Pain in Pregnancy and Labor
Diunggah oleh
Suresh KumarDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Pain in Pregnancy and Labor
Diunggah oleh
Suresh KumarHak Cipta:
Format Tersedia
Core Curriculum for Professional Education in Pain, edited by J.
Edmond Charlton, IASP Press,
Seattle, 2005.
36
Pain and Pregnancy and Labor
I. Perception of pain in pregnancy Know the factors that can influence the perception of pain in pregnancy compared with the nonpregnant state: A. Fear of pain (Saisto and Halmesmaki 2003): may be primary (usually in nulliparous women, and may be associated with pre-existing psychological morbidity and/or ignorance), or secondary (e.g., as a result of a previous bad experience). B. Increased susceptibility to pain due to generalized anxiety (related to the pregnancy, its outcome, its implications for the woman, or other concerns). C. Positive attitudes to pregnancy and its social implications: may increase tolerance to pain, especially in labor (pain is seen as a positive force rather than a destructive one). D. Level of education: poor knowledge and/or misinformation may exacerbate the above. E. Age/parity: younger women may have increased tolerance to pain, but older multiparae may be more relaxed and therefore less fearful. F. Neuroendocrine system (Whipple et al. 1990; Shapira et al. 1995): sex steroids, e.g., 17 beta-estradiol and progesterone, can modulate the opioid system during pregnancy (e.g., via spinal dynorphin pathways), increasing pain tolerance.
II.
Causes of pain in pregnancy Be familiar with the spectrum of conditions that can present with pain during pregnancy: A. Not specific to, but common during, pregnancy. 1. Headache: most commonly tension headache or migraine; both have similar triggers and treatment. Recurrence may be due to reluctance to take analgesics in pregnancy, but the usual pattern is improvement over time, usually in the first trimester. It is important to exclude depression, sleep deprivation, pre-eclampsia, subarachnoid hemorrhage, cerebral tumors, and other focal lesions. Management is with simple measures, nondrug treatments, analgesics, and beta-blockers if headache is recurrent and severe. 2. Back pain: occurs in approximately 50% of pregnant women (Rathmell et al. 1997). Pain is increased by preexisting problems, multiparity, and increased age. Its early presentation (commonly the first trimester) suggests that weight gain is not the only factor; neuronal and endocrine mechanisms have been implicated (the polypeptide relaxin, secreted by the corpus luteum, softens the pelvic ligaments to allow accommodation of the developing fetus and facilitate vaginal delivery, and is thought to contribute to back problems during and after pregnancy). The pain is typically described as dull (lumbar), stabbing (gluteal), burning (thoracic), and/or accompanied by paresthesia (root compression). Management includes normal daily activity where possible, physiotherapy and analgesics. Sacroiliitis is common and may respond to manipulation. Epidural steroid injections are usually avoided in pregnancy if possible.
