Background
Diunggah oleh
Adrian Ridski HarsonoDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Background
Diunggah oleh
Adrian Ridski HarsonoHak Cipta:
Format Tersedia
Background Osteomyelitis is an acute or chronic inflammatory process of the bone and its structures secondary to infection with pyogenic
organisms. Pathophysiology Osteomyelitis may be localized or it may spread through the periosteum, cortex, marrow, and cancellous tissue. The bacterial pathogen varies on the basis of the patient's age and the mechanism of infection. The following are the 2 primary categories of acute osteomyelitis: hematogenous osteomyelitis and direct or contiguous inoculation osteomyelitis. Hematogenous osteomyelitis is an infection caused by bacterial seeding from the blood. Acute hematogenous osteomyelitis is characterized by an acute infection of the bone caused by the seeding of the bacteria within the bone from a remote source. This condition primarily occurs in children. The most common site is the rapidly growing and highly vascular metaphysis of growing bones. The apparent slowing or sludging of blood flow as the vessels make sharp angles at the distal metaphysis predisposes the vessels to thrombosis and the bone itself to localized necrosis and bacterial seeding. Vertebral osteomyelitis at any age is most often a secondary complication of a remote infection with hematogenous seeding. In approximately one half of vertebral osteomyelitis cases, a source can be identified such as urinary tract or skin, and approximately one third may be diagnosed with endocarditis.[1] Acute hematogenous osteomyelitis, despite its name, may have a slow clinical development and insidious onset. Direct or contiguous inoculation osteomyelitis is caused by direct contact of the tissue and bacteria during trauma or surgery. Direct inoculation (contiguous-focus) osteomyelitis is an infection in the bone secondary to the inoculation of organisms from direct trauma, spread from a contiguous focus of infection, or sepsis after a surgical procedure. Clinical manifestations of direct inoculation osteomyelitis are more localized than those of hematogenous osteomyelitis and tend to involve multiple organisms.
Additional categories include chronic osteomyelitis and osteomyelitis secondary to peripheral vascular disease. Chronic osteomyelitis persists or recurs, regardless of its initial cause and/or mechanism and despite aggressive intervention. Although listed as an etiology, peripheral vascular disease is actually a predisposing factor rather than a true cause of infection. Disease states known to predispose patients to osteomyelitis include diabetes
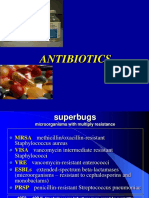
mellitus,[2]sickle cell disease, acquired immune deficiency syndrome (AIDS), intravenous (IV) drug abuse, alcoholism, chronic steroid use, immunosuppression, and chronic joint disease. In addition, the presence of a prosthetic orthopedic device is an independent risk factor, as is any recent orthopedic surgery or open fracture. For the radiologic perspective, see Osteomyelitis, Acute Pyogenic and Osteomyelitis, Chronic. Epidemiology Frequency United States The overall prevalence is 1 case per 5,000 children. Neonatal prevalence is approximately 1 case per 1,000. The annual incidence in patients with sickle cell anemia is approximately 0.36%. The prevalence of osteomyelitis after foot puncture (as is seen in the image below) may be as high as 16% (30-40% in patients with diabetes). The incidence of vertebral osteomyelitis is approximately 2.4 cases per 100,000 population.[1] Osteomyelitis of diabetic foot. Photography by David Effron MD, FACEP. International The overall incidence is higher in developing countries. Mortality/Morbidity Morbidity can be significant and can include localized spread of infection to associated soft tissues or joints; evolution to chronic infection, with pain and disability; amputation of the involved extremity; generalized infection; or sepsis. As many as 10-15% of patients with
vertebral osteomyelitis develop neurologic findings or frank spinal-cord compression. As many as 30% of pediatric patients with long-bone osteomyelitis may develop deep venous thrombosis (DVT). The development of DVT may also be a marker for disseminated infection.[3] Vascular complications appear to be more common with community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) than was previously recognized.[4] Mortality rates are low, unless associated sepsis or an underlying serious medical condition is present. Race No increased incidence of osteomyelitis is noted based on race. Sex Males are at increased relative risk, which increases through childhood, peaking in adolescence and falling to a low ratio in adults.[5] Age In general, osteomyelitis has a bimodal age distribution. Acute hematogenous osteomyelitis is primarily a disease in children. Direct trauma and contiguous focus osteomyelitis are more common among adults and adolescents than in children. Vertebral osteomyelitis is more common in persons older than 45 years. History Hematogenous osteomyelitis usually presents with a slow insidious progression of symptoms. Direct osteomyelitis generally is more localized, with prominent signs and symptoms. General symptoms of osteomyelitis include the following:
