Local Anaesthetic Agents
Diunggah oleh
anaeshklDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Local Anaesthetic Agents
Diunggah oleh
anaeshklHak Cipta:
Format Tersedia
Local Anaesthetic Agents
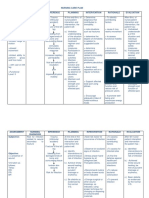
Definition drugs that reversibly block impulse conduction along nerve axons and other excitable membranes that utilise sodium channels as the primary means of action potential generation Ideal local anaesthetic agent
NC Hwang 2008
Structure
Amide-linked agents
Structure activity Amino group primary amines have low activity, and cause irritation secondary amines have good activity but cause irritation tertiary amines have good activity quaternary amines have activity, but poor penetration of tissues size of nitrogen substitution branching and increasing the number of carbons, up to 3-4 carbons, increases the potency (and toxicity), after this, the activity drops off, since the analogues are too lipid soluble usually the N-substituent is methyl, ethyl or propyl, or is included in a ring structure such as a piperidine addition of polar substituents such as a hydroxyl, will greatly diminish activity substitution of the N-methyl with butyl chain increased lipid solubility protein binding potency duration of action Intermediate chain branching, especially at the -carbon of ester local anaesthetic agents, increases duration of action this effect is not seen in the amide local anaesthetic agents increasing the chain length will increase potency but beyond a critical length will also increase toxicity
Ester-linked agents
Aromatic ring adding a second substituent to the aromatic ring increases activity (e.g. procaine vs. propoxycaine), activity increases up to 3-4 carbons, then drops off activity of simple esters of benzoic acid, such as benzocaine, increases as branched or straight chain alkylamino groups are added Potency increased by increasing lipid solubility presence of tertiary amine branching and lengthening the two terminal groups on the tertiary amine domain addition of a butyl group to mepivacaine results in bupivacaine lengthening intermediate alkyl chain of ester agents, but beyond a critical length, toxicity increases positioning carbonyl group of ester next to aromatic ring adding branched or straight chain alkylamino group to aromatic ring of ester agents
Chirality
Local Anaesthetic Agents
Local anaesthetic receptor site
NC Hwang 2008
Local anaesthetic-receptor interaction in fully polarised membrane (resting), channel is closed with voltage activation (activated), voltage-gated sodium channel opens allowing influx of Na+ a millisecond later, channel closes (inactivated), preventing further Na+ entry
Onset of action after administration diffusion into nerve fibres major determinants site of administration drug pKa lipid solubility pathophysiological factors inflammation pKa acid dissociation constant, pKa, (and interaction with pH at site of injection) pKa indicates the pH at which the ionized and unionized (non-ionized) forms are equal local anaesthetics are weak bases pKa of most local anaesthetics are in the range of 8.09.0 at pH 7.4, about 5 to 20% will be in the unionised form local anaesthetic receptor is not accessible from the external side of the cell membrane and the unionized form is important for rapid penetration of cell membrane but once the local anaesthetic has diffused into the nerve trunk the ionized form binds to the Na+ channel the percentage of a specific local anaesthetic agent which is present in the base form when injected into tissue whose pH is 7.4 is inversely proportional to the pKa of that agent local anaesthetic agents with pKa closer to pH 7.4 will have a more rapid onset of action and agents with high pKa have a slow onset of action: onset 1/pKa large portion of agent with high pKa will be in ionic (cationic) form acidification local anaesthetics in the form of the unionized amine and tend to be only slightly water soluble usually formulated as hypochloride salts to form acidic solution, which are soluble and stable in water alkalination addition of NaHCO3 (1 meq/10 ml lidocaine, 0.1 meq/10 ml bupivicaine) will increase the pH of the local anesthetic, increasing the diffusion of the local anesthetic into the cell and, therefore, decrease the time of onset of the block but, the pH of any injected solution is rapidly brought to physiological pH the addition of bicarbonate does not have an effect on the "depth" or duration of the block carbonation use of carbonated local anaesthetic solutions CO2 readily diffuses into the nerve, raising the [H+] by dissociation and increasing the proportion of intracellular ionized species