Pain in Pregnancy and Labor
3. Nerve entrapment: carpal tunnel syndrome is the most common; approximately 50% of sufferers experience pain. Although common in normal pregnancy, it may be associated with excessive fluid retention, e.g., pre-eclampsia, heart failure. Treatment is with elevation and splints, or surgery. Entrapment of the lateral cutaneous nerve of the thigh (meralgia paraesthetica) may also cause pain/paresthesia. Nerve entrapment may cause abdominal pain (see below). 4. Abdominal pain: nonspecific pain is common in pregnancy and may occasionally be severe; it is thought to be related to the physical presence of the enlarging uterus and stretching/displacement of abdominal structures. Softening and stretching of the ligaments of the symphysis pubis may cause suprapubic pain that can be severe, especially if there is distraction of the symphysis. Nerve entrapment may also occur. 5. Other potentially dangerous conditions that may present with pain should also be considered, e.g., sickle crisis, pulmonary embolism. Trauma is also an important cause of pain, and pregnant women are often victims of domestic violence. B. Specific to pregnancy: obstetric causes of abdominal pain include torsion/rupture of ovarian cysts, ectopic pregnancy, amnionitis/pelvic infection, labor, placental abruption, and uterine rupture. III. Management of pain in pregnancy Be familiar with the principles of management: A. Nonpharmacological methods are used where possible. The risk of harm to both mother and fetus should always be considered. B. The neuroendocrine changes of pregnancy mean that parturients are more susceptible to anesthetics (both local and general) and analgesics. C. Placental transfer of drugs depends on protein binding, lipid solubility, maternal metabolism, and molecular weight. With the exception of large polar molecules, e.g., insulin/heparin, all drugs are transferred to a degree. Drugs may also have indirect fetal effects via maternal effects (e.g., by affecting the mothers blood pressure). D. Be aware that the pharmacokinetics and pharmacodynamics of analgesics are altered in pregnancy. IV. Mechanisms and characteristics of labor pain Understand the causes, pathways, and features of labor pain: A. Causes 1. First stage: uterine contractions and dilatation of the lower uterine segment and cervix to allow passage of the fetus. 2. Second stage: greater pressure of the presenting part on pain-sensitive pelvic structures and distension of surrounding structures. B. Pathways 1. Uterus and cervix: mainly via A-delta and C fibers passing in the sympathetic nerves to the sympathetic chain; referred to the T10L1 dermatomes. 2. Vagina and pelvic outlet: via A-delta and C fibers passing in the parasympathetic bundle in the pudendal nerves; referred to the S2S4 dermatomes. 3. Other: contributions from the ilioinguinal, genitofemoral, and perforating branch of the posterior cutaneous nerve of the thigh; somatic pain experienced in the L2S5 dermatomes. C. Features 1. Over 90% of women experience severe/unbearable labor pain, although recollection fades with time.
Pain in Pregnancy and Labor
2. Typically, pain is similar to other types of visceral pain, i.e., intermittent, severe, and colicky; it starts in the lower abdomen and back, spreading to the perineum and thighs (Lowe 2000). 3. Pain may be influenced by the factors already listed above, in particular by social,societal, and cultural aspects. Certain cultures are more emotive and expressive than other, more stoic ones, leading possibly to differences in pain behavior rather than in the extent of pain felt. Fatigue and general debility, common in late pregnancy, may also contribute to the experience of labor pain. V. Consequences of labor pain A. Understand that labor pain may have adverse physiological and psychological consequences: 1. Respiratory: causes hyperventilation, leading to hypocapnia and respiratory acidosis. 2. Cardiovascular: increases cardiac output and blood pressure via sympathetic activity; this may be problematic in cardiac disease and pre-eclampsia. Increased venous return associated with uterine contractions may also contribute. 3. Neuroendocrine: increases maternal catecholamine secretion with risk of uteroplacental constriction. 4. Gastrointestinal: effect of labor on gastric emptying and acidity is unclear, although delayed emptying and increased acid secretion have been suggested. Opioids are well known to induce gastric stasis. 5. Psychological: severe labor pain has been implicated in contributing to long-term emotional stress, with potential adverse consequences on maternal mental health and family relationships. B. Understand also that pain during labor may have benefits: 1. Indicates to the mother and those assisting labor/delivery that contractions are occurring. 2. May have positive connotations regarding childbirth, related to societal/cultural influences. 3. May indicate problems (e.g. uterine rupture, placental abruption). VI. Management of labor pain Be familiar with methods of management of labor pain (available techniques will vary according to local resources and customs): A. Nonpharmacological: 1. Psychological preparation/support, e.g., sympathetic partner, relatives and care-givers; appropriate relaxing environment; psychoprophylaxis, i.e., positive conditioning, distraction, and relaxation techniques (Simkin and OHara 2002). 2. Hypnosis: needs appropriately trained hypnotist; 1020% women are not susceptible to hypnosis, and side effects include anxiety states. 3. Aromatherapy, reflexology, and acupuncture: labor-intensive, and their role is thought to be limited. 4. Transcutaneous electrical nerve stimulation (TENS): often used in early labor and for low levels of pain, but its efficacy in labor is not supported by a systematic review (Carroll et al. 1997). 5. Others: include abdominal decompression and distraction techniques. B. Systemic analgesia: 1. Parenteral: a. Pure opioids, e.g., pethidine (meperidine), morphine, diamorphine; more recently fentanyl and remifentanil. Many of the apparent analgesic effects may be due to sedation (Olofsson et al. 1996). All cross the placenta easily, and both mother and baby need monitoring during and after labor. b. Mixed agents, e.g., meptazinol, tramadol: show no evidence of greater efficacy or safety than traditional opioids.
