CAD Practice Questions
Diunggah oleh
Kristalene SampayanDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CAD Practice Questions
Diunggah oleh
Kristalene SampayanHak Cipta:
Format Tersedia
1) A client is scheduled for a cardiac catherization using a radiopaque dye.
Which of the following assessments is most critical before the procedure? 1. Intake and output 2. Baseline peripheral pulse rates 3. Height and weight 4. Allergy to iodine or shellfish 2) A client with no history of cardiovascular disease comes into the ambulatory clinic with flulike symptoms. The client suddenly complains of chest pain. Which of the following questions would best help a nurse to discriminate pain caused by a non-cardiac problem? 1. Have you ever had this pain before? 2. Can you describe the pain to me? 3. Does the pain get worse when you breathe in? 4. Can you rate the pain on a scale of 1-10, with 10 being the worst? 3) A client with myocardial infarction has been transferred from a coronary care unit to a general medical unit with cardiac monitoring via telemetry. A nurse plans to allow for which of the following client activities? 1. Strict bed rest for 24 hours after transfer 2. Bathroom privileges and self-care activities 3. Unsupervised hallway ambulation with distances under 200 feet 4. Ad lib activities because the client is monitored. 4) A nurse notes 2+ bilateral edema in the lower extremities of a client with myocardial infarction who was admitted 2 days ago. The nurse would plan to do which of the following next? 1. Review the intake and output records for the last 2 days 2. Change the time of diuretic administration from morning to evening 3. Request a sodium restriction of 1 g/day from the physician. 4. Order daily weights starting the following morning. 5) A client is wearing a continuous cardiac monitor, which begins to sound its alarm. A nurse sees no electrocardiogram complexes on the screen. The first action of the nurse is to: 1. Check the client status and lead placement 2. Press the recorder button on the electrocardiogram console. 3. Call the physician 4. Call a code blue 6) A nurse is assessing the blood pressure of a client diagnosed with primary hypertension. The nurse ensures accurate measurement by avoiding which of the following? 1. Seating the client with arm bared, supported, and at heart level. 2. Measuring the blood pressure after the client has been seated quietly for 5 minutes. 3. Using a cuff with a rubber bladder that encircles at least 80% of the limb. 4. Taking a blood pressure within 15 minutes after nicotine or caffeine ingestion. 7) IV heparin therapy is ordered for a client. While implementing this order, a nurse ensures that which of the following medications is available on the nursing unit?
1. Vitamin K 2. Aminocaporic acid 3. Potassium chloride 4. Protamine sulfate 8) A client is at risk for pulmonary embolism and is on anticoagulant therapy with warfarin (Coumadin). The clients prothrombin time is 20 seconds, with a control of 11 seconds. The nurse assesses that this result is: 1. The same as the clients own baseline level 2. Lower than the needed therapeutic level 3. Within the therapeutic range 4. Higher than the therapeutic range 9) A client who has been receiving heparin therapy also is started on warfarin. The client asks a nurse why both medications are being administered. In formulating a response, the nurse incorporates the understanding that warfarin: 1. Stimulates the breakdown of specific clotting factors by the liver, and it takes 2-3 days for this to exert an anticoagulant effect. 2. Inhibits synthesis of specific clotting factors in the liver, and it takes 3-4 days for this medication to exert an anticoagulant effect. 3. Stimulates production of the bodys own thrombolytic substances, but it takes 2-4 days for this to begin. 4. Has the same mechanism of action as Heparin, and the crossover time is needed for the serum level of warfarin to be therapeutic. 10) A 60-year-old male client comes into the emergency department with complaints of crushing chest pain that radiates to his shoulder and left arm. The admitting diagnosis is acute myocardial infarction. Immediate admission orders include oxygen by NC at 4L/minute, blood work, chest x-ray, an ECG, and 2mg of morphine given intravenously. The nurse should first: 1. Administer the morphine 2. Obtain a 12-lead ECG 3. Obtain the lab work 4. Order the chest x-ray 11) When administered a thrombolytic drug to the client experiencing an MI, the nurse explains to him that the purpose of this drug is to: 1. Help keep him well hydrated 2. Dissolve clots he may have 3. Prevent kidney failure 4. Treat potential cardiac arrhythmias. 12) When interpreting an ECG, the nurse would keep in mind which of the following about the P wave? Select all that apply. 1. 2. 3. 4. Reflects electrical impulse beginning at the SA node Indicated electrical impulse beginning at the AV node Reflects atrial muscle depolarization Identifies ventricular muscle depolarization