Mechanism of action with increasing concentrations of local anaesthetic agent applied to the nerve fibre threshold for excitation increases impulse conduction slows the rate of the rise of the action potential declines the action potential amplitude decreases the ability to generate an action potential is abolished if sodium current is blocked over a critical length of the nerve, propagation across the blocked area is no longer possible blockade of sodium channel by local anaesthetics is both voltage- and time-dependent the effect of local anaesthetic at a given concentration is more marked in rapidly firing axons than in resting fibres, (frequencydependent block) channels in the rested state (more negative transmembrane potentials) have less affinity for local anaesthetics than activated (open) state and inactivated channels (more positive transmembrane potentials) except for benzocaine which blocks the resting channel alterations in transmembrane potentials elevated extracellular calcium partially antagonises the action of local anaesthetics reversal caused by calcium-induced increase of the surface potential on the membrane, which favours the low-affinity rested state increase in extracellular potassium depolarises the membrane potential and favours the inactivated state, enhancing the effect of local anaesthetics
Local Anaesthetic Agents
lipid solubility more lipid soluble, the higher the potency lipid solubility expressed as the partition coefficient the smaller and more lipophilic the molecule the faster the rate of interaction with the sodium channel receptor increasing the side chains increases lipid solubility, however it also increases toxicity and irritant effects the agent should retain sufficient water solubility to diffuse to the site of action bupivacaine, etidocaine, tetracaine less water soluble than lignocaine, mepivacaine, procaine more potent with longer duration of action differential blockade critical lengths of axons distance over which nerve fibres can passively propagate an electrical impulse small B and C fibres have shorter critical lengths and are more susceptible to blockade frequency dependence degree of block produced at a given concentration of local anaesthetic agent is markedly dependent upon the recent frequency of nerve stimulation or use resting nerve is far less sensitive due to the requirement for the inner gates of the sodium channel to be open for the local anaesthetic to gain access to the binding site small diameter C and A pain fibres that participate in high frequency pain transmission, are blocked earlier and sooner with low concentrations of local anaesthetic than are the A fibres nerve fibre size small diameter, easily blocked myelination for nerves of the same diameter, myelinated fibres tend to be blocked before unmyelinated nerves channel density being greatest at the nodes of Ranvier, where they may comprise up to 15% of the membrane surface but as 3 successive nodes must be blocked by the local anaesthetic to halt impulse propagation, the thicker the nerve fibre, the further apart the nodes tend to be, hence greater resistance to block large fibres arrangement of fibres bundles in nerve sheath circumferential nerves blocked sooner in large nerve trunks, motor nerves are usually located circumferentially, and are exposed to the drug first when it is deposited into the tissue surrounding the nerve motor nerve block occurs before sensory block in large mixed nerves
NC Hwang 2008
