CNS
Diunggah oleh
Aniket MittalDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CNS
Diunggah oleh
Aniket MittalHak Cipta:
Format Tersedia
PSEUDOTUMOR CEREBRI Background Pseudotumor cerebri, also known as idiopathic intracranial hypertension (IIH) is a disorder of unknown etiology.
It affects predominantly obese women of childbearing age.[1] The primary problem is chronically elevated intracranial pressure (ICP), and the most important neurologic manifestation ispapilledema, which may lead to progressive optic atrophy and blindness.[1]
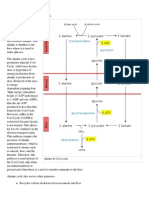
Pathophysiology A dominant early theory concerning the pathogenesis of elevated ICP in these patients was cerebral edema. Against this is the fact that no altered level of alertness, cognitive impairment, or focal neurological findings are associated with the elevated ICP. In addition, no pathologic signs of cerebral edema have been documented in these patients. Early reports describing edema were later considered to represent fixation artifact (ie, from tissue preparation) rather than in vivo edema. Current theories include increased resistance to cerebrospinal fluid (CSF) outflow at the arachnoid granulations that line the dural venous sinuses and through which CSF reabsorption is thought to occur by bulk flow. Alternatively, occult cerebral venous outflow abnormalities may produce IIH. Farb and colleagues have demonstrated that, in a series of 29 patients with IIH, narrowing of the transverse dural venous sinus was demonstrable on MR venography, while none of the 59 control subjects had this finding.[2] These authors suggest that the narrowing is a consequence of elevated intracranial pressure, and, when the narrowing develops, it exacerbates the pressure elevation by increasing venous pressure in the superior sagittal sinus.
CSF production rate (mL/min) should be equal to the CSF reabsorption rate. If production exceeds absorption, ICP rises until it exceeds mean arterial pressure, which, if sustained, would be fatal. In IIH the production rate equals the reabsorption rate; however, a higher than normal pressure is required to achieve this owing to the increased resistance at the arachnoid granulations. Bateman has shown that some patients with IIH with normal dural venous drainage have increased arterial inflow suggesting that collateral venous drainage occurs in addition to that provided by the superior sagittal sinus and transverse sinuses.[3] The same investigator measured MR venography and MR flow quantification in cerebral arteries and veins in a series of 40 patients with IIH, of which 21 patients had venous stenosis. The arterial inflow was 21% higher than normal and superior sagittal sinus outflow was normal, resulting in reduced percentage of venous outflow compared to inflow. The remainder of arterial inflow volume is presumed to have drained via collateral venous channels. With clinical remission of symptoms, the arterial inflow volumes returned to normal.[4] More recently, Bateman et al proposed a mathematical model to account for collapsible dural venous sinuses in the pathogenesis of IIH since this has been shown to be an important factor in many cases. The model includes arterial inflow volume, venous outflow resistance, and CSF pressure. They used combined flow rates in the 2 carotid arteries and the basilar artery as measured by MRI in individual patients as the measure of inflow blood volume and measured values from the literature for the pressure gradient from superior sagittal sinus to jugular bulb and venous outflow resistance.
The model predicts 2 CSF pressure equilibrium points for the collapsible dural sinus cases with greater than 40% stenosis (usually of the transverse sinus)one point in the normal range and the other in the range encountered in IIH patients. This accounts for the prolonged remission of symptoms that follows removal of CSF at lumbar puncture, presumably because this relieves the venous sinus stenosis. Without dural sinus collapse and stenosis, as is encountered in some patients with IIH, the model requires increased arterial inflow volume to account for the elevated intracranial pressure. Interestingly, the model did not require increased resistance to outflow of CSF across the arachnoid villi
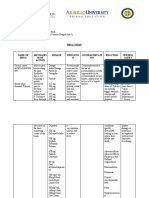
Causes In 1994, Radhakrishnan et al reviewed the literature on IIH associated with other diseases and with drugs. These authors insisted that, to be included in the list of causally related associations, the following criteria should be met:[11]
