Nursing Procedures 2003
Diunggah oleh
jackson2494Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nursing Procedures 2003
Diunggah oleh
jackson2494Hak Cipta:
Format Tersedia
Nursing Procedures 2003 Promotion of Ventilation: Tracheal Suctioning To remove secretions from the nose, mouth, and from
m the tracheobronchial tree. To stimulate coughing and mobilize secretions upward. Points to remember: Implement strict sterile technique. Lubricate catheter with water-soluble lubricant before inserting it to the airway. Do not apply suction when inserting the catheter. Do not suction for more than 15 seconds. Apply suction when withdrawing the catheter in a rotating motion. Oxygenate before and after suctioning the patient. Oro-nasotracheal suctioning: The length of the catheter measures from the tip of the noseearlobe. Suction a conscious patient in fowlers position. Suction a comatose patient in side-lying position. Coughing and deep breathing Exercises: To remove secretions and keep airway patent. To decrease respiratory rate. To relax breathing and lower anxiety level. Points to remember: For post-operative patientssplint chest wall with pillow or palms of hands to minimize discomfort. Administer analgesic prior (chest & abdominal incision) to coughing & deep breathing exercises. Percusion & Vibration To dislodge secretions from the affected lungs. Must be performed few hours after meals to prevent vomiting or aspiration. Postural drainage To drain secretions through gravity. To clear airway. The bronchi being drain should be higher and perpendicular to the floor. May loosen up secretion through bronchodilator or nebulizer before doing the procedure. Best time to performbefore breakfast, before lunch, before bedtime, upon waking up.
Pursed Lip Breathing To slow down respiratory rate. To promote elimination of carbon dioxide. To combat exertional dyspnea. Inhale through the nose and exhale slowly and evenly against pursed lip while tightening the abdominal muscles. Incentive Spirometry To prevent atelectasis. To open up closed alveoli. Copyright by Carmen M. Dimaapi Procedure 2003 Promotion of Circulation Passive-Active Exercise To maintain/promote circulation. Passive exerciseperformed by someone for the patient. Active exercisesthe patient performs the exercise. Isotonic Exercise Similar to aerobic exercise. Promotes circulation; muscle development. Promotion of Tissue Integrity Wound irrigation To wash and remove bacteria. To loosen up debris. To apply heat and enhance healing process. To apply medication such as antimicrobial. Common solutions used: Sterile NS, Daikins solution, Hydrogen peroxide, Antibiotic solution. Equipment needed: sterile gloves, 50 cc syringe, special catheter for dead wound, sterile dressing. Instill the solution gently to the wound; forcing the solution may cause tissue damage. Continue irrigating the wound until the return is clear or free of exudates. Dry up the wound with sterile dressing after the irrigation. 244 Nursing
Moisture in the skin may cause skin irritation and bacterial growth.
DRAINS a. T-tube is usually indicated to post-cholecystectomy to drain bile and prevent bile from spilling into the peritoneal cavity. b. Jackson Pratt to drain excess fluid or blood from the operative site; suction is created by negative pressure in the collection apparatus. c. Hemovac- to drain excess fluids or secretions from the operative sites; commonly used in hip replacement, mastectomy; suction in the collection apparatus is created by negative pressure. Empty when it is half full. d. Penrose drain-prevents purulent materials or serosnaguinous fluids from accumulation in the operative site; facilitates healing from the underlying tissue. Staging Pressure Ulcer Stage 1 = the skin is red, blue or purple hue; warmth/cool to touch, firm boggy. Stage II = partial thickness skin loss including epidermis, dermis, or both. The ulcer is superficial like in abrasion, blister, or shallow crater. Copyright by Carmen M. Dimaapi Procedure 2003 Stage III = full-thickness skin loss involving damage to or necrosis of subcutaneous tissue and up to the underlying fascia i.e. deep crater. Stage IV = full-thickness skin loss with extensive destruction, tissue necrosis, or damage to the muscle, bone, or supporting structures. Preventing Pressures Ulcers: Clean skin at a time of soiling. Use warm not hot water. Use mild antiseptics. Moisturize dry skin. Do not massage bony prominences. Turn and reposition the patient every 2 hours. 245 Nursing
Do not use doughnut-type devices to relieve pressurecause venous congestion. Use pillow or pads to separate skin surfaces and support limbs. Position the patient at a 30 angle on his side, not directly on the trochanter. Ensure adequate intake of protein and calories and fluids.
