Tuberculosa Nasofaring FTP
Diunggah oleh
Diah HayustiningsihDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Tuberculosa Nasofaring FTP
Diunggah oleh
Diah HayustiningsihHak Cipta:
Format Tersedia
The Laryngoscope Lippincott Williams & Wilkins, Inc.
, Philadelphia 2003 The American Laryngological, Rhinological and Otological Society, Inc.
Tuberculosis of the Nasopharynx: A Rare Entity Revisited
Gary M. K. Tse, FRCPC; Tony K. F. Ma, FRCPA; Amy B. W. Chan, MBChB; Fiona N. Y. Ho, FRCS; Ann D. King, FRCR; Kitty S. C. Fung, FRCPA; Anil T. Ahuja, FRCR
Objectives: Tuberculosis of the nasopharynx is uncommon. A large series of 17 cases is reported, and the clinical and pathological features are discussed. Study Design: A retrospective review. Methods: Seventeen archived cases of biopsy-proven nasopharyngeal tuberculosis were reviewed for patient age and sex, presenting complaint and duration, systemic symptoms, cervical lymphadenopathy, and chest x-ray findings. These findings were compared with a compilation of 40 cases reported in the English literature. Results: There was a female predominance (13 women and 4 men), with age range of 20 to 74 years (mean age, 38 y). The most common presentation was enlargement of the cervical lymph nodes (53%), followed by hearing loss (12%), tinnitus, otalgia, nasal obstruction, and postnasal drip (6% each). The duration of the presenting symptoms ranged from 1 week to 1 year (mean duration, 16 wk). Ten patients (59%) had cervical lymphadenopathy, two (12%) had systemic symptoms (fever, weight loss, night sweats), and one patient (6%) had miliary pulmonary tuberculosis. Direct endoscopic examination showed nasopharyngeal mucosal irregularity or mass in the majority of patients (12 patients [70%]). These features were similar to those reported in the literature. Conclusions: Nasopharyngeal tuberculosis is uncommon, usually occurring without pulmonary or systemic involvement. Cervical lymphadenopathy occurs in more than half of the patients and is the most common presenting complaint; this, together with the nasopharyngeal findings of mass or mucosal irregularity, makes differentiation from carcinoma on clinical examination difficult, necessitating histological evaluation. Key Words: Nasopharynx, tuberculosis, undifferentiated carcinoma, granuloma, granulomatous inflammation. Laryngoscope, 113:737740, 2003
INTRODUCTION
Tuberculosis (TB) of the nasopharynx is rare. Although the upper respiratory tract is the usual portal of entry for pulmonary TB, involvement of the upper respiratory tract either in isolation or as part of systemic (or pulmonary) disease remains uncommon. In a large historical series of 843 cases of TB, only 1.8% of cases showed upper respiratory tract involvement, with one case of nasopharyngeal involvement.1 In the English literature, only three large series described nasopharyngeal TB in detail, and these series, respectively, reported 7 to 14 cases.2 4 The remainder of reports in the literature were single case reports, approximately 10 cases in all.514 In the present case series, the authors reviewed 17 cases, with emphasis on the disease features as compared with the previous series.
MATERIALS AND METHODS
Archived material from the Department of Pathology was searched for TB of nasopharynx from 1990 to 2002, yielding 20 cases in all. Three patients had a history of concurrent undifferentiated carcinoma (nasopharyngeal carcinoma [NPC]) and were excluded from the present review. All the medical records were retrieved. The information extracted, when available, included age, sex, presenting complaint and duration, systemic symptoms, clinical examination findings including appearance of the nasopharynx, and chest x-ray findings. The pathological materials of the nasopharyngeal biopsies were retrieved and reviewed, and the diagnosis confirmed. Ziehl Neelsen staining was performed on the biopsy material to detect acid-fast bacilli, and in some cases, multiple sections were examined.
