hypersensitivity reactions. headache, hypotension, tachycardia, nausea, flushing, nervousness/ anxiety, dizziness, ECG changes, peripheral edema, abdominal pain, constipation, diarrhea, vomiting, sweating, hypokalemia, injection site reactions, back pain Allergic reactions, GI bleeding, hepatitis, dyspepsia, confusion, dizziness, drowsiness, headache, renal failure, blurred vision, hearing loss, tinnitus, edema, palpitations, n/v, abdominal pain, diarrhea, constipation, discomfort, cystitis, dysuria, hematuria, pruritis, rashes, sweating Dizziness, drowsiness, abnormal thinking, confusion, hallucinations, headache, insomnia, nervousness, weakness, abnormal vision, respiratory depression, dyspnea, hypotension, nausea, constipation, dry mouth, vomiting, pruritus, rash, sweating, abnormal gait. Laryngospasm, apnea, confusion, blurred/ double vision, paradoxical excitation/delirium, postop depression, n/v, postop drowsiness, allergic bronchospasm, respiratory depression, arrhythmias, bradycardia, circulatory depression, hypotension, biliary spasm, facial itching, skeletal & facial muscle rigidity (rapid IV infusion) Apnea, confusion, dry mouth, sedation, weakness, anorexia, constipation, n/v, sweating, dizziness, bronchoconstriction, restlessness, laryngospasm, respiratory depression, bradycardia, erythema, application site reactions,
Fenoldopam
antihypertensives vasodilators
BP, heart rate, and ECG
Fenoprofen
nonopioid analgesics; propionic acid derivatives
monitor for rhinitis, asthma, and urticaria
Fentanyl
opioid analgesics opioid agonists
Monitor type, location, and intensity of pain before and 15 min after administration. Assess blood pressure, pulse, and respirations before and periodically during administration.
Fentanyl (parenteral)
Opioid analgesics Opioid agonists
respiratory rate and BP
Fentanyl (transdermal)
Opioid analgesics Opioid agonists Analgesic adjunct
BP, pulse, & respirations
89
Rev. 08/21/08
Fentanyl buccal (Fentora)
Opioid analgesics Opioid agonists
BP, pulse, and respirations
Fentanyl iontophoretic transdermal system (Ionsys)
Opioid analgesics Opioid agonists
BP, pulse, and respirations
Ferrous fumarate (33% elemental iron)
Antianemics iron supplement
assess bowel function.
Ferrous gluconate (12% elemental iron)
Antianemics iron supplement
assess bowel function
Ferrous sulfate (30% elemental iron)
Antianemics iron supplement
assess bowel function
Fesoterodine (Toviaz)
urinary tract antispasmodics; anticholinergics vascular headache suppressant
urinary urgency, frequency, and urge incontinence
Feverfew
assess for migraines
Fexofenadine/ Allegra
allergy, cold and cough remedies antihistamines
Filgrastim
colony stimulating factor
Assess allergy symptoms; lung sounds and character of bronchial secretions before and periodically during therapy. BP, heart rate, and respiratory status
skeletal & thoracic muscle rigidity, physical dependence, psychological dependence. Respiratory depression, dizziness, drowsiness, headache, n/v, application site reactions, constipation, confusion, depression, fatigue, insomnia, weakness, cough, dyspnea, abdominal pain, anorexia, diarrhea, edema, dehydration, physical dependence, psychological dependence. Respiratory depression, fever, n/v, application site reactions, anxiety, dizziness, insomnia, somnolence, pharyngitis, hypoxia, bradycardia, back pain, hyper- or hypotension, tachycardia, abdominal pain, constipation, anemia, dyspepsia, flatulence, ileus, urinary retention, itching, hypokalemia nausea, constipation, dark stools, epigastric pain, GI bleeding, dizziness, syncope, headache, temp staining of teeth, vomiting. nausea, constipation, dark stools, epigastric pain, GI bleeding, dizziness, syncope, headache, temp staining of teeth, vomiting. nausea, constipation, dark stools, epigastric pain, GI bleeding, dizziness, syncope, headache, temp staining of teeth, vomiting. dry mouth, tachycardia, constipation, nausea, upper abdominal pain, dysuria, urinary retention, back pain Post-feverfew Syndrome (anxiety, headache, insomnia, muscle & joint aches), tachycardia, n/v, diarrhea, heartburn, mouth ulceration and soreness, contact dermatitis (topical) Drowsiness, fatigue, dyspepsia, dysmenorrhea.
medullary bone pain, redness at subcut site, pain, excessive
90
Rev. 08/21/08
leukocytosis Finasteride hair regrowth stimulant; androgen inhibitors nonopioid analgesics; flavanoids anti-arrhythmias (class IC) symptoms of prostatic hyperplasia; digital rectal exams for BPH pain, ROM, degree of swelling, stiffness in joint BP, pulse, ECG, I&Os decreased libido, decreased volume of ejaculate, erectile dysfunction increased BP, increase in varicose veins, GI upset, psoriasis Arrhythmias, chest pain, CHF, blurred vision, dizziness, anxiety, fatigue, headache, anorexia, visual disturbances, n/v, mental depression, constipation, drug-induced hepatitis, rashes, stomach pain, tremor bleeding, diarrhea, gastritis, n/v, stomatitis, alopecia, erythema, maculopapular rash, anemia, leucopenia, thrombocytopenia, fatigue, headache, anorexia, ulcer, gonadal suppression, fever Hepatotoxicity, exfoliative skin disorders, headache, dizziness, seizures, allergic reactions, diarrhea, n/v, abdominal discomfort, hypertriglyceridemia, hypokalemia Seizures, aplastic anemia, diarrhea, n/v, leucopenia, pancytopenia, ataxia, confusion, dizziness, drowsiness, fatigue, chest pain, headache, hearing loss, abdominal pain, pruritis, dry mouth, photosensitivity, hypoglycemia, azotemia, hypokalemia, anemia, rash, thrombocytopenia, dyspnea, peripheral neuropathy, fever Neurotoxicity, GI bleed, pulmonary hypersensitivity, pancytopenia, fatigue, cough, pneumonia, rashes, diarrhea, anemia, leukopenia, hematuria, thrombocytopenia, agitation, coma, confusion, headache, malaise, weakness, hearing loss, visual disturbances, UTI, dyspnea, sinusitis, edema, anorexia, esophagitis, dysuria, myalgia, gonadal suppression, hemolytic anemia, peripheral neuropathy, fever
Flavocoxid (Limbrel)
Flecainide (Tambocor)
Floxuridine (FUDR)
antineoplastics antimetabolites
vital signs, I/O, abdominal pain, intra-arterial infusion site
Fluconazole (Diflucan)
antifungals (systemic)
assess infected area, monitor CSF cultures
Flucytosine (Ancobon, 5-FC)
antifungals
monitor AST, ALT, serum bilirubin, and alkaline phosphatase
Fludarabine (Fludara)
antineoplastics antimetabolites
respiratory status, visual changes, weakness, confusion, LOC
91
Rev. 08/21/08
Fludrocortisones (Florinef)
hormones corticosteroids mineralcorticoid
BP, fluid retention, serum electrolytes
Flumazenil (Romazicon)
antidotes benzodiazepines
LOC and respiratory status
Flunisolide/ AeroBid, AeroBid-M
anti inflammatories steroidal corticosteroids
Monitor respiratory status and lung sounds; withdrawal symptoms; growth in children; and changing from systemic corticosteroids to inhalation costicosteroids for signs of adrenal insufficiency. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic therapy.
Flunisolide (nasal) (Nasarel)
anti-inflammatories steroidal; corticosteroids
degree of nasal stuffiness, amount and color of discharge
Fluocinolone
anti-inflammatories steroidal; corticosteroids
affected skin; degree of inflammation and pruritus
Fluocinonide
anti-inflammatories steroidal; corticosteroids
degree of inflammation and pruritus in affected skin
dizziness, headache, anorexia, arrhythmias, edema, nausea, hypertension, weight gain, adrenal suppression, CHF, hypokaleima, hypokalemic alkalosis, arthralgia, muscle weakness, tendon contracture, ascending paralysis, hypersensitivity reactions Seizures, dizziness, n/v, agitation, confusion, fatigue, drowsiness, emotional lability, sleep disorders, abnormal hearing, abnormal vision, blurred vision, arrhythmias, hypertension, hiccups, rigors, flushing, sweating, shivering, pain/ injection-site reactions, phlebitis, paresthesia, Headache, dizziness, irritability, nervousness, palpitations, hoarseness, nasal congestion, pharyngitis, dysphonia, oropharyngeal fungal infections, rhinitis, sinusitis, bronchospasm, cough, wheezing, rash, diarrhea, nausea, taste disturbances, vomiting, abdominal pain, anorexia, dry mouth, menstrual disturbances, adrenal suppression (high-dose, longterm therapy only), decreased growth (children), flu-like syndrome. nasal burning, aftertaste, nasal dryness, nasal irritation, cough, nasopharyngeal fungal infections, nausea, adrenal suppression, decreased growth allergic contact dermatitis, atrophy, burning, folliculitis, edema, dryness, maceration, hypersensitivity reactions, hypertrichosis, irritation, hypopigmentation, miliaria, perioral dermatitis, secondary infection, adrenal suppression, striae allergic contact dermatitis, atrophy, burning, folliculitis, edema, dryness, maceration, hypersensitivity reactions, hypertrichosis, irritation, hypopigmentation, miliaria, perioral dermatitis, secondary infection, adrenal suppression,
92
Rev. 08/21/08
striae Fluoride supplements/ oral: Flura-Drops, Luride, Pharmaflur, Phos-Flur//topical: ACT, Fluorigard, Fluorinse, Gel Kam, Gel-Tin, Prevident, Stop, Thera-Flur Fluoride (topical) dental caries prophylactic agents minerals electrolytes Examine teeth for staining or mottling periodically. nausea, vomiting, atopic dermatitis, mottling of teeth
Fluorouracil/Adrucil, Efudex, Fluoroplex, 5-FU
dental caries prophylactic minerals electrolyes antineoplastics antimetabolites
examine teeth for staining or mottling
atopic dermatitis, mottling of teeth (toxicity), n/v
Fluoxetine
antidepressants Selective Serotonin Reuptake Inhibitor (SSRI)
Monitor vital signs before and frequently during therapy. Assess mucous membranes, number and consistency of stools, frequency of vomiting, signs of infection, IV site frequently for inflammation or infiltration, skin for palmar-plantar erythrodysesthesia. Monitor intake and output, appetite, and nutritional intake, and cerebellar dysfunction. Monitor hepatic, renal, and hematologic functions before and periodically throughout therapy. monitor mood and CBC counts
Acute cerebellar dysfunction, diarrhea, nausea, stomatitis, vomiting, alopecia, maculopapular rash, local inflammatory reactions (topical only), melanosis of nails, nail loss, palmar-plantar erythrodysesthesia, phototoxicity, sterility, anemia, leukopenia, thrombocytopenia, thrombophlebitis, fever.
Fluphenazine
Antipsychotics phenothiazines
BP (sitting, standing, lying); ECG; pulse; respiratory rate
Seizures, anxiety, sexual dysfunction, drowsiness, headache, insomnia, tremors, nervousness, diarrhea, pruritus, excessive sweating, abnormal dreams, dizziness, fatigue, hypomania, mania, weakness, stuffy nose, visual disturbances, cough, chest pain, palpitations, abdominal pain, abnormal taste, anorexia, constipation, dyspepsia, dry mouth, weight loss, urinary frequency, flushing, erythema nodusum, rashes, arthralgia, dysmenorrhea, myalgia, fever, hyponatremia, n/v, allergic reactions, flu-like syndrome, hot flashes, back pain, sensitivity reactions, Agranulocytosis, neuroleptic malignant syndrome, photosensitivity, EPS reactions, sedation, tardive dyskinesia, blurred vision, dry
93
Rev. 08/21/08
Flurandrenolide
anti-inflammatories steroidal; corticosteroids
assess affected skin
Flurazepam
sedative/hypnotic; benzodiazepines
Sleep patterns, mental status
Fluriboprofen
antirheumatics nonsteroidal antiinflammatory agents
pain and ROM
Flutamide (Eulexin)
antineoplastics antiandrogens
Monitor ALT
Fluticasone (Flovent HFA; Flovent Diskus)
Anti-inflammaties steroidal; corticosteroids
respiratory status and lung sounds
eyes, hypertension, anorexia, hypotension, tachycardia, dry mouth, constipation, weight gain, drug-induced hepatitis, ileus, urinary retention, rash, nausea, pigment changes, galactorrhea, leukopenia, thrombocytopenia, allergic reactions allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, secondary infection, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, striae, adrenal suppression abnormal thinking, behavior changes, confusion, daytime drowsiness, ataxia, decreased concentration, dizziness, sleep w/ driving, hallucinations, headache, lethargy, mental depression, paradoxical excitation, blurred vision, n/v, constipation, diarrhea, rashes, physical/ psychological dependence, tolerance Allergic reactions, stevensjohnson syndrome, toxic dermal necrolysis, GI bleeding, exfoliative dermatitis, abdominal pain, heartburn, nausea, dizziness, drowsiness, fever, mental depression, psychic disturbances, blurred vision, corneal opacities, tinnitus, changes in BP, palpitations, edema, bloated feeling, chills, constipation, diarrhea, drug-induced hepatitis, stomatitis, incontinence, increased sweating, rashes, prolonged bleeding time, myalgia, blood dyscrasias, Hepatotoxicity, hot flashes, diarrhea, n/v, erectile dysfunction, loss of libido, anxiety, confusion, mental depression, drowsiness, rash, edema, hypertension, photosensitivity Churg-Strauss syndrome, headache, dizziness, dysphonia, nasal stuffiness, oropharyngeal fungal
94
Rev. 08/21/08
Fluticasone nasal/ Flonase
anti inflammatory steroidal, corticosteroids
Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing
Fluticasone (topical) (Cutivate)
Anti-inflammaties steroidal; corticosteroids
degree of inflammation and pruritis in affected skin
Fluvastatin (Lescol)
lipid-lowering agents; hmg coa reductase inhibitors
serum cholesterol and triglyceride levels
Fluvoxamine (Luvox)
antidepressants antiobsessive agents SSRI
monitor mood changes
infections, hoarseness, rhinorrhea, sinusitis, upper respiratory tract infection, bronchospasm, cough, muscle pain, wheezing, diarrhea, adrenal suppression, Cushing syndrome, fever, decreased growth in children Headache, epistaxis, nasal burning, nasal irritation, nasopharyngeal fungal infection, pharyngitis, nausea, vomiting, adrenal suppression, cough allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, irritation, hypersensitivity reactions, hypertrichosis, maceration, hypopigmentation, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression Rhabdomyolysis, n/v, headache, dizziness, fatigue, insomnia, bronchitis, cough, pharyngitis, rhinitis, sinusitis, chest pain, peripheral edema, abdominal pain/cramps, rash/ pruritis, constipation, elevated liver enzymes, flatulence, dyspepsia, photosensitivity, arthritis, myopathy, allergic reactions, arthropathy, back pain dizziness, drowsiness, nausea, headache, insomnia, diarrhea, nervousness, weakness, dry mouth, constipation, dyspepsia, agitation, anxiety, apathy, emotional lability, manic reactions, syncope, manic reactions, mental depression, syncope, sinusitis, cough, dyspnea, hypertension, edema, palpitations, postural hypotension, tachycardia, anorexia, dysphagia, elevated liver enzymes, flatulence, weight gain, decreased libido/ sexual dysfunction, weight gain or loss, chills, excessive sweating, hypertonia, tooth disorder/caries, myoclonus/ twitching, hypokinesia/ hyperkinesia, tremor, yawning, flulike symptoms, allergic reactions
95
Rev. 08/21/08
Folic acid
Follitropin alfa (GonalF)
anti-anemics water soluble vitamins hormones (ovulation stimulant)
signs of megaloblastic anemia assess for ovarian enlargement
Follitropin beta (Follistim AQ)
hormones (ovulation stimulant)
assess for ovarian enlargement
Fondaparinux/Arixtra
anticoagulants active factor x inhibitors
Assess for signs of bleeding and hemorrhage; bleeding from surgical site; and evidence of additional or increased thrombosis. Monitor platelet count closely.
Formoterol/ Foradil, Perforomist
bronchodilators adrenergics
Assess lung sounds, pulse, and blood pressure; pulmonary function tests; paradoxical bronchospasm; ECG; and signs of anaphylaxis before initiating and periodically therapy.
Fosamprenavir (Lexiva)
Antiretrovirals protease inhibitors
assess for skin reactions
rashes, irritability, difficulty sleeping, malaise, confusion, fever Ovarian hyper-stimulation syndrome, abdominal/ pelvic pain, dizziness, rhinitis, headache, pharyngitis, breast pain, constipation, diarrhea, dyspepsia, flatulence, ovarian enlargement, dysmenorrhea, irregular bleeding, injection site reactions, acne, cough, flu-like symptoms, multiple births Ovarian hyper-stimulation syndrome, abdominal/ pelvic pain, flatulence, breast pain/enlargement, nausea, injection site reactions, back pain, dizziness, headache, tachycardia, constipation, dysmenorrheal, irregular bleeding, dyspnea, ovarian enlargement, tachypnea, upper respiratory tract infection, flu-like symptoms, multiple births Confusion, dizziness, headache, insomnia, edema, hypotension, constipation, diarrhea, dyspepsia, increased serum aminotransferases, nausea, vomiting, urinary retention, bullous eruption, hematoma, purpura, rash, bleeding, thrombocytopenia, hypokalemia, fever, increased wound drainage. Dizziness, fatigue, headache, insomnia, malaise, nervousness, paradoxical bronchospasm, angina, arrhythmias, hypertension, hypotension, palpitations, tachycardia, dry mouth, nausea, hypokalemia, hyperglycemia, metabolic acidosis, muscle cramps, tremor, allergic reactions including anaphylaxis. Allergic reactions, stevensjohnson syndrome, angioedema, headache, diarrhea, n/v, rash, fatigue, abdominal pain, mood disorders, glucose intolerance, increased liver enzymes, neutropenia, fat redistribution,
96
Rev. 08/21/08
Fosaprepitant (injection) (Emend) Foscarnet (Foscavir)
antiemetics neurokinin antagonists antivirals
assess n/v, appetite, bowel sounds and abdominal pain ophthalmologic exams, culture for CMV
increased triglycerides, inflammatory response to opportunistic infection dizziness, fatigue, weakness, diarrhea, hiccups Seizures, headache, n/v, diarrhea, renal failure, fever, hypocalcemia, hypokalemia, hypomagnesemia, arthralgia, myalgia, anxiety, confusion, dizziness, fatigue, malaise, mental depression, weakness, conjunctivitis, eye pain, vision abnormalities, coughing, skin ulceration, dyspnea, increased sweating, palpiations, edema, ECG abnormalities, dysuria, chest pain, abdominal pain, abnormal taste sensation, anorexia, constipation, rash, dyspepsia, urinary retention, albuminuria, nocturia, polyuria, pruritis, leukopenia, hyperphosphatemia, sarcoma, hypophosphatemia, back pain, granulocytopenia, lymphoma, pain/inflammation at injection site, chills, involuntary muscle contraction, hypoesthesia, ataxia, neuropathy, flu-like syndrome, paresthesia Pseudomembranous colitis, dizziness, nausea, headache, weakness, diarrhea, dyspepsia, vaginitis dizziness, fatigue, headache, insomnia, weakness, cough, hypotension, chest pain, edema, abdominal pain, diarrhea, nausea, vomiting, erectile dysfunction, impaired renal function, rashes, hyperkalemia, muscle cramps, dyspnea, angioedema. Stevens-johnson syndrome, drowsiness, dizziness, nystagmus, pruritis, ataxia, headache, stupor, brain edema, vertigo, amblyopia, deafness, diplopia, tinnitus, hypotension, tachycardia, dry mouth, n/v, taste perversion, tongue disorder, rash, back pain, dysarthria, hypesthesia, extrapyramidal syndrome, incoordination, paresthesia, tremor, pelvic pain
Fosfomycin (Monurol)
anti-infectives
urine culture and sensitivity; monitor bowel function
Fosinopril/ Monopril
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor weight and assess patient routinely for resolution of fluid overload. Monitor renal function.
Fosphenytoin (Cerebyx)
anticonvulsants
BP, ECG, respiratory function
97
Rev. 08/21/08
Fospropofol (Lusedra)
General anesthetics
Respiratory status, pulse, BP
Frovatriptan (Frova)
vascular headache suppressant; five ht1 agonist
location, intensity, duration, and associated symptoms of pain
Fulvestrant (Faslodex)
antineoplastics estrogen receptor antagonists
Assess for pain
Furosemide/Lasix
Loop diuretics
Monitor BP and pulse Monitor electrolyte levels
Respiratory depression, parasthesia, pruritus, cough, hypoxemia, hypotension, loss of purposeful responsiveness MI, coronary artery vasospasm, ventricular fibrillation/tachycardia, dizziness, drowsiness, fatigue, flushing, chest pain, nausea, myocardial ischemia, dyspepsia, pain, dry mouth, paresthesia, skeletal pain headache, weakness, dyspnea, pharyngitis, increased cough, vasodilation (hot flushes), n/v, abdominal pain, constipation, diarrhea, pain/inflammation at injection site, back pain, bone pain, fever, anemia, flu syndrome, paresthesia, rash, anemia, arthritis, sweating, pelvic pain, UTI, anorexia, chest pain, edema, dizziness, depression, anxiety, insomnia Aplaxtic anemia, anorexia, agranulocytosis, pruritis, dehydration, blurred vision, hypochloremia, nausea, hypokalemia, metabolic acidosis, hypomagnesemia, hyponatremia, excessive urination, hypovolemia, constipation, hyperuricemia
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
Assess seizure activity and pain periodically during therapy. Monitor frequency and intensity of pain on pain scale. May cause leucopenia.
be to
Common Side Effects
Gabapentin/ Neurontin
Analgesic adjuncts anticonvulsants mood stabilizers
Galantamine/Razadyn e, Razadyne ER
anti-Alzheimers's agents cholinergics cholinesterase inhibitors
Assess cognitive function periodically during therapy and monitor heart rate periodically during therapy.
Confusion, depression, drowsiness, sedation, anxiety, concentration difficulties (children), dizziness, emotional lability (children), hostility, hyperkinesia (children), malaise, vertigo, weakness, abnormal vision, nystagmus, arthralgia, hypertension, weight gain, anorexia, ataxia, flatulence, gingivitis, altered reflexes, facial edema, hyperkinesia, paresthesia. Fatigue, dizziness, headache, syncope, bradycardia, chest pain, anorexia, diarrhea, dyspepsia, flatulence, nausea, vomiting, bladder outflow obstruction, incontinence,
98
Rev. 08/21/08
tremor, weight loss. Gallamine/ Flaxedil neuromuscular blocking agents nondepolarizing Assess respiratory status continuously throughout therapy. Monitor ECG, heart rate, and blood pressure throughout administration. Observe the patient for residual muscle weakness and respiratory distress during the recovery period. Monitor infusion site frequently. If signs of tissue irritation or extravasation occur, discontinue and restart in another vein. Assess for signs of infection. Assess for bleeding. Avoid IM injections and taking rectal temperatures. Apply pressure to venipuncture sites for 10 min. Monitor neutrophil and platelet count at least every 2 days during bid therapy and weekly thereafter. Monitor BUN and serum creatinine at least once every 2 wk throughout therapy. Monitor liver function tests. Bronchospasm, rash, arrhythmias, skin flushing, hypotension, excessive salivation, allergic reactions including anaphylaxis. Gallaminehypertension, tachycardia.
Ganciclovir/Cytovene, Vitrasert
antivirals
Ganirelix/ Antagon
hormones (gonadotropinreleasing hormone antagonist)
Galsulface/ Naglazyme
replacement enzyme enzymes
Assess patient for pregnancy prior to therapy. Therapy should not be initiated if patient is pregnant. May cause elevated neutrophil counts and decreased hematocrit and total bilirubin concentrations. Assess patient for infusion reactions; nausea, vomiting, elevated blood pressure, retrosternal pain, abdominal pain, malaise, and joint pain,
Seizures, abnormal dreams, coma, confusion, dizziness, drowsiness, headache, malaise, nervousness, retinal detachment, decreased visual acuity, vitreous hemorrhage, hyphema, intraocular pressure spikes, lens opacities, macular abnormalities, optic nerve changes, uveitis, dyspnea, arrhythmias, edema, hypertension, hypotension, GI bleeding, abdominal pain, increased liver enzymes, nausea, vomiting, gonadal suppression, hematuria, renal toxicity, alopecia, photosensitivity, pruritus, rash, urticaria, hypoglycemia, neutropenia, thrombocytopenia, anemia, eosinophilia, pain/phlebitis at IV site, ataxia, tremor, fever. Ovarian hyperstimulation syndrome, abdominal pain, nausea, pelvic pain, vaginal bleeding, hypersensitivity reactions, injection site reactions.
Malaise, conjunctivitis, cornela opacification, ear pain, dyspnea, chest pain, blood pressure, facial edema, gastroenteritis, abdominal pain, areflexia, infusion reactions, rigors.
99
Rev. 08/21/08
Gefitinib/Iressa
antineoplastics enzyme inhibitors
Gemcitabine/Gemzar
antineoplastics antimetabolites nucleoside analogues
Gemfibrozil/Lopid
fibric acid derivatives, lipidlowering agent
Gemifloxicin/Factive
anti-infectives fluoroquinolones
sleep apnea, vital signs and respiratory status prior to administration. Administration should be delayed in patients with an acute febrile or respiratory illness. Assess for signs of pulmonary toxicity. If interstitial lung disease is confirmed, discontinue gefitinib and treat appropriately. Assess patient for eye symptoms such as pain during therapy. Monitor liver function tests periodically. Monitor for changes in prothrombin time and INR in patients taking warfarin. Monitor vital signs before and frequently during therapy. Assess injection site during administration. Although gemcitabine is not considered a vesicant, local reactions may occur. Monitor for bone marrow depression. Monitor intake and output, appetite, and nutritional intake. Mild to moderate nausea and vomiting occur frequently. Antiemetics may be used prophylactically. Monitor CBC. Obtain patient's diet history, especially regarding fat and alcohol consumption. Serum triglyceride and cholesterol levels should be monitored before and periodically throughout therapy. Liver function tests CBC and electrolytes should be evaluated every 36 mo Assess patient for infection prior to and during therapy. Obtain specimens for culture and sensitivity before initiating therapy. Observe patient for
Weakness, aberrant eyelash, conjunctivitis, corneal erosion/ulcer, eye pain, vision, peripheral edema, pulmonary toxicity, dyspnea, diarrhea, nausea, vomiting, anorexia, hepatotoxicity, mouth ulceration, acne, dry skin, rash, pruritus, weight loss, allergic reactions including angioedema.
Pulmonary toxicity, dyspnea, bronchospasm, arrhythmias, cerebrovascular accident, MI, edema, hypertension, hepatotoxicity, diarrhea, nausea, stomatitis, transient elevation of hepatic transaminases, vomiting, hemolytic uremic syndrome, hematuria, proteinuria, alopecia, rash, anemia, leukopenia, thrombocytopenia, injection site reactions, paresthesias, flu-like symptoms, fever, anaphylactoid reactions.
Dizziness, headache blurred vision abdominal pain, diarrhea, epigastric pain, flatulence, gallstones, heartburn, nausea, vomiting. alopecia, rashes, urticaria anemia, leukopenia myositis.
Drowsiness, dizziness, headache, confusion, QTc prolongation, aarhythmias, pseudomembranous colitis, diarrhea, abdominal pain, nausea, vomiting, photosensitivity, rash,
100
Rev. 08/21/08
Gemtuzumab/ ozogamicin, Mylotarg
antineoplastics monoclonal antibodies antitumor antibiotics
Gentamicin/Garamyci n, G-Mycin, Jenamicin
anti-infectives aminoglycosides
Glatiramer/ Copaxone
anti multiple sclerosis agents immune response modifiers
Glimepiride/Amaryl
Sulfonylureas/ antidiabetics
signs and symptoms of anaphylaxis. Monitor bowel function. Assess patient for postinfusion symptom complex which may occur within the first 24 hr following administration and usually resolve after 2 4 hr with supportive therapy. Monitor vital signs during infusion and for 4 hrs after infusion. Monitor patient for development of tumor lysis syndrome. Assess patient for Infection, evaluate eighth cranial nerve function by audiometry, intake and output and daily weight to assess hydration status and renal function, signs of superinfection. Assess patient for side effects immediately after injection. Symptoms may include flushing, chest pain, palpitations, anxiety, dyspnea, constriction of throat, and urticaria. Symptoms are usually transient and self-limited without requiring treatment. May occur at the beginning of or following several months of therapy, and patients may experience one or several episodes of symptoms. Observe patient for signs and symptoms of hypoglycemic reactions; Assess patient for allergy to sulfonamides Observe for signs and symptoms of hypoglycemic reactions. Patients on concurrent beta-blocker therapy may have very subtle signs and symptoms of hypoglycemia. Assess patient for allergy to sulfonamides. Monitor
tendinitis, tendon rupture.
Headache, dyspnea, hypoxia, hypotension, hypertension, chills, mucositis, nausea, vomiting, infection, hepatotoxicity, rash, hyperglycemia, hypokalemia, fever, neutropenia, anemia, bleeding, allergic reactions, thrombocytopenia, postinfusion reaction, tumor lysis syndrome.
Ataxia, vertigo, ototoxicity (vestibular and cochlear), nephrotoxicity, muscle paralysis (high parenteral doses), hypersensitivity reactions.
Anxiety, weakness, confusion, migraine, vertigo, chest pain, palpitations, edema, syncope, tachycardia, vasodilation, pruritis, rashes, sweating, erythema, rhinitis, nystagmus, diarrhea, nausea, anorexia, vomiting, urgency, injection site reactions, arthralgia, back pain, hypertonia, tremor, dyspnea, flu-like symptoms, lymphadenopathy, fever, immediate postinjection reaction, infection, pain, weight gain. Photosensitivity, hypoglycemia, constipation, cramps, diarrhea, druginduced hepatitis, dyspepsia, increased appetite, nausea, vomiting. Dizziness, drowsiness, headache, weakness, constipation, cramps , diarrhea, drug-induced hepatitis, dyspepsia, increased appetite, nausea, vomiting, photosensitivity, rashes, hypoglycemia, hyponatremia, aplastic anemia, leukopenia, agranulocytosis, pancytopenia,
Glipizide/ Glucotrol, Glucotrol XL
antidiabetics sulfonylureas
101
Rev. 08/21/08
Glucagon/GlucaGen
Pancreatics, hormones
Glyburide/ DiaBeta, Glynase PresTab, Micronase
antidiabetics sulfonylureas
serum glucose and glycosylated hemoglobin periodically during therapy to evaluate effectiveness of treatment. Monitor CBC periodically during therapy. Report in blood counts promptly. Assess for signs of hypoglycemia, neurologic status, nutritional status nausea and vomiting after administration of dose Observe for signs and symptoms of hypoglycemic reactions. Patients on concurrent beta-blocker therapy may have very subtle signs and symptoms of hypoglycemia. Assess patient for allergy to sulfonamides. Monitor serum glucose and glycosylated hemoglobin periodically during therapy to evaluate effectiveness. Monitor CBC periodically during therapy. Report in blood counts Promptly. Assess patient for abdominal distention, presence of bowel sounds, and normal pattern of bowel function. Assess heart rate, blood pressure, and respiratory rate before and periodically during parenteral therapy. Assess for hyperexcitability, a paradoxical response that may occur in children. Monitor intake and output ratios in geriatric or surgical patients. Assess patient routinely for abdominal distention and auscultate for bowel sounds. Periodic intraocular pressure determinations should be made for patients
thrombocytopenia.
Hypotension. Nausea, vomiting, hypersensitivity reactions including anaphylaxis Dizziness, drowsiness, headache, weakness, constipation, cramps, diarrhea, drug-induced hepatitis, dyspepsia, increased appetite, nausea, vomiting, photosensitivity, rashes, hypoglycemia, hyponatremia, aplastic anemia, agranulocytosis, leukopenia, pancytopenia, thrombocytopenia.
Glycerine/ Fleet Babylax, Sani-Supp
Glycopyrrolate/Robinu l, Robinul-Forte
antiglaucoma agents laxatives osmotics antispasmodics anticholinergics
Confusion, headache, diarrhea, cramping, nausea, vomiting, dehydration, thirst. Confusion, drowsiness, blurred vision, cycloplegia, dry eyes, mydriasis, tachycardia, orthostatic hypotension, palpitations, dry mouth, constipation, urinary hesitancy, retention.
102
Rev. 08/21/08
Gold sodium thiomalate/ Aurolate, aurothiomalate, Myochrisine
antirheumatics (diseasemodifying)
Goserelin/ Zoladex
antineoplastics hormones gonadotropin releasing hormones
receiving long-term therapy. Assess patient's range of motion and the degree of swelling and pain in affected joints before and periodically throughout therapy. Monitor patient for nitritoid reaction that may occur immediately to 10 min after injection. Monitor renal, hepatic, and hematologic function and urinalysis before and periodically during therapy. Obtain urinalysis before each injection. Proteinuria or hematuria may necessitate discontinuation of therapy. Monitor CBC and platelets before every other injection or every 24 wk. May cause thrombocytopenia, leukopenia, and anemia. Monitor patients with vertebral metastases for increased back pain and decreased sensory/motor function. Monitor intake and output ratios and assess for bladder distention in patients with urinary tract obstruction during initiation of therapy. Assess patient for signs and symptoms of endometriosis before and periodically during therapy. Amenorrhea usually occurs within 8 wk of initial administration and menses usually resume 8 wk after completion. Assess patient for nausea, vomiting, abdominal distention, and bowel sounds prior to and following administration. Assess for extrapyramidal symptoms during therapy.
Dizziness, headache, neuropathy, conjunctivitis, corneal gold deposition, corneal ulcerations, pneumonitis, bradycardia, abdominal pain, cramping, diarrhea, metallic taste, stomatitis, anorexia, difficulty swallowing, drug-induced hepatitis, dyspepsia, flatulence, nausea, vomiting, hematuria, proteinuria, dermatitis, rash, photosensitivity reactions, pruritus, agranulocytosis, anemia, thrombocytopenia, eosinophilia, leucopenia, arthralgia, allergic reactions including anaphylaxis, angioneurotic edema, nitritoid reactions
Granisetron/ Kytril
antiemetics five ht3 antagonists
Headache, anxiety, depression, dizziness, fatigue, insomnia, weakness, dyspnea, cerebrovascular accident, MI, vasodilation, chest pain, hypertension, palpitations, anorexia, constipation, diarrhea, nausea, ulcer, vomiting, renal insufficiency, urinary obstruction, sweating, rashes, decreased libido, erectile dysfunction, breast swelling, breast tenderness, infertility, ovarian cysts, ovarian hyperstimulation syndrome, peripheral edema, anemia, gout, hyperglycemia, lipids, bone pain, arthralgia, bone density, hot flashes, chills, fever, weight gain Headache, agitation, anxiety, CNS stimulation, drowsiness, weakness, hypertension, constipation, diarrhea, elevated liver enzymes, taste disorder, anaphylactoid reactions, fever.
103
Rev. 08/21/08
Guaifenesin/Alfen Jr, Altarussin, Breonesin, Diabetic Tussin, Ganidin NR, Guiatuss, Hytuss, Hytuss-2X, Mucinex, Naldecon Senior EX, Organidin NR, Robitussin, Scottussin Expectorant, Siltussin SA, Siltussin DAS Guanfacine/ Tenex
allergy, cold and cough remedies expectorant
Assess lung sounds, frequency and type of cough; and character of bronchial secretions periodically during therapy. Maintain fluid intake of 15002000 ml/day to decrease viscosity of secretions.
Dizziness, headache, nausea, diarrhea, stomach pain, vomiting, rashes, urticaria.
antihypertensives centrally acting antiadrenergics
Monitor blood pressure (lying and standing) and pulse frequently during initial dose adjustment and periodically during therapy. Report significant changes.
Drowsiness, weakness, depression, dizziness, fatigue, headache, insomnia, tinnitus, dyspnea, bradycardia, chest pain, palpitations, rebound hypertension, constipation, dry mouth, abdominal pain, nausea, erectile dysfunction.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Halcinonide/ Halog
anti inflammatories steroidal corticosteroids
Assess affected skin and symptoms of infection. Note degree of inflammation and pruritus.
Halobetasol/ Ultravate
anti inflammatories steroidal corticosteroids
Assess affected skin and symptoms of infection. Note degree of inflammation and pruritus.
Haloperidol/ Haldol, Haldol Decanoate
antipsychotics butyrophenones
Assess mental status (orientation, mood, behavior), blood pressure (sitting, standing, lying) and pulse, intake and output ratios and daily weight, tardive dyskinesia, development of neuroleptic malignant syndrome, signs and symptoms of dehydration. onset of akathisia (restlessness or
allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression Seizures, extrapyramidal reactions, confusion, drowsiness, restlessness, tardive dyskinesia, blurred vision, dry eyes, respiratory depression, hypotension, tachycardia, constipation, dry mouth, anorexia, drug-induced hepatitis, ileus, weight gain, urinary retention, diaphoresis, photosensitivity, rashes, galactorrhea, amenorrhea,
104
Rev. 08/21/08
desire to keep moving), which may appear within 6 hr of 1st dose Heparin/Hep-Lok Antithrombotics, anticoagulants Assess for signs of bleeding and hemorrhage, evidence of additional or increased thrombosis, hypersensitivity reactions signs of anaphylaxis (hypotension, flushing, chest tightness, wheezing, fever, dizziness, nausea, vomiting, diaphoresis) after administration. Epinephrine and antihistamines should be available for treatment of anaphylactic reactions Monitor vital signs, CVP, cardiac output, pulmonary capillary wedge pressure, and urinary output, signs of vascular overload. If fever, wheezing, flu-like symptoms, urticaria, periorbital edema, or submaxillary and parotid gland enlargement occurs, stop infusion. Assess surgical patients for increased bleeding after administration. Before therapy, a complete physical and endocrinologic examination, including height, weight, and other appropriate objective measures for monitoring the patient's prostate cancer must be performed. signs of hypersensitivity
Hepatitis B immune globulin/ BayHep B, Nabi-HB
vaccines/immunizin g agents immune globulins
anemia, leucopenia, hyperpyrexia, neuroleptic malignant syndrome, hypersensitivity reactions. Drug-induced hepatitis. alopecia rashes, urticaria, bleeding, anemia, thrombocytopenia osteoporosis fever, hypersensitivity dizziness, faintness, malaise, weakness, pruritus, rashes, urticaria, erythema at IM site, pain, swelling, tenderness, joint pain, allergic reactions including anaphylactic shock and angioedema.
Hetastarch/ Hespan
volume expanders colloids
Headache, CHF, pulmonary edema, vomiting, pruritus, urticaria, fluid overload, peripheral edema of the lower extremities, decreased hematocrit, decreased platelet function, myalgia, hypersensitivity reactions including anaphylactoid reactions, chills, fever, parotid and submaxillary gland enlargement.
Histrelin/ Vantas
hormones gonadotropin releasing hormones
seizures, headache, anxiety, depression, dizziness, insomnia, lethargy, malaise, irritability, visual disturbances, dyspnea, vasodilation, edema, palpitations, tachycardia, abdominal discomfort, constipationnausea, vomiting, dysuria, hematuria, polyuria, urinary retention, rash, acne, pruritis, increased sweating, breast discharge, breast pain, genital pruritis, increased breast size, anemia, itching, erythema, and swelling at implantation site, hyperlipidemia, hypercalcemia, arthralgia, joint stiffness, muscle cramps, muscle stiffness, myalgia, bone pain, tremor, allergic reactions including angioedema , increased appetite, increased pain.
105
Rev. 08/21/08
Human papillomavirus quadrivalent (types 6, 11, 16 and 18) vaccine, recombinant/ Gardasil Hydralazine/ Apresoline
vaccines/immunizin g agents
Assess vital signs prior to administration.
injection site reactions and anaphylaxis
antihypertensives vasodilators
Monitor blood pressure and pulse
Hydralazine/isosorbide dinitrate// BiDil
vasodilators vasodilators nitrates
Monitor blood pressure and pulse
Hydrochlorothiazide/ Esedrix, HCTZ, Hydrochlor, Hydro-D, HydroDIURIL, Microzide, Novo-Hydrazide, Oretic
antihypertensives diuretics
Monitor blood pressure, intake, output, and daily weight and assess feet, legs, and sacral area for edema daily. anorexia, nausea, vomiting, muscle cramps, paresthesia, and confusion
Hydrocodone/ Hycodan, Tussigon
allergy, cold and cough remedies (antitussive) opioid analgesics opioid agonists nonopioid analgesic combinations
Assess blood pressure, pulse, and respirations, level of sedation, bowel function. Assess cough and lung sounds during antitussive use. Assess type, location, and intensity of pain prior to and 1 hr (peak) following administration.
Hydrocodone/ acetaminophen//Anex sia, Co-Gesic, Lorcet-HD,
allergy, cold and cough remedies (antitussive) opioid analgesics
Assess blood pressure, pulse, and respirations, level of sedation, bowel function. Assess cough and lung
dizziness, drowsiness, headache, tachycardia, angina, arrhythmias, edema, orthostatic hypotension, diarrhea, nausea, vomiting, rashes, sodium retention, arthralgias, arthritis, peripheral neuropathy, druginduced lupus syndrome. dizziness, drowsiness, headache, tachycardia, angina, arrhythmias, edema, orthostatic hypotension, diarrhea, nausea, vomiting, rashes, sodium retention, arthralgias, arthritis, peripheral neuropathy, druginduced lupus syndrome, apprehension, weakness, paradoxic bradycardia, syncope, hypotension, abdominal pain, crosstolerance, flushing, tolerance. dizziness, drowsiness, lethargy, weakness, hypotension, anorexia, cramping, hepatitis, nausea, vomiting, photosensitivity, rashes, hyperglycemia, hypokalemia, dehydration, hypercalcemia, hypochloremic alkalosis, hypomagnesemia, hyponatremia, hypophosphatemia, hypovolemia, blood dyscrasias, hyperuricemia, hypercholesterolemia, muscle cramps, pancreatitis. confusion, dizziness, sedation, euphoria, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, dyspepsia, nausea, vomiting, urinary retention, sweating, physical dependence, psychological dependence, tolerance. confusion, dizziness, sedation, euphoria, hallucinations, headache, unusual dreams, blurred vision, diplopia,
106
Rev. 08/21/08
Lortab, Norco, Vicodin, Zydone
opioid agonists nonopioid analgesic combinations
sounds during antitussive use. Assess type, location, and intensity of pain prior to and 1 hr (peak) following administration.
Hydrocodone/aspirin// Azdone
allergy, cold and cough remedies (antitussive) opioid analgesics opioid agonists nonopioid analgesic combinations
Assess blood pressure, pulse, and respirations, level of sedation, bowel function. Assess cough and lung sounds during antitussive use. Assess type, location, and intensity of pain prior to and 1 hr (peak) following administration.
Hydrocodone/ibuprofe n// Vicoprofen
allergy, cold and cough remedies (antitussive) opioid analgesics opioid agonists nonopioid analgesic combinations
Assess blood pressure, pulse, and respirations, level of sedation, bowel function. Assess cough and lung sounds during antitussive use. Assess type, location, and intensity of pain prior to and 1 hr (peak) following administration.
Hydrocortisone/ Cortef, Cortenema, Cortifoam, Solu-Cortef
anti inflammatories steroidal corticosteroids
signs of adrenal insufficiency, peripheral edema, steady weight gain, rales/crackles, or dyspnea, signs of anaphylaxis, ECG.
miosis, respiratory depression, hypotension, bradycardia, constipation, dyspepsia, nausea, vomiting, urinary retention, sweating, physical dependence, psychological dependence, tolerance. confusion, dizziness, sedation, euphoria, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, dyspepsia, nausea, vomiting, urinary retention, sweating, physical dependence, psychological dependence, tolerance. confusion, dizziness, sedation, euphoria, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, dyspepsia, nausea, vomiting, urinary retention, sweating, physical dependence, psychological dependence, tolerance. depression, euphoria, headache, increased intracranial pressure (children only), personality changes, psychoses, restlessness, cataracts, increased intraocular pressure, hypertension, peptic ulceration, anorexia, nausea, vomiting, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, hyperglycemia, fluid retention, hypokalemia, hypokalemic alkalosis, thromboembolism, thrombophlebitis, weight gain, weight loss, muscle wasting, osteoporosis, aseptic necrosis of joints, muscle pain, hypersensitivity reactions, anaphylaxis, cushingoid appearance, increased susceptibility to infection.
107
Rev. 08/21/08
Hydrocortisone topical/ Acticort, Aeroseb-HC, Ala-Cort, Ala-Scalp, Alphaderm, Anusol HC, Bactine, CaldeCORT Anti-Itch, Carmol HC, Cetacort, Cortaid, Cort-Dome, Corticaine, Cortifair, Cortizone, Dermacort, DermiCort, Dermtex HC, FoilleCort, Gynecort, Hemril-HC, Hi-Cor, Hycort, HydroTex, Hytone, LactiCare-HC, Lanacort 9-1-1, Lemoderm, Locoid, Nutracort, OrabaseHCA, Pandel, Penecort, PharmaCort, Prevex HC, Proctocort, Rhulicort, Synacort, Texacort Westcort Hydromorphone/Dilau did, Dilaudid-HP, Hydrostat IR, PMS Hydromorphone
anti inflammatories steroidal corticosteroids
Assess affected skin before and daily during therapy. Note degree of inflammation and pruritus.
Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression.
allergy, cold and cough remedies (antitussives) opioid analgesics opioid agonists
Assess blood pressure, pulse, and respirations, bowel function. Assess type, location, and intensity of pain prior to and 1 hr following IM and 5 min (peak) following IV administration. Assess cough and lung sounds during antitussive use
Hydroxocobalamin/ Cyanokit
antianemics vitamins water soluble vitamins
signs of vitamin B12 deficiency. Monitor BP and HR continuously during and after infusion and immediately report significant changes.