Pain in Pregnancy and Labor
2. Inhalational: a. Nitrous oxide: available premixed 50:50 with oxygen in many countries, where it is widely used but of limited efficacy. May cause nausea, drowsiness, or euphoria and may interact with opioids to cause maternal desaturation. b. Volatile agents: most have been studied and found to be helpful, though limited by difficulties in delivery (e.g. draw-over vaporizers and scavenging required) and side effects, particularly sedation. C. Regional analgesia: 1. Local infiltration/nerve blocks: a. Paracervical block: rarely used because of the high risk of intravascular injection and fetal bradycardia. b. Pudendal block: used for vaginal deliveries (including instrumental). Blocks the pudendal nerve (S2S4) arising from the sacral plexus, supplying the lower vagina, vulva and perineum. Ineffective for procedures requiring extensive manipulation e.g. mid-cavity forceps/rotations. 2. Neuraxial techniques: a. Caudal: rarely used in developed countries because lumbar epidurals are easier to manage and more flexible. b. Spinal: useful for single procedures, e.g., instrumental delivery, but less commonly used for labor, because the effect of a single-shot spinal may not last long enough, even if opioids and local anesthetic are used together. c. Lumbar epidural: widely used in developed countries. Has the following advantages: i. Thought to be the most effective form of analgesia in labor. ii. Provides analgesia for instrumental/assisted delivery. iii. Avoids the need for general anesthesia with its attendant risks, since the epidural can be topped up for cesarean section or other procedures. iv. Improves the management of pre-eclampsia and thought to be of benefit in multiple pregnancy and prematurity. v. Reduces cardiovascular, respiratory, and neurological stress in systemic disease. vi. May improve neonatal acid-base status in maternal exhaustion. 3. Contra-indications are similar to those in non-obstetric practice; hypovolemia and coagulopathy are the most common. Thrombocytopenia, e.g., associated with pre-eclampsia, may contraindicate neuraxial techniques, although the benefits must be weighed against the risks, and the safe cutoff for platelet count is unknown (most authorities using a cut-off of 70100 x 109/l). 4. Brief summary of techniques: a. An epidural catheter is usually placed at L3L4 or L4L5. In combined spinal-epidural (CSE) techniques, intrathecal local anesthetic and opioid (e.g., bupivacaine 24 mg with fentanyl 10 20 g) are injected first, using either a needle-through-needle or separate-space method. More rapid onset and better analgesia have been claimed for CSE, but these are disputed. b. Epidural analgesia is commonly achieved using low-dose mixtures (e.g., bupivacaine 0.1% with fentanyl 2 g/mL) by infusion (815 mL/h) or bolus (1015 mL as required). Patient-controlled analgesia is also used, but it requires more complex delivery systems, and its advantages and disadvantages are still disputed. c. Bupivacaine is still widely used; ropivacaine and levobupivacaine have been introduced more recently. Fentanyl is the most commonly used opioid; in the United States sufentanil is popular. 5. Complications are as for nonpregnant patients. If accidental dural puncture occurs during epidural analgesia, postdural puncture headache occurs in ~50% of cases; the risk of headache after spinal anesthesia with 2527 G pencil-point needles is <2% (Choi et al. 2003). Neurological lesions are common after childbirth, so women should be warned of the small extra risk from regional analgesia (Loo et al. 2000).
