Approach To Unconscious Patients
Diunggah oleh
Mary Joyce Ajero LadimoDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Approach To Unconscious Patients
Diunggah oleh
Mary Joyce Ajero LadimoHak Cipta:
Format Tersedia
Approach to Unconscious Patients Wakefulness depends on the integrity of both cerebral hemi- spheres and the ascending reticular
activating formation of the brain stem. The management of an unconscious patient is never an easy task in clinical practice The duty of physician is Arrive at diagnosis Predict the eventual outcome History i) Onset of coma (abrupt, gradual) ii) Recent complaints ( headache, depression, focal weakness, vertigo ) iii) Recent injury iv) Previous medical illness (diabetes,uremia, heart disease) v) Access to drugs ( sedatives,psychotropic drugs ) Examination General physical Examination i. Vital signs ii. Evidence of trauma iii. Evidence of acute or chronic system illness iv. Evidence of drug ingestion (needle marks alcohol breath) v. Nuchal rigidity (examine with care) Neurological Examination State of consciousness Obtundation: responds-to verbal stimuli although slow and inappropriate. Stupor: the subject can be aroused only by vigorous and repeated noxious stimuli. Coma: unarousable and unresponsive. Respiratory pattern a. Hyperventilation - midbrain and upper pons lesion metabolic diseases e.g. hepatic coma, diabetes and generalised increase in intracranial pressure in its early stages. b. Hypoventilation - medullary, upper cervical spinal lesion, drug overdose, and later stages of cerebral herniation. c. Cheyne-Stoke respiration usually diencephalic lesion, central transtentorial herniation and obstructive hydrocephalus. d. Ataxic respiration (completely irregular breathing) brain-stem dysfunction of a diffuse nature. Pupillary size and reaction Medium to dilated symmetrical pupils fixed to light: structural disease of the brain stem. Small symmetrical pupils reactive to light: metabolic diseases and drug overdose. Unequal pupil fixed to light: intracranial mass lesion producing 3rd nerve palsy e.g. in unilateral uncal herniation. Eye Movements Vestibulo-ocular reflexes douching of one ear with cold water produces ipsi-lateral deviation of both eyes with a contralateral quick phase nystagmus lasting for 1-2 minutes. Use of hot water produces the opposite effect i.e. contralateral deviation with ipsilateral quick phase nystagmus. Bilateral douching with cold water gives rise to downward deviation with upward nystagmus and with hot water the opposite response. Absence or abnormal response indicates brain-stem dysfunction. Oculo-cephalic reflexes (Doll's eye movement ) - Normal response consist of deviation of both eyes to the opposite direction of head rotation. Again absence or abnormal response indicates brain-stem dysfunction. Motor Responses This is elicited by applying peripheral noxious stimuli e.g. pinching of limbs rubbing the sternum to elicit pain.
a. Appropriate response brushing away the source of stimulus. b. Inappropriate response - decerebrate or decorticate rigidity. Motor response is also of localising value. Paralysed limb will show no response and presence of hemiplegia can therefore be evident. Decerebrate rigidity indicates brain-stem damage and if bilateral is usually associated with a very poor prognosis. Complete flaccidity with no response to noxious stimuli is often indicative of severe central nervous system depression due to drug overdose. Decorticate Laboratory Evaluation Supratentorial lesions Skull radiograph Computerised tomographic scan CTscan) Carotid angiography EEG ( electroencephalogram ) Infratentorial lesions Skull radiograph CT scan Vertebral angiography EEG Ventriculography Diffuse neuronal lesions Examination of CSF ( cerebro spinal fluid ) Serum glucose, calcium, Na, K, magnesium Blood gases and Ph Liver and renal functions Drug levels Management Initial Management Airway Breathing Circulation Deformity Exposure Definitive Management In general, management of