Endocrinology 02012012
Diunggah oleh
Jessica Taylor-WeissDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Endocrinology 02012012
Diunggah oleh
Jessica Taylor-WeissHak Cipta:
Format Tersedia
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
"My FLAT PiG"
List all the hormones secreted by the anterior pituitary
MSH - melanotropin FSH - stimulates sex organs LH - stimulates sex organs ACTH - adrenal growth and steroidogenesis Prolactin - stimulates lactation GH - stimulates somatic growth via IGF-1 and is counter-regulatory to insulin B FLAT
Which hormones in the Anterior pituitary are produced by the basophils?
Basophils produce FSH, LH, ACTH, TSH These hormones have a common alpha subunit. The beta subunit determines specicity.
Which hormones in the Anterior pituitary are produced by the acidophils?
GPA GH, Prolactin are produced by Acidophils
Impotence Amenorrhea (Prolactin inhibits GnRH) Gynecomastia (male breasts), Galactorrhea (abnormal milk production) Headache Bitemporal hemianopsia (loss of peripheral vision) General hypopituitary symptoms (if "mass effect" is present)
List 6 signs and symptoms of a prolactinoma
List a common clinical correlation that can mimic a prolactinoma
Dopamine antagonists (ex: antipsychotics) cause galactorrhea, amenorrhea, impotence, etc due to loss of dopamine inhibition on prolactin
1 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
2 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
First line: Bromocriptine or cabergoline (dopamine agonists)
What is the treatment for a prolactinoma?
Second line: Transsphenoidal surgical resection for large tumors NOTE: Bromocriptine can also be used in the treatment of Parkinson's disease.
Bitemporal hemianopsia (loss of peripheral vision) You must do a visual eld test (during the PE) on a patient with signs or symptoms of a prolactinoma! Other sx: amenorrhea, gynecomastia, galactorrhea, etc. What classic sign/symptom is this patient most likely experiencing? Both are caused by pituitary adenoma that secretes growth hormone GH secretion in childhood prior to skeletal epiphyseal closure = Gigantism Lengthening of long bones GH secretion in adulthood after epiphyseal closure = Acromegaly Thickening of bones Coarsening of skin/facial features Thickening hands and feet Prognathism (an overbite or underbite) Large tongue with deep furrows Deep voice Peripheral neuropathies due to nerve compression 1) Surgery or radiation 2) Octreotide: somatostatin analogue that inhibits GH release from the anterior pituitary
Compare and contrast Acromegaly and Gigantism
List 6 clinical signs and sx of Acromegaly
List three treatments for a pituitary adenoma that secretes growth hormone
3 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
3) Pegvisomant: GH receptor antagonist blocking the production of IGF-1
4 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
List the hormones involved in the hypothalamic pituitary axis and their relationships (inhibition/stimulation)
TRH --(+)--> TSH, Prolactin CRH ---(+)--> ACTH, MSH Dopamine --(-)--> Prolactin GHRH ---(+)--> GH Somatostatin ---(-)--> GH, TSH GnRH ---(+)--> FSH LH <---(-)--- Prolactin
The anterior pituitary is derived from which embryological tissue?
Oral ectoderm (Rathkes pouch)
The posterior pituitary is derived from what embryological tissue?
Neuroectoderm
Vasopressin, aka AVP (arginine-vasopressin) or ADH (antidiuretic hormone), has 2 functions:
List the two major function of vasopressin and it's other names.
1) Moderate vasoconstriction 2) Antidiuretic effect, increases passive water reabsorption in renal collecting ducts When ADH is present you make Dark urine
How do you diagnose a GH sectreing toumor?
Increased serum IGF-1, especially after a glucose tolerance test (should be less than 1ng/nL after ingesting 75g of glucose) MRI
5 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
List three normal reasons for an increase in GH
1. Stress 2. Exercise 3. Hypoglycemia Ingesting glucose should cause a decrease in IGF-1, if it doesn't, you dx GH secreting tumor
List two physiologic controls that cause and increase in AVP secretion
1) An increase in serum osmolality is sensed by osmoreceptors in hypothalamus which release AVP into the systemic circulation 2) Baroreceptors sense a decrease in blood volume (5-10%) and afferent inputs to the hypothalamus for more ADH
What are the signs and symptoms of diabetes insipidus?
Intense thirst and polyuria (over 3L/24hrs), together with an inability to concentrate urine Serum osmolarity is high (>290 mOsm/L), urine osmolarity is very low (<150mOsm/L), and urine specic gravity is low (<1.006) 1) Central diabetes insipidus: pituitary is not secreting ADH - Trauma to pituitary - Pituitary tumor
What are the types and causes of diabetes insipidus?
2) Nephrogenic diabetes insipidus: Kidney is not responding to ADH - Lithium - Hereditary Response to desmopressin distinguishes the two Adequate hydration, intranasal desmopressin (ADH analog) for replacement Note: if the DI was caused by trauma, the patient my recover ADH production in a 3-5 days, be careful not to over-hydrate!! Lack of ADH >7 days indicates permanent DI.
What is the treatment for Central diabetes insipidus?
6 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is the treatment for nephrogenic diabetes insipidus?
Adequate hydration, hydrochlorothiazide*, indomethacin, or amiloride * Thiazides increase renal Na excretion ECF volume contraction GFR proximal tubular reabsorption of water and Na less water and Na are lost as urine
What is the Syndrome of Inappropriate Antidiuretic Hormone and what are the causes?
SIAHD occurs when too much ADH is produced by the posterior pituitary (tumor), a lung tumor, or a lung infection. Medications such as chlorpropamide can also cause inappropriate ADH secretion Euvolemic hyponatremia - (Body responds by decreasing Aldo/Na reabsorption... bringing in free water and dumping Na) Abnormal mental status
List 5 signs and symptoms of SIADH?
Convulsions Fatigue Headache Irritability Normal blood pressure, no edema, etc Urine osmolarity will usually be be higher than serum osmolarity 1) Free water restriction if asymptomatic 2) Demeclocycline: inhibits the actions of ADH in the kidney. 3) Hypertonic (5%) saline if severe CNS changes, such as seizures CAUTION: Rapid correction of hyponatremia can lead to central pontine myelinolysis Rapid correction of hyponatremia can lead to central pontine myelinolysis Damage of myelin sheath of pons patient becomes "locked in": muscles paralyzed with exception of eye blinking, but cognitive
Name three treatments for SIADH
Discuss central pontine myelinolysis and its cause
7 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
function is intact
8 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What are the functions of oxytocin?
