Androgens in Women
Diunggah oleh
ardidownDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Androgens in Women
Diunggah oleh
ardidownHak Cipta:
Format Tersedia
ANDROGENS IN WOMEN -Ovarian and Adrenal Androgen Biosynthesis and
MetabolismIn women, androgens are produced in the ovaries, adrenal glands and fat cells. In fact, women may produce too much or too little of these hormones disorders of androgen excess and deficiency are among the more common hormonal disorders in women. Androgens play a key role in the hormonal cascade that kick-starts puberty, stimulating hair growth in the pubic and underarm areas. Additionally, these hormones are believed to regulate the function of many organs, including the reproductive tract, bone, kidneys, liver and muscle. In adult women, androgens are necessary for estrogen synthesis and have been shown to play a key role in the prevention of bone loss, as well as sexual desire and satisfaction. They also regulate body function before, during and after menopause
(http://www.healthywomen.org/condition/androgen). For women excess amounts of androgens can pose a problem, resulting in such "virilizing effects" as acne, hirsutism (excess hair growth in "inappropriate" places, like the chin or upper lip) and thinning hair. Many women with high levels of a form of testosterone called "free" testosterone have polycystic ovary syndrome (PCOS), characterized by irregular or absent menstrual periods, infertility, blood sugar disorders, and, in some cases, symptoms like acne and excess hair growth. Left untreated, high levels of androgens, regardless of whether a woman has PCOS or not, are associated with serious health consequences, such as insulin resistance and diabetes, high cholesterol, high blood pressure and heart disease. In addition to PCOS, other causes of high androgen levels (called hyperandrogenism) include, congenital adrenal hyperplasia (a genetic disorder affecting the adrenal glands that afflicts about one in 14,000 women) and other
adrenal abnormalities, and ovarian or adrenal tumors. Medications such as anabolic steroids can also cause hyperandrogenic symptoms. Low androgen levels can be a problem as well, producing effects such as low libido (interest or desire in sex), fatigue, decreased sense of well-being and increased susceptibility to bone disease. Because symptoms like flagging desire and general malaise have a variety of causes, androgen deficiency, like hyperandrogenism, often goes undiagnosed. Low androgen levels may affect women at any age, but most commonly occur during the transition to menopause, or "perimenopause," a term used to describe the time before menopause (usually two to eight years). Androgen levels begin dropping in a woman's twenties, however; by the time she reaches menopause, they have declined 50 percent or more from their peak as androgen production declines in the adrenal glands and the midcycle ovarian boost evaporates. The biological activity of an androgen depends on its ability to bind to androgen receptors in target tissues and regulate gene transcriptional activity (i.e., its potency), the production rate, metabolic clearance rate, which includes various metabolic conversions and excretion, and the quantitative amount that is available to the target tissues. The metabolic clearance rate and amount of androgen that is bioavailable in the blood to be transported into cells is dependent to a great extent on the degree of binding to the low capacity and high affinity globulin, sex hormone-binding globulin (SHBG), and the high capacity but low affinity albumin. The quantity of androgen in the blood that is not bound to serum proteins or weakly bound to albumin is considered to be bioavailable. The relative potency, serum concentrations, and protein binding of the major androgens or precursors that are present in blood. Taking into account the potency, concentration, and clinical correlations with hyper- and hypoandrogenic states in women, T is a reasonable measure of the androgen status of women. The total T level is markedly influenced by the SHBG concentration. Sex hormone binding globulin levels are decreased in obesity, hyperinsulinism, glucocorticoid or growth hormone excess, hypothyroidism, and hyperandrogenic states. The levels
