Expanded Program On Immunization
Diunggah oleh
Apple Fajardo De JesusDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Expanded Program On Immunization
Diunggah oleh
Apple Fajardo De JesusHak Cipta:
Format Tersedia
Expanded Program on Immunization (Philippines)
From Wikipedia, the free encyclopedia The Expanded Program on Immunization (EPI) in the Philippines began in July 1979. And, in 1986, made a response to the Universal Child Immunization goal. The four major strategies include:[1] 1. 2. 3. 4. Sustaining high routine Full Immunized Child (FIC) coverage of at least 90% in all provinces and cities, Sustaining the polio-free country for global certification Eliminating measles by 2008, Eliminating neonatal tetanus by 2008.
Contents
[hide]
1 Routine Schedule of Immunization 2 Routine Immunization Schedule for Infants 3 General Principles in Infants/Children Immunization 4 Tetanus Toxoid Immunization Schedule for Women 5 Care for the Vaccines 6 References
[edit] Routine Schedule of Immunization
Every Wednesday is designated as immunization day and is adopted in all parts of the country. Immunization is done monthly in barangay health stations, quarterly in remote areas of the country.
[edit] Routine Immunization Schedule for Infants
The standard routine immunization schedule for infants in the Philippines is adopted to provide maximum immunity against the seven vaccine preventable diseases in the country before the child's first birthday. The fully immunized child must have completed BCG 1, DPT 1, DPT 2, DPT 3, OPV 1, OPV 2, OPV 3, HB 1, HB 2, HB 3 and measles vaccines before the child is 12 months of age.[2] Minimum Minimum Number Age Dose Interval Between of Doses at 1st Dose Doses Birth or anytime after 1 dose birth 0.05 mL
Vaccine
Route
Site
Reason
Bacillus CalmetteGurin DiphtheriaPertussisTetanus Vaccine Oral Polio Vaccine
none
3 weeks old 3 doses
6 weeks(DPT 1), 0.5 10 weeks (DPT 2), mL 14 weeks (DPT 3)
6 weeks old 3 doses
2-3 drops
4 weeks
Hepatitis B Vaccine
6 weeks
3 doses
0.5 mL
4 weeks interval
BCG given at earliest possible age protects the possibility of TB Right deltoid Intradermal meningitis and other TB region of the arm infections in which infants are prone[3] Upper outer portion of the An early start with DPT reduces Intramuscular thigh, Vastus the chance of severe pertussis.[4] Lateralis (L-R-L) The extent of protection against polio is increased the earlier the Oral Mouth OPV is given. Keeps the Philippines poliofree.[5] An early start of Hepatitis B vaccine reduces the chance of being infected and becoming a carrier.[6] Upper outer Prevents liver cirrhosis and liver portion of the Intramuscular cancer which are more likely to thigh, Vastus develop if infected with Hepatitis Lateralis (R-L-R) B early in life.[7][8] About 9,000 die of complications of Hepatits B. 10% of Filipinos have Hepatitis B infection[9]
Measles Vaccine (not MMR)
9 months old 1 dose
0.5 mL
none
Upper outer portion of the Subcutaneous arms, Right deltiod
At least 85% of measles can be prevented by immunization at this age.[10]
[edit] General Principles in Infants/Children Immunization
Because measles kills, every infant needs to be vaccinated against measles at the age of 9 months or as soon as possible after 9 months as part of the routine infant vaccination schedule. It is safe to vaccinate a sick child who is suffering from a minor illness (cough, cold, diarrhea, fever or malnutrition) or who has already been vaccinated against measles.[11] If the vaccination schedule is interrupted, it is not necessary to restart. Instead, the schedule should be resumed using minimal intervals between doses to catch up as quickly as possible.[12] Vaccine combinations (few exceptions), antibiotics, low-dose steroids (less than 20 mg per day), minor infections with low fever (below 38.5 Celsius), diarrhea, malnutrition, kidney or liver disease, heart or lung disease, non-progressive encephalopathy, well controlled epilepsy or advanced age, are not contraindications to vaccination. Contrary to what the majority of doctors may think, vaccines against hepatitis B and tetanus can be applied in any period of the pregnancy.[13] There are very few true contraindication and precaution conditions. Only two of these conditions are generally considered to be permanent: severe (anaphylactic) allergic reaction to a vaccine component or following a prior dose of a vaccine, and encephalopathy not due to another identifiable cause occurring within 7 days of pertussis vaccination.[14] Only the diluent supplied by the manufacturer should be used to reconstitute a freeze-dried vaccine. A sterile needle and sterile syringe must be used for each vial for adding the diluent to the powder in a single vial or ampoule of freeze-dried vaccine.[15] The only way to be completely safe from exposure to blood-borne diseases from injections, particularly hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) is to use one sterile needle, one sterile syringe for each child.[16]
[edit] Tetanus Toxoid Immunization Schedule for Women
When given to women of childbearing age, vaccines that contain tetanus toxoid (TT or Td) not only protect women against tetanus, but also prevent neonatal tetanus in their newborn infants.[17] Vaccine Minimum Age/Interval Percent Protected Duration of Protection
TT1 TT2
As early as possible during pregnancy At least 4 weeks later
80% 80%