RESULTS
Seventeen cases were reviewed, of which 13 were in women and four were in men. The patient age range was 20 to 74 years (mean age, 39 y). Ten patients (59%) presented with enlarged neck nodes, including eight (47%) with unilateral nodes and two (12%) with bilateral nodes. Two patients (12%) presented with hearing and one patient (6%) each presented with tinnitus, otalgia, nasal obstruction, and postnasal drip. One patient (6%) did not have any symptoms referable to the head and neck region. The duration of the presenting symptoms ranged from 1 week to 1 year (mean duration, 16 wk). Only two patients (12%) had fever, night sweats, Tse et al.: Nasopharyngeal Tuberculosis
From the Departments of Anatomical and Cellular Pathology (G.M.K.T., A.B.W.C.) and Surgery (F.N.Y.H.), Division of Otorhinolaryngology, and the Departments of Diagnostic Radiology and Organ Imaging (A.D.K., A.T.A.) and Microbiology (K.S.C.F.), Prince of Wales Hospital, Chinese University of Hong Kong; and the Department of Pathology (T.K.F.M.), Alice Ho Min Ling Nethersole Hospital, Republic of China. Editors Note: This Manuscript was accepted for publication November 26, 2002. Send Correspondence to Gary M. K. Tse, FRCPC, Department of Anatomical and Cellular Pathology, Ngan Shing Street, Shatin, NT, Hong Kong, Republic of China. E-mail: garytse@cuhk.edu.hk
Laryngoscope 113: April 2003
737
Fig. 1. Nasopharyngeal biopsy specimen with surface respiratory epithelium (short arrow) and multiple granulomas composed of epithelioid histiocytes (long arrow) in the submucosa (H&E stain, original magnification 00). Inset: Acid-fast bacilli, consistent with Mycobacteria tuberculosis is seen (inset, Ziehl Neelsen, original magnification 400).
and weight loss. Endoscopic examination of the nasopharynx showed mucosal irregularity, resembling lymphoid hyperplasia in six (35%) patients, a nasopharyngeal mass in six patients (35%), mucosal swelling in one patient (6%), white patch on mucosa in one patient (6%), and ulceration in one patient (6%). In one patient (6%)
the nasopharynx appeared normal. In one case, the finding was not recorded. Chest x-ray examination showed miliary TB in one patient (6%) and features of old lesions in four patients (24%). For the remaining 12 patients, 4 (24%) had normal chest x-ray findings and the results were not recorded in 8 patients.
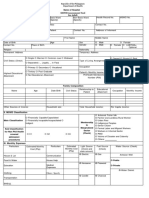
TABLE I. Clinical Features of All Patients.
Case No. Sex Age (y) Duration (wk) Presenting Symptoms Systemic Symptoms Nasopharyngeal Appearance Chest X-ray
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17
F M F F F F F M F F F F F F M F M
24 20 30 69 74 28 19 23 22 64 29 49 29 31 22 61 63
8 Unknown 4 8 16 12 52 1 24 8 Unknown Unknown 16 Unknown 8 8 52
Otalgia Unknown Neck node Right ear tinnitus Neck node Neck node Nasal obstruction Neck node Neck node Neck node Hearing loss Left hearing loss Neck node (bilat) Neck node Neck node (bilat) Neck node Nasal obstruction
Yes Unknown Yes No No No No No No No No No No No No No No
Granular Unknown Lymphoid hyperplasia Roof mass Normal Rough right wall Large exophytic mass at all wall Irregular Central lymphoid hyperplasia Bulging mass Lymphoid Right whitish patch Central swelling Mass Irregular ulcer at right central NP Mass Mass
Not available Not available Normal Pleural thickening Apical pleural thickening Normal Not available Miliary TB Normal Right upper lobe old granuloma Not available Not available Not available Not available Normal Right upper zone fibrocalcified change Not available
Laryngoscope 113: April 2003
Tse et al.: Nasopharyngeal Tuberculosis
738
TABLE II. Clinical Features of All Patients Reported in the Literature.