During labor: stimulates cervical, vaginal distention and uterus contraction Used clinically for: acute postpartum hemorrhage and to induce labor After labor: in the presence of oxytocin, nipple stimulation will "let down" breast milk
What are 3 adverse effects of oxytocin?
1) Hyponatremia 2) Seizures 3) Subarachnoid hemorrhage
Name the types of vitamin D and their sources
Vitamin D3 (cholecalciferol) - Sunlight/Skin and MILK!! Vitamin D2 (ergocalciferol) - Diet Breast milk is relatively vitamin D DEFICIENT! It is important to supplement this vitamin, especially in darker skinned newborns
Explain how vitamin D is activated
Vitamin D3 (skin) and Vitamin D2 (diet) 25OH vitamin D (in liver) ----> 1,25 OH2 vitamin D (via 1-hydroxylase in kidney) Macrophages can also convert vitamin D to it's active 1,25 OH2 form (cause of hypercalcemia in sacroidosis) Increase in both [Ca2+] and [phosphate]
List the four effects of Vitamin D on Ca2+ and Phosphate
Increase intestinal Ca2+ absorption via (calbindin-D-28K) Increase intestinal phosphate absorption Increase renal Ca2+ and phosphate reabsorption
9 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Increase bone resorption of Ca2+ and phosphate
10 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Name 4 factors that regulate 1-hydroxylase and their effect on this enzyme.
serum calcium, serum phosphate, PTH levels --- All INCREASE activity (more D) 1,25-OH2 vitamin D inhibits its own production by inhibiting 1-hydroxylase. Note: High phosphate from CKD inhibits 1-hydroxylase
How does PTH effect bones? (describe the biochemistry)
Binding of PTH to its receptor on osteoblasts osteoblasts secrete M-CSF and RANK-L, which stimulate osteoclasts to break down bone and release calcium.
Describe the mechanism of Paget's Disease and a possible underlying cause
Massive bone turnover due to osteoclastic and osteoblastic activity abnormal bone architecture May be caused by a slow virus infection (eg, paramyxoviruses such as measles or respiratory syncytial virus).
List the three phases of Paget's Disease
1. Hypervascular/Osteolytic phase 2. Intermediate phase 3. Quiescent phase
1. Excessive in osteoclastic activity shaggy lytic bone lesions. 2. Massive osteoblastic response ( alkaline phosphatase) production of woven "mosaic bone" that is weak (radiolucent), thick and highly vascular 3. Mosaic bone is replaced areas of highly cellular lamellar bone with irregular "cement lines"
List the three stages of bone activity in the hypervascular/ostolytic phase of Paget's disease.
11 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Describe the bones activity in the intermediate stage of paget's disease
Osteoclastic activity is still present, but osteoblastic activity predominates
Descrive the activity and physical features of bone during the Quiescent phase of Paget's disease
osteoblastic activity eventually declines Sclerotic bone: - enlarged/widened bones - absent Haversian systems - marrow spaces replaced by vascular brous tissue Enlarged/widened bones that are weak:
List the signs and symptoms of Paget's disease. List at least 4 key symptoms.
Skull headaches; hat size; hearing loss (if ear canal involvement) Weight bearing bones bone pain especially at night, pathologic fractures Pagetoid bone is highly vascular with extensive arteriovenous shunting that may signicantly blood ow cardiac output compensatory left ventricular hypertrophy and, in severe cases, high-output heart failure. Small risk of developing into osteogenic sarcoma
What are the 2 potential complications of Paget's disease
What are the characteristic lab ndings of Paget's disease
Serum levels: - normal calcium, phosphate, parathyroid hormone - alkaline phosphatase
12 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is the treatment for Paget's disease?
Bisphosphonates (eg, alendronate, pamidronate, etidronate) are rst-line agents
What is the mechanism for Primary Osteoporosis Type I (Postmenopausal)
Estrogen deciency increased activity of RANKL/RANK and therefore osteoclasts 1. Osteoclast activity (bone resorption) 2. Osteoblast activity (bone formation compensates but unable to keep up with osteoclast activity)
Name 5 classic characteristics of 22q11.2 Deletion Syndrome (aka DiGeorge Syndrome or velocardiofacial syndrome)
CATCH-22: microdeletion of central portion of chromosome 22 Cardiac defects Abnormal facial features Thymic aplasia - leads to T cell malfunction Cleft palate Hypocalcemia: due to hypoparathyroidism 22 1. Vitamin D decient diets (most common) 1. GI malabsorption of fat-soluble vitamins 2. Renal osteodystrophy: chronic renal failure 1--hydroxylase activity 3. Aluminum-containing phosphatebinding antacids (mechanism?) 4. Phenytoin (seizure drug) 5. Obesity (D is trapped by fat!) Calcepenic rickets (most common) Serum levels: Calcium Phosphate Parathyroid hormone (PTH) Alkaline Phosphatase
List 5 common causes of vitamin D deciency
What are the two types of ricketts? What are the common lab ndings for both?
13 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Phosphopenic rickets (rare): low Phos, normal PTH, Calcium, and Vit D
14 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is the common mechanism for Rickets and Osteomalacia?`
Vitamin D Deciency leads to decreased Ca increased PTH levels decreasing phosphate, and mineralization of newly formed bone matrix (osteoid) Rickets (children) & osteomalacia (adults) Qualitative defects in bone formation versus a quantitative defect like osteoporosis Failure of mineralization leads to changes in the growth plate (increased width and disorientation) and bone (cortical thinning, bowing)
List the clinical ndings specic to Rickets (i.e., not found Osteomalacia)
Genus varus Rachitic "rosary chest": bony prominence at costochondral junctions Harrison's sulci: indentations in lower ribs Craniotabes: softening of skull bones Growth retardation
Genus varus in Rickets
What is the correct term for this condition? What disease causes this?
What are the symptoms of osteomalacia?
Diffuse bone pain, which is distinctly different from osteoporosis, which is painless, unless there is a fracture.
15 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What are the two types of parathyroid cells and what are their functions?
Chief cells: produce parathyroid hormone (PTH) Oxyphil cells: function is unknown
16 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
serum Ca2+ and serum Phos
List the 4 actions of Parathyrdoid Hormone and the overall result.
1) bone resorption of calcium and phosphate 2) PTH stimulates 1-hydroxylase in the kidney increased 1,25-(OH)2 vitamin D production leading to intestinal absorption of Ca2+ 3) renal Ca2+ absorption ( urinary cAMP) 4) kidney reabsorption of phosphate free serum Ca2+ causes PTH
Explain how PTH is regulated by serum Ca2+ and Mg2+
secretion. Ca2+-sensing receptors on chief cells mediate these effects. Mild decreases in Mg2+ stimulate PTH secretion, while severe decreases in Mg2+ inhibit PTH secretion and produce symptoms of hypoparathyroidism.