5. Has duration of normally 0.11 seconds or less. 13) A client has driven himself to the ER. He is 50 years old, has a history of hypertension, and informs the nurse that his father died of a heart attack at 60 years of age. The client is presently complaining of indigestion. The nurse connects him to an ECG monitor and begins administering oxygen at 2 L/minute per NC. The nurses next action would be to: 1. Call for the doctor 2. Start an intravenous line 3. Obtain a portable chest radiograph 4. Draw blood for laboratory studies 14) The nurse receives emergency laboratory results for a client with chest pain and immediately informs the physician. An increased myoglobin level suggests which of the following? 1. Cancer 2. Hypertension 3. Liver disease 4. Myocardial infarction 15) When teaching a client about propranolol hydrochloride, the nurse should base the information on the knowledge that propranolol hydrochloride: 1. Blocks beta-adrenergic stimulation and thus causes decreased heart rate, myocardial contractility, and conduction. 2. Increases norepinephrine secretion and thus decreases blood pressure and heart rate. 3. Is a potent arterial and venous vasodilator that reduces peripheral vascular resistance and lowers blood pressure. 4. Is an angiotensin-converting enzyme inhibitor that reduces blood pressure by blocking the conversion of angiotensin I to angiotensin II. 16) The most important long-term goal for a client with hypertension would be to: 1. Learn how to avoid stress 2. Explore a job change or early retirement 3. Make a commitment to long-term therapy 4. Control high blood pressure 17) Hypertension is known as the silent killer. This phrase is associated with the fact that hypertension often goes undetected until symptoms of other system failures occur. This may occur in the form of: 1. Cerebrovascular accident 2. Liver disease 3. Myocardial infarction 4. Pulmonary disease 18) During the previous few months, a 56-year-old woman felt brief twinges of chest pain while working in her garden and has had frequent episodes of indigestion. She comes to the hospital after experiencing severe anterior chest pain while raking leaves. Her evaluation confirms a diagnosis of stable angina pectoris. After stabilization and treatment, the client is discharged from the hospital. At her follow-up appointment, she is discouraged because she is experiencing
pain with increasing frequency. She states that she is visiting an invalid friend twice a week and now cannot walk up the second flight of steps to the friends apartment without pain. Which of the following measures that the nurse could suggest would most likely help the client deal with this problem? 1. Visit her friend earlier in the day. 2. Rest for at least an hour before climbing the stairs. 3. Take a nitroglycerin tablet before climbing the stairs. 4. Lie down once she reaches the friends apartment. 19) Which of the following symptoms should the nurse teach the client with unstable angina to report immediately to her physician? 1. A change in the pattern of her pain 2. Pain during sex 3. Pain during an argument with her husband 4. Pain during or after an activity such as lawnmowing 20) The physician refers the client with unstable angina for a cardiac catherization. The nurse explains to the client that this procedure is being used in this specific case to: 1. Open and dilate the blocked coronary arteries 2. Assess the extent of arterial blockage 3. Bypass obstructed vessels 4. Assess the functional adequacy of the valves and heart muscle. 21) As an initial step in treating a client with angina, the physician prescribes nitroglycerin tablets, 0.3mg given sublingually. This drugs principle effects are produced by: 1. Antispasmotic effect on the pericardium 2. Causing an increased mycocardial oxygen demand 3. Vasodilation of peripheral vasculature 4. Improved conductivity in the myocardium 22) The nurse teaches the client with angina about the common expected side effects of nitroglycerin, including: 1. Headache 2. High blood pressure 3. Shortness of breath 4. Stomach cramps 23) Sublingual nitroglycerin tablets begin to work within 1 to 2 minutes. How should the nurse instruct the client to use the drug when chest pain occurs? 1. Take one tablet every 2 to 5 minutes until the pain stops. 2. Take one tablet and rest for 10 minutes. Call the physician if pain persists after 10 minutes. 3. Take one tablet, then an additional tablet every 5 minutes for a total of 3 tablets. Call the physician if pain persists after three tablets. 4. Take one tablet. If pain persists after 5 minutes, take two tablets. If pain still persists 5 minutes later, call the physician. 24) Which of the following arteries primarily feeds the anterior wall of the heart?