Patient No. Year 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 1992 1992 1992 1992 1992 1992 1992 1992 1992 1972 1972 1972 1972 1972 1972 1972 1999 1984 1986 Reference 2* 2 2 2 2 2 2 2 2 3 3 3 3 3 3 3 5 6 7 Sex/Age (y) M/37 M/35 F/26 F/38 F/25 F/76 M/48 M/41 F/27 M/18 M/26 F/59 F/22 F/36 F/57 F/47 F/20 M/35 F/54 Complaint Neck node Neck node Decrease hearing Unknown Nasal obstruction Nasal obstruction Neck node Neck node Neck node Neck node Headache Neck node Neck node Neck node Neck node Sore throat Chronic otitis media Neck node Facial pain Duration (wk) 12 16 12 12 4 20 4 12 8 25 4 16 25 16 12 25 52 4 1 NP Appearance Irregularity Mass Irregularity Mass Mass Mass Irregularity Irregularity Mass Mass Mass White discoloration Mass Mass Irregularity Mass Unknown Irregular, right Mass Yes Yes No No Yes Yes Yes Yes Yes Yes No Yes Yes Yes Yes Yes Unknown Yes Unknown LN NP Biopsy Neg Pos Pos Pos Pos Pos Neg Neg Neg Pos Pos Pos Neg Pos Neg Pos Pos Pos Pos No No No Active TB No No No Old TB No No No No No No No No Old TB No Active TB on drug for 1 year No Micronodules, nodes pos No No Old TB No No 14 Active TB No 7 7 Lung
20 21 22 23 24 25 26
1992 1999 1994 2002 1997 1985 1981
8 9 10 11 12 13 14 4
F/58 F/64 F/42 F/58 F/70 F/18 M/62 M F Range Mean 12 2 1761 34
Otalgia Pharyngeal pain Nasal obstruction Snoring Altered taste/smell Neck LN Nasal obstruction Neck node 11 2 2
12 8 Unknown Unknown 16 3 Unknown 16 wk or 12 2
Slough Swelling Mass, midline Swelling Unknown Unknown Mass Mass Normal 11 2
No No Unknown No Unknown Yes Unknown Yes No 12 2
Neg Neg Neg Neg Neg Neg Pos Pos
2740 1996
Post nasal drip Brisk epistasis
16 wk
*This series reported 10 cases, but one patient had NPC and TB and was thus excluded from this review. This series reported 14 cases, but individual patients data were not reported or tabulated separately. LN cervical lymphadenopathy; NP biopsy nasopharyngeal biopsy; neg granulomatous inflammation but direct stain for acid fast bacilli negative; pos granulomatous inflammation and positive direct Ziehl Neelsen stain for acid fast bacilli.
In all cases, nasopharyngeal biopsies were performed to rule out NPC, which has a similar presentation and a high incidence in this locality. The biopsy specimens showed granulomatous inflammation with epithelioid histiocytes and multinucleated giant cells of Langerhans type. Ziehl Neelsen staining for acid-fast bacilli was positive in all cases (Fig. 1). All the patients responded to treatment for TB.