the comatose patient depends on the cause. However, while thepatient is undergoing evaluation, it is essential to : pressure area care care of the mouth, eyes and skin physiotherapy to protect muscles and joints risks of deep vein thrombosis risks of stress ulceration of the stomach nutrition and fluid balance urinary catheterization monitoring of the CVS infection control maintenance of adequate oxygenation, with the assistance of artificial ventilation Examination Vital Signs 1.Pulse tachycardia Hypovolemia/hemorrhage hyperthermia Intoxication bradycardia Raised intracranial pressure Heart blocks
2.Temperature Increased Sepsis Meningitis ,encephalitis Malaria ,Pontine haemorrhage Decreased Hypoglycemia Hypothermia (less than 31 C) Myxedema Alcohol, barbiturate ,sedative or phenothiazine intoxication. 3.Blood pressure increased Hypertensive encephalopathy Cerebral hemorrhage Raised intracranial pressure Decreased Hypovolemia /hemorrhage Myocardial infarction Intoxication/poisoning Profound hypothyroidism, Addisonian crisis 4.Respiratory rate Increased(tachypnea) Pneumonia Acidosis (DKA, renal failure) Pulmonary embolism Respiratory failure Decreased Intoxication/poisoning Skin petechial rash Meningococcal meningitis Endocarditis Sepsis, thrombotic thrombocytopenic purpura Rickettsial infection RMS (rocky mountain spotted fever) Multiple injection marks Drug addiction Acute endocarditis Hepatitis B/C with encephalopathy HIV Neurological assessment; General posture Level of conciousness Posture Lack of movements on one side Intermittent twitching Multifocal myoclonus DECORTICATION DECEREBRATION Level of conciousness Glasgow coma scale (GCS) Best motor response Best verbal response Eye opening GCS score 3 severe injury
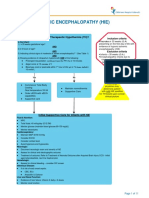
less than or equal to 8 moderate injury 9 to 12 minor injury An abbreviated coma scale is used in the assessment of critically ill patient (primary survey) AVPU A alert V respond to voice stimulus P respond to pain U - unresponsive Brainstem reflexes Pupillary responses to light Spontaneous and elicited eye movements Corneal responses Respiratory movements Ocular Movements Conjugate deviation of eyes to a side ipsilateral hemisphere frontal lesion or contralateral pontine lesion. Rarely eyes may turn paradoxically away from the side of deep hemisphere lesion (WRONG-WAY EYES) Downward conjugate deviation of eyes mesencephalic lesion. Oculocephalic reflex (Dolls eyes response) brisk in cortical depression, lost in brainstem lesion. Oculovestibulo responses two components 1.Conjugate ocular movement lost in brainstem damage. 2.Nystagmus loss in damage to cerebral hemisphere Pupillary Changes Respiratory movements Has less localizing value than other brainstem reflexes. Cheyen-stokes respiration(classic cyclic form ending with a brief apneic period B/L hemisphere damage or metabolic depression. Rapid ,deep breathing (Kussmauls) in metabolic acidosis and in pontomesencephalic lesion. Neck rigidity; Meningitis Subarachnoid hemorrhage Fundoscopy Raised intracranial pressure Hypertensive changes Subarachnoid hemorrhage Diabetic retinopathy History Onset of the symptoms Antecedent symptoms Use of medications Chronic liver, kidney, lung or heart disease CAUSES OF UNCONCIOUSNESS Causes of unconsciousness Metabolic Drugs, poisoning e.g. alcohol Hypoglycemia, hyperglycemia (keto acidotic state) Hypoxia (COPD) Septicemia Hypothermia Myxedema ,addisonian crisis Hepatic/uremic encephalopathies Neurological Trauma Infections meningitis, encephalitis, malaria, typhoid, rabies. Tumors cerebral/meningeal tumors
