Diabetes Herbs
Diunggah oleh
JY MarDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Diabetes Herbs
Diunggah oleh
JY MarHak Cipta:
Format Tersedia
PHYTOTHERAPY RESEARCH Phytother. Res. 17, 11271134 (2003) Published online 11 November 2003 in Wiley InterScience (www.interscience.wiley.com).
DOI: 10.1002/ptr.1398 ANTIDIABETIC HERBAL DRUGS
1127
REVIEW ARTICLE
Antidiabetic Herbal Drugs Ofcially Approved in China
Wei Jia1*, Wenyuan Gao2 and Lida Tang3
1 2
The School of Pharmacy, Shanghai Jiao Tong University, Shanghai, China The College of Pharmaceutical Science and Technology, Tianjin University, Tianjin, China 3 Tianjin Institute of Pharmaceutical Research, Tianjin, China
Over the centuries, Chinese herbal drugs have served as a major source of medicines for the prevention and treatment of diseases including diabetes mellitus (known as Xiao-ke). It is estimated that more than 200 species of plants exhibit hypoglycaemic properties, including many common plants, such as pumpkin, wheat, celery, wax guard, lotus root and bitter melon. To date, hundreds of herbs and traditional Chinese medicine formulas have been reported to have been used for the treatment of diabetes mellitus. This paper provides a brief review of the antidiabetic drugs of plant origin that have been approved by the Chinese health regulatory agency for commercial use in China. It was believed, through pharmacological studies, that medicinal herbs were meticulously organized in these antidiabetic drug formulas such that polysaccharide containing herbs restore the functions of pancreatic tissues and cause an increase in insulin output by the functional beta cells, while other ingredients enhance the microcirculation, increase the availability of insulin and facilitate the metabolism in insulin-dependent processes. Pharmacological and clinical evaluations indicated that these drugs had a mild, but signicant, blood glucose lowering effect and that the long-term use of these agents may be advantageous over chemical drugs in alleviating some of the chronic diseases and complications caused by diabetes. Additionally, the use of these natural agents in conjunction with conventional drug treatments, such as a chemical agent or insulin, permits the use of lower doses of the drug and/or decreased frequency of administration which decreases the side effects most commonly observed. Copyright 2003 John Wiley & Sons, Ltd.
Keywords: diabetes mellitus; traditional Chinese medicine; antidiabetic drugs; herbal medicines.
INTRODUCTION Diabetes mellitus is a chronic condition in which patients may turn to alternative remedies that are purported to improve glycaemic control. The disease is characterized by symptomatic glucose intolerance as well as alterations in lipid and protein metabolism. The long-term complications of untreated or ineffectively treated diabetes include retinopathy, nephropathy and peripheral neuropathy. In addition, diabetic patients have an increased risk of cardiovascular disease and stroke (Guan et al., 2000; Geng and Wang, 1997). Therefore, there is a strong need for safe and effective oral hypoglycaemic agents that provide the clinician with a wider range of options for preventing, treating and managing diabetes. Many herbal extracts or derivatives have been documented in traditional Chinese medicine (TCM) as having clinical effectiveness in treating sugar imbalances in diabetes mellitus. Other extracts and derivatives have been found effective in treating water retention problems that often accompany diabetes. Some representative medicinal herbs listed below are routinely prescribed in TCM for the treatment of diabetes (Guan et al., 2000; Reid, 1999).
* Correspondence to: Dr Wei Jia, The School of Pharmacy, Shanghai Jiao Tong University, 1954 Huashan Road, Shanghai, 200030, P. R. China. E-mail: weijia@mail.sjtu.edu.cn Copyright 2003 John Wiley & Sons, Ltd. Copyright 2003 John Wiley & Sons, Ltd.
Achyranthes bidentata (Twotooth Achyranthes Root) Alisma orientale (Oriental Waterplantain Rhizome) Anemarrhena asphodeloides (Common Anemarrhena Rhizome) Asparagus cochinchinensis (Cochinchinese Asparagus Root) Astragaus membranaceus (Milkvetch Root) Atractylodes macrocephala (Largehead Atractylodes Rhizome) Bupleurum chinense (Chinese Thorowax Root) Cinnamomum cassia (Cassia Bark) Coptis chinensis (Coptis Root) Cornus ofcinalis (Asiatic Cornelian Cherry Fruit) Cucurbita moschata (Cushaw Seed) Dioscorea opposita (Common Yam Rhizome) Eriobotrya japonica (Loquat Leaf) Forsythia suspensa (Weeping Forsythia Capsule) Lonicera japonica Thunb. (Honeysuckle Flower) Morus alba (Mulberry Leaf) Ophiopogon japonicaus (Dwarf Lilyturf Tuber) Panax ginseng (Ginseng) Phragmites communis (Reed Rhizome) Pinellia ternata (Pinellia Tuber) Polygonum cuspidatum (Giant Knotweed Rhizome) Polygonum multiorum (Fleeceower Root) Poria cocos (Indian Bread) Pueraria lobata (Lobed Kudzuvine Root) Rehmannia glutinosa (Chinese Foxglove Root) Scrophularia ningpoensis (Figwort Root)
Received 11 June 2003 Phytother. Res. 17, 11271134 (2003) Accepted 18 June 2003
1128
W. JIA ET AL.
It is estimated that more than 200 species of plants exhibit hypoglycaemic properties, including many common plants, such as pumpkin, wheat, celery, wax guard, lotus root and bitter melon (Guan et al., 2000). To date, there are hundreds of herbs and formulas reported to have been used in traditional Chinese medicine (TCM) for the treatment of diabetes mellitus. Although each of the above listed medicinal herbs has antidiabetic effectiveness, Chinese herbal drugs are used preferably in combinations, i.e. each formula comprises several herbs or plants, to enhance the action of the main herbs, and to mitigate the toxic side effects of the principal component herbs. This paper will discuss the herbal antidiabetic drug products that have been approved by the Chinese health regulatory agency (known as State Drug Administration, SDA) for commercial use. Thus far, there are seven antidiabetic drug products of plant origin that have been approved for clinical use in China (Shang, 2000). Table 1 lists all these approved products and the composition of the formulas.