DISCUSSION
Nasopharyngeal TB represents an uncommon and unique form of TB infection. This disease is rare, and the number of reported cases in the English literature is low. The current report represents the largest series. Before the present report, there were three large series reported in the English literature, being written 6, 10, and 30 years Laryngoscope 113: April 2003
ago, respectively.13 Hence, it is of great interest to compare the clinical features of the current cases (Table I) in the present series with the historical compilation (Table II). In our series, neck lymph node enlargement as a presenting symptom accounted for 53% of cases, whereas symptoms referable to the ear and nose area in terms of tinnitus, nasal obstruction, hearing loss, and otalgia accounted for most of the remainder. These findings were similar to those in the literature, in which enlarged lymph nodes was the most common (58%) presenting symptom followed by nasal obstruction (10%) and pain around the head and neck region, tinnitus, and hearing loss. Direct examination of the nasopharynx revealed a combination of mass and irregularity, which, together, accounted for a major proportion (70%) in our series and 75% of cases in the literature. More important, findings on direct examiTse et al.: Nasopharyngeal Tuberculosis
739
nation may be normal, as was shown in one case (6%) in our series and two cases (5%) in the literature. The relation among TB of the nasopharynx, cervical lymph nodes, and pulmonary infection merits further discussion. In primary nasopharyngeal TB, involvement of the cervical nodes is common, occurring in more than 50% of cases. Co-existing active or old pulmonary involvement or systemic disease is less common, with 30% (five cases) occurring in our series and 25% in the literature. Conversely, nasopharyngeal involvement in TB cervical lymphadenopathy and pulmonary TB is exceeding rare. In an elegant study of 75 patients with excision-proven TB of cervical nodes, the nasopharynx was shown to be the only primary focus of infection in one patient (1%), without pulmonary or systemic involvement.15 The same was true for pulmonary TB, with a reported incidence of nasopharyngeal involvement in 1.8% of cases only.1 The inference is that TB of the nasopharyngeal is usually primary and isolated; the chance of co-existing lung infection is low. The mechanism for such a phenomenon remains unclear. Involvement of TB of the upper airways was by contiguous spread from the active lung lesion through infected sputum or other secretion. In a large series of cases of laryngeal TB, abnormal findings on chest x-ray examination were noted in 95% of patients.16 However, the rate of lung involvement in nasopharyngeal TB is low, suggesting that contiguous spread would have to occur from ongoing or reactivation of subclinical pulmonary TB, or the nasopharynx truly represents the primary portal of transmission from inhalation of TB in airborne droplets. Cervical lymphadenopathy in nasopharyngeal TB is common and does not imply systemic spread of the disease. The common scenario of enlarged cervical lymph nodes with a nasopharyngeal mass or irregularity, but without systemic symptoms, makes the disease virtually indistinguishable from NPC, making histological evaluation imperative in endemic areas such as southern China. The contribution of TB in the causation of granulomatous diseases in the head and neck region remains difficult to estimate. Other causes of granulomas include sarcoidosis, vasculitic diseases such as Wegeners granulomatosis, fungal infections or reactive changes in response to carcinoma or lymphoma (particularly Hodgkins disease), and radiotherapy. Because positive identification of the acid-fast bacilli in smears or cultures is a prerequisite for diagnosis of TB, its incidence is likely to be underestimated. In a study of 22 cases of tonsillar granulomas,17 no underlying cause was identified in one-third of the cases, and the possibility of undiagnosed TB has to be considered. With the improvement of techniques for detecting TB, including polymerase chain reaction for the bacterial DNA, and increased awareness, particularly in view of the resurgence of TB, the incidence of TB of the upper aerodigestive tract is likely to increase.
The authors have reported a large series of cases of nasopharyngeal TB, which showed a female predominance, as well as neck node enlargement as the most common presentation. In the majority of cases, examination showed a mass lesion or mucosal irregularity in the nasopharynx, making differentiation from carcinoma difficult. This poses a particular diagnostic problem in some regions of the world such as Southeast Asia and Africa, where NPC and TB are endemic, particularly because enlarged cervical lymph nodes are a common presenting symptom in both diseases. Furthermore, nasopharynx TB is usually isolated, without pulmonary or systemic symptoms. The similar clinical features of patients included in the current series and those reported 10 to 30 years ago has suggested that little progress has been made in the early detection of the disease. With the recent resurgence of TB, it is imperative to be aware of the rare cases of nasopharyngeal TB.