Pain in Pregnancy and Labor
REFERENCES
Carroll D, Tramer M, McQuay H, Nye B, Moore A. Transcutaneous electrical nerve stimulation in labour pain: a systematic review. Br J Obstet Gynaecol 1997; 104:169175. Choi PT, Galinski SE, Takeuchi L, et al. PDPH is a common complication of neuraxial blockade in parturients: a meta-analysis of obstetrical studies. Can J Anaesth 2003; 50:460469. Loo CC, Dahlgren G, Irestedt L. Neurological complications in obstetric regional anaesthesia. Int J Obstet Anesth 2000; 9:99 124. Lowe N. The nature of labor pain. Am J Obstet Gynecol 2000; 186:S1624. Olofsson C, Ekblom A, Ekman-Ordeberg G, Hjelm A Irestedt L. Lack of analgesic effect of systemically administered morphine or pethidine on labour pain. Br J Obstet Gynaecol 1996; 103:968972. Rathmell J, Viscomi C, Ashburn M. Management of nonobstetric pain during pregnancy and lactation. Anesth Analg 1997; 85:10741087. Saisto T, Halmesmaki E. Fear of childbirth: a neglected dilemma. Acta Obstet Gynecol Scand 2003; 82:201208. Shapira SC, Magora F, Chrubasik S, et al. Assessment of pain threshold and pain tolerance in women in labour and in the early post-partum period by pressure algometry. Eur J Anaesthesiol 1995; 12:495499. Simkin P, OHara M. Nonpharmacologic relief of pain during labor: systematic reviews of five methods. Am J Obstet Gynaecol 2002; 186:S131159. Whipple B, Josimovich JB, Komisaruk BR. Sensory thresholds during the antepartum, intrapartum and postpartum periods. Int J Nursing Stud 1990; 27:213221.
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Essiac Nature's Cure For CancerDokumen14 halamanEssiac Nature's Cure For CancerTrevanian2Belum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- 2023 Psgs Guidelines For Accreditation of Residency Training ProgramDokumen121 halaman2023 Psgs Guidelines For Accreditation of Residency Training ProgramJobelle0% (1)
- AYUSHDokumen39 halamanAYUSHSujatha J Jayabal88% (8)
- DewormingDokumen48 halamanDewormingJulie Ann Escartin80% (5)
- Airway ManagementDokumen42 halamanAirway ManagementKugan KishurBelum ada peringkat
- Physiotherapy Treatment ScarsDokumen3 halamanPhysiotherapy Treatment ScarsYuyun Aryuni MusrifBelum ada peringkat
- Labour Analgesia - Recent ConceptsDokumen18 halamanLabour Analgesia - Recent ConceptsSuresh KumarBelum ada peringkat
- ACLS AlgorithmsDokumen4 halamanACLS Algorithmsmonickams100% (1)
- Anaesthetic Management of Ihd Patients For Non Cardiac SurgeryDokumen18 halamanAnaesthetic Management of Ihd Patients For Non Cardiac SurgerySuresh KumarBelum ada peringkat
- Bed SoreDokumen16 halamanBed SoreKim AquinoBelum ada peringkat
- Case Study - AGE With Some DHNDokumen19 halamanCase Study - AGE With Some DHNJessica Mae Abaquita-javierBelum ada peringkat
- Swiss Guidelines For Safe 1.7 Dry Needling 01Dokumen21 halamanSwiss Guidelines For Safe 1.7 Dry Needling 01monkeyhsuBelum ada peringkat
- Alleviating Cancer PainDokumen9 halamanAlleviating Cancer PainSuresh KumarBelum ada peringkat
- Sri Ganga Ram Policy - From Apps Portal PDFDokumen330 halamanSri Ganga Ram Policy - From Apps Portal PDFmaneeshnithBelum ada peringkat