Hematogenous long-bone osteomyelitis
o
Abrupt onset of high fever (fever is present in only 50% of neonates with osteomyelitis)
o o o
Fatigue Irritability Malaise
o o
Restriction of movement (pseudoparalysis of limb in neonates) Local edema, erythema, and tenderness
Hematogenous vertebral osteomyelitis
o o o o o
Insidious onset History of an acute bacteremic episode May be associated with contiguous vascular insufficiency Local edema, erythema, and tenderness Failure of a young child to sit up normally[6]
Chronic osteomyelitis
o o o o
Nonhealing ulcer Sinus tract drainage Chronic fatigue Malaise
Physical Findings at physical examination may include the following:
Fever (present in only 50% of neonates) Edema Warmth Fluctuance Tenderness to palpation Reduction in the use of the extremity (eg, reluctance to ambulate, if the lower extremity is involved or pseudoparalysis of limb in neonates)
Failure of a young child to sit up normally Sinus tract drainage (usually a late finding or one that occurs with chronic infection)
Causes Note that responsible pathogens may be isolated in only 35-40% of infections. Bacterial causes of acute and direct osteomyelitis include the following:
Acute hematogenous osteomyelitis (Note increasing reports of other pathogens in bone and joint infections including community-associated methicillin-resistant Staphylococcus aureus [MRSA],[7]Kingella kingae,[8] and others.)
o
Newborns (younger than 4 mo): Saureus, Enterobacter species, and group A and B Streptococcus species
Children (aged 4 mo to 4 y): S aureus, group A Streptococcus species, Haemophilus influenzae, and Enterobacter species
Children, adolescents (aged 4 y to adult): S aureus (80%), group A Streptococcus species, H influenzae, and Enterobacter species
Adult - S aureus and occasionally Enterobacter or Streptococcus species
Direct osteomyelitis
o o o
General - S aureus, Enterobacter species, and Pseudomonas species Puncture wound through an athletic shoe - S aureus and Pseudomonas species Sickle cell disease -S aureus and Salmonellae species
Laboratory Studies The following studies are indicated in patients with osteomyelitis:
CBC count: The WBC count may be elevated, but it is frequently normal.
o
A leftward shift is common with increased polymorphonuclear leukocyte counts.
The C-reactive protein level is usually elevated and nonspecific; this study may be more useful than the erythrocyte sedimentation rate (ESR) because it reveals elevation earlier.
The ESR is usually elevated (90%); however, this finding is clinically nonspecific.
CRP and ESR have limited roles in the setting of chronic osteomyelitis and are often normal
Culture: Superficial wound or sinus tract cultures often do not correlate with the bacteria that is causing osteomyelitis and have limited use. Blood culture results are positive in approximately 50% of patients with hematogenous osteomyelitis. However, a positive blood culture may preclude the need for further invasive procedures to isolate the organism. Bone cultures from biopsy or aspiration have a diagnostic yield of approximately 77% across all studies.[1]
Imaging Studies
Radiography
o
Radiographic evidence of acute osteomyelitis is first suggested by overlying soft-tissue edema at 3-5 days after infection. Examples of radiographic evidence of osteomyelitis are presented in the images below. Osteomyelitis of the elbow. Photography by David Effron MD, FACEP. Osteomyelitis of index finger metacarpal head secondary to clenched fist injury. Photography by David Effron MD, FACEP. Osteomyelitis of the great toe. Photography by David Effron MD, FACEP. Osteomyelitis of T10 secondary to streptococcal disease. Photography by David Effron MD, FACEP. Osteomyelitis. Radiography of diabetic foot showing osteomyelitis with gas. Photography by David Effron MD, FACEP.
Bony changes are not evident for 14-21 days and initially manifest as periosteal elevation followed by cortical or medullary lucencies. By 28 days, 90% of patients demonstrate some abnormality.
Approximately 40-50% focal bone loss is necessary to cause detectable lucency on plain films.
MRI
o
The MRI is effective in the early detection and surgical localization of osteomyelitis.[9, 10]
Studies have shown its superiority compared with plain radiography, CT, and radionuclide scanning and is considered to be the imaging of choice.
Sensitivity ranges from 90-100%.