in extremities, proximal sensory fibres are located in the mantle of the nerve trunk, and distal sensory fibres are in the core of the nerve analgesia first develops proximally and then spreads distally as the drug penetrates the core of the nerve Duration of action main determinants lipid solubility protein binding blood flow at site and effect of vasoconstriction dosage: molecular load, plasma : tissue concentration gradient lipid solubility and protein binding longer acting amide local anaesthetic agents have high lipid solubility and are extensively protein bound lipid solubility and protein binding increased by branching and increasing the terminal groups at the tertiary amine (bupivacaine compared with mepivacaine) or at the -carbon of ester local anaesthetic agents having electron donating groups (alkoxy, alkyl, amino, alkylamino) on the aromatic ring, since they stabilize the ester or amide group vasoconstriction addition of vasoconstrictor delays absorption from the active site decreases the peak serum concentration and toxic effect and allows metabolism to keep pace with absorption greatly intensifies and prolongs the duration of action less influence on the uptake and anaesthetic duration of the longer-acting agents preparations with vasoconstrictors usually contain adrenaline 1:200,000, or noradrenaline 1:100,000 agents with vasoconstriction activity cocaine, bupivacaine constricts blood vessels systemic absorption after regional blockade major determinant of systemic absorption site of administration blood flow and effect of vasoconstriction tissue binding the blood : tissue partition coefficient plasma : tissue concentration gradient absorption from various areas (fastest to slowest) intravenous mucous membrane intercostal block caudal block epidural block brachial plexus block peripheral nerve block subcutaneous infiltration systemic absorption after epidural administration biphasic faster with shorter-acting agent adrenaline has less effect on longer-acting agent
Local Anaesthetic Agents
NC Hwang 2008
plasma concentration of 1-acid glycoprotein increased in cancers, trauma, AMI, uraemia, smoking binding of basic drugs increased decreased in neonate, pregnancy the reduced binding of lignocaine in the neonate is due, in part, to lower levels of this protein uptake by the lung reduces distribution of the amidelinked local anaesthetics volume of distribution higher Vd reduces clearance and increases t cardiac failure Elderly Clearance of amide-linked local anaesthetic agents depends on hepatic metabolism which is dependent upon liver blood flow diseases where liver blood flow is reduced, the clearance of amide-linked agent is reduced and serum concentrations will be higher congestive heart failure, hypovolaemia generally degraded in the hepatic endoplasmic reticulum by N-dealkylation, followed by hydrolysis renal excretion accounts for only 1-5% of the administered dose Metabolism of amide-linked local anaesthetic agents lignocaine is a high extraction ratio drug, with high "first pass metabolism and poor bioavailability (<35%) lignocaine glycinexylide (MEGX and GX) and hydroxyxylidine MEGX and GX are pharmacologically active, t: MEGX 2 h, GX 10 h an exception is prilocaine, where the initial step is hydrolysis, forming o-toluidine, which is further metabolised to 4- and 6-hydroxytoluidine, the latter is responsible for methaemoglobinaemia which follows high doses
Predicated local and systemic accumulation during multiple extradural injection regimes for lignocaine and etidocaine
Systemic distribution kinetics major determinants of distribution are the physicochemical properties of the local anaesthetic pKa protein binding lipid solubility regional blood flow acid-base balance protein binding amides are extensively protein bound, between 55-95% being basic drugs, the principal plasma binding protein is 1-acid glycoprotein
Clearance of ester-linked local anaesthetic agents by ester hydrolysis (plasma cholinesterase and liver esterases) spinal fluid contains little or no esterase intrathecal administration produces a prolonged effect, which persists until the agent is absorbed into the blood stream
Local Anaesthetic Agents
clearance decreased and drug activity prolonged in neonates atypical plasma cholinesterase homozygotes presence of liver and renal disease presence of drug interactions presence of anticholinesterases Metabolism of ester-linked local anaesthetic agents plasma cholinesterase activity in the newborn is only 50%, reaching adult values after 1 year benzocaine hydrolysed to para-aminobenzoic acid procaine hydrolysed to para-aminobenzoic acid, diethylaminoethanol in vitro half-life is 39-43 seconds chloroprocaine hydrolysed to 2-chloro-paraaminobenzoic acid (CABA), diethylaminoethanol in vitro half-life is approximately 20 seconds tetracaine hydrolysed to N-butyl-p-aminobenzoic acid (BABA), diethylaminoethanol Properties
