Ebook - Cecil Ed23 - 2
Diunggah oleh
Carlos Alan LopezDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Ebook - Cecil Ed23 - 2
Diunggah oleh
Carlos Alan LopezHak Cipta:
Format Tersedia
Chapter 58 - HEART FAILURE: MANAGEMENT AND PROGNOSIS fr... http://remoto.dgb.uanl.mx:2065/das/book/body/108023714-4/0/1492/251...
Use of this content is subject to the Terms and Conditions
Goldman: Cecil Medicine, 23rd ed.
Copyright © 2007 Saunders, An Imprint of Elsevier
Chapter 58 – HEART FAILURE: MANAGEMENT AND PROGNOSIS
John J.V. McMurray
Marc A. Pfeffer
EVALUATION AND MANAGEMENT OF HEART FAILURE
Heart failure is an overarching term for a syndrome (i.e., a constellation of signs and symptoms) that encompasses a vast spectrum of
cardiovascular disorders and is associated with a greatly heightened risk of death and nonfatal adverse cardiovascular events ( Chapter 57
). Treatment is initially directed toward prevention of cardiac injury (e.g., due to hypertension or myocardial infarction) or toward limiting
structural progression if cardiac damage has already occurred (e.g., left ventricular remodeling with declining left ventricular ejection
fraction) and delaying the development of symptomatic heart failure. Once symptoms develop, treatments are also directed at improving
functional status as well as prognosis.
Approximately one in five adults will develop heart failure. In the United States, the nearly 1 million annual hospitalizations with a primary
diagnosis of heart failure account for 5 million hospital days. The estimated cost of heart failure management ranges from $15 billion to $40
billion annually, depending on the formula used.
Randomized controlled clinical trials (RCTs) supply the framework for quantifying what different therapeutic approaches can offer. Even
when they are definitive, RCTs only generate data about average risks and benefits of the tested therapeutic option in a selected cohort.
Because an individual patient's responses can only be implied from the overall estimated group responses, RCTs cannot definitively direct
the approach of every patient or answer the myriad questions that confront the practitioner regarding the specific circumstances of the
patient. Another major limitation of RCTs is the relatively narrow time frame of observation, generally only months to several years,
compared with epidemiologic experiences during decades. Despite these limitations, RCTs are the premier tool of evidence-based
medicine, and the field of heart failure has fortunately been the focus of relatively high quality RCTs that have provided robust evidence to
improve clinical care and prognosis ( Table 58-1 ). Indeed, the implementation of evidence from RCTs into clinical practice has resulted in
impressive temporal improvements in survival after discharge from a first hospital admission for heart failure. Moreover, the age at which
symptomatic heart failure first becomes evident has increased. Despite these tangible advances, heart failure continues to be a leading
cause of morbidity and mortality in the elderly.
TABLE 58-1 -- CONTROLLED TRIALS [*] IN SYMPTOMATIC HEART FAILURE WITH REDUCED SYSTOLIC FUNCTION
Events Prevented per
1000 Patients
Trial, Estimated Relative Treated [¶¶]
Treatment, Severity of First-Year Trial Risk DEATH
and Year Heart Placebo/Control Background Treatment Duration Primary Reduction HF OR HF
Published N Failure Group Mortality Treatment [†] Added (years) End Point (%) [‡] DEATH HOSP. HOSP.
ACE INHIBITORS
CONSENSUS, 253 End stage 52 Spironolactone Enalapril, 20 0.54 [‡] Death 40 146 — —
1987 [a] mg bid
SOLVD-T, 2569 Mild-severe 15.7 — Enalapril, 20 3.5 Death 16 45 96 108
1991 [b] mg bid
β-BLOCKERS
CIBIS-2, 2647 Moderate- 13.2 ACE-I Bisoprolol, 1.3 [‡] Death 34 55 56 —
1999 [c] severe 10 mg qd
MERIT-HF, 3991 Mild-severe 11.0 ACE-I Metoprolol 1.0 [‡] Death 34 36 46 63
1999 [d] CR/XL, 200
mg qd
COPERNICUS, 2289 Severe 19.7 ACE-I Carvedilol, 0.87 [‡] Death 35 55 65 81
2001 [e] 25 mg bid
ANGIOTENSIN RECEPTOR BLOCKERS
Val-HeFT, 5010 Mild-severe ~8.0 ACE-I Valsartan, 1.9 CV death 13 0 35 33 [¶]
2001 [8] 160 mg bid or
morbidity
CHARM- 2028 Mild-severe 12.6 BB Candesartan, 2.8 CV death 23 30 31 60
Alternative, 32 mg qd or HF
2003 [7] hosp.
1 de 3 21/10/2008 11:34 a.m.
Chapter 58 - HEART FAILURE: MANAGEMENT AND PROGNOSIS fr... http://remoto.dgb.uanl.mx:2065/das/book/body/108023714-4/0/1492/251...