1. Circumflex artery 2. Internal mammary artery 3. Left anterior descending artery 4. Right coronary artery 25) When do coronary arteries primarily receive blood flow? 1. During inspiration 2. During diastolic 3. During expiration 4. During systole 26) Prolonged occlusion of the right coronary artery produces an infarction in which of the following areas of the heart? 1. Anterior 2. Apical 3. Inferior 4. Lateral 27) A murmur is heard at the second left intercostal space along the left sternal border. Which valve is this? 1. Aortic 2. Mitral 3. Pulmonic 4. Tricupsid 28) Which of the following blood tests is most indicative of cardiac damage? 1. Lactate dehydrogenase 2. Complete blood count (CBC) 3. Troponin I 4. Creatine kinase (CK) 29) Which of the following diagnostic tools is most commonly used to determine the location of myocardial damage? 1. Cardiac catherization 2. Cardiac enzymes 3. Echocardiogram 4. Electrocardiogram (ECG) 30) Which of the following types of pain is most characteristic of angina? 1. Knifelike 2. Sharp 3. Shooting 4. Tightness 31) Which of the following parameters is the major determinate of diastolic blood pressure? 1. Baroreceptors 2. Cardiac output
3. Renal function 4. Vascular resistance 32) Which of the following factors can cause blood pressure to drop to normal levels? 1. Kidneys excretion of sodium only 2. Kidneys retention of sodium and water 3. Kidneys excretion of sodium and water 4. Kidneys retention of sodium and excretion of water 33) Baroreceptors in the carotid artery walls and aorta respond to which of the following conditions? 1. Changes in blood pressure 2. Changes in arterial oxygen tension 3. Changes in arterial carbon dioxide tension 4. Changes in heart rate 34) Which of the following terms describes the force against which the ventricle must expel blood? 1. Afterload 2. Cardiac output 3. Overload 4. Preload 35) Which of the following terms is used to describe the amount of stretch on the myocardium at the end of diastole? 1. Afterload 2. Cardiac index 3. Cardiac output 4. Preload 36) A 57-year-old client with a history of asthma is prescribed propanolol (Inderal) to control hypertension. Before administered propranolol, which of the following actions should the nurse take first? 1. Monitor the apical pulse rate 2. Instruct the client to take medication with food 3. Question the physician about the order 4. Caution the client to rise slowly when standing. 37) One hour after administering IV furosemide (Lasix) to a client with heart failure, a short burst of ventricular tachycardia appears on the cardiac monitor. Which of the following electrolyte imbalances should the nurse suspect? 1. Hypocalcemia 2. Hypermagnesemia 3. Hypokalemia 4. Hypernatremia 38) A client is receiving spironolactone to treat hypertension. Which of the following instructions should the nurse provide?