Promotion of Nutrition Nasogastric Tube Can be inserted by RN. Tube is inserted through the nose with head upright then flex head as the tube is passed through the pharynx then esophagus. If the tube touches the pharynx during insertion, the patient may gag or vomit. Length of tube is measured from tip of the noseearlobexyphoid process. Checking for placement of tubeinject 10 cc of air to the stomach then listen simultaneouslywhoosing sound indicates that the tube is in place. Feeding: place patient in sitting position to prevent aspiration.; place patient slightly towards the right side to facilitate digestion flush tube after each feeding to prevent blockage. Check for residual feeding at least 30 minutes or one hour after feeding to check for feeding tolerance100 ml of residual feeding may indicate poor tolerance to feeding. Removing the NG tube Use non-sterile gloves. Instill 50 ml of water to clear up the tube from gastric contents. Ask the patient to take deep breath and hold to close the glottis and prevent aspiration. Pinch tube with gloved hand to prevent gastric content to drain into the patients throat then quickly pull out the tube. Gastrostomy Feeding Before feeding, check tube by instilling at least 15 ml of water. During feeding, place patient in sitting position to prevent aspiration and to promote digestion. Common complications include abdominal distention, diarrhea, fecal impaction, aspiration.
Copyright by Carmen M. Dimaapi
246 Nursing Procedure 2003
Total Parenteral Nutrition (TPN) Uses Hypertonic solution10% to 15% Dextrose. Superior vena cava is commonly used. Dressings and tubing changes should be done with strict sterile technique. Special tubing with filter is used. Do not piggyback any medications except for the lipids. TPN should be at room temperature when being administered to the patient. Common complications of TPN: hyperglycemia, dehydration, sepsis. Promotion of Elimination Levin tube/Salem sump tube To remove fluid or gas from the GI tract. To relieve nausea and vomiting. To obtain specimen (gastric contents) for laboratory testing. Special consideration: a. Never place the end of the tube in a container of water when checking for placementthis may result to aspiration if the tube is in the trachea. b. Irrigate the tube with 30 ml of fluids or inject 10 to 20 ml of air through the blue port of a salem sump tube to keep the tube patent. c. Provide oral hygiene at least once a shift to promote patients comfort. d. Apply cream to nares and lips to prevent crusting of secretions and to maintain tissue soft. e. Levin tube is usually connected to low gomco suction. f. Salem sump tube is usually connected to high suction. g. Clear or yellow-green drainage is normal; dark-brown is usually abnormal. Foley Catheter Types: straight catheter; retention catheter; three-way foley catheter. Sizes: French #16, #18 (adult) with 5-ml balloon or 30-ml balloon. Straight catheter does not have any balloon.--> primarily for intermittent catheterization or checking residual urine. Female: Insertion of catheter: Prepare equipment; explain procedure to the patient. Create a sterile field. Put on sterile gloves. Drape the patient with sterile drape.
Lubricate the insertion tip of the catheter. Cleanse the urethral meatus clean from the anterior to the posterior aspect to prevent contamination. Insert catheter 5 to 7 cm (2 to 3 inches) into the urethral meatus using strict sterile technique. If resistance is met during insertion, do not force catheter into the urethra (it may cause trauma); ask the patient to take deep breath to relax external sphincter. Allow small amount of urine to flow to ensure placement of catheter; inflate balloon. Connect catheter to the drainage bad. Tape catheter and drainage tubing to the patients thigh. 247
Copyright by Carmen M. Dimaapi
Nursing Procedure 2003 Male: Insertion of catheter Gather all equipment and explain procedure to the patient. Create a sterile field. Put on sterile gloves. Lubricate the insertion tip of the catheter. Cleanse the penis and around the urinary meatus. Lift the penis to a perpendicular position to straighten the downward curvature of the urethra, and apply slight traction while inserting the catheter. Advance the catheter 15 to 25 cm (6 to 10 inches) until urine flows. If resistance is felt at the external sphincter, apply a gentle pressure on the catheter and ask the patient to bear down to help relax the sphincter. Slight resistance is normally encounter at the sphincter, to bypass the slight resistance, twist the catheter and ask the patient to bear down; forceful pressure is not recommended for it may traumatize the urethra. Inflate balloon; connect to the drainage bag. Tape the catheter to the lower abdomen and the tubing to the shaved thigh. Enemas Tap water Enema Use 500 ml to 1000 ml of fluids. Fluids distend the bowel and promote peristalsis. Do not give tap water enema to children & infantsit may result to fluid & electrolyte imbalance. Infant (150 ml to 250 ml); Toddler (250 ml to 350 ml); child (300 ml to 500 ml).