At least 2 cases should have been described. The reported cases should have met all the criteria for the diagnosis of IIH. Intracranial dural sinus thrombosis should have been ruled out with reasonable certainty. The following data were obtained from this 1994 study and subsequent case reports. The authors' organization of categories is preserved here Endocrine risk factors confirmed in epidemiological studies Female sex Reproductive age group Menstrual irregularity Obesity Recent weight gain Endocrine risk factors that meet minimal criteria, unconfirmed in case-controlled studies Adrenal insufficiency Cushing disease Hypoparathyroidism Hypothyroidism Excessive thyroxine replacement in children (ie, low thyrotrophin levels) Medication risk factors that meet minimal criteria, unconfirmed in case-controlled studies Cimetidine, corticosteroids, danazol, isotretinoin (Accutane), levothyroxine, lithium,[12] minocycline, nalidixic acid, nitrofurantoin, tamoxifen, tetracycline, trimethoprimsulfamethoxazole[11] All-trans -retinoic acid (ATRA) used in the treatment of promyelocytic leukemia, cyclosporine, levonorgestrel implant (Norplant; 39 women reported to US Food and Drug Administration [FDA] from February 1991-December 1993), pancreatin (pancreatic enzyme replacement for cystic fibrosis patients) Recombinant human growth hormone (7 children in 3 papers)/natural growth hormone (somatotropin) Vitamin A in infants Miscellaneous risk factors that meet minimal criteria, unconfirmed in case-controlled studies Chronic renal failure Systemic lupus erythematosus
NORMAL PRESSURE HYDROCEPHALUS Background Normal pressure hydrocephalus (NPH) is a clinical symptom complex characterized by abnormal gait, urinary incontinence, and dementia. It is an important clinical diagnosis because it is a potentially reversible cause of dementia. First described by Hakim in 1965, NPH describes hydrocephalusin the absence of papilledema and with normal cerebrospinal fluid (CSF) opening pressure on lumbar puncture.[1] Pathophysiology NPH differs from other causes of adult hydrocephalus. An increased subarachnoid space volume does not accompany increased ventricular volume. Clinical symptoms result from distortion of the central portion of the corona radiata by the distended ventricles. This may also lead to interstitial edema of the white matter and impaired blood flow, as suggested in nuclear imaging studies. The periventricular white matter anatomically includes the sacral motor fibers that innervate the legs and the bladder, thus explaining the abnormal gait and incontinence. Compression of the brainstem structures (ie, pedunculopontine nucleus) could also be responsible for gait dysfunction, particularly the freezing of gait that has been well described. Dementia results from distortion of the periventricular limbic system. The term normal pressure hydrocephalus was based on the finding that all 3 patients reported by Hakim and Adams showed low CSF pressures at lumbar puncture, namely 150, 180, and 160 mm H2 O. However, an isolated CSF pressure measurement by lumbar puncture clearly yields a poor estimation of the real intracranial pressure (ICP) in patients with NPH. Hakim first described the mechanism by which a normal or high-normal CSF pressure exerts its effects. Using the equation, Force = Pressure X Area, increased CSF pressure over an enlarged ependymal surface applies considerably more force against the brain than the same pressure in normal-sized ventricles. Normal pressure hydrocephalus may begin with a transient high-pressure hydrocephalus with subsequent ventricular enlargement. With further enlargement of the ventricles, CSF pressure
returns to normal; thus the term NPH, at least in view of the initial pathophysiologic events, is a misnomer. Intermittent intracranial hypertension has been noted in some patients. Some authors prefer the term extraventricular obstructive hydrocephalus. They believe that the initial event is diminished CSF absorption at the arachnoid villi. This obstruction to CSF flow leads to transient high-pressure hydrocephalus with subsequent ventricular enlargement. As the ventricles enlarge, CSF pressure returns to normal. History Patients present with a gradually progressive disorder. As noted above, the classic triad consists of abnormal gait, urinary incontinence, and dementia. The gait disturbance is typically the earliest feature noted and considered to be the most responsive to treatment. The primary feature is thought to resemble an apraxia of gait. True weakness or ataxia is typically not observed. The gait of NPH is characterized as bradykinetic, broad based, magnetic, and shuffling. The urinary symptoms of NPH can present as urinary frequency, urgency, or frank incontinence. While incontinence can result from gait disturbance and dementia, in a study by Sakakibara and colleagues, 95% of patients had urodynamic parameters consistent with detrusor overactivity.