Positron emission tomographic (PET) scanning has accuracy similar to MRI. Radionuclide bone scanning
o
Three phase bone scan, gallium scan and tagged WBC scan are considerations in patients who are unable to have MRI imaging. A three phase bone scan has high sensitivity and specificity in adults with normal findings on radiograph. Specificity is dramatically decreased in the setting of previous surgery or traumatized bone.
In special circumstances, additional information can be obtained from further scanning with leukocytes labeled with gallium 67 and/or indium 111.
CT scanning
CT scans can depict abnormal calcification, ossification, and intracortical abnormalities.
It is not recommended for routine use for diagnosing osteomyelitis but is often the imaging of choice when MRI is not available
Ultrasonography
o
This simple and inexpensive technique has shown promise, particularly in children with acute osteomyelitis.
Ultrasonography may demonstrate changes as early as 1-2 days after onset of symptoms.
Abnormalities include soft tissue abscess or fluid collection and periosteal elevation.
o o
Ultrasonography allows for ultrasound-guided aspiration. It does not allow for evaluation of bone cortex.
Emergency Department Care Osteomyelitis rarely requires emergent stabilization or resuscitation. The primary challenge for ED physicians is considering the appropriate diagnosis in the face of subtle signs or symptoms. Treatment for osteomyelitis involves the following:
Initiation of intravenous antibiotics that penetrate bone and joint cavities Referral of the patient to an orthopedist or general surgeon Possible medical infectious disease consultation
Select the appropriate antibiotics using direct culture results in samples from the infected site, whenever possible. Empiric therapy is often initiated on the basis of the patient's age and the clinical presentation. Empiric therapy should always include coverage for S aureus and consideration of CA-MRSA. Further surgical management may involve removal of the nidus of infection, implantation of antibiotic beads or pumps, hyperbaric oxygen therapy,[11, 12] or other modalities. Diagnosis requires 2 of the 4 following criteria:
Purulent material on aspiration of affected bone
Positive findings of bone tissue or blood culture Localized classic physical findings of bony tenderness, with overlying soft-tissue erythema or edema
Positive radiological imaging study
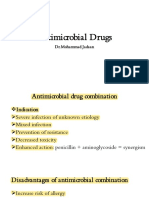
Consultations Order an orthopedics, general surgery, or infectious disease consultation, as needed. Patients with diabetic foot osteomyelitis are best cared for by a multidisciplinary team.[13] Medication Summary The primary treatment for osteomyelitis is parenteral antibiotics that penetrate bone and joint cavities. Treatment is required for at least 4-6 weeks. After intravenous antibiotics are initiated on an inpatient basis, therapy may be continued with intravenous or oral antibiotics, depending on the type and location of the infection, on an outpatient basis. The following are recommendations for the initiation of empiric antibiotic treatment based on the age of the patient and mechanism of infection:
With hematogenous osteomyelitis (newborn to adult), the infectious agents include S aureus, Enterobacteriaceae organisms, group A and B Streptococcus species, and H influenzae. Primary treatment is a combination of penicillinase-resistant synthetic penicillin and a third-generation cephalosporin. Alternate therapy is vancomycin or clindamycin and a third-generation cephalosporin, particularly if methicillin-resistant S aureus (MRSA) is considered likely. Linezolid is also used in these circumstances. In addition to these above-mentioned antibacterials, ciprofloxacin and rifampin may be an appropriate combination therapy for adult patients. If evidence of infection with gram-negative bacilli is observed, include a third-generation cephalosporin.
In patients with sickle cell anemia and osteomyelitis, the primary bacterial causes are S aureus and Salmonellae species. Thus, the primary choice for treatment is a fluoroquinolone antibiotic (not in children). A third-generation cephalosporin (eg, ceftriaxone) is an alternative choice.
When a nail puncture occurs through an athletic shoe, the infecting agents may include S aureus and Pseudomonas aeruginosa. The primary antibiotics in this scenario include ceftazidime or cefepime. Ciprofloxacin is an alternative treatment.
For patients with osteomyelitis due to trauma, the infecting agents include S aureus, coliform bacilli, and Pseudomonas aeruginosa. Primary antibiotics include nafcillin and ciprofloxacin. Alternatives include vancomycin and a third-generation cephalosporin with antipseudomonal activity.