How to give enema: a. Place patient on left side lying position with right leg flexed. b. Insert 7 cm (3 inches) of well-lubricated tube into the patients rectum. c. If resistance is met during catheter insertion, ask the patient to take deep breaths. d. Administer the enema slowly (cold fluid may precipitate cramps). e. Stop the enema (momentarily) if the patient complains of pain or cramps.
Colostomy/Ileostomy Ostomy appliance can be changed Q 3 to 5 days. Best time to change is before breakfast or 2 hours post meal or before bedtime when peristalsis is least active. Burning sensation beneath the plate may indicate skin irritation. Wash periostomal skin with warm water and soap; dry skin thoroughly. Apply skin barrier (karaya) and the ostomy bag. Irrigate the colostomy to regulate bowel movement: a. Best time is after meal. b. Place patient in semi-fowlers position if irrigation is done in bed. c. Most patients prefer to have it done in the toilet. d. Tubing should be lubricated, insert 2 inches to 3 inches into bowel. e. Maintain the height of the irrigating solution at 18 inches or shoulder height when patient is seated.
Copyright by Carmen M. Dimaapi Procedure 2003 Administration of drugs Subcutaneous injection Use 45 to 90 angles. Volume should not be more than 1.5 ml.
248 Nursing
Intramuscular injection Use 90 angle. Volume not more than 2 ml into small muscle. Volume no more than 5 ml into large muscle. For children 0.1 ml to 1.0 ml to the vastus lateralis. Z-tract method Used to prevent tissue irritation or leakage of the medication. Change needle after medication has been drawn up.
Displace the skin and subcutaneous tissue about 2 cm and maintain traction while medication is injected. Insert needle at 90. Hold alcohol swab firmly on the injection site. Do not massage the site it may cause seepage of medication causing tissue damage.
Intradermal Injection Used 15 angle. The medication should from a bleb or a wheal under the dermis. Inject 0.1 to 0.5 ml into the dermal layer. Instilling medication into the ear Clean the external ear with cotton tip applicator. Straighten the auditory canal: Adultgently pull the pinna upward and back. Childrengently pull the pinna down and back. Instill the medication at room temperature for the ear is very sensitive to cold. Place patient in side-lying position with affected ear facing up. Following administration of medication, plug the external ear with cotton ball for about 15 minutes to 25 minutes. Keep the patient to the side for at least 5 minutes to prevent leakage of medication. Administering medication into the vagina Place patient in a supine position with knees flexed, feet apart. For vaginal suppository-insert lubricated suppository approximately 8 cm to 10 cm to the vaginal canal. For vaginal cream insert applicator approximately 5 cm (2 inches); patient remains in supine position for 10 minutes following treatment.
Copyright by Carmen M. Dimaapi
249
Nursing Procedure 2003 Rectal Suppositories Place patient in side lying position.
Ask patient to take deep breath to facilitate relaxation. Gently insert the suppository using index finger to direct the suppository. Insert suppository 3 inches to 4 inches (adult), and 2 inches for children. Keep the patient in side lying position for 30 minutes to facilitate absorption of medication.
Promotion of Ambulation Cane Measurementflex elbow at 30 angle and hold the cane 15 cm (6 inches) on the side of the 5th toethe cane should e at the level of the greater trochanter. Technique in walking: a. Hold the cane in the hand of the good side. b. Advance the cane and the affected leg forward at the same time. c. Keep the cane closer to the body to prevent leaning. d. If the cane cannot be held by the opposite hand, it may be carried by the hand of the affected leg, and move simultaneously forward with the bad leg. Walker Fitting with walker: elbows slightly bent and hand grip at wrist level or when arm is hanging by the side. Non-weight bearingno weight on the injured leg. Affected leg should be off the floor. Partial weight bearingable to put half of the weight through the affected leg. Featherweight bearingable to put affected leg to floor, just for balance. Weight bearing as toleratedmay take all weight through affected leg. Move the affected leg forward, then push down on the walker using the arms. Move good leg forward, even with or slightly ahead of the affected leg. Put the walker no more than one step length in front of the patient. Types of Exercise Aerobic bodys oxygen consumption if done for 5 minutes or more. endurance, improves strength and flexibility. i.e. walking, running, bicycling, swimming. Isotonic strength and flexibility; prevent stiffness & weakness. i.e. weight lifting, calesthenics, active ROM. Active Range of Motion Under the category of isotonic. Maintains flexibility & strength.
