Blood Transfusion
Diunggah oleh
Rebecca JolieDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Blood Transfusion
Diunggah oleh
Rebecca JolieHak Cipta:
Format Tersedia
BLOOD TRANSFUSION
Definition
Blood transfusion is the transfusion of whole blood or its components such as blood cells and plasma from one person (donor) to another person (recipient).
1. Most donated red blood cells can be stored for Forty-two days. 2. Most donated platelets can be stored for Five days 3. Frozen plasma can be stored for One year.
Selection of Donor:
Should not be suffering from disease of heart, kidneys, liver, lungs, cancer, jaundice, tuberculosis, hepatitis, AIDS, allergies etc. Should not have donated blood within the previous 90 days. Should be healthy and in the age group of 18-65 years. Should not be pregnant. Should have Hb level above 12 gm%. Should have normal vital signs. Should not be empty stomach.
Procedure
Preparation of the recipient * * * * Explain the procedure to the patient, blood product which is to be given, approximate length of time and desired outcome of the transfusion. Determine whether the patient has undergone prior transfusion and reactions, if any. Get an informed consent from the patient/relation. Prior to administration of blood, the patient`s vital signs should be recorded correctly on the nurse`s record to provide a base line for further observation. 1
* * *
Ask the patient to report chills, headaches, itching, or rash immediately so that prompt reporting and discontinuation of transfusion can help in minimizing reactions.
Provide a comfortable position.
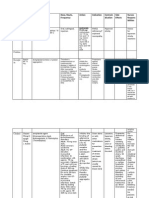
Preparation of articles: A tray containing
Articles
Rationale
A blood transfusion set. A mackintosh and towel. A tourniquet. Cotton swabs with antiseptic (iodine/ spirit) 18 gauge needle Adhesive tape and scissors Gloves A kidney tray, a paper bag IV stand Normal Saline. Blood or any of its components with cover received from the Blood Bank with the name of the recipient.
To transfuse blood. To protect the bed. To constrict the blood vessel To clean the site of infusion. To start IV line. To secure the tubings and needle. To prevent infection. To discard the waste. To hold the blood bottle. To start the blood transfusion line. To make sure that the blood sent from the Blood Bank is meant only for this particular patient. Avoid mistake in identification.
Performance of Procedure: Steps of Procedure Rationales
Check physician`s orders, patient`s condition, and history of Obtains specific data and initiates patient transfusion/ infusion reaction, reason for present transfusion etc. education if required. Identify patient. Check availability of blood with the blood bank. Explain the procedure to the patient, need for transfusion, blood product to be given, approximate length of time, desired outcome, etc. Emphasize the need for patient to report unusual symptoms immediately. Obtain informed consent from patient. Obtain blood from blood bank in accordance with agency policy. If transfusion cannot begin immediately, return product to blood bank. Blood which is out of refrigerator for more than 30 minutes, above degree centrigrade cannot above 10 degree centrigrade cannot be re-issued. Never store blood in unauthorized area-like ward refrigerator. Blood must be stored in refrigerator until at carefully controlled temperature. Encourage patient to empty bowel and bladder and assist to a comfortable position. Ensure privacy Faulty techniques in storing blood products can cause hemolysis. Provides reassurance and facilitates cooperation. Early identification of transfusion reactions aids in instituting prompt corrective measures. Prevents errors and thus eliminates possibility of transfusion reactions.
Ensures comfort of the patient. Urine specmen collected before transfusion if temperature is more than 101.8 degree farenhiet. Prevents cross infection.
Wash and dry hands. Check vital signs and record.
Reduces risk of infection. Obtains baseline data to compare with changes post transfusion. Delay transfusion if temperature is more than 101.8degree 3
Farenhiet. Reduces risk of infection.
If the patient has an IV infusion, check whether the needle and solution are appropriate to administer blood. The needle should be 18 gauge and the solution must be normal saline.
Large gauge needle permit infusion of whole blood. Normal saline prevents hemolysis.
Identify accessible veins. Select a large vein which allows the patient`s mobility. Open the sterile packing of the blood transfusion set aseptically. Insert the infusion set into the bag of blood to be transfused.
Prolonged restriction of arm movement is uncomfortable and inconvenient for the patient. Maintain sterility of the blood.
Check for any complications or allergic reactions.