Antibiotics Class Summary Empiric antimicrobial therapy must be comprehensive and should cover all likely pathogens in the context of the clinical setting. View full drug information Nafcillin (Nafcil, Unipen)
Initial therapy for suspected penicillin Gresistant streptococcal or staphylococcal infections. Use parenteral therapy initially in severe infections. Change to oral therapy as condition warrants. Because of thrombophlebitis, particularly in elderly patients, administer parenterally for only the short term (1-2 d). Change to PO route as clinically indicated. Note: Administer in combination with a third-generation cephalosporin to treat osteomyelitis. Do not admix with aminoglycosides for IV administration. View full drug information Ceftriaxone (Rocephin)
Third-generation cephalosporin with broad-spectrum gram-negative activity; lower efficacy against gram-positive organisms; higher efficacy against resistant organisms; arrests bacterial
growth by binding to one or more penicillin-binding proteins. Note: Administer with a penicillinase-resistant synthetic penicillin, when treating osteomyelitis. View full drug information Cefazolin (Ancef)
First-generation semisynthetic cephalosporin that arrests bacterial cell wall synthesis, inhibiting bacterial growth; primarily active against skin flora, including S aureus; typically used alone for skin and skin-structure coverage. View full drug information Ciprofloxacin (Cipro)
Fluoroquinolone with activity against pseudomonads, streptococci, MRSA, Staphylococcus epidermidis, and most gram-negative organisms, but no activity against anaerobes. Inhibits bacterial DNA synthesis and, consequently, growth. Continue treatment for at least 2 d (typical treatment, 7-14 d) after signs and symptoms disappear. View full drug information Ceftazidime (Fortaz, Ceptaz)
Third-generation cephalosporin with broad-spectrum gram-negative activity; lower efficacy against gram-positive organisms; higher efficacy against resistant organisms; arrests bacterial growth by binding to one or more penicillin-binding proteins. View full drug information Clindamycin (Cleocin)
Lincosamide for the treatment of serious skin and soft-tissue staphylococcal infections; also effective against aerobic and anaerobic streptococci (except enterococci); inhibits bacterial growth, possibly by blocking dissociation of peptidyl t-RNA from ribosomes, arresting RNAdependent protein synthesis. View full drug information Vancomycin (Vancocin)
Potent antibiotic directed against gram-positive organisms and active against Enterococcus species. Useful in the treatment of septicemia and skin structure infections. Indicated for patients who can not receive or have failed to respond to penicillins and cephalosporins or have infections with resistant staphylococci. For abdominal penetrating injuries, it is combined with an agent active against enteric flora and/or anaerobes. To avoid toxicity, current recommendation is to assay vancomycin trough levels after third dose drawn 0.5 h prior to next dosing. Use creatinine clearance to adjust dose in patients with renal impairment. Used in conjunction with gentamicin for prophylaxis in penicillin-allergic patients undergoing gastrointestinal or genitourinary procedures. View full drug information Linezolid (Zyvox)
Prevents formation of functional 70S initiation complex, which is essential for bacterial translation process. Bacteriostatic against staphylococci.
The FDA warns against the concurrent use of linezolid with serotonergic psychiatric drugs, unless indicated for life-threatening or urgent conditions. Linezolid may increase serotonin CNS levels as a result of MAO-A inhibition, increasing the risk of serotonin syndrome. Deterrence/Prevention
Acute hematogenous osteomyelitis can potentially be avoided by preventing bacterial seeding of bone from a remote site. This involves the appropriate diagnosis and treatment of primary bacterial infections.
Direct inoculation osteomyelitis can best be prevented with appropriate wound management and consideration of prophylactic antibiotic use at the time of injury.