Passive ROM Does not prevent muscle atrophy. Maintains joint flexibility.
Copyright by Carmen M. Dimaapi Procedure 2003
250 Nursing
Isometric Useful for maintaining muscle tone and strength. Prevents excessive bone loss especially if stimulate weight bearing. Exercise in which muscle tension is but the length of the muscle is not changed. i.e. quadriceps setting. Abdominal setting. Gluteal setting, hand squeeze, kegel exercises.
Copyright by Carmen M. Dimaapi
251
Anda mungkin juga menyukai
- Basic Nursing ProceduresDokumen9 halamanBasic Nursing Proceduresbernadette_olaveBelum ada peringkat
- PharmacologyDokumen9 halamanPharmacologyRPh Krishna Chandra JagritBelum ada peringkat
- Medical and Surgical NursingDokumen4 halamanMedical and Surgical NursingCrystal Ann Monsale TadiamonBelum ada peringkat
- Physiologic Changes of Aging: System AlterationDokumen1 halamanPhysiologic Changes of Aging: System Alterationshenric16100% (1)
- Disorders of The Genitourinary SystemDokumen49 halamanDisorders of The Genitourinary SystemYemaya84Belum ada peringkat
- How To Calculate IV Flow Rates:: ExampleDokumen3 halamanHow To Calculate IV Flow Rates:: ExampleJericho Duque0% (1)
- Management For CTD - MsDokumen63 halamanManagement For CTD - MsNarz CupahanBelum ada peringkat
- IV TherapyDokumen39 halamanIV TherapyRichard SiahaanBelum ada peringkat
- Principles of Medication AdministrationDokumen22 halamanPrinciples of Medication AdministrationTina TalmadgeBelum ada peringkat
- Urinary EliminationDokumen7 halamanUrinary EliminationJeityynnee Tubeo100% (1)
- Compilation of Nursing Theories With Concept AnalyzationDokumen164 halamanCompilation of Nursing Theories With Concept AnalyzationPatrick PantuaBelum ada peringkat
- Obstetric NursingDokumen36 halamanObstetric NursingpauchanmnlBelum ada peringkat
- CLIN PHARM - Fluids and ElectrolytesDokumen11 halamanCLIN PHARM - Fluids and ElectrolytesAlodia RazonBelum ada peringkat
- Airway-Obstruction NCLEX QuestionsDokumen27 halamanAirway-Obstruction NCLEX Questionschicas0sexy128100% (1)
- Hematologic DisordersDokumen40 halamanHematologic DisordersMary Grace LeronBelum ada peringkat
- Med-Surge QuestionsDokumen17 halamanMed-Surge QuestionsRosa0% (1)
- Fluids and Electrolytes ConceptDokumen31 halamanFluids and Electrolytes ConceptDarwin AndalBelum ada peringkat
- Nursing Management in Abdominal SurgeryDokumen19 halamanNursing Management in Abdominal Surgeryejguy7777100% (2)
- Pediatric Vital Sign Normal RangesDokumen5 halamanPediatric Vital Sign Normal Rangestinea nigraBelum ada peringkat
- Medical-Surgical Skills ChecklistDokumen7 halamanMedical-Surgical Skills ChecklistVin BitzBelum ada peringkat
- Respiratory DiseasesDokumen14 halamanRespiratory DiseasesKira100% (6)
- Sexually Transmitted DiseasesDokumen5 halamanSexually Transmitted Diseasesreghpineda28Belum ada peringkat
- Bullets in Bioethics, NLE, NUrse, NursingDokumen3 halamanBullets in Bioethics, NLE, NUrse, NursingKatBelum ada peringkat
- NoteesDokumen177 halamanNoteespearlanne1292100% (1)
- Dosage & CalculationsDokumen20 halamanDosage & CalculationsKnight-Zussette VillarBelum ada peringkat
- Medical Surgical Nursing TionkoDokumen40 halamanMedical Surgical Nursing TionkojeshemaBelum ada peringkat
- Gastrointestinal DiseasesDokumen11 halamanGastrointestinal DiseasesFreeNursingNotes100% (1)
- Pruritus PRURITIS Pruritis (Itching) Is One of The Most CommonDokumen2 halamanPruritus PRURITIS Pruritis (Itching) Is One of The Most CommonFreeNursingNotesBelum ada peringkat
- Blood Disorders AnemiaDokumen6 halamanBlood Disorders AnemiaFreeNursingNotesBelum ada peringkat