Vascular subdural / subarachnoid hemorrhage, stroke, hypertensive encephalopathy Epilepsy nonconvulsive status Summary ABC of life support Oxygen and I.V access Stabilize cervical spine Blood glucose Control seizures Consider I.V glucose, thiamine, naloxone, flumazenil Brief examination and obtain history Investigate Reassess the situation and plan further Discharge Plan/Health Teaching Early management Prompt diagnosis Increased ICP Normal range: 5 13 mmHg Collaborative Management for Clients with Increased ICP Semi-fowlers position, lateral position Adequate oxygenation Safety Rest Avoid factors that increased ICP such as nausea and vomiting, valsalva maneuver, oversuctioning, restraints application, rectal examination, enema, and bending or stooping Continuation Control hypertension Restrict fluid intake Pharmacotherapy Pharmacotherapy Mannitol Lasix (furosemide) Decadron (dexamethasone) Anticonvulsants (Diazepam, Dilantin,Phenobarbital, Tegretol) Antacids Histamine- H2 blocker antagonist anticoagulants Care of the Client with Altered Levels of Consciousness Maintain stimulation Maintain nutrition Maintain elimination Maintain circulation Maintain normal body temperature Promote safety Promote activity Maintain skin integrity Maintain good hygiene Support family
Anda mungkin juga menyukai
- Book Index The Art of Heavy TransportDokumen6 halamanBook Index The Art of Heavy TransportHermon Pakpahan50% (2)
- Wang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Dokumen961 halamanWang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Paritosh PandeyBelum ada peringkat
- Rachel Joyce - A Snow Garden and Other Stories PDFDokumen118 halamanRachel Joyce - A Snow Garden and Other Stories PDFИгорь ЯковлевBelum ada peringkat
- Neuro CH 14 Study GuideDokumen9 halamanNeuro CH 14 Study GuideMichael J MillerBelum ada peringkat
- PAS Quick GuideDokumen1 halamanPAS Quick GuideTracyBelum ada peringkat
- Dharmakirti39s Commentary On ChakrasamvaraDokumen15 halamanDharmakirti39s Commentary On ChakrasamvaraThiago AlbuquerqueBelum ada peringkat
- Neuro Disorders Study OutlineDokumen9 halamanNeuro Disorders Study OutlineHeather Russell100% (1)
- Hepatic Encephalopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHepatic Encephalopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPenilaian: 4 dari 5 bintang4/5 (1)
- Hepatic Encephalopathy: Causes, Tests, and Treatment OptionsDari EverandHepatic Encephalopathy: Causes, Tests, and Treatment OptionsPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- 1228 HFStroke Altered Neuro 2011Dokumen74 halaman1228 HFStroke Altered Neuro 2011Cyndy EnterlineBelum ada peringkat
- Assessing Neurologic FunctionsDokumen10 halamanAssessing Neurologic FunctionsDenise DizonBelum ada peringkat
- Downtime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimeDokumen5 halamanDowntime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimerupaliBelum ada peringkat
- Hypoxic Ischemic Encephalopathy (Hie) : AlgorithmDokumen11 halamanHypoxic Ischemic Encephalopathy (Hie) : AlgorithmAndreiMunteanuBelum ada peringkat
- How To Treat: Septic ShockDokumen6 halamanHow To Treat: Septic ShockmeeandsoeBelum ada peringkat
- Weekly Clinical Prep Packet 12 REVISEDDokumen12 halamanWeekly Clinical Prep Packet 12 REVISEDMei SarteBelum ada peringkat
- An Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFDokumen6 halamanAn Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFkatherine dayagBelum ada peringkat
- Hepatic EncephalopathyDokumen21 halamanHepatic Encephalopathydhanya jayan100% (1)
- NURS 225V Principles III Data Collection ToolDokumen2 halamanNURS 225V Principles III Data Collection ToolKrisBelum ada peringkat
- Fluids and Electrolytes Lesson Outline For BBDokumen14 halamanFluids and Electrolytes Lesson Outline For BBdlneisha61100% (1)
- DDX NeuroradiologyDokumen12 halamanDDX NeuroradiologyTuan NguyenBelum ada peringkat
- Review 2Dokumen12 halamanReview 2Christine Rubio100% (1)
- ThrombocytopeniaDokumen1 halamanThrombocytopeniaanum786110Belum ada peringkat
- CASE 1 Neuro PDFDokumen23 halamanCASE 1 Neuro PDFthe KLAWBelum ada peringkat
- Lab Workup: Practical Nursing Mohawk College 2014Dokumen2 halamanLab Workup: Practical Nursing Mohawk College 2014Pawel PietruszczakBelum ada peringkat
- Ostomias PDFDokumen17 halamanOstomias PDFRicardo Uzcategui Arregui100% (1)
- Pulmonary Clinic History and PhysicalDokumen3 halamanPulmonary Clinic History and Physicale-MedTools100% (5)
