Or Write Up-Cystectomy
Diunggah oleh
Mark Jude GapuzDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Or Write Up-Cystectomy
Diunggah oleh
Mark Jude GapuzHak Cipta:
Format Tersedia
Patients Profile Case No.:23832 Name: C.
B Age: 28 Address: Poblacion Bontoc, Mountain Province Gender: Male Pre-op diagnosis: Multiple Cholelitiasis Post-op diagnosis: Multiple Cholelitiasis Operation Performed: Open Cholecystectomy
Anatomy and Physiology:
Gallbladder is a muscular organ that serves as a reservoir for bile, present in most vertebrates. In humans, it is a pearshaped membranous sac on the undersurface of the right lobe of the liver just below the lower ribs. It is generally about 7.5 cm (about 3 in) long and 2.5 cm (1 in) in diameter at its thickest part; it has a capacity varying from 1 to 1.5 fluid ounces. The body (corpus) and neck (collum) of the gallbladder extend backward, upward, and to the left. The wide end (fundus) points downward and forward, sometimes extending slightly beyond the edge of the liver. Structurally, the gallbladder consists of an outer peritoneal coat (tunica serosa); a middle coat of fibrous tissue and unstriped muscle (tunica muscularis); and an inner mucous membrane coat (tunica mucosa). The gallbladder lies in a shallow depression on the interior surface of the liver, to which it is attached by loose connective tissue. Its wall is composed largely of smooth muscle. The gallbladder is connected to the common bile duct by the cystic duct.
The function of the gallbladder is to store bile, secreted by the liver and transmitted from that organ via the cystic and hepatic ducts, until it is needed in the digestive process. The gallbladder, when functioning normally, releases bile through the biliary ducts into the duodenum to aid digestion by promoting peristalsis and absorption, preventing putrefaction, and emulsifying fat. During storage, a large portion of the water in bile is absorbed through the walls of the gallbladder, so that bile in the gallbladder is five to 10 times more concentrated than that originally secreted by the liver. When food enters the duodenum, the gallbladder contracts and the sphincter of oddi relaxes. Relaxation of this sphincter allows the bile to enter the intestine. This response is mediated by secretion of the hormone cholecystokin-pancreozymin (CCK-PZ) from the intestinal wall.
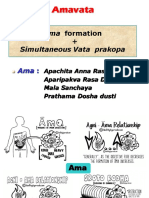
Pathophysiology: A. Narrative form: Cholesterol, a normal constituent of bile, is insoluble in water. Its solubility depends on bile acids and lecithin (phospholipids) in bile. In gallstone- prone patients, there is decreased bile acid synthesis and increased cholesterol synthesis in the live, resulting in bile supersaturated with cholesterol, which precipitates out of the bile to form stones. The cholesterol- saturated bile predisposes to the formation of gallstones and acts as an irritant that produces inflammatory changes in the gallbladder. Two to three times more women than men develop cholesterol stones and gallbladder disease; affected women are usually older than 40 years of age, multiparous, and obese patient. Stone formation is more frequent in people who use oral contraceptives, estrogens, or clofibrate; these medications are known to increase biliary cholesterol saturation. The incidence of stone formation increases with age as a result of increased hepatic secretion of cholesterol and decreased bile acid synthesis.
B. Schematic form: Predisposing Factors: Advanced Age Gender Ileal Resection/Disease Race Genetics
Precipitating Factors: Obesity/ Overweight Pregnancy/ Contraception Frequent Starvation, total parenteral nutrition Clofibrate Use Diet/ Weight loss
Decreased level of Bile Acids
Increased levels of fat in The blood stream Synthesis of cholesterol In the liver Excretion of cholesterol to the bile
Ratio of bile salts & lecithin with cholesterol is no longer within the area of solubility
Cholesterol concentration > Solubility capacity of the bile
No formation of mixed miccelles
Lithogenic bile/ supersaturated bile (creamy) Mucoprecipitates of organic & inorganic calcium salts become nucleation sites Nucleation and production of cholesterol monohydrate crystals
Large cholesterol stones
Extrusion of stones from gallbladder
Impaction at cystic and bile duct
Distention of billiary and fundus of gallbladder Forceful contraction of gallbladder
Bile not excreted to duodenum
Backflow of the bile and goes to the circulation
Spasms of smooth muscle in the duct
Levels of bilirubin/ bile pigments in the circulation
Conversion of bilirubin to urobilinogen in the intestines
Fat not emulsified No absorption of fat in the intestines
PAIN
Increased renal excretion of Dark urine
Excretion of urobinilogen in the stool Grayish stool
Nausea and Vomiting Fullness Indigestion Vit. ADEK
y y y
Preparation of the patient: A. Skin preparation: Begin at the intended sight of incision, either right subcostal, right paramedian, or midline, extending from the axilla to the pubic symphysis and down to the table on the sides. Skin is prepared with appropriate antiseptic solution (povidone iodine solution) at least 1/2-1 hour before surgery and just before surgery.