What are common causes of magnesium deciency?
Common causes of Mg2+: diarrhea, aminoglycosides, diuretics, and alcohol abuse
"Stones, bones and groans"
What are 5 signs and symptoms of hypercalcemia?
1) Mental status changes 2) Kidney (stones) 3) Muscle weakness 4) Cardiac Arrythmias 5) Constipation (groans) 6) Osteitis brosa cystica - cystic bone lled with brown berous tissue, causes (bone) pin
What are the three primary causes for primary hyperparathyroidism?
Single benign adenoma: majority of cases Hyperplasia of parathyroid glands: rare incidence MEN (multiple endocrine neoplasia) I and IIA
17 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Occurs when parathyroid glands are chronically stimulated by hypocalcemia to release PTH List the three most common causes of secondary hyperparathyroidism. What do they all have in common? Chronic renal failure: decreases Ca absorption and decreased hydroxylation of Vit D GI Malabsorptive disorder Rickets
List the primary cause of tertiary primary
Long standing hyperparathyroidism, usually due to chronic renal failure, progresses into autonomous hypersecretion of PTH even after correction of chronic hypocalcemia
What are the lab values for primary hyperparathyroidism
Calcium: High PTH: High (or inappropriately normal) Serum phosphate: low Urine phosphate: high Urine cAMP: high If the PTH is normal consider Vit Dtoxicity, sarcoidosis, thiazidediuretics, milk-alkali syndrome is a possible cause for the hypercalcemia Calcium: LOW (this is the cause!) PTH: High Serum phosphate: low, normal, or high depending on kidney function Urine phosphate: low, normal, or high depending on kidney function Alk phosphatase: high P will be low hypocalcemia is due to a GI problem, and high if due to CKD Parafollicular cells (C cells) of thyroid produce calcitonin
What are 5 pertinent lab ndings for secondary hyperparathyroidism
What cells produce calcitonin and what is its function?
Calcitonin is released due to increased serum calcium. It serves to decrease bone resorption of calcium, therefore decreasing serum Ca This hormone opposes PTH Not normally important in Ca homeostasis
18 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What are 4 classic signs and sx of hypocalcemia
1) Tetany 2) Carpal-pedal spasms (Trousseau's sign) 3) Prolonged QT interval 4) Parasthesias (numbness and tingling of extremities)
What is the cause of Vitamin D dependent Rickets Type 2
NOT ON BOARDS (1/5/12) - A mutation in the vitamin D receptor (on liver? kidney?) - Commonly associated with allopecia
What is the cause of Vitamin D dependent Rickets Type 1
NOT ON BOARDS (1/5/12) - A mutation in the alpha 1 hydroxylase enzyme Type 1 = alpha 1 - Low serum calcium - High serum phosphate - Low serum Vit D - Low PTH Hypocalcemic symptoms: tetany, neuromuscular irritability, carpal-pedal spasms
What are the 4 characteristic lab ndings of hypoparathyroidism
What are 3 classic signs and sx of hypoparathyroidism?
19 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Describe the mutation responsible for Pseudo-hypoparathyroidism and three classic features of this disease. How is this mutation inherited?
Autosomal dominant kidney unresponsiveness to PTH Classic sign: Shortened metacarpals 4th and 5th digits, hypocalcemia, short stature Pseudohypoparathyroidism is caused by a fault in the G protein receptor signaling pathway in the kidney leading to decreased urinary cAMP levels
What are the two PE signs that indicate hypoparathyroidism
Chvostek's sign: tapping the facial nerve --> elicit spasm of facial muscles Trousseau's sign: cut off blood ow to distal arm with BP cuff --> carpal spasm
List all ve layers of the adrenal gland and the hormones they make (if applicable)
1) Capsule Cortex 2) Zona Glomerulosa --> Mineralocorticoid Aldosterone (salt) 3) Zona Fasiculata --> Glucocorticoid Cotrisol (sugar) and sex hormones 4) Zona Reticularis --> Sex hormones (sex) 5) Medulla --> Catecholamines (Epi & Norepi)
List the primary regulatory control for the three layers of the adrenal cortex
1) ACTH, Renin-Angiotensin, Potassium ---> Zona Glomerulosa 2) ACTH (from CRH) --> Zona Fasiculata 3) ACTH (from CRH) --> Zona Reticularis
List the primary regulatory control for the adrenal medulla
Preganglionic sympathetic bers to the chromafn cells in the medulla
20 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Explain the mechanism behind the hyperplasia, in congenital adrenal hyperplasia
All congenital adrenal enzyme deciencies are characterized by enlargement of the adrenal glands due to an increase in ACTH stimulation (due to the decreased levels of cortisol)
Describe the pathophysiology behind 17 alpha hydroxylase deciency
A congenital adrenal hyperplasia that results in the inability of pregnenalone and progesterone to convert to 17-hydroxypregnenalone (percursor to cortisol and sex hormones) Leads to increased aldosterone (back-up) and decreased cortisol and sex hormones 1) Hypertension (too much aldo/Na) 2) Males become pseudohermaphroditic due to low levels of testosterone 3) Females will have normal genital development, but will not have enough estrogen to develop secondary sex characteristics
Describe the classic signs and sx of 17 alpha hydroxylase deciency
Describe the pathophysiology behind 21-hydroxylase deciency
MOST COMMON congenital adrenal hyperplasia that results in the inability of Progesterone and 17-Hydroxyprednisone to convert into 11-deoxycorticosterone and 11 deoxycortisol, respectively. Leads to decreased levels of aldo and cortisol, respectively, and an increase in sex hormones 1) Hypotension (low aldo) 2) Masculinization/female pseudohermaphroditism (clitoromegaly) 3) Hyperkalemia (low aldo) 4) Volume depletion due to salt wasting --> can lead to hypovolemic shock in newborns 5) Increased serum renin (due to volume depletion) with low serum aldo
Describe the classic signs and sx of 21-hydroxylase deciency
21 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Describe the venous drainage of adrenal gland
Left adrenal gland drainage: left adrenal vein --> left renal vein --> inferior vena cava Right adrenal gland drainage: right adrenal vein --> inferior vena cava
Describe the pathophysiology of Pheochromocytoma
Neuroendocrine tumor of adrenal medulla chromafn cells (arise from neural crest cells) that secretes catecholamine (norepi, epi, and dopamine) into the blood stream Most common tumor of the adrenal medulla in adults. Associated with MEN 2A and 2B. The 5 P's of Pheo
List the ve episodic hyperadrenergic symptoms of pheochromocytoma
Elevated blood Pressure Pain (headache) Perspiration Palpitations Pallor Symptoms occur in spells (unknown mechanism)
What is the treatment for pheochromocytoma?