- MSC 1st Yr Unit PlanDokumen10 halamanMSC 1st Yr Unit PlanSilja ManojBelum ada peringkat
- GO S For Tamilnadu DoctorsDokumen160 halamanGO S For Tamilnadu DoctorsSuresh KumarBelum ada peringkat
- Ventilator Associated Pneumonia (Vap)Dokumen11 halamanVentilator Associated Pneumonia (Vap)Suresh KumarBelum ada peringkat
- Spinal Anesthesia For Caeserian Section: Comparison of 5.0% Lignocaine and 0.5% BupivacaineDokumen4 halamanSpinal Anesthesia For Caeserian Section: Comparison of 5.0% Lignocaine and 0.5% BupivacaineSuresh KumarBelum ada peringkat
- Cerebral Protection What Is New ?Dokumen11 halamanCerebral Protection What Is New ?Suresh Kumar100% (1)
- Medico-Legal Issues in AnaesthesiaDokumen2 halamanMedico-Legal Issues in AnaesthesiaSuresh KumarBelum ada peringkat
- Local Anaesthetic AgentsDokumen21 halamanLocal Anaesthetic AgentsSuresh KumarBelum ada peringkat
- Anaesthetic Management of Blunt Chest TraumaDokumen11 halamanAnaesthetic Management of Blunt Chest TraumaSuresh KumarBelum ada peringkat
- Controversial Issues in NeuroanaesthesiaDokumen12 halamanControversial Issues in NeuroanaesthesiaSuresh KumarBelum ada peringkat
- Anesthesia For Fetal SurgeryDokumen8 halamanAnesthesia For Fetal SurgerySuresh KumarBelum ada peringkat
- Day Care AnesthesiaDokumen4 halamanDay Care AnesthesiaSuresh KumarBelum ada peringkat
- Role of The Anaesthesiologists in The Management of BurnsDokumen12 halamanRole of The Anaesthesiologists in The Management of BurnsSuresh KumarBelum ada peringkat
- Anaesthesia in The Gastrointestinal Endoscopy SuiteDokumen3 halamanAnaesthesia in The Gastrointestinal Endoscopy SuiteSuresh KumarBelum ada peringkat
- Anaesthesia Care Beyond Operating Rooms: Newer Opportunities & Challenges.Dokumen8 halamanAnaesthesia Care Beyond Operating Rooms: Newer Opportunities & Challenges.Suresh Kumar100% (1)
- Perioperative Management of A Patient With Left Ventricular FailureDokumen6 halamanPerioperative Management of A Patient With Left Ventricular FailureSuresh KumarBelum ada peringkat
- Depth of Anesthesia & MonitoringDokumen2 halamanDepth of Anesthesia & MonitoringSuresh KumarBelum ada peringkat
- Surgical Patients at Risk For Renal FailureDokumen35 halamanSurgical Patients at Risk For Renal FailureSuresh KumarBelum ada peringkat
- Analysis of Arterial Blood GasesDokumen17 halamanAnalysis of Arterial Blood GasesSuresh KumarBelum ada peringkat
- Anaesthetic Management of Bleeding Obstetric PatientDokumen10 halamanAnaesthetic Management of Bleeding Obstetric PatientSuresh KumarBelum ada peringkat
- Muscle Relaxants in Current PracticeDokumen6 halamanMuscle Relaxants in Current PracticeSuresh KumarBelum ada peringkat
- Anaesthesia Breathing SystemsDokumen15 halamanAnaesthesia Breathing SystemsSuresh KumarBelum ada peringkat
- Anaesthesia For Bleeding TonsilDokumen6 halamanAnaesthesia For Bleeding TonsilSave MedicalEducation Save HealthCareBelum ada peringkat
- Pre-Operative Cardio-Pulmonary Exercise Testing (Cpet)Dokumen14 halamanPre-Operative Cardio-Pulmonary Exercise Testing (Cpet)Suresh KumarBelum ada peringkat
