Jurnal Egg Alergy
Diunggah oleh
cristieristiieDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Jurnal Egg Alergy
Diunggah oleh
cristieristiieHak Cipta:
Format Tersedia
Khristy Chang 1 07120100107
EGG ALLERGY AND MMR VACCINATION By: Adam Fox and Gideon Lack
Introduction Anaphylaxis is a recognized side effect of any vaccination. Life threatening allergic reactions to the measles, mumps, and rubella (MMR)) vaccination are very rare but the possibility still causes considerable anxiety among parents. This anxiety is particularly marked in parents of children with egg allergy.
Sequence of events A child presented to the allergy clinic at 1 year of age following type 1 hypersensitivity reactions to peanuts and eggs. The reactions had no cardiorespiratory features. Skin prick testing confirmed sensitisation to peanuts and eggs and these were thereafter excluded from the diet. The child also had eczema and later developed asthma. Owing to initial parental concern about the risks of anaphylaxis to the MMR vaccine in egg-allergic children, the advice of the general practitioner (GP) was sought. The parents were counselled that an increased risk of anaphylaxis meant that hospital admission was required for vaccination. Frightened by this potential risk, they decided against vaccination at 13 months and against having the preschool booster. By the age of 7 years old, the child remained sensitised to both peanuts and eggs. While attending an accident and emergency department, he came into contact with another child infected with the measles virus. Two weeks later he developed coryzal symptoms and a cough. As well as extreme misery, pyrexia, conjunctivitis, anorexia and lethargy, the child soon developed a rash that spread from his ears and head to become confluent over the rest of his body. On examination he was found to have
Khristy Chang / 07120100107 cervical and axillary lymphadenopathy. His severe symptoms led to a complete refusal to take fluids, and the resulting dehydration required a 3-day hospital admission. Nasopharyngeal aspirate revealed the measles virus, and serology confirmed the presence of immunoglobulin M antibody to the measles virus. Two weeks after an initial recovery, the child represented with bilateral hip pain that prevented weight bearing. There was no associated temperature and inflammatory markers were mildly elevated. The pain eventually settled with 5 days of bed rest and anti-inflammatory medication. A presumptive A Fox, MA, MSc, MRCPCH, specialist registrar; G Lack, FRCPCH, consultant, Department of Paediatric Allergy and Immunology, St Marys Hospital, London. Address for correspondence Dr Adam Fox, 48 Lansdowne Road, Stanmore, Middlesex, HA7 2SA. E-mail: adam.fox2@virgin.net Submitted: 4 March 2003; Editors response: 26 June 2003; final acceptance: 29 July 2003. British Journal of General Practice, 2003, 53, 801-802. diagnosis of reactive arthritis was made. The family later requested single vaccinations to mumps and rubella. Discussion MMR vaccine contains attenuated virus that has been grown in chick embryo fibroblasts, and has been shown to contain tiny amounts of egg protein.3 Despite this, most severe allergic reactions to MMR vaccine occur in children who are not allergic to eggs. Sensitisation to other vaccine compo- nents, such as gelatine or neomycin, is
Khristy Chang 3 07120100107