system; (2) stimulate liver functions, including synthesis of RNA, DNA and vital proteins; (3) regulate blood glucose levels; (4) regulate white and red blood cell counts; (5) relieve fatigue and increase cerebral circulation; and (6) antioxidant properties (Reid, 1999). Yu-san-xiao An Shiming et al. reported 30 cases of type II diabetes treatment with Yu-san-xiao in 1998 (An et al., 1998; Guo, 1998). Among 30 patients treated with Yu-san-xiao, (oral administration, three times a day) for 1 month, ve cases were concluded with no effect. About 40% of patients (12 cases) showed signicant improvement in blood glucose level. Other diabetic symptoms such as thirst and hunger disappeared, and glucose tests in urine became negative. Blood glucose and insulin levels of these 12 patients before and after treatment are summarized in Table 2. In addition to ve patients with no effect and 12 patients with signicant improvement, there were 13 patients who experienced a reasonable improvement after treatment, the clinical results are summarized in Table 3. Yi-jin Yi-jin, upon single or multiple administration, signicantly lowered blood glucose levels in alloxan induced diabetic mice (Li et al., 2000). The efcacy was similar to that of the chemical drug, phenformin (DBI), which was used in the experiments as a positive control. The fact that Yi-jin was not able to alter the blood
POLYSACCHARIDE CONTAINING DRUGS WHICH HELP PROTECT PANCREATIC ISLETS AND BETA CELLS Many Chinese herbs contain polysaccharides, which are found to lower the blood sugar. Therapeutic herbal drugs listed in Table 1 with polysaccharide compositions as the main ingredients are: Yu-san-xiao, Yi-jin and Shen-qi. These drugs contain panaxans, anemarans, dioscorans, astragalus and poria cocos polysaccharides, etc. These polysaccharide containing herbs are found to have the following medical virtues: (1) stimulate immune
Table 1. Drug products and their ingredients approved in China
Drug product Yi-jin Ingredients
Ke-le-nin Yu-san-xiao
Qi-zhi
Shen-qi
Jin-qi
Xiao-ke-an
Panax ginseng (Ginseng) Atractylodes macrocephala (Largehead Atractylodes Rhizome) Poria cocos (Indian Bread) Opuntia dillenii (Cactus) Radix Astragalus (Milkvetch Root) Rehmannia glutinosa (Chinese Foxglove Root) Radix Astragalus (Milkvetch Root) Scrophularia ningpoensis (Figwort Root) Anemarrhena asphodeloides (Common Anemarrhena Rhizome) Rehmannia glutinosa (Chinese Foxglove Root) Radix Astragalus (Milkvetch Root) Rehmannia glutinosa (Chinese Foxglove Root) Hirudo nipponia (Leech) Panax ginseng (Ginseng) Radix Astragalus (Milkvetch Root) Dioscorea opposita (Common Yam Rhizome) Coptis chinensis (Coptis Root) Rehmannia glutinosa (Chinese Foxglove Root) Cornus ofcinalis (Asiatic Cornelian Cherry Fruit) Hirudo nipponia (Leech) Lonicera japonica (Honeysuckle ower) Radix Astragalus (Milkvetch Root) Coptis chinensis (Coptis Root) Radix Astragalus (Milkvetch Root) Pueraria lobata (Lobed Kudzuvine Root) Ophiopogon japonicus (Dwarf Lilyturf Tuber) Hirudo nipponia (Leech)
Phytother. Res. 17, 11271134 (2003)
Copyright 2003 John Wiley & Sons, Ltd.
ANTIDIABETIC HERBAL DRUGS
1129
Table 2. Blood glucose and insulin levels of 12 patients treated with Yu-san-xiao
Blood glucose (mmol/L) Insulin (mU/L) Before meal 8.6 4.8 7.86 4.57 14.0 11.1 After meal (at 2 h) 35.6 13.99 40.17 8.85 41.56 12.59
n = 12
Before treatment At 2-weeks during treatment At 4-weeks during treatment
FBG 9.7 2.28 8.6 3.16 6.58 3.38
PBG (at 2 h) 15.28 3.16 12.13 3.57 9.0 1.24
Table 3. Blood glucose and insulin levels of 13 patients treated with Yu-san-xiao
Blood glucose (mmol/L) Insulin (mU/L) Before meal 15.23 9.4 data not available 17.28 7.22 After meal (at 2 h) 27.5 14.83 data not available 39.32 20.25
n = 13
Before treatment At 2-weeks during treatment At 4-weeks during treatment
FBG 9.7 1.86 7.1 2.0 7.4 1.19
PBG (at 2 h) 15.19 2.55 14.14 1.0 10.6 0.92
Table 4. The effect of Yi-jin on blood glucose level in alloxan induced diabetic mice by single oral administration
Dose (g/kg) 30 Mice no. 15 14 Blood glucose (x s) (mg/dL) Before 358.46 14.98 363.17 77.46 After 2 h 330.19 85.68 245.55 108.16a Change (%) 6.44 33.49
Group Control (water) Yi-jin
a
p < 0.01 compared with control.