- Intake and Output (I&O) : Key TerminologyDokumen5 halamanIntake and Output (I&O) : Key TerminologyJack KeurigBelum ada peringkat
- NUR100 Sherpath Oxygenation and PerfusionDokumen17 halamanNUR100 Sherpath Oxygenation and Perfusioncaloy2345caloyBelum ada peringkat
- MedSurg CH 44 & 45 Study GuideDokumen5 halamanMedSurg CH 44 & 45 Study GuideMichele ShepardBelum ada peringkat
- Pulmonary Assessment and Disorders CH 33 34 35 36 Osborn 2012Dokumen321 halamanPulmonary Assessment and Disorders CH 33 34 35 36 Osborn 2012parmeshoriBelum ada peringkat
- 220 Nursing Bullets Fundamentals of Nursing Reviewer 1Dokumen23 halaman220 Nursing Bullets Fundamentals of Nursing Reviewer 1Kyles JumaritoBelum ada peringkat
- Nursing Lecture RespiratoryDokumen13 halamanNursing Lecture RespiratoryAedge010100% (1)
- Diabetic Ketoacidosis: 4 Signs of DKA: Acidosis (Metabolic, Raised Anion Gap), Ketosis, Dehydration and HyperglycaemiaDokumen3 halamanDiabetic Ketoacidosis: 4 Signs of DKA: Acidosis (Metabolic, Raised Anion Gap), Ketosis, Dehydration and HyperglycaemiajsdlzjBelum ada peringkat
- IV InsertionDokumen9 halamanIV InsertionSharmaine Grace FlorigBelum ada peringkat
- Pedia NotesDokumen7 halamanPedia NotesFreeNursingNotes100% (1)
- Respiratory DisordersDokumen18 halamanRespiratory Disordersjdigal100% (4)
- NCLEXDokumen7 halamanNCLEXmsdrewn30Belum ada peringkat
- Burn 2Dokumen4 halamanBurn 2lyn_aiBelum ada peringkat
- Basic Nursing Fundamentals EliminationDokumen35 halamanBasic Nursing Fundamentals Eliminationlisa100% (1)
- Fundamentals of NursingDokumen5 halamanFundamentals of NursingKaren Mae Santiago AlcantaraBelum ada peringkat
- Flaccid BladderDokumen29 halamanFlaccid BladderphotosaurusrapBelum ada peringkat
- Physical AssessmentDokumen19 halamanPhysical AssessmentMamerto Q. Flores IIIBelum ada peringkat
- Posttest. Renal DisordersDokumen3 halamanPosttest. Renal Disordersjbagacay100% (3)
- Nursing Mnemonics 2Dokumen3 halamanNursing Mnemonics 2ja100% (10)
- Colorectal CancerDokumen31 halamanColorectal CancerIrene RealinoBelum ada peringkat
- Pulmonary PathoPhysiologyDokumen45 halamanPulmonary PathoPhysiologySuliman Garalleh100% (1)
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDokumen42 halamanHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezBelum ada peringkat
- Medical Surgical Nursing - RespiratoryDokumen15 halamanMedical Surgical Nursing - RespiratoryChristian Esteves75% (4)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDari EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideBelum ada peringkat
- Enema AdministrationDokumen37 halamanEnema Administrationapi-3722454100% (6)
- Urinary-Catheterization (1)Dokumen31 halamanUrinary-Catheterization (1)hazel jamisBelum ada peringkat
- Insertion of TubesDokumen29 halamanInsertion of Tubesqopcyrus10Belum ada peringkat
- Fundamental Nsg-IiDokumen46 halamanFundamental Nsg-IiabiyotBelum ada peringkat
- EnemaDokumen2 halamanEnemaMelanie ZoiloBelum ada peringkat
- Additional Nursing ProceduresDokumen28 halamanAdditional Nursing ProceduresRona LynBelum ada peringkat
- Administering An EnemaDokumen13 halamanAdministering An EnemaNai DhavalBelum ada peringkat
- Group 2 - Rose & Sadava - Chest Tube InsertionDokumen19 halamanGroup 2 - Rose & Sadava - Chest Tube InsertionRay Anthony RoseBelum ada peringkat
- Motor DeiselShip Latest PDFDokumen154 halamanMotor DeiselShip Latest PDFCadet Prateek SaxenaBelum ada peringkat
- Design of Marina Structures and FacilitiesDokumen23 halamanDesign of Marina Structures and FacilitiesAhmed Balah0% (1)