responsible for many reactions. Large case series have demonstrated that administration of MMR vaccine is safe in children with egg allergy,4 and the Royal College of Paediatrics and Child Health, and the British Society of Allergy and Clinical Immunology have endorsed the guidelines shown in Box 1. However, concern among parents over the safety of vaccination in these children, and confusion among profes- sionals5 is still leading to its erroneous deferral or exclusion from the vaccination schedule of some children.4 Given that egg allergy has a prevalence of up to 2.4% of 3-year-olds,6 this confusion poses a significant public health risk. The Green Book7 is the most commonly used source of information when vaccination queries arise. Unfortunately, the current issue, published in 1996, predates the published guidelines and recommends paediatric advice is sought when there is uncertainty regarding the need for vaccination to take place in hospital. As a result, issues surrounding MMR vaccination in egg-allergic children are the most common reason for GP correspondence to our allergy clinic. Failure to vaccinate against measles leaves a child vulner- able, not only to an unpleasant viral illness, but also to its potentially lethal sequelae. Pneumonitis and encephalitis are among the well-recognised complications, whereas mumps may also lead to pancreatitis and orchitis. With vaccine uptake falling as a result of misinformation regarding other associations with the MMR vaccine, herd immunity cannot be relied on to protect an individual child. All vaccines, in any child, should only be administered in a setting where there is access to appropriate equipment and expertise were an allergic reaction to occur. Although evidence is lacking regarding the significant danger of vaccinating eggallergic children, guidelines suggest, for extra precaution, selection only of those most at risk of life threathening hypersensitivity reactions. Extra precautions, including continuous observation for 20 minutes
Khristy Chang / 07120100107 after vaccination with further monitoring of cardiorespiratory
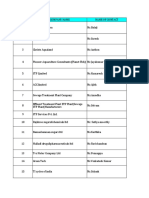
parameters to a total of 2 hours, are needed if: Or There is the presence of active, chronic asthma Theres a history of any cardiorespiratory symptoms or signs after egg ingestion
Conclusions
With good evidence that MMR vaccination is safe in egg- allergic children, excluding or delaying vaccination in these children cannot be justified and places the child at risk of developing a potentially serious infection. Guidelines exist to select those children most at risk of any form of life- threatening hypersensitivity reaction and provide them with extra precautions.
Anda mungkin juga menyukai
- Serological Markers of HBV InfectionDokumen8 halamanSerological Markers of HBV InfectioncristieristiieBelum ada peringkat
- Manual IV (DSM-IV) of The American Psychiatric AssociationDokumen24 halamanManual IV (DSM-IV) of The American Psychiatric AssociationcristieristiieBelum ada peringkat
- Neoclassical Paintings 1Dokumen4 halamanNeoclassical Paintings 1cristieristiieBelum ada peringkat
- Background: Alpha ThalassemiaDokumen24 halamanBackground: Alpha ThalassemiacristieristiieBelum ada peringkat
- Jurnal HipertensiDokumen17 halamanJurnal HipertensiWiny Ch'amhada TtarudaBelum ada peringkat
- In NeuroanatomyDokumen42 halamanIn NeuroanatomycristieristiieBelum ada peringkat
- Manual IV (DSM-IV) of The American Psychiatric AssociationDokumen24 halamanManual IV (DSM-IV) of The American Psychiatric AssociationcristieristiieBelum ada peringkat
- Insomnia PathophysiologyDokumen10 halamanInsomnia PathophysiologycristieristiieBelum ada peringkat
- What Are Extrapyramidal SymptomsDokumen2 halamanWhat Are Extrapyramidal SymptomscristieristiieBelum ada peringkat
- Insomnia PathophysiologyDokumen10 halamanInsomnia PathophysiologycristieristiieBelum ada peringkat
- Brain Stem Lesions: Midline Structures DeficitDokumen1 halamanBrain Stem Lesions: Midline Structures DeficitcristieristiieBelum ada peringkat