[6] The dementia of NPH is characterized by prominent memory loss and bradyphrenia. Frontal and subcortical deficits are particularly pronounced. Such deficits include forgetfulness, decreased attention, inertia, and bradyphrenia. The presence of cortical signs such as aphasia or agnosia should raise suspicion for an alternate pathology such as Alzheimer diseaseor vascular dementia. However, comorbid pathology is not uncommon with advancing age. In one study, more than 60% of patients with iNPH had cerebrovascular disease.[7] In another similar study, more than 75% had Alzheimer disease pathology at the time of shunt surgery.[8] Patients commonly present with a gait disorder and dementia. On neurologic examination, pyramidal tract findings may be present in addition to the above findings. Causes Normal pressure hydrocephalus may occur due to a variety of secondary causes but may be idiopathic in approximately 50% of patients. Secondary
causes of NPH include head injury, subarachnoid hemorrhage, meningitis, and CNS tumor. Another potential cause could be previously compensated congenital hydrocephalus.[9]
Anda mungkin juga menyukai
- Polychromasia - Wikipedia, The Free EncyclopediaDokumen1 halamanPolychromasia - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- List of Hematologic Conditions - Wikipedia, The Free EncyclopediaDokumen14 halamanList of Hematologic Conditions - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Mentzer Index - Wikipedia, The Free EncyclopediaDokumen1 halamanMentzer Index - Wikipedia, The Free EncyclopediaAniket Mittal0% (1)
- Pentose Phosphate Pathway - NADPH NADPH NADPH Wikipedia, The Free EncyclopediaDokumen5 halamanPentose Phosphate Pathway - NADPH NADPH NADPH Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Oxygen-Haemoglobin Dissociation Curve - Wikipedia, The Free EncyclopediaDokumen5 halamanOxygen-Haemoglobin Dissociation Curve - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Hemoglobin Op A Thy - Wikipedia, The Free EncyclopediaDokumen3 halamanHemoglobin Op A Thy - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Heme - Wikipedia, The Free EncyclopediaDokumen3 halamanHeme - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Cytochrome b5 - Wikipedia, The Free EncyclopediaDokumen3 halamanCytochrome b5 - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Fetal Hemoglobin - Wikipedia, The Free EncyclopediaDokumen4 halamanFetal Hemoglobin - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Erythropoietin - Wikipedia, The Free EncyclopediaDokumen12 halamanErythropoietin - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Cytochrome b5 Reductase - Wikipedia, The Free EncyclopediaDokumen2 halamanCytochrome b5 Reductase - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Cori Cycle - Wikipedia, The Free EncyclopediaDokumen2 halamanCori Cycle - Wikipedia, The Free EncyclopediaAniket Mittal100% (1)
- Duodenal Cytochrome B - Wikipedia, The Free EncyclopediaDokumen1 halamanDuodenal Cytochrome B - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Coombs Test - Wikipedia, The Free EncyclopediaDokumen6 halamanCoombs Test - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Bone Morphogenetic Protein - Wikipedia, The Free EncyclopediaDokumen3 halamanBone Morphogenetic Protein - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Hot Flash - Wikipedia, The Free EncyclopediaDokumen3 halamanHot Flash - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Anemia of Pre Maturity - Wikipedia, The Free EncyclopediaDokumen4 halamanAnemia of Pre Maturity - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- 2,3-Bisphosphoglyceric Acid - Wikipedia, The Free EncyclopediaDokumen6 halaman2,3-Bisphosphoglyceric Acid - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Blood Smear - Med Line Plus Medical EncyclopediaDokumen4 halamanBlood Smear - Med Line Plus Medical EncyclopediaAniket MittalBelum ada peringkat
- Acidosis Activates ComplementDokumen4 halamanAcidosis Activates ComplementAniket MittalBelum ada peringkat
- Alanine Cycle - Wikipedia, The Free EncyclopediaDokumen2 halamanAlanine Cycle - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Iron Overload - Wikipedia, The Free EncyclopediaDokumen7 halamanIron Overload - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Effect of Exogenous Glucocorticoid On Osmotic Ally Stimulated Anti Diuretic Hormone Secretion and On Water Re Absorption in ManDokumen6 halamanEffect of Exogenous Glucocorticoid On Osmotic Ally Stimulated Anti Diuretic Hormone Secretion and On Water Re Absorption in ManAniket MittalBelum ada peringkat
- Hereditary Hemorrhagic Telangiectasia - Wikipedia, The Free EncyclopediaDokumen14 halamanHereditary Hemorrhagic Telangiectasia - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Glomus Body - Wikipedia, The Free EncyclopediaDokumen1 halamanGlomus Body - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Git HormonesDokumen17 halamanGit HormonesAniket MittalBelum ada peringkat