Adjust rate to 2ml/mt for the first 15 minutes and remain with the patient. If any reaction is suspected, notify the blood bank and the physician. Monitor vital signs every five minutes for the first 15 minutes and every hour thereafter. Observe for flushing, itching, dyspnoea, or rash. Stop transfusion immediately, if any reaction is suspected.
Allows detection of reaction while infusing the smallest possible volume of the blood product. Any change in vital signs indicates an early sign of reaction.
After Care: Remove and dispose gloves, wash hands. Record administration of blood, date, time, blood group, any adverse reaction and the amount of blood infused. Reduces transmission of micro-organism. Documents administration of the blood components is necessary for accuracy in treatment and also for legal purposes.
Complications of Blood Transfusion: The complications can be broadly classified into two categories: * * Immune Complications Non-immune Complications
Immune Complications Immune complications can further be classified into two categories:
o o
Hemolytic (acute and delayed) Non-Hemolytic (includes febrile, urticarial, anaphylactic, purpura, etc.)
These are primarily due to the sensitization of the recipient to donor blood cells (either red or white), platelets or plasma proteins. Less commonly, the transfused cells or serum may mount an immune response against the recipient. The immune complications are easily classified into hemolytic and non-hemolytic reactions. Hemolytic reactions usually involve the destruction of transfused blood cells by the recipient's antibodies. Less commonly, the transfused antibodies can cause hemolysis of the recipient's blood cells. There are acute (also known as intravascular) hemolytic reactions and delayed (also known as extravascular) hemolytic reactions. Acute hemolytic reactions are usually due to ABO blood type incompatibility - in other words, human error plays a large part in these reactions. Blood given to the wrong patient has been attributed to physician error approximately 20% of the time, the operating room is the most common site of this error, and the anesthesiologist is the most commonly implicated physician. This type of reaction has been reported to occur approximately 1 in 25,000 transfusions - but it is often very severe and accounts for over 50% of reported deaths related to transfusion. The severity of the reaction often depends in the amount of blood given. Symptoms of acute hemolytic reactions include chills, fever, nausea, chest pain and flank pain in awake patients. In anesthetized patients, we should look for rise in temperature, unexplained tachycardia, hypotension, hemoglobinuria, oozing in the surgical field, DIC, shock and renal shutdown. Management of acute hemolytic reactions mandates that the transfusion be stopped immediately. The unit should be re-checked. Blood from the recipient patient should be drawn to test for hemoglobin in plasma, repeat compatibility testing and coagulation tests. A Foley catheter should be placed to check for hemoglobin in the urine. Osmotic diuresis with mannitol and fluids should be utilized (low-dose dopamine may help renal function and support blood pressure). With rapid blood loss, platelets and fresh frozen plasma may be indicated. Delayed hemolytic reactions are generally mild in comparison. These are caused by antibodies to non-D antigens of the Rh system or to foreign alleles in other systems such as the Kell, Duffy or Kidd antigens. Following a normal, compatible transfusion there is a 1-1.6% chance of developing antibodies to these foreign antibodies. This takes weeks or months to happen - and by that time, the original transfused cells have already been cleared. Re-exposure to the same foreign antigen can then cause an immune response. Thus