- Preoperative Anaesthetic Risk Assessment and Risk Reduction Before SurgeryDokumen17 halamanPreoperative Anaesthetic Risk Assessment and Risk Reduction Before SurgerySuresh KumarBelum ada peringkat
- Anaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Dokumen16 halamanAnaesthetic Management of Patients With Pacemakers and Implantable Cardioverter Defibrillator.Suresh KumarBelum ada peringkat
- Basic Physics Applied To AnaesthesiologyDokumen10 halamanBasic Physics Applied To AnaesthesiologySuresh KumarBelum ada peringkat
- Fluid Resuscitation in TraumaDokumen17 halamanFluid Resuscitation in TraumaSuresh Kumar100% (1)
- Pulmonary Function Test in Pre Anaesthetic EvaluationDokumen10 halamanPulmonary Function Test in Pre Anaesthetic EvaluationSuresh KumarBelum ada peringkat
- CVA - Case ScenarioDokumen3 halamanCVA - Case ScenarioHarvey T. Dato-onBelum ada peringkat
- LeptospirosisDokumen13 halamanLeptospirosis천사천사Belum ada peringkat
- 2019 CIS - 1 Dysphagia - Odynaphagia - Atypical CPDokumen22 halaman2019 CIS - 1 Dysphagia - Odynaphagia - Atypical CPorangenarwhalBelum ada peringkat
- Drugs Abuse in RomaniaDokumen5 halamanDrugs Abuse in RomaniaGiorcoata AlexandruBelum ada peringkat
- Drug-induced rheumatic syndromes: the need to be awareDokumen2 halamanDrug-induced rheumatic syndromes: the need to be awaredentsavvyBelum ada peringkat
- A Simple Technique To Measure The Volume of Removed Buccal FatDokumen3 halamanA Simple Technique To Measure The Volume of Removed Buccal FatGuilherme GuerraBelum ada peringkat
- 31-10-19, Mrs. SY, 33 Y.O. Fraktur Blow Out+Fraktur Maxilla Le Fort I+Fr. Nasal. Dr. Saktrio D Subarno, Sp. BP-REDokumen28 halaman31-10-19, Mrs. SY, 33 Y.O. Fraktur Blow Out+Fraktur Maxilla Le Fort I+Fr. Nasal. Dr. Saktrio D Subarno, Sp. BP-REanon_893244902Belum ada peringkat
- Methodology For The Systematic Reviews On Occupational Therapy For Adults With Alzheimer's Disease and Related DementiasDokumen7 halamanMethodology For The Systematic Reviews On Occupational Therapy For Adults With Alzheimer's Disease and Related DementiasPedro Quintulén MillalénBelum ada peringkat
- Treadmill Test: Khairul Nizam Abdul Rahman 4262143008Dokumen12 halamanTreadmill Test: Khairul Nizam Abdul Rahman 4262143008Dea Amelia YolandaBelum ada peringkat
- 香港脊醫 Hong Kong Chiropractors May 2018Dokumen18 halaman香港脊醫 Hong Kong Chiropractors May 2018CDAHKBelum ada peringkat
- Reports 1Dokumen1 halamanReports 1ziauddin2Belum ada peringkat
- CHAPTER 1 Thesis ProposalDokumen2 halamanCHAPTER 1 Thesis ProposalPaul BejarBelum ada peringkat
- PenicillinsDokumen21 halamanPenicillinssekarenthangavelBelum ada peringkat
- Priyadarshini, 2010Dokumen9 halamanPriyadarshini, 2010AmandaBelum ada peringkat
- Notice To Kettle Falls SDDokumen2 halamanNotice To Kettle Falls SDErin RobinsonBelum ada peringkat
- September 2011Dokumen38 halamanSeptember 2011Ricardo Huchiyama TakayamaBelum ada peringkat
- Paracetamol Drug StudyDokumen1 halamanParacetamol Drug Studyrain peregrinoBelum ada peringkat
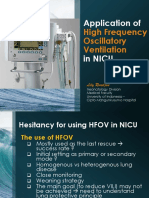
- Application HFOV in NICU - Lily RundjanDokumen43 halamanApplication HFOV in NICU - Lily Rundjandiah ayu pitalokaBelum ada peringkat