NC Hwang 2008
anaesthetic index of > 1.0 means the anaesthetic potency is greater than the relative toxicity Central nervous system effects earliest signs of toxicity circumoral and tongue numbness, tinnitus, nystagmus, and dizziness central nervous system excitation with increasing plasma concentrations depression of cortical inhibitory pathways, thereby allowing the unopposed activity of excitatory components, leading to restlessness, tremor, and eventually tonic-clonic convulsions central nervous system stimulation is then followed by depression with increasing plasma concentrations death is usually due to respiratory depression
Local anaesthetic toxicity systemic toxicity (unintended) central and peripheral nervous systems cardiovascular system direct myocardial effects peripheral vascular effects local tissue toxicity allergic reactions miscellaneous effects membrane stabilization neuromuscular junction, anticholinergic autonomic ganglia methaemoglobinaemia toxic effects are frequently determined by relative rates of absorption and metabolism tissue binding removes the agent from the circulation and reduces toxicity e.g. Bier block, about of the administered dose is still bound to the peripheral tissues 30 minutes after removal of the tourniquet toxicity can be assessed by two parameters
factors influencing development of toxicity relative potency rate of intravenous administration rate at which a particular blood concentration is achieved hypercarbia and acidosis, both decrease convulsive threshold management of seizures hyperventilation prevents hypercarbia and acidosis results in alkalosis lowers extracellular potassium, which will favour the rested state or lowaffinity state of sodium channels, resulting in decreased local anaesthetic toxicity suppression of seizures intravenous thiopentone 1-2mg/kg or diazepam 0.1mg/kg secure airway by tracheal intubation if necessary
Local Anaesthetic Agents
Peripheral nervous system effects when applied at excessively high concentration all local anaesthetics agents with low pH can be toxic to nerve tissue prolonged sensory and motor deficits following spinal analgesia with large volumes of chloroprocaine (metabisulphite) pooling of high concentrations of heavy lignocaine in cauda equina (high osmolarity of 5% glucose) Cardiovascular system effects all local anaesthetic exerts a dose-dependent negative inotropic effect more potent agents such as bupivacaine, appear to depress myocardial contraction at lower doses and concentrations than less potent agents, such as lignocaine pregnant patients may be more susceptible to toxic effects mechanism of action all agents depress the maximal rate of increase of the cardiac action potential or Vmax (the maximum upstroke velocity of the action potential), slow phase 1 conduction, increase refractory period, prolongation of the PR and QRS interval on ECG myocardial depression and vasodilatation leading to hypotension (except cocaine) Bupivacaine cardiotoxicity of bupivacaine results from its high lipid solubility R(+)enantiomer is more toxic than the S()enantiomer LD50 less for R(+) bupivacaine minor cardiovascular toxicity occurred at lower dosage and lower plasma concentration with bupivacaine compared with ropivacaine bupivacaine and sodium channel blockade bupivacaine binds to inactivated channels and dissociates slowly from them during diastole, fast-in-slow-out pharmacodynamics characteristics at sodium receptor; while lignocaine binds to both activated and inactivated channels and dissociates rapidly Kdbupivacaine 2s; Kdlignocaine 0.2s bupivacaine has considerably greater cardiac depressant effect than is suggested by its relative potency at sodium channels compared to lignocaine EC50 for inactivated state of channel 39% lower for R(+) bupivacaine persistence of block causes AV block, prolongation of PR intervals, slow idioventricular rhythm, broad QRS complexes, electromechanical dissociation and re-entrant arrhythmias bupivacaine exhibits lower Cardiovascular Collapse Dose : Convulsive Dose ratio than lignocaine causes nodal and ventricular arrhythmias and wide QRS complexes at plasma concentrations associated with central nervous system toxicities, while lignocaine does not
NC Hwang 2008
Cardiovascular Collapse Dose : Convulsive Dose ratio