protection for the mother for the first delivery infants born to the mother will be protected from neonatal tetanus gives 3 years protection for the mother infants born to the mother will be protected from neonatal tetanus gives 5 years protection for the mother infants born to the mother will be protected from neonatal tetanus gives 10 years protection for the mother gives lifetime protection for the mother all infants born to that mother will be protected
TT3
At least 6 months later
95%
TT4
At least 1 year later
99%
TT5
At least 1 year later
99%
In June 2000, the 57 countries that have not yet achieved elimination of neonatal tetanus were ranked and the Philippines was listed together with 22 other countries in Class A, a classification for countries close to maternal and neonatal tetanus elimination.[18]
[edit] Care for the Vaccines
To ensure the optimal potency of vaccines,a careful attention is needed in handling practices at the country level. These include storage and transport of vaccines from the primary vaccine store down to the end-user at the health facility, and further down at the outreach sites.[19] Inappropriate storage, handling and transport of vaccines wont protect patients and may lead to needless vaccine wastage.[20] A "first expiry and first out" (FEFO) vaccine system is practiced to assure that all vaccines are utilized before its expiry date. Proper arrangement of vaccines and/or labeling of expiry dates are done to identify those close to expiring. Vaccine temperature is monitored twice a day (early in the morning and in the afternoon) in all health facilities and plotted to monitor break in the cold chain. Each level of health facilities has cold chain equipment for use in the storage vaccines which included cold room, freezer, refrigerator, transport box, vaccine carriers, thermometers, cold chain monitors, ice packs, temperature monitoring chart and safety collector boxes.[21]
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Mbaeri Accuracy of Prader OrchidometerDokumen4 halamanMbaeri Accuracy of Prader OrchidometerChikezie OnwukweBelum ada peringkat
- Bitter Kola PDFDokumen2 halamanBitter Kola PDFadeolaodukoyaBelum ada peringkat
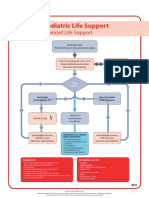
- Poster 10 PALS 01 01 ENG V20100927 PDFDokumen1 halamanPoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoBelum ada peringkat
- Acne Vulgaris PDFDokumen8 halamanAcne Vulgaris PDFsmackooooooBelum ada peringkat
- The Art of ConsultationDokumen8 halamanThe Art of Consultationhow_veryBelum ada peringkat
- Age Estimation Using Secondary DentinDokumen50 halamanAge Estimation Using Secondary DentinManjiri Joshi100% (1)
- DT Asia Pacific No 5 2013 0513 (04 04)Dokumen1 halamanDT Asia Pacific No 5 2013 0513 (04 04)SkAliHassanBelum ada peringkat
- Management of Flabby Ridge Case Report.20150524060252Dokumen7 halamanManagement of Flabby Ridge Case Report.20150524060252Rico AnasBelum ada peringkat
- Guideline Hypoglycemia PDFDokumen13 halamanGuideline Hypoglycemia PDFleslyjanet100% (1)
- Case Presentation OnDokumen30 halamanCase Presentation OnShweta ChaurasiaBelum ada peringkat
- Fraktur Dan DislokasiDokumen77 halamanFraktur Dan DislokasiRicky Jawwa0% (1)
- Voluson E Series - Transducer Guide (En) PDFDokumen4 halamanVoluson E Series - Transducer Guide (En) PDFZákány ZoltánBelum ada peringkat
- Letter From The Manitoba Medical Students AssociationDokumen3 halamanLetter From The Manitoba Medical Students AssociationRileyBelum ada peringkat
- DV - Laringoskopi IndirekDokumen4 halamanDV - Laringoskopi Indirekdies_vadisBelum ada peringkat
- From The Backyard To The Frontline: Initiatives of Philippine Hospital Workers On Best Environmental PracticesDokumen60 halamanFrom The Backyard To The Frontline: Initiatives of Philippine Hospital Workers On Best Environmental PracticesHealth Care Without Harm - AsiaBelum ada peringkat
- 7 FTPDokumen6 halaman7 FTPhaddig8Belum ada peringkat
- BromihdrosisDokumen4 halamanBromihdrosisPantelis PouliopoulosBelum ada peringkat
- Chranjivi HospitalsDokumen12 halamanChranjivi HospitalsRATI RAMBelum ada peringkat
- Gosssypiboma: Dr. B.V AmruthavalliDokumen3 halamanGosssypiboma: Dr. B.V AmruthavalliInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Show Dad HowDokumen20 halamanShow Dad HowWeldon Owen Publishing100% (5)
- Spec Newport e360T-LKPPDokumen4 halamanSpec Newport e360T-LKPPDwi SanitaBelum ada peringkat
- 630f32d80d4ba Changes in Medical EducationDokumen5 halaman630f32d80d4ba Changes in Medical Educationkennedy othoro100% (1)
- Interproximal Height of BoneDokumen3 halamanInterproximal Height of Bonefinislux1Belum ada peringkat
- PEDIA EndorsementDokumen4 halamanPEDIA EndorsementFlorie Lei BulosBelum ada peringkat
- Pulmonary Function TestsDokumen24 halamanPulmonary Function TestsSachin KonkaniBelum ada peringkat
- Report Clinical Internship at Dschang District HospitalDokumen35 halamanReport Clinical Internship at Dschang District HospitalAIME WILFRIED BEASSO FOZOCK100% (2)
- Supraventricular TachycardiaDokumen20 halamanSupraventricular TachycardiaBenyWirananggalaBelum ada peringkat
- Intensified Testing For Attention-Deficit Hyperactivity Disorder (ADHD) in Girls Should Reduce Depression and Smoking in Adult Females ADokumen4 halamanIntensified Testing For Attention-Deficit Hyperactivity Disorder (ADHD) in Girls Should Reduce Depression and Smoking in Adult Females ARafael MartinsBelum ada peringkat
- Match Data Main Match Program Results 2010 2014Dokumen142 halamanMatch Data Main Match Program Results 2010 2014Mariana GomezBelum ada peringkat
- BrochureDokumen6 halamanBrochureNikita JacobsBelum ada peringkat