are increased with oral estrogen therapy, hyperthyroidism, cirrhosis, and some antiepileptic medications. Therefore, the free or bioavailable T level more accurately reflects androgen status than does the total T concentration. Free T is best measured by equilibrium dialysis and not by the various direct or analogue assays on the market (Deborah, 7270066-Sexuality-Androgen-ReplacementWomen: 2004). The Free T Index (also called the Free Androgen Index) closely correlates with the free T measurement, and can be calculated from measurements of total T and SHBG. Androgens are directly secreted into the circulation by the ovaries and adrenals. In addition, various peripheral tissues, such as adipose tissue, muscle, and fat, convert androgens and androgen precursors from the ovaries and adrenals into androgens that then enter the circulation as part of the androgen pool. The relative contributions of these sources to androgen production in preand postmenopausal women. The circulating concentrations of the androgens may not reflect androgen action at a specific target tissue. For instance, the expression of the levels of 5_-reductase, the enzyme that catalyzes the conversion of T to dihydrotestosterone (DHT), varies in different target organs and at different sites. Indeed, the term intracrinology has been used to describe hormone production, metabolism, and effect occurring in the same local target tissue . This process allows androgens to be biologically available for physiologic effects, but unavailable for direct biologic measurement in serum. An indirect measurement of androgen status of peripheral tissues may be assessed by biological assay of DHT metabolites: androsterone-glucoronide (ADT-G), androstane-3_, 17_-diol-glucoronide (3_-diol-G), androstane-3_, 17_diol-glucoronide (3_-diol-G), and ADT-sulfate. Androgen production and serum levels decrease with age. Both T and androstenedione (A) levels decrease before menopause. One study in a small number of women noted that the mean serum T concentration at age 21 years was approximately twice that at age 40 years, whereas an approximate 25% decrease was noted between ages 42 and 50 years in the Study of Womens Health Across the Nation (SWAN).
There is conflicting data, however, as to whether T levels decrease further during the menopause transition. Some studies suggest that an approximately 15% decline occurs. In contrast, the large longitudinal Melbourne Womens Midlife Health Project, which studied women through the menopausal transition, did not demonstrate a decline in total serum T; indeed, a decrease in SHBG levels resulted in an increase in the calculated free androgen index. Similarly, the SWAN study did not find a reduction in T concentrations during the menopausal transition. There is no controversy surrounding the observations that production of the major androgen precursor from the adrenals, DHEA, and its sulfate peak during the third decade and then sharply decline between ages 30 and 60 years. Between the ages of 20 and 80 years, serum DHT levels steadily decrease an average of 44% in association with a decrease between 48% and 72% of various conjugated metabolites. Thus, the relatively low androgen levels found in women after the menopause in comparison to women in their 20s and 30s reflects an age related decrease, rather than a specific menopausal effect (Deborah, 7270066Sexuality-Androgen-Replacement-Women: 2004). The pathways of adrenal and ovarian steroid biosynthesis use the same enzymes for the initial steps of steroidogenesis but express different enzymes that convert steroid precursors to the final active products. Both the adrenal and ovary produce dehydroepiandrosterone (DHEA), the principal precursor of androgens and estrogens. The key enzyme in DHEA production is P450c17, which catalyzes both 17-hydroxylation and 17,20- lyase activities. The 17,20-lyase activity of human P450c17 strongly favors 17-hydroxypregnenolone rather than 17 hydroxyprogesterone (17-OHP) as a substrate, producing abundant DHEA, so that most human androgens and estrogens derive from DHEA. Understanding the biochemistry of P450c17 is central to understanding the hyperandrogenism of polycystic ovary syndrome (PCOS). Rare genetic disorders of steroidogenesis provide human genetic knockout experiments of nature, yielding important information about the biosynthesis and physiological roles of steroids (Richard, 36327773-Androgen-Excess-Disorders-in-Women: 2006).