bupivacaine and potassium channel blockade resulting in prolonged QTc intervals noted, a feature of cardiotoxicity of bupivacaine KdR(+)bupivacaine 27.3mM, KdS(+)bupivacaine 4.1mM direct action on medulla can produce malignant ventricular arrhythmias Management of cardiovascular toxicity resuscitation ABC can be successful with standard cardiopulmonary support prompt correction of acidosis by hyperventilation and administration of bicarbonate aggressive administration of adrenaline, atropine, and bretylium local anaesthetics inhibit basal and adrenalinestimulated cAMP production bretylium to raise threshold for ventricular fibrillation Ropivacaine amide local anaesthetic, only available in S-stereoisomer has less affinity for cardiac sodium channel less intense motor block than bupivacaine lower cardiovascular toxicity than bupivacaine minor symptoms of toxicity with accidental intravenous injection of ropivacaine, but no adverse cardiac effects Cocaine blocks noradrenaline, dopamine, and serotonin reuptake vasoconstriction hypertension, ischaemia, and ulceration of mucous membranes can precipitate arrhythmias Methaemoglobinaemia administration of large doses (>10mg/kg) of prilocaine for regional anaesthesia may lead to accumulation of the metabolite o-toluidine, an oxidising agent capable of converting haemoglobin to methaemoglobin with more than 3-5mg/dl of methaemoglobin, the patient will appear cyanotic, and the blood chocolate-coloured treatment: intravenous of reducing agent such as methylene blue 1-2mg/kg or ascorbic acid, to rapidly convert methaemoglobin to haemoglobin
Local Anaesthetic Agents
Allergic reactions p-aminobenzoic acid ester type local anaesthetics are metabolised to p-aminobenzoic acid derivatives which may provoke an allergic reaction in small percentage of population PABA was a common ingredient in topical sunscreens amide type of local anaesthetics are not metabolised to p-aminobenzoic acid, and allergic reactions to this group is rare additives lowering pH to increase ionisation hydrochloride metabisulphite metabisulphite in 2chloroprocaine generate sulphur dioxide (lipid soluble) which can diffuse into neural tissue and generate intracellular sulphurous acid, causing profound local acidosis and neurotoxicity vasoconstriction to prolong nerve block adrenaline antimicrobial for multi-dose vial methyl hydroxybenzoate increase baricity 5% dextrose Tachyphylaxis as local anaesthetic agents available as hydrochloride (HCl), with more local anaesthetic being administered into the epidural space, the tissue pH decreases more of the agent remains in the ionised form in the epidural space, preventing diffusion of the drug across the nerve membrane Individual local anaesthetic agent Cocaine ester-linked local anaesthetic agent an alkaloid obtained from leaves of Erythroxylon coca (coca tree) pKa 8.7, 91% protein binding onset of action - pKa, pH, lipid solubility medium duration of action mechanism of action: unionised form for passage through cell membrane; ionised form for Na+ channel blockade blocks uptake of noradrenaline vasoconstriction hypertension ischaemia and ulceration of mucous membranes can precipitate arrhythmias mydriasis blocks uptake of dopamine and serotonin
NC Hwang 2008
with chronic use, interferes with the cytosolic calcium increase that normally occurs during systole; this could explain its negative inotropic effect metabolism benzoylecgonine and ecgonine methyl ester are the major hydrolytic metabolites formed by hepatic and plasma esterases, both are pharmacologically inactive, not hepatotoxic and are often used for forensic purposes both are further hydrolyzed to ecgonine cocaine is demethylated to an active metabolite, norcocaine, by cytochrome P450 enzyme systems; and is then hydrolyzed to benzoylnorecgonine cocaine and norcocaine are hepatotoxic
clearance decreased and drug activity prolonged in neonates atypical plasma cholinesterase homozygotes presence of liver and renal disease presence of drug interactions presence of anticholinesterases maximum dose 2mg/kg, with or without epinephrine at low dose produces a feeling of well-being and euphoria causes central vagal stimulation resulting in bradycardia blocks uptake of noradrenaline resulting in vasoconstriction and mydriasis higher dose stimulates vomiting centre causes central and peripheral sympathetic stimulation resulting in tachycardia increasing capacity for muscular work eventually causes convulsion, coma, medullary depression, respiratory depression and myocardial depression, ventricular fibrillation and death