B. Draping: 4 folded towels and a laparotomy sheet, sterile sheets are used to cover all of the body except the operation site and adhesive drapes are stuck on the operation site. Position of patient during induction of anesthesia:
Lateral position: patient begins in supine position. Rolled onto side- operative side up. Bottom leg flexed; top leg straight. Bottom arm on armboard, top arm on special arm support or pillow. Head supported in alignment with body.
Position of the patient during the surgery:
Supine position: a position of the body: lying down with the face up, as opposed to the prone position, which is face down, sometimes with the hands behind the head or neck. When used in surgical procedures, it allows access to the peritoneal, thoracic and pericardial regions; as well as the head, neck and extremities. Using terms defined in the anatomical position, the dorsal side is down, and the ventral side is up.
C. Anesthesia Subarachnoid block or Spinal anesthesia is an extensive nerve block that is produced into the subarachnoid space at the lumbar level, usually between L4 and L5. It produces anesthesia of the lower extremities, perineum, and lower abdomen. For lumbar puncture procedure, the patient usually lies on the side in a knee- chest position. Sterile technique is used as a spinal puncture is made and medication is injected through the needle. As soon as the injection has been made, the patient is positioned on her back. The spread of anesthetic agent and the level of anesthesia depend on the amount of fluid injected, the speed with which it is injected, the positioning of the
8
patient affecter the injection, and the specific gravity of the agent. Discussion of the Procedure: The incision is right subcostal. The abdominal cavity is entered in the usual manner. The gallbladder is grasped. The cystic duct, cystic artery, and common bile duct are exposed. The surgeon must be aware of anomalies of these structures. The cystic artery is clamped using two right angle clamps and ligated with a suture passed on a long instrument or by clips, as is the cystic duct. The gallbladder is mobilized by incising the overlying peritoneum and after local dissection is removed. The underlying liver bed may be reperitonealized. A drain may be employed exiting a stab wound and secured to the skin with a stitch. The wound is closed layer by layer. The skin is closed with interrupted stitches.
INSTRUMENTATION Retractors: Army navy retractor
Held at one to shallow or superficial incisions.
Richardson retractor
Used to pull layers of tissue aside in deep abdominal or chest incision.
Deaver
Used to retract deep abdominal or chest incisions.
10
Doyen:
Used by surgeons to either actively separate the edges of a surgical incision or wound, or can hold back underlying organs and tissues, so that body parts under the incision may be accessed.
Forceps: Tissue forceps
An instrument with one or more fine teeth at the tip of each blade for controlling especially during suturing. tissues during surgery,
Thumb forceps
The forceps used for grasping soft tissue; used especially during suturing.
11
Scissors: Mayo (curved)
designed for cutting body tissues near the surface of the
wound. used for cutting heavy fascia and sutures.
Mayo (straight)
Used to cut suture and supplies.
Metzenbaum
Is more delicate than Mayo scissors which is used to cut delicate tissues.
12
Clamps: Towel clip
Allis
Used to hold towels and drapes in place.
Give surgeons the freedom to access internal organs and structures with minimal damage to the overlying tissues.
These forceps can grasp, hold, move or lock a tissue into a specific position so the surgeon can concentrate on the area requiring the surgical procedure. The locking and nonlocking options give surgeons more options and flexibility. Right-angle or Mixter - provides a straight surface to cut along when dividing tissue that has been occluded. - used to clamp hard-to-reach vessels and to place sutures behind or around a vessel.
13
Straight clamp:
They may be used for occluding blood vessels, manipulating [tissues], or for assorted other purposes.
Curved clamp:
They may be used for occluding blood vessels, manipulating [tissues], or for assorted other purposes.
Needle holder
Locks the needle in place, allowing the user to maneuver the needle through various tissues.
14
Miscellaneous: Knife or blade holder (#3)
Used to cut superficial tissue.
15
Others:
The dissection is started from gall bladder downwards. Anterior and posterior peritoneal leaves are stripped off gently. Cystic duct is gradually exposed by stripping fibrous bands and lymphatics. A lymph node is usually a land mark for cystic artery. Cystic artery is similarly exposed and skeletonised. It is critical that no structure is divided until the cystic duct and cystic artery are unequivocally identified.
The fundus of gall bladder is then pushed in lateral and cephalad direction. This maneuver exposes the entire gall bladder, cystic duct and porta hepatis.
16
The gall bladder is dissected off the liver bed while maintaining traction on the fundus of gall bladder, with the help of electro-cautery.
Clip ligation of cystic duct and artery is performed under vision, and cut between clips.
After securing hemostasis and suction of free fluid, gallbladder is retrieved through umbilical port with "BERT" bag (bag for endoscopic retrieval of tissue). A tube drain is left through the portal under vision in the subhepatic space and all fluid is sucked out.