The pathways of steroidogenesis employ a relatively small number of steroidogenic enzymes, but variations in their tissue specificity of expression and in the availability of substrates and cofactors result in the widely varying patterns of steroid production in each steroidogenic tissue. Although no cell type expresses all the steroidogenic enzymes, their interrelationships can be seen in the idealized integrated pathway. Cholesterol is the precursor for all steroid hormones. The human adrenal and ovary can synthesize cholesterol de novo from acetate, but most cholesterol is provided by plasma low-density lipoproteins (LDLs) derived from dietary cholesterol (Richard, 36327773-Androgen-Excess-Disorders-inWomen: 2006). The presence of adequate LDL suppresses 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the rate-limiting step in cholesterol synthesis. HMG-CoA reductase, as well as LDL receptor number and uptake of LDL cholesterol, are stimulated by adrenocorticotropic hormone (ACTH) in the adrenal and by follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in the ovary. Steroidogenic cells take up LDL cholesterol esters by receptormediated endoctytosis to be either stored or immediately converted to free cholesterol for use as substrate in steroidogenesis. Storage of cholesterol esters in lipid droplets is under the control of two opposing enzymes, cholesterol esterase (cholesterol ester hydrolase) and cholesterol synthetase. LH and ACTH stimulate esterase to increase the availability of free cholesterol for steroidogenesis while inhibiting synthetase.
Ovarian theca and granulosa cells in individual follicular units synthesize both androgens and estrogens. The steroidogenic enzymes expressed in the theca or granulosa cells vary with the menstrual cycle. In the follicular phase, theca cells express StAR, P450scc, 3-HSD-II, and P450c17 to produce androstenedione, some of which is converted to testosterone by 17-HSD-V. Most thecal steroids diffuse to the granulosa cell, but some are secreted into the circulation. Rising thecal androstenedione production during the follicular phase plus increased expression of 17-HSD-I and P450aro in the granulosa cells results in abundant estradiol production by the preovulatory follicle (Richard, 36327773-AndrogenExcess-Disorders-in-Women: 2006). Theca cells continue to provide androstenedione to the granulosa cell during the luteal phase, while the granulose cell undergoes granulosa-lutein transformation and expresses StAR, P450scc, and 3-HSD-II, but not P450c17. This permits the granulosa-lutein cell to produce progesterone while converting C-19 steroids from the theca to estrogens. Numerous follicles grow simultaneously in the reproductive ovary. During the recruitment and growth phase, the granulosa cells proliferate, differentiate, and become steroidogenic. During the growth phase, most follicles undergo atresia, while some remain viable. The antral follicular stage is characterized by antrum formation and acquisition of differentiated steroidogenic cells. LH induces theca cells to
synthesize androgens before FSH induces the granulosa cells to aromatize them. Only the granulosa cells surrounding the follicle express aromatase and produce estradiol. During the 2 weeks before ovulation (the follicular phase), LH increases the theca cell expression of the LH receptor, StAR, P450scc, 3-HSD-II, and P450c17, whereas FSH increases granulosa cell expression of aromatase and 17HSD-I. The majority of ovarian C-19 steroids are produced from DHEA. While rodents and other species produce androstenedione directly from 17-OHP, the 17,20lyase activity of human P450c17 strongly favors 17-
hydroxypregnenolone as a substrate and utilizes 17-OHP inefficiently. Intraovarian peptides, including members of the insulin-like growth factor, transforming growth factor, and epidermal growth factor families, modulate both folliculogenesis and steroidogenesis (Richard, 36327773-Androgen-ExcessDisorders-in-Women: 2006). Germ cell differentiating factor-9, expressed by the oocyte throughout folliculogenesis, appears to promote granulosa cell differentiation, stimulate theca cells, and inhibit luteal cell formation. Insulin-like growth factors appear to enhance responses to FSH. Both insulin-like growth factor (IGF)-1 and IGF-2 can increase granulosa cell proliferation and estradiol secretion, but only IGF-2 mRNA is expressed in the ovary, particularly in the granulosa cells. Women with IGF-1 deficiency can be induced to ovulate by stimulation with gonadotropins, consistent with the view that IGF-1 is not required for folliculogenesis. Granulosa cells also produce inhibin, an / heterodimer that exists in two forms differing in the -subunit. Serum concentrations of inhibin A and B vary with the menstrual cycle: inhibin A rises in follicular fluid with increasing follicular size, beginning just before ovulation and peaking during the luteal phase, and inhibin B increases in granulosa cells following stimulation with FSH. Serum