Complications Complications of osteomyelitis may include the following:
Bone abscess Paravertebral/epidural abscess Bacteremia Fracture Loosening of the prosthetic implant Overlying soft-tissue cellulitis Draining soft-tissue sinus tracts
Prognosis The prognosis for osteomyelitis varies but is markedly improved with timely diagnosis and aggressive therapeutic intervention.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Septic Arthritis in AdultsDokumen19 halamanSeptic Arthritis in AdultsIvelisse TaverasBelum ada peringkat
- Cephalosporins in Veterinary MedicineDokumen23 halamanCephalosporins in Veterinary MedicineSunil100% (3)
- Treatment of Community-Acquired Pneumonia in Adults Who Require Hospitalization - UpToDateDokumen80 halamanTreatment of Community-Acquired Pneumonia in Adults Who Require Hospitalization - UpToDateTran Thai Huynh NgocBelum ada peringkat
- Historical Overview of The Cephalosporin Spectrum: Four Generations of Structural EvolutionDokumen8 halamanHistorical Overview of The Cephalosporin Spectrum: Four Generations of Structural EvolutionBagus FitraBelum ada peringkat
- Top 10 List of Antibiotic ClassesDokumen10 halamanTop 10 List of Antibiotic ClassesZubair khanBelum ada peringkat
- Medmastery Antimicrobial - Stewardship - HandbookDokumen65 halamanMedmastery Antimicrobial - Stewardship - HandbookHhaBelum ada peringkat
- B-Lactam Ab 2Dokumen34 halamanB-Lactam Ab 2Ph.first SBelum ada peringkat
- DRUG CeftazidimeDokumen1 halamanDRUG Ceftazidimerholiboi0% (1)
- Topic 1 PseudomonashhjjunDokumen8 halamanTopic 1 PseudomonashhjjunRachel Marie M. GaniaBelum ada peringkat
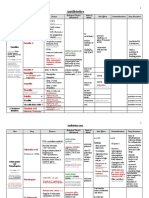
- Antimicrobial Drugs TableDokumen19 halamanAntimicrobial Drugs TableLaylee ClareBelum ada peringkat
- Jurnal BronchopneumoniaDokumen5 halamanJurnal BronchopneumoniaBianti Nur'ainiBelum ada peringkat
- Drug Name Indication Mode of Action Contraindications Side Effects Nursing ConsiderationsDokumen3 halamanDrug Name Indication Mode of Action Contraindications Side Effects Nursing ConsiderationsAlyssa RodriguezBelum ada peringkat
- List of AntibioticsDokumen10 halamanList of AntibioticsPitetLaiBelum ada peringkat
- Febra La Pacientul Imunodeprimat (Romana)Dokumen59 halamanFebra La Pacientul Imunodeprimat (Romana)ialomitaBelum ada peringkat
- CeftazidimeDokumen16 halamanCeftazidimeNakorn BaisriBelum ada peringkat
- Antimicrobial AgentDokumen46 halamanAntimicrobial Agentسامر الرفاعيBelum ada peringkat
- Ivf: Therapeutics: Anti-Pyretics: PenicillinsDokumen6 halamanIvf: Therapeutics: Anti-Pyretics: PenicillinsJenny CiBelum ada peringkat
- Alternative Intravitreal Antibiotics A Systematic.2Dokumen15 halamanAlternative Intravitreal Antibiotics A Systematic.2Daniel MirandaBelum ada peringkat
- Ceftazidime+Avibactum-2gm +0.5gm InjectionDokumen10 halamanCeftazidime+Avibactum-2gm +0.5gm InjectionMd. Abdur RahmanBelum ada peringkat
- Clinical Pharmacokinetics in Burn Patients 1 PDFDokumen8 halamanClinical Pharmacokinetics in Burn Patients 1 PDFClaudio Luis VenturiniBelum ada peringkat
- Antibiotics and Antibacterial Drugs SDokumen67 halamanAntibiotics and Antibacterial Drugs Somar hameed100% (1)
- Nelson's Pediatric Antimicrobial PDFDokumen331 halamanNelson's Pediatric Antimicrobial PDFMADHANKUMAR MANICKAVELBelum ada peringkat
- أدوية الطوارىءDokumen162 halamanأدوية الطوارىءManar22Belum ada peringkat
- Case Study 103Dokumen8 halamanCase Study 103Jonah MaasinBelum ada peringkat
- Continuous and Extended Infusion Beta Lactams PDFDokumen3 halamanContinuous and Extended Infusion Beta Lactams PDFarnaldops333Belum ada peringkat
- Dental RoshetttaDokumen29 halamanDental RoshetttaKORMAX LEAGUEBelum ada peringkat
- Cephalosporins GenerationDokumen7 halamanCephalosporins GenerationSam SmileyBelum ada peringkat
- Antibacerials PharmacolgyDokumen53 halamanAntibacerials PharmacolgyHamid AryanBelum ada peringkat
- 1) Cephalosporins: Generation Common Dosages/Regimens Spectrum of Activity 1 Cephalexin (Keflex) 250-500mg PO q6hDokumen1 halaman1) Cephalosporins: Generation Common Dosages/Regimens Spectrum of Activity 1 Cephalexin (Keflex) 250-500mg PO q6hjoe thomasBelum ada peringkat
- Antibiotic Guideline BIRDEM 2021.pdf Version 1Dokumen92 halamanAntibiotic Guideline BIRDEM 2021.pdf Version 1Imran Khan100% (6)