17
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- AppendicitisDokumen15 halamanAppendicitisMark Jude GapuzBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Or Write Up-CystectomyDokumen17 halamanOr Write Up-CystectomyMark Jude GapuzBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Different Leadership Styles in Nursing(NCENHO7Dokumen11 halamanDifferent Leadership Styles in Nursing(NCENHO7Mark Jude GapuzBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- School NursingDokumen8 halamanSchool NursingMark Jude GapuzBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- CLASS 1 - Image - Roles Revised June 260Dokumen48 halamanCLASS 1 - Image - Roles Revised June 260Marie-Lynne L'orBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Multiple Births Definition, Causes & CareDokumen11 halamanMultiple Births Definition, Causes & CareCacing UcilBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Fphar 12 768268Dokumen25 halamanFphar 12 768268Araceli Anaya AlvaradoBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Army Medicine:: Maintaining, Restoring, and Improving HealthDokumen92 halamanArmy Medicine:: Maintaining, Restoring, and Improving HealthLeo Mak Hoi-fong100% (1)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Daftar Pustaka KolelitiasisDokumen2 halamanDaftar Pustaka KolelitiasisReni IstiarBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- You Can Grow Your IntelligenceDokumen6 halamanYou Can Grow Your IntelligenceSoniaBelum ada peringkat
- BSP Price List Agustus 2020Dokumen46 halamanBSP Price List Agustus 2020Anonymous aaAQ6dgBelum ada peringkat
- Rheumatoid Arthritis: Pathophysiology PathophysiologyDokumen34 halamanRheumatoid Arthritis: Pathophysiology PathophysiologyOmair RiazBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Annexure 'CD - 01' FORMAT FOR COURSE CURRICULUMDokumen4 halamanAnnexure 'CD - 01' FORMAT FOR COURSE CURRICULUMYash TiwariBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- CPV/CCV Ag (3 Lines) : VcheckDokumen2 halamanCPV/CCV Ag (3 Lines) : VcheckFoamfab WattikaBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Types of Hyperlipoproteinemia and Lipid AbnormalitiesDokumen22 halamanTypes of Hyperlipoproteinemia and Lipid Abnormalitiescollege3Belum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Morning Report (Cardiology) : On Duty: Nadya Julaifa, Nadya Julaifa Supervisor: Dr. Yusra Pintaningrum, Sp. JP (K) FIHADokumen16 halamanMorning Report (Cardiology) : On Duty: Nadya Julaifa, Nadya Julaifa Supervisor: Dr. Yusra Pintaningrum, Sp. JP (K) FIHAAdisti NurutamiBelum ada peringkat
- OT AssistantDokumen9 halamanOT AssistantIshfaq LoneBelum ada peringkat
- Fatal Airway Obstruction Due To Ludwig'sDokumen6 halamanFatal Airway Obstruction Due To Ludwig'sRegina MugopalBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Closed Tibia and Fibula Fracture Case PresentationDokumen30 halamanClosed Tibia and Fibula Fracture Case Presentationzhafran_darwisBelum ada peringkat
- Chapter 1Dokumen6 halamanChapter 1Hema Priya AdityanBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Contact AllergyDokumen39 halamanContact AllergylintangBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- 11 16 16Dokumen22 halaman11 16 16WoodsBelum ada peringkat
- Calculation SeatworkDokumen2 halamanCalculation SeatworkBenedict James BermasBelum ada peringkat
- Best Practice & Research Clinical Obstetrics and GynaecologyDokumen12 halamanBest Practice & Research Clinical Obstetrics and GynaecologyGrit WingsBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Youtsey Kristen Cover LetterDokumen1 halamanYoutsey Kristen Cover Letterapi-457850399Belum ada peringkat
- MCPS Form For Annual Sports Physical Exam - (PPE) 2010 Edition Prepared by Am Academy of Ped, Am. Academy of Family Phys Et Al.Dokumen5 halamanMCPS Form For Annual Sports Physical Exam - (PPE) 2010 Edition Prepared by Am Academy of Ped, Am. Academy of Family Phys Et Al.Concussion_MCPS_MdBelum ada peringkat
- BLS Adult Skills Checklist 2016Dokumen2 halamanBLS Adult Skills Checklist 2016Wahyudi QorahmanBelum ada peringkat
- Stroke Awareness EducationDokumen7 halamanStroke Awareness EducationIneke PutriBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- History Taking in JaundiceDokumen2 halamanHistory Taking in Jaundiceshanyiar100% (5)
- Aur VedaDokumen4 halamanAur VedaLalit MishraBelum ada peringkat
- DCTMDDokumen58 halamanDCTMDHanzara PanolBelum ada peringkat
- Joint Disorders - Ay NewDokumen46 halamanJoint Disorders - Ay NewPraisingson SyiemliehBelum ada peringkat
- IRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)Dokumen4 halamanIRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)analyn123Belum ada peringkat
- Create Consent Form (39 charactersDokumen3 halamanCreate Consent Form (39 charactersJan Diel100% (2)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)