Table 5. The effect of Yi-jin on blood glucose level in alloxan induced diabetic mice by multiple oral administration once a day, with phenformin (DBI) as positive control
Blood glucose (x s) (mg/dL) Dose (g/kg) Water 30 20 10 0.075
b
After No. 17 16 16 15 18 Before 365.4 375.8 371.1 370.0 376.4 66.5 70.5 61.0 56.7 79.8 1 wk 396.3 293.8 379.7 392.5 347.2 71.9 103.0b 66.0 106.3 88.0a 2 wk 422.1 280.5 404.7 410.0 308.3 105.6 139.4c 93.5 74.0 128.0b 4 wk 422.1 260.2 340.6 360.0 263.2 100.8 138.8c 76.6a 101.2a 121.1c
Group Control Yi-jin Yi-jin Yi-jin DBI
a
p < 0.05,
p < 0.01,
p < 0.001 compared with the control group.
glucose level in normal mice (Table 7) suggested that this herbal drug could not stimulate the pancreatic islets and beta cells to produce more insulin. The hypoglycaemic effect might be due to its capacity to restore activity of pancreatic beta cells. Additionally, this herbal drug signicantly reduced the concentration of cholesterol, triglyceride and lactic acid in serum, suggesting that this agent is also useful for the complications of diabetes. Li Xiangzhong et al. reported that Yi-jin was evaluated in 328 type II diabetic patients in a multicentre clinical trial in Northeast China, and 85.8% of the patients treated with Yi-jin showed a clinical improvement (Li et al., 2000). The acute toxicity of Yi-jin appeared to be very low, the maximum tolerance level being 384 g/kg, which was about 320 times the recommended human dosage. No
Copyright 2003 John Wiley & Sons, Ltd.
signicant long-term toxicity was observed with oral administration of Yi-jin at 30, 15, 7.5 g/kg in 120 rats for 6 months, no signicant changes were observed in the body weight, blood, liver, kidney and other organs. Part of the pharmacological studies in various animal models is summarized in Tables 48. Shen-qi Yang Yingwu and Wang Chun reported the hypoglycaemic efcacy of Shen-qi in a clinical study conducted at Ruzhou Hospital, in which 150 diabetic patients were included (Yang and Wang, 2000). In the group with 150 patients treated with Shen-qi, blood glucose levels were tested before a meal, and at 2 h after the meal. Glucose levels in urine, cholesterol
Phytother. Res. 17, 11271134 (2003)
1130
W. JIA ET AL.
Table 6. The blood glucose level vs time of alloxan diabetic mice treated with Yi-jin
Blood glucose (x s) mg/dL Dose (g/kg) Water 30
b
After No. 15 15 Before 403.1 72.5 398.1 80.5 1h 411.0 71.9 365.2 49.5a 2h 419.0 71.1 325.09 60.45b 8h 241.8 94.3 184.4 104.3b
Group Control Yi-jin
a
p < 0.05,
p < 0.001 compared with the control group.
Table 7. The effect of Yi-jin on blood glucose level in normal mice by single oral administration
Dose (g/kg) 30 Mice no. 8 10 Blood glucose (x s) mg/dL Before 104.9 21.4 115.7 25.4 After 2 h 83.8 27.6 92.8 14.6 Change (%) 18.5 18.6
Group Control (water) Yi-jin
Table 8. The improvement of lactic acid, cholesterol, triglyceride and beta-lipoprotein levels in alloxan diabetic rats after 1 month treatment with Yi-jin
Dose (g/kg) No. Water 20 10 5 9 9 9 9 Lactic acid Before 47.75 52.20 48.55 44.92 23.88 21.60 24.36 20.37 After 53.62 44.40 44.83 36.14 21.18 20.28 12.91 9.66 Cholesterol (mmol/L) Before 2.25 2.28 2.14 2.22 0.32 0.36 0.30 0.30 After 2.07 1.77 1.76 1.89 0.31 0.29 0.29 0.25 Triglyceride (mmol/L) Before 0.92 0.92 0.85 0.81 0.38 0.40 0.43 0.37 After 0.65 0.39 0.42 0.56 0.26 0.22 0.29 0.24
-lipoprotein (mmol/L)
Before 3.02 2.47 1.94 2.56 1.83 1.14 0.84 1.59 After 1.82 1.83 1.37 1.67 0.63 0.87 0.45 0.67
Group Control Yi-jin Yi-jin Yi-jin
Table 9. Changes of FBG, PBG and glucose in urine, total cholesterol and triglyceride after treatment with Shen-qi
Glucose in urine (g/24 h) 29.40 10.30 15.10 9.80a Total cholesterol (mmol/L) 7.49 1.42 5.84 1.06a
n = 150
Before treatment After treatment
a
FBG (mmol/L) 12.44 3.34 8.98 3.38a
PBG (mmol/L) 15.53 4.06 11.50 4.26a
Triglyceride (mmol/L) 2.96 0.95 1.53 0.86a
p < 0.01 compared with before treatment group.
and triglyceride were also analysed quantitatively. The clinical results are summarized in Table 9. Despite the results indicating a signicant dosedependent blood sugar lowering activity, the hypoglycaemic mechanisms and pharmacology of these herbal extracts remains unknown. It was generally believed, however, by a number of investigators that the polysaccharides in the herbal drugs may protect pancreatic islets and beta cells, help the regeneration of beta cells, and therefore, increase the insulin secretion from pancreas (Wang et al., 2000; Zhang and Li, 2000; Hong, 2001). Typical polysaccharides in medicinal herbs that have been reported to have bloodsugar lowering activities are listed below (Wang et al., 2000). Aconitan A, B, C, and D (from Aconitum carmichi Debeaux.) Abelmosan A, B, and C (from Abelmoschus manihot) Anemarans A, B, C, and D (from Anemarrhena asphodeloides Bunge.)