Hydroxychloroquine/ Plaquenil
antimalarials antirheumatics (DMARDs)
Assess patient monthly for pain, swelling, and range of motion, improvement in signs and symptoms of
confusion, sedation, dizziness, dysphoria, euphoria, floating feeling, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, dry mouth, nausea, vomiting, urinary retention, flushing, sweating, physical dependence, psychological dependence, tolerance. Diarrhea, itching, hypokalemia, pain at IM site, hypersensitivity reactions including anaphylaxis, dizziness, headache, memory impairment, restlessness, hypertension, chest pain, edema, tachycardia, dry throat, eye redness, eye swelling, dyspnea, abdominal discomfort, diarrhea, dyspepsia, dysphagia, hematochezia, nausea, vomiting, red urine, erythema, rash, pruritis, urticaria, injection site reaction. Seizures, aggressiveness, anxiety, apathy, confusion, fatigue, headache, irritability, personality changes,
108
Rev. 08/21/08
condition, deep tendon reflexes
Hydroxyprogesterone/ Hy/Gesterone, Hylutin, Pro-Depo, Prodrox, ProSpan
hormones progestins
Blood pressure, pattern and amount of vaginal bleeding (pad count)
Hydroxyurea/ Droxia, Hydrea, Mylocel
antineoplastics antimetabolites
Assess for signs of infection, increased fatigue, dyspnea, and orthostatic hypotension, bleeding, intake and output, appetite, and nutritional intake
Hydroxyzine/ Atarax, Hyzine-50, Vistaril
antianxiety agents antihistamines sedative/hypnotics
Hyoscyamine/ Anaspaz, A-Spas S/L, Cystospaz, CystospazM, Donnamar, EDSPAZ, Gastrosed, Levsinex, Levsin, Levbid, LHyoscyamine, NuLev
antispasmodics anticholinergics
Assess patient for profound sedation, mental status (orientation, mood, and behavior), degree of nausea and frequency and amount of emesis, degree of itching and character of involved skin Assess vital signs and ECG tracings frequently during IV drug therapy. Assess patients routinely for abdominal distention and auscultate for bowel sounds. Monitor intake and output ratios in elderly or surgical patients because hyoscyamine may cause urinary retention.
psychoses, keratopathy, ototoxicity, retinopathy, tinnitus, visual disturbances, ECG changes, hypotension, abdominal cramps, anorexia, diarrhea, epigastric discomfort, nausea, vomiting, hepatic failure, bleaching of hair, alopecia, neuromyopathy, hyperpigmentation, photosensitivity, StevensJohnson syndrome, agranulocytosis, aplastic anemia, leukopenia, thrombocytopenia, peripheral neuritis. Cerebral thrombosis, depression, coughing, dyspnea, pulmonary embolism, edema, thrombophlebitis, cholestatic jaundice, breakthrough bleeding, amenorrhea, cervical changes, increased pigmentation, rashes, allergic reactions, weight changes. Drowsiness, anorexia, diarrhea, nausea, vomiting, constipation, hepatitis, stomatitis, dysuria, infertility, renal tubular dysfunction, alopecia, exacerbation of postradiation erythema, erythema, pruritus, rashes, leukopenia, anemia, thrombocytopenia, hyperuricemia, chills, fever, malaise. drowsiness, agitation, ataxia, dizziness, headache, weakness, wheezing, dry mouth, bitter taste, constipation, nausea, urinary retention, flushing, pain at IM site, abscesses at IM sites, chest tightness. blurred vision, nausea, allergic reactions including anaphylaxis, confusion/excitement (especially in geriatric patients), dizziness, flushing, headache, insomnia, lightheadedness (IM, IV, subcut), nervousness, decreased sweating, urticaria
109
Rev. 08/21/08
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Ibandronate/ Boniva
bone resorption inhibitors biphosphonates
Assess patients for low bone mass before and periodically during therapy
Ibritumomab tiuxetan/ Zevalin
antineoplastics monoclonal antibodies radioisotopes
Ibuprofin lysine/ NeoProfen
nonsteroidal anti inflammatory agents
Assess patient for signs of infusion reaction usually seen within 30 120 min following infusion. Monitor patient for neutropenia and thrombocytopenia during and for 3 mo following treatment. Biodistribution of indium-111 Zevalin should be assessed at 2 24 hr and 4872 hr after injection. Monitor CBC and platelet counts prior to administration, weekly during therapy, and until counts recover. Monitor respiratory status, heart rate, blood pressure, ECG, and heart sounds routinely during therapy. May mask signs of infection; monitor closely. Assess pain and range of motion prior to and 12 hr following administration. Monitor temperature; note signs associated with fever. Assess for signs and symptoms of GI bleeding, renal dysfunction, and hepatic impairment. BUN, serum creatinine, CBC, and liver function tests should be evaluated periodically in patients receiving prolonged therapy.
diarrhea, dyspepsia, esophagitis, esophageal/gastric ulcer, musculoskeletal pain, pain in arms/legs, osteonecrosis (primarily of jaw), injection site reactions. anxiety, dizziness, rhinitis, dyspnea, increased cough, bronchospasm, abdominal pain, anorexia, diarrhea, nausea, vomiting, ecchymoses, pruritis, leucopenia, thrombocytopenia, anemia, arthralgia, infections, infusion reactions, allergic reactions including anaphylaxis, secondary malignancies.
Atelectasis, edema, hypoglycemia, adrenal insufficiency, anemia, bleeding, irritation or infection site.
Ibuprofen oral/Advil, Advil Migraine LiquiGels, Children's Advil, Children's Motrin, Excedrin IB, Genpril, Haltran, Junior Strength Advil, Menadol, Medipren, Midol Maximum Strength Cramp Formula, Motrin, Motrin Drops, Motrin IB, Motrin Junior Strength, Motrin Migraine Pain, NuIbuprofen, Nuprin, PediaCare Children's Fever Ibutilide/Corvert
antipyretics antirheumatics nonopioid analgesics nonsteroidal anti inflammatory agents nonopioid analgesics
Headache, dizziness, drowsiness, psychic disturbances, amblyopia, blurred vision, tinnitus, arrhythmias, edema, GI bleeding, hepatitis, constipation, dyspepsia, nausea, vomiting, abdominal discomfort, cystitis, hematuria, renal failure, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, rashes, blood dyscrasias, prolonged bleeding time, allergic reactions including anaphylaxis. Headache, arrhythmias, nausea.
antiarrhythmics (class III)
Monitor ECG continuously throughout and for 4 hr after infusion or until QT
110
Rev. 08/21/08
Idarubicin/ Idamycin
antineoplastics anthracyclines
Idursulface/ Elaprase
replacement enzyme enzymes
Ifosfamide/ Ifex
antineoplastics alkylating agents
interval normalizes. Clinicians trained to treat ventricular arrhythmias, medications, and equipment (defibrillator/ cardioverter) should be available during therapy and monitoring of patient Monitor blood pressure, pulse, respiratory rate, and temperature, bone marrow depression, signs of myocardial toxicity, bleeding and avoid IM injections and taking rectal temperatures if platelet count is low. Monitor intake and output ratios, nausea and vomiting may occur as early as 1 hr after therapy and may last 24 hr. Parenteral antiemetics should be administered 3045 min prior to therapy and routinely around the clock for the next 24 hr as indicated. Assess injection site frequently infiltrate painlessly. Monitor CBC, differential, and platelet count. Observe for signs and symptoms of anaphylaxis. Keep epinephrine, an antihistamine, corticosteroids, and resuscitation equipment close by in case of anaphylactic reaction. Monitor for infusionrelated reactions. Monitor blood pressure, pulse, respiratory rate, and temperature; urinary output; neurologic status; nausea, vomiting, and appetite; weight; bone marrow depression; and bleeding frequently during therapy. Monitor CBC, differential, and platelet count; AST, ALT, serum alkaline phosphatase, bilirubin, and LDH; and BUN, serum creatinine, phosphate, and potassium
headache, mental status changes, pulmonary toxicity, pulmonary allergic reactions, arrhythmias, cardiotoxicity, CHF, abdominal cramps, diarrhea, mucositis, nausea, vomiting, alopecia, photosensitivity, rashes, gonadal suppression, bleeding, anemia, leukopenia, thrombocytopenia, phlebitis at IV site, hyperuricemia, peripheral neuropathy, fever.
headache, malaise, hypertension, dyspepsia, cutaneous reactions, infusion site swelling, arthralgia, anaphylactoid reactions, fever.
CNS toxicity (somnolence, confusion, hallucinations, coma), cranial nerve dysfunction, disorientation, dizziness, cardiotoxicity, nausea, vomiting, anorexia, constipation, diarrhea, hepatotoxicity, hemorrhagic cystitis, dysuria, sterility, renal toxicity, alopecia, anemia, leukopenia, thrombocytopenia, phlebitis, allergic reactions.
111
Rev. 08/21/08
Iloprost/ Ventavis
vasodilators prostacyclins
prior to and periodically during therapy. Urinalysis should be evaluated before each dose. Assess respiratory status, vital signs prior to and throughout therapy. Do not administer if BP <85 mmHg. Assess for signs of pulmonary edema.
Imatinib/ Gleevec
antineoplastics enzyme inhibitors
Monitor for fluid retention, Weigh regularly, signs of pleural effusion, pericardial effusion, pulmonary edema, ascites, vital signs, fever. Monitor liver function before and monthly during treatment or when clinically indicated. Monitor CBC weekly for the first month, biweekly for the second month, and periodically during therapy. Monitor for an improvement in symptoms including hepatomegaly, splenomegaly, anemia, thrombocytopenia, bone demineralization, and increased appetite and energy level periodically throughout therapy. Assess liver and spleen size every 6 mo to determine effectiveness of therapy. Monitor patient for signs of hypersensitivity reactions. Monitor hemoglobin and platelet count monthly to determine effectiveness of therapy. Assess affected area(s) prior to and periodically during therapy. Assess patient for infection, signs and
fainting, headache, insomnia, cough, dyspnea, hemoptysis, CHF, vasodilation, chest pain, hypotension, peripheral edema, supraventricular tachycardia, nausea, vomiting, renal failure, facial flushing, back pain, jaw-muscle spasm, muscle cramps. fatigue, headache, weakness, cough, dyspnea, epistaxis, nasopharyngitis, pneumonia, fever, hepatotoxicity, abdominal pain, anorexia, constipation, diarrhea, dyspepsia, nausea, vomiting, petechiae, pruritus, skin rash, edema, hypokalemia, bleeding, neutropenia, thrombocytopenia, weight gain, arthralgia, muscle cramps, musculoskeletal pain, myalgia, night sweats.
Imiglucerase/ Cerezyme
replacement enzyme
dizziness, headache, mild hypotension, abdominal discomfort, nausea, decreased urinary frequency, pruritus, rash, antibody production, hypersensitivity reactions, fever.
Imiquimod/ Aldara
Imipenim/ Primaxin
antivirals immune modifiers immune response modifiers anti-infectives carbapenems
Irritation, pain, pruritis, burning, swelling, fungal infections (women). Seizures, dizziness, somnolence, hypotension,
112
Rev. 08/21/08
Imipramine/ Norfranil, Tipramine, Tofranil, Tofranil PM
antidepressants tricyclic antidepressants
Immune Globin/ gamma globulin, IG, ISG, immune serum globulin
vaccines/immunizin g agents immune globulins
symptoms of anaphylaxis at beginning of and throughout therapy. Obtain a history before initiating therapy to determine previous use of and reactions to penicillins. Monitor blood pressure and pulse rate, weight and BMI, sexual dysfunction, ECG, mental status, suicidal tendencies, frequency of bedwetting, pain, plasma levels in treatmentresistant patients. Assess leukocyte and differential blood counts and renal and hepatic functions prior to and periodically during prolonged or highdose therapy. Assess patient for aseptic meningitis syndrome (AMS). Monitor patient for signs of infection during therapy. Monitor platelet counts in patients being treated for idiopathic thrombocytopenic purpura.
pseudomembranous colitis, diarrhea, nausea, vomiting, rash, pruritus, sweating, urticaria, eosinophilia, phlebitis at IV site, allergic reactions including anaphylaxis, fever, superinfection. drowsiness, fatigue, agitation, confusion, hallucinations, insomnia, blurred vision, dry eyes, arrhythmias, hypotension, ECG changes, constipation, dry mouth, nausea, paralytic ileus, weight gain, urinary retention, decreased libido, photosensitivity, gynecomastia, blood dyscrasias.
Immune globulin IM/ BayGam, IGIM
vaccines/immunizin g agents immune globulins
Assess patient for aseptic meningitis syndrome (AMS). Monitor patient for signs of infection during therapy. Monitor platelet counts in patients being treated for idiopathic thrombocytopenic purpura.
Immune globulin IV/ Gamimune N, Gammagard S/D,
vaccines/immunizin g agents immune globulins
Monitor vital signs continuously during infusion of immune
aseptic meningitis syndrome, headache, light-headedness, malaise, dyspnea, wheezing, chest pain, vascular occlusion, nausea, renal failure, diuresis (maltose containing-products), nephrotic syndrome, cyanosis, urticaria, arthralgia, back pain, hip pain, allergic reactions including anaphylaxis, angioedema, chills, fever, sweating. SQ or IM sitemuscle stiffness, pain, tenderness, IV sitelocal inflammation, phlebitis, urticaria. aseptic meningitis syndrome, headache, light-headedness, malaise, dyspnea, wheezing, chest pain, vascular occlusion, nausea, renal failure, diuresis (maltose containing-products), nephrotic syndrome, cyanosis, urticaria, arthralgia, back pain, hip pain, allergic reactions including anaphylaxis, angioedema, chills, fever, sweating. SQ or IM sitemuscle stiffness, pain, tenderness, IV sitelocal inflammation, phlebitis, urticaria. aseptic meningitis syndrome, headache, light-headedness, malaise, dyspnea, wheezing,
113
Rev. 08/21/08
Gammar-P IV, Iveegam, Panglobulin, Polygam S/D, Privigen, Sandoglobulin, Venoglobulin-S
globulin IV and assess patient for signs of anaphylaxis for 1 hr following initiation of infusion. Assess patient for aseptic meningitis syndrome (AMS). Monitor patient for signs of infection during therapy. Monitor platelet counts in patients being treated for idiopathic thrombocytopenic purpura.
chest pain, vascular occlusion, nausea, renal failure, diuresis (maltose containing-products), nephrotic syndrome, cyanosis, urticaria, arthralgia, back pain, hip pain, allergic reactions including anaphylaxis, angioedema, chills, fever, sweating. SQ or IM sitemuscle stiffness, pain, tenderness, IV sitelocal inflammation, phlebitis, urticaria.
Immune globulin SQ/ Vivaglobin
vaccines/immunizin g agents immune globulins
Assess patient for aseptic meningitis syndrome (AMS). Monitor patient for signs of infection during therapy. Monitor platelet counts in patients being treated for idiopathic thrombocytopenic purpura.
Inamrinone/ Inocor
inotropics bipyridines
Inotropic effects may be additive with digoxin. Monitor blood pressure, pulse, ECG, respiratory rate, cardiac index, pulmonary capillary wedge pressure, and central venous pressure frequently during administration. Monitor intake and output and weigh daily. Assess for resolution of signs of CHF. Platelet counts, serum electrolytes, liver enzymes, and renal function should be evaluated periodically throughout therapy Monitor blood pressure, intake and output, and daily weight and assess feet, legs, and sacral area for edema daily. Assess patient, especially if taking digoxin, for anorexia, nausea,
aseptic meningitis syndrome, headache, light-headedness, malaise, dyspnea, wheezing, chest pain, vascular occlusion, nausea, renal failure, diuresis (maltose containing-products), nephrotic syndrome, cyanosis, urticaria, arthralgia, back pain, hip pain, allergic reactions including anaphylaxis, angioedema, chills, fever, sweating. SQ or IM sitemuscle stiffness, pain, tenderness, IV sitelocal inflammation, phlebitis, urticaria. Dyspnea, arrhythmias, hypotension, diarrhea, hepatotoxicity, nausea, vomiting, hypokalemia, thrombocytopenia, tachyphylaxis, fever, hypersensitivity reactions.
Indapimide/ Lozol
antihypertensives diuretics thiazide like diuretics
dizziness, drowsiness, lethargy, arrhythmias, hypotension, anorexia, cramping, nausea, vomiting, photosensitivity, rashes, hyperglycemia, hypokalemia, dehydration, hypochloremic alkalosis, hyponatremia,
114
Rev. 08/21/08
Indinavir/ Crixivan
antiretrovirals protease inhibitors
vomiting, muscle cramps, paresthesia, and confusion. Patients taking digoxin have an increased risk of digitalis toxicity due to the potassiumdepleting effect of the diuretic. Assess patient for allergy to sulfonamides. Monitor electrolytes (especially potassium), blood glucose, BUN, serum creatinine, and uric acid levels periodically throughout therapy. Assess for change in severity of symptoms of HIV infection and for symptoms of opportunistic infections throughout therapy. Monitor viral load and CD4 cell count periodically during therapy. Assess limitation of movement and pain note type, location, and intensity before and 12 hr after administration. Monitor respiratory status, heart rate, blood pressure, ECG, heart sounds, intake and output. Evaluate BUN, serum creatinine, CBC, serum potassium levels, and liver function tests periodically in patients receiving prolonged therapy. Assess for infusionrelated reactions during and for 2 hr after infusion. Assess for latent tuberculosis with a tuberculin skin test prior to initiation of therapy. Observe patient for hypersensitivity reactions during infusion. Assess pain and range of motion prior to and periodically during therapy. Assess for signs and symptoms
hypovolemia, hyperuricemia, muscle cramps.
Indomethacin/ Indocin, Indocin I.V, Indocin SR, Indochron E-R
antirheumatics ductus arteriosus patency adjuncts (IV only) nonsteroidal anti inflammatory agents
Infliximab/ Remicade
antirheumatics (DMARDs) gastroinestinal anti inflammatories monoclonal antibodies
dizziness, drowsiness, fatigue, headache, insomnia, weakness, abdominal pain, acid regurgitation, altered taste, asymptomatic hyperbilirubinemia, diarrhea, nausea, vomiting, nephrolithiasis, hyperglycemia, ketoacidosis, back pain, flank pain, redistribution of body fat. dizziness, drowsiness, headache, psychic disturbances, blurred vision, tinnitus, hypertension, edema, cystitis, hematuria, renal failure, rashes, hyperkalemia, thrombocytopenia, blood dyscrasias, prolonged bleeding time, phlebitis at IV site, allergic reactions including anaphylaxis. POdruginduced hepatitis, GI bleeding, constipation, dyspepsia, nausea, vomiting, discomfort, necrotizing enterocolitis. IVdilutional hyponatremia, hypoglycemia. fatigue, headache, anxiety, depression, dizziness, insomnia, conjunctivitis, upper respiratory tract infection, bronchitis, cough, dyspnea, laryngitis, pharyngitis, respiratory tract allergic reaction, rhinitis, sinusitis, chest pain, hypertension, hypotension, pericardial effusion, tachycardia, CHF, abdominal pain, nausea, vomiting, constipation, diarrhea, dyspepsia,
115
Rev. 08/21/08
of Crohns Disease and ulcerative Colitis before, during, and after therapy. Monitor liver function tests periodically during therapy. Monitor CBC with differential periodically during therapy.
Influenza vaccine/ FluMist
vaccines/immunizin g agents
Insulin aspart/Novolog
Pancreatics, antidiabetics, hormones
Insulin aspart protamine suspension/insulin aspart solution mixtures, rdna origin (NovoLog Mix 70/30)
antidiabetics hormones pancreatics
Assess patient for history of asthma or reactive airway disease. Monitor patient for signs of allergic reaction following administration. Assess for symptoms of hypoglycemia and hyperglycemia during therapy. Monitor body weight Assess for symptoms of hypoglycemia and hyperglycemia, body weight periodically. Monitor blood glucose every 6 hr during therapy. Overdose is manifested by symptoms of hypoglycemia. Assess patient for signs and symptoms of hypoglycemia and hyperglycemia, body weight periodically. Monitor blood glucose every 6 hr during therapy, more frequently in ketoacidosis and times of stress. A1C may be monitored every 36
flatulence, hepatotoxicity, intestinal obstruction, oral pain, tooth pain, ulcerative stomatitis, dysuria, urinary frequency, urinary tract infection, acne, alopecia, dry skin, ecchymosis, eczema, erythema, flushing, hematoma, increased sweating, hot flushes, pruritus, urticaria, rash, neutropenia, arthralgia, arthritis, back pain, involuntary muscle contractions, myalgia, paresthesia, infections including reactivation TB, pneumonia and invasive fungal infections, fever, infusion reactions, chills, flu-like syndrome, herpes simplex, herpes zoster, hypersensitivity reactions, risk of lymphoma, lupus-like syndrome, moniliasis, pain, peripheral edema, vasculitis. Headache, rhinitis, nasal congestion, fever.
Hypoglycemia, lipodystrophy, pruritis, erythema, swelling, allergic reactions including anaphylaxis Hypoglycemia, erythema, lipodystrophy, pruritis, swelling, allergic reactions including anaphylaxis.
Insulin Detemir/ Levemir
antidiabetics hormones pancreatics
Hypoglycemia, lipodystrophy, pruritis, erythema, swelling, allergic reactions including anaphylaxis.
116
Rev. 08/21/08
Insulin glargine/Lantus
Pancreatics, hormones
Insulin Glulisine (rDNA origin)/ Apidra
antidiabetics hormones pancreatics
months to determine effectiveness. Assess for symptoms of hypoglycemia and hyperglycemia periodically during therapy Assess for symptoms of hypoglycemia and hyperglycemia, body weight periodically. Monitor blood glucose every 6 hr during therapy, more frequently in ketoacidosis and times of stress. A1C may be monitored every 36 months to determine effectiveness. Assess for symptoms of hypoglycemia and hyperglycemia, body weight periodically. Monitor blood glucose every 6 hr during therapy, more frequently in ketoacidosis and times of stress. A1C may be monitored every 36 months to determine effectiveness. Assess for symptoms of hypoglycemia and hyperglycemia, body weight periodically. Monitor blood glucose every 6 hr during therapy. Overdose is manifested by symptoms of hypoglycemia. Assess patient periodically for symptoms of hypoglycemia and hyperglycemia during therapy. Monitor body weight periodically. Assess for symptoms of hypoglycemia and hyperglycemia, body weight periodically. Monitor blood glucose every 6 hr during therapy. Overdose is manifested by symptoms of hypoglycemia.
Hypoglycemia, lipodystrophy, pruritis, erythema, swelling, allergic reactions including anaphylaxis Hypoglycemia, lipodystrophy, pruritis, erythema, swelling, allergic reactions including anaphylaxis.
Insulin lispro (rDNA)/ Humalog
antidiabetics hormones pancreatics
Hypoglycemia, erythema, lipodystrophy, pruritis, swelling, allergic reactions including anaphylaxis.
Insulin lispro protamine suspension/insulin lispro solution mixtures, rdna origin (Humalog Mix 75/25, Humalog Mix 50/50)
antidiabetics hormones pancreatics
Hypoglycemia, erythema, lipodystrophy, pruritis, swelling, allergic reactions including anaphylaxis.
Insulin nph/Novolin N
Pancreatics, hormones/ antidiabetics
Hypoglycemia, lipodystrophy, pruritis, erythema, swelling, allergic reactions including anaphylaxis
Insulin Regular/ Humulin R, Novolin R, Iletin II Regular, Velosulin BR, Humulin R Regular U-500 (Concentrated)
Pancreatics, hormones/ antidiabetics
Hypoglycemia, lipodystrophy, pruritis, erythema, swelling, allergic reactions including anaphylaxis
117
Rev. 08/21/08
Interferon Alfacon-1/ Infergen
immune modifiers interferons
Assess patient for symptoms of hepatitis C, mood, depression, suicidal ideation, and other severe psychiatric disorders. Monitor liver function studies prior to and periodically during therapy. Monitor platelet count, hemoglobin, hematocrit, absolute neutrophil count (ANC), serum creatinine, bilirubin, and albumin concentrations, and TSH and T prior to and 2 wk after initiation of therapy and periodically during therapy. Assess for signs of neuropsychiatric disorders, signs of infection, cardiovascular disorders, ECG, signs of colitis and pancreatitis during therapy. Colitis usually resolves within 1 3 wks of discontinuation. Assess for development of flu-like syndrome. Symptoms often appear suddenly 36 hr after therapy. Monitor for bone marrow depression, bleeding, pulmonary status periodically during therapy. Perform a baseline eye exam in all patients prior to initiation of therapy. Assess for signs of thyroid dysfunction. Monitor number, size, and character of Kaposi Sarcoma lesions prior to and throughout therapy. Monitor for CBC and differential; liver function and renal function tests. Assess for signs of neuropsychiatric disorders, signs of infection, cardiovascular disorders, ECG, signs of colitis and pancreatitis during therapy. Colitis usually resolves within 1 3 wks of discontinuation.
anxiety, depression, dizziness, insomnia, nervousness, malaise, suicidal ideation, loss of visual acuity or visual field, tinnitus, abdominal pain, anorexia, diarrhea, dyspepsia, vomiting, constipation, dry mouth, flatulence, alopecia, pruritus, rash, hypothyroidism, anemia, leucopenia, thrombocytopenia, injection site reactions, body pain, paresthesia, allergic reactions including anaphylaxis, flu-like symptoms (headache, fatigue, fever).
Interferon alpha-2b/ Intron A
immune modifiers interferons
Neuropsychiatric disorders, confusion, depression, dizziness, fatigue, headache, insomnia, irritability, anxiety, blurred vision, nose bleeds, rhinitis, ischemic disorders, arrhythmias, chest pain, edema, colitis, pancreatitis, anorexia, abdominal pain, diarrhea, dry mouth, nausea, taste disorder, vomiting, weight loss, drug-induced hepatitis, flatulence, alopecia, dry skin, pruritus, rash, sweating, thyroid disorders, leucopenia, thrombocytopenia, anemia, hemolytic anemia (with ribavirin), arthralgia, myalgia, leg cramps, paresthesia, cough, dyspnea, injection site reactions, autoimmune disorders, infectious disorders, allergic reactions including anaphylaxis, chills, fever, flulike syndrome.
Interferon alpha-n3/ Alferon N
immune modifiers interferons
Neuropsychiatric disorders, confusion, depression, dizziness, fatigue, headache, insomnia, irritability, anxiety, blurred vision, nose bleeds, rhinitis, ischemic disorders, arrhythmias, chest pain, edema, colitis, pancreatitis, anorexia, abdominal pain,
118
Rev. 08/21/08
Assess for development of flu-like syndrome. Symptoms often appear suddenly 36 hr after therapy. Monitor for bone marrow depression, bleeding, pulmonary status periodically during therapy. Perform a baseline eye exam in all patients prior to initiation of therapy. Assess for signs of thyroid dysfunction. Monitor number, size, and character of Kaposi Sarcoma lesions prior to and throughout therapy. Monitor for CBC and differential; liver function and renal function tests. Interferon Beta-1a/ Avonex, Rebif anti multiple sclerosis agents immune modifiers interferons Assess frequency of exacerbations of symptoms of multiple sclerosis periodically during therapy Monitor patient for signs of depression during therapy. If depression occurs, notify physician or other health care professional immediately Monitor hemoglobin, WBC, platelets, and blood chemistries including liver function tests prior to and 1, 3, and 6 mo after initiation of therapy.
diarrhea, dry mouth, nausea, taste disorder, vomiting, weight loss, drug-induced hepatitis, flatulence, alopecia, dry skin, pruritus, rash, sweating, thyroid disorders, leucopenia, thrombocytopenia, anemia, hemolytic anemia (with ribavirin), arthralgia, myalgia, leg cramps, paresthesia, cough, dyspnea, injection site reactions, autoimmune disorders, infectious disorders, allergic reactions including anaphylaxis, chills, fever, flulike syndrome.
Interferon Beta-1B/ Betaseron
anti multiple sclerosis agents immune modifiers interferons
Assess frequency of exacerbations of symptoms of multiple sclerosis periodically during therapy. Monitor patient for signs of depression during therapy. If depression occurs, notify physician or other health care professional immediately. Monitor hemoglobin, WBC, platelets, and blood chemistries including liver
Seizures, depression, dizziness, fatigue, headache, drowsiness, incoordination, rigors, suicidal ideation, sinusitis, vision abnormalities, upper respiratory tract infection, chest pain, heart failure, abdominal pain, nausea, autoimmune hepatitis, dry mouth, elevated liver function studies, urinary tract infection, urinary incontinence, polyuria, alopecia, rash, hyperthyroidism, hypothyroidism, spontaneous abortion, neutropenia, anemia, thrombocytopenia, injectionsite reactions, injection site necrosis, myalgia, arthralgia, back pain, muscle spasm, allergic reactions including anaphylaxis, chills, fever, flulike symptoms, pain. depression, headache, incoordination, insomnia, suicidal ideation, dyspnea, edema, chest pain, hypertension, abdominal pain, constipation, nausea, vomiting, autoimmune hepatitis, elevated liver function studies, urgency, erectile dysfunction, rash, menstrual disorders, hyperthyroidism, hypothyroidism, menorrhagia,
119
Rev. 08/21/08
function tests prior to and 1, 3, and 6 mo after initiation of therapy and periodically thereafter.
Interferon gamma1b/ Actimmune
immune modifiers interferons
Iodine / Iodide (strong iodine solution/Lugol's solution)
antithyroid agents iodine containing agents
Ipecac syrup
emetic
overdose/ poisoning from noncaustic substance COPD, rhinorrhea from rhinitis or common cold
Assess patient for signs and symptoms of infection before and throughout therapy. Flu-like syndrome is a frequent side effect that may decrease in severity as treatment continues. Monitor CBC with differential, platelet count, blood chemistries including liver and kidney function, and urinalysis before and every 3 mo throughout therapy. Assess for signs and symptoms of iodism, symptoms of hyperthyroidism, hypersensitivity reaction. Monitor thyroid function, serum potassium levels, thyroid stimulating hormone (TSH) and free T4 in neonates. assess LOC
spontaneous abortion, neutropenia, anemia, thrombocytopenia, injectionsite reactions , injection site necrosis, myalgia, muscle spasm, allergic reactions including anaphylaxis, chills, fever, flu-like symptoms, pain. Headache, decreased mental status, dizziness, nausea, vomiting, abdominal pain, rash, neutropenia, thrombocytopenia, edema or tenderness at injection site, arthralgia, myalgia, back pain, gait disturbances, chills, fever.
confusion, weakness, GI bleeding, diarrhea, nausea, vomiting, acneiform eruptions, hypothyroidism, goiter, hyperthyroidism, hyperkalemia, tingling, joint pain, hypersensitivity, iodism.
Ipratropium (Atrovent HFA)
allergy, cold and cough remedies; bronchodilators; anticholinergics
assess respiratory status
Irbesartan (Avapro)
antihypertensives; angiotensin ii receptor antagonists
Hypertension; diabetic nephropathy
BP (standing, sitting, lying), pulse; monitor renal function
Irinotecan (Camptosar)
antineoplastics; enzyme inhibitors
metastatic colorectal cancer
monitor vital signs, assess for bleeding
Myocarditis, sedation, arrhythmias, diarrhea, aspiration (can be fatal) dizziness, headache, epistaxis, nervousness, nasal dryness/ irritation, blurred vision, sore throat, bronchospasm, cough, hypotension, palpitations, GI irritation, nausea, rash, allergic reactions Angioedema, dizziness, hyperkalemia, fatigue, anxiety, headache, hypotension, edema, hypotension, tachycardia, chest pain, abdominal pain, rashes, diarrhea, dyspepsia, impaired renal function, n/v, pain Diarrhea, elevated liver enzymes, dizziness, headache, insomnia, weakness, rhinitis, dyspnea, vasodilation, coughing, edema, abdominal pain/cramping, anorexia, n/v, constipation, dyspepsia,
120
Rev. 08/21/08
Iron dextran (Dexferrum, InFeD)
antianemics; iron supplements
Iron deficiency
monitor BP and HR following IV admin
Iron polysaccharide (Hytinic, Nu-Iron, Niferex)
antianemics; iron supplements
treatment and prevention of iron deficiency anemia
assess bowel function for constipation or diarrhea
Iron sucrose (Venofer)
antianemics; iron supplements
iron deficiency anemia in chronic renal failure
monitor BP during infusion
Isocarboxazid (Marplan)
antidepressants; monamine oxidase inhibitors
depression
BP and pulse, I&Os, assess hepatic function
Isoniazid
antituberculars
Active or latent TB infection
Monitor hepatic function monthly
Isoproterenol/ Isuprel, Medihaler-Iso
antiarrhythmics bronchodilators adrenergics
Assess lung sounds, respiratory pattern, pulse, and blood pressure; and pulmonary function tests before initiating therapy and periodically throughout.
weight loss, flatulence, alopecia, rash, leukopenia, stomatitis, chills, dehydration, anemia, sweating, fever, back pain, injection site reactions, thrombocytopenia, colonic ulceration, abdominal enlargement, neutropenia Allergic reactions, seizures, hypotension, skin staining at IM site, dizziness, headache, syncope, abdominal pain, tachycardia, arthralgia, urticaria, phlebitis at IV site, fever, lymphadenopathy, n/v, pain at IM site, sweating epigastric pain, nausea, dark stools, constipation, dizziness, headache, syncope, vomiting, temporary staining of teeth, GI bleeding Hypersensitivity reactions, headache, n/v, diarrhea, leg cramps, dyspnea, dizziness, weakness, increased liver enzymes, cough, pruritus, hypotension, chest pain, CHF, hypertension, abdominal pain, taste perversion, hypervolemia, injection site reactions, sepsis, musculoskeletal pain, fever Hypertensive crisis, seizures, dizziness, blurred vision, headache, nausea, dry mouth, akathisia, restlessness, anxiety, ataxia, euphoria, black tongue, drowsiness, weakness, insomnia, dysuria, orthostatic hypotension, diarrhea, sexual dysfunction, dysuria, urinary incontinence, urinary retention, photosensitivity, constipation Drug-induced HEP, n/v, peripheral neuropathy, visual disturbances, psychosis, rashes, seizures, gynecomastia, blood dyscrasias, fever Nervousness, restlessness, tremor, headache, insomnia, arrhythmias, angina, hypertension, tachycardia, nausea, vomiting, xerostomia, hyperglycemia, pink/red discoloration of saliva.
121
Rev. 08/21/08
Isosorbide group
antianginals; nitrates
angina pectoris, chronic CHF
monitor BP and pulse routinely
Isotretinoin/ Accutane, Amnesteem
antiacne agents retinoids
Isradipine (DynaCirc, DynaCirc CR)
antianginals; antihypertensives; calcium channel blockers
hypertension; angina pectoris; vasospastic (Prinzmetals) angina
Assess skin, allergy to parabens prior to and periodically during therapy. Verify that patient receiving isotretinoin is registered with the iPLEDGE program and is completing all required interactions with their health care provider. Monitor liver function prior to therapy, after 1 mo of therapy, and periodically thereafter. BP, pulse, I&Os, daily weight, monitor ECG periodically
hypotension, tachycardia, dizziness, headache, paradoxic bradycardia, syncope, flushing, tolerance, n/v conjunctivitis, epistaxis, cheilitis, dry mouth, nausea, vomiting, pruritus, anemia, decreased high-density lipoproteins, hypercholesterolemia, hypertriglyceridemia, arthralgia, back pain, muscle/bone pain, suicide attempt, pseudotumor cerebri, severe birth defects
Itraconazole (Sporanox)
antifungal (systemic)
histoplasmosis; blastomycosis; aspergillosis; dermatophyte infection; oropharyngeal esophageal candidiasis
assess for s&s of infection periodically (vital signs, lung sounds, sputum, WBC, nail beds)
CHF, arrhythmias, stevensjohnson syndrome, peripheral edema, abnormal dreams, chest pain, anxiety, confusion, rash, dizziness, drowsiness, blurred vision, headache, nervousness, psychiatric disturbances, dry mouth, disturbed equilibrium, epistaxis, tinnitus, bradycardia, cough, dyspnea, palpitations, hypotension, constipation, n/v, syncope, tachycardia, abnormal liver function studies, anorexia, diarrhea, dysgeusia, dyspepsia, dysuria, nocturia, polyuria, sexual dysfunction, increased sweating, urinary frequency, dermatitis, flushing, erythema multiforme, photosensitivity, increased sweating, prutitus/ urticaria, gynecomastia, hyperglycemia, thrombocytopenia, anemia, leukopenia, gingival hyperplasia, paresthesia, joint stiffness, paresthesia, weight gain, muscle cramps, tremor Hepatotoxicity, toxic epidermal necrolysis, nausea, dizziness, drowsiness, fatigue, headache, flatulence, malaise, tinnitus, CHF, edema, hypertension, abdominal pain, anorexia, diarrhea, vomiting, albuminuria, decreased libido, erectile dysfunction, pruritus, photosensitivity, hypokalemia, adrenal insufficiency, allergic reactions, rash, fever
122
Rev. 08/21/08
Ixabepilone (Ixempra)
antineoplastics; epothilone B analog
metastatic or locally advanced breast cancer
monitor for hypersensitivity reaction; monitor CBC
Myelosuppression, nail disorder, fatigue, constipation, weakness, abdominal pain, n/v, anorexia, diarrhea, mucositis, stomatitis, hyperpigmentation, alopecia, myalgia, palmar-plantar erythrodysesthesia, arthralgia, musculoskeletal pain, peripheral neuopathy, dizziness, headache, insomnia, increased lacrimation, edema, chest pain, rash, myocardial ischemia, dyspnea, exfoliation, altered taste, pruritus, hot flushes, hypersensitivity reactions
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Kanamycin/ Kantrex
anti-infectives aminoglycosides
Kaolin/pectin/ KaoSpen, Kapectolin
antidiarrheals adsorbents
Kava-kava (Piper Methysticum)/ Ava pepper, intoxicating pepper, kao, kew, tonga, wurzelstock, yagona
antianxiety agents sedative/hypnotics
Assess patient for infection (vital signs, wound appearance, sputum, urine, stool, WBC); intake and output and daily weight; evaluate eighth cranial nerve function by audiometry; signs of superinfection at beginning of and throughout therapy. Monitor renal function by BUN and creatinine before and throughout therapy. Assess the frequency and consistency of stools and bowel sounds before and throughout course of therapy. Assess fluid and electrolyte balance and skin turgor for dehydration. Assess muscle spasm, associated pain, limitations of movement; degree of anxiety and level of sedation; sleep patterns prior to and periodically throughout therapy.
Ototoxicity, nephrotoxicity, muscle paralysis, hypersensitivity reactions.
Constipation
Ketamine/ Ketalar
general anesthetics
Monitor blood pressure, ECG, and respiratory status; and level of consciousness
Dizziness, headache, drowsiness, sensory disturbances, extrapyramidal effects, Pupil dilation, red eyes, visual accommodation disorders, hepatictoxicity, gastrointestinal complaints, allergic skin reactions, yellow discoloration of skin, pellagroid dermopathy, decreased lymphocytes, decreased platelets, weight loss, ataxia, muscle weakness. Emergence reactions, elevated intracranial pressure, diplopia, increased intraocular pressure,
123
Rev. 08/21/08
frequently throughout therapy.
Ketoconazole (systemic)/ Nizoral
antifungals (systemic)
Assess patient for symptoms of infection prior to and periodically during therapy. Monitor hepatic function tests prior to and monthly for 34 mo and then periodically during therapy.
Ketoconazole (topical)/ Extina, Nizoral, Nizoral AD, Xolegel Ketoprofen/ Actron, Orudis, Orudis KT, Oruvail
antifungals imidazoles
Inspect involved areas of skin and mucous membranes before and frequently during therapy. Assess pain and range of motion prior to and 1 hr following administration. Monitor temperature; note signs associated with fever. Evaluate BUN, serum creatinine, CBC, and liver function tests periodically in patients receiving prolonged therapy. Assess pain (note type, location, and intensity) prior to and 12 hr following administration. Evaluate liver function tests, especially AST and ALT, periodically in patients receiving prolonged therapy.
nystagmus, laryngospasm, respiratory depression and apnea, hypertension, tachycardia, arrhythmias, bradycardia, hypotension, excessive salivation, nausea, vomiting, erythema, rash, pain at injection site, increased skeletal muscle tone. Dizziness, drowsiness, photophobia, druginduced hepatitis, nausea, vomiting, abdominal pain, constipation, diarrhea, flatulence, azoospermia, decreased male libido, menstrual irregularities, oligospermia, rashes, gynecomastia. Burning, itching, local hypersensitivity reactions, redness, stinging, increased hair loss. Drowsiness, headache, druginduced hepatitis, GI bleeding, constipation, diarrhea, dyspepsia, nausea, vomiting, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, allergic reactions including anaphylaxis. Drowsiness, abnormal thinking, dizziness, euphoria, headache, asthma, dyspnea, edema, pallor, vasodilation, GI bleeding, abnormal taste, diarrhea, dry mouth, dyspepsia, GI pain, nausea, oliguria, renal toxicity, urinary frequency, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, pruritus, purpura, sweating, urticaria, prolonged bleeding time, injection site pain, paresthesia, allergic reactions including, anaphylaxis. Phimosis, burning, edema, erosion, erythema, itching.
antipyretics antirheumatics nonopioid analgesics nonsteroidal anti inflammatory agents nonopioid analgesics nonsteroidal anti inflammatory agents nonopioid analgesics pyrroziline carboxylic acid
Ketorolac/ Toradol
Kunecatechins/ Veregen
catechins
Assess genital and perianal area prior to and periodically during therapy.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
124
Rev. 08/21/08
Labetalol/ Trandate
antianginals antihypertensives beta blockers
Monitor blood pressure and pulse; orthostatic hypotension; intake and output ratios and daily weight frequently during dose adjustment and periodically during therapy. Patients receiving labetalol IV must be supine during and for 3 hr after administration. Vital signs should be monitored every 515 min during and for several hours after administration.
Lacosamide/ Vimpat
anticonvulsants
Lactulose/Cephulac
Osmotic; laxative
Lamotrigine/ Lamictal
anticonvulsants
Lamivudine/ Epivir, Epivir HBV, 3TC
antiretrovirals antivirals nucleoside reverse transcriptase inhibitors
Assess location, duration, and characteristics of seizure activity. Monitor closely for notable changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression. Assess ECG prior to therapy in patients with pre-existing cardiac disease. Assess patient for abdominal distention, presence of bowel sounds, and normal pattern of bowel function; color, consistency, and amount of stool produced Monitor for hypersensitivity reactions, and skin rash frequently during therapy. Assess location, duration, and characteristics of seizure activity. Assess mood, ideation, and behaviors frequently. Lamotrigine plasma concentrations may be monitored periodically during therapy, especially in patients concurrently taking other anticonvulsants. Assess patient for change in severity of symptoms of HIV infection and for symptoms of opportunistic infection; peripheral neuropathy; hepatitis; and signs of pancreatitis periodically during therapy. Monitor serum amylase, lipase,
Fatigue, weakness, anxiety, depression, dizziness, drowsiness, insomnia, memory loss, mental status changes, nightmares, blurred vision, dry eyes, nasal stuffiness, bronchospasm, wheezing, arrhythmias, bradycardia, CHF, pulmonary edema, orthostatic hypotension, constipation, diarrhea, nausea, erectile dysfunction, decreased libido, itching, rashes, hyperglycemia, hypoglycemia, arthralgia, back pain, muscle cramps, paresthesia, druginduced lupus syndrome. Dizziness, headache, syncope, vertigo, diplopia, PR interval prolongation, nausea, vomiting, ataxia, multiorgan hypersensitivity reactions
Belching, cramps, distention, flatulence, hyperglycemia (diabetic patients).
Ataxia, dizziness, headache, behavior changes, depression, drowsiness, insomnia, tremor, blurred vision, double vision, rhinitis, nausea, vomiting, vaginitis, photosensitivity, rash (higher incidence in children, patients taking VPA, high initial doses, or rapid dose increases), arthralgia, allergic or hypersensitivity reactions including StevensJohnson syndrome. Seizures, fatigue, headache, insomnia, malaise, depression, dizziness, cough, hepatomegaly with steatosis, pancreatitis, anorexia, diarrhea, nausea, vomiting, musculoskeletal pain, arthralgia, muscle weakness, myalgia, rhabdomyolysis,
125
Rev. 08/21/08
Lanreotide/ Somatuline Depot
hormones somatostatin analogues
Lansoprazole/ Prevacid
antiulcer agents proton pump inhibitors
Lanthanum carbonate/ Fosrenol
hypophosphatemics phosphate binders
Lapatinib/ Tykerb
antineoplastics enzyme inhibitors kinase inhibitors
Laronidase/Aldurazym e
replacement enzyme enzymes
triglycerides, liver function, viral load and CD4 levels before and periodically during therapy. Assess for GI side effects (diarrhea, abdominal pain, nausea, gas, constipation); usually decrease with continued treatment. Assess patient routinely for epigastric or abdominal pain and for frank or occult blood in stool, emesis, or gastric aspirate. Monitor INR and prothrombin time in patients taking warfarin. Assess patient for nausea and vomiting during therapy. Monitor serum phosphate levels prior to and periodically during therapy. Evaluate left ventricular ejection fraction (LVEF) prior to therapy to determine if within institution's normal limits. Monitor ECG and respiratory status for symptoms of interstitial lung disease and pneumonitis prior to and periodically during therapy. Monitor liver function tests prior to initiation and every 46 wks during therapy and as clinically indicated. Monitor serum potassium and magnesium prior to and periodically during therapy. Assess vital signs; anaphylaxis; and infusionrelated reaction during therapy. Assess range of motion and degree of swelling and pain in affected joints before and periodically during therapy. Monitor liver function throughout therapy. Assess ALT at baseline, then monthly during initial 6 mo of therapy, then every 68 wks. Monitor CBC with platelets monthly for 6 mo following initiation of therapy and every 68 wks thereafter.
neuropathy, hypersensitivity reactions including anaphylaxis and StevensJohnson syndrome. Bradycardia, hypertension, abdominal pain, diarrhea, gallstones, hyperglycemia, hypoglycemia, anemia, injection site reactions. Dizziness, headache, diarrhea, abdominal pain, nausea, rash.
Nausea, vomiting, diarrhea.
Fatigue, insomnia, dyspnea, interstitial lung disease, pneumonitis, left ventricular ejection fraction, hepatotoxicity, diarrhea, nausea, vomiting, dyspepsia, liver enzymes, stomatitis, palmar-plantar erythrodysesthesia, rash, dry skin, neutropenia, back pain, extremity pain.
Leflunomide/ Arava
antirheumatics (DMARDs) immune response modifiers
Respiratory tract infections, rash, injection site reactions, allergic reactions including anaphylaxis, infusion related reactions. Headache, dizziness, weakness, bronchitis, increased cough, pharyngitis, pneumonia, respiratory infection, rhinitis, sinusitis, chest pain, hypertension, diarrhea, nausea, alopecia, rash, dry skin, eczema, pruritus, hypokalemia, weight loss, arthralgia, back pain, joint disorder, allergic reactions, flu syndrome, infections including sepsis, pain.