- Neurological Examination of The NewbornDokumen21 halamanNeurological Examination of The Newborncristieristiie100% (1)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Rtr-Internal Medicine: Case PresentationDokumen71 halamanRtr-Internal Medicine: Case PresentationJhon Carlo TegioBelum ada peringkat
- ANGIOSARCOMA pdf3 PDFDokumen9 halamanANGIOSARCOMA pdf3 PDFعبدالعزيز عماد محمودBelum ada peringkat
- Terminology For Implant Prostheses PDFDokumen5 halamanTerminology For Implant Prostheses PDFHugoMoralesTecnicoDentalBelum ada peringkat
- Zollinger-Ellison Syndrome (Gastrinoma)Dokumen15 halamanZollinger-Ellison Syndrome (Gastrinoma)Huy QuangBelum ada peringkat
- MSDS Baybl T65 901510Dokumen8 halamanMSDS Baybl T65 901510gnavarroBelum ada peringkat
- Recall GuidelinesDokumen31 halamanRecall GuidelinesSandy PiccoloBelum ada peringkat
- Gefico Maritime SectorDokumen28 halamanGefico Maritime SectorAugustine Dharmaraj100% (1)
- 16-23 July 2011Dokumen16 halaman16-23 July 2011pratidinBelum ada peringkat
- Human Factors and Safety Culture in Maritime Safety (Revised)Dokumen10 halamanHuman Factors and Safety Culture in Maritime Safety (Revised)Al-aayan D. IsmaelBelum ada peringkat
- School Form 2 (SF2) Daily Attendance Report of LearnersDokumen4 halamanSchool Form 2 (SF2) Daily Attendance Report of LearnersRyan A. CabalidaBelum ada peringkat
- Diffuse Large B-Cell Lymphoma: The History, Current View and New PerspectivesDokumen14 halamanDiffuse Large B-Cell Lymphoma: The History, Current View and New PerspectivesPepe PintoBelum ada peringkat
- Unani Therapeutic Index 28english29Dokumen24 halamanUnani Therapeutic Index 28english29Shahid BalochBelum ada peringkat
- Anaemia in Pregnancy: Dr. Lama MehaisenDokumen11 halamanAnaemia in Pregnancy: Dr. Lama MehaisenWendy EvansBelum ada peringkat
- CFPC SampsDokumen39 halamanCFPC SampsSumer Chauhan100% (9)
- SDS N 7330 NorwayDokumen15 halamanSDS N 7330 NorwaytimbulBelum ada peringkat
- Medical PalmistryDokumen5 halamanMedical PalmistryvivekpatelbiiBelum ada peringkat
- Dentistry Indonesia, 20 (1), 5-8.: Daftar PustakaDokumen6 halamanDentistry Indonesia, 20 (1), 5-8.: Daftar PustakaSari RahayuniBelum ada peringkat
- CFSS Monitoring Tool 2019Dokumen7 halamanCFSS Monitoring Tool 2019JULIE100% (10)
- Vieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMDokumen17 halamanVieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMFranciscoBelum ada peringkat
- Hazops Should Be Fun - The Stream-Based HazopDokumen77 halamanHazops Should Be Fun - The Stream-Based HazopHector Tejeda100% (1)
- Lepage Job WRKSHP 10-26-11Dokumen2 halamanLepage Job WRKSHP 10-26-11Andi ParkinsonBelum ada peringkat
- Analytical Customer UpdationDokumen16 halamanAnalytical Customer UpdationSathish SmartBelum ada peringkat
- 9401-Article Text-17650-1-10-20200718Dokumen5 halaman9401-Article Text-17650-1-10-20200718agail balanagBelum ada peringkat
- Daftar Obat Klinik MPHDokumen3 halamanDaftar Obat Klinik MPHxballzBelum ada peringkat
- Pollution of The WaterDokumen25 halamanPollution of The WaterJeprox Martinez100% (1)
- LlageriDokumen8 halamanLlageriBlodin ZylfiuBelum ada peringkat
- CLC - Good Copy Capstone ProposalDokumen6 halamanCLC - Good Copy Capstone Proposalapi-549337583Belum ada peringkat
- A Report - Noise Pollution in Urban AreasDokumen14 halamanA Report - Noise Pollution in Urban AreasArjita SinghBelum ada peringkat
- Citations Issued Due To COVID-19Dokumen726 halamanCitations Issued Due To COVID-19Maritza NunezBelum ada peringkat
- Nov 19 INTEGUMENTARY-INFLAMMATORY-DISORDERS-for-presentation-2022Dokumen79 halamanNov 19 INTEGUMENTARY-INFLAMMATORY-DISORDERS-for-presentation-2022Jean Gwyneth GatchalianBelum ada peringkat