- Area Technique Normal Findings Analysis and Interpretation A. SkullDokumen7 halamanArea Technique Normal Findings Analysis and Interpretation A. Skullkingawesome21100% (1)
- Final Assessing Female and Male Genitourinary SystemDokumen7 halamanFinal Assessing Female and Male Genitourinary SystemJo Marchianne PigarBelum ada peringkat
- Cerebral Vascular Accident (Stroke)Dokumen5 halamanCerebral Vascular Accident (Stroke)SN. CaRBelum ada peringkat
- Ragasa - Neurologic DisordersDokumen51 halamanRagasa - Neurologic DisordersremeroseBelum ada peringkat
- Sign and SymptomsDokumen8 halamanSign and SymptomsCaral Grace Gatdula-PenalbaBelum ada peringkat
- Blood Sample Normal Panic Values For Abgs: Clinical SignificanceDokumen7 halamanBlood Sample Normal Panic Values For Abgs: Clinical SignificancegeonarcisoBelum ada peringkat
- IV Solutions CheatsheetDokumen1 halamanIV Solutions CheatsheetYelle QuilatanBelum ada peringkat
- SHOCK Slide WorkbookDokumen10 halamanSHOCK Slide WorkbookPATHMAPRIYA GANESANBelum ada peringkat
- Vital Signs 1Dokumen2 halamanVital Signs 1carlyBelum ada peringkat
- Pead 3 - Abdominal Pain and VommitingDokumen22 halamanPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- ShockDokumen9 halamanShockapocruBelum ada peringkat
- Sepsis Quick Reference GuideDokumen1 halamanSepsis Quick Reference GuideRavin DebieBelum ada peringkat
- Abdomenal Exam HandoutDokumen5 halamanAbdomenal Exam HandoutNesma AdelBelum ada peringkat
- Medical Abbreviations: Beautiful Nursing LLCDokumen2 halamanMedical Abbreviations: Beautiful Nursing LLCcarlyBelum ada peringkat
- HypertensionDokumen19 halamanHypertensionmr_coolz282344Belum ada peringkat
- Nur 111 Session 6 Sas 1Dokumen12 halamanNur 111 Session 6 Sas 1Zzimply Tri Sha UmaliBelum ada peringkat
- Journal Herpes Simplex EncephalitisDokumen2 halamanJournal Herpes Simplex EncephalitissavinaumarBelum ada peringkat
- Physical and Neurological ExaminationDokumen7 halamanPhysical and Neurological ExaminationMelissa Marie SkillingsBelum ada peringkat
- Patient Care SkillsDokumen15 halamanPatient Care SkillsIts John100% (1)
- Pediatric Cardio-Respiratory AssessmentDokumen9 halamanPediatric Cardio-Respiratory AssessmentRicky SpideyBelum ada peringkat
- Vital Sign Na (1) by ZWBDokumen52 halamanVital Sign Na (1) by ZWBAshraf Ali100% (1)
- PericarditisDokumen29 halamanPericarditisPavin KumarBelum ada peringkat
- Basic Neuroanatomy and Stroke Syndromes PDFDokumen15 halamanBasic Neuroanatomy and Stroke Syndromes PDFFrancisco A. Villegas-López100% (2)
- Disease and Drug Consult Neurology DisordersDokumen447 halamanDisease and Drug Consult Neurology DisordersÁi MỹBelum ada peringkat
- Medical AbbreviationsDokumen7 halamanMedical AbbreviationsBilly Braine Kho BanlatBelum ada peringkat
- Charting Terminology 2Dokumen11 halamanCharting Terminology 2Danielle ShullBelum ada peringkat
- MS Final 46 Blood or Lymphatic DisorderDokumen4 halamanMS Final 46 Blood or Lymphatic DisorderZachary T Hall0% (1)
- Adrenal Insufficiency and Addison's DiseaseDokumen8 halamanAdrenal Insufficiency and Addison's DiseaseyancefinceBelum ada peringkat
- UNIT: Internal Medicine REG NO.: BMS/2014/72732 DATE: 30/7/2021 ASSIGNMENT: Status EpilepticusDokumen10 halamanUNIT: Internal Medicine REG NO.: BMS/2014/72732 DATE: 30/7/2021 ASSIGNMENT: Status EpilepticusGladys MainaBelum ada peringkat
- ASSESSMENT FORM: Spring 2006 Client's Number: InstructionsDokumen6 halamanASSESSMENT FORM: Spring 2006 Client's Number: Instructionsdenisemw88Belum ada peringkat
- PD OSCE GuideDokumen19 halamanPD OSCE GuideChorong ParkBelum ada peringkat
- Basic Nursing SkillDokumen6 halamanBasic Nursing SkillIsmawatiBelum ada peringkat
- How Do I Diagnose The Cause of A Cough of Less Than 3 Weeks' Duration?Dokumen14 halamanHow Do I Diagnose The Cause of A Cough of Less Than 3 Weeks' Duration?Sudhir TyagiBelum ada peringkat
- Hypertension Potassium: DO NOT Delegate What You Can EAT! E - Evaluate A - Assess T - TeachDokumen35 halamanHypertension Potassium: DO NOT Delegate What You Can EAT! E - Evaluate A - Assess T - TeachEsterly Puracan AmparoBelum ada peringkat