Events Prevented per
1000 Patients
Trial, Estimated Relative Treated [¶¶]
Treatment, Severity of First-Year Trial Risk DEATH
and Year Heart Placebo/Control Background Treatment Duration Primary Reduction HF OR HF
Published N Failure Group Mortality Treatment [†] Added (years) End Point (%) [‡] DEATH HOSP. HOSP.
CHARM- 2548 Moderate- 10.6 ACE-I + BB Candesartan, 3.4 CV death 15 28 47 39
Added, severe 32 mg qd or HF
2003 [9] hosp.
ALDOSTERONE BLOCKADE
RALES, 1663 Severe ~25 ACE-I Spirolactone, 2.0 [‡] Death 30 113 95 —
1999 [11] 25–50 mg qd
HYDRALAZINE-ISDN
V-HeFT-1, 459 Mild-severe 26.4 — Hydralazine, 2.3 Death 34 52 0 —
1986 [f] 75 mg tid-qid
ISDN, 40 mg
qid
A-HeFT, 1050 Moderate- ~9.0 ACE-I + BB + Hydralazine, 0.83 [‡] Composite — 40 80 —
2004 [14] severe spironolactone 75 mg tid
ISDN, 40 mg
tid
DIGITALIS GLYCOSIDES
DIG, 1997 [13] 6800 Mild-severe ~11.0 ACE-I Digoxin 3.1 Death 0 0 79 73
CRT
COMPANION, 925 Moderate- 19.0 ACE-I + BB + CRT 1.35 [‡] Death or 19 38 — 87
2004 [17] severe spironolactone any
hospital
admission
CARE-HF, 813 Moderate- 12.6 ACE-I + BB + CRT 2.45 Death or 37 97 151 184
2005 [g] severe spironolactone CV
hospital
admission
CRT-D
COMPANION, 903 Moderate- 19.0 ACE-I + BB + CRT-ICD 1.35 [‡] Death or 20 74 — 114
2004 [17] severe spironolactone any
hospital
admission
IMPLANTABLE CARDIOVERTER DEFIBRILLATOR
SCD-HeFT, 1676 Mild-severe ~7.0 ACE-I + BB ICD 3.8 Death 23 — — —
2005 [16]
VENTRICULAR ASSIST DEVICE
REMATCH, 129 End stage 75 ACE-I + LVAD 1.8 Death 48 282 — —
2001 [h] spironolactone
Modified from McMurray JJ, Pfeffer MA: Heart failure. Lancet 2005;365:1877–1889.
ACE-I = ACE inhibitor; BB = β-blocker; CRT = cardiac resynchronization therapy (biventricular pacing); CRT-D = CRT device that also
defibrillates; CV = cardiovascular; HF hosp. = patients with at least one hospital admission for worsening heart failure—some patients had
multiple admissions; ICD = implantable cardioverter defibrillator; ISDN = isosorbide dinitrate; LVAD = left ventricular assist device.
* Excluding active-controlled trials.
† In more than one third of patients, ACE-I + BB means that ACE inhibitors were used in almost all patients and BB in the majority; most patients were also taking
diuretics, and many digoxin (except in DIG). Spirono-lactone was used at baseline in 5% Val-HeFT, 8% MERIT-HF, 17% CHARM-Added, 19% SCD-HeFT, 20%
COPERNICUS, and 24% CHARM-Alternative.
‡ Relative risk reduction in primary end point. §Stopped early for benefit.
¶¶ Individual trials may not have been designed or powered to evaluate effect of treatment on these outcomes.
¶ Primary end point that also included treatment of heart failure with intravenous drugs for 4 hours or more without admission and resuscitated cardiac arrest (both added
small numbers).
2 de 3 21/10/2008 11:34 a.m.
Chapter 58 - HEART FAILURE: MANAGEMENT AND PROGNOSIS fr... http://remoto.dgb.uanl.mx:2065/das/book/body/108023714-4/0/1492/251...
a The CONSENSUS Trial Study Group: Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril
Survival Study (CONSENSUS). N Engl J Med 1987;316:1429–1435.
b The SOLVD Investigators: Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med
1991;325:293–302.
c The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): A randomised trial. Lancet 1999;353:9–13.
d Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet
1999;353:2001–2007.
e Packer M, Coats AJ, Fowler MB, et al: Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651–1658.
f Cohn JN, Archibald DG, Ziesche S, et al: Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative
Study. N Engl J Med 1986;314:1547–1552.
g Cleland JG, Daubert JC, Erdmann E, et al: The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352:1539–1549.
h Rose EA, Gelijns AC, Moskowitz AJ, et al: Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med 2001;345:1435–1443.
Copyright © 2008 Elsevier Inc. All rights reserved. - www.mdconsult.com
Bookmark URL: /das/book/0/view/1492/251.html
3 de 3 21/10/2008 11:34 a.m.