Alpha antagonists: phenoxybenzamine (non-selective and irreversible) Followed by surgery to remove the tumor
What are the typical lab ndings of pheochromocytoma? Name 4 (three are UA results)
1) Elevated plasma catecholamines Elevated urinary biproducts of the catecholamines - Dopamine --> HVA - Norepi --> VMA - Epinepherine --> metanepherines
22 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What its the "rule of tens" for pheochromocytoma
10% malignant 10% bilateral 10% extra-adrenal 10% familial (Men 2A or 2B) 10% calcify 10% kids
Neuroendocrine tumor derived from neural crest cells. Most often found in adrenal medulla but can also be found anywhere along sympathetic chain. Causes elevation in catecholamines and urinary HVA Most common extracranial solid cancer in infancy 1) Spinal cord compression 2) Weakness 3) Bone lesions 4) Swollen neck and abdomen ** Hypertension is uncommon!**
Describe the pathophysiology of Neuroblastoma
What 4 complications/clinical symptoms are associated with neuroblastoma.
What are the 2 lab ndings of Neuroblastoma? What is the clinical signicance of the second?
1) Homovanillic acid (HVA) a breakdown product of dopamine is found in urine 2) Overexpression of N-myc oncogene is associated with rapid tumor progression
Waterhouse-Friderichsen syndrome Acute adrenocortical insufciency associated with meningococcal septicemia Massive hemorrhage within adrenal glands leads to hypotension and shock, with widespread purpura.
23 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is the pathophysiology of this diagnosis?
24 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Describe the pathophysiology of Primary Addison's disease and 6 common causes.
Adrenal Atrophy or destruction leading to absence of hormone production in all 3 cortical divisions. Caused by: 1) Autoimmune 2) TB granuloma 3) Infarction of adrenal gland 4) HIV 5) Waterhouse-Friderichsen syndrome 6) DIC (disseminated intravascular coagulation) 1) Hyponatremic volume contraction 2) Hyperkalemia 3) Constipation, diarrhea, fatigue 4) Skin hyperpigmentation* *ACTH is high, trying to make more cortisol. Melanocyte-stimulating hormone MSH shares the same precursor molecule as ACTH 1) Hyperpigmentation 2) Abnormal cosyntropin (synthetic ACTH) stimulation test: subnormal response of plasma cortisol following cosyntropin is denitive and diagnostic of adrenocortical insufciency 3) Abnormal metyrapone test: ACTH, but no in 11-deoxycortisol
What are the classic signs and symptoms of Primary Adrenocortical Insufciency (Addison's)
List three ways to diagnose Primary Addison's
What is the treatment of Addison's disease?
1) Fluid replacement for hypovolemin shock 2) IV dexamethasone 3) Eventual syntheic mineralocorticoid replacement
What is the pathophysiology of Secondary Adrenocortical Insufciency and name three things that distinguish it from primary disease.
Decreased production of pituitary ACTH Secondary Adrenocortical Insufciency is not associated by hyperpigmentation (no MSH) If given cosyntropin (synthetic ACTH), cortisol will rise appropriately
25 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
List the 5 functions of Cortisol (BBIIG)
1) Upregulates alpha 1 receptors to maintain Blood pressure 2) Decreased Bone formation (inhibits osteoblasts and GI Ca2+ absorption) 3) Anti-Inammatory 4) Decreases Immune function (inhibition of PLA2 IL-2 via lipocortin) 5) Increases nutrient catabolism (Gluconeogenisis) 1) Paraventricular nuclei of the hypothalamus release CRH 2) CRH stimulates corticotrophs in anterior pituitary to synthesize POMC --> ACTH and MSH 3) ACTH increases steroid hormone synthesis in the adrenal cortex by activating cholesterol desmolase 4) Cortisol inhibits the release of CRH 1) Low dose causes suppression of ACTH: Normal 2) ACTH is still produced after low dose dexamethasone: Cushing's disease (pituitary adenoma) 3) ACTH is still produced after high dose dexamethasone: Ectopic ACTH producing tumor Late distal tubule/collecting duct 1) renal Na+ reabsorption by principal cells + secretion by principal cells 2) renal K cells + secretion bu -intercalated 3) renal H cells Excess aldo = hypokalemia and metabolic alkolosis are common, hypernaremia is rare! Aldosterone is under tonic control by ACTH, but is separately regulated by the reninangiotensin-aldo system and by potassium Hyperkalemia & low BP will cause and increase in aldo secretion Angiotensin II increases the activity of aldosterone synthase in the zona glomerulosa
List the 3 steps leading to cortisol production and how it is regulated
Explain the three results of a Dexamethasone suppression test and what they indicate
List the three actions (and the location of action) of Mineralocoritoids (Aldosterone)
List three factors that regulate aldosterone secretion
26 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is renal osteodystrophy?
Bone lesions (osteoclastic resorption of cortical bone subperiosteal thinning with cystic degeneration, may or may not be "brown") due to primary or tertiarty hyperarathyroidism caused by chronic kidney faliure
What is the pathophysiology of renal osteodystrophy
Chronic renal failure activity of 1--hydroxylase 1,25-(OH)-vitamin D absorption of calcium from the gut hypocalemia production of parathyroid hormone (PTH) osteoclastic resorption of cortical bone subperiosteal thinning with cystic degeneration cystic bone lesions/tumors
What are three charateristics of Osteitis Fibrosa Cystica and what is the cause?
1) osteoclastic resorption of calcied bone 2) Peritrabecular brosis 3) Cystic "brown tumors" in bone Caused by prolonged, severe hyperparathyroidism (Primary, secondary, or tertiary) A single benign adrenal tumor (adenoma) or bilateral hyperplasia of the adrenal glands result in overproduction of aldosterone Elevated aldosterone levels Mild hypertension (due to Na/H2O retention), hypokalemia (K dumping), metabolic alkalosis due to cell exchange of H for K. NO hypernatremia!
Describe the pathophysiology of Primary Hyperaldosteronism (Conn's Disease)
What are 2 classic signs of hypokalemia?