concentrations of inhibin B correlate with the volume of granulosa cells, serving as an index for the size of the growing cohort of follicles (ovarian reserve). Inhibin B peaks in the early follicular phase and inhibits pituitary production of FSH during the later follicular phase. The antral follicle grows 12 mm in diameter daily during the antral phase of follicular development in response to
gonadotropins. reaching a diameter of about 20 mm, primarily representing accumulated follicular fluid. The theca interna continues to differentiate into interstitial cells, generating more androstenedione. The granulosa cell layers differentiate into discrete zones: the membrana layer subsequently acquires LH receptors in response to FSH, whereas the cumulus layer constituitively expresses LH receptors. One dominant follicle destined for ovulation develops into a mature graafian follicle. Following ovulation, LH induces granulosa membrana cells to differentiate into granulosa lutein cells and the remaining thecal interstitial cells to differentiate into theca lutein cells, thus forming the corpus luteum. LH also induces the granulosa lutein cells to produce vascular endothelial growth factor, which is required for neovascularization of the corpus luteum that penetrates the basement membrane to provide the LDLs necessary for steroidogenesis. After ovulation, the luteal cells accumulate more LH receptors, allowing basal LH levels to maintain the corpus luteum. Early in pregnancy, human chorionic gonadotropin stimulates these LH receptors, inducing progesterone synthesis by the corpus luteum during the first trimester. In contrast to the preovulatory follicle, the granulosalutein cells and the corpus luteum of pregnancy express large amounts of P450scc and 3-HSD, permitting the synthesis of progesterone (Richard, 36327773-Androgen-ExcessDisorders-in-Women: 2006). The regulation of adrenal androgen production is poorly understood. The fetal adrenal produces large amounts of DHEAS, but these serve no essential role, because fetuses that cannot produce these steroids (e.g., those having no P450c17) develop normally. Following birth, the fetal zone of the adrenal involutes and the production of DHEAS falls to very low levels. The adrenal zona reticularis becomes morphologically identifiable after about 3 years of age, but production of DHEAS does not begin until the onset of adrenarche at about 78 years of age. Adrenarche is defined by this rise in serum DHEAS and is the basis of so-called pubarchethe onset of small amounts of pubic hair before the onset of puberty. Adrenarche typically precedes true puberty (i.e., the activation of the hypothalamic/pituitary/gonadal axis) by about 2 years and is completely
independent of puberty, gonadotropins, and the gonads themselves. The stimulus to adrenarche is unknown. Adrenarche occurs only in human beings, chimpanzees, gorillas, and possibly orangutans, and hence is rather difficult to study. Some have hypothesized a peptide stimulator of the zona reticularis (analogous to ACTH), but no solid evidence for an adrenal androgen-stimulating hormone has appeared. Serum concentrations of DHEAS continue to rise after puberty, reaching maximal levels at 2530 years, and then begin to decline (adrenopause). Despite the 100-fold change in DHEAS concentrations during adrenarche, concentrations of ACTH and cortisol do not change. Thus most contemporary studies of adrenarche focus on intra-adrenal events. The onset of adrenarche is accompanied by a decrease in 3-HSD and an increase in P450c17 and cytochrome b5 in the zona reticularis, favoring the production of DHEA. Serine phosphorylation of P450c17 also favors DHEA production, but it is not known whether the phosphorylation of P450c17 changes during adrenarche. A developmentally programmed trigger, possibly IGF-1, may induce cellular proliferation in the zona reticularis while promoting synthesis of the steroidogenic machinery. At the same time, increased synthesis of cytochrome b5 promotes the 17,20-lyase activity of P450c17, which, together with decreased 3-HSD expression, favors DHEA production. Serine phosphorylation of P450c17 may also be developmentally programmed, and also facilitates 17,20 lyase activity. Unlike the neighboring fasciculata, the reticularis expresses sulfotransferase preferentially over steroid sulfatase, ensuring augmented DHEAS production. Premature exaggerated adrenarche has been linked to insulin resistance, and girls with premature exaggerated adrenarche appear to be at greater risk of developing PCOS as adults (Richard, 36327773-Androgen-Excess-Disorders-in-Women: 2006).