Local Anaesthetic Agents
Chloroprocaine ester-linked local anaesthetic agent halogenated derivative of procaine pKa 8.9, onset in 6-12 minutes maximum dose 10mg/kg, with epinephrine 15 mg/kg mechanism of action: unionised form for passage through cell membrane; ionised form for Na+ channel blockade rapidly cleared in plasma and liver by plasma cholinesterase, at 4.7 mol/ml/h, resulting in shortest duration of action, 30-60 minutes hydrolysed to 2-chloro-para-aminobenzoic acid (CABA), diethylaminoethanol toxicity p-aminobenzoic acid derivatives which may provoke an allergic reaction in small percentage of population local neurotoxicity due to preservative, sodium bisulphite metabisulphite in 2-chloroprocaine generated sulphur dioxide (lipid soluble) which diffused into neural tissue and generated intracellular sulphurous acid, profound local acidosis and, thus, neurotoxicity Prilocaine amide-linked local anaesthetic agent potency less than lignocaine pKa 7.9, 3x the potency of procaine (1), medium duration of action 55% protein binding, majority to plasma 1-acid glycoprotein increased in cancers, trauma, AMI, uraemia, smoking binding of basic drugs increased decreased in neonate, pregnancy uptake by the lung reduces distribution of the amidelinked local anaesthetics most rapidly cleared hydrolysed to form o-toluidine, which is further metabolised to 4-OH and 6-OH-toluidine lung clearance as well mechanism of action: unionised form for passage through cell membrane; ionised form for Na+ channel blockade maximum dose 5mg/kg, with epinephrine 7.5 mg/kg > 10mg/kg may lead to accumulation of the metabolite o-toluidine and 6OH-toluidine, which convert haemoglobin to methaemoglobin symptoms of hypoxaemia with > 16mg/kg with > 3-5mg/dl of methaemoglobin, the patient will appear cyanotic, and the blood chocolate-coloured treatment intravenous administering of either reducing agent such as methylene blue 1-2mg/kg or ascorbic acid to rapidly convert methaemoglobin to haemoglobin
NC Hwang 2008
Lignocaine amide-linked local anaesthetic agent pKa 7.9, 4x potency of procaine (1), medium duration of action 60-80% protein binding, majority to plasma 1-acid glycoprotein maximum dose 3mg/kg, with epinephrine 7 mg/kg rapid onset Vd 0.6-1L/kg larger in neonates, and decreased in elderly increased in oedema, ascites, pleural effusion, renal disease metabolised to monoethylglycine-xylide and glycine xylide both of these agents are pharmacologically active and their respective t are, 2 hours for MEGX, 10 hours for GX formulated as hypochloride salts to form acidic solution, which are soluble and stable in water Bupivacaine amide-linked local anaesthetic agent, available as racemic mixture, R(+) and S(-) enantiomers pKa 8.1, 16x potency of procaine (1) 90-97% protein binding (1-acid glycoprotein) competes with muscle relaxants and is known to prolong the action of pancuronium and suxamethonium Vd 0.9 L/kg, VDss 73L distributed into breast milk in small quantities crosses the placenta but the ratio of fetal concentrations to maternal concentrations is relatively low also diffuses into the cerebrospinal fluid metabolised in the liver to 3-OH bupivacaine, 4-OH bupivacaine, and 2,6-pipecoloxilidine clearance is 7 ml/min/kg, t 2.4 hours, longer in neonates 2% excreted unchanged in urine degradation into PPX is mediated by CYP3A order of loss of function is as follows: pain, temperature, touch, proprioception, and skeletal muscle tone toxic blood concentrations may depress cardiac conduction, excitability, and cause cardiac arrest maximum dose with or without epinephrine 2mg/kg used for infiltration anaesthesia, epidural and spinal anaesthesia, nerve block popular drug for providing prolonged analgesia during labour and the postoperative period long duration of action tendency to provide more sensory than motor block
Local Anaesthetic Agents