1) Muscle weakness 2) Cardiac changes visible on EKG (classically described as U-waves)
27 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
How is primary hyperaldosteronism diagnosed? (what do the labs look like)
High aldosterone suppresses the secretion of renin. In primary hyperaldosteronism, low levels of renin are seen. By contrast, a high renin level suggests secondary hyperaldosteronism as in reno-vascular hypertension (due to RAS, CHF, chronic renal failure, etc)
What are 2 treatments for primary hyperaldosteronism?
1) Surgery 2) Spirinolactone to block the aldo being produced by the tumor
CHF cirrhosis, chronic renal failure, nephrotic syndrome, and renal artery stenosis cause low renal vascular volume --> stimulates renin-angiotensin system which increases aldosterone production Diagnosis: increased aldosterone levels with high plasma renin. Too much cortisol!
What is the cause and effect of Secondary Hyperaldosteronism. How is it diagnosed?
List the four causes of cushings syndrome and their respective levels of ACTH
1) Iatrogenic steroid use --- low ACTH due to feedback inhibition 2) Cushings disease (pituitary adenoma of ACTH) -- lots of ACTH 3) Ectopic ACTH tumor -- lots of ACTH 4) Zona Fasiculata Adenoma -- low ACTH due to feed back inhibition 1) Hypertension (excess alpha 1) 2) Weight gain 3) Proximal muscle weakness 4) Buffalo hump 5) Eccymosis over arms and legs 6) Moon face 7) Osteoporosis 8) Amenorrhea 9) Immune diciency 10) Skin thinning and striae
What are the 5 of the 10 classic symptoms of Cushing's syndrom
28 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What are the three key characteristics of MEN 1? And what is the most common clinical complaints?
1) Parathyroid tumors 2) Pitutary tumors (prolactin or GH) 3) Pancreatic endocrine tumors (Zollingerellison syndrome, insulinomas, VIPomas, etc) Clinically presents as: Kidney stones and stomach ulcers
All via autosomal dominant inheritance
How are all MEN (multiple endocrine neoplasia) syndromes acquired?
MEN 2A and 2B are specically associated with the ret gene, which causes a defect in neural crest cells, the cell lines that give rise to the parafollicular cells in the thyroid and chromafn cells in the medulla.
What are the three characteristics of MEN 2A?
1) Medullary thyroid carcinomas (secretes calcitonin) 2) Pheochromocytoma 3) Parathyroid tumors
What are the three characteristics of MEN 2B?
1) Medullary thyroid carcinomas (secretes calcitonin) 2) Pheochromocytoma 3) Marfanoid habitus/mucosal neuromas
What are neurophysins and what are their function?
Neurophysins are carrier proteins released from the posterior pituitary that carry ADH from the supraoptic nuclei and oxytocin from the paraventricular nuclei, through the portal blood supply to the posterior pituitary. Defects = diabetes insipidis
29 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Explain the process of insulin production, make sure to name the cells responsible
Synthesized and secreted by pancreatic cells Synthesized as proinsulin, which gets cleaved to insulin & C-peptide (essential for proper folding) and stored in secretion granules
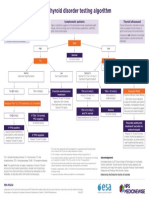
List the three types of hypothyroidism and their corresponding TSH values
1) Primary hypothyroidism (caused by thyroid hypofunction): TSH 2) secondary hypothyroidism (caused by pituitary hypofunction): TSH 3) tertiary hypothyroidism (caused by hypothalamic hypofunction): TSH 1) Hashimoto thyroiditis (chronic autoimmune thyroiditis) 2) Post ablation: surgical or I-131 radiation (people treated for Graves) 3) Iodine deciency 4) Drugs: lithium, amioderone, and sulfonamides 5) Subacute lymphocytic (painless) thyroiditis: 1/3rd of patients become hypothyroid within 10 years Disease due to severe fetal hypothyroidism
What are 5 common causes of primry hypothyroidism?
What is cretinism? How can it be avoided?
mental retardation pot-bellied stomach protruding umbilicus and tongues - Mental retardation can be minimized when thyroid hormone is administered in neonatal period. Congenital hypothyroidism is most commonly caused by thyroid dysgenesis due to thyroid aplasia/hypoplasia/ectopy
What is/are the most common cause and symptoms of congenital hypothyroidism?
Hoarse cry Macroglossia Enlarged fontanelles Pot belly with umbilical hernia Big puffy eyes and faces Jaundice Poor feeding and hypotonia
2/1/12 8:57 PM
30 of 47
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
31 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What are 7 common signs and symptoms of hypothroidism?
1) Cold intolerance 2) Weight gain 3) Fatuige/depression 4) Dry akey skin 5) Myxedema (facia, periorbital) 6) Bradycardia 7) Carpal tunnel 8) Slow deep tendon reexes 9) Constipation Emergent hypothyroid condition
What are the symptoms of myxedema coma and how do you treat it?
S/Sx: hypothermic stupor/coma, hypoventilation with CO2 retention, hypotension Treatment: respiratory support, intravenous levothyroxine, cortis
What are the three types of hyperthryoidism and what are their corresponding TSH trends?
1) Primary hyperthyroidism: TSH 2) Secondary hyperthyroidism: TSH ; in the rare case that a patient has secondary hyperthyroidism due to a TSH-secreting pituitary adenoma inject TRH and look for in TSH
What is the pathophysiology behind the clinical manifestations of hyperthyroidism
1) Hypermetabolic state (e.g., Na+/K+ ATPase activity): due to T4 and T3 2) Sympathetic nervous system overactivity: T4 and T3 synthesis of adrenergic receptors adrenergic tone
List 7 common symptoms of hyperthyroidism
1) Sweating, heat intolerance 2) Weight loss 3) Warm, ushed skin 4) Tremor, anxiety, palpitations 5) Opthalmopathy 6) Increased bone turnover --> osteoporosis 7) Diarrhea 8) Brisk tendon reexes
32 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Explain the pathophysiology behind the opthalmopathy in non-graves thyroiditis
- SNS overstimulation of levator palpebrae superioris wide-eyed staring gaze and lid lag - Note: true thyroid ophthalmopathy with exophthalmos (proptosis) is only seen in Graves disease, the exopthalmos has it's own pathophysiology
List 3, non-thyroid-related, lab tests that are important to hyperthyroidism
1) bone turnover serum calcium (hypercalcemia) 2) glycogenolysis serum glucose (hyperglycemia) 3) LDL receptor synthesis serum cholesterol (hypocholesterolemia)
List the triad of clinical ndings in Graves Disease?