PCOS is characterized by hirsutism, virilism, hyperandrogenism, menstrual irregularities, chronic anovulation, obesity, insulin resistance, acanthosis nigricans, high concentrations of LH, and ovarian cysts.
Hyperandrogenism and insulin resistance appear to be primary lesions, and the other findings are secondary events. The hyperandrogenism in women with PCOS is of both ovarian and adrenal origin. The adrenal hyperandrogenism of PCOS resembles an exaggerated form of adrenarche, and girls with premature adrenarche are more likely to develop PCOS. A gain-offunction disorder in the pathway leading to the serine/threonine phosphorylation of P450c17 could account for such increases in both adrenal and ovarian androgen secretion and an earlier age of adrenarche, but such mutations have not yet been reported. The hyperinsulinism and insulin resistance of PCOS is at the level of insulin receptor signal transduction. Serine phosphorylation of the chain of the insulin receptor interferes with the tyrosine phosphorylation of the receptor that normally follows binding of insulin. Furthermore, some PCOS women appear to have insulin receptors in their fibroblasts that are hyperphosphorylated. Thus, a gainof-function mutation in a serine-threonine kinase or its signal transduction pathway might increase the serine hyperphosphorylation of both P450c17 and the chain of the insulin receptor, thus accounting for both the hyperandrogenism
and insulin resistance of PCOS with a single molecular lesion (Richard, 36327773-Androgen-Excess-Disorders-in-Women: 2006).
CONCLUSION The pathways of adrenal and ovarian steroid biosynthesis use the same enzymes for the initial steps of steroidogenesis, but express different enzymes that convert steroid precursors to the final active products. Both the adrenal and ovary produce DHEA as the key precursor of androgens and estrogens. The key enzyme in DHEA production is P450c17, which catalyzes both 17-hydroxylation and 17,20-lyase activities. The 17,20-lyase activity of human P450c17 strongly favors the 5 pathway, so that most human androgens and estrogens derive from DHEA. Consequently, understanding the biochemistry and regulation of P450c17, and in particular its 17,20-lyase activity, is central to understanding the
hyperandrogenism of PCOS.
REFERENCES
Anonim. _______ . http://www.healthywomen.org/condition/androgen. Diakses pada tanggal 01 Desember 2010 pukul 07.00 WIB
Deborah, et.al. 2004. 7270066-Sexuality-Androgen-Replacement-Women. USA: Elservier Inc
Richard, et.al. 2006. 36327773-Androgen-Excess-Disorders-in-Women. Totowa: Humana Press Inc.