- Conduct of Physical Examination: I. General SurveyDokumen10 halamanConduct of Physical Examination: I. General SurveyWeng RamojalBelum ada peringkat
- Airway and The NurseDokumen7 halamanAirway and The NursecarmenbuleandraBelum ada peringkat
- I Got the Flu! What is Influenza? - Biology Book for Kids | Children's Diseases BooksDari EverandI Got the Flu! What is Influenza? - Biology Book for Kids | Children's Diseases BooksBelum ada peringkat
- Conquest CXAX Air-to-Water Heat PumpDokumen6 halamanConquest CXAX Air-to-Water Heat PumpAlexandre LopesBelum ada peringkat
- Dna Adduct As Biomarker: Prof. Dr. Yahdiana Harahap, MS, AptDokumen68 halamanDna Adduct As Biomarker: Prof. Dr. Yahdiana Harahap, MS, AptNadia AaqilahBelum ada peringkat
- Basics of Population EducationDokumen4 halamanBasics of Population EducationLAILANIE DELA PENABelum ada peringkat
- Discrete Wavelet TransformDokumen10 halamanDiscrete Wavelet TransformVigneshInfotechBelum ada peringkat
- Worksheet - 143760187HS-II, TUTORIAL ON CH-5Dokumen14 halamanWorksheet - 143760187HS-II, TUTORIAL ON CH-5A MusaverBelum ada peringkat
- BITS Pilani: Determination of Extreme Pressure, Wear Preventive Characteristics of Lubricants Using Four Ball TesterDokumen10 halamanBITS Pilani: Determination of Extreme Pressure, Wear Preventive Characteristics of Lubricants Using Four Ball Testerakash chBelum ada peringkat
- Tips For A Healthy PregnancyDokumen2 halamanTips For A Healthy PregnancyLizaBelum ada peringkat
- Ecological Quality RatioDokumen24 halamanEcological Quality RatiofoocheehungBelum ada peringkat
- Clocks (New) PDFDokumen5 halamanClocks (New) PDFAbhay DabhadeBelum ada peringkat
- The Manufacture and Uses of Expanded Clay Aggregate: Thursday 15 November 2012 SCI HQ, LondonDokumen36 halamanThe Manufacture and Uses of Expanded Clay Aggregate: Thursday 15 November 2012 SCI HQ, LondonVibhuti JainBelum ada peringkat
- Bchem 455 - Module 3Dokumen42 halamanBchem 455 - Module 3WilliamBelum ada peringkat
- Para Lec CombinedDokumen83 halamanPara Lec CombinedClent Earl Jason O. BascoBelum ada peringkat
- Tabla de Avances de AcesoriosDokumen3 halamanTabla de Avances de AcesoriosPedro Diaz UzcateguiBelum ada peringkat
- Petersen Coils Basic 20principle and ApplicationDokumen3 halamanPetersen Coils Basic 20principle and ApplicationasotozuazuaBelum ada peringkat
- Statics: Vector Mechanics For EngineersDokumen39 halamanStatics: Vector Mechanics For EngineersVijay KumarBelum ada peringkat
- Preview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextDokumen24 halamanPreview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextFelipe AguilarBelum ada peringkat
- English2 Q2 Summative Assessment 4 2Dokumen4 halamanEnglish2 Q2 Summative Assessment 4 2ALNIE PANGANIBANBelum ada peringkat
- 1.1.3.12 Lab - Diagram A Real-World ProcessDokumen3 halaman1.1.3.12 Lab - Diagram A Real-World ProcessHalima AqraaBelum ada peringkat
- V. Jovicic and M. R. Coop1997 - Stiffness, Coarse Grained Soils, Small StrainsDokumen17 halamanV. Jovicic and M. R. Coop1997 - Stiffness, Coarse Grained Soils, Small StrainsxiangyugeotechBelum ada peringkat
- SMC VM Eu PDFDokumen66 halamanSMC VM Eu PDFjoguvBelum ada peringkat
- 23001864Dokumen15 halaman23001864vinodsrawat33.asiBelum ada peringkat
- Nomenclatura SKFDokumen1 halamanNomenclatura SKFJuan José MeroBelum ada peringkat
- Investigation of Skew Curved Bridges in Combination With Skewed Abutments Under Seismic ResponseDokumen5 halamanInvestigation of Skew Curved Bridges in Combination With Skewed Abutments Under Seismic ResponseEditor IJTSRDBelum ada peringkat
- Welcome To Our 2Nd Topic: History of VolleyballDokumen6 halamanWelcome To Our 2Nd Topic: History of VolleyballDharyn KhaiBelum ada peringkat
- Integration ConceptDokumen34 halamanIntegration ConceptJANELLA ALVAREZBelum ada peringkat
- PH & TemperatureDokumen8 halamanPH & TemperatureNanaBelum ada peringkat