126
Rev. 08/21/08
Lemon verbena/ Aloysia Triphylla, herb Louisa, louisa
antianxiety agents gastroinestinal anti inflammatories sedative/hypnotics
Lenalidomide/ Revlimid
antianemics immune response modifiers
Lepirudin (rDNA)/ Refludan
anticoagulants thrombin inhibitors
Letrozole/ Femara
antineoplastics aromatase inhibitors Antidotes (for methotrexate) vitamins folic acid analogues
Leucovorin calcium/ citrovorum factor, folinic acid, Wellcovorin
Leuprolide/ Eligard, Lupron, Lupron Depot, Lupron Depot-PED, Lupron Depot-3 Month
antineoplastics hormones gonadotropin releasing hormones
Assess patient for epigastric or abdominal pain, frank or occult blood in the stool that may be indicative of an ulcer. Assess degree and manifestations of anxiety and response and quantity of herb consumed. Assess pregnancy status prior to therapy. Effective contraception must be used for at least 4 wk prior to initiating therapy, during therapy, during dose interruptions, and for 4 wk following discontinuation of therapy, even with a history of infertility unless due to a hysterectomy or patient has been postmenopausal naturally for 24 consecutive months. Assess for signs of deep venous thrombosis and pulmonary edema; and skin rash periodically during therapy. Monitor CBC with differential, platelet count, hemoglobin and hematocrit weekly for first 8 wk of therapy and at least monthly thereafter. Assess patient for signs of bleeding and hemorrhage, and hypersensitivity reactions during therapy. Assess patient for pain and other side effects periodically throughout therapy. Assess patient for nausea and vomiting; and development of allergic reactions during therapy. Assess degree of weakness and fatigue. Monitor serum methotrexate levels to determine dosage and effectiveness of therapy. Leucovorin calcium levels should be equal to or greater than methotrexate level. Assess patient for an increase in bone pain, especially during the first few weeks of therapy. Monitor patients with vertebral metastases for
Contact dermatitis, kidney irritation from volatile oil excretion.
Dizziness, fatigue, headache, insomnia, depression, cough, pharyngitis, pulmonary embolism, edema, chest pain, deep vein thrombosis, palpitations, abdominal pain, constipation, diarrhea, nausea, vomiting, abnormal taste, anorexia, dry mouth, StevensJohnson syndrome, pruritus, rash, dry skin, sweating, hypothyroidism, hypokalemia, hypomagnesemia, neutropenia, thrombocytopenia, arthralgia, myalgia, fever, chills.
Bleeding, allergic reactions including anaphylaxis.
Nausea, weight gain, musculoskeletal pain, arthralgia, fractures. Thrombocytosis, allergic reactions
Dizziness, headache, syncope, depothair growth, rash, Subcutdry skin, hair loss, pigmentation, skin cancer, skin lesions, breast swelling, breast tenderness, diabetes,
127
Rev. 08/21/08
Levalbuterol/ Xopenex, Xopenex HFA
bronchodilators adrenergics
Levamisole/ Ergamisol
antineoplastics immune response modifiers
Levetiracetam/ Keppra
anticonvulsants pyrrolidines
Levocetirizine/ Xyzal
antihistamines piperazines
Levodopa/ Dopar, Larodopa, l-dopa
antiparkinson agents dopamine agonists
increased back pain and decreased sensory/motor function; intake and output ratios; bladder distention; severity of symptoms; endometrial pain prior to and periodically during therapy. Assess patient for signs of precocious puberty periodically during therapy. Monitor testosterone, prostatic acid phosphate, and prostate-specific antigen (PSA) levels to evaluate response to therapy. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; and paradoxical bronchospasm before initiating therapy and periodically throughout. Assess mucous membranes, number and consistency of stools, and frequency of vomiting. Assess for signs of infection; bleeding; and central nervous system toxicity during therapy. Hematologic functions should be monitored prior to and throughout therapy. CBC with differential and platelets, electrolytes, and liver function tests should be performed on the 1st day of therapy. Assess location, duration, and characteristics of seizure activity; somnolence and fatigue (asthenia), coordination difficulties (ataxia, abnormal gait, or incoordination), and behavioral abnormalities throughout therapy. Assess allergy symptoms; lung sounds and character of bronchial secretions before and periodically during therapy. Assess parkinsonian symptoms, blood pressure and pulse frequently during therapy. Monitor hepatic and renal function and CBC periodically in patients on
hypercalcemia, lower extremity edema, burning, itching, swelling at injection site, depothyperuricemia, increased bone density, fibromyalgia, transient increase in bone pain (prostate cancer only), Subcut ankylosing spondylitis, joint pain, pelvic fibrosis, temporal bone pain, Subcutperipheral neuropathy, hot flashes, chills, decreased libido, fever, depotbody odor, epistaxis.
Anxiety, dizziness, headache, nervousness, increased cough, paradoxical bronchospasm, turbinate edema, tachycardia, dyspepsia, vomiting, hyperglycemia, hypokalemia, tremor. Fatigue, anxiety, central nervous system toxicity, depression, depression, dizziness, drowsiness, conjunctivitis, diarrhea, metallic taste, nausea, stomatitis, vomiting, abdominal pain, anorexia, dyspepsia, flatulence, alopecia, dermatitis, pruritus, skin discoloration, agranulocytosis, anemia, leukopenia, thrombocytopenia, arthralgia, myalgia, ataxia, paresthesia, chills, fever. Dizziness, fatigue/somnolence, weakness, behavioral abnormalities, coordination difficulties.
Drowsiness, fatigue, weakness, dry mouth.
Involuntary movements, anxiety, dizziness, hallucinations, memory loss, psychiatric problems, blurred vision, mydriasis, nausea, vomiting, anorexia, dry
128
Rev. 08/21/08
long-term therapy.
Levofloxacin/ Levaquin
anti-infectives fluoroquinolones
Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC; urinalysis; frequency and urgency of urination; cloudy or foulsmelling urine); anaphylaxis; and bowel function at beginning of and during therapy.
Levoleucovorin calcium/ Fusilev
Antidotes (for methotrexate) vitamins folic acid analogues
Levonorgestrel/ Plan B
contraceptive hormones
Levorphanol/ LevoDromoran, Levorphan
opioid analgesics opioid agonists
Assess patient for nausea and vomiting; development of allergic reactions during therapy. Monitor serum methotrexate and creatinine at least once daily levels to determine dosage and effectiveness of therapy. Assess blood pressure and skin lesion before and periodically during therapy. Monitor hepatic function periodically during therapy. Assess type, location, and intensity of pain prior to and 90120 min following PO, 6090 min following subcut, and 20 min (peak) following IV administration. Assess blood pressure, pulse, and respirations; and bowel function before and periodically during therapy.
mouth, hepatotoxicity, melanoma, hemolytic anemia, leucopenia, darkening of urine or sweat. Seizures, dizziness, drowsiness, headache, insomnia, agitation, confusion, QTc prolongation, arrhythmias, hepatotoxicity, pseudomembranous colitis, abdominal pain, diarrhea, nausea, vomiting, vaginitis, photosensitivity, rash, hyperglycemia, hypoglycemia, phlebitis at IV site, peripheral neuropathy, arthralgia, tendinitis, tendon rupture, hypersensitivity reactions including anaphylaxis. Confusion, dyspnea, nausea, stomatitis, vomiting, altered taste, diarrhea, dyspepsia, dermatitis, abnormal renal function, neuropathy, allergic reactions.
Levothyroxine/ Synthroid
thyroid preparations, hormones
Assess apical pulse and blood pressure prior to therapy; tachyarrhythmias and chest pain.
Lidocaine/ LidoPen, Xylocaine, Anestacon, Xylocaine Viscous, Lidoderm, L-M-X 4, LM-
anesthetics topical local antiarrhythmics (class IB)
Monitor ECG continuously and blood pressure and respiratory status frequently during administration. Assess degree of numbness
Cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, melasma, rash, bone loss, weight change. Confusion, sedation, dysphoria, euphoria, dizziness, floating feeling, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, dry mouth, nausea, vomiting, urinary retention, flushing, sweating, pruritis, physical dependence, psychological dependence, tolerance. Insomnia, irritability, headache, arrhythmias, tachycardia, angina pectori, abdominal cramps, diarrhea, vomiting hyperhidrosis, hyperthyroidism, menstrual irregularities. weight loss, heat intolerance Seizures, confusion, drowsiness, blurred vision, dizziness, nervousness, slurred speech, tremor, mucosal usedecreased or
129
Rev. 08/21/08
X 5, Solarcaine Aloe Extra Burn Relief, Zilactin-L
of affected part. Serum electrolyte levels should be monitored periodically during prolonged therapy.
Lidocaine/prilocaine// EMLA
anesthetics topical local
Lindane/ gamma benzene hexachloride, G-Well, Scabene
pediculocides scabicide
Linezolid/ Zyvox
anti-infectives oxazolidinones
Liothyronine/ Cytomel, ltriiodothyronine, T3, Triostat
hormones thyroid preparations
Liotrix/ T3/T4, Thyrolar
hormones thyroid preparations
Assess application site for open wounds. Apply only to intact skin. Assess application site for anesthesia following removal of system and prior to procedure. Assess skin and hair for signs of infestation before and after treatment. Examine family members and close contacts for infestation. When used in treatment of pediculosis pubis or scabies, sexual partners should receive concurrent prophylactic therapy. Assess for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC); visual function; and bowel function at beginning of and during therapy. Monitor CBC and platelet count weekly, especially in patients at risk for increased bleeding, having pre-existing bone marrow suppression, receiving concurrent medications that may cause myelosuppression, or requiring >2 weeks of therapy. Assess apical pulse and blood pressure; tachyarrhythmias and chest pain; height, weight, and psychomotor development prior to and periodically during therapy. Monitor thyroid function studies prior to and during therapy. Monitor blood and urine glucose in diabetic patients. Assess apical pulse and blood pressure prior to and periodically during therapy.
absent gag reflex, cardiac arrest, arrhythmias, bradycardia, heart block, hypotension, nausea, vomiting, bronchospasm, stinging, burning, contact dermatitis, erythema, allergic reactions including anaphylaxis. Blanching, redness, alteration in temperature sensation, edema, itching, rash, allergic reactions including anaphylaxis.
Seizures, headache, tachycardia, nausea, vomiting, contact dermatitis (repeated application), local irritation.
Headache, insomnia, pseudomembranous colitis, diarrhea, increased liver function tests, nausea, taste alteration, vomiting, lactic acidosis, thrombocytopenia, optic neuropathy, peripheral neuropathy.
Insomnia, irritability, headache, arrhythmias, tachycardia, angina pectoris, abdominal cramps, diarrhea, vomiting, hyperhidrosis, hyperthyroidism, menstrual irregularities, weight loss, heat intolerance, accelerated bone maturation in children.
Insomnia, irritability, headache, arrhythmias, tachycardia, angina pectoris,
130
Rev. 08/21/08
Lisdexamfetamine/ Vyvanse
central nervous system stimulants sympathomimetics
Lisinopril/ Prinivil, Zestril
antihypertensives ace inhibitors
Assess for tachyarrhythmias and chest pain. Monitor thyroid function studies prior to and during therapy. Monitor blood and urine glucose in diabetic patients. Assess child's attention span, impulse control, and interactions with others. Monitor blood pressure, pulse, and respiration; growth, both height and weight; behavior change; dependence and abuse before administering and periodically during therapy. Monitor BP, pulse, and signs of angioedema. Monitor weight and assess patient routinely for resolution of fluid overload. Monitor renal function.
Lithium/Eskalith, Lithobid
mood stabilizers
Assess mental status; manic symptoms; intake and output ratios; and weight should also be monitored at least every 3 mo at baseline and periodically through treatment. Evaluate renal and thyroid function, WBC with differential, serum electrolytes, and glucose periodically during therapy. Monitor for bone marrow depression; bleeding; nausea and vomiting; and pulmonary function tests prior to initiation of therapy and periodically during therapy. Monitor CBC and differential; liver function studies (AST, ALT, LDH, bilirubin) and renal function studies (BUN, creatinine) prior to and periodically during therapy. Assess frequency and consistency of stools and bowel sounds prior to and during therapy. Assess fluid and electrolyte balance and skin turgor for dehydration.
Lomustine/ CCNU, CeeNu
antineoplastics alkylating agents
abdominal cramps, diarrhea, vomiting, hyperhidrosis, hyperthyroidism, menstrual irregularities, weight loss, heat intolerance, accelerated bone maturation in children. Behavioral disturbances, dizziness, hallucinations, insomnia, irritability, mania, psychomotor hyperactivity, thought disorder, tics, blurred vision, poor accommodation, abdominal pain, appetite, dry mouth, nausea, vomiting, rash, weight, long-term growth suppression. Dizziness, fatigue, headache, weakness, cough, hypotension, chest pain, abdominal pain, diarrhea, nausea, vomiting, erectile dysfunction, impaired renal function, rashes, hyperkalemia, angioedema. Seizures, fatigue, headache, impaired memory, arrhythmias, ECG changes, edema, hypotension, abdominal pain, anorexia, bloating, diarrhea, nausea, dry mouth, metallic taste, polyuria, acneiform eruption, folliculitis, hypothyroidism, leukocytosis, weight gain, muscle weakness, rigidity, tremors. Ataxia, disorientation, dysarthria, lethargy, fibrosis, pulmonary infiltrates, nausea, vomiting, anorexia, hepatotoxicity, stomatitis, azotemia, renal failure, alopecia, infertility, leukopenia, thrombocytopenia, anemia, hyperuricemia, secondary malignancy (longterm use).
Loperamide/Diar-aid Caplets, Imodium, Imodium A-D, Kaopectate II Caplets, Maalox Antidiarrheal Caplets, Neo-Diaral, Pepto Diarrhea Control
antidiarrheals
Drowsiness, dizziness, constipation, abdominal pain/distention/discomfort, dry mouth, nausea, vomiting, allergic reactions.
131
Rev. 08/21/08
Lopinavir/ritonavir// Kaletra
antiretrovirals protease inhibitors metabolic inhibitors
Loracarbef/ Lorabid
anti-infectives second generation cephalosporins
Assess for signs of pancreatitis; change in severity of HIV symptoms and for symptoms of opportunistic infections during therapy. Monitor triglyceride and cholesterol levels; and viral load and CD4 counts regularly during therapy. Assess patient for infection; anaphylaxis; obtain a history to determine previous use of and reactions to penicillins or cephalosporins at beginning of and throughout therapy.
Headache, insomnia, weakness, diarrhea( in children), abdominal pain, nausea, pancreatitis, taste aversion (in children), vomiting( in children), rash.
Loratadine
antihistamines
Assess allergy symptoms, lung sounds and character of bronchial secretions during therapy. Assess degree and manifestations of anxiety & mental status prior to & periodically throughout therapy. Assess blood pressure (lying, sitting, standing) and pulse; and signs of angioedema frequently during initial dosage adjustment and periodically during therapy. Monitor renal function.
Lorazepam/Ativan
Benzodiazepines; analgesic adjuncts, antianxiety agents, sedative, hypnotics antihypertensives angiotensin ii receptor antagonists
Losartan/ Cozaar
Lovage/ Angelica Levisticum, Hipposelecnum levisticum, lavose, Levisticum officinale, maggi plant, smellage Lovastatin/ Mevacor
diuretics
lipid-lowering agents hmg coa reductase inhibitors statin
Assess fluid intake, urine output and pedal edema. Monitor serum electrolytes, BUN and creatinine periodically throughout therapy. Obtain a diet history, especially with regard to fat consumption. Evaluate serum cholesterol and triglyceride levels before initiating, after 46 wk of therapy, and periodically thereafter. Monitor liver function tests, including AST, before, 12 wk after initiation of therapy or after dose elevation, and then
Seizures, pseudomembranous colitis, abdominal pain, diarrhea, nausea, vomiting, rashes, urticaria, vaginal moniliasis, vaginitis, eosinophilia, hemolytic anemia, leukopenia, thrombocytopenia, allergic reactions including anaphylaxis, superinfection. Confusion, drowsiness (rare), paradoxical excitation, blurred vision, dry mouth, GI upset, photosensitivity, rash, weight gain. Dizziness, drowsiness, lethargy, apnea, cardiac arrest, constipation, nausea, vomiting, confusion, mental depression Dizziness, fatigue, headache, insomnia, weakness, chest pain, edema, hypotension, nasal congestion, hypoglycemia, weight gain, diarrhea, abdominal pain, dyspepsia, nausea, impaired renal function, hyperkalemia, back pain, myalgia, angioedema, fever. Phototoxic dermatitis.
Dizziness, headache, insomnia, weakness, blurred vision, abdominal cramps, constipation, diarrhea, flatus, heartburn, altered taste, druginduced hepatitis, dyspepsia, elevated liver enzymes, nausea, pancreatitis, erectile dysfunction, rashes, pruritus, rhabdomyolysis, arthralgia, myalgia, myositis, hypersensitivity reactions.
132
Rev. 08/21/08
Loxapine/ Loxitane, Loxitane C, Loxitane IM
antipsychotics
Lubiprostone/ Amitiza
laxatives chloride channel activators
Lymphocyte immune globulin/ ATG, antilymphocyte globulin, Atgam, LIG
immunosuppressan ts immune globulins
every 6 mo. If patient develops muscle tenderness during therapy, CPK levels should be monitored. Monitor patient's mental status; positive (delusions, hallucinations, agitation) and negative (social withdrawal) symptoms of schizophrenia; weight and BMI; blood pressure (sitting, standing, lying) and pulse; onset of akathisia; extrapyramidal side effects; tardive dyskinesia; frequency and consistency of bowel movements; and development of neuroleptic malignant syndrome before and periodically during therapy. Monitor CBC and differential before and periodically throughout therapy. Monitor liver function studies and urine bilirubin and bile concentrations if patient develops jaundice. Assess for abdominal distention, presence of bowel sounds, and usual bowel patterns prior to and periodically during therapy. Assess color, consistency, and amount of stool produced. Assess patient for hypersensitivity reaction and vital signs frequently throughout therapy. Monitor CBC and platelets throughout therapy.
Neuroleptic malignant syndrome, confusion, dizziness, drowsiness, extrapyramidal reactions, headache, insomnia, syncope, tardive dyskinesia, weakness, blurred vision, lens opacities, nasal congestion, orthostatic hypotension, tachycardia, constipation, drug-induced hepatitis, dry mouth, ileus, nausea, vomiting, urinary retention, dermatitis, edema, facial photosensitivity, pigment changes, rashes, seborrhea, galactorrhea, agranulocytosis, ataxia, allergic reactions.
Dizziness, headache, peripheral edema, dyspnea, diarrhea, nausea, abdominal pain, abdominal distention, dyspepsia, dry mouth, reflux, arthralgia.
Headache, dyspnea, chest pain, hypotension, diarrhea, nausea, stomatitis, vomiting, dermatologic reactions, erythema, itching, leukopenia, thrombocytopenia, anemia, hemolysis, pain/phlebitis at IV site, arthralgia, allergic reactions including anaphylaxis, chills, fever, serum sicknesslike reactions, clotted AV fistula, night sweats.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Magnesium chloride/Mag Delay, Mag-SR, Slo-Mag
mineral electrolyte replacements supplements
Assess for signs and symptoms of hypomagnesemia Assess serum magnesium
diarrhea
133
Rev. 08/21/08
level and renal function before administering
Magnesium gluconate/ Almoate, Magtrate, Magonate
mineral electrolyte replacements supplements
Magnesium hydroxide/ Aluminum hydroxide/ Alamag, Maalox, Mylanta Ultimate, Rulox
antiulcer agents antacids
Magnesium oxide/Mag-Ox 400, Uro-Mag
mineral electrolyte replacements supplements
Magnesium salicylate
antipyretics non-opioid analgesics
Malathion
pediculocides
Mannitol
diuretics
Maraviroc
anti-retrovirals
Assess for signs and symptoms of hypomagnesemia Assess serum magnesium level and renal function before administering Assess for heartburn and indigestion as well as location, duration, character, and precipitating factors of gastric pain. Monitor serum phosphate, potassium, and calcium levels periodically during chronic use. Assess for signs and symptoms of hypomagnesemia Assess serum magnesium level and renal function before administering Assess pain and limitation of movement; note type, location, and intensity before and at the peak after administration. Assess fever and note associated signs (diaphoresis, tachycardia, malaise, chills) Assess scalp for presence of lice and their ova (nits) prior to and 1 wk after application Monitor vital signs, urine output, CVP, and pulmonary artery pressures (PAP) before and hourly throughout administration. Assess patient for signs and symptoms of dehydration or signs of fluid overload. Assess patient for anorexia, muscle weakness, numbness, tingling, paresthesia, confusion, and excessive thirst. Monitor neurologic status and intracranial pressure, persistent or increased eye pain or decreased visual acuity Assess patient for change in severity of HIV symptoms
diarrhea
aluminum salts constipation; magnesium saltsdiarrhea; magnesium salts hypermagnesemia; aluminum saltshypophosphatemia.
diarrhea
Allergic reactions including anaphylaxis and laryngeal edema, GI bleeding, dyspepsia, epigastric distress
Transient volume expansion
Allergic reactions, hepatotoxicity, abdominal
134
Rev. 08/21/08
Mebendazole
Anti-helmintics
Mecasermin
hormones
Mechlorethamine/ Mustargen, nitrogen mustard
antineoplastics alkylating agents
and for symptoms of opportunistic infections throughout therapy Assess for signs of hepatitis or allergic reaction (pruritic rash, jaundice, dark urine, and vomiting, abdominal pain). If symptoms occur, discontinue maraviroc immediately Pinworm: Perianal examinations should be performed to detect the presence of adult worms in the perianal area, and cellophane tape swabs of the perianal area should be taken before and starting 1 wk after treatment to detect the presence of ova. Swabs should be taken each morning before defecation or bathing for at least 3 days. Patients are not considered cured unless perianal swabs have been negative for 7 days Roundworm: Stool examinations should be monitored before and 13 wk after treatment Assess tonsils for hypertrophy periodically during therapy. To assess for intracranial hypertension, fundoscopic examinations are recommended prior to and periodically during therapy. May cause headache with nausea and vomiting, allergic reactions (rash, difficulty breathing), thickening of soft tissues of the face Monitor blood pressure, pulse, and respiratory rate; injection site; intake and output, appetite, and nutritional intake; nausea and vomiting; bone marrow depression; bleeding; and symptoms of gout during therapy. Monitor CBC and differential; liver function studies (AST, ALT, LDH, bilirubin); renal function studies (BUN, creatinine);
pain, dizziness, cough, upper respiratory tract infection, fever.
Seizures (rare)
Hypoglycemia, seizures, tonsillar hypertrophy.
Seizures, drowsiness, headache, vertigo, weakness, nausea, vomiting, anorexia, diarrhea, infertility, rashes, alopecia, leucopenia, thrombocytopenia, anemia, tissue necrosis, phlebitis at IV site, hyperuricemia, reactivation of herpes zoster.
135
Rev. 08/21/08
Meclizine
antiemetics antihistamines
Meclofenamate
anti-rheumatics non-opioid analgesics
Medroxyprogesterone (Depo-Provera, DeposubQ Provera 104)
contraceptive hormones
and uric acid concentrations before and periodically during therapy. Assess patient for level of sedation, nausea and vomiting before and 60 min after administration Assess degree of vertigo periodically in patients receiving meclizine for labyrinthitis Monitor for rhinitis, asthma, and urticaria Arthritis: Assess pain and range of movement before and periodically during therapy Pain: Assess location, duration, and intensity of pain before and 1 hr after administration Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Drowsiness
GI bleeding, drug-induced hepatitis, allergic reactions including anaphylaxis and stevens-johnson syndrome, dizziness, headache, diarrhea, dyspepsia, nausea, vomiting
Megestrol
anti-neoplastics hormones
Meloxicam
non-steroidal anti inflammatory agents
Assess patient for swelling, pain, or tenderness in legs. Report these signs of deep vein thrombophlebitis Anorexia: Monitor weight, appetite, and nutritional intake in patients with AIDS Patients who have asthma, aspirin-induced allergy, and nasal polyps are at increased risk for developing hypersensitivity reactions. Assess for rhinitis, asthma, and urticaria Assess pain and range of motion prior to and 12 hr following administration
depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. Thromboembolism, asymptomatic adrenal suppression (chronic therapy).
GI bleeding, exfoliative dermatitis, stevens-johnson syndrome, toxic epidermal necrolysis
136
Rev. 08/21/08
Melphalan/Alkeran, LPAM, phenylalanine mustard
antineoplastics alkylating agents
Assess for signs of infection; bleeding; nausea and vomiting; symptoms of gout; fatigue and dyspnea; and allergy to chlorambucil. Monitor CBC and differential weekly during therapy. Assess cognitive function (memory, attention, reasoning, language, ability to perform simple tasks) periodically during therapy Review patient's immunization history for contraindications and history of sensitivity to vaccine, a similar vaccine, or latex. Stopper of vial contains dry natural latex, which may cause allergic reactions in latex-sensitive patients Female Infertility : Gynecologic and endocrine examinations to determine the cause of infertility should be completed before therapy. Male Infertility: Urologic and endocrine examinations to determine the cause of infertility should be completed before therapy Monitor patients on chronic or high-dose therapy for CNS stimulation (restlessness, irritability, seizures) due to accumulation of normeperidine metabolite. Risk of toxicity increases with doses >600 mg/24 hr, chronic administration (>2 days), and renal impairment. Assess degree and manifestations of anxiety before and periodically throughout therapy Monitor blood pressure and pulse rate before and during initial therapy Prolonged high-dose therapy may lead to psychological or physical dependence. Restrict amount of drug
Bronchopulmonary dysplasia, pulmonary fibrosis, diarrhea, hepatitis, nausea, stomatitis, vomiting, infertility, alopecia, pruritus, rashes, menstrual irregularities, leukopenia, hyperuricemia, thrombocytopenia, anemia.
Memantine
anti-Alzheimers agents
Meningococcal polysaccharide diphtheria toxoid conjugate vaccine
vaccines/immunizin g agents
Pain at injection site
Menotropins
hormones
Thromboembolism, abdominal pain, bloating, pelvic pain
Meperidine
opioid analgesics
Seizures, confusion, sedation, hypotension, constipation, nausea, vomiting
Meprobamate
anti-anxiety agents sedative/hypnotics
Drowsiness, ataxia
137
Rev. 08/21/08
Mercaptopurine
anti-neoplastics
Meropenem
anti-infectives
Mesalamine
gastrointestinal anti-inflammatories
Mesna
antidotes
Mestranol/norethindro ne (Necon 1/50, Norethin 1/50M, Norinyl 1+50, Ortho-Novum 1/50)
contraceptive hormones
available to patient Geri: Assess fall risk and institute fall prevention strategies. Monitor hepatic function (AST, ALT, alkaline phosphatase, LDH, and bilirubin) weekly during therapy Observe patient for signs and symptoms of anaphylaxis (rash, pruritus, laryngeal edema, wheezing). Discontinue the drug and notify physician immediately if these symptoms occur. Have epinephrine, an antihistamine, and resuscitative equipment close by in the event of an anaphylactic reaction Monitor intake and output ratios. Fluid intake should be sufficient to maintain a urine output of at least 12001500 mL daily to prevent crystalluria and stone formation. Assess abdominal pain and frequency, quantity, and consistency of stools at the beginning of and during therapy Monitor for development of hemorrhagic cystitis in patients receiving ifosfamide Assess blood pressure, acne before and periodically during therapy. Monitor hepatic function periodically during therapy. Estrogens onlyMay cause serum glucose, sodium, triglyceride, VHDL, total cholesterol, prothrombin, and factors VII, VIII, IX, and X levels. May cause LDL and antithrombin III Levels.
Hepatotoxicity, anemia, leukopenia, thrombocytopenia
Seizures, apnea, pseudomembranous colitis, allergic reactions including anaphylaxis, diarrhea, nausea, vomiting
Anaphylaxis, headache
Metaproterenol/ Alupent
bronchodilators adrenergics
Assess lung sounds, pulse, and blood pressure;
depression, migraine headache, contact lens intolerance, optic neuritis, retinal thrombosis, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, edema, hypertension, Raynaud's phenomenon, thromboembolic phenomena, thrombophlebitis, abdominal cramps, bloating, cholestatic jaundice, gallbladder disease, liver tumors, nausea, vomiting, amenorrhea, breakthrough bleeding, dysmenorrhea, spotting, melasma, rash, hyperglycemia, weight change. Nervousness, restlessness, tremor, headache, insomnia,
138
Rev. 08/21/08
Metaxalone
skeletal muscle relaxants (centrally acting)
Metformin/Glucophage
Biguanides/ antidiabetics
Methadone
opioid analgesics
Methazolamide
diuretics
Methimazole
Anti-thyroid agents
pulmonary function tests; and paradoxical bronchospasm before initiating therapy and periodically throughout. Observe patient for drug tolerance and rebound bronchospasm. Symptoms of overdose include persistent agitation, chest pain or discomfort, decreased blood pressure, dizziness, hyperglycemia, hypokalemia, seizures, tachyarrhythmias, persistent trembling, and vomiting. Assess patient for pain, muscle stiffness, and range of motion before and periodically during therapy Geri: Assess geriatric patients for anti-cholinergic effects (sedation and weakness) When combined with oral sulfonylureas, observe for signs and symptoms of hypoglycemic reactions. assess for ketoacidosis or lactic acidosis. Assess type, location, and intensity of pain prior to and 12 hr (peak) following administration. Assess blood pressure, pulse, and respirations before and periodically during administration. Assess bowel function routinely. Assess patient for signs of opioid withdrawal (irritability, runny nose and eyes, abdominal cramps, body aches, sweating, loss of appetite, shivering, unusually large pupils, trouble sleeping, weakness, yawning). Assess for eye discomfort or decrease in visual acuity, signs of hypokalemia (muscle weakness, malaise, fatigue, ECG changes, vomiting) Monitor response for symptoms of hyperthyroidism or thyrotoxicosis, development
paradoxical bronchospasm (excessive use of inhalers), angina, arrhythmias, hypertension, tachycardia, nausea, vomiting, hyperglycemia.
Drowsiness, dizziness, nausea
abdominal bloating, diarrhea, nausea, vomiting, unpleasant metallic taste, hypoglycemia, lactic acidosis, decreased vitamin B12 levels Confusion, sedation, hypotension, constipation
Aplastic anemia, hemolytic anemia, leucopenia, depression, tiredness, weakness, anorexia, metallic taste, hyperchloremic acidosis, weight loss Agranulocytosis, rash
139
Rev. 08/21/08
Methocarbamol
skeletal muscle relaxants (centrally acting)
Methohexital
general anesthetics
Methotrexate
anti-neoplastics anti-rheumatics (DMARDs) immunosuppressan ts
of hypothyroidism, skin rash or swelling of cervical lymph nodes. Assess patient for pain, muscle stiffness, and range of motion before and periodically throughout therapy Monitor pulse and blood pressure every 15 min during parenteral administration. Geri: Assess geriatric patients for anticholinergic effects (sedation and weakness) Assess patient for allergic reactions (skin rash, asthma, hives, wheezing, hypotension) after parenteral administration. Keep epinephrine and oxygen on hand in the event of a reaction Monitor IV site. Injection is hypertonic and may cause thrombophlebitis. Avoid extravasation Assess blood pressure, ECG, heart rate, and respiratory status continuously throughout methohexital therapy. Methohexital should be used only by individuals qualified to administer anesthesia and experienced in endotracheal intubation. Apnea may occur immediately after IV injection, especially in the presence of opioid premedication Monitor IV site carefully. Extravasation may cause pain, swelling, ulceration, and necrosis. Intra-arterial injection may cause arteritis, vasospasm, edema, thrombosis, and gangrene of the extremity Monitor vital signs, abdominal pain, diarrhea, or stomatitis; bone marrow depression, bleeding. Apply pressure to venipuncture sites for 10 min. Assess for signs of infection during neutropenia. Monitor for increased fatigue, dyspnea,
Seizures (IV, IM only), allergic reactions including anaphylaxis (IM, IV use only) , dizziness, drowsiness, lightheadedness, anorexia, GI upset, nausea
Seizures, apnea, laryngospasm, cardiorespiratory arrest, shivering
Pulmonary fibrosis, aplastic anemia, arachnoiditis (IT use only), anorexia, hepatotoxicity, nausea, stomatitis, vomiting, anemia, leukopenia, thrombocytopenia, nephropathy
140
Rev. 08/21/08
Methoxypolyethylene glycol-epoetin beta
anti-anemics
and orthostatic hypotension, intake and output ratios and daily weights. Monitor for symptoms of pulmonary toxicity, symptoms of gout (increased uric acid, joint pain, edema). Encourage patient to drink at least 2 L of fluid each day. Assess nutritional status. Assess for development of nuchal rigidity, headache, fever, confusion, drowsiness, dizziness, weakness, or seizures, pain and range of motion, skin lesions prior to and periodically during therapy Monitor blood pressure, signs of allergic reactions, neurological status periodically during therapy, symptoms of anemia Assess lesions prior to and 3 months after last treatment Monitor blood pressure and pulse; intake and output ratios and weight and assess for edema daily; depression or other alterations in mental status; temperature during therapy. Monitor renal and hepatic function and CBC before and periodically during therapy. Monitor blood pressure, heart rate, and uterine response, signs of ergotism (cold, numb fingers and toes, chest pain, nausea, vomiting, headache, muscle pain, weakness) Assess bowel sounds and frequency, quantity, and consistency of stools; pain intensity during therapy. Monitor blood pressure, pulse, and respiration before administering and periodically during therapy. Pedi: Monitor growth, both height and weight, attention span, impulse control, and interactions with others.
Methyl aminolevulinate Methyldopa/ Aldomet
anti-neoplastics
antihypertensives centrally acting antiadrenergics
Seizures, cardiovascular and thrombotic events, pure red aplasia, allergic reactions including anaphylaxis, headaches, hypertension, diarrhea Burning, contact sensitization, erythema, irritation, itching, pain in area of application Sedation, decreased mental acuity, depression, nasal stuffiness, myocarditis, bradycardia, edema, orthostatic hypotension, druginduced hepatitis, diarrhea, dry mouth, erectile dysfunction, eosinophilia, hemolytic anemia, fever. Hypertension, nausea, vomiting, cramps
Methylergonovine
oxytocic
Methylnatrexone
laxatives
Abdominal pain, flatulence, nausea
Methylphenidate
central nervous system stimulants
Hyperactivity, insomnia, restlessness, tremor, hypertension, palpitations, tachycardia, anorexia
141
Rev. 08/21/08
Methylprednisolone / A-Methapred, depMedalone, Depoject, DepoMedrol, Depopred, Depo-Predate, Duralone, Medralone, Medrol, Meprolone, Rep-Pred, Solu-Medrol
anti inflammatories steroidal immunosuppressan ts corticosteroids
Metoclopramide
anti-emetics
Metocurine/ Metubine
neuromuscular blocking agents nondepolarizing
Metolazone
anti-hypertensives diuretics
Metoprolol/Lopressor
Beta blocker, antianginals, antihypertensive
Assess patient for signs of adrenal insufficiency; intake and output ratios; daily weights; and signs of anaphylaxis before and periodically throughout therapy. Observe patient for peripheral edema, steady weight gain, rales/crackles, or dyspnea. Children should have periodic evaluations of growth. Guaiac test stools. Promptly report presence of guaiac-positive stools Assess patient for nausea, vomiting, abdominal distention, and bowel sounds before and after administration Assess patient for extrapyramidal side effects, tardive dyskinesia, neuroleptic malignant syndrome Assess respiratory status, Neuromuscular response, ECG, heart rate, and blood pressure, residual muscle weakness and respiratory distress, infusion site Monitor blood pressure, intake and output, and daily weight, feet, legs, and sacral area for edema daily , anorexia, nausea, vomiting, muscle cramps, paresthesia, and confusion. Monitor blood pressure before and periodically during therapy Monitor blood pressure, ECG, and pulse frequently during dose adjustment and periodically during therapy
depression, euphoria, hypertension, peptic ulceration, anorexia, nausea, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, thromboembolism, muscle wasting, osteoporosis, cushingoid appearance,
neuroleptic malignant syndrome, drowsiness, extrapyramidal reactions, restlessness
Bronchospasm, hypotension (increased with tubocurarine), allergic reactions including anaphylaxis.
Hypokalemia, hyperuricemia
Metronidazole
anti-infectives anti-protozoals anti-ulcer agents
Mexiletine
anti-arrhythmics (class IB)
Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC), neurologic status during and after IV infusions, intake and output and daily weight. Monitor pulse, blood pressure, and ECG periodically throughout therapy. Continuous Holter monitoring and chest x-ray
fatigue, weakness, anxiety, depression, dizziness, drowsiness, insomnia, memory loss, mental status changes, nervousness, nightmares, bradycardia, CHF, pulmonary edema, decreased libido Seizures, dizziness, headache, abdominal pain, anorexia, nausea
Arrhythmias, hepatic necrosis, dizziness, nervousness, heartburn, nausea, vomiting, tremor
142
Rev. 08/21/08
Micafungin/ Mycamine
antifungals echinocandins
examinations may be necessary to determine efficacy and aid in dosage adjustment Assess type, location, and severity of pain prior to and periodically throughout therapy Assess symptoms of esophageal candidiasis, injection site reactions (phlebitis, thrombophlebitis)
Miconazole (topical)/ Fungoid, Lotrimin AF, Micatin, MonistatDerm, Zeasorb-AF Miconazole (vaginal)/ Monistat-1, Monistat3, Monistat-7, Vagistat-3 Midazolam/ Versed
antifungals (topical)
Inspect involved areas of skin and mucous membranes
worsening hepatic function/hepatitis, renal impairment, hemolysis/ hemolytic anemia, injection site reactions, allergic reactions including anaphylaxis. burning, itching, local hypersensitivity reactions, redness, stinging.
antifungals (vaginal)
Inspect involved areas of skin and mucous membranes Assess level of sedation and level of consciousness throughout and for 26 hr following administration. Monitor blood pressure, pulse, and respiration continuously during IV administration. Monitor supine and sitting blood pressure, pattern of urinary output, renal and hepatic function
cramping, itching, vulvovaginal burning
antianxiety agents sedative/hypnotics benzodiazepines
Midodrine/ProAmatine
vasopressors
Mifepristone/ Mifeprex
abortifacients antiprogestational agents
Assess amount of bleeding and cramping during treatment. Determine duration of pregnancy. signs and symptoms of hypoglycemic reactions Assess for tremor, diarrhea and weight loss
Miglitol/ Glyset
Miglustat/ Zavesca
antidiabetics alpha glucosidase inhibitors enzyme inhibitors D-glucose analogue substrate reduction therapy
agitation, drowsiness, excess sedation, headache, blurred vision, apnea, laryngospasm, respiratory depression, bronchospasm, coughing, cardiac arrest, arrhythmias, hiccups, nausea, vomiting, rashes, phlebitis at IV site, pain at IM site. anxiety, confusion, head pressure/fullness, headache, nervousness, supine hypertension, bradycardia, urinary urge/retention/frequency, dysuria, facial flushing, piloerection, pruritus, rash, paresthesia, chills, pain. abdominal pain, diarrhea, nausea, vomiting, uterine bleeding, uterine cramping, dizziness, fainting, headache, weakness. abdominal pain, diarrhea, flatulence, low serum iron. Headache, abdominal pain, diarrhea, flatulence, nausea, weight loss, anorexia, dyspepsia, male fertility, thrombocytopenia, weight loss, paresthesia, peripheral neuropathy, tremor.
143
Rev. 08/21/08
Milnacipran/ Savella
antifibromyalgia agents selective norepinephrine reuptake inhibitors
Milrinone/ Primacor
inotropics
Assess intensity, quality, and location of pain, blood pressure and heart rate, notable changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression. Treat per-existing hypertension and cardiac disease prior to therapy. Monitor heart rate and blood pressure, ECG continuously during administration.
dizziness, headache, insomnia, hypertension, tachycardia, constipation, dry mouth, liver function abnormalities, nausea, vomiting, hot flushes, hyperhydrosis.
Mineral oil/ Fleet Mineral Oil, Kondremul Plain, Milkinol Minocycline/ Arestin, Dynacin, Minocin, Solodyn
laxatives lubricant laxatives
anti-infectives tetracyclines
Assess patient for abdominal distention, presence of bowel sounds, and usual pattern of bowel function Assess patient for infection
headache, tremor, ventricular arrhythmias, angina pectoris, chest pain, hypotension, supraventricular arrhythmias, skin rash, liver function abnormalities, hypokalemia, thrombocytopenia. lipid pneumonia, diarrhea, anal irritation, rectal seepage of mineral oil. benign intracranial hypertension, dizziness, vestibular reactions, diarrhea, nausea, vomiting, esophagitis, hepatotoxicity, pancreatitis, photosensitivity, rash, pigmentation of skin and mucous membranes, blood dyscrasias, lupus-like syndrome, hypersensitivity reactions, superinfection. Headache, pulmonary edema, CHF, ECG changes, tachycardia, angina, pericardial effusion, nausea, hypertrichosis, pigment changes, rashes, gynecomastia, menstrual irregularities, sodium and water retention, intermittent claudication. drowsiness, abnormal dreams, abnormal thinking, agitation, anxiety, apathy, confusion, dizziness, malaise, weakness, sinusitis, dyspnea, increased cough, edema, hypotension, vasodilation, constipation, dry mouth, increased appetite, abdominal pain, anorexia, elevated liver enzymes, nausea, vomiting, urinary frequency, pruritus, rash, increased thirst, agranulocytosis, weight gain, hypercholesterolemia,
Minoxidil (systemic)/ Loniten
antihypertensives vasodilators
Monitor blood pressure and pulse, intake and output ratios and daily weight and assess for edema daily
Mirtazapine/ Remeron, Remeron Soltabs
antidepressants tetracyclic antidepressants
Assess mental status (orientation, mood, behavior), suicidal tendencies, weight and BMI, blood pressure and pulse rate. Monitor for seizure activity in patients with a history of seizures or alcohol abuse.
144
Rev. 08/21/08
Misoprostol/ Cytotec
antiulcer agents cytoprotective agents prostaglandins
Mitomycin/ MitoExtra, Mutamycin
antineoplastics antitumor antibiotics
Assess patient routinely for epigastric or abdominal pain and for frank or occult blood in the stool, emesis, or gastric aspirate. Assess women of childbearing age for pregnancy. Monitor vital signs, respiratory status and chest x-ray examination. Nausea and vomiting usually occur within 12 hr. Vomiting may stop within 34 hr.
increased triglycerides, arthralgia, back pain, myalgia, hyperkinesia, hypesthesia, twitching, flu-like syndrome. Headache, abdominal pain, diarrhea, constipation, dyspepsia, flatulence, nausea, vomiting, miscarriage, menstrual disorders.
Mitotane/ o,p'-DDD, Lysodren
antineoplastics
Monitor for symptoms of adrenal insufficiency, development of doselimiting side effects (severe nausea, vomiting, anorexia, or diarrhea), neurologic status; report depression, lethargy, and complaints of dizziness
Mitoxantrone/Novantr one
antineoplastics immune modifiers antitumor antibiotics
Monitor for hypersensitivity reaction, bleeding, chest xray, ECG, echocardiography or MUGA, and radionuclide angiography to determine ejection fraction, symptoms of gout. Encourage patient to drink at least 2 L of fluid per day.
Modafinil/ Provigil
central nervous system stimulants
Observe and document frequency of narcoleptic
Pulmonary toxicity, edema, nausea, vomiting, anorexia, stomatitis, infertility, renal failure, alopecia, desquamation, leukopenia, thrombocytopenia, anemia, phlebitis at IV site, hemolytic uremic syndrome, fever, prolonged malaise. lethargy, somnolence, brain damage, dizziness, fatigue, functional impairment (highdose, long-term therapy), headache, irritability, mental depression, tremors, vertigo, weakness, blurred vision, decreased hearing, diplopia, lens opacities, optic neuritis, toxic retinopathy, shortness of breath, wheezing, hypertension, hypotension, anorexia, diarrhea, nausea, vomiting, increased salivation, albuminuria, hematuria, hemorrhagic cystitis, maculopapular rash, flushing, adrenal suppression, gynecomastia, hypercholesterolemia, hypouricemia, aching, arthralgia, myalgia, fever. Seizures, headache, bluegreen sclera, conjunctivitis, cough, dyspnea, cardiotoxicity, arrhythmias, ECG changes, abdominal pain, diarrhea, hepatic toxicity, nausea, stomatitis, vomiting, blue-green urine, gonadal suppression, renal failure, alopecia, rashes, anemia, leukopenia, secondary leukemia, thrombocytopenia, hyperuricemia, fever, hypersensitivity reactions. headache, amnesia, anxiety, cataplexy, confusion,
145
Rev. 08/21/08
episodes
Moexipril/ Univasc
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor renal function.
Molindone/ Moban
antipsychotics
Assess patient's mental status (orientation, mood, behavior), weight and BMI, fluid intake and bowel function, onset of akathisia (restlessness or desire to keep moving) and extrapyramidal side effects, tardive dyskinesia, development of neuroleptic malignant syndrome,
Mometasone (nasal)/ Nasonex
anti inflammatories steroidal corticosteroids
Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing,
Mometasone (topical)/ Elocon
anti inflammatories steroidal corticosteroids
Assess affected skin prior to and daily during therapy. Note degree of inflammation and pruritus.
depression, dizziness, insomnia, nervousness, rhinitis, abnormal vision, amblyopia, epistaxis, pharyngitis, dyspnea, lung disorder, arrhythmias, chest pain, hypertension, hypotension, syncope, vasodilation, nausea, abnormal liver function, anorexia, diarrhea, gingivitis, mouth ulcers, thirst, vomiting, abnormal ejaculation, albuminuria, urinary retention, dry skin, herpes simplex, hyperglycemia, eosinophilia, joint disorder, neck pain, ataxia, dyskinesia, hypertonia, paresthesia, tremor, infection. dizziness, fatigue, headache, cough, hypotension, chest pain, edema, diarrhea, dyspepsia, impaired renal function, flushing, rashes, hyperkalemia, myalgia, angioedema, flu-like symptoms. Neuroleptic malignant syndrome, extrapyramidal reactions, sedation, depression, dizziness, euphoria, headache, insomnia, tardive dyskinesia, blurred vision, dry eyes, nasal congestion, hypotension, tachycardia, constipation, dry mouth, anorexia, drug-induced hepatitis, nausea, photosensitivity, rashes, galactorrhea, increased libido, irregular menses, allergic reactions. Headache, pharyngitis, epistaxis, nasal burning, nasal irritation, nasopharyngeal fungal infection, sinusitis, vomiting, dysmenorrheal, adrenal suppression (increased dose, long-term therapy only), decreased growth (children), pain, cough. allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral
146
Rev. 08/21/08
Monobasic potassium phosphate/ K-Phos Original
antiurolithics mineral electrolyte replacements supplements
Assess patient for signs and symptoms of hypokalemia, hypophosphatemia, pulse, blood pressure, and ECG, intake and output ratios and daily weight
Montelukast/ Singulair
allergy, cold and cough remedies bronchodilators leukotriene antagonists
Assess lung sounds and respiratory function, allergy symptoms (rhinitis, conjunctivitis, hives), notable changes in behavior
Morphine/ Astramorph, Astramorph PF, Avinza, Duramorph, DepoDur, Infumorph, Kadian, MS, MS Contin, MSIR, MSO4, MS Concentrate, Oramorph SR, RMS, Roxanol, Roxanol Rescudose, Roxanol-T Moxifloxacin/ Avelox
opioid analgesics opioid agonists
anti-infectives fluoroquinolones
Assess type, location, and intensity of pain prior to and 1 hr following PO, subcut, IM, and 20 min (peak) following IV administration. Patients on a continuous infusion should have additional bolus doses provided every 1530 min, as needed, for breakthrough pain. Assess level of consciousness, blood pressure, pulse, and respirations, bowel function Assess for infection (vital signs, appearance of sputum, WBC), signs and symptoms of anaphylaxis, bowel function. Diarrhea, abdominal cramping, fever, and bloody stools
dermatitis, secondary infection, striae, adrenal suppression confusion, listlessness, weakness, arrhythmias, cardiac arrest, ECG changes, hypotension, diarrhea, abdominal pain, nausea, vomiting, hyperkalemia, hyperphosphatemia, hypocalcemia, hypomagnesemia, irritation at IV site, phlebitis, flaccid paralysis, heaviness of legs, paresthesias. hyperkalemiamuscle cramps; arrhythmias, ECG hypercalcemiatremors. anxiety, depression, fatigue, headache, suicidal thoughts/behaviors, weakness, cough, rhinorrhea, increased liver enzymes, tremor, rash, eosinophilic conditions including churgstrauss syndrome, fever. Children: otitis, sinusitis, abdominal pain, diarrhea, dyspepsia, nausea. confusion, sedation, dizziness, dysphoria, euphoria, floating feeling, hallucinations, headache, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, hypotension, bradycardia, constipation, nausea, vomiting, urinary retention, flushing, itching, sweating, physical dependence, psychological dependence, tolerance. agitation, anxiety, dizziness, headache, insomnia, QTc prolongation, arrhythmias, pseudomembranous colitis, abdominal pain, abnormal liver function tests, diarrhea, dyspepsia, nausea, vomiting, photosensitivity, tendinitis, tendon rupture, hypersensitivity reactions including anaphylaxis. Urine discoloration (preparations with B vitamins), allergic reactions to preservatives, additives, or
MULTIPLE VITAMINS/ Adavite, Certagen, Dayalets, Hexavitamin, LKV
vitamins
Assess patient for signs of nutritional deficiency before and throughout therapy.