1) Hyperthyroidism: nontender hyperfunctional enlargement of the thyroid 2) Inltrative ophthalmopathy: due to accumulation of glycosaminoglycans and adipose in retro-orbital tissue 3) Inltrative dermopathy: scaly thickening and induration of the skin overlying the shins with nonpitting edema (pretibial myxedema)
What is the would the radioactive iodine study look like in a patient with a Toxic Adenoma of the thyroid?
Uneven 123I uptake with occasional autonomous "hot" nodules demonstrating 123I uptake
123I uptake - becuase T4 is in the blood stream, not in the thyroid - fever - painful thyroid - painful cervical lymphadenopathy Course: Hyperthyroid, followed by hypothyroid, followed by normalization Cause: Viral or bacterial infection
List the triad of clinical ndings Acute Thyroiditis and how a radioactive iodine study would appear. What is the common cause & course of this disease?
33 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Describe the radioactive iodine uptake pattern in Iatrogenic hyperthyroidism (accidental or for diet reasons)
123I uptake - decreased T4 in thyroid due to feedback inhibition
What is the pathophysiology behind initrative opthalmopathy?
TSI autoantibodies cross-react with orbital preadipocyte broblasts (which have TSH receptors, wtf) causing them to synthesize glycosaminoglycans Accumulation of GAGs, fat and T cells in the retro-orbital space (esp muscle, but not tendon) --> exopthalmos... not easily treated Type II Hypersensitivity TSI (thyroid-stimulating immunoglobulin) auto-ab = IgG that binds and activates TSH receptor relatively specic for Graves Anti- thyroglobulin and anti-thyroid peroxidase antibodies are often present - Normally due to aggravated Graves - high fever (hyperpyrexia) - tachycardia out of proportion to fever - tachyarrhythmias common cause of death in patients with thyroid storm - shock due to heart failure and/or vomitinginduced volume depletion - coma Most common cause of hypothyroid. Auto-abs attack thyroid 1) Anti-thyroid autoantibodies (anti-Tg and anti-TPO) 2) CD8+ T-cell mediated cell death 3) Cytokines activate TH1 IFN- recruits and activates macrophages follicle damage
What is the pathophisiology behind Graves disease?
What are 5 features of Thyroid Storm
What is the pathohysiology behind Hashimoto Thyroiditis
34 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
risk of developing other autoimmune diseases
What are some complications of Hashimotos Thyroiditis?
risk of primary thyroid lymphoma: - B-cell non-Hodgkin lymphomas, especially extranodal marginal zone lymphomas of MALT (mucosa-associated lymphoid tissue) type
Describe the clinical course of subacute thyroiditis. List 4 signs/sx.
1) Preceded by u-like illness with sore throat and fever, jaw pain, tender thyroid, and a markedly elevated ESR 2) Tender thyroid 3) Early phase can manifest as hyperthyroidism, as damaged gland spills T4 4) Resolves in 8ish weeks
Describe the pathophysiology of Reidel thyroiditis and the clinical consequences
Fibrous tissue replaces thyroid parenchyma, with brosis extending beyond the thyroid capsule into surrounding tissue. Hypothyroidism may occur.
List the three functional parts of the thyroid gland and their functions
Thyroid follicular cells: synthesize, store and secrete thyroid hormone Colloid: central space in follicle where thyroid hormone is stored as a component of thyroglobulin Parafollicular cells: synthesize and secrete hormone calcitonin
Name the cancer that forms in parafolicular cells and its important association
Medullary thyroid cancer, associated with MEN 2A and 2B
35 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
How would an radioactive iodine study appear in a patient with Graves?
Diffusely 123I uptake in the whole thyroid gland
What would the radioactive uptake scan look like in a patient with thyroid cancer
A COLD focal nodule, that is NOT taking up iodine becuase cancers do not normally produce thyroid hormone.
What would the radioactive uptake scan look like in a patient with thyroiditis?
Thyroiditis: 123I uptake
1) -blocker to control symptoms of SNS tone AND decrease peripheral conversion of T4 to T3 (mech unknown) 2) Propylthiouracil: inhibition of the organication and coupling steps of T4 & T3 synthesis, also inhibits peripheral conversion of T4 to T3 3) Methimazole: same as PTU, without peripheral benet. Category X. 1) High-dose iodine blocks release of T4 and T3 into the circulation via Wolffe-Chaikoff cycle 2) High-dose radioactive iodine: 131I (versus the 123I used in imaging studies) becomes concentrated in the thyroid gland ablation of thyroid function
Name the three most common pharmacologic treatments for hyperthyroidism
Compare and contrast the two different treatments involving iodine for hyperthyroidism
36 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
1) Iodine enters the follicular cell via Na-I symporter, I moves to lumen via pendrin channel 2) Thyroid peroxidase:
Describe the biochemical pathway that leads to the formation of T4/T3
Oxidizes I- to I0 Conjugates the I0 to tyrosine residues on thyroglobulin to form MIT & DIT. (organication) Couples MIT and DIT to form T3 and T4 (still attached to thyroglobulin) Iodinated thyroidglobulin is stored in the follicular lumen. Upon stimulation by TSH, follicular cells endocytoses thyroglobulin and lysosomal enzymes digest thyroglobulin, releasing T3 and T4 into the circulation. Residual MIT and DIT are deiodinated by thyroid deiodinase. The I2 that is generated is recycled to synthesize more thyroid hormone
Describe how T4 & T3 are released into the blood stream?
What inhibits the Na-I transporter in the thyroid follicular cell?
The Na-I transporter is inhibited by thiocyanate and perchlorate anions
Name two medications that inhibit thyroid peroxidase
Thyroid peroxidase is inhibited by propylthiouracil (PTU) and methimazole!!!
Name the phenomenon in the thyroid that occurs due to Iodine overload?
Wolff-Chaikoff effect : High levels of I- inhibit thyroid hormone synthesis by blocking the organication step. Remember high levels of I can come from a CT or angiogram!
37 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
38 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
How and where is T4 converted to T3
T4 is deiodinated in peripherial tissue to T3 by the enzyme 5'-deiodinase. T3 is signicantly more potent than T4.
What HLA type is associated with Hashimotos thyroiditis?
HLA-DR5
Explain the pathogensis of Riedel's thyroiditis and two common physical exam ndings
1) Thyroid is replaced by berous tissue leading to hypothyroidism 2) xed, rock-like, painless goiter
Describe the pathophysiology behind a Toxic Multinodular Goiter
Focal patches of hyperfunctioning follicular cells that work independently of TSH due to a mutation in the TSH receptor Appear as hot nodules (increased uptake) on iodine study. Rarely malignant
Name the two types of cancer associated with Follicular cells along with their associations and prognoses
1) Papillary carcinoma: associated with childhood radiation exposure, excellent prognosis, most common 2) Follicular carcinoma: not associated with radiation, less common, good prognosis
39 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is the prognosis for a patient with Anaplastic Thyroid Cancer. Who gets this cancer?