Copyright 2003 John Wiley & Sons, Ltd.
Astragalus mongholicus polysaccharide G Atractan A, B, and C (from Atractylodes macrocephala Koidz) Auricularia auricula polysaccharide Cordyceps sinensis polysaccharides Dioscoran C and D Eleutheran F and G (from Eleutherococus senticocus) Ephedran C (from Ephedra distachya) Ganoderan A and B (from Ganoderma lucidum) Hericium erinacaus polysaccharide Laminarin Lithosperman A, B, and C (from Lithospermum erythrorhizon) Lycium barbarum polysaccharide D and X Moran A (from Morus alba) Ophipogon japonicus polysaccharide Panaxan AU (from Panax ginseng C. A. Meyer)) Pestalotiopsis Porphyrayezoensis Ueda polysaccharide Poria cocos polysaccharide
Phytother. Res. 17, 11271134 (2003)
ANTIDIABETIC HERBAL DRUGS
1131
Rhodiola sachalinensis polysaccharide Tremella fuciformis polysaccharide Trichosan A, B, C, D and E (from Trichosanthes ririlowii Maxim.)
DRUG COMPOSITIONS THAT IMPROVE THE MICROCIRCULATION Many herbs and natural products have been found to regulate carbohydrate and fat metabolism and to improve the blood circulation and immunity, and therefore, have the effect of lowering the blood glucose level of diabetic patients. The following are typical natural products that can improve the microcirculation (Long, 1998): Achyranthes bidentata, Astragalus membranaceus, Atractylodes macrocephala, Carthamus tinctosius, Codonopsis pilosula, Dioscorea opposita, Hirudo nipponia, Ligusticum, Opuntia dillenii, Panax ginseng, Rehmannia glutinosa and Salvia miltiorrhiza. These agents have been studied most extensively by modern medical science, which not only validated most of the traditional therapeutic claims but also discovered many important pharmacological effects (Xiao, 2002). For instance, Astragalus and Dioscorea have been under intensive medical research in China and in many countries of the world as tonic restoratives for immune deciency. Astragalus is present in most of the products listed in Table 1. Astragalus root is found to strengthen nonspecic immunity, signicantly enhance the function of T-lymphocytes, and to promote humoral immunity. It can dilate peripheral, coronary, cerebral and intestinal vessels, and improve microcirculation. These herbs help to restore impaired immune functions, stimulate secretions of vital immune factors, and to enhance overall immune response throughout the system. Several drug products listed in Table 1, the compositions of which contain the above extracts, were developed and approved for both type I and II diabetes. These drugs are Ke-le-nin, Qi-zhi and Xiao-ke-an. Both Ke-le-nin and Xiao-ke-an contain an extract from
Hirudo nipponia (leech), a non-herbal ingredient. The main ingredient of leech extract is hirudin, which can readily inhibit the action of thrombin on brinogen, and hence has an anticoagulant effect. Both Ke-le-nin and Qi-zhi contain an extract from Rehmannia glutinosa, which is the root of the perennial herb, produced mainly in Hunan, Hebei, Inner Mongolia and Northeast China. Dried Rehmannia root has been widely used for deciency of body uid, thirst, diabetes and constipation. Its decoction is believed to possess the effects of protecting the liver and preventing the decrease of hepatic glycogen. The pharmacological studies of these three drugs are discussed as follows. Ke-le-nin Liu Yunling et al. reported that the clinical evaluation of Ke-le-nin with 30 type II diabetic patients showed a signicant hypoglycaemic effect (Liu and Li, 1996). Oral administration of Ke-le-nin, four capsules, three times a day, for 90 days lowered the blood glucose level (FBS) from 10.35 mmol/L to 7.54 mmol/L. Other analyses are summarized in Table 10. Qi-zhi Xing Haiyan of Henan TCM College conducted pharmacological studies on several herbal drugs in alloxan induced diabetic rats (Xing, 2000). Qi-zhi was found to lower the blood glucose levels in diabetic animals in a 30 day trial. The chemical drug, phenformin (DBI), was used as a positive control. The experimental results are partially included in Table 11. Xiao-ke-an Xiao-ke-an contains extracts from two types of medicinal herbs, Astragalus mongholicus and Ophiopogon japonicus Ker-Gawl, which mainly contain
Table 10. Comparison of various parameters before and after treatment with Ke-le-nin
Before treatment FBG (mmol/L) PBG (mmol/L) at 2 h HBA1 (%) Insulin (mU/L) C peptide (nmol/L) Triglyceride (mmol/L) Cholesterol (mmol/L) 10.85 14.88 9.96 14.51 0.78 1.22 4.98 3.11 3.28 0.74 6.47 0.22 0.81 1.27 After treatment 17.54 10.36 7.32 13.98 0.77 1.20 4.87 4.01 3.94 0.87 6.49 0.24 0.92 1.32
p value
<0.05 <0.01 <0.01 >0.05 >0.05 >0.05 >0.05
Table 11. Hypoglycaemic effect of Qi-zhi on alloxan induced rats
FBG mmol/L at time 0 7.58 20.62 21.14 20.92 1.07 6.54 4.47 6.23 FBG mmol/L at 10 days 7.14 21.80 9.70 12.45 1.10 6.19 7.07 7.52 FBG mmol/L at 20 days 7.21 23.87 24.17 15.96 1.19 10.00 10.75 6.49 FBG mmol/L at 30 days 7.02 19.17 16.72 12.84 1.11 9.41 13.33 4.14
Group Normal Diabetic DBI Qi-zhi
n
10 10 10 10
Copyright 2003 John Wiley & Sons, Ltd.