- Bone ChapterDokumen1 halamanBone ChapterAniket MittalBelum ada peringkat
- Cardiac Rhythm Disorders With RMP and Inactivcating Sodium ChannelsDokumen37 halamanCardiac Rhythm Disorders With RMP and Inactivcating Sodium ChannelsAniket MittalBelum ada peringkat
- Axon - Wikipedia, The Free EncyclopediaDokumen7 halamanAxon - Wikipedia, The Free EncyclopediaAniket MittalBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Felten 2019 - LES - AnifrolumabDokumen9 halamanFelten 2019 - LES - AnifrolumabSimina BarbuBelum ada peringkat
- Pharmacology of The GIT System: CIC Ragasa, RN-MDDokumen70 halamanPharmacology of The GIT System: CIC Ragasa, RN-MDCarmencita Ileen Ragasa - AhmedBelum ada peringkat
- Nervous System: Nur Nabilah Binti Abdullah Nur Izyan Shahirah Binti Mohd BakriDokumen67 halamanNervous System: Nur Nabilah Binti Abdullah Nur Izyan Shahirah Binti Mohd BakriNur NabilahBelum ada peringkat
- Amenorrhea: Definition - This Is The Symptom of Absence of MenstruationDokumen10 halamanAmenorrhea: Definition - This Is The Symptom of Absence of MenstruationSuhas IngaleBelum ada peringkat
- The Weight of Traditional Therapy in The Management of Chronic Skin Diseases in Donka National HospitalDokumen7 halamanThe Weight of Traditional Therapy in The Management of Chronic Skin Diseases in Donka National HospitalAthenaeum Scientific PublishersBelum ada peringkat
- This Condition Is Caused by Mutations in The RBM10 GeneDokumen2 halamanThis Condition Is Caused by Mutations in The RBM10 GeneAbdi KebedeBelum ada peringkat
- Common Lab Tests & Their Use in Diagnosis & Treatment PDFDokumen17 halamanCommon Lab Tests & Their Use in Diagnosis & Treatment PDFChAwaisBelum ada peringkat
- Crush InjuryDokumen14 halamanCrush InjuryDioBelum ada peringkat
- Vicente Sotto Memorial Medical Center Department of Obstetrics & GynecologyDokumen9 halamanVicente Sotto Memorial Medical Center Department of Obstetrics & GynecologyIrah FloresBelum ada peringkat
- Anton'S Syndrome and Cortical Blindness: Case ReportDokumen3 halamanAnton'S Syndrome and Cortical Blindness: Case ReportDevasyaBelum ada peringkat
- Exceptional DevelopmentDokumen12 halamanExceptional DevelopmentMa. IvoryVan SantillanBelum ada peringkat
- Anaesthesia: Single Best Answer Mcqs inDokumen212 halamanAnaesthesia: Single Best Answer Mcqs indr rayyanBelum ada peringkat
- SilicossisDokumen72 halamanSilicossisAauLiiaa Lia LiiaBelum ada peringkat
- Denas Book Engl 2006 PDFDokumen138 halamanDenas Book Engl 2006 PDFParallaxsterBelum ada peringkat
- Acne Vulgaris A Disease of Western CivilizationDokumen7 halamanAcne Vulgaris A Disease of Western CivilizationMaab MurshidBelum ada peringkat
- 1 Drugs For HypertensionDokumen62 halaman1 Drugs For HypertensionSaniBelum ada peringkat
- Definition and Management of Odontogenic MaxillaryDokumen11 halamanDefinition and Management of Odontogenic MaxillaryAlleste OrenBelum ada peringkat
- P Wave AbnormalitiesDokumen20 halamanP Wave AbnormalitiesToufiqurRahmanBelum ada peringkat
- Mechanisms of Hypoxemia: Review ArticleDokumen14 halamanMechanisms of Hypoxemia: Review ArticleJhon CruzBelum ada peringkat
- Drug Study - Atorvastatin CalciumDokumen2 halamanDrug Study - Atorvastatin CalciumCath Bril50% (2)
- Pharmacogenetics and The Concept of Individualized Medicine: BS ShastryDokumen6 halamanPharmacogenetics and The Concept of Individualized Medicine: BS Shastrykunalprabhu148Belum ada peringkat
- Dialysis Treatment - A Comprehensive DescriptionDokumen13 halamanDialysis Treatment - A Comprehensive Descriptionrmprskgwk5Belum ada peringkat
- Dr. Alurkur's Book On Cardiology - 2Dokumen85 halamanDr. Alurkur's Book On Cardiology - 2Bhattarai ShrinkhalaBelum ada peringkat
- FDA Executive Summary Dermal FillersDokumen41 halamanFDA Executive Summary Dermal FillersAhmed Sad100% (1)
- wk8 Nursing Care of A Family When A Child Has An Immune Disorders Part 1Dokumen19 halamanwk8 Nursing Care of A Family When A Child Has An Immune Disorders Part 1claire yowsBelum ada peringkat
- Tylenol - Acetaminophen - Fabros, JennyDokumen3 halamanTylenol - Acetaminophen - Fabros, JennyJenny Agustin FabrosBelum ada peringkat
- WP Contentuploads201902yin Yang Qiao Yin Yang Wei Dai Mai PDFDokumen240 halamanWP Contentuploads201902yin Yang Qiao Yin Yang Wei Dai Mai PDFAnissa Hamid100% (1)
- ICD 10 Volume 3 - Alfabet PDFDokumen779 halamanICD 10 Volume 3 - Alfabet PDFDediBelum ada peringkat
- SPINAL NERVE Presentation Completed-2Dokumen51 halamanSPINAL NERVE Presentation Completed-2Sheikh Muhammad MuhallilBelum ada peringkat
- b1 3 OriginalDokumen1 halamanb1 3 OriginalfabianBelum ada peringkat