147
Rev. 08/21/08
Drops, Multi-75, MultiDay, Nutrox, One-ADay, Optilets, Poly-ViSol, Quintabs, Ru-lets, Sesame Street Vitamins, Sigtab, Syrvite, Tab-A-Vite, Therabid, Theragran, Thera Multi-Vitamin, Theravee, Theravim, Theravite, Therems, Unicaps, Vita-Bob, Vita-Kid, Zymacap Multivitamin infusion/ B complex with C and B, Cernevit-12, Multi Vitamin Concentrate, M.V.I.-12, M.V.I. Pediatric Mupirocin/ Bactroban, Bactroban Nasal
colorants.
vitamins
Assess patient for signs of nutritional deficiency before and throughout therapy.
Urine discoloration (preparations with B vitamins), allergic reactions to preservatives, additives, or colorants.
anti-infectives
Assess lesions before and daily during therapy
Muromonab-CD3/ Orthoclone OKT3
immunosuppressan ts monoclonal antibodies
Mycophenolic acid/ Myfortic
immunosuppressan ts
Assess for fluid overload, vital signs and breath sounds, signs of anaphylactic or hypersensitivity reactions, infection, development of aseptic meningitis. Assess for cytokine release syndrome (CRS), usually manifested by high fever and chills, headache, tremor, nausea and vomiting, chest pain, muscle and joint pain, generalized weakness, shortness of breath, dizziness, abdominal pain, malaise, diarrhea, and trembling of hands, but may occasionally cause a severe, life-threatening, shock-like reaction. Assess for symptoms of organ rejection, signs of progressive multifocal leukoencephalopathy (hemiparesis, apathy, confusion, cognitive deficiencies and ataxia)
nasal onlyheadache, cough, itching, pharyngitis, rhinitis, upper respiratory tract congestion, altered taste. nausea topical onlyburning, itching, pain, stinging. tremor, aseptic meningitis, dizziness, pulmonary edema, dyspnea, shortness of breath, wheezing, chest pain, diarrhea, nausea, vomiting, cytokine release syndrome, infections, chills, fever, hypersensitivity reactions, increased risk of lymphoma.
Progressive multifocal leukoencephalopathy, anxiety, dizziness, headache, insomnia, paresthesia, tremor, edema, hypertension, hypotension, tachycardia, rashes, hypercholesterolemia, hyperglycemia, hyperkalemia, hypocalcemia, hypokalemia, hypomagnesemia, GI
148
Rev. 08/21/08
Mycophenolate mofetil/ CellCept
immunosuppressan ts
Assess for symptoms of organ rejection, signs of progressive multifocal leukoencephalopathy (hemiparesis, apathy, confusion, cognitive deficiencies and ataxia)
bleeding, anorexia, constipation, diarrhea, nausea, vomiting, abdominal pain, renal dysfunction, leukocytosis, leukopenia, thrombocytopenia, anemia, cough, dyspnea, fever, infection, increased risk of malignancy. Progressive multifocal leukoencephalopathy, anxiety, dizziness, headache, insomnia, paresthesia, tremor, edema, hypertension, hypotension, tachycardia, rashes, hypercholesterolemia, hyperglycemia, hyperkalemia, hypocalcemia, hypokalemia, hypomagnesemia, GI bleeding, anorexia, constipation, diarrhea, nausea, vomiting, abdominal pain, renal dysfunction, leukocytosis, leukopenia, thrombocytopenia, anemia, cough, dyspnea, fever, infection, increased risk of malignancy.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Nabilone/ Cesamet
antiemetics cannabinoids
Monitor patient closely for altered mental status. Monitor vital signs periodically during therapy. Assess pain and range of motion before and periodically throughout therapy. Monitor for rhinitis, asthma, and urticaria throughout therapy. Evaluate BUN, serum creatinine, CBC, and liver function periodically in patients receiving prolonged therapy. Monitor blood pressure and pulse; orthostatic hypotension; intake and output ratios and daily weight; and evidence of fluid overload frequently during dose adjustment and periodically during therapy. Assess frequency and
Nabumetone/ Relafen
antirheumatics nonsteroidal anti inflammatory agents
Nadolol/ Corgard
antianginals antihypertensives beta blockers
Concentration difficulty, drowsiness, euphoria, sleep disturbance, vertigo, ataxia, hypotension, dry mouth, tachycardia, depression. GI bleeding, abdominal pain, diarrhea, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, allergic reactions including anaphylaxis, angioneurotic edema, agitation, anxiety, confusion, depression, dizziness, drowsiness, fatigue, headache, insomnia, weakness. Fatigue, weakness, anxiety, depression, dizziness, drowsiness, insomnia, blurred vision, dry eyes, bronchospasm, wheezing, arrhythmias, bradycardia, CHF, pulmonary edema, orthostatic hypotension, peripheral vasoconstriction,
149
Rev. 08/21/08
Nafarelin/ Synarel
hormones gonadotropin releasing hormones
Nafcillin/Nallpen, Unipen
anti-infectives penicillinase resistant penicillins
characteristics of angina periodically during therapy. Monitor patients receiving beta blockers for signs of overdose. Assess patient for endometriotic pain; signs of precocious puberty; onset of normal puberty and assess menstrual cycle, reproductive function, and final adult height periodically throughout therapy. Assess for infection; signs and symptoms of anaphylaxis; and vein for signs of irritation and phlebitis at beginning of and throughout therapy. Change IV site every 48 hr to prevent phlebitis. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Assess type, location, and intensity of pain before and 1 hr after IM or 30 min (peak) after IV administration. Assess blood pressure, pulse, and respirations before and periodically during administration. Monitor respiratory rate, rhythm, and depth; pulse, ECG, and blood pressure; and level of sedation frequently until effects of opioid wear off. Assess patient for signs and symptoms of opioid withdrawal. Assess patient for intensity of pain when nalmefene is used to treat postoperative respiratory depression. Monitor respiratory rate, rhythm, and depth; pulse, ECG, blood pressure; and level of consciousness frequently for 34 hr after the expected peak of blood concentrations. Assess patient for level of pain after administration when used to
constipation, nausea, erectile dysfunction, back pain, muscle cramps, paresthesia, druginduced lupus syndrome. Emotional instability, headaches, nasal irritation, edema, vaginal dryness, acne, hirsutism, seborrhea, cessation of menses, impaired fertility, reduced breast size, decreased bone density, myalgia, decreased libido, hot flashes, weight gain. Seizures, rash, urticaria, pseudomembranous colitis, diarrhea, epigastric distress, nausea, vomiting, interstitial nephritis, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis and serum sickness, superinfection. Burning, dryness, itching, local hypersensitivity reactions, redness, stinging. Dizziness, headache, sedation, respiratory depression, hypertension, orthostatic hypotension, palpitations, dry mouth, nausea, vomiting, urinary urgency, clammy feeling, sweating, physical or psychological dependence, tolerance. Dysphoria, headache, hypertension, hypotension, tachycardia, vasodilation, abdominal cramps, nausea, joint pain, myalgia, chills, fever, postoperative pain.
Naftifine/ Naftin
antifungals (topical)
Nalbuphine/ Nubain
opioid analgesics opioid agonists analgesics
Nalmefene/ Revex
antidotes opioid antagonists
Naloxone/ Narcan
antidotes (for opioids) opioid antagonists
Hypertension, hypotension, ventricular fibrillation, ventricular tachycardia, nausea, vomiting.
150
Rev. 08/21/08
Naltrexone/ ReVia, Vivitrol
alcohol abuse therapy adjuncts opioid antagonists
treat postoperative respiratory depression. Assess patient for signs and symptoms of opioid withdrawal. Assess patient for last time opioids or alcohol were taken. Assess for signs of eosinophilic pneumonia.
Naltrexone injection/ Vivitrol
alcohol abuse therapy adjuncts opioid antagonists
Assess patient for last time opioids or alcohol were taken. Assess for signs of eosinophilic pneumonia. Monitor response for symptoms of anemia during therapy. Monitor CBC periodically throughout therapy. Assess pain and range of motion prior to and 12 hr following administration. Monitor temperature. Evaluate BUN, serum creatinine, CBC, and liver function tests periodically in patients receiving prolonged therapy. Assess pain location, character, intensity, and duration and associated symptoms (photophobia, phonophobia, nausea, vomiting) during migraine attack. Assess frequency of exacerbations of symptoms of multiple sclerosis periodically during therapy. Assess for signs of hypersensitivity reactions; new signs or symptoms that may be suggestive of PML, an opportunistic infection of the brain that leads to death or severe disability during therapy. Observe patient during infusion and for 1 hr after infusion is completed. Observe for signs and symptoms of hypoglycemic reactions. Monitor serum glucose and HbA1c periodically during therapy
Nandrolone decanoate/ Deca-Durabolin, Hybolin Decanoate, Kabolin Naproxen/Aleve, Anaprox, Anaprox DS, Apo-Napro-Na DS, ECNaprosyn, Naprelan, Napron X, Naprosyn
antianemics hormones anabolic steroids
nonopioid analgesics nonsteroidal anti inflammatory agents antipyretics
Naratriptan/ Amerge
vascular headache suppressants five ht1 agonists
Natalizumab/ Tysabri
anti multiple sclerosis agents monoclonal antibodies
Anxiety, fatigue, headache, insomnia, nervousness, eosinophilic pneumonia, hepatotoxicity, abdominal cramps/pain, nausea, injection site reactions. Dizziness, headache, eosinophylic pneumonia, anorexia, nausea, vomiting, eosinophils, platelets, injection site reactions. Insomnia, edema, muscle cramps, diarrhea, hepatic dysfunction, changes in libido, prostatic hyperplasia, acne, virilism in women and prepubertal men. Dizziness, drowsiness, headache, tinnitus, visual disturbances, dyspnea, tachycardia, drug-induced hepatitis, GI bleeding, constipation, dyspepsia, nausea, allergic reactions including anaphylaxis and Stevens-Johnson syndrome. Dizziness, drowsiness, malaise/fatigue, coronary artery vasospasm, MI, ventricular fibrillation, ventricular tachycardia, myocardial ischemia, nausea, paresthesia, pain/pressure sensation in throat/neck. Depression, fatigue, cholelithiasis, allergic reactions including anaphylaxis, infections, progressive multifocal leukoencephalopathy (PML), infusion-related reactions.
Nateglinide/ Starlix
antidiabetics meglitinides
Dizziness, bronchitis, coughing, upper respiratory infection, diarrhea, hypoglycemia, arthropathy, back pain, flu symptoms.
151
Rev. 08/21/08
to evaluate effectiveness Nebivolol/ Bystolic antihypertensives beta blockers selective Monitor blood pressure, ECG, and pulse; intake and output ratios and daily weights; signs and symptoms of CHF prior to and periodically during therapy. Assess mental status; suicidal tendencies; blood pressure and pulse; liver function tests; and sexual dysfunction before and periodically during therapy. Monitor liver function periodically. Assess neurologic status frequently. Monitor CBC regularly. Assess patient for change in severity of HIV symptoms and opportunistic infections throughout therapy. Monitor viral load and CD4 cell counts regularly during therapy. Assess patient for infection at beginning of and throughout therapy. Monitor neurologic status. Prior to administering oral medication, assess patient"s ability to swallow. Assess pulse, respiratory rate, and blood pressure prior to administration. Assess neuromuscular status, including vital capacity, ptosis, diplopia, chewing, swallowing, hand grasp, and gait, prior to administering and at peak effect. Monitor abdominal status, bladder distention, intake and output during therapy. Monitor reversal of effects of neuromuscular blocking agents with a peripheral nerve stimulator. Monitor blood pressure, pulse, ECG, respiratory rate, cardiac index, PCWP, and central venous pressure frequently during administration. Monitor intake and output and weigh Dizziness, fatigue, headache.
Nefazodone
antidepressants
Nelarabine/ Arranon
antineoplastics antimetabolites
Nelfinavir/ Viracept
antiretrovirals protease inhibitors
Neomycin/ Neo-Fradin
anti-infectives aminoglycosides
Dizziness, insomnia, somnolence, dyspnea, bradycardia, hypotension, hepatic failure, hepatotoxicity, constipation, dry mouth, nausea, gastroenteritis, erectile dysfunction, rashes, decreased hematocrit. Anemia, leukopenia, neutropenia, thrombocytopenia, severe neurologic events. Seizures, diarrhea, anxiety, depression, pharyngitis, rhinitis, dyspnea, rash, dyspepsia, GI bleeding, arthritis, back pain, myalgia, myopathy, allergic reactions, fever, sweating, urticaria. Diarrhea, nausea, vomiting, hypersensitivity reactions.
Neostigmine/ Prostigmin
antimyasthenics cholinergics
Seizures, dizziness, weakness, lacrimation, miosis, bronchospasm, excess secretions, bradycardia, hypotension, abdominal cramps, diarrhea, excess salivation, nausea, vomiting, sweating, rashes.
Nesiritide/ Natrecor
vasodilators human B-type natriuretic peptide
Anxiety, confusion, dizziness, headache, hypotension (dose related), insomnia, drowsiness, amblyopia, apnea, cough, hemoptysis, hypotension, arrhythmias, bradycardia, abdominal pain,
152
Rev. 08/21/08
daily; and decrease in signs of CHF during therapy. Monitor BUN and serum creatinine.
Nevirapine/ Viramune
antiretrovirals non nucleoside reverse transcriptase inhibitors
Niacin/ Edur-Acin, NiaBid, Niac, Niacels, Niacor, Niaspan, Nicobid, Nico400, Nicolar, Nicotinex, nicotinic acid, SloNiacin, vitamin B Niacinamide/nicotina mide
lipid-lowering agents vitamins water soluble vitamins
Assess for change in severity of HIV symptoms and for symptoms of opportunistic infections throughout therapy. Assess for rash especially during 1st 6 wks of therapy. Monitor viral load and CD4 cell count regularly during therapy. Monitor for liver function at baseline and frequently during the first 18 wks for toxicity, especially during first 6 wks of therapy. Assess patient for signs of niacin deficiency prior to and periodically during therapy. Obtain a diet history, especially with regard to fat consumption. Monitor serum glucose and uric acid levels and hepatic function tests periodically during prolonged high-dose therapy. Assess patient for signs of niacin deficiency prior to and periodically during therapy. Obtain a diet history, especially with regard to fat consumption. Monitor serum glucose and uric acid levels and hepatic function tests periodically during prolonged high-dose therapy. Monitor blood pressure and pulse prior to therapy, during dosage titration, and periodically throughout therapy. Monitor ECG, intake and output ratios and daily weight, signs of CHF periodically during prolonged therapy. Assess location, duration, intensity, and precipitating factors of patient's anginal pain. Monitor serum potassium
nausea, vomiting, creatinine, renal failure, itching, rash, sweating, anemia, injection site reactions, back pain, leg cramps, paresthesia, tremor, fever. Headache, hepatotoxicity, elevated liver enzyme levels, nausea, abdominal pain, diarrhea, hepatitis, ulcerative stomatitis, rash (may progress to toxic epidermal necrolysis), granulocytopenia, myalgia, paresthesia, peripheral neuropathy, Stevens-Johnson syndrome, fever.
lipid-lowering agents vitamins water soluble vitamins
Nicardipine/ Cardene, Cardene SR, Cardene IV
antianginals antihypertensives calcium channel blockers
Nervousness, panic, blurred vision, loss of central vision, proptosis, toxic amblyopia, orthostatic hypotension, hepatotoxicity, GI upset, bloating, diarrhea, nausea, peptic ulceration, flushing of the face and neck, pruritus, burning, dry skin, increased sebaceous gland activity, rashes, stinging or tingling of skin, glycosuria. Nervousness, panic, blurred vision, loss of central vision, proptosis, toxic amblyopia, orthostatic hypotension, hepatotoxicity, GI upset, bloating, diarrhea, nausea, peptic ulceration, flushing of the face and neck, pruritus, burning, dry skin, increased sebaceous gland activity, rashes, stinging or tingling of skin, glycosuria. Abnormal dreams, anxiety, weakness, blurred vision, epistaxis, tinnitus, cough, dyspnea, shortness of breath, arrhythmias, CHF, peripheral edema, bradycardia, chest pain, hypotension, palpitations, syncope, tachycardia, abnormal results in liver function studies, anorexia, constipation, diarrhea, dry mouth, vomiting, dysuria, nocturia, polyuria,
153
Rev. 08/21/08
periodically. Monitor renal and hepatic functions periodically during longterm therapy.
Nicotine gum/ Nicorette, Thrive
smoking deterrents
Prior to therapy, assess smoking history. Assess patient for symptoms of smoking withdrawal periodically during nicotine replacement therapy. Evaluate progress in smoking cessation periodically during therapy. Prior to therapy, assess smoking history. Assess patient for symptoms of smoking withdrawal periodically during nicotine replacement therapy. Evaluate progress in smoking cessation periodically during therapy. Prior to therapy, assess smoking history. Assess patient for symptoms of smoking withdrawal periodically during nicotine replacement therapy. Evaluate progress in smoking cessation periodically during therapy. Prior to therapy, assess smoking history. Assess patient for symptoms of smoking withdrawal periodically during nicotine replacement therapy. Evaluate progress in smoking cessation periodically during therapy. Prior to therapy, assess smoking history. Assess patient for symptoms of smoking withdrawal periodically during nicotine replacement therapy. Evaluate progress in smoking cessation periodically during therapy. Monitor blood pressure and pulse; intake and output ratios; daily weight; ECG; and signs of CHF before and periodically during therapy.
Nicotine inhaler/ Nicotrol Inhaler
smoking deterrents
Nicotine lozenge/ Commit
smoking deterrents
Nicotine nasal spray/ Nicotrol NS
smoking deterrents
Nicotine transdermal/ Nicoderm CQ
smoking deterrents
NIFEdipine/ Adalat, Adalat CC, Afeditab CR, Nifedical XL, Procardia, Procardia XL
antianginals antihypertensives calcium channel blockers
flushing, pruritus/urticaria, rash, hyperglycemia, anemia, thrombocytopenia, weight gain, joint stiffness, tremor, Stevens-Johnson syndrome, gingival hyperplasia. Headache, insomnia, nervousness, weakness, pharyngitis, sinusitis, tachycardia, chest pain, hypertension, belching, increased appetite, increased salivation, oral injury, sore mouth, jaw ache, arthralgia, back pain, myalgia, paresthesia, allergy, pain. Headache, anxiety, local mouth/throat irritation, rhinitis, sinusitis, cough, tachycardia, dyspepsia, abnormal taste, diarrhea, flatulence, hiccups, nausea, back pain, jaw pain, myalgia, paresthesia, allergy, fever, flulike symptoms, pain. Headache, insomnia, nervousness, weakness, sinusitis, tachycardia, abdominal pain, constipation, diarrhea, dry mouth, dyspepsia, nausea, vomiting, dysmenorrheal, arthralgia, back pain, myalgia, paresthesia, allergy, pain. Anxiety, headache, impaired concentration, irritability, insomnia, restlessness, flatulence, nasopharyngeal irritation, sneezing, watering eyes, cough, sweating, chest pain, hypertension, acne, palpitations, tachycardia, dry mouth, hiccups. Headache, insomnia, dizziness, drowsiness, nervousness, weakness, sinusitis, tachycardia, abdominal pain, diarrhea, dry mouth, dyspepsia, nausea, vomiting, burning at patch site, erythema, pruritis, rash, sweating, back pain, myalgia, paresthesia, allergy, pain. Headache, peripheral edema, bradycardia, chest pain, hypotension, arrhythmias, CHF, palpitations, syncope, tachycardia, abnormal liver
154
Rev. 08/21/08
Assess location, duration, intensity, and precipitating factors of patient's anginal pain. Monitor serum potassium, renal and hepatic functions periodically during longterm therapy. Nilotinib/ Tasigna antineoplastics enzyme inhibitors kinase inhibitors Monitor ECG to assess the QTc interval at baseline, 7 days after initiation of therapy, and periodically thereafter. Monitor for myelosuppression, bleeding, fatigue, dyspnea, and othrostatic hypotension during therapy. Apply pressure to venipuncture sites for at least 10 min. Monitor serum electrolytes prior to and periodically during therapy. Monitor CBC every 2 wks for first 2 mo and monthly thereafter or as indicated. Patients should have a chest x-ray prior to initiation of therapy. Assess patient for symptoms of interstitial pneumonitis. Monitor hepatic function prior to and every 3 mo throughout therapy. Assess patient's neurologic status; blood pressure and pulse; intake and output ratios and daily weight; signs of CHF prior to and periodically following therapy. Monitor serum potassium; renal and hepatic functions periodically.
Nilutamide/ Nilandron
antineoplastics antiandrogens
Nimodipine/ Nimotop
subarachnoid hemorrhage therapy agents calcium channel blockers
Nisoldipine/ Sular
antihypertensives calcium channel blockers
Nitazoxanide/ Alinia
antiprotozoals benzamides
Monitor blood pressure and pulse prior to therapy, during dosage titration, and periodically throughout therapy. Monitor intake and output ratios and daily weight; and CHF during therapy. Assess frequency and consistency of stools and bowel sounds; fluid and electrolyte balance and skin
function studies, anorexia, dysgeusia, dyspepsia, nausea, vomiting, dysuria, nocturia, polyuria, sexual dysfunction, urinary frequency, flushing, joint stiffness, muscle cramps, paresthesia, tremor, StevensJohnson syndrome, gingival hyperplasia. Fatigue, headache, dizziness, vertigo, arrhythmias, hypertension, palpitations, QT prolongation, constipation, diarrhea, nausea, vomiting, abdominal discomfort, anorexia, dyspepsia, flatulence, hepatotoxicity, pruritus, rash, alopecia, flushing, hyperkalemia, hypocalcemia, hypokalemia, hyponatremia, fever, hypophosphatemia, myelosupression, lipase, hyperglycemia, musculoskeletal pain, paresthesia, night sweats. Dizziness, impaired adaptation to darkness, abnormal vision, interstitial pneumonitis, hypertension, hepatotoxicity, constipation, hepatitis, increased liver enzymes, nausea, hot flashes, hair loss, sweating. Abnormal dreams, anxiety, nervousness, weakness, blurred vision, tinnitus, arrhythmias, CHF, chest pain, hypotension, syncope, tachycardia, abnormal liver function studies, anorexia, pruritus/urticaria, rash, anemia, weight gain, joint stiffness, muscle cramps, paresthesia, tremor, StevensJohnson syndrome. Headache, dizziness, pharyngitis, sinusitis, peripheral edema, chest pain, hypotension, palpitations, nausea, rash, gynecomastia.
Dizziness, yellow eye discoloration, abdominal pain, diarrhea, vomiting, discolored urine, pruritus, sweating,
155
Rev. 08/21/08
Nitrofurantoin/ Furadantin, Macrobid, Macrodantin
anti-infectives
turgor for dehydration before and during therapy. Assess for signs and symptoms of urinary tract infection; intake and output ratios; and bowel function before and periodically during therapy. Monitor CBC routinely with patients on prolonged therapy.
fever. Dizziness, drowsiness, headache, nystagmus, pneumonitis, chest pain, pseudomembranous colitis, anorexia, nausea, vomiting, abdominal pain, diarrhea, drug-induced hepatitis, rust/brown discoloration of urine, blood dyscrasias, peripheral neuropathy, hypersensitivity reactions. Dizziness, headache, apprehension, restlessness, weakness, blurred vision, hypotension, tachycardia, syncope, abdominal pain, nausea, vomiting, contact dermatitis (transdermal or ointment), alcohol intoxication (large IV doses only), crosstolerance, flushing, tolerance. Dizziness, headache, restlessness, blurred vision, tinnitus, dyspnea, hypotension, palpitations, abdominal pain, nausea, vomiting, acidosis, phlebitis at IV site, cyanide toxicity, thiocyanate toxicity.
Nitroglycerin/ NitroTime, Nitro-Bid IV, Tridil, Nitrolingual, Nitromist, Nitro-Bid, Nitrostat, NitroQuick, Minitran, Nitrek, Nitro-Dur
antianginals nitrates
Assess location, duration, intensity, and precipitating factors of patient's anginal pain. Monitor blood pressure and pulse before and after administration. Patients receiving IV nitroglycerin require continuous ECG and blood pressure monitoring. Monitor blood pressure, heart rate, and ECG frequently throughout therapy; continuous monitoring is preferred. Pulmonary capillary wedge pressure (PCWP) may be monitored in patients with MI or CHF. Monitor serum methemoglobin concentrations in patients receiving >10 mg/kg and exhibiting signs of impaired oxygen delivery despite adequate cardiac output and arterial Pco2. Assess patient for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate. Assess geriatric and debilitated patients routinely for confusion. CBC with differential should be monitored periodically during therapy
Nitroprusside/ Nitropress
antihypertensives vasodilators
Nizatidine/ Axid, Axid AR
antiulcer agents histamine h2 antagonists
Norepinephrine/Levop hed
vasopressors
Monitor blood pressure every 23 min until stabilized and every 5 min thereafter. ECG should be monitored continuously. Monitor urine output and notify physician if it
Confusion, dizziness, drowsiness, hallucinations, headache, arrhythmias, constipation, diarrhea, druginduced hepatitis, nausea, decreased sperm count, erectile dysfunction, gynecomastia, anemia, agranulocytosis, aplastic anemia, neutropenia, thrombocytopenia, hypersensivity reactions. Anxiety, dizziness, phlebitis at IV site, headache, insomnia, restlessness, tremor, weakness, dyspnea, arrhythmias, bradycardia, chest pain, hypertension, decreased urine output, renal
156
Rev. 08/21/08
Norethindrone/ Errin, Camila, Jolivette, Micronor, Nor-Q D
contraceptive hormones
decreases to <30 ml/hr. Assess IV site frequently throughout infusion. Assess blood pressure and skin lesion before and periodically during therapy. Monitor hepatic function periodically during therapy.
failure, metabolic acidosis, hyperglycemia, fever. Depression, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, hypertension, Raynaud's phenomenon, amenorrhea, breakthrough bleeding, hyperglycemia, weight change. Depression, cerebral hemorrhage, cerebral thrombosis, coronary thrombosis, pulmonary embolism, hypertension, Raynaud's phenomenon, amenorrhea, breakthrough bleeding, hyperglycemia, weight change. Seizures, headache, arrhythmias, hepatoxicity, pseudomembranous colitis, diarrhea, nausea, hypersensitivity reactions including anaphylaxis. Drowsiness, fatigue, lethargy, agitation, confusion, extrapyramidal reactions, hallucinations, headache, insomnia, blurred vision, dry eyes, dry mouth, arrhythmias, hypotension, ECG changes, constipation, nausea, paralytic ileus, unpleasant taste, weight gain, urinary retention, photosensitivity, gynecomastia, blood dyscrasias.
Norethindrone/ethinyl acetate// Estrostep, Estrostep Fe
contraceptive hormones
Assess blood pressure and skin lesion before and periodically during therapy. Monitor hepatic function periodically during therapy.
Norfloxacin/ Noroxin
anti-infectives fluoroquinolones
Assess for infection, signs and symptoms of anaphylaxis, and bowel function at beginning of and during therapy. Monitor mental status, suicidal tendencies, weight and BMI, blood pressure and pulse, FBS and cholesterol levels before and during initial therapy. Monitor baseline and periodic ECGs in geriatric patients or patients with heart disease. Assess type, location, and severity of pain before and periodically during therapy. Assess leukocyte and differential blood counts, liver function, and serum glucose periodically. Assess for symptoms of hypoglycemia and hyperglycemia periodically during therapy. Monitor body weight periodically. Monitor blood glucose every 6 hr during therapy, more frequently in ketoacidosis and times of stress. Assess for symptoms of hypoglycemia and hyperglycemia periodically during therapy. Monitor body weight periodically. Monitor blood glucose every
Nortriptyline/ Aventyl, Pamelor
antidepressants tricyclic antidepressants
NPH insulin (isophane insulin suspension)/ Humulin N, NPH Iletin II, Novolin N
antidiabetics hormones pancreatics
Hypoglycemia, erythema, lipodystrophy, pruritis, swelling, allergic reactions including anaphylaxis.
NPH/regular insulin mixtures// Humulin 50/50, Humulin 70/30, Novolin 70/30
antidiabetics hormones pancreatics
Hypoglycemia, erythema, lipodystrophy, pruritis, swelling, allergic reactions including anaphylaxis.
157
Rev. 08/21/08
Nystatin/ Mycostatin, Nilstat, Nystex
antifungals (topical/local)
Nystatin (topical)/ Mycostatin, Nystop
antifungals
Nystatin (vaginal)/ Mycostatin
antifungals
6 hr during therapy, more frequently in ketoacidosis and times of stress. Inspect oral mucous membranes before and frequently throughout therapy. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Inspect involved areas of skin and mucous membranes before and frequently during therapy.
Diarrhea, nausea, stomach pain, vomiting, contact dermatitis, Stevens-Johnson syndrome. Burning, itching, local hypersensitivity reactions, redness, stinging. Irritation, sensitization.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Octreotide/ Sandostatin, Sandostatin LAR
antidiarrheals hormones
Ofloxacin/ Floxin
anti-infectives fluoroquinolones
Olanzapine/ Zyprexa
Antipsychotics, mood stabilizers, thienobenzodiazepi nes
Olmesartan/ Benicar
antihypertensives angiotensin ii receptor
Assess frequency and consistency of stools and bowel sounds; pulse and blood pressure; fluid and electrolyte balance and skin turgor for dehydration; signs of hypoglycemia; gallbladder disease; and pain prior to and periodically during therapy. Monitor 5HIAA, plasma serotonin, and plasma substance P in patients with carcinoid; plasma vasoactive intestinal peptide (VIP) in patients with VIPoma; and free T4 and serum glucose concentrations prior to and periodically during therapy. Assess patient for infection; signs and symptoms of anaphylaxis; and bowel function at beginning of and during therapy. Assess mental status, weight, BMI, fasting blood glucose, cholesterol levels, fluid intake and bowel function. Monitor BP, ECG, pulse, respiratory rate, for onset of akathisia, extrapyramidal side effects, tardive dyskinesia, development of neuroleptic malignant syndrome Assess blood pressure (sitting, lying, standing) and pulse; signs of angioedema
Dizziness, drowsiness, fatigue, headache, weakness, visual disturbances, edema, orthostatic hypotension, palpitations, abdominal pain, cholelithiasis, diarrhea, fat malabsorption, nausea, vomiting, flushing, hyperglycemia, hypoglycemia, injection-site pain.
Seizures, dizziness, headache, insomnia, pseudomembranous colitis, diarrhea, nausea, hypersensitivity reactions including anaphylaxis. Neuroleptic malignant syndrome, seizures, agitation, dizziness, headache, restlessness, sedation, weakness, amblyopia, rhinitis, constipation, dry mouth, weight loss or gain, tremor.
Dizziness, hypotension, hyperkalemia, impaired renal function, angioedema.
158
Rev. 08/21/08
antagonists Olopatadine (nasal spray)/ Patanase allergy, cold and cough remedies antihistamines
Olsalazine/ Dipentum
gastroinestinal anti inflammatories
Omalizumab/ Xolair
antiasthmatics monoclonal antibodies
Omega-3-acid ethyl esters/ Lovaza
lipid-lowering agents fatty acids
Omeprazole/Prilosec OTC
proton pump inhibitors, antiulcer agent
periodically during therapy. Monitor renal function. Assess for symptoms of seasonal allergic rhinitis (sneezing, runny nose, nasal itching) prior to and during therapy. Assess patient for allergy to sulfonamides and salicylates. Monitor intake and output ratios; abdominal pain and frequency, quantity, and consistency of stools at the beginning of and throughout therapy. Monitor urinalysis, BUN, and serum creatinine prior to and periodically during therapy. Monitor CBC prior to and every 36 mo during prolonged therapy. Assess lung sounds and respiratory function; allergy symptoms; allergic reactions within 2 hr of first or subsequent injections; and injection site reactions prior to and periodically during therapy. Obtain a diet history, especially with regard to fat consumption. Monitor serum triglyceride levels prior to and periodically during therapy. Monitor serum ALT periodically during therapy. Monitor serum LDL cholesterol levels periodically during therapy. Assess patient routinely for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate Assess patient for nausea, vomiting, abdominal distention, and bowel sounds prior to and following administration. Assess patient for extrapyramidal effects Assess patient for signs of fluid retention during therapy. Monitor platelet count prior to and periodically during therapy. CBC should be monitored
Drowsiness, headache, epistaxis, nasal perforation, nasal ulcerations, pharyngolaryngeal pain, postnasal drip, bitter taste, cough. Ataxia, confusion, dizziness, drowsiness, headache, mental depression, psychosis, restlessness, diarrhea, abdominal pain, anorexia, exacerbation of colitis, druginduced hepatitis, nausea, vomiting, itching, rash, blood dyscrasias.
Injection site reactions, allergic reactions including anaphylaxis, risk of malignancy.
Altered taste, eructation, rash.
Ondansetron/Zofran
five ht3 antagonists; antiemetic
Abdominal pain, acid regurgitation, constipation, diarrhea, flatulence, nausea, vomiting. Dizziness, drowsiness, fatigue, headache, weakness itching, rash. Headache, dizziness, drowsiness, fatigue, weakness. Constipation, diarrhea, abdominal pain, dry mouth, increased liver enzymes. extrapyramidal reactions. Dizziness, headache, bone pain, insomnia, alopecia, nervousness, weakness, conjunctival hemorrhage, cough, chills, dyspnea, pleural effusions, atrial fibrillation,
Oprelvekin/ Neumega
colony stimulating factors interleukins thrombopoetic growth factors
159
Rev. 08/21/08
prior to and at regular intervals during therapy. Monitor electrolyte concentrations in patients receiving chronic diuretic therapy.
Orlistat/ Xenical
weight control agents lipase inhibitors
Orphenadrine/ Antiflex, Banflex, Flexoject, Flexon, Mio-Rel, Myolin, Myotrol, Norflex, Orfro, Orphenate
skeletal muscle relaxants (centrally acting) diphenhydramine analogues
Oseltamivir/ Tamiflu
antivirals neuramidase inhibitors
Oxacillin/ Bactocill
anti-infectives penicillinase resistant penicillins
Monitor patients for weight loss and adjust concurrent medications (antihypertensives, antidiabetics, lipid-lowering agents) as needed. Assess geriatric patients for anticholinergic adverse effects and sedation. Assess patient for pain, muscle stiffness, and range of motion; parkinsonian and extrapyramidal symptoms before and periodically throughout therapy. Monitor CBC and renal and hepatic function tests periodically during prolonged therapy. Monitor influenza symptoms. Additional supportive treatment may be indicated to treat symptoms. Assess patient for infection; signs and symptoms of anaphylaxis; vein for signs of irritation and phlebitis at beginning of and throughout therapy. Change IV site every 48 hr to prevent phlebitis.
edema, myalgia, palpitations, syncope, tachycardia, vasodilation, anorexia, constipation, diarrhea, dyspepsia, fever, mucositis, nausea, oral moniliasis, vomiting, rash, ecchymoses, infection, pain. Fecal urgency, flatus with discharge, increased defecation, oily evacuation, oily spotting, fecal incontinence. CNS excitation, confusion, dizziness, drowsiness, blurred vision, dry eyes, orthostatic hypotension, tachycardia, constipation, dry mouth, urinary retention.
Oxaliplatin/ Eloxatin
antineoplastics
Oxaprozin/ Daypro
antirheumatics nonsteroidal anti inflammatory agents
Assess for peripheral sensory neuropathy, signs of pulmonary fibrosis, and signs of anaphylaxis at beginning and periodically during therapy. Monitor WBC with differential, hemoglobin, platelet count, and blood chemistries before each oxaliplatin cycle Assess pain and range of motion prior to and periodically during therapy. Evaluate BUN, serum creatinine, CBC, and liver function tests periodically in patients receiving prolonged
Seizures, abnormal behavior, agitation, confusion, delirium, hallucinations, insomnia, nightmares, vertigo, bronchitis, nausea, vomiting. Seizures, diarrhea, epigastric distress, nausea, vomiting, eosinophilia, pseudomembranous colitis, interstitial nephritis, rash, urticaria, leucopenia, pain at IM site, phlebitis at IV site, allergic reactions including anaphylaxis and serum sickness, superinfection. Fatigue, chest pain, edema, pulmonary fibrosis, coughing, dyspnea, diarrhea, nausea, vomiting, abdominal pain, anorexia, gastroesophageal reflux, neutropenia, thrombocytopenia, anemia, back pain, neurotoxicity, anaphylaxis/anaphylactoid reactions, fever. GI bleeding, abdominal pain, diarrhea, dyspepsia, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, allergic reactions including anaphylaxis, angioneurotic
160
Rev. 08/21/08
therapy. Oxazepam/ Serax antianxiety agents sedative/hypnotics benzodiazepines Assess patient for anxiety and orientation, mood and behavior; level of sedation; regularly for continued need for treatment periodically throughout therapy. Monitor CBC and liver function tests periodically during prolonged therapy. Assess frequency, location, duration, and characteristics of seizure activity; CNS changes during therapy. Monitor ECG and serum electrolytes before and periodically during therapy. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Monitor voiding pattern and intake and output ratios, and assess abdomen for bladder distention prior to and periodically during therapy. Monitor voiding pattern and intake and output ratios, and assess abdomen for bladder distention prior to and periodically during therapy. Monitor voiding pattern and intake and output ratios, and assess abdomen for bladder distention prior to and periodically during therapy. Assess type, location, and intensity of pain prior to and 1 hr (peak) after administration. Assess blood pressure, pulse, and respirations; bowel function before and periodically during administration. Assess type, location, and intensity of pain prior to and 1 hr (peak) after administration. Assess blood pressure, pulse, and respirations; bowel function
Oxcarbazepine/Trilept al
anticonvulsants carbamazepine analogues
Oxiconazole/ Oxistat
antifungals (topical)
edema, dyspnea, edema, vasculitis, tremor. Dizziness, drowsiness, confusion, hangover, headache, respiratory depression, tachycardia, constipation, diarrhea, druginduced hepatitis, nausea, vomiting, weight gain, urinary problems, rashes, leucopenia, physical and psychological dependence, tolerance. Dizziness/vertigo, drowsiness/fatigue, headache, abnormal vision, diplopia, nystagmus, abdominal pain, nausea, vomiting, ataxia, gait disturbances, tremor, lymphadenopathy. Burning, itching, local hypersensitivity reactions, redness, stinging. Dizziness, drowsiness, constipation, dry mouth, nausea, urinary retention, agitation, confusion, hallucinations, headache, tachycardia, abdominal pain, diarrhea. Application site reactions, Dizziness, drowsiness, constipation, dry mouth, nausea, urinary retention, agitation, confusion, hallucinations, headache, tachycardia. Dizziness, fatigue, headache, dry mouth, constipation, application site reactions, pruritus.
Oxybutynin (oral)/ Ditropan, Ditropan XL
urinary tract antispasmodics anticholinergics
Oxybutynin (transdermal)/ Oxytrol
urinary tract antispasmodics anticholinergics
Oxybutynin transdermal gel/ Gelnique
urinary tract antispasmodics anticholinergics
Oxycodone/ Oxycontin, OxyFAST, OxyIR, Percolone, Roxicodone, Endocodone, M-Oxy
opioid analgesics opioid agonists opioid agonists nonopioid analgesic combinations
Oxycodone/ acetaminophen//Endo cet, Magnacet, Oxycet, Percocet, Roxicet, Roxilox, Tylox
opioid analgesics opioid agonists opioid agonists nonopioid analgesic combinations
Confusion, sedation, dysphoria, diplopia, miosis, respiratory depression, orthostatic hypotension, constipation, dry mouth, nausea, vomiting, urinary retention, flushing, sweating, physical and psychological dependence, tolerance. Confusion, sedation, dysphoria, diplopia, miosis, respiratory depression, orthostatic hypotension, constipation, dry mouth, nausea, vomiting, urinary
161
Rev. 08/21/08
before and periodically during administration. Oxycodone/aspirin// Endodan, Percodan opioid analgesics opioid agonists opioid agonists nonopioid analgesic combinations Assess type, location, and intensity of pain prior to and 1 hr (peak) after administration. Assess blood pressure, pulse, and respirations; bowel function before and periodically during administration. Assess type, location, and intensity of pain; BP, pulse, and respirations before and periodically during administration. Prolonged use may lead to physical and psychological dependence and tolerance. Bowel function routinely. Assess type, location, and intensity of pain prior to and 1 hr following IM and 1530 min (peak) following IV administration. Assess blood pressure, pulse, and respirations; bowel function before and periodically during administration.
Oxycodone Compound/ Percocet PAIN LEVEL 5, on a scale of 1-10
Opioid agonists, opioid agonists nonopioid analgesic combinations; opioid analgesics
retention, flushing, sweating, physical and psychological dependence, tolerance. Confusion, sedation, dysphoria, diplopia, miosis, respiratory depression, orthostatic hypotension, constipation, dry mouth, nausea, vomiting, urinary retention, flushing, sweating, physical and psychological dependence, tolerance. Confusion, sedation, constipation, respiratory depression
Oxymorphone/ Opana, Opana ER
opioid analgesics opioid agonists
Oxymorphone (oral)/ Opana, Opana ER
opioid analgesics opioid agonists
Assess type, location, and intensity of pain prior to and 1 hr (peak) after administration. Assess blood pressure, pulse, and respirations; bowel function before and periodically during administration. Fetal maturity, presentation, and pelvic adequacy should be assessed prior to administration of oxytocin for induction of labor. Assess character, frequency, and duration of uterine contractions; resting uterine tone; and fetal heart rate frequently throughout administration. Monitor maternal blood pressure and pulse frequently and fetal heart rate continuously throughout administration. Monitor maternal
Oxytocin/ Pitocin, Syntocinon
hormones oxytocics
Confusion, sedation, dysphoria, euphoria, hallucinations, unusual dreams, blurred vision, diplopia, miosis, respiratory depression, orthostatic hypotension, constipation, dry mouth, nausea, vomiting, urinary retention, flushing, sweating, physical and psychological dependence, tolerance. Drowsiness, confusion, dizziness, headache, respiratory depression, hypoxia, hypotension, tachycardia, nausea, abdominal distention, constipation, dry mouth, flatulence, ileus, vomiting, itching, sweating, fever. Fetalintracranial hemorrhage, asphyxia, hypoxia, arrhythmias, Maternalhypochloremia, hyponatremia, water intoxication, increased uterine motility, painful contractions, abruptio placentae, decreased uterine blood flow, hypersensitivity, coma, seizures, hypotension,
162
Rev. 08/21/08
electrolytes.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Paclitaxel/Abraxane, Onxol, Taxol
antineoplastics taxoids
Palifermin/ Kepivance
Paliperidone/ Invega
cytoprotective agents keratinocyte growth factors rDNA antipsychotics benzisoxazoles
Assess for development of peripheral neuropathy; arthralgia and myalgia; vital signs; cardiovascular status especially during first 3 hr of infusion; bone marrow depression; bleeding; intake and output, appetite, and nutritional intake; hypersensitivity reactions continuously during the first 30 min and frequently thereafter. Monitor CBC and differential prior to and periodically during therapy. Assess level of oral mucositis prior to and periodically during therapy.
ECG changes, hypotension, hypotension, bradycardia, abnormal liver function tests, diarrhea, mucositis, nausea, vomiting, alopecia, anemia, neutropenia, thrombocytopenia, arthralgia, myalgia, peripheral neuropathy, cough, dyspnea, injection site reactions, hypersensitivity reactions including anaphylaxis, Stevens-Johnson syndrome; toxic epidermal necrolysis. Skin toxicity, oral toxicity, amylase, lipase, arthralgia, dysesthesia.
Monitor patient's mental status, suicidal tendencies, weight and BMI, blood pressure (sitting, standing, lying down) and pulse, onset of extrapyramidal side effects, tardive dyskinesia, development of neuroleptic malignant syndrome before and periodically during therapy. Monitor fasting blood glucose and cholesterol levels before and periodically during therapy.