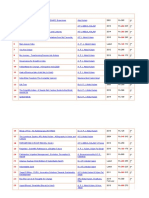
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Logic of English - Spelling Rules PDFDokumen3 halamanLogic of English - Spelling Rules PDFRavinder Kumar80% (15)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Materials System SpecificationDokumen14 halamanMaterials System Specificationnadeem shaikhBelum ada peringkat
- Extinct Endangered Species PDFDokumen2 halamanExtinct Endangered Species PDFTheresaBelum ada peringkat
- 2019 09 20 New Balance Harvard Business CaseDokumen7 halaman2019 09 20 New Balance Harvard Business CaseFrans AdamBelum ada peringkat
- Ruahsur Vangin Basket-Ball Court Lungrem ChimDokumen4 halamanRuahsur Vangin Basket-Ball Court Lungrem ChimchanmariansBelum ada peringkat
- Information Security Policies & Procedures: Slide 4Dokumen33 halamanInformation Security Policies & Procedures: Slide 4jeypopBelum ada peringkat
- Pa Print Isang Beses LangDokumen11 halamanPa Print Isang Beses LangGilbert JohnBelum ada peringkat
- Impact Grammar Book Foundation Unit 1Dokumen3 halamanImpact Grammar Book Foundation Unit 1Domingo Juan de LeónBelum ada peringkat
- Principles of Communication PlanDokumen2 halamanPrinciples of Communication PlanRev Richmon De ChavezBelum ada peringkat
- BirdLife South Africa Checklist of Birds 2023 ExcelDokumen96 halamanBirdLife South Africa Checklist of Birds 2023 ExcelAkash AnandrajBelum ada peringkat
- Genomics - FAODokumen184 halamanGenomics - FAODennis AdjeiBelum ada peringkat
- Thomas Noochan Pokemon Review Final DraftDokumen6 halamanThomas Noochan Pokemon Review Final Draftapi-608717016Belum ada peringkat
- 9francisco Gutierrez Et Al. v. Juan CarpioDokumen4 halaman9francisco Gutierrez Et Al. v. Juan Carpiosensya na pogi langBelum ada peringkat
- Design of Corn ThresherDokumen11 halamanDesign of Corn ThresherFrancisco ToroBelum ada peringkat
- MCS 033 NotesDokumen7 halamanMCS 033 NotesAshikBelum ada peringkat
- China Daily 20181031Dokumen24 halamanChina Daily 20181031JackZhangBelum ada peringkat
- Medicidefamilie 2011Dokumen6 halamanMedicidefamilie 2011Mesaros AlexandruBelum ada peringkat
- Soal Bahasa Inggris Sastra Semester Genap KLS Xi 2023Dokumen3 halamanSoal Bahasa Inggris Sastra Semester Genap KLS Xi 2023Ika Endah MadyasariBelum ada peringkat
- HTTP Parameter PollutionDokumen45 halamanHTTP Parameter PollutionSpyDr ByTeBelum ada peringkat
- KalamDokumen8 halamanKalamRohitKumarSahuBelum ada peringkat
- PHD Thesis - Table of ContentsDokumen13 halamanPHD Thesis - Table of ContentsDr Amit Rangnekar100% (15)
- Effect of Added Sodium Sulphate On Colour Strength and Dye Fixation of Digital Printed Cellulosic FabricsDokumen21 halamanEffect of Added Sodium Sulphate On Colour Strength and Dye Fixation of Digital Printed Cellulosic FabricsSumaiya AltafBelum ada peringkat
- Statistics NotesDokumen7 halamanStatistics NotesAhmed hassanBelum ada peringkat
- All Zone Road ListDokumen46 halamanAll Zone Road ListMegha ZalaBelum ada peringkat
- RESO NO. 4 - LANYARD FinalDokumen1 halamanRESO NO. 4 - LANYARD FinalsharonleefulloBelum ada peringkat
- Animal Welfare in Bangladesh and The Role of Obhoyaronno CaseDokumen11 halamanAnimal Welfare in Bangladesh and The Role of Obhoyaronno CaseZarin Tanjim WoyshorjoBelum ada peringkat
- L 1 One On A Page PDFDokumen128 halamanL 1 One On A Page PDFNana Kwame Osei AsareBelum ada peringkat
- Feuerhahn Funeral Bullet 17 March 2015Dokumen12 halamanFeuerhahn Funeral Bullet 17 March 2015brandy99Belum ada peringkat
- DMSCO Log Book Vol.25 1947Dokumen49 halamanDMSCO Log Book Vol.25 1947Des Moines University Archives and Rare Book RoomBelum ada peringkat
- Session Guide - Ramil BellenDokumen6 halamanSession Guide - Ramil BellenRamilBelum ada peringkat