R (+) bupivacaine shows marked stereoselectivity for inactivated state of the sodium channel binds 3x more firmly to sodium channel and unbinds 4.4x as slowly (39% lower EC50, AV conduction time 50% longer, significantly lower LD50, recovers slower from block (981 ms vs 560 ms) greater cardiotoxicity, toxicity induced is more difficult to reverse has 7-fold more potent in blocking potassium channel, prolongation of cardiac action potential, and pro-arrhythmogenic binds 3x more firmly to sodium channel and unbinds 4.4x as slowly (39% lower EC50, AV conduction time 50% longer, significantly lower LD50, recovers slower from block (981 ms vs 560 ms) toxicity induced is more difficult to reverse S (-) bupivacaine produces vasoconstriction, provides longer duration of action after skin infiltration has reduced sodium channel blockade has lesser reduction in Vmax (in vitro- studies) faster unblocking of sodium channels higher arrhythmogenic dose higher convulsive dose has markedly reduced potassium channel blockade equivalent efficacy for analgesia Ropivacaine amide-linked local anaesthetic agent, available as a single enantiomer S-N-n-propyl homologue of the S-enantiomer of the mepivacaine/bupivacaine series formulation as hydrochloride monohydrate, preservative free 0.2%, 0.75%, 1% stability 36 months, with adrenaline 24 months pH of solution adjusted with NaOH or HCL to remain between 4.0-6.0, with adrenaline pH 3.03.5 94% bound to 1-acid glycoprotein (competes with muscle relaxants and is known to prolong the action of pancuronium and suxamethonium) Vdss 59 L clearance occurs almost entirely by metabolism, 0.82 L/min, elimination half life 110 minutes hepatic extraction ratio 0.49 most metabolised oxidatively by hepatic enzymes and excreted in urine as 2,6,pipecoloxylidine, 3-hydroxyropivacaine, 4hydroxyropivacaine 85% of all metabolites are recovered in urine, and 9% recovered in faeces 1% is excreted unchanged conjugated 3-hydroxyropivacaine is the main metabolite formation of 3-hydroxyropivacaine (37% of a dose) mediated by CYP1A2, while minor products are formed by the action of CYP3A4 CYP1A2 is inhibited by fluvaxamine, quinolone antibacterials, induced by cigarette Ropivacaine versus bupivaaine
NC Hwang 2008
PR, QRS and QT prolonged but at 2-3 times the concentration of bupivacaine of shorter duration, less malignant arrhythmias for similar prolongation distinct advantages in epidural analgesia in labour, but ropivacaine less potent than bupivacaine for analgesia in early labour a greater number of spontaneous vertex deliveries and higher neonatal Neuroadaptive Capacity scores with ropivacaine compared with bupivacaine provides long duration of neural blockade 0.75% - 1.% for surgery 0.2% for postoperative pain relief and labour pain
anti-inflammatory effects inhibition of leukocyte adhesion, promoting vascular perfusion inhibition of inflammatory mediators (LTB4, 5HETE) potential beneficial effects in the treatment of ulcerative colitis inhibition of superoxide production
Local Anaesthetic Agents
Eutectic mixture of local anaesthetic (EMLA) cream denoting specifically mixtures of certain chemical compounds that have a lower melting point than any of their individual ingredients, melts at a temperature at which a eutectic mixture becomes fluid semi-solid, oil-in-water emulsion active ingredients mixture of lignocaine and prilocaine in their base forms in a 1:1 weight ratio (lignocaine 25mg: prilocaine 25mg) oil phase in the cream mixture emulsified by a non-ionic polyoxyethylene ester hydrogenated castor oil (Arlatone 298) the viscosity-controlling agent in the cream carboxypolymethylene (Carbomer 934P) pH adjusted to 9.4 by addition of NaOH melting point 18oC
NC Hwang 2008
Anda mungkin juga menyukai
- Inhalational AgentsDokumen17 halamanInhalational Agentsanaeshkl100% (1)
- Bio StatisticsDokumen21 halamanBio StatisticsanaeshklBelum ada peringkat
- Antiarrhythmic AgentsDokumen11 halamanAntiarrhythmic AgentsanaeshklBelum ada peringkat
- Antiarrhythmic AgentsDokumen11 halamanAntiarrhythmic AgentsanaeshklBelum ada peringkat
- Intravenous AgentDokumen12 halamanIntravenous AgentanaeshklBelum ada peringkat
- Inotropic AgentsDokumen5 halamanInotropic AgentsanaeshklBelum ada peringkat
- NarcoticsDokumen6 halamanNarcoticsanaeshkl100% (1)
- Anaesthesia For Endovascular Surgery (Tevar and EvarDokumen18 halamanAnaesthesia For Endovascular Surgery (Tevar and EvaranaeshklBelum ada peringkat
- Pharmaco KineticsDokumen16 halamanPharmaco KineticsanaeshklBelum ada peringkat
- Transfusion Error and Near MissesDokumen35 halamanTransfusion Error and Near Missesanaeshkl100% (1)