Palivizumab/ Synagis
antivirals monoclonal antibodies
Palonosetron/ Aloxi
antiemetics five ht3 antagonists
Pamidronate/ Aredia
bone resorption inhibitors biphosphonates hypocalcemics
Assess patient for signs of lower respiratory tract disease; and signs of anaphylactic reaction periodically during therapy. Assess patient for nausea, vomiting, abdominal distention, and bowel sounds prior to and following administration. Monitor intake/output ratios and blood pressure; signs of fluid overload; symptoms of hypercalcemia; evidence of hypocalcemia; IV site for
Neuroleptic malignant syndrome, drowsiness, headache, anxiety, confusion, dizziness, extrapyramidal disorders, fatigue, Parkinsonism, syncope, tardive dyskinesia, weakness, blurred vision, dyspnea, cough, palpitations, tachycardia, bradycardia, orthostatic hypotension, QTc interval, abdominal pain, dry mouth, dyspepsia, nausea, swollen tongue, hyperglycemia, back pain, dystonia, akithisia, dyskinesia, tremor, fever. Diarrhea, vomiting, erythema, induration, hypersensitivity reactions including anaphylactoid reactions and anaphylaxis. Dizziness, headache, constipation, diarrhea
Fatigue, conjunctivitis, blurred vision, eye pain/inflammation, rhinitis, rales, arrhythmias, hypertension, syncope, tachycardia, nausea,
163
Rev. 08/21/08
phlebitis; and bone pain frequently during therapy. Assess serum creatinine prior to each treatment. Monitor serum electrolytes, hemoglobin, and creatinine closely. Monitor CBC and platelet count during the first 2 wk of therapy
Pancrelipase/ Cotazym, Cotazym E.C.S. 8, Cotazym E.C.S. 20, Cotazym-S, Creon 10, Creon 25, Enzymase16, Ilozyme, Ku-Zyme HP, Lipram-PN16, LipramCR20, Lipram-UL12, Lipram-PN10, LipramUL18, Lipram-UL20, Pancoate, Pancrease, Pancrease MT 4, Pancrease MT 10, Pancrease MT 16, Pancrease MT 20, Pancrebarb MS-8, Protilase, Ultrase MT 12, Ultrase MT 20, Viokase, Zymase Pancuronium/ Pavulon
digestive agent pancreatic enzymes
Assess patient's nutritional status, stools for high fat content, and allergy to pork prior to and periodically throughout therapy.
abdominal pain, anorexia, constipation, vomiting, hypocalcemia, hypokalemia, hypomagnesemia, hypophosphatemia, fluid overload, nephrotoxicity, leukopenia, anemia, phlebitis at injection site, hypothyroidism, muscle stiffness, musculoskeletal pain, osteonecrosis. Nasal stuffiness, dyspnea, shortness of breath, wheezing, abdominal pain (high doses only), diarrhea, nausea, stomach cramps, oral irritation, hematuria, hives, rash, hyperuricemia, allergic reactions.
neuromuscular blocking agents nondepolarizing
Panitumumab/ Vectibix
antineoplastics monoclonal antibodies
Pantoprazole/ Protonix, Protonix I.V
antiulcer agents proton pump inhibitors
Assess respiratory status, ECG, heart rate, and blood pressure; and infusion site throughout therapy. Observe the patient for residual muscle weakness and respiratory distress during the recovery period. Assess for dermatologic toxicity; inflammatory or infectious sequelae; severe infusion reactions; pulmonary fibrosis; and diarrhea during therapy. Monitor electrolyte levels periodically during and for 8 wks after completion of therapy. Assess patient routinely for epigastric or abdominal pain and for frank or occult blood in stool, emesis, or gastric aspirate during therapy.
Bronchospasm, hypertension, tachycardia, excessive salivation, rash, allergic reactions including anaphylaxis.
Fatigue, ocular toxicity, eyelash growth, pulmonary fibrosis, cough, abdominal pain, constipation, diarrhea, nausea, vomiting, edema, stomatitis, dermatologic toxicity, paromychia, photosensitivity, infusion reactions, hypocalcemia, hypomagnesemia. Headache, abdominal pain, diarrhea, eructation, flatulence, hyperglycemia.
164
Rev. 08/21/08
Papaverine/ Pavabid, Pavagen TD
erectile dysfunction agents vasodilators
Paregoric/ camphorated tincture of opium
antidiarrheals opioid agonists
Paricalcitol/ Zemplar
vitamins fat soluble vitamins
Monitor blood pressure and pulse; ECG; and IV site for thrombosis before and periodically throughout course of therapy. Monitor liver function studies. Assess frequency and consistency of stools and bowel sounds; fluid and electrolyte balance and skin turgor for dehydration; respiratory rate; resolution of withdrawal symptoms before and throughout course of therapy. Assess for symptoms of vitamin deficiency; bone pain and weakness; and evidence of hypocalcemia prior to and periodically during therapy. Serum calcium, phosphorus, and intact PTH concentrations should be monitored at least every 2 wk for the first 3 mo of therapy or following any dosage adjustment, then monthly for 3 mo, then every 3 mo. Assess patient for infection and neurologic status at beginning of and throughout therapy. Prior to administering oral medication, assess patient's ability to swallow. Monitor appetite and nutritional intake; Weigh weekly; mental status; suicidal tendencies; frequency of obsessivecompulsive behaviors; frequency and severity of panic attacks and episodes of anxiety; manifestations of post-traumatic stress disorder; symptoms of premenstrual distress prior to and during therapy. Monitor CBC and differential periodically during therapy. Monitor appetite and nutritional intake; Weigh weekly; mental status; suicidal tendencies; frequency of obsessive-
Depression, dizziness, vertigo, sedation, dry throat, visual changes, apnea, arrhythmias, hypotension, dry mouth, sweating, thrombosis at injection site. Dizziness, drowsiness, miosis, respiratory depression, orthostatic hypotension, bradycardia, vasodilation, biliary tract spasm, constipation, urinary retention, histamine release.
Paromomycin/ Humatin
amebicide aminoglycosides
Dizziness, conjunctivitis, photophobia, rhinorrhea, arrhythmias, edema, hypertension, palpitations, anorexia, constipation, diarrhea, dry mouth, liver function test elevation, metallic taste, nausea, pancreatitis, polydipsia, albuminuria, azotemia, decreased libido, pruritus, rash, gout, hypercalcemia, hyperthermia, bone pain, metastatic calcification, muscle pain. Abdominal cramps, diarrhea, nausea, vomiting, hypersensitivity reactions.
Paroxetine hydrochloride/ Paxil, Paxil CR
antianxiety agents antidepressants selective serotonin reuptake inhibitors ssris
Paroxetine mesylate/ Pexeva
antianxiety agents antidepressants selective serotonin reuptake inhibitors ssris
Anxiety, dizziness, drowsiness, headache, insomnia, weakness, constipation, diarrhea, dry mouth, nausea, ejaculatory disturbance, sweating, back pain, myalgia, myopathy, paresthesia, tremor, chills, fever, agitation, amnesia, confusion, emotional lability, blurred vision, rhinitis, chest pain, edema, hypertension, palpitations, postural hypotension, tachycardia, vasodilation, dyspepsia, flatulence, pruritus, rash. Anxiety, dizziness, drowsiness, headache, insomnia, weakness, constipation, diarrhea, dry mouth, nausea, ejaculatory disturbance,
165
Rev. 08/21/08
compulsive behaviors; frequency and severity of panic attacks and episodes of anxiety; manifestations of post-traumatic stress disorder; symptoms of premenstrual distress prior to and during therapy. Monitor CBC and differential periodically during therapy. Pegaptanib/ Macugen ocular agents vascular endothelial growth factor antagonists Assess eye for signs of infection frequently during week following injection. Check perfusion of optic nerve head immediately after injection, use tonometry to measure intraocular pressure within 30 min following the injection, and biomicroscopy between 2 and 7 days following injection. Increases in intraocular pressure have been seen within 30 min of injection. Monitor for hypersensitivity reaction; development of bone marrow depression; fever, sore throat, and signs of infection; platelet count; bleeding; increased fatigue, dyspnea, and orthostatic hypotension; signs of pancreatitis; nausea, vomiting, and appetite; and weigh patient weekly during therapy. Monitor CBC prior to and periodically throughout therapy. Monitor serum amylase frequently to detect pancreatitis. Monitor blood glucose.
sweating, back pain, myalgia, myopathy, paresthesia, tremor, chills, fever, agitation, amnesia, confusion, emotional lability, blurred vision, rhinitis, chest pain, edema, hypertension, palpitations, postural hypotension, tachycardia, vasodilation, dyspepsia, flatulence, pruritus, rash. Cataract, blurred vision, conjunctival bleeding, irritation/pain, intraocular pressure, ocular inflammation, infection (rare), retinal detachment (rare), traumatic cataract formation (rare), anaphylaxis, angioedema.
Pegaspargase/ Oncaspar, PEG-l-asparaginase
antineoplastics enzymes
Pegfilgrastim/ Neulasta
colony stimulating factors
Peginterferon alfa-2a/ Pegasys
immune modifiers interferons
Assess patient for bone pain and signs of ARDS throughout therapy. Obtain CBC and platelet count before chemotherapy. Monitor hematocrit and platelet count regularly. Assess patient for signs of neuropsychiatric disorders; signs of infection; cardiovascular disorders; pulmonary status; signs of hypersensitivity reactions;
Seizures, headache, chills, malaise, pancreatitis, abdominal pain, abnormal liver function tests, nausea, anorexia, diarrhea, lip edema, vomiting, jaundice, hyperglycemia, peripheral edema, fibrinogen, disseminated intravascular coagulation, hemolytic anemia, increased thromboplastin, leukopenia, pancytopenia, arthralgia, thrombocytopenia, injection site hypersensitivity, injection site pain, thrombosis, myalgia, pain in extremities, paresthesia, hypersensitivity reactions, night sweats. Adult respiratory distress syndrome (ARDS), splenic rupture, sickle cell crisis, leukocytosis, medullary bone pain, allergic reaction including anaphylaxis. Neuropsychiatric reactions, skin reactions (including Stevens-Johnson syndrome and exfoliative dermatitis), decreased vision, optic neuritis, papilledema, retinal
166
Rev. 08/21/08
Peginterferon alfa-2B/ Pegintron
immune modifiers interferons
Pegvisomant/ Somavert
hormones growth hormones
Pemetrexed/ Alimta
antineoplastics antimetabolites folate antagonists
signs of colitis; pre-existing diabetic or hypertensive retinopathy; and skin reactions periodically during therapy. Monitor CBC with platelet count prior to, 2 wks and 4 wks after initiation of therapy. May cause hemolytic anemia. Monitor liver function tests, uric acid and triglyceride levels every 4 wks during therapy. Monitor thyroid stimulating hormone (TSH) every 12 wks during therapy. Monitor renal function periodically during therapy. Assess patient for development of flu-like syndrome; mental status; cardiac status; signs and symptoms of ulcerative colitis; signs of pancreatitis; signs and symptoms of hypersensitivity reactions periodically during therapy. Monitor serum HCV RNA levels after 24 wks of treatment. Monitor for CBC and differential; and liver function tests prior to and periodically during therapy. Assess patient for signs and symptoms of acromegaly; signs and symptoms or hepatitis or other liver injury periodically during therapy. Monitor serum IGF-1 levels 46 wk after therapy is initiated or any dose adjustments are made and at least every 6 mo after IGF-1 levels have normalized. Monitor serum glucose carefully in patients with insulin-dependent diabetes. Measure liver tests at baseline. Monitor for rash; hematologic and GI; bone marrow depression; bleeding; and neurotoxicity during therapy. Monitor CBC and platelet counts for nadir and recovery, before each dose and on days 8 and 15 of each cycle and chemistry
hemorrhage/cotton wool spots, retinal vascular thrombosis, retinopathy, MI, chest pain, hypertension, supraventricular arrhythmias, dyspnea, interstitial pneumonitis, pulmonary infiltrates, colitis, pancreatitis, hyperglycemia, hypoglycemia, hyperthyroidism, hypothyroidism, bone marrow depression, development/exacerbation of autoimmune disorders, infections.
Anxiety, depression, dizziness, fatigue, headache, insomnia, pharyngitis, pulmonary infiltrates/pneumonitis, colitis, pancreatitis, abdominal pain, anorexia, diarrhea, nausea, alopecia, neutropenia, flu-like syndrome, musculoskeletal pain, thrombocytopenia, injection site pain/reactions, aggressive behavior, homicidal ideation, dry skin, flushing, allergic reactions including anaphylaxis, fever, rigors. Hypertension, peripheral edema, LFTs, back pain, growth hormone deficiency, glucose tolerance, lipohypertrophy.
Pharyngitis, chest pain, constipation, nausea, stomatitis, vomiting, anorexia, diarrhea, esophagitis, mouth pain, desquamation, rash, anemia, leukopenia, thrombocytopenia, neuropathy, fever, infection.
167
Rev. 08/21/08
Penbutolol/ Levatol
antihypertensives beta blockers
Penciclovir/ Denavir Penicillamine/ Cuprimine, Depen
antivirals (topical) antidotes antirheumatics (DMARD) antiurolithics chelating agents
for renal and liver functions periodically. Monitor blood pressure and pulse frequently; intake and output ratios and daily weight; orthostatic hypotension; and evidence of fluid overload during dosage adjustment period and periodically throughout therapy. Assess lesions prior to and daily during therapy. Monitor intake and output and daily weight; edema; allergic reactions; pain and range of motion periodically during therapy. Arthritis: Monitor 24-hr urinary protein levels every 12 wk in patients with moderate proteinuria.
Penicillin G/ Pfizerpen
anti-infectives penicillins
Penicillin V/ BeepenVK, Pen-Vee K, Veetids
anti-infectives penicillins
Assess for infection; reactions to penicillins, cephalosporins, or other beta-lactam antibiotics; and signs and symptoms of anaphylaxis at beginning of and during therapy. Monitor serum sodium concentrations in patient with hypertension or CHF. Assess for infection; reactions to penicillins, cephalosporins, or other beta-lactam antibiotics; and signs and symptoms of anaphylaxis at beginning of and during therapy.
Pentamidine/ NebuPent, Pentam 300
antiprotozoals
Assess patient for infection; signs of hypoglycemia and hyperglycemia; pulse and ECG and monitor respiratory status at beginning of and
Fatigue, weakness, arrhythmias, bradycardia, CHF, pulmonary edema, erectile dysfunction, anxiety, depression, dizziness, drowsiness, insomnia, itching, rashes, arthralgia, back pain, muscle cramps, drug-induced lupus syndrome. Headache, application site reactions. Blurred vision, eye pain, coughing, shortness of breath, wheezing, altered taste, anorexia, cholestatic jaundice, diarrhea, drug-induced pancreatitis, dyspepsia, epigastric pain, hepatic dysfunction, oral ulceration, vomiting, proteinuria, pemphigus, ecchymoses, hives, itching, rashes, wrinkling, aplastic anemia, anemia, nausea, eosinophilia, leukopenia, allergic reactions, fever, thrombocytopenia, thrombocytosis, arthralgia, migratory polyarthritis, myasthenia gravis syndrome, Goodpastures syndrome, systemic lupus erythematosuslike syndrome. Seizures, diarrhea, epigastric distress, nausea, vomiting, eosinophilia, pseudomembranous colitis, interstitial nephritis, rash, urticaria, leucopenia, allergic reactions including anaphylaxis and serum sickness, superinfection, pain at IM site, phlebitis at IV site. Seizures, diarrhea, epigastric distress, nausea, vomiting, eosinophilia, pseudomembranous colitis, interstitial nephritis, rash, urticaria, leucopenia, allergic reactions including anaphylaxis and serum sickness, superinfection. Anxiety, headache, confusion, dizziness, hallucinations, arrhythmias, hypotension, pancreatitis, abdominal pain, anorexia, drug-induced
168
Rev. 08/21/08
throughout therapy. Monitor blood pressure frequently during and following IM or IV administration. Monitor blood glucose concentrations prior to, daily during, and for several months following therapy. Monitor BUN and serum creatinine prior to and daily during therapy. Monitor CBC and platelet count; serum calcium and magnesium concentrations prior to and every 3 days during therapy.
hepatitis, nausea, unpleasant metallic taste, vomiting, pallor, rash, nephrotoxicity, hypoglycemia, anemia, hyperglycemia, chills, hyperkalemia, fever, hypocalcemia, leukopenia, thrombocytopenia, allergic reactions including anaphylaxis and stevensjohnson syndrome. Inhalationburning in throat, bronchospasm, cough. IVphlebitis, pruritus, urticaria at IV site, IMsterile abscesses at IM sites. Dizziness, euphoria, hallucinations, headache, sedation, dysphoria, blurred vision, diplopia, miosis, respiratory depression, hypertension, hypotension, palpitations, nausea, constipation, dry mouth, urinary retention, sweating, severe tissue damage at subcut sites, physical and psychological dependence, tolerance. Headache, lightheadedness, chest pain, diarrhea, metallic taste, nausea, depletion of zinc, manganese, magnesium (prolonged treatment), injection site reactions, cough, wheezing (inhalation only), dermatitis, allergic reactions. Lightheadedness, depletion of manganese, magnesium, injection site reactions, cough, wheezing (inhalation only).
Pentazocine/ Talwin, Talwin NX
opioid analgesics opioid agonists antagonists
Assess type, location, and intensity of pain prior to and 1 hr following PO, subcut, or IM and 1530 min (peak) following IV administration. Assess blood pressure, pulse, and respirations; analgesic history; falls risk; and CNS effects before and periodically during administration.
Pentetate calcium trisodium/ Ca-DTPA
radiation protectants chelating agents
Pentetate zinc trisodium / Zn-DTPA
radiation protectants chelating agents
Pentobarbital/ Nembutal
anticonvulsants sedative/hypnotics barbiturates
Obtain information regarding contamination with plutonium, americium, or curium. Obtain baseline CBC with differential, BUN, serum chemistries and electrolytes, urinalysis, blood and urine radioassays. Obtain information regarding contamination with plutonium, americium, or curium. Obtain baseline CBC with differential, BUN, serum chemistries and electrolytes, urinalysis, blood and urine radioassays. Monitor respiratory status, pulse, and blood pressure; psychological or physical dependence; pain; sleep patterns; intracranial pressure and level of consciousness; location, duration, and characteristics of seizure activity at beginning and throughout therapy.
Drowsiness, hangover, lethargy, laryngospasm, delirium, excitation, mental depression, vertigo, rashes, respiratory depression, bronchospasm, urticaria, hypotension, constipation, diarrhea, nausea, vomiting, hypersensitivity reactions including angioedema and serum sickness.
169
Rev. 08/21/08
Pentostatin/ Nipent
antineoplastics enzyme inhibitors
Monitor patient for CNS toxicity; intake and output and renal function; allergic reactions; bone marrow depression; and bleeding at beginning and throughout therapy. Before initiating therapy, assess renal function by measuring serum creatinine or CCr. Serum creatinine; CBC with differential and platelet count; serum uric acid should be measured before each dose. Monitor peripheral blood for hairy cells periodically throughout therapy.
Pentoxifylline/ Trental
blood viscosity reducing agent
Assess patient for intermittent claudication prior to and periodically throughout therapy. Monitor blood pressure periodically in patients on concurrent antihypertensive therapy.
Perindopril/Aceon
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor renal function.
Permethrin/Acticin, Elimite, Nix
Pediculocides
Perphenazine/ Trilafon
antiemetics antipsychotics (conventional) phenothiazines
Assess scalp for presence of lice and their ova (nits) prior to and 1 wk after application of permethrin. Assess skin for scabies prior to and following therapy. Assess patient's mental status; fasting blood glucose, cholesterol level, weight, and BMI; positive (hallucinations, delusions, agitation) and negative (social withdrawal) symptoms of schizophrenia; blood pressure (sitting, standing, lying), ECG, pulse, and respiratory rate; fluid intake and bowel function; onset of akathisia and extrapyramidal side effects; tardive dyskinesia; development of neuroleptic
CNS toxicity, fatigue, skin rash, headache, weakness, epistaxis, flatulence, dry skin, keratoconjunctivitis, pharyngitis, rhinitis, itching, sinusitis, vision changes, pulmonary toxicity, fever, bronchitis, dyspnea, flu-like syndrome, pneumonia, cough, pulmonary edema, MI, angina pectoris, weight loss, diarrhea, arrhythmias, leukopenia, constipation, thrombophlebitis, anorexia, hepatotoxicity, nausea, vomiting, abdominal pain, stomatitis, renal toxicity, anemia, thrombocytopenia, arthralgia, myalgia, allergic reactions including anaphylaxis. Agitation, dizziness, flatus, drowsiness, headache, insomnia, nervousness, blurred vision, dyspnea, angina, arrhythmias, edema, flushing, diarrhea, hypotension, abdominal discomfort, dyspepsia, nausea, vomiting, tremor. Dizziness, headache, weakness, cough, hypotension, diarrhea, dyspepsia, impaired renal function, rashes, hyperkalemia, back pain, angioedema. Burning, itching, rash, redness, stinging, swelling, numbness, tingling.
Neuroleptic malignant syndrome, extrapyramidal reactions, sedation, tardive dyskinesia, blurred vision, dry eyes, lens opacities, hypotension, tachycardia, constipation, dry mouth, anorexia, ileus, weight gain, discoloration of urine, urinary retention, photosensitivity, pigment changes, rashes, galactorrhea, amenorrhea, agranulocytosis, leucopenia, hyperthermia, allergic reactions.
170
Rev. 08/21/08
Phenazopyridine/ AzoStandard, Baridium, Geridium, Prodium, Pyridiate, Pyridium, Pyridium Plus, Urodine, Urogesic, UTI Relief Phenelzine/ Nardil
nonopioid analgesics urinary tract analgesics
antidepressants monamine oxidase inhibitors
malignant syndrome; nausea and vomiting; intake and output initially and periodically throughout therapy. Assess patient for urgency, frequency, and pain on urination prior to and throughout therapy. Renal function should be monitored periodically during course of therapy. Assess mental status, mood changes, and anxiety level, suicidal tendencies; blood pressure and pulse rate; intake and output ratios and daily weight; peripheral edema and urinary retention before and frequently during therapy. Assess hepatic function periodically during prolonged or high-dose therapy. Monitor serum glucose closely in diabetic patients.
Headache, vertigo, hepatotoxicity, nausea, brightorange urine, renal failure, rash, hemolytic anemia, methemoglobinemia.
Phenobarbital/ Luminal, Solfoton
anticonvulsants sedative/hypnotics barbiturates
Monitor respiratory status, pulse, and blood pressure; psychological or physical dependence; location, duration, and characteristics of seizure activity; level of consciousness and anxiety; postoperative patients for pain with a pain scale before and frequently during therapy.
Phentermine/ Adipex-P, Banobese, Fastin, Ionamin, ObiNix, OBY-CAP, Phentercot, Phentride, T-Diet, Teramine, Zantryl
weight control agents appetite suppressants
Monitor patients for weight loss and adjust concurrent medications (antihypertensives, antidiabetics, lipid-lowering agents) as needed.
Phentolamine/Regitine
agents pheochromocytoma alpha adrenergic blockers
Monitor blood pressure, pulse, and ECG every 2 min until stable during IV administration.
Seizures, dizziness, drowsiness, fatigue, headache, hyperreflexia, insomnia, tremor, twitching, weakness, euphoria, paresthesia, restlessness, blurred vision, glaucoma, nystagmus, hypertensive crisis, edema, orthostatic hypotension, constipation, dry mouth, abdominal pain, liver function test elevation, nausea, vomiting, sexual dysfunction, urinary retention, pruritis, rashes, hypernatremia, weight gain. Hangover, delirium, depression, drowsiness, excitation, lethargy, vertigo, respiratory depression, constipation, diarrhea, nausea, vomiting, photosensitivity, rashes, urticaria, phlebitis at IV site, arthralgia, myalgia, neuralgia, hypersensitivity reactions including angioedema and serum sickness, physical dependence, psychological dependence. IVlaryngospasm, bronchospasm, hypotension. CNS stimulation, confusion, dizziness, dysphoria, euphoria, headache, insomnia, mental depression, restlessness, blurred vision, hypertension, palpitations, tachycardia, constipation, diarrhea, dry mouth, nausea, unpleasant taste, vomiting, changes in libido, erectile dysfunction. Cerebrovascular spasm, dizziness, weakness, nasal stuffiness, hypotension, MI, angina, arrhythmias, tachycardia, abdominal pain,
171
Rev. 08/21/08
Phenylephrine/ NeoSynephrine
vasopressors adrenergics
Monitor blood pressure every 23 min until stabilized and every 5 min thereafter during IV administration. Monitor ECG continuously for arrhythmias during IV administration. Assess IV site frequently throughout infusion.
Phenytoin/ Dilantin, Phenytek
antiarrhythmics (group IB) anticonvulsants hydantoins
Assess oral hygiene; hypersensitivity syndrome; location, duration, frequency, and characteristics of seizure activity; EEG; blood pressure, ECG, and respiratory function; ECG at beginning of and periodically throughout therapy. Monitor CBC, serum calcium, albumin, and hepatic function tests; serum folate concentrations prior to and monthly for the first several months, then periodically throughout therapy.
Phosphate/biphosphat e// Fleet Enema, Fleet Phospho-Soda, Visicol
laxatives (saline)
Physostigmine/ Antilirium
antidotes cholinergics anticholinesterases
Phytonadione/ AquaMEPHYTON, Mephyton, vitamin K
antidotes vitamins fat soluble vitamins
Assess patient for fever, abdominal distention, presence of bowel sounds, and usual pattern of bowel function; color, consistency, and amount of stool produced; underlying cardiovascular disease, renal disease, bowel perforation, misuse or overdose at beginning of and throughout therapy. Monitor pulse, respiratory rate, and blood pressure; neurologic status frequently throughout parenteral administration. Monitor ECG during IV administration. Monitor for frank and occult bleeding; pulse and blood pressure; side effects and adverse reactions at beginning of and throughout therapy. Monitor prothrombin time (PT) prior
diarrhea, nausea, vomiting, aggravation of peptic ulcer, flushing. Anxiety, dizziness, headache, insomnia, nervousness, restlessness, trembling, weakness, dyspnea, respiratory distress, arrhythmias, bradycardia, chest pain, hypertension, tachycardia, vasoconstriction, blanching, pallor, piloerection, sweating, phlebitis, sloughing at IV sites, tremor. Ataxia, agitation, confusion, dizziness, drowsiness, dysarthria, dyskinesia, extrapyramidal syndrome, headache, insomnia, weakness, diplopia, fever, nystagmus, hypotension, tachycardia, gingival hyperplasia, nausea, constipation, drug-induced hepatitis, vomiting, hypertrichosis, rash, pruritus, agranulocytosis, aplastic anemia, leukopenia, megaloblastic anemia, thrombocytopenia, osteomalacia, allergic reactions including stevensjohnson syndrome. Arrhythmias, cramping, nausea, colonic aphtous ulcerations, hyperphosphatemia, hypocalcemia, hypokalemia, sodium retention. Visicoldizziness, headache, abdominal bloating, abdominal pain, vomiting.
Seizures, restlessness, dizziness, bronchospasm, bradycardia, hypotension, abdominal cramps, diarrhea, nausea, vomiting, excess salivation, rash. Gastric upset, unusual taste, flushing, rash, urticaria, hemolytic anemia, erythema, pain at injection site, swelling, allergic reactions, kernicterus, hyperbilirubinemia.
172
Rev. 08/21/08
Pilocarpine (oral)/Salagen
cholinergics
to and throughout vitamin K therapy to determine response to and need for further therapy. Assess oral mucosa for dryness and ulceration periodically during therapy. Assess skin lesions prior to and periodically during therapy. Discontinue therapy after signs and symptoms of atopic dermatitis have resolved. Resume treatment at the first signs and symptoms of recurrence. Assess patient for frequency of tics; positive (hallucinations, delusions, agitation) and negative (social withdrawal) symptoms of psychotic disorder; weight and BMI; blood pressure (sitting, standing, lying) and ECG; intake and output ratios and daily weight; fluid intake and bowel function; onset of akathisia; extrapyramidal side effects; tardive dyskinesia; development of neuroleptic malignant syndrome prior to and periodically during therapy. Obtain EKG and serum potassium levels; and fasting blood glucose and cholesterol levels initially and throughout therapy. Monitor blood pressure and pulse; orthostatic hypotension; intake and output ratios and daily weight; evidence of fluid overload; frequency and characteristics of anginal attacks at beginning of and periodically throughout therapy. Observe patient taking concurrent insulin for signs and symptoms of hypoglycemic reactions. Monitor serum glucose and Hb A1c periodically during therapy to evaluate effectiveness.
Pimecrolimus/ Elidel
immunosuppressan ts (topical)
Nausea, vomiting, flushing, sweating, edema, chills, hypertension, tachycardia, amblyopia, epistaxis. Burning, increased risk of lymphoma/skin cancer.
Pimozide/ Orap
antipsychotics (conventional)
Neuroleptic malignant syndrome, mood/behavior effects, weakness, drowsiness, blurred vision, dry eyes, arrhythmias, hypotension, constipation, dry mouth, decreased appetite, nausea, vomiting, weight loss, decreased libido, erectile dysfunction, skin discoloration, galactorrhea (women), blood dyscrasias, akathisia, parkinsonism, dystonic reactions, tardive dyskinesia, akinesia.
Pindolol/ Visken
antihypertensives beta blockers
Pioglitazone/Actos
antidiabetics (oral) thiazolidinediones
Fatigue, weakness, anxiety, arrhythmias, bradycardia, CHF, pulmonary edema, erectile dysfunction, dry eyes, bronchospasm, wheezing, arthralgia, back pain, muscle cramps, drug-induced lupus syndrome, depression, dizziness, nasal stuffiness, itching, rashes. Edema, hepatitis, liver enzymes, anemia, fractures (arm, hand, foot) in female patients.
173
Rev. 08/21/08
Pipecuronium/ Arduan
neuromuscular blocking agents nondepolarizing
Piperacillin/tazobacta m// Zosyn
anti-infectives extended spectrum penicillins
Assess respiratory status, ECG, heart rate, and blood pressure; and infusion site throughout therapy. Observe the patient for residual muscle weakness and respiratory distress during the recovery period. Assess patient for infection; previous use of and reactions to penicillins or cephalosporins; and signs and symptoms of anaphylaxis at beginning of and during therapy. Evaluate renal and hepatic function, CBC, serum potassium, and bleeding times prior to and routinely during therapy. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; and paradoxical bronchospasm before initiating therapy and periodically throughout. Observe patient for drug tolerance and rebound bronchospasm. Monitor for rhinitis, asthma, and urticaria; hypersensitivity reactions at beginning of and during therapy. Assess pain and range of motion prior to and 12 hr following administration. Monitor liver function tests periodically during therapy. Monitor BUN, serum creatinine, and electrolytes periodically during therapy. Monitor vital signs, CVP, pulmonary capillary wedge pressure (PCWP), and intake and output; signs of vascular overload; increased bleeding before and frequently throughout therapy. Monitor hemoglobin, hematocrit, serum protein, and electrolytes throughout therapy.
Bronchospasm, arrhythmias, hypotension, hypertension, tachycardia, excessive salivation, rash, skin flushing, allergic reactions including anaphylaxis.
Pirbuterol/ Maxair
bronchodilators adrenergics
Seizures, dizziness, pseudomembranous colitis, diarrhea, constipation, druginduced hepatitis, nausea, vomiting, interstitial nephritis, rashes, urticaria, bleeding, leukopenia, neutropenia, thrombocytopenia, pain, phlebitis at IV site, hypersensitivity reactions including anaphylaxis and serum sickness, fever, superinfection. Nervousness, restlessness, tremor, headache, insomnia, paradoxical bronchospasm, angina, arrhythmias, hypertension, tachycardia, nausea, vomiting, hyperglycemia.
Piroxicam/ Feldene
antirheumatics nonsteroidal anti inflammatory agents
Plasma protein fraction/ Plasmanate, PlasmaPlex, Plasmatein, Protenate
volume expanders blood products
Drowsiness, headache, tinnitus, edema, drug-induced hepatitis, GI bleeding, discomfort, dyspepsia, nausea, vomiting, anorexia, constipation, diarrhea, flatulence, renal failure, exfoliative dermatitis, stevensjohnson syndrome, toxic epidermal necrolysis, rashes, blood dyscrasias, prolonged bleeding time, allergic reactions including anaphylaxis. Headache, hypotension, tachycardia, vascular overload, excess salivation, nausea, vomiting, erythema, urticaria, back pain, infection, chills, fever, flushing.
174
Rev. 08/21/08
Plerixafor/ Mozobil
hematopoietic stem cell mobilizers
Assess for splenic enlargement and potential rupture (left upper abdominal pain and/or scapular or shoulder pain) periodically during therapy. Monitor WBC and platelets during therapy. Assess for fever, nausea, vomiting, abdominal distention, and pain. Inquire about patient's usual diet, fluid intake, activity level, and bowel function. Monitor for color, consistency, and amount of stool produced. Monitor for signs of dehydration. Assess patient for abdominal distention, presence of bowel sounds, and usual pattern of bowel function, color, consistency, and amount of stool produced Assess patient for abdominal distention, presence of bowel sounds, and usual pattern of bowel function; and color, consistency, and amount of stool produced during therapy. Monitor semiconscious or unconscious patients closely for regurgitation when administering via NG tube. Assess patient for substernal chest pain after therapy. Before each new course of therapy, the patient should be examined for either bronchoesophageal or tracheoesophageal fistula.
Polycarbophil/ Bulk Forming Fiber Laxative, Equalactin, FiberCon, Fiber-Lax, Konsyl Fiber, Mitrolan
antidiarrheals laxatives bulk forming agents
Dizziness, fatigue, headache, insomnia, splenic rupture, diarrhea, nausea, vomiting, abdominal distention/pain, dry mouth, constipation, dyspepsia, erythema, sweating, leukemia/tumor cell mobilization, injection site reactions, oral hypoesthesia. Abdominal fullness.
Polyethylene glycol/ Miralax
Osmotic, laxative
abdominal bloating, cramping, flatulence, nausea
Polyethylene glycol/ electrolyte// Colovage, Colyte, GoLYTELY, NuLytely, OCL, Peglyte, TriLyte
Osmotic, laxative
Abdominal fullness, diarrhea, bloating, cramps, nausea, vomiting, allergic reactions
Porfimer/ Photofrin
antineoplastics photosensitizers
Posaconazole/ Noxafil
antifungals triazoles
Potassium acetate
mineral electrolyte replacements supplements
Assess for signs and symptoms of fungal infection. Monitor liver function tests prior to and periodically during therapy. Assess for signs and symptoms of hypokalemia and hyperkalemia; pulse, blood pressure, and ECG periodically during IV therapy. Monitor serum potassium before and
Insomnia, dyspnea, chest pain, mucositis reaction, pharyngitis, heart failure, pleural effusion, anemia, pneumonia, respiratory insufficiency, abdominal pain, constipation, nausea, vomiting, photosensitivity, fever, pain, esophageal rupture, GI bleeding. Hepatocellular damage, diarrhea, nausea, vomiting, adrenal insufficiency, allergic reactions. Confusion, restlessness, weakness, arrhythmias, ECG changes, irritation at IV site, paralysis, paresthesia.
175
Rev. 08/21/08
Potassium acid phosphate/ K-Phos Original
antiurolithics
Potassium and sodium phosphates/ K-Phos M.F, K-Phos Neutral, KPhos No. 2, Neutra-Phos, UroKP Neutral
antiurolithics mineral electrolyte replacements supplements
Potassium bicarbonate/ K+Care ET, KElectrolyte, K-Ide, Klor-Con/EF, KLyte, K-Vescent
mineral electrolyte replacements supplements
Potassium bicarbonate/ potassium chloride// K-Dur Lyte/Cl
mineral electrolyte replacements supplements
Potassium bicarbonate/ potassium citrate// Effer-K, K-Lyte DS
mineral electrolyte replacements supplements
periodically during therapy. Monitor renal function, serum bicarbonate, and pH. Monitor intake and output ratios and daily weight. Report significant discrepancies. Monitor serum phosphate, potassium, and calcium levels prior to and periodically throughout therapy. Monitor renal function prior to and periodically throughout course of therapy. Monitor urinary pH when using as a urinary acidifier. Assess patient for signs and symptoms of hypokalemia and hypophosphatemia throughout therapy. Monitor intake and output ratios and daily weight. Monitor serum phosphate, potassium, sodium, and calcium levels prior to and periodically throughout therapy. Monitor renal function studies prior to and periodically throughout therapy. Monitor urinary pH in patients receiving potassium and sodium phosphate as a urinary acidifier. Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH. Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH. Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH.
Confusion, listlessness, weakness, arrhythmias, cardiac arrest, ECG changes, hypotension, abdominal pain, diarrhea, flatulence, nausea, vomiting, hyperkalemia, hyperphosphatemia, hypocalcemia, hypomagnesemia, muscle cramps, tremors, flaccid paralysis, heaviness of legs, paresthesias. Hyperkalemia arrhythmias, bradycardia, ECG changes. Confusion, dizziness, headache, weakness, arrhythmias, cardiac arrest, bradycardia, ECG changes, edema, diarrhea, abdominal pain, nausea, vomiting, hyperkalemia, hypernatremia, hyperphosphatemia, hypocalcemia, hypomagnesemia, muscle cramps, flaccid paralysis, heaviness of legs, paresthesias, tremors.
Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions. Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions. Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions.
176
Rev. 08/21/08
Potassium chloride
mineral electrolyte replacements supplements
Potassium chloride (oral)/ Cena-K, Gen-K, K+ Care, K+ 10, Kaochlor, Kaochlor S-F, KaonCl, Kay Ciel, KCl, K-Dur, KLease, K-Lor, KlorCon, Klorvess Liquid, Klotrix, K-Lyte/Cl Powder, KMed, K-Norm, K-Sol, K-Tab, Micro-K, Micro-K ExtenCaps, Micro-LS, Potasalan, Roychlor, Rum-K, Slow-K, Ten-K Potassium chloride/ Potassium bicarbonate/ Potassium citrate// Kaochlor Eff
mineral electrolyte replacements supplements
Assess for signs and symptoms of hypokalemia and hyperkalemia; pulse, blood pressure, and ECG periodically during IV therapy. Monitor serum potassium before and periodically during therapy. Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH.
Confusion, restlessness, weakness, arrhythmias, ECG changes, irritation at IV site, paralysis, paresthesia.
Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions.
mineral electrolyte replacements supplements
Potassium gluconate/ Kaon, Kaylixir, K-G Elixir
mineral electrolyte replacements supplements
Potassium gluconate/ Potassium chloride// Kolyum
mineral electrolyte replacements supplements
Potassium iodide/ Pima, SSKI, ThyroSafe, ThyroShield
antithyroid agents iodine containing agents
Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH. Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH. Assess for signs and symptoms of hypokalemia and hyperkalemia during therapy. Monitor serum potassium before and periodically during therapy. Monitor renal function, serum bicarbonate, and pH. Assess for signs and symptoms of iodism; symptoms of hyperthyroidism; and hypersensitivity reaction before and periodically
Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions. Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions. Confusion, restlessness, weakness, arrhythmias, ECG changes, abdominal pain, diarrhea, flatulence, nausea, vomiting, paralysis, paresthesia. Tablets, capsules onlyGI ulceration, stenotic lesions. Confusion, weakness, GI bleeding, diarrhea, nausea, vomiting, acneiform eruptions, hypothyroidism, goiter, hyperthyroidism, hyperkalemia, tingling, joint
177
Rev. 08/21/08
Potassium phosphate/ Neutra-Phos-K
mineral electrolyte replacements supplements
throughout therapy. Monitor thyroid function before and periodically during therapy. Assess patient for signs and symptoms of hypokalemia and hypophosphatemia; pulse, blood pressure, and ECG; intake and output ratios and daily weight prior to and periodically throughout IV therapy. Monitor serum phosphate, potassium, and calcium levels; and renal function prior to and periodically throughout therapy. Monitor neuromuscular status; respirations, pulse, and blood pressure before and periodically throughout therapy. Determine type of insecticide and time of patient's exposure. Therapy should begin as soon as possible within 24 hr. Assess patient for confusion or hallucinations; ECG and blood pressure; drowsiness and sleep attacks; signs and symptoms of Parkinson's disease; sleep patterns and frequency of restless leg disturbances before and periodically throughout therapy.
pain, hypersensitivity, iodism.
Pralidoxime/ Protopam
antidotes cholinesterase reactivators
Pramipexole/ Mirapex
antiparkinson agents dopamine agonists
Pramlintide/ Symlin
antidiabetics hormones
Pramoxine/Fleet Relief, ProctoFoam NS, Tronolane, Tronothane
anesthetics topical local
Assess hemoglobin A1c, recent blood glucose monitoring data, history of insulin-induced hypoglycemia, current insulin regimen, and body weight prior to initiation of therapy. Assess for signs and symptoms of hypoglycemia, occurs within 3 hr of injection. Monitor blood glucose frequently, including pre- and postmeals and at bedtime. Assess type, location, and intensity of pain before and a few minutes after administration of anesthetic. Assess integrity of involved skin and mucous
Confusion, listlessness, weakness, arrhythmias, cardiac arrest, ECG changes, hypotension, bradycardia, abdominal pain, diarrhea, flatulence, nausea, vomiting, hyperkalemia, hyperphosphatemia, hypocalcemia, hypomagnesemia, irritation at IV site, phlebitis, muscle cramps, tremors, flaccid paralysis, heaviness of legs, paresthesias. Dizziness, drowsiness, headache, blurred vision, diplopia, rash, impaired accommodation, nausea, laryngospasm, muscle weakness, hyperventilation, tachycardia, pain at injection site, muscle rigidity, neuromuscular blockade. Sleep attacks, amnesia, dizziness, drowsiness, hallucinations, weakness, confusion, dyskinesia, extrapyramidal syndrome, headache, insomnia, postural hypotension, constipation, dry mouth, dyspepsia, nausea, tooth disease, urinary frequency, leg cramps, hypertonia, unsteadiness/falling. Dizziness, fatigue, headache, cough, nausea, abdominal pain, anorexia, vomiting, hypoglycemia, local allergy, arthralgia, injection site reactions, systemic allergic reactions.
Mucosal usedecreased or absent gag reflex. Topical useburning, edema, irritation, stinging, tenderness, urticaria. Allergic reactions including
178
Rev. 08/21/08
Pravastatin/ Pravachol
lipid-lowering agents hmg coa reductase inhibitors statins
Prazosin/ Minipress
antihypertensives peripherally acting antiadrenergics
Prednicarbate/ Dermatop
anti inflammatories steroidal immune modifiers corticosteroids topical
Prednisolone/ FloPred, Orapred, Pediapred, Prelone
anti inflammatories steroidal (intermediateacting) immune modifiers
membranes before and periodically throughout course of therapy. Obtain a diet history, especially with regard to fat consumption. Obtain a diet history, especially with regard to fat consumption. Monitor liver function tests, including AST, prior to, at 612 wk after initiation of therapy or after dose elevation, and then every 6 mo. Monitor intake and output ratios and daily weight and assess for edema daily; blood pressure and pulse frequently; urinary symptoms at beginning and throughout therapy. Assess affected skin prior to and daily during therapy. Note degree of inflammation and pruritus. Periodic adrenal function tests may be ordered to assess for hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected. Assess patient for signs of adrenal insufficiency; intake and output ratios and daily weights; peripheral edema, steady weight gain, rales/crackles, or dyspnea prior to and periodically throughout therapy. Monitor serum electrolytes and glucose. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal axis suppression in systemic and chronic topical therapy. Assess patient for signs of adrenal insufficiency; intake and output ratios and daily weights; peripheral edema, steady weight gain, rales/crackles, or dyspnea before and periodically throughout therapy. Monitor serum electrolytes and glucose. Periodic adrenal
anaphylaxis.
Dizziness, headache, rhinitis, bronchitis, chest pain, peripheral edema, abdominal cramps, rashes, constipation, diarrhea, flatus, heartburn, altered taste, dyspepsia, elevated liver enzymes, nausea, pancreatitis, pruritus, rhabdomyolysis, arthralgia, arthritis, myalgia, myositis, hypersensitivity reactions. Dizziness, headache, weakness, first-dose orthostatic hypotension, palpitations, angina, edema, abdominal cramps, diarrhea, dry mouth, nausea, vomiting, erectile dysfunction, priapism. Allergic contact dermatitis, atrophy, burning, dryness, edema, pruritis, hypertrichosis, hypopigmentation, irritation, maceration, adrenal suppression
Prednisone/ Sterapred
anti inflammatories steroidal (intermediate acting) immune modifiers
Depression, euphoria, increased intracranial pressure, restlessness, cataracts, increased intraocular pressure, hypertension, peptic ulceration, anorexia, nausea, vomiting, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, fluid retention, hypokalemia, hypokalemic alkalosis, thromboembolism, weight gain, weight loss, muscle wasting, osteoporosis, aseptic necrosis of joints, muscle pain. Depression, euphoria, increased intracranial pressure, increased intraocular pressure, hypertension, peptic ulceration, anorexia, nausea, vomiting, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, fluid retention, weight gain,
179
Rev. 08/21/08
Pregabalin/ Lyrica
analgesics anticonvulsants gamma aminobutyric acid gaba analogues nonopioid analgesics anticonvulsants
function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal axis suppression in systemic and chronic topical therapy. Assess location, characteristics, and intensity of pain periodically during therapy. Assess location, duration, and characteristics of seizure activity.
Primidone/ Myidone, Mysoline
Probenecid/ Probalan
antigout agents uricosurics
Procainamide/ Pronestyl
antiarrhythmics (class IA)
Procaine penicillin G/ Wycillin
anti-infectives penicillins
Assess location, duration, frequency, and characteristics of seizure activity; allergy to Phenobarbital; signs of folic acid deficiency at beginning of and during therapy. CBC and sequential multiple analysis12 (SMA-12) tests should be monitored every 6 mo throughout course of therapy. Monitor serum folate concentrations periodically during therapy. Assess involved joints for pain, mobility, and edema throughout course of therapy. Monitor intake and output ratios. CBC, serum uric acid levels, and renal function should be monitored routinely during long-term therapy. Serum and urine uric acid determinations may be measured periodically when probenecid is used to treat hyperuricemia. Monitor ECG, pulse, and blood pressure continuously throughout IV administration. Monitor CBC every 2 wk during the first 3 mo of therapy. Monitor ANA periodically during prolonged therapy or if symptoms of lupus-like reaction occur. Assess for infection; reactions to penicillins, cephalosporins, or other beta-lactam antibiotics; and signs and symptoms of anaphylaxis at beginning of
thromboembolism, weight loss, thrombophlebitis, muscle wasting, muscle pain, osteoporosis, cushingoid appearance, increased susceptibility to infection. Dizziness, drowsiness, impaired attention/ concentration/thinking, edema, blurred vision, dry mouth, constipation, appetite, vomiting, platelet count, weight gain, allergic reactions, fever. Ataxia, drowsiness, vertigo, excitement, visual changes, dyspnea, edema, orthostatic hypotension, anorexia, druginduced hepatitis, nausea, vomiting, alopecia, rash, blood dyscrasias, megaloblastic anemia, folic acid deficiency.
Headache, dizziness, nausea, vomiting, abdominal pain, diarrhea, drug-induced hepatitis, sore gums, uric acid stones, urinary frequency, flushing, rashes, aplastic anemia, anemia.