Phytother. Res. 17, 11271134 (2003)
1132
W. JIA ET AL.
Table 12. Blood glucose lowering effect on normal mice treated with Xiao-ke-an
Group Blank Glyburide Xiao-ke-an high dose Xiao-ke-an low dose
a
Dosage (g/kg) 0.05 10 5
No. mice/group 12 12 12 12
Blood glucose (mmol/L) 8.21 6.47 4.69 6.00 0.70 1.38a 1.47a 1.59a
p < 0.01 compared with control blank.
Table 13. Blood glucose lowering effect on streptozocin induced diabetic model mice
Group Blank Diabetic model Phenformin Xiao-ke-an high dose Xiao-ke-an low dose
a
Dosage (g/kg) 0.05 10 5
No. mice/group 10 10 10 10 10
Blood sugar (mmol/L) 8.18 29.88 15.31 19.56 21.09 1.90 7.09 5.90a 4.34a 6.53a
p < 0.01, compared with diabetic model.
polysaccharides, and Pueraria lobata and Hirudo nipponia, which contain ingredients that can improve the microcirculation (Ji, 2001). Pueraria lobata include puerain, the pharmacology of which has been extensively studied. Puerain can readily promote the blood circulation, and has been used to treat heart problems including myocardial ischaemia and infarction. Puerain also showed a signicant hypoglycaemic effect in alloxan induced diabetic mice. Yang Xiaofeng et al. investigated the pharmacological effect of Xiao-ke-an in animal models and reported that this agent was able to lower the blood glucose level in normal mice as well as streptozocin induced diabetic mice (Yang et al., 1999). The study with normal animals was conducted using four groups, a total of 48 mice, for a 14 day test. The agent, Xiao-ke-an, was orally administered, and a chemical drug, glyburide, was used as control. Blood samples were collected on the last day and analysed for blood sugar values. A 14 day study with a drug induced diabetic animal model was also conducted using 50 mice (2224 g), and a chemical drug, phenformin, as control. Experimental data are given in Tables 12 and 13.
DRUG PRODUCTS THAT CAN REDUCE INSULIN RESISTANCE Many type II diabetic patients have normal levels of insulin in the blood. The diabetes is not caused by the destruction of beta cells in the pancreas but by other mechanisms, such as insulin resistance, related to downregulation of insulin receptors, defects in insulin secretion from the pancreatic beta cells and other changes to the glucose transporter system. Jin-qi was reported to have the pharmacological effect of restoring sensitivity to insulin and therefore, reducing insulin resistance (Cui, 2000). Jin-qis composition comprises extracts from honeysuckle ower, milkvetch root and coptis root. Honeysuckle ower is a vinelike shrub that grows to a height of 69 m, with slender, prickly branches and
Copyright 2003 John Wiley & Sons, Ltd.
owers that bloom white then turn yellow, hence the Chinese name meaning gold and silver ower. The ower, stem and leaves contain inositol, saponin and tannin. Honeysuckle ower is routinely used for detoxication and thirst. Coptis root is a perennial herb with long trifoliated leaves, small yellowish white owers and a reddish brown root covered with ne rootlets. This plant is cultivated throughout China and also in parts of northern India. The root is yellowish orange on the inside, the inner pith being deeper in colour, and contains berberine, alkaloids coptisine, palmatine, jatrorrhizine and magnoorine, etc. Among these ingredients, berberine is the most popular and wellcharacterized compound with demonstrated antidiabetic effects (Xiao, 2002). Pharmacological studies with Jin-qi were performed using genetically diabetic KK mice (female, 2022 g) and hydrocortisone (HC) induced diabetic mice (Shen et al., 1997). Both groups were insulin-resistant and during the experiment, were given Jin-qi daily, and were injected with insulin at 23 and 9 days, respectively. Table 14 and Figs 1 and 2 summarize the experimental results, showing that Jin-qi was able to reduce the insulin resistance in the two animal models. The blood glucose levels in the Jin-qi group were higher than those in the normal control groups, upon i.p. injection of insulin, but signicantly lower than those in diabetic groups which were insulin-resistant. The serum insulin concentration in Jin-qi treated KK mice was 12.1 5.5 mU/L, compared with 21.4 14.9 mU/L in the KK mice control. A single-blinded, randomized, multicentre clinical investigation of Jin-qi was conducted in 1993 at four major hospitals in Beijing, in which a total of 442 patients with type II diabetes participated. The clinical dosage was 710 pills (0.42 g/pill) of Jin-qi, per dose, and three doses per day (Cui, 2000). A different antidiabetic herbal drug was used, at eight pills per dose, and three doses per day, as a control. Combined drug treatment using Jin-qi and chemical hypoglycaemic agents was also used to evaluate the synergistic effect of chemical herbal therapeutic drugs. The clinical results are shown in Table 15.