BIBLIOGRAPHY
1. Rohwedder JJ. Upper respiratory tract tuberculosis: sixteen cases in a general hospital. Ann Intern Med 1974;80: 708 713. 2. Waldron J, van Hasselt CA, Skinner DW, Arnold M. Tuberculosis of the nasopharynx: clinicopathological features. Clin Otolaryngol 1992;17:5759. 3. Sim T, Ong BH. Primary tuberculosis of the nasopharynx. Singapore Med J 1972;13:39 43. 4. Eng HL, Su CY, Chen WJ. Nasopharyngeal tuberculosis. Chang Gung Med J 1996;19:149 153. 5. Case records of the Massachusetts General Hospital: case 13. N Engl J Med 1999;340:1349 1354. 6. Raizada RM, Behl R, Bhongsade V, Khan N. Primary nasopharyngeal tuberculosis. Ear Nose Throat J 1984;63: 70 74. 7. Narendran K, Chan R, Poh WT. Nasopharyngeal tuberculosis presenting as a mass. Singapore Med J 1986;27:170 172. 8. Bath AP, OFlynn P, Gibbin KP. Nasopharyngeal tuberculosis. J Laryngol Otol 1992;106:1079 1080. 9. Percodani J, Braun F, Arrue P, et al. Nasopharyngeal tuberculosis. J Laryngol Otol 1999;113:928 931. 10. Chopra RK, Kerner MM, Calcaterra TC. Primary nasopharyngeal tuberculosis: a case report and review of this rare entity. Otolaryngol Head Neck Surg 1994;111:820 823. 11. Atkan B, Selimoglu E, Ucuncu H, Sutbeyaz Y. Primary nasopharyngeal tuberculosis in a patient with the complaint of snoring. J Laryngol Otol 2002;116:301303. 12. Butt AA. Nasal tuberculosis in the 20th century. Am J Med Sci 1997;313:332335. 13. Lesser THJ, Jefferis AS, Shaw HJ. Pseudotumoral mycobacterial infections of the head and neck. J Laryngol Otol 1985;99:277283. 14. Goodman RS, Mattel S, Kaufman D, Grant JM. Tuberculoma of the nasopharynx. Laryngoscope 1981;91:194 197. 15. Lau SK, Kwan S, Lee J, Wei WI. Source of tubercle bacilli in cervical lymph nodes: a prospective study. J Laryngol Otol 1991;105:558 561. 16. Rupa V, Bhanu TS. Laryngeal tuberculosis in the eighties: an Indian experience. J Laryngol Otol 1989;103:864 868. 17. Kardon DE, Lester DR, Thompson MD. A clinicopathologic series of 22 cases of tonsillar granulomas. Laryngoscope 2000;110:476 481.
Laryngoscope 113: April 2003
Tse et al.: Nasopharyngeal Tuberculosis
740
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Derajat Paresis Nervus FasialisDokumen1 halamanDerajat Paresis Nervus FasialisDiah HayustiningsihBelum ada peringkat
- 2010 Article 116Dokumen6 halaman2010 Article 116Diah HayustiningsihBelum ada peringkat
- Derajat Paresis Nervus FasialisDokumen1 halamanDerajat Paresis Nervus FasialisDiah HayustiningsihBelum ada peringkat
- 2011 Article 271Dokumen4 halaman2011 Article 271Diah HayustiningsihBelum ada peringkat
- Prognosis RHSDokumen6 halamanPrognosis RHSDiah HayustiningsihBelum ada peringkat
- O To SclerosisDokumen4 halamanO To SclerosisDiah HayustiningsihBelum ada peringkat
- Tympanometry in Clinical Practice: Janet Shanks and Jack ShohetDokumen32 halamanTympanometry in Clinical Practice: Janet Shanks and Jack ShohetDiah HayustiningsihBelum ada peringkat
- A Singer's Notes: Preventing Vocal Nodules: Teresa Radomski, MMDokumen21 halamanA Singer's Notes: Preventing Vocal Nodules: Teresa Radomski, MMDanis WaraBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Compiled Quiz RLEDokumen29 halamanCompiled Quiz RLEbabesBelum ada peringkat