Seizures, confusion, dizziness, asystole, heart block, ventricular arrhythmias, hypotension, diarrhea, anorexia, bitter taste, nausea, vomiting, rashes, agranulocytosis, eosinophilia, leukopenia, thrombocytopenia, chills, drug-induced systemic lupus syndrome, fever. Seizures, diarrhea, epigastric distress, nausea, vomiting, eosinophilia, pseudomembranous colitis, interstitial nephritis, rash, urticaria, leucopenia, allergic
180
Rev. 08/21/08
Procarbazine/ Matulane
antineoplastics alkylating agents
and during therapy. Monitor serum sodium concentrations in patient with hypertension or CHF. Monitor blood pressure, pulse, and respiratory rate; nutritional status; bone marrow depression; bleeding; Signs and symptoms of hypertensive crisis during therapy. Monitor hemoglobin, hematocrit, WBC, differential, reticulocytes, and platelet count prior to and every 34 days during therapy. Monitor urinalysis, AST, ALT, alkaline phosphatase, and BUN at least weekly during therapy. Monitor blood pressure (sitting, standing, lying down), ECG, pulse, and respiratory rate; level of sedation; onset of akathisia and extrapyramidal side effects; tardive dyskinesia; development of neuroleptic malignant syndrome; fluid intake and bowel function; degree and manifestations of anxiety and mental status before and frequently during therapy. Assess patient for nausea and vomiting before and 3060 min after administration. Monitor intake and output ratios and weekly weight; BP; usual menstrual history; pattern and amount of vaginal bleeding before and throughout therapy. Monitor hepatic function before and periodically during therapy.
Prochlorperazine/ Compazine, Ultrazine
antiemetics antipsychotics phenothiazines
reactions including anaphylaxis and serum sickness, superinfection, pain at IM site, phlebitis at IV site. Seizures, confusion, dizziness, drowsiness, hallucinations, headache, mania, mental depression, nightmares, psychosis, syncope, tremor, nystagmus, photophobia, retinal hemorrhage, cough, pleural effusions, edema, hypotension, tachycardia, nausea, vomiting, anorexia, dysphagia, hepatic dysfunction, stomatitis, gonadal suppression, alopecia, gynecomastia, anemia, neuropathy, paresthesia, ascites, secondary malignancy. Neuroleptic malignant syndrome, extrapyramidal reactions, sedation, tardive dyskinesia, blurred vision, dry eyes, lens opacities, ECG changes, hypotension, tachycardia, constipation, dry mouth, anorexia, drug-induced hepatitis, ileus, pink or reddish-brown discoloration of urine, urinary retention, photosensitivity, pigment changes, rashes, galactorrhea, agranulocytosis, leucopenia, hyperthermia, allergic reactions. Depression, pulmonary embolism, changes in menstrual flow, weight gain, thromboembolism, cervical erosions, chloasma, rashes, melasma, breast tenderness, amenorrhea, edema, allergic reactions including anaphylaxis and angioedema, weight loss. Neuroleptic malignant syndrome, confusion, disorientation, sedation, dizziness, extrapyramidal reactions, fatigue, insomnia, nervousness, blurred vision, diplopia, tinnitus, bradycardia, hypertension, hypotension, tachycardia, constipation, drug-induced hepatitis, dry
Progesterone/ Crinone, Endometrin, Prochieve, Prometrium
hormones progestins
Promethazine/ Antinaus, Pentazine, Phenadoz, Phenergan, Promacot, Promet, Prorex
antiemetics antihistamines sedative/hypnotics phenothiazines
Monitor blood pressure, pulse, and respiratory rate; level of sedation; onset of extrapyramidal side effects; adverse anticholinergic effects; allergy symptoms; nausea and vomiting before and periodically throughout course of therapy. If administered IV, assess for
181
Rev. 08/21/08
Propafenone/ Rythmol
antiarrhythmics (class IC)
burning and pain at IV site; may cause severe tissue injury. CBC should be evaluated periodically during chronic therapy. Monitor ECG or use Holter monitor; blood pressure and pulse; intake and output ratios and daily weight; signs of CHF prior to and periodically during therapy. Monitor prothrombin level in patients taking warfarin; may effects of warfarin Assess for abdominal pain prior to and periodically throughout therapy. Antagonizes effects of pentagastrin and histamine during gastric acid secretion test. Avoid administration for 24 hr preceding the test. Assess respiratory status, pulse, and blood pressure continuously throughout propofol therapy. Assess level of sedation and level of consciousness throughout and following administration. Assess level of sedation and level of consciousness throughout and following administration. Monitor for propofol infusion syndrome. Assess type, location, and intensity of pain prior to and 2 hr (peak) following administration. Assess blood pressure, pulse, and respirations; bowel function; CNS effects before and periodically during therapy.
mouth, photosensitivity, severe tissue necrosis upon infiltration at IV site, rashes, blood dyscrasias. Dizziness, shaking, weakness, blurred vision, supraventricular arrhythmia, ventricular arrhythmias, conduction disturbances, angina, bradycardia, hypotension, altered taste, constipation, nausea, vomiting, diarrhea, dry mouth, rash, joint pain. Confusion, dizziness, drowsiness, excitement, blurred vision, mydriasis, photophobia, tachycardia, orthostatic hypotension, palpitations, constipation, dry mouth, rash, urinary hesitancy, urinary retention, decreased sweating. Dizziness, headache, apnea, cough, bradycardia, hypotension, hypertension, abdominal cramping, hiccups, nausea, vomiting, flushing, burning, pain, stinging, coldness, numbness, tingling at IV site, involuntary muscle movements, perioperative myoclonia, discoloration of urine (green), propofol infusion syndrome, fever. Dizziness, weakness, dysphoria, euphoria, headache, insomnia, paradoxical excitement, sedation, blurred vision, hypotension, nausea, abdominal pain, rash, constipation, vomiting, physical or psychological dependence, tolerance. Dizziness, weakness, dysphoria, euphoria, headache, insomnia, paradoxical excitement, sedation, blurred vision, hypotension, nausea, abdominal pain, rash, constipation, vomiting, physical or psychological dependence, tolerance.
Propantheline/ ProBanthine
antiulcer agents anticholinergics antimuscarinics
Propofol/ Diprivan
general anesthetics
Propoxyphene hydrochloride/ Darvon
opioid analgesics opioid agonists
Propoxyphene hydrochloride/ acetaminophen// Wygesic
opioid analgesics opioid agonists opioid agonists nonopioid analgesic combinations
Assess type, location, and intensity of pain prior to and 2 hr (peak) following administration. Assess blood pressure, pulse, and respirations; bowel function; CNS effects before and periodically during therapy.
182
Rev. 08/21/08
Propoxyphene hydrochloride/aspirin/ caffeine// Darvon Compound-65
opioid analgesics opioid agonists opioid agonists nonopioid analgesic combinations
Assess type, location, and intensity of pain prior to and 2 hr (peak) following administration. Assess blood pressure, pulse, and respirations; bowel function; CNS effects before and periodically during therapy.
Propoxyphene napsylate/ Darvon N
opioid analgesics opioid agonists
Assess type, location, and intensity of pain prior to and 2 hr (peak) following administration. Assess blood pressure, pulse, and respirations; bowel function; CNS effects before and periodically during therapy.
Propoxyphene napsylate/ acetaminophen// Darvon A500, Darvocet-N 50, Darvocet-N 100
opioid analgesics opioid agonists opioid agonists nonopioid analgesic combinations
Assess type, location, and intensity of pain prior to and 2 hr (peak) following administration. Assess blood pressure, pulse, and respirations; bowel function; CNS effects before and periodically during therapy.
Propranolol/ Inderal, Inderal LA, InnoPran XL
antianginals antiarrhythmics (Class II) antihypertensives vascular headache suppressants beta blockers
Monitor blood pressure and pulse; ECG monitoring and may have pulmonary capillary wedge pressure (PCWP) or central venous pressure (CVP); orthostatic hypotension; intake and output ratios and daily weight; evidence of fluid overload; frequency and characteristics of anginal attacks; frequency, severity, characteristics, and location of vascular headaches before and periodically during therapy. Abrupt withdrawal of propranolol may precipitate lifethreatening arrhythmias, hypertension, or myocardial ischemia. Drug should be tapered over a 2 week period before discontinuation. Assess patient carefully during tapering and after medication is discontinued.
Dizziness, weakness, dysphoria, euphoria, headache, insomnia, paradoxical excitement, sedation, blurred vision, hypotension, nausea, abdominal pain, rash, constipation, vomiting, physical or psychological dependence, tolerance. Dizziness, weakness, dysphoria, euphoria, headache, insomnia, paradoxical excitement, sedation, blurred vision, hypotension, nausea, abdominal pain, rash, constipation, vomiting, physical or psychological dependence, tolerance. Dizziness, weakness, dysphoria, euphoria, headache, insomnia, paradoxical excitement, sedation, blurred vision, hypotension, nausea, abdominal pain, rash, constipation, vomiting, physical or psychological dependence, tolerance. Fatigue, weakness, anxiety, dizziness, drowsiness, insomnia, memory loss, mental depression, mental status changes, nervousness, nightmares, blurred vision, dry eyes, nasal stuffiness, bronchospasm, wheezing, arrhythmias, bradycardia, CHF, pulmonary edema, orthostatic hypotension, peripheral vasoconstriction, constipation, diarrhea, nausea, erectile dysfunction, decreased libido, itching, rashes, hyperglycemia, hypoglycemia, arthralgia, back pain, muscle cramps, paresthesia, druginduced lupus syndrome.
183
Rev. 08/21/08
Propylthiouracil/ PTU
antithyroid agents
Monitor response of symptoms of hyperthyroidism or thyrotoxicosis; development of hypothyroidism; skin rash or swelling of cervical lymph nodes prior to and during therapy.
Protamine sulfate
antidotes antiheparins
Prussian blue (insoluble)/ ferric (III) hexacyanoferrate (II), Radiogardase
antidotes radiation protectants insoluble complex
Pseudoephedrine/ Cenafed, Congestaid, Decofed, Dimetapp Maximum Strength 12 Hour Non-Drowsy Extentabs, Dimetapp Decongestant Pediatric, Drixoral 12 Hour NonDrowsy Formula, Efidac 24, Genafed, Halofed, Kid Kare, Medi-First Sinus Decongestant, PediaCare Infants' Decongestant Drops, Pediatric Nasal Decongestant, Simply Stuffy, Sinustop,
allergy, cold and cough remedies nasal drying agents decongestants
Assess for bleeding and hemorrhage; allergy to fish (salmon), previous reaction to or use of protamine insulin or protamine sulfate; signs and symptoms of hypersensitivity reaction prior to and during therapy. Assess for hypovolemia before initiation of therapy. Monitor clotting factors, activated clotting time (ACT), activated partial thromboplastin time (aPTT), and thrombin time (TT) 5 15 min after therapy and again as necessary. Assess patient for signs of radiation toxicity. Measure and record radioactivity counts in urine and fecal samples at baseline and weekly to monitor 137Cs elimination rate. Monitor CBC, serum chemistry and electrolytes closely during therapy. Assess congestion, pulse and blood pressure; lung sounds and character of bronchial secretions before and periodically during therapy. Maintain fluid intake of 15002000 ml/day to decrease viscosity of secretions.
Drowsiness, headache, vertigo, nausea, vomiting, diarrhea, drug-induced hepatitis, loss of taste, rash, skin discoloration, urticaria, hypothyroidism, agranulocytosis, leukopenia, arthralgia, thrombocytopenia, fever, lymphadenopathy, parotitis. Dyspnea, bradycardia, hypertension, hypotension, pulmonary hypertension, nausea, vomiting, flushing, warmth, bleeding, back pain, hypersensitivity reactions including anaphylaxis, angioedema, and pulmonary edema.
Constipation, hypokalemia.
Seizures, anxiety, nervousness, dizziness, drowsiness, excitability, fear, hallucinations, headache, insomnia, restlessness, weakness, respiratory difficulty, cardiovascular collapse, palpitations, hypertension, tachycardia, anorexia, dry mouth, dysuria, diaphoresis.
184
Rev. 08/21/08
Silfedrine, Sudafed, Sudafed Childrens's NonDrowsy, Sudafed 12 Hour, Sudafed NonDrowsy Maximum Strength, Sudodrin, Triaminic Allergy Congestion Softchews, Unifed Psyllium/ Alramucil, Cillium, Effer-Syllium, Fiberall, Fibrepur, Hydrocil, Konsyl, Metamucil, Modane Bulk, Mylanta Natural Fiber Supplement, Naturacil Caramels, Perdiem, ProLax, Reguloid Natural, Serutan, Siblin, Syllact, Vitalax, V-Lax Pyridostigmine/Mestin on, Mestinon Timespan, Regonol
laxatives bulk forming agents
Assess patient for abdominal distention, presence of bowel sounds, and usual pattern of bowel function. Assess color, consistency, and amount of stool produced.
Bronchospasm, cramps, intestinal or esophageal obstruction, nausea, vomiting.
antimyasthenics cholinergics
Pyridoxine/ Beesix, Doxine, Nestrex, Pyri, Rodex, Vitabee 6, vitamin B6 Pyrimethamine/ Daraprim
vitamins water soluble vitamins
Assess pulse, respiratory rate, and blood pressure; overdose, underdose, or resistance prior to and during therapy. Assess neuromuscular status, including vital capacity, ptosis, diplopia, chewing, swallowing, hand grasp, and gait before administering and at peak effect. Assess patient for signs of vitamin B6 deficiency before and periodically throughout therapy. Assess patient for improvement in signs and symptoms of infection daily during therapy. Monitor CBC and platelet count periodically during therapy; semiweekly in patients with toxoplasmosis.
Seizures, dizziness, weakness, lacrimation, miosis, bronchospasm, excessive secretions, bradycardia, hypotension, abdominal cramps, diarrhea, excessive salivation, nausea, vomiting, sweating, rashes.
Sensory neuropathy, paresthesia, pyridoxinedependency syndrome.
antimalarials antiprotozoals
Seizures, arrhythmias, atrophic glossitis, fever, megaloblastic anemia, headache, insomnia, lightheadedness, malaise, mental depression, dry throat, pulmonary eosinophilia, anorexia, diarrhea, nausea.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Quazepam/ Doral
sedative/hypnotics benzodiazepines
Assess sleep patterns before and periodically throughout course of therapy. Prolonged therapy may lead to psychological or physical
Abnormal thinking, behavior changes, daytime drowsiness, palpitations, abdominal pain, itching, constipation, muscle spasm, ataxia, trembling,
185
Rev. 08/21/08
dependence. Quetiapine/ Seroquel, Seroquel XR antipsychotics mood stabilizers Monitor mental status; suicidal tendencies; weight and BMI; blood pressure (sitting, standing, lying) and pulse; onset of extrapyramidal side effects; tardive dyskinesia; and development of neuroleptic malignant syndrome before and periodically during therapy.
allergic reactions, tolerance. Neuroleptic malignant syndrome, seizures, dizziness, cognitive impairment, extrapyramidal symptoms, sedation, tardive dyskinesia, ear pain, rhinitis, pharyngitis, cough, dyspnea, palpitations, peripheral edema, postural hypotension, anorexia, constipation, dry mouth, dyspepsia, sweating, leucopenia, weight gain, hyperglycemia, flu-like syndrome. dizziness, fatigue, headache, cough, hypotension, chest pain, abdominal pain, diarrhea, nausea, vomiting, impaired renal function, rashes, hyperkalemia, back pain, myalgia, dyspnea, angioedema. Abdominal cramps/pain, diarrhea, nausea, vomiting, cinchonism, hypersensitivity reactions including fever and anaphylaxis, hemolytic uremic syndrome, Stevens-Johnson syndrome. Headache, pruritus, rash, thrombophlebitis, pseudomembranous colitis, diarrhea, nausea, vomiting, edema/inflammation/pain at infusion site, infusion site reactions, allergic reactions including anaphylaxis, pain.
Quinapril/Accupril
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor weight and assess patient routinely for resolution of fluid overload. Monitor renal function.
Quinine/ Qualaquin
antimalarials
Assess patient for improvement in signs and symptoms of condition daily during therapy.
Quinupristin/dalfoprist in// Synercid
anti-infectives streptogramins
Assess patient for infection; pain or inflammation at the infusion site; signs and symptoms of anaphylaxis; myalgia and arthralgia at beginning of and throughout therapy.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Rabeprazole/ Aciphex
antiulcer agents proton pump inhibitors
Raloxifene/ Evista
bone resorption inhibitors selective estrogen receptor modulators
Assess routinely for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate. Monitor CBC with differential periodically during therapy. Assess patient for bone mineral density with x-ray, serum, and urine bone turnover markers before and periodically during therapy.
Dizziness, headache, malaise, abdominal pain, constipation, diarrhea, nausea, photosensitivity, rash, neck pain, allergic reactions, chills, fever. Stroke, deep vein thrombosis, pulmonary embolism, retinal vein thrombosis, leg cramps, hot flashes.
186
Rev. 08/21/08
Raltegravir/ Isentress
antiretrovirals integrase strand transfer inhibitor (INSTI)
Assess patient for change in severity of HIV symptoms and for symptoms of opportunistic infections during therapy. Monitor viral load and CD4 counts regularly during therapy.
Ramelteon/ Rozerem
sedative/hypnotics melatonin receptor agonists
Assess sleep patterns before and periodically throughout therapy.
Ramipril/Altace
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor weight and assess patient routinely for resolution of fluid overload. Monitor renal function. Assess eye for signs of infection frequently during week following injection. Increases in intraocular pressure have been seen within 30 min of injection. Assess patient for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate Assess location, duration, intensity, and precipitating factors of anginal pain; and ECG at baseline and periodically during therapy. Assess signs and symptoms of Parkinson's disease; blood pressure; and skin for melanomas prior to and during therapy. Monitor patients for signs of allergic reactions and anaphylaxis during therapy. Monitor patients for hemolysis; and methemoglobinemia during therapy. Monitor respiratory rate and blood pressure frequently during therapy. Assess type, location, and intensity of pain before and 35 min after administration when
Ranibizumab/ Lucentis
ocular agents monoclonal antibodies
Ranitidine/ Zantac
histamine h2 antagonists, antiulcer agents antianginals
Headache, dizziness, fatigue, weakness, MI, diarrhea, abdominal pain, gastritis, hepatitis, vomiting, renal failure/ impairment, anemia, neutropenia, lipodystrophy, hypersensitivity reactions, immune reconstitution syndrome, fever. Abnormal thinking, behavior changes, dizziness, fatigue, hallucinations, headache, insomnia, sleepdriving, nausea, prolactin levels, testosterone levels. Dizziness, fatigue, headache, vertigo, weakness, cough, hypotension, chest pain, diarrhea, nausea, vomiting, impaired renal function, rashes, hyperkalemia, angioedema. Conjunctival hemorrhage, eye pain, intraocular pressure, intraocular inflammation, vitreal floaters, endophthalmitis, retinal detachment, arterial thromboembolic events. confusion, arrhythmias, agranulocytosis, aplastic anemia Dizziness, headache, tinnitus, palpitations, QTc prolongation, abdominal pain, constipation, dry mouth, nausea, vomiting. Depression, chest pain, albuminuria, libido, alopecia, ecchymosis, melanoma risk, rash, dyskinesia, allergic reactions, flu-like syndrome, fall risk, fever. Headache, abdominal pain, constipation, diarrhea, nausea, vomiting, mucositis, rash, hemolysis, methemoglobinemia, neutropenia, fever, sepsis, hypersensitivity reactions including anaphylaxis. Confusion, blurred/double vision, apnea, shivering, laryngospasm, allergic bronchospasm, respiratory depression, arrhythmias, bradycardia, circulatory
Ranolazine/ Ranexa
Rasagiline/ Azilect
antiparkinson agents monoamine oxidase type b inhibitors Anti-gout agents antihyperuricemics enzymes
Rasburicase/ Elitek
Remifentanil/ Ultiva
opioid analgesics opioid agonists
187
Rev. 08/21/08
used to treat pain.
Repaglinide/ Prandin
antidiabetics meglitinides
Reserpine/Novoreserpi ne, Reserfia
antihypertensives peripherally acting antiadrenergics
Retapamulin/ Altabax
anti-infectives pleuromutilins
Reteplase/ Retavase
thrombolytics plasminogen activators
rho(d) immune globulin standard dose IM/ HyperRHO S/D Full Dose, RhoGAM rho(d) immune globulin microdose IM/ HyperRHO S/D Mini-Dose, MICRhoGAM, MiniGamulin R
vaccines/immunizin g agents immune globulins
Observe patient for signs and symptoms of hypoglycemic reactions during therapy. Monitor fasting serum glucose and glycosylated hemoglobin periodically during therapy to evaluate effectiveness. Monitor blood pressure and pulse; intake and output ratios and daily weight and assess for edema daily; depression; early morning insomnia, anorexia, erectile dysfunction, and selfdeprecation periodically throughout course of therapy. Assess lesions before and daily during therapy. Monitor for application site irritation. Monitor vital signs, including temperature, continuously for myocardial infarction and at least every 4 hr during therapy for other indications. Assess patient carefully for bleeding every 15 min during the 1st hr of therapy, every 1530 min during the next 8 hr, and at least every 4 hr for the duration of therapy. Assess patient for hypersensitivity reaction; ECG; intensity, character, location, and radiation of chest pain; heart sounds and breath sounds; and neurologic status throughout therapy. Monitor patient for signs and symptoms of intravascular hemolysis (IVH), anemia, and renal insufficiency.
depression, hypotension, skeletal and thoracic muscle rigidity. Angina, chest pain, hypoglycemia, hyperglycemia.
Depression, drowsiness, lethargy, nasal stuffiness, conjunctival congestion, miosis, bradycardia, angina, arrhythmias, edema, diarrhea, cramps, dry mouth, GI bleeding, nausea, vomiting, erectile dysfunction, flushing, galactorrhea, gynecomastia, sodium and water retention. Application site irritation.
Intracranial hemorrhage, epistaxis, gingival bleeding, bronchospasm, hemoptysis, reperfusion arrhythmias, hypotension, recurrent ischemia, thromboembolism, GI bleeding, nausea, retroperitoneal bleeding, vomiting, GU tract bleeding, ecchymoses, flushing, urticaria, bleeding, hemorrhage at injection site, phlebitis at injection site, musculoskeletal pain, allergic reactions including anaphylaxis, fever.
vaccines/immunizin g agents immune globulins
Monitor patient for signs and symptoms of intravascular hemolysis (IVH), anemia, and renal insufficiency.
Dizziness, headache, hypertension, hypotension, rash, diarrhea, nausea, vomiting, arthralgia, anemia, intravascular hemolysis, myalgia, pain at injection site, fever. Dizziness, headache, hypertension, hypotension, rash, diarrhea, nausea, vomiting, arthralgia, anemia, intravascular hemolysis, myalgia, pain at injection site, fever.
188
Rev. 08/21/08
rho(d) immune globulin IV/ WinRho SDF
vaccines/immunizin g agents immune globulins
Assess vital signs periodically during therapy in patients receiving IV Rho(D) immune globulin.
rho(d) immune globulin microdose IM, IV / Rhophylac
vaccines/immunizin g agents immune globulins
Ribavirin/ Copegus, Rebetol, Virazole
antivirals nucleoside analogues
Riboflavin/ vitamin B2
vitamins water soluble vitamins agents atypical mycobacterium
Rifabutin/ Mycobutin
Monitor patient for signs and symptoms of intravascular hemolysis (IVH), anemia, and renal insufficiency. Assess vital signs periodically during therapy in patients receiving IV Rho(D) immune globulin. Assess patient for infection; respiratory; symptoms of hepatitis; signs of depression; cardiovascular disorders; signs of colitis; pancreatitis; pulmonary status; and fluid status at beginning and during therapy. Monitor CBC with differential and platelet count prior to initiation, at week 2, and week 4, and regularly during therapy. Monitor liver function tests and thyroid stimulating hormone prior to and periodically during therapy. Monitor liver function tests and thyroid stimulating hormone prior to and periodically during therapy. Assess patient for signs of vitamin B2 deficiency prior to and periodically throughout therapy. Monitor patient for signs of active tuberculosis and bowel function throughout therapy. Monitor CBC periodically during therapy.
Dizziness, headache, hypertension, hypotension, rash, diarrhea, nausea, vomiting, arthralgia, anemia, intravascular hemolysis, myalgia, pain at injection site, fever. Dizziness, headache, hypertension, hypotension, rash, diarrhea, nausea, vomiting, arthralgia, anemia, intravascular hemolysis, myalgia, pain at injection site, fever. Dizziness, faintness, blurred vision, conjunctivitis, erythema of the eyelids, ocular irritation, photosensitivity, cardiac arrest, hypotension, rash, hemolytic anemia (with interferon alpha 2b), reticulocytosis, emotional lability ( in children), fatigue ( in children), impaired concentration ( in children), insomnia ( in children), iritability ( in children), dry mouth, dyspnea( in children), anorexia ( in children), dyspepsia ( in children), vomiting ( in children), hemolytic anemia, pruritus ( in children), arthralgia ( in children), fever ( in children). Yellow discoloration of urine.
Rifampin/ Rifadin, Rimactane
antituberculars rifamycins
Assess lung sounds and character and amount of sputum periodically during therapy. Perform
Brown-orange discoloration of tears, ocular disturbances, dyspnea, chest pain, chest pressure, pseudomembranous colitis, brown-orange discoloration of saliva, altered taste, drug-induced hepatitis, brown-orange discoloration of urine, rash, skin discoloration, hemolysis, neutropenia, thrombocytopenia, arthralgia, myositis, brown-orange discoloration of body fluids, flu-like syndrome. Ataxia, confusion, drowsiness, fatigue, headache, weakness, red discoloration of tears, abdominal pain, diarrhea,
189
Rev. 08/21/08
Rifapentine/ Priftin
agents amyotrophic lateral sclerosis antituberculars
mycobacterial studies and susceptibility tests prior to and periodically during therapy to detect possible resistance. Evaluate renal function, CBC, and urinalysis periodically and during therapy. Monitor hepatic function at least monthly during therapy. Assess lung sounds and character and amount of sputum periodically throughout therapy. Assess hepatic enzymes, bilirubin, CBC, and platelet count prior to therapy. Monitor at least monthly, especially in relation to adverse reactions.
flatulence, heartburn, nausea, vomiting, drug-induced hepatitis, red discoloration of saliva, red discoloration of urine, hemolytic anemia, thrombocytopenia, arthralgia, myalgia, red discoloration of all body fluids, flu-like syndrome. Dizziness, headache, hemoptysis, hypertension, pseudomembranous colitis, anorexia, diarrhea, dyspepsia, increased liver enzymes, nausea, vomiting, hematuria, proteinuria, pyuria, urinary casts, acne, pruritus, rash, anemia, leukopenia, lymphopenia, neutropenia, thrombocytosis, arthralgia, pain. Dizziness, pseudomembranous colitis.
Rifaximin/ Xifaxan
anti-infectives rifamycins
Rilonacept/ Arcalyst
orphan drugs fusion proteins interleukin antagonists
Assess frequency and consistency of stools and bowel sounds prior to and during therapy. Assess fluid and electrolyte balance and skin turgor for dehydration. Assess for signs of infections and signs of hypersensitivity reactions during therapy. Monitor lipid profiles every 23 months during therapy. Assess patient for aggravation reaction causing worsening of ALS symptoms. Monitor AST, ALT, serum bilirubin, and GGT before and during therapy.
Riluzole/ Rilutek
agents amyotrophic lateral sclerosis
Rimantadine/ Flumadine
antivirals
Monitor respiratory status (rate, breath sounds, sputum) and temperature periodically.
Risedronate/ Actonel
bone resorption inhibitors biphosphonates
Assess patients via bone density study for low bone mass; and symptoms of Paget's disease before and periodically during therapy. Assess serum calcium and alkaline phosphatase before
Upper respiratory tract infections, cough, injection site reactions, changes in lipid profile, hypoesthesia, serious life-threatening infections, hypersensitivity reactions. Dizziness, weakness, headache, decreased lung function, hypertension, peripheral edema, abdominal pain, anorexia, diarrhea, dyspepsia, flatulence, nausea, vomiting, weight loss, arthralgia, back pain, circumoral paresthesia. Seizures, agitation, dizziness, fatigue, headache, impaired concentration, insomnia, mental depression, tinnitus, dyspnea, abdominal pain, anorexia, diarrhea, dry mouth, dyspepsia, nausea, vomiting, rash. Weakness, amblyopia, conjunctivitis, dry eyes, eye pain/inflammation, tinnitus, chest pain, edema, abdominal pain, diarrhea, belching, colitis, constipation, dysphagia, esophagitis,
190
Rev. 08/21/08
and periodically during therapy.
Risperidone/ Risperdal, Risperdal M-TAB, Risperdal Consta
Benzisoxazoles/ mood stabilizers/ Antipsychotics
Ritodrine/ Yutopar
tocolytic adrenergics
Ritonavir/ Norvir
antiretrovirals protease inhibitors
Monitor patient's mental status; weight and BMI; mood changes; suicidal tendencies; blood pressure (sitting, standing, lying down) and pulse; onset of extrapyramidal side effects; tardive dyskinesia; and development of neuroleptic malignant syndrome before and periodically during therapy. Obtain fasting blood glucose and cholesterol levels initially and periodically during therapy Assess uterine activity, gestational age and fetal maturity to determine premature labor, maternal blood pressure and pulse and fetal heart rate, intake and output ratios throughout therapy. Assess patient frequently during IV infusion for signs and symptoms of pulmonary edema. Blood glucose and electrolytes should be monitored carefully during prolonged therapy. Assess patient for change in severity of HIV symptoms and for symptoms of opportunistic infections during therapy. Monitor viral load and CD4 counts regularly during therapy. Monitor patient for fever, chills/rigors, nausea, urticaria, fatigue, headache, pruritus, bronchospasm, dyspnea, sensation of tongue or throat swelling, rhinitis, vomiting, hypotension, flushing, hypersensitivity reactions, ECG, signs of progressive multifocal leukoencephalopathy, and pain at disease sites. Monitor patient for tumor
esophageal ulcer, gastric ulcer, nausea, rash, arthralgia, musculoskeletal pain, osteonecrosis, flu-like syndrome. Neuroleptic malignant syndrome, aggressive behavior, dizziness, extrapyramidal reactions, headache, increased dreams, increased sleep duration, insomnia, sedation, pharyngitis, rhinitis, visual disturbances, cough, constipation, diarrhea, dry mouth, nausea, weight gain, decreased libido, dysmenorrhea/ menorrhagia, itching/skin rash. Headache, anxiety, nervousness, pulmonary edema, angina, hypotension, tachycardia (maternal and fetal), nausea, vomiting, druginduced hepatitis, erythema, hyperglycemia, agranulocytosis, leucopenia, tremors.
Rituximab/ Rituxan
antineoplastics monoclonal antibodies
Seizures, abnormal thinking, weakness, angioedema, heart block, abdominal pain, altered taste, anorexia, diarrhea, nausea, vomiting, hypersensitivity reactions including Stevens-Johnson syndrome and anaphylaxis. Progressive multifocal leukoencephalopathy, headache, bronchospasm, cough, dyspnea, arrhythmias, hypotension, peripheral edema, abdominal pain, altered taste, dyspepsia, mucocutaneous skin reactions, flushing, urticaria, hyperglycemia, hypocalcemia, anemia, neutropenia, thrombocytopenia, arthralgia, back pain, allergic reactions including anaphylaxis and
191
Rev. 08/21/08
Rivastigmine/ Exelon, Exelon Patch
anti-Alzheimers's agents cholinergics cholinesterase inhibitors vascular headache suppressants five ht1 agonists
lysis syndrome due to rapid reduction in tumor volume usually occurring 1224 hr after first infusion. Monitor CBC and platelet count regularly during therapy. Assess cognitive function periodically throughout therapy. Monitor patient for nausea, vomiting, anorexia, and weight loss. Assess pain location, character, intensity, and duration and associated symptoms during migraine attack.
angioedema, infections, infusion reactions, tumor lysis syndrome, fever/chills/rigors
Rizatriptan/ Maxalt, Maxalt-MLT
Rocuronium/ Zemuron
neuromuscular blocking agents nondepolarizing
Romiplostim/ Nplate
Antithrombocytope nic thrombopoetin receptor agonists
Ropinirole/ Requip, Requip XL
antiparkinson agents dopamine agonists
Ropivacaine/ Naropin
epidural local anesthetics anesthetics topical local
Assess respiratory status; ECG, heart rate, and blood pressure; residual muscle weakness and respiratory distress; infusion site throughout therapy and administration. Assess for bruising and bleeding throughout therapy. Monitor CBC, including platelet counts and periperal blood smears, prior to, weekly until a stable platelet count is achieved, and at least monthly thereafter. Monitor peripheral blood for signs of marrow fibrosis. Assess blood pressure; drowsiness and sleep attacks; signs and symptoms of Parkinson's disease; sleep patterns and frequency of restless leg disturbances periodically during therapy. Assess for systemic toxicity; BP, HR, and respiratory rate continuously during therapy. Monitor for return of sensation after procedure. Observe patient taking concurrent insulin for signs and symptoms of hypoglycemia. Assess patient for edema and signs of CHF; and signs of lactic acidosis during therapy.
Weakness, dizziness, drowsiness, headache, sedation, edema, heart failure, hypotension, anorexia, dyspepsia, nausea, vomiting, diarrhea. Dizziness, drowsiness, weakness, coronary artery vasospasm, MI, ventricular fibrillation, ventricular tachycardia, hypersensitivity reactions including angioedema. Bronchospasm, rash, allergic reactions including anaphylaxis.
Dizziness, insomnia, headache, abdominal pain, dyspepsia, bone marrow fibrosis, thrombosis/ thromboembolism, extremity pain, myalgia, arthralgia, shoulder pain, paresthesia.
Rosiglitazone/ Avandia
antidiabetics thiazolidinediones
Sleep attacks, dizziness, syncope, confusion, drowsiness, abnormal vision, orthostatic hypotension, peripheral edema, constipation, dry mouth, dyspepsia, nausea, vomiting, increased sweating. Seizures, cardiovascular collapse, arrhythmias, hypotension, tachycardia, nausea, vomiting, anemia, paresthesia, dyspnea, allergic reactions, fever. CHF, edema, new onset and worsening diabetic macular edema, urticaria, hepatitis, liver enzymes, anemia, lactic acidosis, total cholesterol, LDL and HDL, weight gain, angioedema (rare), fractures
192
Rev. 08/21/08
Rosuvastatin/ Crestor
lipid-lowering agents hmg coa reductase inhibitors statins
Rota virus vaccine live oral/Rotarix
vaccines/immunizin g agents active immunizer
Rufinamide/ Banzol
anticonvulsants triazoles
Obtain a diet history, especially with regard to fat consumption. Evaluate serum cholesterol and triglyceride levels before initiating, after 24 wk of therapy, and periodically thereafter. Monitor liver function tests, including AST, before, at 12 wk after initiation of therapy or after dose elevation, and then every 6 mo. Determine current health status and previous vaccination history of infant, including any reactions to previous dose of rotavirus vaccine. Delay administration in infants with acute diarrhea and vomiting. Assess location, duration, and characteristics of seizure activity. Monitor closely for notable changes in behavior that could indicate the emergence or worsening of suicidal thoughts or behavior or depression.
(arm, hand, foot) in female patients. Weakness, abdominal pain, constipation, nausea, rash, rhabdomyolysis, myalgia.
Cough, runny nose, flatulence, loss of appetite, rotavirus shedding in stool, vomiting, fussiness/irritability.
Dizziness, fatigue, headache, somnolence, suicidal thoughts/behavior, diplopia, QT prolongation, nausea, changes in appetite, urinary frequency, rash, anemia, ataxia, coordination abnormalities, gait disturbances, multi-organ hypersensitivity reactions.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Saliva substitutes/ Entertainers' Secret, MoiStir, Mouthkote, Optimoist, Salivart, Salix Salmeterol/ Serevent
saliva substitutes
bronchodilators adrenergics
Salsalate/ Amigesic, Anaflex, Disalcid, Marthritic, MonoGesic, Salflex, Salgesic, Salsitab
antipyretics nonopioid analgesics salicylates
Assess patient for xerostomia (dry mouth) or dry throat before and periodically throughout therapy. Assess gingiva and oral mucosa for stomatitis. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; and paradoxical bronchospasm before initiating therapy and periodically throughout. Assess pain and limitation of movement; note type, location, and intensity before and at the peak after administration. Assess fever and note associated signs.
Excessive absorption of electrolytes.
Headache, nervousness, palpitations, tachycardia, abdominal pain, diarrhea, nausea, muscle cramps/soreness, trembling, paradoxical bronchospasm, cough. Tinnitus, GI bleeding, dyspepsia, epigastric distress, nausea, abdominal pain, anorexia, hepatotoxicity, vomiting, exfoliative dermatitis, Stevens-Johnson
193
Rev. 08/21/08
Samarium Sm 153 lexidronam/ Quadramet
SAMe/Ademetionine,
nonopioid analgesics radiopharmaceutica ls antidepressants
Monitor hepatic function; and serum salicylate levels before antirheumatic therapy. Assess pain (intensity, location) periodically throughout therapy. Assess mental status for symptoms of depression and symptoms of pain and fatigue prior to and periodically during therapy. Assess diet prior to and during therapy. Monitor for signs of allergic reaction. Monitor blood Phe levels after 1 wk of treatment and periodically for up to 1 month. Assess for change in severity of symptoms of HIV and for symptoms of opportunistic infections during therapy. Monitor viral load and CD4 count regularly during therapy. Monitor hematologic and hepatic function before and periodically during therapy. Monitor heart rate, blood pressure, and respiratory status during and immediately after infusion. Assess for peripheral edema daily; first-dose reaction; fever daily; arthralgias and myalgias throughout therapy. Assess patient for symptoms of benign prostatic hypertrophy (BPH) before and periodically throughout therapy.
S-adenosylmethionine
syndrome, toxic epidermal necrolysis, allergic reactions including anaphylaxis and laryngeal edema. Arrhythmias, hypertension, anemia, neutropenia, thrombocytopenia, transient increase in bone pain. Agitation, dizziness, mild insomnia, manic reactions (in patients with bipolar disorder), vomiting, diarrhea, flatulence. Headache, pharyngolaryngeal pain, abdominal pain, diarrhea, nausea, vomiting, neutropenia.
Sapropterin/ Kuvan
antihyperphenylala ninemics synthetic BH4
Saquinavir/ Invirase
antiretrovirals protease inhibitors
Sargramostim/ Leukine, rHu GM-CSF (recombinant human granulocyte/macropha ge colony-stimulating factor) Saw palmetto/ American Dwarf Palm Tree, Cabbage Palm, JuZhong, Palmier Nain, Sabal, Sabal Fructus, Saw Palmetto Berry, Serenoa repens Scopolamine/ Isopto Hyoscine, TransdermScop
colony stimulating factors biologic response modifiers
Seizures, confusion, headache, abdominal discomfort, diarrhea, increased liver enzymes, jaundice, nausea, severe cutaneous reactions, hyperglycemia, acute myeloblastic leukemia, hemolytic anemia, thrombocytopenia, ataxia, Stevens-Johnson syndrome. Headache, malaise, weakness, dyspnea, pericardial effusion, peripheral edema, transient supraventricular tachycardia, diarrhea, itching, rash, arthralgia, bone pain, myalgia, chills, fever, first-dose reaction. Dizziness, headache, nausea, vomiting, constipation and diarrhea.
antiemetics anticholinergics
Secobarbital/ Seconal
sedative/hypnotics barbiturates
Assess patient for signs of urinary retention; heart rate; pain; nausea and vomiting periodically during therapy. Assess sleep patterns; respiratory status, pulse, and blood pressure; and pain prior to and periodically
Drowsiness, confusion, blurred vision, mydriasis, tachycardia, dry mouth, urinary hesitancy, urinary retention. Excess sedation, excitation, hallucinations, mental depression, vertigo, respiratory depression,
194
Rev. 08/21/08
throughout therapy. Selegiline/ApoSelegiline, Carbex, Eldepryl, GenSelegiline, NuSelegiline, SD-Deprenyl, Zelapar Selegiline transdermal/ Emsam antiparkinson agents monoamine oxidase type b inhibitors Assess patient for signs and symptoms of Parkinson's disease prior to and during therapy. Assess blood pressure periodically during therapy. Assess mental status, mood changes, and anxiety level frequently; suicidal tendencies, agitation, irritability, and unusual changes in behavior; blood pressure and pulse rate especially during early therapy. Monitor pediatric patients face-to-face weekly during first 4 wks, every other week for 4 wks, at 12 weeks, and as clinically indicated during therapy. Assess patient for abdominal distention, presence of bowel sounds, and usual pattern of bowel function. Assess color, consistency, and amount of stool produced.
arthralgia, myalgia, neuralgia, rashs, urticaria. Confusion, dizziness, fainting, hallucinations, insomnia, vivid dreams, nausea, abdominal pain, dry mouth.
antidepressants monoamine oxidase type b inhibitors
Sennosides/BlackDraught, Ex-Lax, ExLax Chocolated, Fletchers' Castoria, Maximum Relief Ex-Lax, Sena-Gen, Senexon, Senokot, SenokotXTRA Sertaconazole/ Ertaczo
laxatives stimulant laxatives
Insomnia, tinnitus, cough, hypertensive crisis, chest pain, orthostatic hypotension, peripheral edema, diarrhea, altered taste, anorexia, constipation, flatulence, gastroenteritis, vomiting, dysmenorrhea, metrorrhagia, urinary frequency, application site reactions , acne, ecchymoses, pruritus, sweating, mylagia, neck pain, pathologic fracture, paresthesia. Cramping, diarrhea, nausea, pink-red or brown-black discoloration of urine, electrolyte abnormalities, laxative dependence.
antifungals imidazoles
Sertraline/ Zoloft
antidepressants selective serotonin reuptake inhibitors ssris
Sevelamer/ Renagel, Renvela
electrolyte modifiers phosphate binders
Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Assess for suicidal tendencies, especially during early therapy. Monitor appetite and nutritional intake; weigh weekly; mood changes; frequency of obsessivecompulsive behaviors; frequency and severity of panic attacks; feelings of fear, helplessness, and horror; symptoms of social anxiety disorder; and symptoms of premenstrual dysphoric disorder periodically during therapy. Assess patient for GI side effects periodically during therapy. Monitor serum
Application site reactions, burning, contact dermatitis, dry skin, tenderness.
Suicidal thoughts, dizziness, drowsiness, fatigue, headache, insomnia, diarrhea, dry mouth, nausea, sexual dysfunction, urinary disorders, urinary frequency, increased sweating, hot flashes, rash, hyponatremia, back pain, myalgia, tremor, hypertonia, hypoesthesia, paresthesia, twitching, fever, thirst, impaired concentration, manic reaction, nervousness, weakness, yawning, agitation, anxiety. Diarrhea, dyspepsia, vomiting, constipation, flatulence, nausea.
195
Rev. 08/21/08
Sibutramine/ Meridia
weight control agents appetite suppressants
Sildenafil/Revatio, Viagra
erectile dysfunction agents phosphodiesterase type 5 inhibitors
phosphorous, calcium, bicarbonate, and chloride levels periodically during therapy. Monitor patients for weight loss and adjust concurrent medications as needed. Monitor blood pressure and heart rate regularly during therapy. Determine erectile dysfunction before administration. Monitor hemodynamic parameters and exercise tolerance prior to and periodically during therapy.
Silodosin/ Rapaflo
benign prostatic hyperplasia bph agents alpha adrenergic blockers
Silver sulfadiazine/Flint SSD, Sildimac, Silvadene, Thermazene Simethicone/Degas, Extra Strength Gas-X, Flatulex, Gas-X, Genasyme, Maximum Strength Mylanta Gas, Mylanta Gas, Mylicon, Phazyme Simvastatin/ Zocor
anti-infectives (topical) sulfonamides
antiflatulent
Sirolimus/ Rapamune
hmg coa reductase inhibitors statin, lipidlowering agents immunosuppressan ts
Assess patient for symptoms of benign prostatic hyperplasia; orthostatic reaction and syncope; BP (lying and standing) before and periodically during therapy. Assess burned tissue for infection and sepsis; hypersensitivity reaction prior to and throughout course of therapy. Assess patient for abdominal pain, distention, and bowel sounds prior to and periodically throughout course of therapy. Frequency of belching and passage of flatus should also be assessed. Obtain a diet history, especially with regard to fat consumption Monitor blood pressure and hyperlipidemia closely during therapy. Monitor sirolimus blood levels when dose forms are changed and in patients likely to have altered drug metabolism, patients >=13 yr who weigh <40 kg, patients with hepatic impairment, and during concurrent administration of drugs that may interact with sirolimus. Observe patient for signs and symptoms of
Seizures, headache, insomnia, CNS stimulation, anorexia, constipation, dry mouth, altered taste, increased appetite, increased sweating, rash. Headache, dizziness, insomnia, hearing loss, vision loss, epistaxis, nasal congestion, MI, sudden death, cardiovascular collapse, dyspepsia, diarrhea, priapism, urinary tract infection, flushing, rash, mylagia, paresthesias. Dizziness, headache, orthostatic hypotension, diarrhea, retrograde ejaculation.
Burning, itching, pain, rash, skin discoloration, skin necrosis, leukopenia.
None significant.
Sitagliptin/ Januvia
antidiabetics enzyme inhibitors
abdominal cramps, constipation, diarrhea, flatus, heartburn, rashes, rhabdomyolysis Insomnia, interstitial lung disease, edema, hypotension, hepatic toxicity, renal impairment, acne, rash, thrombocytopenic purpura, hypokalemia, leukopenia, thrombocytopenia, anemia, hyperlipidemia, arthralgias, tremor, risk of infection, risk of lymphoma, risk of lymphocele, mucosal herpes simplex infections, wound healing, lymphocele. Headache, nausea, diarrhea, upper respiratory tract
196
Rev. 08/21/08
Sodium bicarbonate/ Baking Soda, BellAns, Citrocarbonate, Neut, Soda Mint Sodium citrate and citric acid/ Bicitra, Oracit, Shohl's Solution modified
antiulcer agents alkalinizing agents
antiurolithics mineral electrolyte replacements supplements alkalinizing agents
Sodium chloride (IV/oral)/ Slo-Salt
mineral electrolyte replacements supplements
hypoglycemic reactions during therapy. Monitor hemoglobin A1C prior to and periodically during therapy. Monitor renal function prior to and periodically during therapy. Assess fluid balance, signs of acidosis, epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate throughout therapy. Assess patient for signs of alkalosis or hypernatremia throughout therapy. Monitor patients with renal dysfunction for fluid overload. 24-hr urine for citrate. Assess fluid balance; symptoms of hyponatremia or hypernatremia throughout therapy. Assess bowel function for constipation or diarrhea; blood pressure and heart rate; signs and symptoms of anaphylaxis; nutritional status and dietary history during therapy.
infection, nasopharyngitis, hypersensitivity reactions including anaphylaxis, angioedema, and exfoliative skin conditions (StevensJohnson syndrome), rash, urticaria. Edema, flatulence, gastric distention, metabolic alkalosis, hypernatremia, hypocalcemia, hypokalemia, sodium and water retention, irritation at IV site, tetany. Diarrhea, fluid overload, hypernatremia (severe renal impairment), hypocalcemia, metabolic alkalosis (large doses only), tetany.
Sodium ferric gluconate complex/ Ferrlecit
antianemics iron supplements
Sodium fluoride (oral)/ Flura-Drops, Luride, Pharmaflur, Phos-Flur Sodium oxybate/ Xyrem, gamma hydroxybutyrate (GHB)
dental caries prophylactic agents minerals electrolytes anticataplectic hydroxybutyrate
Examine teeth for staining or mottling periodically.