Phytother. Res. 17, 11271134 (2003)
ANTIDIABETIC HERBAL DRUGS
1133
Table 14. Experimental method using genetically diabetic KK mice or hydrocortisone induced diabetic mice
Group Control (normal) Model mice Jin-qi group Mice SWR/J KK or HC KK or HC No. 10 10 10 Duration 22 d or 9 d 22 d or 9 d 22 d or 9 d Insulin injection (i.p.) at 0.5 U/kg Measure glucose level at 0, 30, 120 min As above As above
Table 15. Clinical blood glucose lowering effect with Jin-qi
Patient no. 120 35 216 71 Before meal After meal Before meal After meal Before meal After meal Before meal After meal Avg. blood glucose (mg/dL) Before 195.5 292.2 184.9 268.6 206.0 291.7 198.7 275.1 After 147.4 219.1 173.9 233.2 168.6 251.4 172.6 258.4 Change (%) 24.5 25.0 6.0 13.2 18.2 13.8 13.1 9.8
Group Jin-qi Controla Combined (Jin-qi + chemical drugsb) Control
a b
A herbal antidiabetic drug (the name of which was not given in the report) was used in two control groups. Names of chemical drugs used in this group were not available in the report.
Figure 1. The effect of Jin-qi on the insulin-tolerance level of KK mice. , normal control group; , KK model mice; , KK mice treated with Jin-qi.
Figure 2. The effect of Jin-qi on the insulin-tolerance level of HC diabetic mice. , normal control group; , HC model mice; , HC model mice treated with Jin-qi.
DISCUSSION There are several review articles (Liu and Lu, 2000; Li, 2000; Jiang and Li, 2001) published in various Chinese journals discussing traditional antidiabetic agents and
Copyright 2003 John Wiley & Sons, Ltd.
pharmacological studies in China. Due to the different pharmacological roles of those hydro-alcohol extracts, the hypoglycaemic mechanism of drug products containing a mixture of those extracts becomes complicated. The authors speculated that polysaccharide-containing agents restored the functions of pancreatic tissues and caused an increase in insulin output by the functional beta cells. Others attributed the hypoglycaemic effect of many products to their ability to inhibit the intestinal absorption of glucose, to the increased availability of insulin, or to the facilitation of metabolites in insulindependent processes. However, none of the investigators was able to provide conclusive evidence to ascertain the actual hypoglycaemic mechanism(s) of a single herbal drug developed in China. This paper reviews the compositions, pharmacological and clinical effects of seven antidiabetic herbal drugs commercially available in China. Combination formulas, i.e. mixtures of certain herbal extracts, were used in all the drug products, and each product possessed signicant dose-dependent blood glucose lowering activity in various animal models as well as in humans. These alterations will further lead to a decrease in atherosclerosis. The difference between a single-herb formula and a multi-herb combination formula is not merely the addition of more herbs, but also the interaction between the components of mixtures of herbs. A system of synergistic interactions among herbal drugs is formed in a combination formula which is believed to take a multi-targeted therapeutic approach in the treatment. The treatment of diabetic patients with naturally derived agents has the advantage that it does not cause the signicant side effects as do chemical agents such as sulfonylurea. One of the side effects with sulfonylurea is that it causes a decreased amount of insulin production by putting too great a strain on the insulin producing beta cells. Treatment with herbal drugs has an effect of protecting beta cells and smoothing out uctuations
Phytother. Res. 17, 11271134 (2003)
1134
W. JIA ET AL.
in glucose levels. Some agents, such as Jin-qi, can reduce the insulin resistance and, hence, improve the apparent insulin activity. Improved insulin activity leads to decreased circulating insulin, which leads to lower blood glucose and glycosylated haemoglobin levels as well as total cholesterol, LDL-cholesterol and triglyceride levels, and increased HDL-cholesterol levels. Additionally, the use of these natural agents in conjunction with conventional drug treatments such as a chemical agent or insulin permits the use of lower doses of the drug
and/or decreased frequency of administration which decreases the side effects most commonly observed. It was also widely observed during the clinical studies in China that the mixtures of herbal extracts could lower the cholesterol and triglyceride levels, in addition to the blood glucose level. This suggests that the longterm use of herbal drugs may be advantageous over chemical drugs in alleviating some chronic diseases and complications caused by diabetes, while adverse effects of these herbal extracts are minimal.