- Presentation On Dysuria 1Dokumen25 halamanPresentation On Dysuria 1ankur acharyaBelum ada peringkat
- Cocoa Nursery Manual Feb 2013Dokumen51 halamanCocoa Nursery Manual Feb 2013jeffreyBelum ada peringkat
- Boiler Installation - AfbcDokumen2 halamanBoiler Installation - AfbcSarah FrazierBelum ada peringkat
- Fdocuments - in From The Margins To The Mainstream Disaster Research at The CrossroadsDokumen26 halamanFdocuments - in From The Margins To The Mainstream Disaster Research at The CrossroadsHanan M. HadidiBelum ada peringkat
- 10 Effective Ayurvedic Treatment For Hair LossDokumen9 halaman10 Effective Ayurvedic Treatment For Hair Lossrpav77Belum ada peringkat
- Barista Coffee Company LTDDokumen3 halamanBarista Coffee Company LTDGanesh AnandBelum ada peringkat
- DSE8620 MKII Operator ManualDokumen224 halamanDSE8620 MKII Operator Manualhenrygrados44Belum ada peringkat
- Kf22Qt Sec4 FRDDokumen21 halamanKf22Qt Sec4 FRDMauro PerezBelum ada peringkat
- LF1325LC 装机准备要求 LF1325LC installation requirementsDokumen12 halamanLF1325LC 装机准备要求 LF1325LC installation requirementsEliasDraBelum ada peringkat
- Issues Pertaining To Maintenance of WifeDokumen2 halamanIssues Pertaining To Maintenance of WifeVaishnavi YadavBelum ada peringkat
- Leon County Sheriff'S Office Daily Booking Report 18-Oct-2020 Page 1 of 3Dokumen3 halamanLeon County Sheriff'S Office Daily Booking Report 18-Oct-2020 Page 1 of 3WCTV Digital TeamBelum ada peringkat
- Safety Data Sheet: Rhodamine B (C.I.45170) For MicrosDokumen9 halamanSafety Data Sheet: Rhodamine B (C.I.45170) For MicrosSeshagiri KalyanasundaramBelum ada peringkat
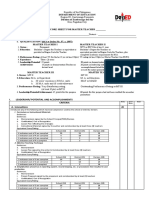
- I. Leadership/ Potential and Accomplishments Criteria A. InnovationsDokumen5 halamanI. Leadership/ Potential and Accomplishments Criteria A. InnovationsDEXTER LLOYD CATIAG100% (1)
- Made in His ImageThe Amazing Design of The Human BodyDokumen4 halamanMade in His ImageThe Amazing Design of The Human BodyAriam MariaBelum ada peringkat
- AnswersDokumen4 halamanAnswersamitmehta29Belum ada peringkat
- Module-1-ISO 13485-DocumentDokumen7 halamanModule-1-ISO 13485-Documentsri manthBelum ada peringkat
- EP-HQ-GDL-008-00 Safety - Critical - Elements - Integrity - Management - GuidelineDokumen57 halamanEP-HQ-GDL-008-00 Safety - Critical - Elements - Integrity - Management - GuidelineAHMED AMIRA100% (5)
- PROD - Section 1 PDFDokumen1 halamanPROD - Section 1 PDFsupportLSMBelum ada peringkat
- Predrag Mladenovic CVDokumen3 halamanPredrag Mladenovic CVStefan Markovic JagodinacBelum ada peringkat
- Imteyaz ResumeDokumen2 halamanImteyaz ResumeImteyaz AhmadBelum ada peringkat
- Diesel Engine Lab ReportDokumen27 halamanDiesel Engine Lab ReportParadoodleBelum ada peringkat
- NPMHU, USPS Contract Arbitration AwardDokumen73 halamanNPMHU, USPS Contract Arbitration AwardPostalReporter.comBelum ada peringkat
- Sample Emg/Ncv Report - Normal StudyDokumen5 halamanSample Emg/Ncv Report - Normal StudyPhysiotherapist AliBelum ada peringkat
- Antithesis Essay Joseph JaroszDokumen3 halamanAntithesis Essay Joseph JaroszJoseph JaroszBelum ada peringkat
- By Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSDokumen9 halamanBy Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSAngela SaldajenoBelum ada peringkat
- Resume PLPDokumen2 halamanResume PLPapi-302180779Belum ada peringkat
- EO MNC 10 June 2022Dokumen4 halamanEO MNC 10 June 2022LeulaDianneCantosBelum ada peringkat
- Carjackked TrainingDokumen7 halamanCarjackked TrainingErios 50Belum ada peringkat