CHF, pulmonary edema, edema, hypernatremia, hypervolemia, hypokalemia, IVextravasation, irritation at IV site. Dizziness, headache, syncope, hypotension, hypertension, chest pain, nausea, vomiting, diarrhea, flushing, urticaria, pain or erythema at injection, arthralgia, myalgia, allergic reactions including anaphylaxis, fever, lymphadenopathy. Nausea, vomiting, atopic dermatitis, mottling of teeth.
Sodium phenylacetate/sodium benzoate// Ammonul
Sodium phosphate
mineral electrolyte replacements supplements phosphate supplements
Assess respiratory status, sleep patterns, and number of cataplexy attacks before starting sodium oxybate. Patients must be monitored at least every 3 months for effectiveness and side effects. Assess neurological status and infusion site frequently during therapy. Monitor plasma ammonia levels frequently during therapy. Assess patient for signs and symptoms of hypophosphatemia; and intake and output ratios and daily weight throughout therapy. Monitor serum phosphate, potassium,
Seizures, dizziness, pain, headache, somnolence, confusion, depression, insomnia, nervousness, weakness, respiratory depression, nausea, vomiting, urinary incontinence, arthritis, myalgia, hyperhidrosis. Seizures, mental impairment, vomiting, hyperglycemia, hypokalemia.
Confusion, listlessness, weakness, hypernatremia shortness of breath, arrhythmias, cardiac arrest, ECG changes, hypotension; hypernatremiaedema, diarrhea, abdominal pain,
197
Rev. 08/21/08
sodium, and calcium levels prior to and periodically throughout therapy. Monitor renal function studies prior to and periodically throughout therapy.
Sodium polystyrene sulfonate/Kayexalate, SPS
hypokalemic electrolyte modifiers cationic exchange resins
Solifenacin/ VESIcare
urinary tract antispasmodics anticholinergics hormones growth hormones
Somatrem/ Protropin
Somatropin (recombinant)/ Saizen
hormones growth hormones
Sorafenib/ Nexavar
antineoplastics kinase inhibitors
Monitor response of symptoms of hyperkalemia; intake and output ratios and daily weight; symptoms of fluid overload; symptoms of digitalis toxicity; abdomen and note character and frequency of stools during course of therapy. Monitor voiding pattern and assess symptoms of overactive bladder to and periodically during therapy. Monitor bone age annually and growth rate determinations, height, and weight every 36 mo during therapy. Monitor blood glucose periodically during therapy. Monitor bone age annually and growth rate determinations, height, and weight every 36 mo during therapy. Monitor thyroid function; blood glucose; and alkaline phosphatase prior to and during therapy. Monitor for development of neutralizing antibodies if growth rate does not exceed 2.5 cm/6 mo. Monitor blood pressure weekly during first 6 wks and then periodically during therapy. Assess for dermatologic toxicities; bleeding; and chest pain during therapy.
nausea, vomiting, hyperkalemia, hypernatremia, hyperphosphatemia, hypocalcemia, hypomagnesemia, irritation at IV site, phlebitis, hypocalcemiatremors, flaccid paralysis, heaviness of legs, paresthesias of extremities. Constipation, fecal impaction, anorexia, gastric irritation, nausea, vomiting, hypocalcemia, hypokalemia, sodium retention, hypomagnesemia.
Blurred vision, constipation, dry mouth, dyspepsia, nausea.
Edema of the hands and feet, hyperglycemia, hypothyroidism, insulin resistance, pain at injection site, local lipoatrophy or lipodystrophy with subcutaneous use, arthralgia. Edema of the hands and feet, exacerbation of pre-existing psoriasis, hyperglycemia, hypothyroidism, insulin resistance, pain at injection site, local lipoatrophy or lipodystrophy with subcutaneous use, arthralgia, musculoskeletal pain, swelling, stiffness.
Sotalol/ Betapace, Betapace AF, Sorine
antiarrhythmics (classes II and III)
Monitor blood pressure and pulse frequently; orthostatic
Depression, fatigue, weakness, hoarseness, hypertension, constipation, diarrhea, dyspepsia, dysphagia, myalgia, mucositis/stomatitis, nausea, anorexia, acne, erythema, exfoliative dermatitis, flushing, hand-foot skin reaction, pruritus, rash, hypophosphatemia, anemia, bleeding, leukopenia, neuropathy, thrombocytopenia, lymphopenia, athralgia, pain. Fatigue, weakness, arrhythmias, bradycardia,
198
Rev. 08/21/08
beta blockers
Spironolactone/ Aldactone
diuretics potassium sparing diuretics
hypotension; intake and output ratios and daily weight; evidence of fluid overload during dosage adjustment period and periodically throughout therapy. Monitor intake and output ratios and daily weight; signs and symptoms of hypokalemia during therapy. Evaluate serum potassium levels prior to and routinely during therapy.
St. John's wort (Hypericum Perforatum)/ Amber, Demon chaser, Goatweed, Hardhay, Klamath weed, Rosin rose, Tipton weed Stavudine/ d4T, Zerit, Zerit XR
antidepressants
Assess patient for depression periodically throughout therapy. Assess skin or skin lesions periodically throughout therapy.
CHF, pulmonary edema, erectile dysfunction, itching, rashes, hyperglycemia, hypoglycemia, arthralgia, back pain, muscle cramps, paresthesia, drug-induced lupus syndrome. Dizziness, clumsiness, headache, arrhythmias, GI irritation, erectile dysfunction, dysuria, gynecomastia (in males), breast tenderness, deepening of voice, increased hair growth (in females), hyperkalemia, hyponatremia, hyperchloremic metabolic acidosis, agranulocytosis, muscle cramps, allergic reactions. Dizziness, restlessness, sleep disturbances, hypertension, abdominal pain, bloating, constipation, dry mouth, feeling of fullness, flatulence, nausea, vomiting, allergic skin reactions, phototoxicity. Headache, insomnia, weakness, hepatic toxicity, pancreatitis, anorexia, diarrhea, lactic acidosis, anemia, arthralgia, myalgia, peripheral neuropathy.
antiretrovirals nucleoside reverse transcriptase inhibitors
Streptokinase/ Kabbikinase, Streptase
thrombolytics plasminogen activators
Assess patient for change in severity of symptoms of HIV infection and for symptoms of opportunistic infection during therapy. Monitor patient for signs and symptoms of peripheral neuropathy; signs of pancreatitis periodically throughout therapy. Monitor vital signs, including temperature, continuously for myocardial infarction. Assess patient carefully for bleeding every 15 min during the 1st hr of therapy, every 1530 min during the next 8 hr, and at least every 4 hr for the duration of therapy. Assess patient for hypersensitivity reaction; recent streptococcal infection; ECG continuously; intensity, character, location, and radiation of chest pain; heart sounds and breath sounds; pulse, blood pressure, hemodynamics, and respiratory status; and neurologic status
Intracranial hemorrhage, epistaxis, gingival bleeding, bronchospasm, hemoptysis, reperfusion arrhythmias, hypotension, recurrent ischemia/thromboembolism, GI bleeding, hepatotoxicity, nausea, retroperitoneal bleeding, vomiting, GU tract bleeding, ecchymoses, flushing, urticaria, bleeding, hemorrhage at injection site, phlebitis at injection site, musculoskeletal pain, allergic reactions including anaphylaxis, fever.
199
Rev. 08/21/08
throughout therapy. Streptomycin anti-infectives aminoglycosides Assess patient for infection; eighth cranial nerve function; intake and output and daily weight to assess hydration status and renal function; and signs of superinfection at beginning of and throughout therapy. Monitor vital signs; intake and output and daily weight; IV site; bone marrow depression; and hydration status, appetite, and nutritional intake prior to and periodically during therapy. Monitor for hepatotoxicity; serum uric acid; and CBC and differential prior to and weekly during therapy. Assess pain (intensity, location) periodically throughout therapy. Assess patient and family members for evidence of lead poisoning prior to and frequently throughout therapy. Monitor strict intake and output and daily weight; neurologic status; and signs of allergic reactions during therapy. Monitor blood and urine lead levels prior to and periodically throughout therapy. Ototoxicity, nephrotoxicity, hypomagnesemia, muscle paralysis, hypersensitivity reactions.
Streptozocin/ Zanosar
antineoplastics antitumor antibiotics
Strontium-89 chloride/ Metastron Succimer/ Chemet
nonopioid analgesics radiopharmaceutica ls antidotes chelating agents
Confusion, lethargy, mental depression, drug-induced hepatitis, nausea, vomiting, diarrhea, duodenal ulcer, nephrotoxicity, gonadal suppression, proteinuria, hypophosphatemia, anemia, leukopenia, thrombocytopenia, eosinophilia, phlebitis at IV site, injection site reactions, hypoglycemia, hyperglycemia, fever. Anemia, neutropenia, thrombocytopenia, transient increase in bone pain. Dizziness, drowsiness, headache, cloudy film in eye, otitis media, plugged ears, watery eyes, cough, nasal congestion, rhinorrhea, sore throat, arrhythmias, nausea, vomiting, abdominal cramps, anorexia, diarrhea, elevated liver function tests, hemorrhoidal symptoms, metallic taste, oliguria, proteinuria, voiding difficulty, mucocutaneous eruptions, pruritus, rashes, eosinophilia, chills, fever, thrombocytosis, back, rib, flank pain, leg pain, paresthesia, sensorimotor neuropathy, flu-like syndrome, moniliasis. Apnea, bronchospasm, arrhythmias, bradycardia, hypotension, hyperkalemia, rhabdomyolysis, muscle fasciculation, malignant hyperthermia, myoglobinemia, myoglobinuria, tachyphylaxis. Dizziness, drowsiness, constipation, diarrhea, dry mouth, gastric discomfort, indigestion, nausea, pruritus, rashes.
Succinylcholine/Anecti ne, Quelicin
neuromuscular blocking agents depolarizing
Sucralfate/ Carafate
antiulcer agents gi protectants
Assess respiratory status; neuromuscular response; ECG, heart rate, and blood pressure; signs of malignant hyperthermia; residual muscle weakness and respiratory distress throughout therapy. Assess patient routinely for abdominal pain and frank or occult blood in the stool.
200
Rev. 08/21/08
Sufentanil/ Sufenta
opioid analgesics analgesic adjuncts opioid agonists
Monitor respiratory rate and blood pressure frequently throughout therapy. Assess type, location, and intensity of pain before and 35 min after IV administration when sufentanil is used to treat pain.
Sulconazole/ Exelderm
antifungals (topical)
Sulfamethoxazole/ Gantanol, Urobak
anti-infectives sulfonamides
Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Assess patient for infection; allergy to sulfonamides; and intake and output ratios at beginning of and throughout therapy. Monitor CBC and urinalysis periodically throughout therapy.
Confusion, postoperative depression, postoperative drowsiness, apnea, cardiac arrest, laryngospasm, allergic bronchospasm, respiratory depression, arrhythmias, bradycardia, hypotension, biliary spasm, allergic reactions including anaphylaxis. Burning, itching, local hypersensitivity reactions, redness, stinging.
Sulfasalazine/ Azulfidine, Azulfidine EN-tabs
antirheumatics (DMARD) gastroinestinal anti inflammatories
Sulfinpyrazone/ Anturane
Anti-gout agents uricosurics
Sulfisoxazole/ ApoSulfisoxazole, Gantrisin
anti-infectives sulfonamides
Assess patient for allergy to sulfonamides and salicylates. Monitor intake and output ratios; abdominal pain and frequency, quantity, and consistency of stools; range of motion and degree of swelling and pain in affected joints before and periodically during therapy. Monitor urinalysis, BUN, and serum creatinine before and periodically during therapy. Monitor CBC before and every 36 mo during prolonged therapy. Assess involved joints for pain, mobility, and edema; and intake and output ratios throughout course of therapy. Assess patient for infection; allergy to sulfonamides; and intake and output ratios at beginning of and throughout therapy. Monitor CBC prior to and monthly during prolonged therapy. Monitor urinalysis prior to and periodically throughout therapy for crystalluria and
Nausea, anorexia, fever, crystalluria, rashes, agranulocytosis, aplastic anemia, eosinophilia, thrombocytopenia, peripheral neuropathy, hypersensitivity reactions including StevensJohnson syndrome and serum sickness, superinfection. Headache, pneumonitis, anorexia, diarrhea, nausea, vomiting, drug-induced hepatitis, crystalluria, oligospermia, orange-yellow discoloration of urine, rashes, exfoliative dermatitis, photosensitivity, yellow discoloration, agranulocytosis, aplastic anemia, blood dyscrasias, eosinophilia, megaloblastic anemia, thrombocytopenia, peripheral neuropathy, hypersensitivity reactions including serum sickness and Stevens-Johnson syndrome, fever. GI bleeding, nausea, vomiting, abdominal pain, rash, blood dyscrasias, fever.
Ataxia, confusion, dizziness, drowsiness, mental depression, psychosis, restlessness, nausea, diarrhea, anorexia, hepatitis, vomiting, crystalluria, rash, exfoliative dermatitis, photosensitivity, agranulocytosis, aplastic anemia, eosinophilia, thrombocytopenia, peripheral
201
Rev. 08/21/08
formation of urinary calculi.
Sulindac/ Clinoril
antirheumatics nonsteroidal anti inflammatory agents
Sumatriptan/ Imitrex, Imitrex STATdose
vascular headache suppressants five ht1 agonists
Sunitinib/ Sutent
antineoplastics kinase inhibitors
Patients who have asthma, aspirin-induced allergy, and nasal polyps are at increased risk for developing hypersensitivity reactions. Monitor for rhinitis, asthma, and urticaria; pain and range of movement before and after 12 wk of therapy. Evaluate BUN, serum creatinine, CBC, and liver function periodically in patients receiving prolonged therapy. Assess pain location, intensity, duration, and associated symptoms during migraine attack. Monitor blood pressure before and for 1 hr after initial injection. If angina occurs, monitor ECG for ischemic changes. Monitor for signs of CHF; left ventricular ejection fraction (LVEF); and hypertension during therapy. Monitor CBC with platelet count and serum chemistries including phosphate at the beginning of each treatment cycle. Monitor thyroid function in patients with symptoms of hypothyroidism.
neuropathy, hypersensitivity reactions including serum sickness and Stevens-Johnson syndrome, fever, superinfection. Dizziness, headache, tinnitus, edema, GI bleeding, druginduced hepatitis, constipation, diarrhea, discomfort, dyspepsia, nausea, vomiting, anorexia, renal failure, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, rashes, blood dyscrasias, prolonged bleeding time, allergic reactions including anaphylaxis and hypersensitivity syndrome. Dizziness, vertigo, tingling, warm sensation, injection site reaction, MI, angina, chest pressure, chest tightness, coronary vasospasm, ECG changes, transient hypertension, jaw discomfort, muscle cramps, numbness. Fatigue, dizziness, myalgia,headache, CHF, back pain, hypertension, peripheral edema, fever, thromboembolic events, diarrhea, dyspepsia, nausea, stomatitis, vomiting, rash, skin discoloration, adrenal insufficiency, hemorrhage, anemia, lymphopenia, neutropenia, limb pain, thrombocytopenia, hyperuricemia, arthralgia.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Tacrine/ Cognex
Tacrolimus (oral, IV)/ Prograf
anti-Alzheimers's agents cholinergics cholinesterase inhibitors immunosuppressan ts
Assess cognitive function and heart rate periodically throughout therapy.
Monitor blood pressure closely during therapy. Observe patients receiving IV tacrolimus for the development of anaphylaxis for at least 30 min and frequently thereafter. Monitor CBC, serum
Dizziness, headache, bradycardia, GI bleeding, anorexia, diarrhea, druginduced hepatitis, dyspepsia, nausea, vomiting. Seizures, dizziness, headache, insomnia, tremor, cough, pleural effusion, hypertension, peripheral edema, GI bleeding, abdominal pain, anorexia, ascites, constipation, diarrhea, dyspepsia, increased liver function studies, nausea,
202
Rev. 08/21/08
creatinine, potassium, and glucose closely.
Tacrolimus (topical)/ Protopic
immunosuppressan ts
Assess skin lesions prior to and periodically during therapy. Determine erectile dysfunction before administration. Tadalafil has no effect in the absence of sexual stimulation. Assess for an increase in bone or tumor pain. Monitor CBC, platelets, and calcium levels before and during therapy. Monitor serum cholesterol and triglyceride concentrations in patients with pre-existing hyperlipidemia. Assess patient for symptoms of prostatic hyperplasia; first-dose orthostatic hypotension and syncope; intake and output ratios and daily weight, and assess for edema daily before and periodically throughout therapy. Assess type, location, and intensity of pain before and 1 hr (peak) after administration. Assess blood pressure and respiratory rate; bowel function; seizures; serotonin syndrome during therapy. Assess patient for symptoms of IBS (abdominal pain or discomfort, bloating, constipation). Monitor signs of hepatitis and signs of myopathy during therapy.
Tadalafil/ Cialis
erectile dysfunction agents phosphodiesterase type 5 inhibitors antineoplastics antiestrogens
Tamoxifen/ Soltamox
Tamsulosin/ Flomax
peripherally acting antiadrenergics
vomiting, nephrotoxicity, urinary tract infection, pruritus, rash, arthralgia, hyperglycemia, fever, hyperkalemia, generalized pain, hyperlipidemia, hypokalemia, leukopenia, hypomagnesemia, hypophosphatemia, anemia, leukocytosis, thrombocytopenia, allergic reactions including anaphylaxis. Erythema, pruritis, skin infection, flu-like symptoms, increased risk of lymphoma/skin cancer. Headache, hearing loss, vision loss, nasal congestion, hypotension, dyspepsia, priapism, flushing, back pain, limb pain, myalgia. Confusion, depression, headache, weakness, blurred vision, pu.monary embolism, stroke, edema, nausea, vomiting, uterine malignancies, vaginal bleeding, hypercalcemia, leukopenia, thrombocytopenia, hot flashes, bone pain, tumor flare. Dizziness, headache, rhinitis, orthostatic hypotension, retrograde/diminished ejaculation.
Tapentadol/ Nucynta
analgesics (centrally acting) opioid analgesics opioid agonists
Seizures, dizziness, headache, somnolence, respiratory depression, nausea, vomiting.
Tegaserod/ Zelnorm
anti irritable bowel syndrome agents five ht4 agonists antivirals nucleoside analogues
Headache and diarrhea.
Telbivudine/ Tyzek
Fatigue, headache, hepatomegaly, neutropenia, lactic acidosis, myopathy, fever.
203
Rev. 08/21/08
Telithromycin/ Ketek
anti-infectives ketolides
Telmisartan/ Micardis
antihypertensives angiotensin ii receptor antagonists
Temazepam/ Restoril
sedative/hypnotics benzodiazepines
Assess for infection (vital signs; sputum, WBC) and signs or symptoms of hepatitis at beginning of and during therapy. Monitor liver function periodically during therapy and if signs of hepatitis occur. Assess blood pressure (lying, sitting, standing) and pulse; and signs of angioedema frequently during initial dosage adjustment and periodically throughout therapy. Monitor renal function. Assess mental status; sleep patterns before and periodically throughout therapy.
Loss of consciousness, visual disturbances, arrhythmias, QTc prolongation, pseudomembranous colitis, diarrhea, hepatitis, HEPATIC FAILURE, nausea, exacerbation of myasthenia gravis. Dizziness, fatigue, headache, hypotension, sinusitis, hyperkalemia, abdominal pain, diarrhea, dyspepsia, impaired renal function, back pain, myalgia, angioedema.
Temozolomide/Temod ar Temsirolimus/ Torisel
antineoplastics alkylating agents antineoplastics enzyme inhibitors kinase inhibitors
Monitor patient for seizures. Monitor CBC with differential and platelet count. Assess for signs of hypersensitivity reactions; signs of infection, including opportunistic infection; and signs of interstitial lung disease during therapy. Monitor CBC and platelet count prior to and during therapy. Monitor serum glucose; cholesterol and triglycerides; and liver enzymes prior to and periodically during therapy.
Tenecteplase/ TNKase
thrombolytics plasminogen activators
Assess patients for bleeding every 15 min during the 1st hr, every 1530 min during the next 8 hr and at least every 4 hr for the duration of therapy. Monitor vital signs, including temperature, every 4 hr during course of therapy. Assess neurologic status throughout therapy. Monitor ECG continuously in patients with coronary thrombosis
Abnormal thinking, behavior changes, hangover, dizziness, drowsiness, hallucinations, lethargy, paradoxic excitation, sleepdriving, blurred vision, constipation, diarrhea, nausea, vomiting, rashes, physical dependence, psychological dependence, tolerance. Seizures, fatigue, headache, nausea, vomiting, leukopenia, thrombocytopenia. Weakness, conjunctivitis, hypertension, venous thromboembolism, interstitial lung disease, bowel perforation, anorexia, liver enzymes, mucositis, nausea, renal failure, rash, abnormal wound healing, hyperglycemia, edema, hypophosphatemia, anemia, leukopenia, lymphopenia, thrombocytopenia, hyperlipidemia, hypertriglyceridemia, hypersensitivity reactions including anaphylaxis, risk of infections. Arrhthymias, cardiogenic shock, cardiac tamponade, embolism, heart failure, myocardial infarction, myocardial rupture, pericarditis, pericardial effusion, pulmonary edema, recurrent myocardial ischemia, thrombosis, hypotension, nausea, vomiting, bleeding, allergic reactions including anaphylaxis, fever.
204
Rev. 08/21/08
Teniposide/Vumon, VM-26
antineoplastics podophyllotoxin derivatives
Tenofovir/ Viread
antiretrovirals nucleoside reverse transcriptase inhibitors
for significant arrhythmias. Assess intensity, character, location, and radiation of chest pain. Monitor heart and breath sounds frequently. Monitor hematocrit, hemoglobin, platelet count, prothrombin time, thrombin time, activated partial thromboplastin time, and fibrinolytic activity prior to and frequently throughout therapy. Monitor blood pressure prior to and every 15 min during infusion. Monitor for hypersensitivity reaction; bone marrow depression; intake and output, appetite, and nutritional intake; infusion and infusion site during therapy. Monitor CBC and differential prior to and periodically throughout therapy. Monitor for change in severity of HIV symptoms and for symptoms of opportunistic infection before and during therapy.
Acute CNS depression, hypotension, diarrhea, mucositis, nausea, vomiting, alopecia, rashs, gonadal suppression, neutropenia, anemia, leukopenia, thrombocytopenia, phlebitis at IV site, peripheral neurotoxicity, allergic reactions including anaphylaxis, fever. Depression, headache, weakness, hepatomegaly, diarrhea, nausea, abdominal pain, anorexia, vomiting, flatulence, renal impairment, lactic acidosis, hypophosphatemia, rash, bone mineral density. Dizziness, headache, weakness, drowsiness, nervousness, nasal congestion, blurred vision, conjunctivitis, sinusitis, dyspnea, first-dose orthostatic hypotension, arrhythmias, chest pain, palpitations, peripheral edema, tachycardia, nausea, abdominal pain, paresthesia, fever. Burning, itching, local hypersensitivity reactions, redness, stinging.
Terazosin/ Hytrin
antihypertensives peripherally acting antiadrenergics
Monitor blood pressure (lying and standing) and pulse; first-dose orthostatic reaction and syncope; intake and output ratios and daily weight; symptoms of prostatic hyperplasia; and edema frequently during initial dose adjustment and periodically during therapy. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Assess lung sounds, pulse, and blood pressure; pulmonary function tests; and paradoxical bronchospasm before initiating therapy and
Terbinafine/ Lamisil AT
antifungals (topical)
Terbutaline/ Brethaire, Bricanyl
bronchodilators adrenergics
Nervousness, restlessness, tremor, headache, insomnia, paradoxical bronchospasm (excessive use of inhalers), angina, arrhythmias, hypertension, tachycardia,
205
Rev. 08/21/08
Terconazole/ Terazol3, Terazol-7
antifungals (vaginal)
Teriparatide/ Forteo
Testosterone buccal system, mucoadhesive/ Striant
hormones parathyroid hormones rDNA origin hormones androgens
periodically throughout. Observe patient for drug tolerance and rebound bronchospasm. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate sensitization and warrant discontinuation of medication. Assess patient for bone mineral density before and periodically during therapy. Monitor intake and output ratios, weigh patient twice weekly, and assess patient for edema. Monitor for breast enlargement, persistent erections, and increased urge to urinate in men. Monitor for difficulty urinating in elderly men, because prostate enlargement may occur. Monitor intake and output ratios, weigh patient twice weekly, and assess patient for edema. Monitor for precocious puberty in boys; breast enlargement, persistent erections, and increased urge to urinate in men; difficulty urinating in elderly men, because prostate enlargement may occur.
nausea, vomiting, hyperglycemia.
Abdominal pain, dysmenorrhea, irritation, itching, vulvovaginal burning, fever.
Orthostatic hypotension and muscle spasms.
Anxiety, fatigue, headache, edema, abdominal cramps, bitter taste, gingivitis, gum edema, gum tenderness, liver function test elevation, nausea, taste perversion, vomiting, priapism, prostatic enlargement, acne, gynecomastia, hypercholesterolemia. Deepening of voice, edema, cholestatic jaundice, druginduced hepatitis, liver function test elevation, nausea, vomiting, change in libido, erectile dysfunction, priapism, prostatic enlargement, gynecomastia, hirsutism, oligospermia, hypercholesterolemia, hypercalcemia, hyperkalemia, hyperphosphatemia, male pattern baldness, pain at injection site. Deepening of voice, edema, cholestatic jaundice, druginduced hepatitis, liver function test elevation, nausea, vomiting, women- change in libido, clitoral enlargement, menstrual irregularities, men-erectile dysfunction, priapism, prostatic enlargement, hypercholesterolemia, womenhirsutism, men- gynecomastia, oligospermia, hypercalcemia, hyperkalemia, hyperphosphatemia, male pattern baldness, pain at injection site.
Testosterone cypionate/ DepoTestosterone
hormones androgens
Testosterone enanthate/ Delatestryl
hormones androgens
Monitor intake and output ratios, weigh patient twice weekly, and assess patient for edema. Monitor for precocious puberty in boys; breast enlargement, persistent erections, and increased urge to urinate in men; difficulty urinating in elderly men, because prostate enlargement may occur.
206
Rev. 08/21/08
Testosterone gel/ Androgel, Testim
hormones androgens
Monitor intake and output ratios, weigh patient twice weekly, and assess patient for edema. Monitor for breast enlargement, persistent erections, and increased urge to urinate in men. Monitor for difficulty urinating in elderly men, because prostate enlargement may occur. Monitor intake and output ratios, weigh patient twice weekly, and assess patient for edema. Monitor for precocious puberty in boys; breast enlargement, persistent erections, and increased urge to urinate in men; difficulty urinating in elderly men, because prostate enlargement may occur.
Testosterone pellets/ Testopel
hormones androgens
Testosterone transdermal system/ Androderm
hormones androgens
Monitor intake and output ratios, weigh patient twice weekly, and assess patient for edema. Monitor for breast enlargement, persistent erections, and increased urge to urinate in men. Monitor for difficulty urinating in elderly men, because prostate enlargement may occur.
Tetrabenazine/ Xenazine
antichoreas reversible monoamine depleters
Assess signs of Huntington's disease; new or worsening depression or suicidality; signs of neuroleptic malignant syndrome; onset of akathisia; tardive dyskinesia; blood pressure sitting and standing periodically during therapy.
Tetracaine/Pontocaine , Viractin
anesthetics topical local
Assess type, location, and intensity of pain before and a few minutes after administration of anesthetic. Assess integrity of involved skin and mucous membranes before and periodically throughout
Edema, hot flashes, hypertension, liver function test elevation, nausea, vomiting, nocturia, priapism, prostatic enlargement, urinary hesitancy, urinary incontinence, acne, breast pain, change in libido, gynecomastia, hypercholesterolemia, alopecia, dry skin, pruritis, anemia, chronic skin irritation. Deepening of voice, edema, cholestatic jaundice, druginduced hepatitis, liver function test elevation, nausea, vomiting, change in libido, erectile dysfunction, priapism, prostatic enlargement, gynecomastia, hirsutism, oligospermia, hypercholesterolemia, hypercalcemia, hyperkalemia, hyperphosphatemia, male pattern baldness, pain at implantation site. Anxiety, confusion, depression, fatigue, headache, vertigo, edema, hypertension, bleeding, increased appetite, dysuria, erectile dysfunction, priapism, prostatic enlargement, urinary incontinence, application site reactions (e.g. pruritis, blisters, erythema, burning), rash, acne, decreased libido, gynecomastia, paresthesia, chronic skin irritation. Anxiety, fatigue, insomnia, depression, sedation/ somnolence, cognitive defects, dizziness, headache, shortness of breath, hypotension, QTc prolongation, nausea, dysphagia, akathisia, balance difficulty, dysarthria, parkinsonism, unsteady gait, neuroleptic malignant syndrome. mucosal usedecreased or absent gag reflex, topical useburning, edema, irritation, stinging, tenderness, urticaria, allergic reactions including anaphylaxis.
207
Rev. 08/21/08
course of therapy. Tetracycline/ Achromycin, Panmycin, Sumycin, Robitet, Tetracyn anti-infectives Assess patient for infection. Renal and hepatic functions and CBC should be monitored periodically during long-term therapy. Benign intracranial hypertension (increased in children), dizziness, diarrhea, nausea, vomiting, esophagitis, hepatotoxicity, pancreatitis, photosensitivity, rashes, blood dyscrasias, hypersensitivity reactions, superinfection. Dizziness, drowsiness, bradycardia, edema, orthostatic hypotension, thromboembolic events, constipation, rash, photosensitivity, neutropenia, peripheral neuropathy, severe birth defects, hypersensitivity reactions, increased HIV viral load. Seizures, anxiety, headache, insomnia, irritability, arrhythmias, tachycardia, angina, palpitations, nausea, vomiting, anorexia, tremor.
Thalidomide/ Thalomid
immunosuppressan ts
Theophylline/Elixophyl lin, Quibron-T, Theochron, Theo-24, Uniphyl
bronchodilators xanthines
Thiamine/ Biamine, vitamin B1
vitamins water soluble vitamins
Thiethylperazine/Norzi ne, Torecan
antiemetics phenothiazines
Thioguanine/ 6-thioguanine
antineoplastics antimetabolites
Assess patient monthly for initial 3 months and periodically during therapy to detect early signs of peripheral neuropathy. Monitor for signs of hypersensitivity reaction; venous thromboembolism; and side effects periodically during therapy. Assess blood pressure, pulse, respiratory status; intake and output ratios for an increase in diuresis or fluid overload; chest pain and ECG changes; and pulmonary function tests before and periodically during therapy. Assess patient for signs and symptoms of thiamine deficiency; andnutritional status prior to and throughout therapy. Monitor patients receiving IV thiamine for anaphylaxis (wheezing, urticaria, edema). Assess patient for nausea and vomiting prior to and 3060 min following administration. Monitor blood pressure (sitting, standing, lying down), pulse, and respiratory rate; level of sedation; onset of akathisia; tardive dyskinesia; development of neuroleptic malignant syndrome prior to and frequently during initial therapy. CBC and liver function tests should be evaluated periodically throughout course of prolonged therapy. Monitor for bone marrow depression; bleeding; intake
Restlessness, weakness, tightness of the throat, pulmonary edema, respiratory distress, vascular collapse, hypotension, vasodilation, GI bleeding, nausea, cyanosis, pruritus, sweating, tingling, urticaria, warmth, angioedema. Neuroleptic malignant syndrome, sedation, cerebral vascular spasm, extrapyramidal reactions, headache, restlessness, tardive dyskinesia, dry eyes, blurred vision, lens opacities, tinnitus, hypotension, peripheral edema, constipation, dry mouth, altered taste, anorexia, druginduced hepatitis, ileus, urinary retention, photosensitivity, pigment changes, rashes, galactorrhea, agranulocytosis, leucopenia, hyperthermia, trigeminal neuralgia, allergic reactions. Loss of vibratory sense, diarrhea, hepatotoxicity,
208
Rev. 08/21/08
Thioridazine/ Mellaril, Mellaril-S
antipsychotics phenothiazines
Thiotepa/ Thioplex
antineoplastics alkylating agents
and output, appetite, and nutritional intake; increased fatigue, dyspnea, and orthostatic hypotension; signs of infection; and symptoms of tumor lysis syndrome during therapy. Monitor CBC and differential at least weekly, daily in patients with elevated leukocyte counts. Assess mental status; positive (delusions, hallucinations, agitation) and negative (social withdrawal) symptoms of schizophrenia; weight and BMI; blood pressure (sitting, standing, lying), ECG, pulse, and respiratory rate; level of sedation; intake and output ratios and daily weight; onset of akathisia; tardive dyskinesia; and development of neuroleptic malignant syndrome before and periodically during therapy. Monitor vital signs; bone marrow depression; bleeding; intake and output, appetite, and nutritional intake; and symptoms of tumor lysis syndrome prior to and periodically during therapy. Monitor CBC and differential prior to and weekly during therapy and for at least 3 wk after therapy. Assess mental status; positive (delusions, hallucinations, agitation) and negative (social withdrawal) symptoms of schizophrenia; weight and BMI; blood pressure (sitting, standing, lying), ECG, pulse, and respiratory rate; level of sedation; intake and output ratios and daily weight; onset of akathisia; tardive dyskinesia; and development of neuroleptic malignant syndrome before and periodically during therapy.
jaundice, nausea, stomatitis, vomiting, anorexia, hepatic veno-occlusive disease, gonadal suppression, dermatitis, rash, anemia, leukopenia, thrombocytopenia, pancytopenia, hyperuricemia, unsteady gait.
Thiothixene/ Navane
antipsychotics (conventional) thioxanthenes
Neuroleptic malignant syndrome, sedation, extrapyramidal reactions, tardive dyskinesia, blurred vision, dry eyes, lens opacities, pigmentary retinopathy, arrhythmias, QTC prolongation, hypotension, tachycardia, constipation, dry mouth, anorexia, drug-induced hepatitis, ileus, weight gain, urinary retention, priapism, photosensitivity, pigment changes, rashes, galactorrhea, amenorrhea, agranulocytosis, leucopenia, hyperthermia, allergic reactions. Dizziness, headache, blurred vision, throat tightness, anorexia, nausea, stomatitis, vomiting, gonadal suppression, dysuria, urinary retention, alopecia, hives, pruritus, rash, anemia, leukopenia, thrombocytopenia, pain at IV site, pain at site of intracavitary instillation, hyperuricemia, allergic reactions, fever, fatigue, weakness. Neuroleptic malignant syndrome, extrapyramidal reactions, sedation, tardive dyskinesia, seizures, blurred vision, dry eyes, lens opacities, hypotension, tachycardia, non-specific ECG changes, constipation, dry mouth, anorexia, ileus, nausea, urinary retention, photosensitivity, pigment changes, rashes, breast enlargement, galactorrhea, leukocytosis, leucopenia, hyperpyrexia, allergic reactions.
209
Rev. 08/21/08
Thyroid/ Armour thyroid, Thyrar, Thyroid Strong, Westhroid
hormones thyroid preparations
Tiagabine/ Gabitril
anticonvulsants
Ticarcillin/clavulanate/ / Timentin
anti-infectives extended spectrum penicillins
Ticlopidine/ Ticlid
antiplatelet agents platelet aggregation inhibitors
Tigecycline/ Tygacil
anti-infectives glycylcyclines
Assess apical pulse and blood pressure prior to and periodically during therapy. Assess for tachyarrhythmias and chest pain. Monitor thyroid function studies prior to and during therapy. Monitor blood and urine glucose in diabetic patients. Assess location, duration, and characteristics of seizure activity. Assess mental status. Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC); determine use of and reactions to penicillins or cephalosporins; and signs and symptoms of anaphylaxis at beginning of and throughout therapy. Evaluate renal and hepatic function, CBC, serum potassium, and bleeding times prior to and routinely throughout therapy Assess patient for symptoms of stroke periodically throughout therapy. Monitor bleeding time throughout therapy. Monitor CBC with differential and platelet count every 2 wk from the 2nd wk to the end of the 3rd mo of therapy; more frequently if absolute neutrophil count (ANC) is declining or <30% of baseline. Assess patient for infection (vital signs; appearance of wound, sputum, urine, and stool; WBC) at beginning of and throughout therapy. Assess for symptoms of Paget's disease (bone pain, headache, decreased visual and auditory acuity, increased skull size). Monitor alkaline phosphatase prior to and periodically during therapy. Monitor blood pressure and pulse frequently during dose
Insomnia, irritability, headache, arrhythmias, tachycardia, angina pectoris, abdominal cramps, diarrhea, vomiting, hyperhidrosis, hyperthyroidism, menstrual irregularities, weight loss, heat intolerance, accelerated bone maturation in children. Dizziness, drowsiness, nervousness, weakness, chest pain, edema, ataxia, tremors, epistaxis. Seizures, confusion, lethargy, CHF, arrhythmias, pseudomembranous colitis, diarrhea, nausea, hematuria (children only), rashes, urticaria, hypokalemia, hypernatremia, bleeding, blood dyscrasias, increased bleeding time, phlebitis, metabolic alkalosis, hypersensitivity reactions including anaphylaxis, superinfection.
Tiludronate/ Skelid
bone resorption inhibitors biphosphonates
Timolol/ Blocadren
antihypertensives vascular headache
Dizziness, headache, weakness, epistaxis, tinnitus, diarrhea, abnormal liver function tests, anorexia, GI fullness, GI pain, nausea, vomiting, hematuria, rashes, ecchymoses, pruritus, urticaria, agranulocytosis, aplastic anemia, intracerebral bleeding, neutropenia, bleeding, thrombocytopenia, hypercholesterolemia, hypertriglyceridemia. Pseudomembranous colitis, nausea, vomiting, changes in heart rate, vasodilation, injection site reactions, allergic reactions, anorexia, dry mouth, jaundice. Anxiety, drowsiness, cataracts, rhinitis, chest pain, abdominal pain, anorexia, urinary tract infection, flushing, musculoskeletal pain, arthrosis, paresthesia, dry mouth, dysphagia, hypertension, peripheral edema. Fatigue, weakness, arrhythmias, bradycardia,
210
Rev. 08/21/08
suppressants beta blockers
adjustment; orthostatic hypotension; intake and output ratios and daily weight; and evidence of fluid overload period and periodically during therapy. Assess frequency, severity, characteristics, and location of vascular headaches periodically during therapy.
Tinidazole/ Tindamax
antiprotozoals imidazoles
Tinzaparin/ Innohep
anticoagulants antithrombotics
Tioconazole/1Day, Monistat-1Day, Vagistat-1
antifungals (vaginal)
Tiotropium/ Spiriva
bronchodilators anticholinergics
Tipranavir/ Aptivus
antiretrovirals protease inhibitors
Tirofiban/ Aggrastat
antiplatelet agents glycoprotein iib iiia inhibitors
Assess patient for symptoms of infection (discharge, itching); and neurologic status during and after IV infusions prior to and during therapy. Assess for signs of bleeding and hemorrhage; and neurological status frequently for signs of neurological impairment during therapy. Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Assess respiratory status (rate, breath sounds, degree of dyspnea, pulse) before administration and at peak of medication. If paradoxical bronchospasm (wheezing) occurs, withhold medication and notify physician or other health care professional immediately. Assess for change in severity of HIV symptoms and for symptoms of opportunistic infections during therapy. Monitor for hepatitis and sulfa allergy. Monitor viral load and CD4 counts; triglyceride and cholesterol levels; and blood glucose prior to and periodically during therapy. Assess patient for bleeding and signs of thrombocytopenia during therapy. Assess hemoglobin, hematocrit, and platelet count prior to tirofiban
CHF, pulmonary edema, erectile dysfunction, anaphylaxis, arthralgia, back pain, muscle cramps, paresthesia, constipation, diarrhea, nausea, anxiety, depression, dizziness, drowsiness, insomnia, memory loss, mental status changes, nervousness, nightmares, itching, rashes, nasal stuffiness. Dizziness, headache, malaise, constipation, dyspepsia, metallic/bitter taste, vomiting, transient leukopenia/neutropenia. Increased liver function tests, bleeding, thrombocytopenia, ecchymoses, hematoma, local irritation, pain, hypersensitivity reactions. Irritation, vulvovaginal burning.
Glaucoma, paradoxical bronchospasm, heart rate, dry mouth, constipation, urinary difficulty, urinary retention, hypersensitivity reactions including angioedema.
Intracranial hemorrhage, fatigue, headache, hepatotoxicity, abdominal pain, diarrhea, nausea, vomiting, rash ( in women and peds), hyperglycemia, cholesterol, triglycerides, allergic reactions, bleeding, fat redistribution, fever, immune reconstitution syndrome. Dizziness, headache, bradycardia, coronary dissection, edema, vasovagal reaction, nausea, hives, rash, bleeding, thrombocytopenia, leg pain, fever,
211
Rev. 08/21/08
Tizanidine/ Zanaflex
antispasticity agents (centrally acting) adrenergics
therapy, within 6 hr following loading infusion, and at least daily during therapy. Assess muscle spasticity; blood pressure and pulse; and drowsiness, dizziness, and asthenia before and periodically during therapy. Monitor liver function tests before and at 1, 3, and 6 mo of therapy.
hypersensitivity reactions, pelvic pain, sweating.
Tobramycin/Nebcin, TOBI
anti-infectives aminoglycosides
Assess patient for infection; eighth cranial nerve function; intake and output and daily weight to assess hydration status and renal function; and signs of superinfection at beginning of and throughout therapy. ECG, pulse, lungs, and blood pressure should be monitored before and periodically throughout therapy. CBC and WBC with differential and platelet counts should be monitored weekly during the first 3 mo of therapy and frequently thereafter. Observe patient for signs and symptoms of hypoglycemic reactions. Assess patient for allergy to sulfonamides; intake and output ratios and daily weight during therapy. Monitor CBC periodically throughout therapy.
Tocainide/ Tonocard
antiarrhythmics (class IB)
Tolazamide/ Tolamide, Tolinase
antidiabetics sulfonylureas
Tolbutamide/ Orinase, Tol-Tab
antidiabetics sulfonylureas
Observe patient for signs and symptoms of hypoglycemic reactions. Assess patient for allergy to sulfonamides; intake and output ratios and daily weight during therapy. Monitor CBC periodically
Anxiety, depression, dizziness, sedation, weakness, dyskinesia, hallucinations, nervousness, blurred vision, pharyngitis, rhinitis, hypotension, bradycardia, abdominal pain, diarrhea, dry mouth, dyspepsia, constipation, hepatocellular injury, increased liver enzymes, vomiting, urinary frequency, rash, skin ulcers, sweating, back pain, myasthenia, paresthesia, fever, speech disorder. Ototoxicity (vestibular and cochlear)Ophth only : burning, stinging, blurred vision (oint only), Inhalation only tinnitus, voice alteration, nephrotoxicity, hypomagnesemia, muscle paralysis, hypersensitivity reactions. Seizures, changes in mood, drowsiness, hallucinations, headache, restlessness, tremor, blurred vision, pulmonary fibrosis, sinus arrest, CHF, arrhythmias, bradycardia, hypotension, palpitations, tachycardia, anorexia, diarrhea, nausea, vomiting, agranulocytosis. Dizziness, drowsiness, headache, weakness, constipation, cramps, diarrhea, drug-induced hepatitis, dyspepsia, increased appetite, nausea, vomiting, photosensitivity, rashes, hypoglycemia, hyponatremia, aplastic anemia, agranulocytosis, leukopenia, pancytopenia, thrombocytopenia. Dizziness, drowsiness, headache, weakness, constipation, cramps, diarrhea, drug-induced hepatitis, heartburn, increased appetite, nausea, vomiting, photosensitivity, rashes, hypoglycemia, hyponatremia,
212
Rev. 08/21/08
throughout therapy.
Tolcapone/ Tasmar
antiparkinson agents catechol o methyltransferase inhibitors
Assess patient for signs and symptoms of Parkinson's disease and blood pressure periodically throughout therapy. Monitor liver function tests monthly during the first 3 mo of therapy and every 6 wk for the next 6 wk of treatment.
Tolmetin/ Tolectin, Tolectin DS
antirheumatics nonsteroidal anti inflammatory agents
Patients who have asthma, aspirin-induced allergy, and nasal polyps are at increased risk for developing hypersensitivity reactions. Monitor for rhinitis, asthma, and urticaria; pain and range of motion prior to and weekly during therapy. Evaluate BUN, serum creatinine, CBC, and liver function periodically in patients receiving prolonged therapy.
Tolnaftate/ Podactin, QNaftate, Tinactin, Ting
antifungals (topical)
Tolterodine/ Detrol, Detrol LA
urinary tract antispasmodics anticholinergics
Topiramate/ Topamax
anticonvulsants mood stabilizers
Inspect involved areas of skin and mucous membranes before and frequently during therapy. Increased skin irritation may indicate need to discontinue medication. Assess patient for urinary urgency, frequency, and urge incontinence periodically throughout therapy. Assess location, duration, and characteristics of seizure activity; pain location, intensity, duration, and associated symptoms; and manic symptoms throughout therapy. Monitor CBC with differential and platelet count before therapy to determine baseline levels and periodically during therapy. Hepatic function should be monitored periodically
aplastic anemia, agranulocytosis, leukopenia, pancytopenia, thrombocytopenia. Headache, sleep disorder, hallucinations, syncope, orthostatic hypotension, hepatotoxicity, hepatic failure, constipation, diarrhea, anorexia, elevated liver enzymes, nausea, vomiting, hematuria, yellow discoloration of urine, increased sweating, dyskinesia, dystonia. Dizziness, headache, drowsiness, mental depression, sleep disturbances, tinnitus, visual disturbances, edema, hypertension, drug-induced hepatitis, GI bleeding, diarrhea, discomfort, dyspepsia, nausea, vomiting, constipation, flatulence, renal failure, exfoliative, dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, rashes, prolonged bleeding time, muscle weakness, allergic reactions including anaphylaxis. Burning, itching, local hypersensitivity reactions, redness, stinging.
Headache, dizziness, blurred vision, dry eyes, dry mouth, constipation, dyspepsia.