- Disseminated Intravascular CoagulationDokumen22 halamanDisseminated Intravascular Coagulationanaeshkl100% (2)
- Corticosteroid After Etomidate in Critically IllDokumen41 halamanCorticosteroid After Etomidate in Critically IllanaeshklBelum ada peringkat
- Severe Dengue in ICUDokumen35 halamanSevere Dengue in ICUanaeshklBelum ada peringkat
- Anaesthesia For Robotic Surgery: An Experience in KoreaDokumen42 halamanAnaesthesia For Robotic Surgery: An Experience in KoreaanaeshklBelum ada peringkat
- Laryngoscopy and Tracheal Intubation in The Head-Elevated Position in Obese Patients: A Randomized, Controlled, Equivalence TrialDokumen51 halamanLaryngoscopy and Tracheal Intubation in The Head-Elevated Position in Obese Patients: A Randomized, Controlled, Equivalence TrialanaeshklBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDokumen2 halamanNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDat boiBelum ada peringkat
- Post TestDokumen11 halamanPost TestDemuel Dee L. BertoBelum ada peringkat
- Medical Management of Missed AbortionDokumen4 halamanMedical Management of Missed AbortionJonathan San MartinBelum ada peringkat
- Cholangiocarcinoma: Adeel S. Khan,, Leigh Anne DagefordeDokumen21 halamanCholangiocarcinoma: Adeel S. Khan,, Leigh Anne DagefordeCirugía General HEVESBelum ada peringkat
- DM Reporting ZDokumen52 halamanDM Reporting ZZsazsaBelum ada peringkat
- Multiple Choice Question (MCQ) Exam: 15 Sample QuestionsDokumen4 halamanMultiple Choice Question (MCQ) Exam: 15 Sample QuestionsAnkita AgarwallBelum ada peringkat
- Private Practice in Ophthalmology: - Making It WorkDokumen16 halamanPrivate Practice in Ophthalmology: - Making It WorkFuadBelum ada peringkat
- Edacs Plainenglish SummaryDokumen4 halamanEdacs Plainenglish SummaryTO Joss AguilarBelum ada peringkat
- 3003 - Position Description-Performance Evaluation - Dialysis Services Medical DirectorDokumen8 halaman3003 - Position Description-Performance Evaluation - Dialysis Services Medical DirectorPriambadaPutraBelum ada peringkat
- Optimum Medical Solutions CatalogueDokumen20 halamanOptimum Medical Solutions CatalogueOptimum Medical SolutionsBelum ada peringkat
- SMBG En2Dokumen44 halamanSMBG En2Andreea GherasimBelum ada peringkat
- United Biotech WorldDokumen9 halamanUnited Biotech Worldswtyneha33Belum ada peringkat
- Upper Respiratory Tract Infection NCPDokumen2 halamanUpper Respiratory Tract Infection NCPAngelica Cassandra Villena100% (2)
- Preanalytical ErrorsSDokumen4 halamanPreanalytical ErrorsSARIF AHAMMED P100% (1)
- Hospital Standards For Accreditation For Afghanistan Hosp - Standards - PharmacyDokumen10 halamanHospital Standards For Accreditation For Afghanistan Hosp - Standards - PharmacyMaria Camila100% (1)
- Objectives of Staffing in NursingDokumen10 halamanObjectives of Staffing in NursingEli Zza KoiralaBelum ada peringkat
- Inlays and Onlays ReportDokumen32 halamanInlays and Onlays ReportAlnielJoManlapigBelum ada peringkat
- Anil Degaonkar, Nikhil Bhamare, Mandar Tilak Arterio-Enteric Fistula A Case ReportDokumen6 halamanAnil Degaonkar, Nikhil Bhamare, Mandar Tilak Arterio-Enteric Fistula A Case ReportDr. Krishna N. SharmaBelum ada peringkat
- Case Study FIXDokumen66 halamanCase Study FIXPatrick Kelvian100% (1)
- Hospital Disaster Management Guidelines: Directorate of Health Services, KeralaDokumen56 halamanHospital Disaster Management Guidelines: Directorate of Health Services, KeralaPrasetya PerwiraBelum ada peringkat
- Goal Management Training in Adults With ADHD An Intervention StudyDokumen9 halamanGoal Management Training in Adults With ADHD An Intervention StudyalilaBelum ada peringkat
- Care of Patients With Chest TubesDokumen2 halamanCare of Patients With Chest Tubesaurezea100% (1)
- Kuliah 16 Cor PulmonaleDokumen41 halamanKuliah 16 Cor PulmonalecaturwiraBelum ada peringkat
- HEattDokumen11 halamanHEattCarlos GuiterizBelum ada peringkat
- PBL PharmaDokumen4 halamanPBL PharmaCassandra HsergBelum ada peringkat
- Hemothorax HandoutsDokumen2 halamanHemothorax HandoutsJunathan L. DelgadoBelum ada peringkat
- Mini EssayDokumen1 halamanMini EssayNonny Tentia MBelum ada peringkat
- Uterine CancerDokumen10 halamanUterine CancerKristen Leigh MarianoBelum ada peringkat
- ERAS - Personal StatementDokumen1 halamanERAS - Personal StatementfewBelum ada peringkat