REFERENCES
An SM, Chen W, Feng XL et al. 1998. The treatment of 30 type II diabetic patients with Yu-san-xiao. J Pract Trad Chin Med 14: 4445. Cui WQ. 2000. Clinical observation on the treatment of type II diabetes with Jinqi. Chin Trad Herbal Drugs 31: 1819. Geng HY, Wang SH. 1997. Practical Therapeutic Drugs. Peoples Health Press: Beijing. Guan ZA, Sun MX, Guan DS et al. 2000. Modern Diabetes Mellitus. Tianjin Science and Technology Press: Tianjin. Guo YY. 1998. Clinical studies on the treatment of diabetes with Yu-san-xiao. Commun Med Res 27: 1214. Hong H. 2001. Progress of experimental studies on hypoglycemic mechanisms by TCM. J Anhui TCM College 20: 5963. Ji YB. 2001. Pharmacological Application of Anti-senescence Composition of Traditional Chinese Medicine. Heilongjiang Science and Technology Press: Haerbin. Jiang LJ, Li L. 2001. Research progress of the therapeutic mechanisms of diabetic complications with active ingredients from TCM. J Anhui TCM College 20: 6365. Li QM. 2000. The mechanisms of TCM for the treatment of diabetes. Chin J Exp Formulas 6: 5658. Li XZ, Gui LH, Liu YL et al. 2000. Blood glucose and blood lipids lowering effects of the liquid formulation of Yijin. J Shenyang Pharmaceu Univ 17: 371373. Liu TH, Lu RH. 2000. The mechanisms of TCM for the prevention of diabetes and its complications. J Beijing Univ TCM 23: 6971. Liu YL, Li CS. 1996. The treatment of 30 qi-yin-decient diabetic patients with Ke-le-nin. J Shandong TCM 15: 302303. Long ZX. 1998. The Chinese Materia Medica. Academy Press: Beijing. Reid D. 1999. Chinese Healing Herbs. Barnes & Noble Books: New York. Shang MF. 2000. Status of the development of antidiabetic TCM in China. Chin J TCM Inform 7: 7881. Shen ZF, Xie MZ, Liu HF. 1997. The inuence of Jinqi on blood lipid level, insulin resistance, and immunity in experimental animals. Trad Chin Drug Res Clin Pharm 8: 2326. Wang L, Li SL, Wang T. 2000. Progress on the study of polysaccharides and glucosides of hypoglycemic plants. Chin Med Mater 23: 575577. Xiao PG. 2002. The New Edition of the Annals of Traditional Chinese Medicine. Chemical Industry Press: Beijing. Xing HY. 2000. Studies on the treatment type II diabetes and its chronic complications with Tang-yu-ping. Henan Trad Chin Med 20: 2931. Yang XF, Li SG, Yu DZ et al. 1999. The study of Xiao-ke-an on blood sugar and blood lipid lowering effects. Trad Chin Drug Res Clin Pharm 10: 288290. Yang YW, Wang C. 2000. Clinical study on Shenqi for the treatment of type II diabetes. Henan Trad Chin Med 20: 3335. Zhang HF, Li SM. 2000. Research progress of natural hypoglycemic agents. Chin Trad Herbal Drugs 31: 184186.
Copyright 2003 John Wiley & Sons, Ltd.
Phytother. Res. 17, 11271134 (2003)
Anda mungkin juga menyukai
- Japan Food Additives Standards For Use 15 Jan 2020Dokumen25 halamanJapan Food Additives Standards For Use 15 Jan 2020JY MarBelum ada peringkat
- 21 CFR 101.22Dokumen7 halaman21 CFR 101.22JY MarBelum ada peringkat
- SG Food Import Requirements 1 Oct 2019Dokumen16 halamanSG Food Import Requirements 1 Oct 2019JY MarBelum ada peringkat
- Consumer Decision Making Process in Shopping For Halal Food in MalaysiaDokumen10 halamanConsumer Decision Making Process in Shopping For Halal Food in MalaysiaJY MarBelum ada peringkat
- Andrographis Paniculata WHO Monographs On Selected Medicinal Plants Volume 2Dokumen13 halamanAndrographis Paniculata WHO Monographs On Selected Medicinal Plants Volume 2JY MarBelum ada peringkat
- Regulating Halal and Kosher Foods Different Arrangements Between State Industry and Religious Actors PDFDokumen15 halamanRegulating Halal and Kosher Foods Different Arrangements Between State Industry and Religious Actors PDFJY MarBelum ada peringkat
- P 65 Single 10212016Dokumen22 halamanP 65 Single 10212016JY MarBelum ada peringkat
- Codex NRV - Nutrient Reference Values (20191204) PDFDokumen96 halamanCodex NRV - Nutrient Reference Values (20191204) PDFsusantika murtiniBelum ada peringkat
- Food AdditivesDokumen223 halamanFood AdditivesJY MarBelum ada peringkat
- 21CFR172 515Dokumen18 halaman21CFR172 515JY MarBelum ada peringkat
- ESCOP Monographs Order Form Euro 2011Dokumen1 halamanESCOP Monographs Order Form Euro 2011JY MarBelum ada peringkat
- Sweet ProteinDokumen8 halamanSweet Proteinsudha2987Belum ada peringkat
- Regulation on Flavourings and Food IngredientsDokumen196 halamanRegulation on Flavourings and Food IngredientsJY MarBelum ada peringkat
- CFR Code of Federal Regulations Title 21: The Information On This Page Is Current As of April 1 2015Dokumen14 halamanCFR Code of Federal Regulations Title 21: The Information On This Page Is Current As of April 1 2015JY MarBelum ada peringkat
- Guidance For Industry Botanical Drug ProductsDokumen52 halamanGuidance For Industry Botanical Drug ProductsJY MarBelum ada peringkat
- Triphala Dose 2Dokumen11 halamanTriphala Dose 2JY MarBelum ada peringkat
- Practical Organic ChemistryDokumen598 halamanPractical Organic ChemistryGerardo Estrada99% (127)