Increased seizures, dizziness, drowsiness, fatigue, impaired concentration/memory, nervousness, psychomotor slowing, speech problems, sedation, abnormal vision, diplopia, nystagmus, nausea, weight loss, ataxia, paresthesia, suicide attempt, aggressive reaction, agitation, anxiety, cognitive disorders, confusion, depression, malaise, mood problems, abdominal pain, anorexia,
213
Rev. 08/21/08
Topotecan/ Hycamtin
antineoplastics enzyme inhibitors
Toremifene/ Fareston
antineoplastics antiestrogens
throughout therapy. Evaluate serum bicarbonate prior to and periodically during therapy. Monitor vital signs; bone marrow depression; bleeding; signs of infection; Nausea and vomiting; IV site frequently for extravasation during therapy. Monitor CBC with differential and platelet count prior to administration and frequently during therapy. Monitor liver function. Assess for an increase in bone or tumor pain. Gynecologic examinations should be done regularly; may cause variations in Papanicolaou and vaginal smears. Monitor CBC, platelets, and calcium levels prior to and throughout therapy. Monitor hepatic function tests periodically during therapy. Assess fluid status; daily weight, intake and output ratios, amount and location of edema, lung sounds, skin turgor, and mucous membranes; blood pressure and pulse; anorexia, nausea, vomiting, muscle cramps, paresthesia, and confusion; tinnitus and hearing loss; and allergy to sulfonamides during therapy. Monitor electrolytes, renal and hepatic function, serum glucose, and uric acid levels before and periodically during therapy. Observe patient for signs and symptoms of anaphylaxis; infusional toxicity during or within 48 hr of infusion; and signs of hypothyroidism periodically during therapy. Monitor CBC prior to and at least weekly for at least 1012 wks or until severe cytopenias have resolved. Monitor serum
constipation, dry mouth, kidney stones, tremor, fever, leukopenia. Headache, fatigue, weakness, dyspnea, abdominal pain, diarrhea, nausea, vomiting, anorexia, constipation, increased liver enzymes, stomatitis, alopecia, anemia, leukopenia, thrombocytopenia, arthralgia.
Torsemide/ Demadex
antihypertensives loop diuretics
Depression, dizziness, headache, lethargy, blurred vision, cataracts, corneal keratopathy, dry eyes, glaucoma, CHF, MI, pulmonary embolism, angina, arrhythmias, edema, thrombophlebitis, nausea, elevated liver enzymes, vomiting, vaginal discharge, vaginal bleeding, sweating, hypercalcemia, anemia, hot flashes, tumor flare. Dizziness, headache, nervousness, hearing loss, tinnitus, hypotension, constipation, diarrhea, dry mouth, dyspepsia, nausea, vomiting, excessive urination, photosensitivity, rash, hyperglycemia, hyperuricemia, dehydration, hypocalcemia, hypochloremia, hypokalemia, hypomagnesemia, hyponatremia, hypovolemia, metabolic alkalosis, arthralgia, muscle cramps, myalgia, increased BUN.
Tositumomab (I 131 tositumomab)/ Bexxar
antineoplastics monoclonal antibodies radiolabled monoclonal antibodies
Dizziness, drowsiness, headache, weakness, edema, hypotension, abdominal pain, diarrhea, nausea, vomiting, hypothyroidism, neutropenia, thrombocytopenia, anemia, weight loss, arthralgia, back pain, myalgia, neck pain, hypersensitivity reactions including anaphylaxis, infusional toxicity, fever, pain,
214
Rev. 08/21/08
Trace metal combination additive/ Concentrated Multiple Trace Element, ConTE-PAK-4, M.T.E.4, M.T.E.-4 Concentrated, M.T.E.-5, M.T.E.-5 Concentrated, M.T.E.6, M.T.E.-6 Concentrated, M.T.E.-7, MulTE-PAK4, MulTE-PAK-5, Multiple Trace Element, Multiple Trace Element Neonatal, Multiple Trace Element Pediatric, Neotrace 4, PedTE-PAK-4, Pedtrace4, P.T.E.-4, P.T.E.-5
mineral electrolyte replacements supplements
Tramadol/ Ultram, Ultram ER
Analgesics (centrally acting)
creatinine levels immediately prior to administration. Assess nutritional status by 24-hr recall prior to therapy. Monitor patient for signs and symptoms of trace metal deficiencies prior to and throughout therapy. Chromiumglucose intolerance, ataxia, peripheral neuropathy, confusion. Copper leukopenia, neutropenia, anemia, iron deficiency, skeletal abnormalities, defective tissue formation. Iodineimpaired thyroid function, goiter, cretinism. Manganesenausea, vomiting, weight loss, dermatitis, changes in hair. Molybdenumtachycardia, tachypnea, headache, night blindness, nausea, vomiting, edema, lethargy, disorientation, coma, hypouricemia, hypouricosuria. Selenium cardiomyopathy, muscle pain, kwashiorkor, Keshan disease. Zincdiarrhea, apathy, depression, anorexia, hypogonadism, growth retardation, anemia, hepatosplenomegaly, impaired wound healing, decreased sense of taste and smell. Assess type, location, and intensity of pain before and 23 hr (peak) after administration. Assess blood pressure and respiratory rate; bowel function; seizures; serotonin syndrome; serotonin syndrome; neuromuscular aberrations; gastrointestinal symptoms before and periodically during administration.
secondary malignancies.
ChromiumCOMA, Seizures, GI ulceration, hepatic damage, nausea, renal damage, vomiting, Copperbehavioral changes, diarrhea, peripheral edema, photophobia, progressive marasmus, weakness, Iodineacneiform skin lesions, headache, increased salivation, metallic taste, parotitis, runny nose, sneezing, sore mouth, swelling of eyelids, Manganese anorexia, apathy, gait disturbances, headache, erectile dysfunction, irritability, speech difficulties, Molybdenumgout-like syndrome, Seleniumgarliclike breath, garlic-like sweat, GI discomfort, hair loss, mental depression, metallic taste, nervousness, vomiting, weak nails, Zincblurred vision, hypotension, jaundice, loss of consciousness, oliguria, pulmonary edema, tachycardia, toxicity poorly defined but may include hypothermia, vomiting.
Trandolapril/ Mavik
antihypertensives ace inhibitors
Monitor BP, pulse, and signs of angioedema. Monitor
Seizures, dizziness, headache, somnolence, anxiety, CNS stimulation, confusion, coordination disturbance, euphoria, malaise, nervousness, sleep disorder, weakness, visual disturbances, vasodilation, constipation, nausea, abdominal pain, anorexia, diarrhea, dry mouth, dyspepsia, flatulence, vomiting, menopausal symptoms, urinary retention/frequency, pruritus, sweating, hypertonia, physical dependence, psychological dependence, tolerance. Weakness, cough, hypotension, hyperuricemia,
215
Rev. 08/21/08
Tranexamic acid/ Cyklokapron
hemostatic agents antifibrinolytics plasminogen inactivators
Tranylcypromine/ Parnate
antidepressants monamine oxidase inhibitors
weight and assess patient routinely for resolution of fluid overload. Monitor renal function. Observe site of surgery for excessive bleeding. Patients taking tranexamic acid for more than several days should have ophthalmologic examinations to detect visual abnormalities prior to and at regular intervals during and after therapy. Assess mental status, mood changes, and anxiety level; intake and output ratios and daily weight; peripheral edema and urinary retention; blood pressure and pulse rate before and frequently during therapy. Assess hepatic function periodically during prolonged or high-dose therapy. Monitor serum glucose closely in diabetic patients Assess for infusion-related symptoms; severe reactions; signs and symptoms of HF; and signs of pulmonary hypersensitivity reactions prior to and frequently during therapy. Assess mental status, suicidal tendencies, blood pressure and pulse rate before and during initial therapy. Monitor patient for signs of improvement in pulmonary arterial hypertension and infusion site reactions periodically throughout therapy. Monitor patient for retinoic acidacute promyelocytic leukemia (RA-APL) syndrome, and risk is increased if leukocytosis occurs during therapy. Monitor WBC frequently during therapy; may cause rapidly progressing leukocytosis. Monitor hepatic function tests;
diarrhea, dyspepsia, impaired renal function, rashes, hyperkalemia, hypocalcemia, myalgia, angioedema. Dizziness, visual abnormalities, hypotension, thromboembolism, thrombosis, diarrhea, nausea, vomiting.
Trastuzumab/ Herceptin
antineoplastics monoclonal antibodies
Trazodone/Trialodine
Antidepressant
Seizures, confusion, dizziness, drowsiness, headache, insomnia, restlessness, tremor, paresthesia, weakness, blurred vision, tinnitus, hypertensive crisis, edema, orthostatic hypotension, tachycardia, abdominal pain, anorexia, rashes, constipation, diarrhea, dry mouth, hepatitis, nausea, sexual dysfunction, urinary retention, agranulocytosis, leukopenia, muscle spasm, thrombocytopenia, alopecia. Abdominal pain, anorexia, diarrhea, nausea, vomiting, rash, back pain, chills, fever, infection, pain, interstitial pneumonitis, pulmonary edema, pulmonary fibrosis, arrhythmias, HF, hypersensitivity reactions. drowsiness, confusion, hypotension, dry mouth, constipation
Treprostinil/ Remodulin
vasodilators prostacyclins
Tretinoin (oral)/ Vesanoid
antineoplastics retinoids
Dizziness, headache, vasodilation, hypotension, edema, diarrhea, nausea, rash, pruritus, flushing, infusion site pain/reaction, jaw pain. Seizures, anxiety, confusion, depression, dizziness, fatigue, headache, insomnia, malaise, pseudotumor cerebri, weakness, cardiac failure, MI, stroke, arrhythmias, chest discomfort, edema, hypertension, hypotension, peripheral edema, phlebitis, renal insufficiency, disseminated intravascular
216
Rev. 08/21/08
Cholesterol and triglyceride concentrations frequently during therapy. Tretinoin (topical)/ Altinac, Avita, Retin-A, Retin-A Micro, Renova, vitamin A Acid Triamcinolone/ Azmacort antiacne agents retinoids Assess skin prior to and periodically during therapy. Transient worsening of acne may occur at initiation of therapy. Monitor respiratory status and lung sounds; signs of adrenal insufficiency; withdrawal symptoms; and growth rate in children during therapy. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic therapy. Monitor degree of nasal stuffiness, amount and color of nasal discharge, and frequency of sneezing. Patients on long-term therapy should have periodic otolaryngologic examinations to monitor nasal mucosa and passages for infection or ulceration Assess patient for signs of adrenal insufficiency; intake and output ratios and daily weights; peripheral edema, steady weight gain, rales/ crackles, or dyspnea prior to and periodically throughout therapy. Monitor serum electrolytes and glucose. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal axis suppression in systemic and chronic topical therapy. Assess affected skin prior to and daily during therapy. Note degree of inflammation and pruritus. Periodic adrenal function tests may be ordered to assess degree of hypothalamic-pituitaryadrenal (HPA) axis suppression in chronic topical therapy if suspected.
coagulation, hemorrhage, leukocytosis, weight gain, weight loss, paresthesias, fever, infections, pain. Photosensitivity, redness, blistering, edema, crusting, hyperpigmentation, hypopigmentation. Headache, rash, pharyngitis, dysphonia, oropharyngeal fungal infections, sinusitis, bronchospasm, wheezing, abdominal pain, diarrhea, dry mouth, vomiting, adrenal suppression, decreased growth (children), weight gain, vaginal moniliasis, back pain, myalgia, flu-like syndrome.
anti inflammatories steroidal corticosteroids
Triamcinolone (nasal)/ Nasacort AQ, TriNasal
anti inflammatories steroidal
Headache, epistaxis, nasal burning, nasal irritation, nasopharyngeal fungal infection, otitis media, pharyngitis, rhinitis, sinusitis, sneezing, vomiting, adrenal suppression (increased dose, long-term therapy only), cough. Depression, euphoria, hypertension, peptic ulceration, anorexia, nausea, vomiting, acne, decreased wound healing, ecchymoses, fragility, hirsutism, petechiae, adrenal suppression, hyperglycemia, fluid retention, hypokalemia, thromboembolism, thrombophlebitis, weight gain, weight loss, muscle wasting, osteoporosis, aseptic necrosis of joints, muscle pain, cushingoid appearance, increased susceptibility to infection. Allergic contact dermatitis, atrophy, burning, dryness, edema, folliculitis, hypersensitivity reactions, hypertrichosis, hypopigmentation, irritation, maceration, miliaria, perioral dermatitis, secondary infection, striae, adrenal suppression
Triamcinolone (systemic)/ Aristospan, Kenalog, Trivaris
anti inflammatories steroidal (intermediateacting) immunosuppressan ts
Triamcinolone (topical)/ Aristocort, DeltaTritex, Flutex, Kenalog, Kenonel
anti inflammatories steroidal corticosteroids
217
Rev. 08/21/08
Triamterene/ Dyrenium
diuretics (potassiumsparing)
Triazolam/ Halcion
sedative/hypnotics benzodiazepines
Trifluoperazine/ Stelazine
antipsychotics (conventional) phenothiazines
Trihexyphenidyl/ Artane, Trihexane, Trihexy
antiparkinson agents anticholinergics
Monitor intake and output ratios and daily weight; signs and symptoms of hypokalemia or hyperkalemia during therapy. Evaluate serum potassium levels; BUN, serum creatinine, and electrolytes; platelet count and total and differential leukocyte count prior to and routinely during therapy. Assess sleep patterns prior to and periodically throughout therapy. Assess CNS effects and risk of falls in elderly. Prolonged highdose therapy may lead to psychological or physical dependence. Assess mental status and degree of anxiety; weight and BMI; positive (hallucinations, delusions, agitation) and negative (social withdrawal) symptoms of schizophrenia; blood pressure (sitting, standing, lying), ECG, pulse, and respiratory rate; level of sedation; intake and output ratios and daily weight; onset of akathisia; tardive dyskinesia; and development of neuroleptic malignant syndrome prior to and periodically during therapy. Assess parkinsonian and extrapyramidal symptoms; intake and output ratios and assess patient for urinary retention prior to and throughout therapy. Assess patient for urinary tract infection or other signs of infection; and intake and output ratios at beginning of and throughout therapy. Monitor CBC and urinalysis periodically throughout therapy. Assess for infection; IV site; allergy to sulfonamides; intake and output ratios at beginning of and during therapy. Monitor CBC and
Dizziness, arrhythmias, nausea, vomiting, erectile dysfunction, bluish urine, nephrolithiasis, photosensitivity, hyperkalemia, hyponatremia, blood dyscrasias, muscle cramps, allergic reactions.
Dizziness, excessive sedation, hangover, headache, blurred vision, constipation, diarrhea, nausea, vomiting, rashes, physical dependence, psychological dependence, tolerance, confusion, hallucinations. Neuroleptic malignant syndrome, extrapyramidal reactions, sedation, tardive dyskinesia, dry eyes, blurred vision, lens opacities, hypotension, tachycardia, constipation, anorexia, dry mouth, hepatitis, ileus, urinary retention, priapism, photosensitivity, pigment changes, rashes, galactorrhea, amenorrhea, agranulocytosis, leucopenia, hyperthermia, allergic reactions.
Trimethoprim/ Primsol, Proloprim, Trimpex
anti-infectives folate antagonists
Dizziness, nervousness, confusion, drowsiness, headache, psychoses, weakness, blurred vision, mydriasis, orthostatic hypotension, tachycardia, dry mouth, nausea. Altered taste, epigastric discomfort, glossitis, nausea, vomiting, drug-induced hepatitis, pruritus, rash, megaloblastic anemia, neutropenia, thrombocytopenia, fever. Pseudomembranous colitis, hepatic necrosis, nausea, vomiting, toxic epidermal necrolysis, rashes, aplastic anemia, agranulocytosis,
Trimethoprim/ sulfamethoxazole// Bactrim, Bactrim DS, Cofatrim, Cotrim, Cotrim
anti-infectives antiprotozoals folate antagonists sulfonamides
218
Rev. 08/21/08
DS, Septra, Septra DS, SMZ/TMP, Sulfatrim, Sulfatrim DS, TMP/SMX, TMP/SMZ Trimipramine/ Surmontil
urinalysis periodically during therapy.
phlebitis at IV site, allergic reactions including erythema multiforme, Stevens-Johnson syndrome.
antidepressants tricyclic antidepressants
Monitor blood pressure and pulse; ECG; mental status and affect; suicidal tendencies; bipolar disorder before and during initial therapy. Assess leukocyte and differential blood counts, liver function, and serum glucose before and periodically during therapy. Assess symptoms (rhinitis, conjunctivitis, hives); and lung sounds and character of bronchial secretions prior to and periodically throughout therapy. Assess patient for symptoms of prostate cancer; signs and symptoms of anaphylaxis; bone pain, neuropathy, hematuria, urethral or bladder outlet obstruction prior to and throughout therapy. Monitor response by measuring serum testosterone and prostate-specific antigen levels periodically during therapy. Monitor voiding pattern and intake and output ratios.
Triprolidine
antihistamines
Triptorelin/Trelstar Depot
antineoplastics hormones
Lethargy, sedation, blurred vision, dry eyes, dry mouth, arrhythmias, hypotension, ECG changes, constipation, hepatitis, paralytic ileus, increased appetite, weight gain, urinary retention, libido, photosensitivity, changes in blood glucose , gynecomastia, blood dyscrasias. Sedation, dizziness, excitation, blurred vision, arrhythmias, hypertension, hypotension, palpitations, dry mouth, constipation, urinary hesitancy, urinary retention. Dizziness, emotional lability, fatigue, headache, insomnia, hypertension, diarrhea, vomiting, erectile dysfunction, urinary retention, urinary tract infection, pruritus, anemia, injection site pain, musculoskeletal pain, allergic reactions including anaphylaxis and angioedema.
Trospium/ Sanctura, Sanctura XR
urinary tract antispasmodics antimuscarinics
Headache, constipation, dry mouth, urinary retention, urinary tract infection.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Urokinase/ Abbokinase
thrombolytics plasminogen activators
Assess patient carefully for bleeding every 15 min during the 1st hr of therapy, every 1530 min during the next 8 hr, and at least every 4 hr; neurologic status; and hypersensitivity reaction for the duration of therapy. Frank bleeding may occur from sites of invasive procedures or from body orifices. Monitor vital signs, including temperature, continuously for myocardial
Intracranial hemorrhage, epistaxis, gingival bleeding, bronchospasm, hemoptysis, reperfusion arrhythmias, hypotension, recurrent ischemia/thromboembolism, GI bleeding, nausea, retroperitoneal bleeding, vomiting, GU tract bleeding, ecchymoses, flushing, urticaria, bleeding, hemorrhage at injection site, phlebitis at injection site, musculoskeletal pain, allergic
219
Rev. 08/21/08
infarction and at least every 4 hr during therapy for other indications.
reactions including anaphylaxis, fever
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Valacyclovir/ Valtrex
antivirals
Valdecoxib/ Bextra
nonsteroidal anti inflammatory agents nonopioid analgesics cox 2 inhibitors
Valerian/ Amantilla, AllHeal, Baldrian, Baldrianwurzel, Belgium Valerian, Common Valerian, Fragrant Valerian, Garden Heliotrope, Garden Valerian, Indian Valerian, Mexican Valerian, Pacific Valerian, Tagara, Valeriana, Valeriana officinalis, Valerianae radix, Valeriana rhizome, Valeriane Valganciclovir/ Valcyte
antianxiety agents sedative/hypnotics
Assess lesions before and daily during therapy. Monitor patient for signs of thrombotic thrombocytic purpura/hemolytic uremic syndrome. Patients who have asthma, aspirin-induced allergy, and nasal polyps are at increased risk for developing hypersensitivity reactions. Assess for rhinitis, asthma, and urticaria. Assess pain, range of motion, and degree of swelling in affected joints prior to and 23 hr following administration. Assess degree of anxiety and level of sedation; sleep patterns; and loss of balance prior to and periodically throughout therapy.
Headache, dizziness, weakness, nausea, abdominal pain, anorexia, constipation, diarrhea, thrombotic thrombocytopenic purpura/ hemolytic uremic syndrome Increased blood pressure, edema, fluid retention, GI bleeding, abdominal pain, rash, anemia, allergic reactions including anaphylactoid reactions, anaphylaxis, angioedema, Stevens-Johnson syndrome.
Drowsiness, headache, Benzodiazepine-like withdrawal symptoms with discontinuation after long-term use.
antivirals
Valproate sodium/ Depacon
anticonvulsants vascular headache suppressants
Assess for signs of infection and bleeding prior to and throughout therapy. Diagnosis of CMV retinitis should be determined by ophthalmoscopy prior to treatment with ganciclovir. Monitor BUN and serum creatinine at least once every 2 wk throughout therapy. Monitor neutrophil and platelet count closely throughout therapy. Assess location, duration, and characteristics of seizure activity. Assess
Seizures, headache, insomnia, agitation, confusion, dizziness, hallucinations, psychosis, sedation, abdominal pain, diarrhea, nausea, vomiting, renal impairment, neutropenia, paresthesia, thrombocytopenia, anemia, aplastic anemia, bone marrow depression, pancytopenia, ataxia, peripheral neuropathy, fever, hypersensitivity reactions, infections. Agitation, dizziness, headache, insomnia, sedation, confusion, depression, peripheral edema,
220
Rev. 08/21/08
Valproic acid/ Depakene
anticonvulsants vascular headache suppressants
Valsartan/ Diovan
antihypertensives angiotensin ii receptor antagonists
Vancomycin/ Lyphocin, Vancocin, Vancoled
anti-infectives
mood, ideation, and behavior frequently. Monitor frequency of migraine headaches. Monitor hepatic function (LDH, AST, ALT, and bilirubin) and serum ammonia concentrations prior to and periodically during therapy. Monitor CBC, platelet count, and bleeding time prior to and periodically during therapy. Assess location, duration, and characteristics of seizure activity. Assess mood, ideation, and behavior frequently. Monitor frequency of migraine headaches. Monitor hepatic function (LDH, AST, ALT, and bilirubin) and serum ammonia concentrations prior to and periodically during therapy. Monitor CBC, platelet count, and bleeding time prior to and periodically during therapy. Assess blood pressure (lying, sitting, standing) and pulse; signs of angioedema; daily weight; and resolution of fluid overload throughout therapy. Monitor renal function. Assess patient for infection; IV site; blood pressure; eighth cranial nerve function; intake and output ratios and daily weight; and signs of superinfection at beginning of and throughout therapy.
visual disturbances, hepatotoxicity, pancreatitis, abdominal pain, anorexia, anorexia, diarrhea, indigestion, nausea, vomiting, constipation, increased appetite, alopecia, rashes, weight gain, leukopenia, thrombocytopenia, hyperammonemia, hypothermia, tremor, ataxia. Agitation, dizziness, headache, insomnia, sedation, confusion, depression, peripheral edema, visual disturbances, hepatotoxicity, pancreatitis, abdominal pain, anorexia, anorexia, diarrhea, indigestion, nausea, vomiting, constipation, increased appetite, alopecia, rashes, weight gain, leukopenia, thrombocytopenia, hyperammonemia, hypothermia, tremor, ataxia. Dizziness, fatigue, headache, hypotension, edema, rhinitis, sinusitis, pharyngitis, hyperkalemia, abdominal pain, diarrhea, nausea, impaired renal function, arthralgia, back pain, angioedema. Ototoxicity, hypotension, nausea, vomiting, nephrotoxicity, rashes, eosinophilia, leucopenia, phlebitis, back and neck pain, hypersensitivity reactions including anaphylaxis, chills, fever, "red man" syndrome (with rapid infusion), superinfection. Headache, amnesia, dizziness, hearing loss, vision loss, rhinitis, sinusitis, dyspepsia, nausea, priapism, flushing, flu syndrome. attention span, anxiety, depression, insomnia, irritability, dizziness, restlessness, diarrhea, gingivitis, nausea, flushing, hyperhydrosis, arthralgia, back pain, musculoskeletal pain. Bronchospasm, rash, allergic reactions including
Vardenafil/ Levitra
erectile dysfunction agents phosphodiesterase type 5 inhibitors smoking deterrents nicotine agonists
Varenicline/ Chantix
Determine erectile dysfunction before administration. Vardenafil has no effect in the absence of sexual stimulation. Assess for desire to stop smoking. Assess for nausea.
Vecuronium/ Norcuron
neuromuscular blocking agents
Assess respiratory status; ECG, heart rate, and blood
221
Rev. 08/21/08
nondepolarizing
Verapamil/ ApoVerap, Calan, Calan SR, CoveraHS, Isoptin, Isoptin SR, Verelan, Verelan PM
antianginals antiarrhythmics (class IV) antihypertensives vascular headache suppressants calcium channel blockers
pressure; residual muscle weakness and respiratory distress; infusion site throughout therapy and administration. Monitor blood pressure and pulse before therapy, during dosage titration, and periodically throughout therapy. Monitor ECG periodically during prolonged therapy. Monitor intake and output ratios and daily weight; signs of CHF; location, duration, intensity, and precipitating factors of patient's anginal pain during therapy. Monitor serum potassium periodically. Monitor renal and hepatic functions periodically during long-term therapy.
anaphylaxis.
Vitamin B complex with vitamin C/ AlbeeT, Albee with C, Arcobee with C, BComplex/Vitamin C, Beminal, Econo B & C, Enviro-Stress, Farbee with Vitamin C, Genbee with C, High Potency N-Vites, Nion B Plus C, Probec-T, Sublingual B Total Liquid, Surbex T, Surbu-Gen-T, SurplexT, Therapeutic B Complex with C, ThexForte, T-Vites, Vicon-C, Viogen-C, Vita-Bee with C, Key Plex, Neurodep, Vicam
vitamins water soluble vitamins
Assess patient for signs of vitamin deficiency and anaphylaxis throughout therapy.
Abnormal dreams, anxiety, confusion, drowsiness, headache, blurred vision, disturbed equilibrium, epistaxis, tinnitus, cough, dyspnea, shortness of breath, arrhythmias, CHF, bradycardia, chest pain, hypotension, palpitations, peripheral edema, syncope, tachycardia, abnormal liver function studies, anorexia, urinary frequency, dermatitis, erythema multiforme, flushing, increased sweating, rash, thrombocytopenia, weight gain, joint stiffness, muscle cramps, paresthesia, tremor, Stevens-Johnson syndrome. Bright-yellow urine, anaphylaxis (vitamin B1thiamine), allergic reactions to preservatives.
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Warfarin/Coumadin
anticoagulants coumarins
Assess for signs of bleeding and hemorrhage; evidence of additional or increased thrombosis during therapy. PT, INR and other clotting factors should be monitored frequently during therapy.
Cramps, nausea, dermal necrosis, bleeding, fever.
222
Rev. 08/21/08
Name: Generic/Trade
Dose, Route and Times
Drug Classification
Dosage Calculations
Indications for Use in this Client
Assessments to Done Prior Administration
be to
Common Side Effects
Zafirlukast/Accolate
antiasthmatics bronchodilators leukotriene antagonists
Assess lung sounds and respiratory function before and periodically during therapy. Monitor liver function periodically during therapy. Assess patient for change in severity of symptoms of AIDS and for symptoms of opportunistic infections; signs and symptoms of peripheral neuropathy; and symptoms of pancreatitis throughout therapy. Monitor serum amylase, lipase, triglyceride, and calcium throughout therapy. Monitor viral load and CD4 levels prior to and periodically throughout therapy. Monitor liver function. Assess mental status, sleep patterns, and potential for abuse; alertness at time of peak effect; pain during therapy. Assess patient for signs and symptoms of influenza (fever, headache, myalgia, cough, sore throat) before administration. Assess level of pain; mental status; signs of meningitis prior to and periodically during therapy. Monitor serum CK levels every other week for the first month, monthly thereafter. Assess patient for change in severity of symptoms of HIV and for symptoms of opportunistic infections during therapy. Monitor viral load and CD4 counts prior to and periodically during therapy. Monitor CBC every 2 wk during the first 8 wk of therapy in patients with advanced HIV disease, and decrease to every 4 wk after the first 2 mo if zidovudine
Zalcitabine/ ddC, Dideoxycitidine, HIVID
antiretrovirals nucleoside reverse transcriptase inhibitors
Zaleplon/ Sonata
sedative/hypnotics
Zanamivir/ Relenza
antivirals neuramidase inhibitors
Ziconotide/ Prialt
analgesics n type calcium channel blockers
Zidovudine/ AZT, azidothymidine, Retrovir
antiretrovirals nucleoside reverse transcriptase inhibitors
headache, dizziness, weakness, hepatotoxicity, abdominal pain, diarrhea, dyspepsia, nausea, vomiting, arthralgia, back pain, myalgia, Churg-Strauss syndrome, fever, infection, pain Confusion, dizziness, fatigue, headache, impaired concentration, pharyngitis, cardiomyopathy, CHF, chest pain, pancreatitis/ hepatomegaly/steatosis, oral ulcers, abdominal pain, anorexia, diarrhea, dysphagia, esophageal ulcerations increased liver enzymes, nausea, vomiting, dermatitis, pruritus, rash, lactic acidosis, leukopenia, neutropenia, arthralgia, myalgia, peripheral neuropathy, hypersensitivity reactions, weight loss. Abnormal vision, ear pain, epistaxis, hearing sensitivity, ocular pain, altered sense of smell, peripheral edema, abdominal pain, anorexia. Seizures, abnormal behavior, agitation, delirium, hallucinations, nightmares, bronchospasm, allergic reactions. Meningitis, confusion, dizziness, drowsiness, headache, impaired memory, weakness, nystagmus, nausea, hypertonia, urinary retention, abnormal gait, ataxia. Seizures, headache, weakness, anxiety, confusion, decreased mental acuity, dizziness, insomnia, mental depression, restlessness, syncope, abdominal pain, diarrhea, nausea, anorexia, drug-induced hepatitis, dyspepsia, oral mucosa pigmentation, vomiting, nail pigmentation, gynecomastia, anemia, granulocytopenia, pure red-cell aplasia,
223
Rev. 08/21/08
Zileuton/ Zyflo CR
bronchodilators leukotriene antagonists
is well tolerated or monthly during the first 3 mo and every 3 mo thereafter. Assess lung sounds and respiratory function prior to and periodically during therapy. Monitor ALT prior to therapy, monthly for the first 3 mo, every 2 mo for the 1st yr of therapy, and periodically thereafter.
thrombocytosis, back pain, myopathy, tremor. Headache, dizziness, insomnia, malaise, nervousness, somnolence, weakness, conjunctivitis, chest pain, abdominal pain, constipation, dyspepsia, flatulence, increased liver enzymes, nausea, vomiting, urinary tract infection, vaginitis, pruritus, arthralgia, myalgia, neck pain, hypertonia, fever, lymphadenopathy. Gastric irritation (oral use only), nausea, vomiting.
Zinc sulfate/ Orazinc, Verazinc, Zinc 220, Zincate, Zinkaps
mineral electrolyte replacements supplements trace metals
Ziprasidone/ Geodon
antipsychotics mood stabilizers piperazine derivatives
Zoledronic acid/ Reclast, Zometa
bone resorption inhibitors electrolyte modifiers hypocalcemics biphosphonates
Monitor progression of zinc deficiency symptoms (impaired wound healing, growth retardation, decreased sense of taste, decreased sense of smell) during therapy. Monitor patient's mental status; weight and BMI; blood pressure (sitting, standing, lying) and pulse rate; rash; onset of akathisia; tardive dyskinesia; frequency and consistency of bowel movements; and development of neuroleptic malignant syndrome prior to and periodically during therapy. Monitor intake and output ratios; acute-phase reaction (fever, mylagia, flu-like symptoms, headache, arthralgia); symptoms of hypercalcemia; evidence of hypocalcemia; Paget's disease during therapy. Monitor serum creatinine prior to each treatment.
Neuroleptic malignant syndrome, seizures, dizziness, drowsiness, restlessness, extrapyramidal reactions, syncope, tardive dyskinesia, cough/runny nose, prolonged QT interval, orthostatic hypotension, constipation, diarrhea, nausea, dysphagia, rash, urticaria.
Zolmitriptan/ Zomig, Zomig- ZMT
vascular headache suppressants five ht1 agonists
Assess pain location, intensity, duration, and associated symptoms (photophobia, phonophobia, nausea, vomiting) during migraine attack.
Agitation, anxiety, confusion, insomnia, conjunctivitis, hypotension, chest pain, leg edema, abdominal pain, constipation, diarrhea, nausea, vomiting, dysphagia, renal failure, pruritus, rash, hypophosphatemia, hypocalcemia, hypokalemia, hypomagnesemia, anemia, musculoskeletal pain, osteonecrosis, fever, flu-like syndrome. Dizziness, drowsiness, vertigo, weakness, throat pain/tightness/pressure, chest pain/pressure/ tightness/ heaviness, hypertension, palpitations, dry mouth, dyspepsia, dysphagia, nausea, sweating, warm/cold sensation, myalgia,
224
Rev. 08/21/08
Zolpidem / Ambien
Sedative, hypnotics
For pain, mental status, sleep patterns, and potential for abuse prior to administration; alertness at time of peak effect
Zonisamide/ Zonegran
anticonvulsants sulfonamides
Monitor frequency, duration, and characteristics of seizures; development of skin rash; and allergy to sulfa drugs during therapy. Assess patient for immunosuppressant medications or reactions to previous vaccines. Administration may result in a more extensive vaccineassociated rash or disseminated disease in immunocompromised patients.
Zoster vaccine live/ Zostavax
vaccines/immunizin g agents active immunizer
myasthenia, hypesthesia, paresthesia, feeling of heaviness, pain. abnormal thinking, amnesia, behavior changes, daytime drowsiness, dizziness, "drugged" feeling, hallucinations, sleep-driving; nausea, vomiting; physical dependence, psychological dependence, tolerance Drowsiness, fatigue, amblyopia, tinnitus, allergic reactions including StevensJohnson syndrome, abnormal gait, hyperasthesia, incoordination, tremor. Swelling, redness, pain.
225
Rev. 08/21/08
Anda mungkin juga menyukai
- Drug StudyDokumen8 halamanDrug StudyJheryck SabadaoBelum ada peringkat
- DrugsDokumen20 halamanDrugsLee Won100% (1)
- Drug Study Feu NRMF IcuDokumen9 halamanDrug Study Feu NRMF IcuAnne Genesis V. PinedaBelum ada peringkat
- Drugs For Clinicals 1Dokumen4 halamanDrugs For Clinicals 1justjesko0lBelum ada peringkat
- Drug Study Generic Name/ Trade Name Dosage/ Frequency Indication Contraindication Side Effects Nursing ResponsibilitiesDokumen8 halamanDrug Study Generic Name/ Trade Name Dosage/ Frequency Indication Contraindication Side Effects Nursing ResponsibilitiesTrojangBaboyBelum ada peringkat
- Drug Study (MS)Dokumen9 halamanDrug Study (MS)Kristine GallardoBelum ada peringkat
- Drug Study 2Dokumen3 halamanDrug Study 2Steve tarucBelum ada peringkat
- Felodipine Nursing ResponsibilitiesDokumen22 halamanFelodipine Nursing ResponsibilitiesPaula Xavier AlfalahiBelum ada peringkat
- Drug Study ICUDokumen4 halamanDrug Study ICUArthadian De PeraltaBelum ada peringkat
- Pharmacological: Drug Features Therapeutic Effects Nursing Responsibilities Indication Contraindication Desired UntowardDokumen7 halamanPharmacological: Drug Features Therapeutic Effects Nursing Responsibilities Indication Contraindication Desired UntowardyannahmaeBelum ada peringkat
- Drug Study Index CardDokumen4 halamanDrug Study Index CardPatricia OrtegaBelum ada peringkat
- Drug StudyDokumen9 halamanDrug Studykcbabee0333% (3)
- Nicardipine (: ClassificationDokumen14 halamanNicardipine (: ClassificationWilliam CiferBelum ada peringkat
- Drug Study GuideDokumen9 halamanDrug Study GuideSh3meeBelum ada peringkat
- POC Drug StudyDokumen9 halamanPOC Drug Studydanni LBelum ada peringkat
- Rheumatoid Arthritis Arthritis Osteoarthritis Ankylosing Spondylitis Gout PainDokumen4 halamanRheumatoid Arthritis Arthritis Osteoarthritis Ankylosing Spondylitis Gout Paincicilvasquez0817Belum ada peringkat
- Amphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-4Dokumen4 halamanAmphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-4Vh TRBelum ada peringkat
- Drug StudyDokumen44 halamanDrug StudyLohrhen Lheighh CahreeniyowBelum ada peringkat
- Drugstudy Last DutyDokumen5 halamanDrugstudy Last DutyJoeven HilarioBelum ada peringkat
- Drugs StudyDokumen6 halamanDrugs StudyAllan MacacapagalBelum ada peringkat
- Nursing Care Plan: Assessment Diagnosis Planning Implementation Rationale EvaluationDokumen4 halamanNursing Care Plan: Assessment Diagnosis Planning Implementation Rationale Evaluationthomasfinley44Belum ada peringkat
- Nephrolithiasis - Drug StudyDokumen5 halamanNephrolithiasis - Drug StudyAia JavierBelum ada peringkat
- Pharma Sheet1Dokumen7 halamanPharma Sheet1Lyssa ShannenBelum ada peringkat
- Antiplatelet and Proton Pump Inhibitor Drug Study SummaryDokumen9 halamanAntiplatelet and Proton Pump Inhibitor Drug Study SummaryrocketwapBelum ada peringkat
- Celecoxib drug guideDokumen10 halamanCelecoxib drug guidejessica_omegaBelum ada peringkat
- Drug Study 68-75Dokumen8 halamanDrug Study 68-75joshua_santiago_5Belum ada peringkat
- Drug StudyDokumen8 halamanDrug StudyMaria Charlene Orpilla0% (1)
- Felodipine CefuroximeDokumen3 halamanFelodipine CefuroximecotyboyBelum ada peringkat
- CVA Drug StudyDokumen51 halamanCVA Drug StudyKarel LuBelum ada peringkat
- Dopamine Drug StudyDokumen14 halamanDopamine Drug StudyHannah Philene D. CalubBelum ada peringkat
- Drug Study (Medication Nurse)Dokumen42 halamanDrug Study (Medication Nurse)Ellen Grace CalayBelum ada peringkat
- Drug StudyDokumen22 halamanDrug StudyColleen Fretzie Laguardia NavarroBelum ada peringkat
- Drug Study 2Dokumen9 halamanDrug Study 2Justin PasaronBelum ada peringkat
- C C C Vertigo,: Electrolyte and Water Balance AgentDokumen12 halamanC C C Vertigo,: Electrolyte and Water Balance AgentEarl Tony TrinidadBelum ada peringkat
- Ix. Pharmacologic Management Brand Name Classification Indication Mechanism of Action Dosage and Frequency Adverse Reactions Nursing ConsiderationDokumen21 halamanIx. Pharmacologic Management Brand Name Classification Indication Mechanism of Action Dosage and Frequency Adverse Reactions Nursing ConsiderationDizerine Mirafuentes RolidaBelum ada peringkat
- Definitions OF DiagnosisDokumen25 halamanDefinitions OF DiagnosisGlaire ZarateBelum ada peringkat
- DrugsDokumen17 halamanDrugsRenzkie GeronimoBelum ada peringkat
- Piperacillin-Tazobactam AntibioticDokumen9 halamanPiperacillin-Tazobactam Antibiotic배기숭Belum ada peringkat
- Drug StudyDokumen10 halamanDrug StudyHelen ReonalBelum ada peringkat
- CNS: GI: Assessment & Drug Effects: Generic Name Brand Name Indications Action Side Effects Nursing ResponsibilitiesDokumen4 halamanCNS: GI: Assessment & Drug Effects: Generic Name Brand Name Indications Action Side Effects Nursing ResponsibilitiesJon Adam Bermudez SamatraBelum ada peringkat
- Epinephrine Classifications: Therapeutic: Antiasthmatics, Bronchodilators, Vasopressors Pharmacologic: Adrenergics IndicationsDokumen14 halamanEpinephrine Classifications: Therapeutic: Antiasthmatics, Bronchodilators, Vasopressors Pharmacologic: Adrenergics IndicationsLindy Shane BoncalesBelum ada peringkat
- Drug StudyDokumen9 halamanDrug StudyShiara Ruth EdrosoloBelum ada peringkat
- Ncp&drugstudDokumen12 halamanNcp&drugstudSarah Mae Billano BermudezBelum ada peringkat
- Name of Drug Route/Dose Mechanism of Action Indication Side Effects/Adverse Reactions Nursing ResponsibilitiesDokumen9 halamanName of Drug Route/Dose Mechanism of Action Indication Side Effects/Adverse Reactions Nursing ResponsibilitiespauchanmnlBelum ada peringkat
- Drug StudyDokumen9 halamanDrug StudyRachel PerandoBelum ada peringkat
- DRUG STUDY SUMMARYDokumen7 halamanDRUG STUDY SUMMARYEloisa Abarintos RacalBelum ada peringkat
- Drug Indication Action Side Effects and Adverse Reaction Nursing ConsiderationDokumen8 halamanDrug Indication Action Side Effects and Adverse Reaction Nursing Considerationkier khierBelum ada peringkat
- Cavite State University drug study on mefenamic acidDokumen3 halamanCavite State University drug study on mefenamic acidAngelica Cassandra VillenaBelum ada peringkat
- PHARMACARDS-not CompleteDokumen9 halamanPHARMACARDS-not CompleteAnonymous hv6m7kFbD40% (1)
- Drug StudyDokumen6 halamanDrug StudyNajmah Saaban100% (1)
- Drug StudyDokumen9 halamanDrug StudyMaye HerbitoBelum ada peringkat
- Salbutamol to Pantoprazole Nursing ResponsibilitiesDokumen6 halamanSalbutamol to Pantoprazole Nursing ResponsibilitiesElla FajardoBelum ada peringkat
- Drug StudyDokumen28 halamanDrug StudyJheryck SabadaoBelum ada peringkat
- ValdecoxibDokumen3 halamanValdecoxibapi-3797941Belum ada peringkat
- Generic / Brand Name Classification Mechanism of Action Indications Adverse Effects Nursing ResponsibilitiesDokumen3 halamanGeneric / Brand Name Classification Mechanism of Action Indications Adverse Effects Nursing ResponsibilitiesJommel Ryan Corpus LumibaoBelum ada peringkat
- LasixDokumen1 halamanLasixKatie McPeek100% (2)
- Alert Medical Series: Emergency Medicine Alert I, II, IIIDari EverandAlert Medical Series: Emergency Medicine Alert I, II, IIIBelum ada peringkat
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesDari EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesPenilaian: 4 dari 5 bintang4/5 (2)
- ElectrolyteImbalances Chart CopyRTrILifeDokumen3 halamanElectrolyteImbalances Chart CopyRTrILifeTr-I-Life100% (3)
- Clinical Pathway PPDokumen3 halamanClinical Pathway PPTr-I-Life0% (1)
- Medical Surgical NCLEXDokumen1 halamanMedical Surgical NCLEXTr-I-LifeBelum ada peringkat
- Psych MedsNCLEXDokumen6 halamanPsych MedsNCLEXTr-I-Life100% (4)
- Chapter 35Dokumen14 halamanChapter 35Tr-I-LifeBelum ada peringkat
- Caring For A TracheostomyDokumen7 halamanCaring For A TracheostomyTr-I-LifeBelum ada peringkat
- Ondansetron 2 MG - ML Solution For Injection - (EMC) Print FriendlyDokumen10 halamanOndansetron 2 MG - ML Solution For Injection - (EMC) Print FriendlyDewi Wara ShintaBelum ada peringkat
- Nursing Diagnosis DKA Care PlanDokumen2 halamanNursing Diagnosis DKA Care Planعبدالله خليل العسلBelum ada peringkat
- NURSING CARE ON CLIENTS WITH DIARRHEADokumen30 halamanNURSING CARE ON CLIENTS WITH DIARRHEAyustiBelum ada peringkat
- Klinik Rawat Inap Asa Ppni: Data Diagnosa PasienDokumen29 halamanKlinik Rawat Inap Asa Ppni: Data Diagnosa PasienGita Putri KencanaBelum ada peringkat
- Latihan POMR: Dr. Venna Febrian KDokumen39 halamanLatihan POMR: Dr. Venna Febrian KLoudry ElfaBelum ada peringkat
- Cloxacillin Classification, Mechanism, IndicationsDokumen3 halamanCloxacillin Classification, Mechanism, IndicationsKrizzia CarlosBelum ada peringkat
- Nursing Care Plan Assessment Diagnosis Inference Planning Interventio N Rationale EvaluationDokumen3 halamanNursing Care Plan Assessment Diagnosis Inference Planning Interventio N Rationale EvaluationDianne100% (2)
- Hyperemesis Gravidarum: A Current Review: Rami Eliakim, M.D., Ovadia Abulafia, M.D., and David M. Sherer, M.DDokumen12 halamanHyperemesis Gravidarum: A Current Review: Rami Eliakim, M.D., Ovadia Abulafia, M.D., and David M. Sherer, M.DTitis Retno Sawitri SawitriBelum ada peringkat
- Mediation OshoDokumen2 halamanMediation OshoRahulKumarBelum ada peringkat
- Drug StudyDokumen10 halamanDrug StudybaniniycsebBelum ada peringkat
- Upper Gastrointestinal ProblemsDokumen64 halamanUpper Gastrointestinal Problemssho bartBelum ada peringkat
- Holy Trinity Church FlyerDokumen1 halamanHoly Trinity Church Flyermarkkerrward5Belum ada peringkat
- Nursing Interventions for 10 Common DiseasesDokumen11 halamanNursing Interventions for 10 Common DiseasesKyla LatadaBelum ada peringkat
- Gastrointestinal effects of zinc ingestionDokumen2 halamanGastrointestinal effects of zinc ingestiongnana deepBelum ada peringkat
- Milk RemediesDokumen12 halamanMilk RemediesElham Elahi100% (1)
- DIY Lemon Candle Cures StressDokumen13 halamanDIY Lemon Candle Cures StressEliza Adrianne CorderoBelum ada peringkat
- Drug Study AzithromycinDokumen2 halamanDrug Study Azithromycinkuro hanabusaBelum ada peringkat
- Nursing Skills ManualDokumen52 halamanNursing Skills ManualCamille BattungBelum ada peringkat
- Possible Drugs of Acute GlomerulonephritisDokumen10 halamanPossible Drugs of Acute GlomerulonephritisJai - HoBelum ada peringkat
- Drug StudyDokumen13 halamanDrug Studyapi-3757116100% (4)
- Medicinal Agents for GI Disorders: Emetics & Anti-EmeticsDokumen5 halamanMedicinal Agents for GI Disorders: Emetics & Anti-EmeticsAhmed BajahBelum ada peringkat
- Overcoming Helicobacter Pylori NaturallyDokumen130 halamanOvercoming Helicobacter Pylori NaturallywoofpaxBelum ada peringkat
- PJT Confrence December 5th - FixDokumen27 halamanPJT Confrence December 5th - Fixmaya_rosmariaBelum ada peringkat
- Super Solv Remover MSDS PDFDokumen3 halamanSuper Solv Remover MSDS PDFGiniBelum ada peringkat
- NCP FormatDokumen2 halamanNCP FormatNaotaka KohinataBelum ada peringkat
- Drug Study DulcolaxDokumen2 halamanDrug Study DulcolaxReisha Fungo0% (1)
- Dr. E.P.Y. reviews bethanecol for urinary retentionDokumen1 halamanDr. E.P.Y. reviews bethanecol for urinary retentionCen Janber CabrillosBelum ada peringkat
- Blister Agents (HN T Q L HL)Dokumen65 halamanBlister Agents (HN T Q L HL)Reid Kirby100% (2)
- Nursing Care Plan of CKDDokumen6 halamanNursing Care Plan of CKDPabhat Kumar100% (2)