Anda mungkin juga menyukai
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Ebook - Fisiopato Braunwald Cardio - 2Dokumen2 halamanEbook - Fisiopato Braunwald Cardio - 2Carlos Alan Lopez100% (1)
- Diagnostico HF 2004Dokumen8 halamanDiagnostico HF 2004Carlos Alan Lopez100% (1)
- MyPyramid AnatomyDokumen1 halamanMyPyramid AnatomyCarlos Alan LopezBelum ada peringkat
- Ob GdlnsDokumen262 halamanOb Gdlnsapi-3728652Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1091)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Arrhythmias Types, Pathophysiology AtfDokumen9 halamanArrhythmias Types, Pathophysiology AtfAmir mohammad moori MohammadiBelum ada peringkat
- Chest TraumaDokumen47 halamanChest Traumafrenee aradanasBelum ada peringkat
- MCCQE CollectionDokumen103 halamanMCCQE Collectionleo_toronto100% (10)
- Coronary Artery Calcium: CirculationDokumen5 halamanCoronary Artery Calcium: CirculationAlice Valeria WiyonoBelum ada peringkat
- OK - Modul Ortho - Bone Cement Implantation SyndromeDokumen18 halamanOK - Modul Ortho - Bone Cement Implantation SyndromeWanditoGayuhUtomoBelum ada peringkat
- Ebook Ebook PDF Principles of Human Physiology 6th Edition PDFDokumen41 halamanEbook Ebook PDF Principles of Human Physiology 6th Edition PDFdonita.nichols650100% (36)
- Allen: (Conceptual Questions)Dokumen24 halamanAllen: (Conceptual Questions)Sachin Kumar GautamBelum ada peringkat
- Sotry Board Dan ScriptDokumen4 halamanSotry Board Dan Scriptnuex01Belum ada peringkat
- CNA Exam Notes PDFDokumen7 halamanCNA Exam Notes PDFErin100% (3)
- PALS Provider ManualDokumen51 halamanPALS Provider Manualdanix manaliliBelum ada peringkat
- Shu Physical AssessmentDokumen3 halamanShu Physical AssessmentJulbert Ian MejicaBelum ada peringkat
- Physical Fitness PPT NewDokumen19 halamanPhysical Fitness PPT Newg12001 Stella Marie MaristelaBelum ada peringkat
- Physiology Paper 1 Question BankDokumen8 halamanPhysiology Paper 1 Question BankVeshalinee100% (1)
- ABS-Anatomy of The ThoraxDokumen52 halamanABS-Anatomy of The ThoraxAtti Tamas100% (1)
- College of Nursing: Pharmacological ManagementDokumen4 halamanCollege of Nursing: Pharmacological ManagementBianca Mikaela DosdosBelum ada peringkat
- Cardiac Tamponade 2Dokumen23 halamanCardiac Tamponade 2Jethro Floyd QuintoBelum ada peringkat
- Patient Monitoring System Using GSM For Hospitals and Old Age HomesDokumen5 halamanPatient Monitoring System Using GSM For Hospitals and Old Age Homesvgmanjunatha100% (1)
- Assessment V 4Dokumen12 halamanAssessment V 4spam100% (1)
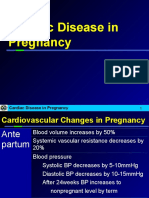
- Cardiac Disease in PregnancyDokumen21 halamanCardiac Disease in PregnancyRenata CilestrinaBelum ada peringkat
- Common Valvular Heart Disease (At A Glance)Dokumen1 halamanCommon Valvular Heart Disease (At A Glance)Tamim IshtiaqueBelum ada peringkat
- David Montgomery MD PHD BioDokumen2 halamanDavid Montgomery MD PHD Biolilsowell89Belum ada peringkat
- AQA A Level Biology Unit 1 NotesDokumen17 halamanAQA A Level Biology Unit 1 NotesMuadh Chati100% (3)
- First AidDokumen1.202 halamanFirst AidAnonymous QVovunM100% (17)
- Ncm101rle - Midterm ReviewerDokumen15 halamanNcm101rle - Midterm RevieweraragonjonathanryanabcomBelum ada peringkat
- Nbme 1Dokumen77 halamanNbme 1Rezo BagashviliBelum ada peringkat
- Learning Activity Worksheet Science 9 Q1 Weeks 1 2Dokumen7 halamanLearning Activity Worksheet Science 9 Q1 Weeks 1 2GINALYNROSE ROSIQUEBelum ada peringkat
- Benefits of Ajwa Dates.Dokumen1 halamanBenefits of Ajwa Dates.mamun31Belum ada peringkat
- Pig Human Comparison PDFDokumen15 halamanPig Human Comparison PDFBoban ArsovskiBelum ada peringkat
- NiSchool - PaediatricsDokumen48 halamanNiSchool - PaediatricsNurul Izzah AzmiBelum ada peringkat
- AQA A2 Biology Revision NotesDokumen46 halamanAQA A2 Biology Revision NotesShiv SongaraBelum ada peringkat