the reaction is typically delayed from two to twenty-one days after transfusion. Symptoms are generally mild and include malaise, jaundice, fever, a fall in hematocrit despite transfusion, and an increase in unconjugated bilirubin. Diagnosis may be facilitated by the direct Coombs test which can detect the presence of antibodies on the membranes of red cells. Treatment is generally supportive. These reactions occur in approximately 1 in 2,500 transfusions and most often in females with previous exposure secondary to pregnancy. Non-Hemolytic reactions are due to sensitization of the recipient to donor white cells, platelets or plasma proteins. These reactions include:
o
Febrile 6
Anda mungkin juga menyukai
- WEEK 5: Pediatric Specimen CollectionDokumen129 halamanWEEK 5: Pediatric Specimen Collectiontibinj6767% (3)
- Surgical DressingDokumen2 halamanSurgical Dressinggao1989Belum ada peringkat
- Bone Marrow Aspiration and BiopsyDokumen7 halamanBone Marrow Aspiration and BiopsyPriyanjali SainiBelum ada peringkat
- AYUSH: Understanding India's Traditional Medicine SystemsDokumen93 halamanAYUSH: Understanding India's Traditional Medicine SystemsMamta RajputBelum ada peringkat
- Eye InstillationDokumen3 halamanEye Instillationshubham rathodBelum ada peringkat
- Nasogastric Tube Feeding GuideDokumen20 halamanNasogastric Tube Feeding GuideKrishna Sonu SoniBelum ada peringkat
- Gastric Lavage ProcedureDokumen2 halamanGastric Lavage Procedurejoel david knda mj75% (20)
- Colostomy Dressing ProcedureDokumen2 halamanColostomy Dressing Procedurejoel david knda mj100% (1)
- Procedure On Lumber PunctureDokumen8 halamanProcedure On Lumber PunctureDimpal ChoudharyBelum ada peringkat
- Demo Eye IrrigationDokumen5 halamanDemo Eye IrrigationSachin Dwivedi100% (4)
- Administration of Topical MedicationsDokumen14 halamanAdministration of Topical MedicationsgireeshsachinBelum ada peringkat
- Thoracocentasis: INTRODUCTION:-Thoracentasis Also Known As The Thoracocentasis or Plural Tap Is AnDokumen7 halamanThoracocentasis: INTRODUCTION:-Thoracentasis Also Known As The Thoracocentasis or Plural Tap Is AnaparnaBelum ada peringkat
- Colostomy Care Procedure StepsDokumen5 halamanColostomy Care Procedure StepsEsmareldah Henry SirueBelum ada peringkat
- Hb TEST FILTER PAPERDokumen4 halamanHb TEST FILTER PAPERSujatha J Jayabal100% (1)
- Abdominal ParacentesisDokumen5 halamanAbdominal ParacentesisSivaprasad S100% (1)
- NGT LavageDokumen16 halamanNGT LavageTina Alteran100% (1)
- Performing Urine Analysis: Nursing Action RationaleDokumen2 halamanPerforming Urine Analysis: Nursing Action RationaleRaja Kumar0% (1)
- Naso Gastric Tube FeedingDokumen14 halamanNaso Gastric Tube FeedingSathya100% (2)
- Promoting Effective Breathing and Airway ClearanceDokumen7 halamanPromoting Effective Breathing and Airway ClearanceJinaan MahmudBelum ada peringkat
- Urine & Stool Collection GuideDokumen21 halamanUrine & Stool Collection GuideOem Boed ColectionBelum ada peringkat
- Blood TransfusionDokumen63 halamanBlood TransfusionMary Joy F. Ching100% (3)
- TSU Nursing Performance Evaluation ChecklistDokumen7 halamanTSU Nursing Performance Evaluation ChecklistKatKat Bognot100% (2)
- Bowel Wash: Child Health Nursing ProcedureDokumen4 halamanBowel Wash: Child Health Nursing ProcedureEllen Angel100% (1)
- St. Francis College Nursing ChecklistDokumen7 halamanSt. Francis College Nursing ChecklistSharon LawrenceBelum ada peringkat
- Lumber Puncture ProcedureDokumen8 halamanLumber Puncture ProcedureDimpal ChoudharyBelum ada peringkat
- How Pulse Oximetry WorksDokumen16 halamanHow Pulse Oximetry WorksValarmathi100% (6)
- URINALYSIS (Test For Albumin and Sugar in The Urine)Dokumen3 halamanURINALYSIS (Test For Albumin and Sugar in The Urine)Geno Adrian T Pampanga100% (1)