VERY poor prognosis Older patients
Brain maturation - critical in neonatal period Bone growth - via synergism with GH and IGF-1 Beta-adrenergic effects - increases the number of Beta 1 receptors on heart muscle BMR - Na/K-ATPase activity More O2 TBG (thyroxine-binding globulin) binds most T3 or T4 in peripheral blood
What are the four major effects of thyroid hormone?
Explain the difference between free thyroid hormone and bound thyroid hormone. What is it bound to?
Only free T3 or T4 is active. TBG bound T3 or T4 is inactive. Conditions where TBG is increased or decreased can affect total T3 or T4 levels. (Pregnancy increases TGB, but thyroid compensates) Rare syndrome caused by neuroendocrine carcinoid tumors that secrete high levels of 5-HT serotonin. The seritonin will be undetectable in the blood stream due to rst pass effect by the liver.
Describe the pathophysiology of Carcinoid Syndrome
What 4 are the common sx of Carcinoid syndrome?
Carcinoid 1) Cutaneous ushing 2) Asthmatic wheezing 3) Right-sided valvular disease 4) Diarrhea
40 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
How do you diagnose Carcinoid syndrome?
Increased urinary secretion of 5 HIAA (5 hydroxyindoleacetic acid) a degradation product of serotonin
How do you treat Carcinoid syndrome?
Octreotide somatostatin analogue that neutralizes serotonin Surgical resection and chemotherapy with 5-FU (uorouracil) and doxorubicin
Gastrin secreting tumor of the pancreas or duodenem
What is the pathophysiology, clinical consequence and important association of Zollinger-Ellison Syndrome?
Causes recurrent ulcers Associated with MEN-1
Describe the hormonal abnormalities in Klinefelters syndrome and their cause
Hyaliniaztion and brosis of the seminiferous tubules leads to lack of testosterone synthesis - Increased LH and FSH - Testosterone is low --> infertility and absence of secondary sex characteristics
Dene agranulocytosis, the primary symptoms, and the cause. How would you proceed with a patient if you suspect this condition?
Def: absolute PMN count less than 500/mL Sx: Fever & sore throat Cause: propylthiouracil and methimazole (in patient with a history of hyperthyroidism) Tx: d/c medication and order CBC with diff
41 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
What is a lingual thyroid. What complications can occur with treatment of this problem?
Due to failure of migration, the thyroid ca form at any part along the thyroglossal duct's usual path, including the tongue = lingual thyroid. Sometimes this may be the only thyroid tissue in the body and removal of the mass can lead to life threatening hypothyroidism. LH: elevated FSH: elevated Testosterone: very low Sperm count: low Due to the brosis of the seminiferous tubules & damage to the Leydig cells, testo is very low and there is no feedback inhibition to the pituitary.... LH and FSH are high. Beta bockers prevent the conversion of T4 to T3 in peripheral tissues. The mechanism behind this effect is unknown Thyroid hormone also increases the number of beta receptors on cell membranes. Beta blocker will mitigate this and decrease sympathetic tone.
What would the LH, FSH, Testosterone, and sperm count levels be in a patient with Klinefelters syndrome?
What effect does a beta blocker have on thyroid hormone?
Mutations in what gene are responisble for the majority of familial medullary thyroid cancers
A mutation that activates the proto-oncogene "RET". This is the underlying mechanism behind medullary thyroid cancers in MEN 2A and 2B
List three features of Marfanoid Habitus and three clinical diseases associated with this body type.
1) Long limbs 2) Arachnodactyly (abnormally long and slender limbs) 3) Hyperlaxity - Marfan syndrome, MEN 2B, Homocystinuria
42 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Marfanoid habitus 1) long limbs 2) Arachnodactyly 3) Hyperlaxity (double jointedness)
Describe this man's appearance ADH is sythesized in the supraoptic nuclei of the hypothalamus. Damage to the nuclei or the pituitary stalk results in central DI. While ADH is released from the posterior pituitary (hypophysis), damage to this area only causes transient DI, because ADH can still be secreted from the pituitary stalk.
Where is ADH synthesized?
What does 5-alpha reductase do and where does it function?
5-alpha reductase converts testosterone to DHT in target tissues
Describe the effect of GnRH on hormone production from the gametes
Normally GnRH release from the hypothalamus is pulsitile, leading to transient release of LH and FSH, and therefore testosterone However, if GnRH levels are constantly elevated, LH and FSH production is suppressed
Describe the mechanism and clinical application of the drug Leuprolide
Leuprolide is a long-long acting GnRH analogue that causes eventual suppression of the GnRH/LH-FSH axis and therefore a decrease in testosterone and DHT. Preceded by a "air up" of testo and DHT. Used to treat prostate cancer
43 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
44 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Explains why hypernatremia is rare in patients with hyperaldosteronism
Explain the concept of aldosterone escape
Increaed Na/Cl uptake by excess aldo leads to hypervolemia. This triggers Atrial natruetic peptide, which causes diurese and compensatory Na loss. --> mild hypertension due to volume expansion, but not hypernatremia Hypotension, Hypoglycemia, and tachycardia Presenting with one or more of the following: voimiting, abdominal pain, weight loss, hyperpigmentation Tx: urgent administration of glucocorticoids is always warrented when adrenal crisis is suspected. You do not need lab conrmation.
What is the clinical presentation of adrenal crisis? What is the treatment?
Describe the hormonal axis involving leydig cells
Hypothalamus secretes GnRH --> Pituitary secretes LH --> LH stimulates leydig cells to produce testosterone --> Testosterone inhibits the pituitary release of LH and the hypothalamic release of GnRH
Describe the hormonal axis involving sertoli cells
Hypothalamus produces GnRH --> pituitary secretes FSH --> FSH stimulates sertoli cells to produce inhibin --> inhibin inhibits the pituitary from releasing FSH, but has no effect on the GnRH production of the hypothalamus (LH and testo can keep going)
Sertoli cells are damaged. What happens to the hormone axis involving the testes?
No inhibin is produced, which allows the FSH to be produced unchecked (inhibin low and FSH high). Testosterone and LH will be uneffected.
45 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
Rare pancreatic tumor that presents with necrolytic migratory erythema
List the 3 key characteristics of a Glucagonoma
Patients are usually diagnosed as "diabetic" due to hyperglycemia Other sx: stomatitis (gum inammation), cheilosis (corners of mouth), and abdominal pain.