- Guadalquiver v. Sea Power Shipping Enterprise, Inc. GR No. 226200Dokumen2 halamanGuadalquiver v. Sea Power Shipping Enterprise, Inc. GR No. 226200Maynard Gabayno100% (1)
- Vampires and Death in New England, 1784 To 1892Dokumen17 halamanVampires and Death in New England, 1784 To 1892Ferencz IozsefBelum ada peringkat
- Unlock Your Tight Hip FlexorsDokumen63 halamanUnlock Your Tight Hip FlexorsPina Olson Campbell100% (2)
- Mental HealthDokumen31 halamanMental HealthGelo Angeles100% (1)
- Case Study of Children With Special NeedsDokumen21 halamanCase Study of Children With Special NeedsGrf Trust83% (69)
- General Objecti-Wps OfficeDokumen3 halamanGeneral Objecti-Wps OfficeSumit YadavBelum ada peringkat
- Valley Sports Winter 2019-20 ProfileDokumen32 halamanValley Sports Winter 2019-20 ProfileAaron YoungBelum ada peringkat
- Report #5 (Tomás Castro)Dokumen26 halamanReport #5 (Tomás Castro)Tomas Castro D SantosBelum ada peringkat
- V. Self-Assessment ACTIVITY 1: Warm You UpDokumen3 halamanV. Self-Assessment ACTIVITY 1: Warm You UpNerissa Lejano RosasBelum ada peringkat
- Goodhope Asia Holdings Sustainability Journey - June 2018Dokumen9 halamanGoodhope Asia Holdings Sustainability Journey - June 2018Tapian PadBelum ada peringkat
- Adult Mswd-ToolDokumen3 halamanAdult Mswd-Toolclaverialc10Belum ada peringkat
- Medical TattooingDokumen66 halamanMedical TattooingTattooTattoo100% (4)
- Sagittal First - Ortho TribuneDokumen8 halamanSagittal First - Ortho TribuneOrtho OrganizersBelum ada peringkat
- Ethics, Privacy, and SecurityDokumen10 halamanEthics, Privacy, and SecuritySittie Aina Munder100% (1)
- GMP History PDFDokumen49 halamanGMP History PDFSubhradipBelum ada peringkat
- MSDS Serat Kaca PDFDokumen11 halamanMSDS Serat Kaca PDFGita AzhariBelum ada peringkat
- Questions KatzungDokumen46 halamanQuestions KatzungYalman Eyinç100% (3)
- Statement Uni - SenithaDokumen2 halamanStatement Uni - SenithaSenitha MindulaBelum ada peringkat
- Healthy Food EssayDokumen2 halamanHealthy Food EssayFebri FebrianiBelum ada peringkat
- Ellen Respiratory Module PortraitDokumen11 halamanEllen Respiratory Module PortraitAbdelmar SusulanBelum ada peringkat
- Aquaponics DesignDokumen74 halamanAquaponics Designwilliam_pepito100% (8)
- Organic Anti-Aging Blend Essential Oil (100 Pure - USDA Certified Organic) Best Therapeutic Grade Essential Oil - 1Dokumen1 halamanOrganic Anti-Aging Blend Essential Oil (100 Pure - USDA Certified Organic) Best Therapeutic Grade Essential Oil - 1Leandro LucatoBelum ada peringkat
- Dependent Personality DisorderDokumen3 halamanDependent Personality DisorderRanaAdnanShafiqueBelum ada peringkat
- KKP Mpu3022Dokumen4 halamanKKP Mpu3022Zulbasim ZiyadBelum ada peringkat
- List of Crash Cart SuppliesDokumen2 halamanList of Crash Cart SuppliesMariefel Villanueva AlejagaBelum ada peringkat
- CF 756Dokumen100 halamanCF 756Manoj KumarBelum ada peringkat
- DapusDokumen7 halamanDapusPutriPasaribuBelum ada peringkat
- PMF-015-HSE-110 v2 HSE Guideline For Construction Sites ExcavationDokumen17 halamanPMF-015-HSE-110 v2 HSE Guideline For Construction Sites ExcavationmerinofalBelum ada peringkat
- Pencarrow Lighthouse Conservation PlanDokumen98 halamanPencarrow Lighthouse Conservation PlanClarice Futuro MuhlbauerBelum ada peringkat