- Eye Irrigation DemoDokumen5 halamanEye Irrigation DemoBabita DhruwBelum ada peringkat
- Grastric Gavage & LavageDokumen17 halamanGrastric Gavage & LavageJuliet Pua74% (19)
- Application of SplintsDokumen8 halamanApplication of SplintsMary Rose Enar100% (1)
- Procedure Steam Inhalation.Dokumen10 halamanProcedure Steam Inhalation.PINKI DEBBelum ada peringkat
- RestraintsDokumen47 halamanRestraintsSAYMABANU100% (1)
- Applying An Icecap or Ice CollarDokumen1 halamanApplying An Icecap or Ice CollarAparna KinginiBelum ada peringkat
- Capillary Blood Glucose Monitoring (CBG)Dokumen23 halamanCapillary Blood Glucose Monitoring (CBG)Jaylord Verazon0% (1)
- Gastric LavageDokumen19 halamanGastric LavageAnita Santiago Soguilon100% (1)
- SuctionDokumen15 halamanSuctionMissy Shona100% (1)
- Suctioning Techniques and ProceduresDokumen18 halamanSuctioning Techniques and Proceduresjothi100% (1)
- Nasogastric Feeding or Gavage FeedingDokumen47 halamanNasogastric Feeding or Gavage FeedingDr. Jayesh Patidar100% (1)
- Endotracheal Suctioning PDFDokumen4 halamanEndotracheal Suctioning PDFDebipriya MistryBelum ada peringkat
- MSN II 01.7.2020-OSCE in Instillation of Ear DropsDokumen3 halamanMSN II 01.7.2020-OSCE in Instillation of Ear DropsYAMINIPRIYANBelum ada peringkat
- Tepid-Sponging Check ListDokumen1 halamanTepid-Sponging Check ListSumi100% (2)
- Time Specific Objective Content Teachin G Learning Activity Av Aids EvaluationDokumen7 halamanTime Specific Objective Content Teachin G Learning Activity Av Aids Evaluationrittika dasBelum ada peringkat
- Bone Marrow Aspiration GuideDokumen7 halamanBone Marrow Aspiration GuideTHAMAYANTHY A/P RAMAN STUDENTBelum ada peringkat
- Community Health Bag Nursing ProceduresDokumen10 halamanCommunity Health Bag Nursing Proceduresmariet abraham100% (1)
- Endotracheal IntubationDokumen7 halamanEndotracheal Intubationsimonjosan67% (3)
- Care unconscious clientsDokumen27 halamanCare unconscious clientsDonelie Kay Tapel AsanzaBelum ada peringkat
- Wound Dressing ProcedureDokumen2 halamanWound Dressing ProcedureCaptainMarksmanBelum ada peringkat
- Oxygen AdministrationDokumen6 halamanOxygen AdministrationAsma SaleemBelum ada peringkat
- Bowel Wash.Dokumen12 halamanBowel Wash.Sathya75% (4)
- Performance Checklist Catheter Care NOT Done 1 3 3 3 3 3 3 3 4Dokumen1 halamanPerformance Checklist Catheter Care NOT Done 1 3 3 3 3 3 3 3 4Mhel MG0% (1)
- Procedure for Staple and Suture RemovalDokumen15 halamanProcedure for Staple and Suture RemovalRajaBelum ada peringkat
- Types and Collection of Urine SpecimenDokumen12 halamanTypes and Collection of Urine SpecimengireeshsachinBelum ada peringkat
- Procedure in Blood TransfusionDokumen7 halamanProcedure in Blood Transfusionevangelo22656100% (1)
- Removing Secretions from the AirwayDokumen5 halamanRemoving Secretions from the AirwayNina Buenaventura100% (1)
- HemodialysisDokumen2 halamanHemodialysisJanelle MarceraBelum ada peringkat
- Intravenous Injection: Presented by Mrs. Silpa Jose T Assistant Professor STCON, KattanamDokumen33 halamanIntravenous Injection: Presented by Mrs. Silpa Jose T Assistant Professor STCON, KattanamSilpa Jose TBelum ada peringkat
- Exchange TransfusionDokumen21 halamanExchange TransfusionJOSLIN100% (2)
- Blood Transfusion CONTENTDokumen7 halamanBlood Transfusion CONTENTDr-Sanjay SinghaniaBelum ada peringkat
- Revalida 1Dokumen3 halamanRevalida 1herrabiel solisBelum ada peringkat
- Blood Transfusion ProceduresDokumen5 halamanBlood Transfusion ProceduresAngie Doctolero100% (1)
- Genetic BiniDokumen13 halamanGenetic BiniRebecca JolieBelum ada peringkat
- Clotting Factor Lesson Plan Recovered)Dokumen5 halamanClotting Factor Lesson Plan Recovered)Rebecca Jolie100% (1)
- Down SyndromeDokumen4 halamanDown SyndromeRebecca JolieBelum ada peringkat
- DrugsDokumen10 halamanDrugsRebecca JolieBelum ada peringkat