- Japanese Pharmacopoeia notification revisionDokumen301 halamanJapanese Pharmacopoeia notification revisionJY MarBelum ada peringkat
- Dietary Supplements 3rd Edition LecithinDokumen4 halamanDietary Supplements 3rd Edition LecithinJY MarBelum ada peringkat
- Designing The Selenium and Vitamin E Cancer Prevention Trial (SELECT)Dokumen9 halamanDesigning The Selenium and Vitamin E Cancer Prevention Trial (SELECT)JY MarBelum ada peringkat
- Aromatic Damp-Dissolving Herbs PDFDokumen20 halamanAromatic Damp-Dissolving Herbs PDFJY MarBelum ada peringkat
- Comparison of Risk Factors of Diabetes Mellitus Type 2 Between Vegetarians and Non-Vegetarians in Kulim, KedahDokumen92 halamanComparison of Risk Factors of Diabetes Mellitus Type 2 Between Vegetarians and Non-Vegetarians in Kulim, KedahJY MarBelum ada peringkat
- Olive OilDokumen13 halamanOlive OilJY Mar100% (1)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Name: - Class: - Read The Passage Carefully. Then, Answer The Following Questions. The CoconutDokumen2 halamanName: - Class: - Read The Passage Carefully. Then, Answer The Following Questions. The CoconutIrdawati Shuib63% (8)
- Effect of Sweet Potato Flour On Quality of CookiesDokumen14 halamanEffect of Sweet Potato Flour On Quality of CookiesRahma NusandariBelum ada peringkat
- Sam BongDokumen4 halamanSam BongAngelique GABelum ada peringkat
- Ficus Carica PDFDokumen2 halamanFicus Carica PDFPierreBelum ada peringkat
- 5.3 Classification of BiodiversityDokumen34 halaman5.3 Classification of BiodiversityKritika ChugBelum ada peringkat
- Kelimpahan Populasi Dan Tingkat Serangan Kutu Daun (Mysuz Persicae Sulzer) (Homoptera: Aphididae) Pada Tanaman Cabai Merah (Capsicum Annuum L.)Dokumen8 halamanKelimpahan Populasi Dan Tingkat Serangan Kutu Daun (Mysuz Persicae Sulzer) (Homoptera: Aphididae) Pada Tanaman Cabai Merah (Capsicum Annuum L.)Niko ChanBelum ada peringkat
- Cereals and StarchDokumen25 halamanCereals and StarchRonnell Arlan Arranguez EñegoBelum ada peringkat
- Aizoaceae InfoDokumen59 halamanAizoaceae InfoMaria Agneta100% (2)
- English Name of Common Indian Spices IngredientsDokumen9 halamanEnglish Name of Common Indian Spices IngredientsPawan AgarwalBelum ada peringkat
- Changes in climate and their effectsDokumen7 halamanChanges in climate and their effectsSamuel WagalukaBelum ada peringkat
- Status of Biological Control in MealybugDokumen19 halamanStatus of Biological Control in MealybugDinesh KumarBelum ada peringkat
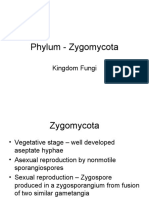
- Phylum - Zygomycota: Kingdom FungiDokumen44 halamanPhylum - Zygomycota: Kingdom FungiabdulqadirBelum ada peringkat
- Lightning Strikes and Tree Damage ExplainedDokumen3 halamanLightning Strikes and Tree Damage ExplainedAmmar MarBelum ada peringkat
- Diagnostic Test Natural Science 4Aº Primaria Byme PDFDokumen2 halamanDiagnostic Test Natural Science 4Aº Primaria Byme PDFpabloBelum ada peringkat
- Usabo2012 Open ExamDokumen11 halamanUsabo2012 Open ExamsiderabioBelum ada peringkat
- Whole GrainsDokumen16 halamanWhole GrainsiumilitanteBelum ada peringkat
- Class-IX Phase-1 Revision QuestionsDokumen2 halamanClass-IX Phase-1 Revision QuestionsDivyansh Jain KingBelum ada peringkat
- Growing Radish with VermicompostDokumen59 halamanGrowing Radish with VermicompostNikki Charm Aguilar DeronioBelum ada peringkat
- Spelling BeeDokumen20 halamanSpelling BeeDanna LupenaBelum ada peringkat
- ARCO SAT Subject Biology EM Practice TestDokumen31 halamanARCO SAT Subject Biology EM Practice TestMansoor AhmedBelum ada peringkat
- The Pruning Book 1000826660Dokumen114 halamanThe Pruning Book 1000826660adiseifBelum ada peringkat
- Wo gtr79 83 091Dokumen12 halamanWo gtr79 83 091Lavinia PîndaruBelum ada peringkat
- Establishment of Center of Excellence On Dry-Land Agriculture With Focus On Pulses and Oilseed CropsDokumen21 halamanEstablishment of Center of Excellence On Dry-Land Agriculture With Focus On Pulses and Oilseed CropsAkhilesh SrivastavaBelum ada peringkat
- Alternate Bearing in Olive - A ReviewDokumen18 halamanAlternate Bearing in Olive - A ReviewAli Abdelmoniem AhmedBelum ada peringkat
- Herbs For MERP Listed by ClimateDokumen11 halamanHerbs For MERP Listed by ClimateAlcarinalataBelum ada peringkat
- Harvest Public School, Khammam: Class:-VI (SEP) Mid Exam - 1 Time: - 3hr Sub:-Biology Marks: - 40Dokumen4 halamanHarvest Public School, Khammam: Class:-VI (SEP) Mid Exam - 1 Time: - 3hr Sub:-Biology Marks: - 40Prem RajBelum ada peringkat
- NematologyDokumen46 halamanNematologyJayson BasiagBelum ada peringkat
- Mango Malformation TreatmentDokumen2 halamanMango Malformation TreatmentShabbir HussainBelum ada peringkat
- COCA AND COCAINE COCA AND COCAINE Effects On People and Policy in Latin America (CULTURAL SURVIVAL REPORT 23)Dokumen172 halamanCOCA AND COCAINE COCA AND COCAINE Effects On People and Policy in Latin America (CULTURAL SURVIVAL REPORT 23)jeronimo m.m.Belum ada peringkat
- Genetics MidtermDokumen5 halamanGenetics Midterm정위영Belum ada peringkat