What is the function of demeclocycline? What is it used for? Side effects?
ADH antagonist used to treat SIADH Side effects: nephrogenic DI, photosensitivity, abnormalities of bones and teeth
Name four clinical syndromes (all discussed this this section) that can be treated with somatostatin
1) Acromegally 2) Carcinoid syndrome 3) Gastrinoma 4) Glucagonoma
What is the effect of testosterone and estrogen on bone growth
Sex hormones promote both growth and epiphysial plate closure, so the earlier they are introduced the shorter the stature. This is in contrast to GLP-1 (somatostatin-C), causes bone growth without epiphyseal closure leading to gigantism.
Explain the cause of amenorrhea in an anorexic patient
Patients with anorexia nervosa often experience amenorrhea due to loss of pulsatile secretion of GnRH from the hypothalamus. This leads to low estrogen production from the ovaries, but this problem begins in the hypothalamus.
46 of 47
2/1/12 8:57 PM
StudyBlue Flashcard Printing of Endocrinology
http://www.studyblue.com/servlet/printFlashcardDeck?deckId=...
List three scenarios where desmopressin (DDAVP) is the standard treatment
1) Central Diabetes Insipidus 2) Mild Von Willibrand's disease (also useful in hemophelia A) 3) Enuresis (bed wetting)
47 of 47
2/1/12 8:57 PM
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- IR Light Therapy PDFDokumen97 halamanIR Light Therapy PDFcamarondelaisla100% (3)
- Hypothyroidism and ThyroiditisDokumen35 halamanHypothyroidism and ThyroiditisXochil RmzBelum ada peringkat
- Art 3A10.1007 2Fs00259 013 2535 3 PDFDokumen477 halamanArt 3A10.1007 2Fs00259 013 2535 3 PDFHerryAsu-songkoBelum ada peringkat
- Cme Endocrinology Saqs (80447) : Self-Assessment QuestionnaireDokumen3 halamanCme Endocrinology Saqs (80447) : Self-Assessment QuestionnaireAbu AhmedBelum ada peringkat
- Enf Tiroidea y Embarazo Lancet 2018Dokumen12 halamanEnf Tiroidea y Embarazo Lancet 2018Jair Alexander Quintero PanucoBelum ada peringkat
- 70 Years of LevothyroxineDokumen141 halaman70 Years of LevothyroxinecavrisBelum ada peringkat
- Cretenism Case StudyDokumen8 halamanCretenism Case StudyMonica Marie MoralesBelum ada peringkat
- Bhs Inggris PerbaikanDokumen4 halamanBhs Inggris PerbaikanDolly cupingBelum ada peringkat
- Anatomy and Physiology of ThyroidDokumen74 halamanAnatomy and Physiology of ThyroidSajid NadafBelum ada peringkat
- Magnetic Resonance Imaging Versus Serum Iron Status As Diagnostic Tools For Pituitary Iron Overload in Children With Beta ThalassemiaDokumen13 halamanMagnetic Resonance Imaging Versus Serum Iron Status As Diagnostic Tools For Pituitary Iron Overload in Children With Beta ThalassemiaAbdurrahman HasanuddinBelum ada peringkat
- 2nd Journal - Andre Parmonangan Panjaitan - 013Dokumen7 halaman2nd Journal - Andre Parmonangan Panjaitan - 013Andre Parmonangan PanjaitanBelum ada peringkat
- DissertationDokumen88 halamanDissertationShohida NaimovaBelum ada peringkat
- Hormones and Related DrugsDokumen42 halamanHormones and Related DrugsRamya PrabhuBelum ada peringkat
- NPS MedicineWise Thyroid Testing Algorithm v3Dokumen1 halamanNPS MedicineWise Thyroid Testing Algorithm v3Mikhael JHBelum ada peringkat
- Endocrine HarmonyDokumen68 halamanEndocrine HarmonyafnanBelum ada peringkat
- ОВБ-2 Ответы фулDokumen70 halamanОВБ-2 Ответы фулMoldir AkynbayBelum ada peringkat
- Common Drugs To ExplainDokumen2 halamanCommon Drugs To ExplainJeemeenee Haerim SonBelum ada peringkat
- Management of of Clients With Metabolic and EndocrineDokumen79 halamanManagement of of Clients With Metabolic and Endocrineagbogoodness100% (1)
- Title: Congenital Hypothyroidism: A Ran Sacker Escaping Under The Nose AbstractDokumen6 halamanTitle: Congenital Hypothyroidism: A Ran Sacker Escaping Under The Nose AbstractKavita KhannaBelum ada peringkat
- Nursing Practice Test - EndocrineDokumen20 halamanNursing Practice Test - Endocrinemay17sanchez100% (7)
- Endocrine, Metabolic & Nephrology MCQS: Thyroid Eye DiseaseDokumen78 halamanEndocrine, Metabolic & Nephrology MCQS: Thyroid Eye DiseaseDr.younes95 RekaaneyBelum ada peringkat
- The Prevalence of Anti-Thyroid Peroxidase Antibodies and Autoimmune Thyroiditis in Children and Adolescents in An Iodine Replete AreaDokumen7 halamanThe Prevalence of Anti-Thyroid Peroxidase Antibodies and Autoimmune Thyroiditis in Children and Adolescents in An Iodine Replete AreaAkshay BankayBelum ada peringkat
- Thyroid Benign TumorDokumen30 halamanThyroid Benign TumormackieccBelum ada peringkat
- Endocrin E Diseases: by Group 3Dokumen53 halamanEndocrin E Diseases: by Group 3Ash AshBelum ada peringkat
- Pediatric in ReviewDokumen10 halamanPediatric in ReviewkafosidBelum ada peringkat
- Pathologic Conditios of Endocrine Disorder.Dokumen42 halamanPathologic Conditios of Endocrine Disorder.ramoli1988Belum ada peringkat
- BHTbook StevenWmFowkes 141016Dokumen67 halamanBHTbook StevenWmFowkes 141016Sparklight JackBelum ada peringkat
- Hypothyroidism Case AnalysisDokumen3 halamanHypothyroidism Case AnalysisKrisianne Mae Lorenzo FranciscoBelum ada peringkat
- Armour Thyroid (Thyroid Tablets, USP) RX Only: I I NHDokumen10 halamanArmour Thyroid (Thyroid Tablets, USP) RX Only: I I NHAdam GolsbyBelum ada peringkat
- Thyroid Case StudyDokumen68 halamanThyroid Case Studyshadydogv5Belum ada peringkat