- Development of EmbryoDokumen11 halamanDevelopment of EmbryoRebecca JolieBelum ada peringkat
- Lady With The LampDokumen15 halamanLady With The LampRebecca JolieBelum ada peringkat
- Adult Transfusion GuidelinesDokumen18 halamanAdult Transfusion GuidelinesConnor ScanlonBelum ada peringkat
- BurnsDokumen44 halamanBurnsJANARTHANAN VBelum ada peringkat
- C72IA025EN-B Viscosity of Whole BloodDokumen3 halamanC72IA025EN-B Viscosity of Whole BloodMartín PerezBelum ada peringkat
- BIOLABO - Applications Humastar 180Dokumen32 halamanBIOLABO - Applications Humastar 180Nguyễn Bảo Huân100% (1)
- Organizational Study of Terumo PenpolDokumen57 halamanOrganizational Study of Terumo Penpolവിനോദ്കുമാർ ജ്ഞാനോദയപുരംBelum ada peringkat
- Plasbumin 25 enDokumen19 halamanPlasbumin 25 enlenaBelum ada peringkat
- Widal TestDokumen11 halamanWidal TestlialestariBelum ada peringkat
- CA-270 Service ManualDokumen499 halamanCA-270 Service ManualLambertGuevarraBelum ada peringkat
- Pretransfusion or Compatibility Testing: NotesDokumen7 halamanPretransfusion or Compatibility Testing: NotesABHINABA GUPTABelum ada peringkat
- Transport System Overcomes Diffusion LimitationsDokumen27 halamanTransport System Overcomes Diffusion Limitationsdania0% (1)
- The Immune System British English StudentDokumen6 halamanThe Immune System British English StudentIzabela WiśniewskaBelum ada peringkat
- TotalBhCG ARCDokumen7 halamanTotalBhCG ARCLau GómezBelum ada peringkat
- New w7 Cholesterol, Triglyceride Determination, HDL CholesterolDokumen118 halamanNew w7 Cholesterol, Triglyceride Determination, HDL Cholesterollily beautyBelum ada peringkat
- Adv Materials Inter - 2023 - Saifullah - Sampling Dermal Interstitial Fluid Using Microneedles A Review of RecentDokumen23 halamanAdv Materials Inter - 2023 - Saifullah - Sampling Dermal Interstitial Fluid Using Microneedles A Review of RecentAndisheh ChoupaniBelum ada peringkat
- RCS PreparationDokumen3 halamanRCS PreparationMaria Charlene OrpillaBelum ada peringkat
- Etika Penelitian Pada ManusiaDokumen32 halamanEtika Penelitian Pada ManusiaAhmad NazharBelum ada peringkat
- Attributes of blood donors in SubicDokumen61 halamanAttributes of blood donors in SubicMaxsus SmithBelum ada peringkat
- Plasma Refilling in HemodialysDokumen4 halamanPlasma Refilling in Hemodialysahmed AlayoudBelum ada peringkat
- Laboratory Instrumentation GuideDokumen4 halamanLaboratory Instrumentation GuideKry VillanuevaBelum ada peringkat
- Albumin (Human) 20%: Presentation ClassificationDokumen3 halamanAlbumin (Human) 20%: Presentation ClassificationZamzam DomaBelum ada peringkat
- 3rd All Surgery Question FileDokumen136 halaman3rd All Surgery Question FileСымбат КулдасоваBelum ada peringkat
- Phlebotomy - Lab Draws Final 09.17.2015Dokumen8 halamanPhlebotomy - Lab Draws Final 09.17.2015ashanti wrightBelum ada peringkat
- Comprehensive Lab Test Price List for Haematology, Biochemistry, Serology, Microbiology and Hormone AssaysDokumen4 halamanComprehensive Lab Test Price List for Haematology, Biochemistry, Serology, Microbiology and Hormone AssaysSUMA MANOJBelum ada peringkat
- DIALAB ProductRange 2017 Rev01 v2 2017 02 21Dokumen40 halamanDIALAB ProductRange 2017 Rev01 v2 2017 02 21Khaled0% (1)
- MAGLUMI Vitamin B12 (CLIA) Test KitDokumen4 halamanMAGLUMI Vitamin B12 (CLIA) Test KitMohamed BoulkadidBelum ada peringkat
- Bovine Serum Albumin 22%Dokumen1 halamanBovine Serum Albumin 22%Sameeh MohBelum ada peringkat
- Cholesterol ARC CHEMDokumen8 halamanCholesterol ARC CHEMSalah AnamBelum ada peringkat
- Virology User ManualDokumen24 halamanVirology User ManualMedo2012Belum ada peringkat
- Manual Coleta Greiner Bio-OneDokumen37 halamanManual Coleta Greiner Bio-OneHelton Resende SilvaBelum ada peringkat
- Nursing Glossary TermsDokumen13 halamanNursing Glossary Termsgab77Belum ada peringkat