1. Eat foods high in potassium. 2. Take daily potassium supplements. 3. Discontinue sodium restrictions. 4. Avoid salt substitutes. 39) When assessing an ECG, the nurse knows that the P-R interval represents the time it takes for the: 1. Impulse to begin atrial contraction 2. Impulse to transverse the atria to the AV node 3. SA node to discharge the impulse to begin atrial depolarization 4. Impulse to travel to the ventricles 40) Following a treadmill test and cardiac catheterization, the client is found to have coronary artery disease, which is inoperative. He is referred to the cardiac rehabilitation unit. During his first visit to the unit he says that he doesnt understand why he needs to be there because there is nothing that can be done to make him better. The best nursing response is: 1. Cardiac rehabilitation is not a cure but can help restore you to many of your former activities. 2. Here we teach you to gradually change your lifestyle to accommodate your heart disease. 3. You are probably right but we can gradually increase your activities so that you can live a more active life. 4. Do you feel that you will have to make some changes in your life now? 41) To evaluate a clients condition following cardiac catheterization, the nurse will palpate the pulse: 1. In all extremities 2. At the insertion site 3. Distal to the catheter insertion 4. Above the catheter insertion 42) A clients physician orders nuclear cardiography and makes an appointment for a thallium scan. The purpose of injecting radioisotope into the bloodstream is to detect: 1. Normal vs. abnormal tissue 2. Damage in areas of the heart 3. Ventricular function 4. Myocardial scarring and perfusion 43) A client enters the ER complaining of severe chest pain. A myocardial infarction is suspected. A 12 lead ECG appears normal, but the doctor admits the client for further testing until cardiac enzyme studies are returned. All of the following will be included in the nursing care plan. Which activity has the highest priority? 1. Monitoring vital signs 2. Completing a physical assessment 3. Maintaining cardiac monitoring 4. Maintaining at least one IV access site 44) A client is experiencing tachycardia. The nurses understanding of the physiological basis for this symptom is explained by which of the following statements?
1. The demand for oxygen is decreased because of pleural involvement 2. The inflammatory process causes the body to demand more oxygen to meet its needs. 3. The heart has to pump faster to meet the demand for oxygen when there is lowered arterial oxygen tension. 4. Respirations are labored. 45) A client enters the ER complaining of chest pressure and severe epigastric distress. His VS are 158/90, 94, 24, and 99*F. The doctor orders cardiac enzymes. If the client were diagnosed with an MI, the nurse would expect which cardiac enzyme to rise within the next 3 to 8 hours? 1. Creatine kinase (CK or CPK) 2. Lactic dehydrogenase (LDH) 3. LDH-1 4. LDH-2 46) A 45-year-old male client with leg ulcers and arterial insufficiency is admitted to the hospital. The nurse understands that leg ulcers of this nature are usually caused by: 1. Decreased arterial blood flow secondary to vasoconstriction 2. Decreased arterial blood flow leading to hyperemia 3. Atherosclerotic obstruction of the arteries 4. Trauma to the lower extremities 47) Which of the following instructions should be included in the discharge teaching for a patient discharged with a transdermal nitroglycerin patch? 1. Apply the patch to a nonhairy, nonfatty area of the upper torso or arms. 2. Apply the patch to the same site each day to maintain consistent drug absorption. 3. If you get a headache, remove the patch for 4 hours and then reapply. 4. If you get chest pain, apply a second patch right next to the first patch. 48) In order to prevent the development of tolerance, the nurse instructs the patient to: 1. Apply the nitroglycerin patch every other day 2. Switch to sublingual nitroglycerin when the patients systolic blood pressure elevates to >140 mm Hg 3. Apply the nitroglycerin patch for 14 hours each and remove for 10 hours at night 4. Use the nitroglycerin patch for acute episodes of angina only 49) Direct-acting vasodilators have which of the following effects on the heart rate? 1. Heart rate decreases 2. Heart rate remains significantly unchanged 3. Heart rate increases 4. Heart rate becomes irregular 50) When teaching a patient why spironolactone (Aldactone) and furosemide (Lasix) are prescribed together, the nurse bases teaching on the knowledge that: 1. Moderate doses of two different types of diuretics are more effective than a large dose of one type 2. This combination promotes diuresis but decreases the risk of hypokalemia 3. This combination prevents dehydration and hypovolemia
4. Using two drugs increases osmolality of plasma and the glomerular filtration rate ANSWERS 1. 4. This procedure requires an informed consent because it involves injection of a radiopaque dye into the blood vessel. The risk of allergic reaction and possible anaphylaxis is serious and must be assessed before the procedure. 2. 3. Chest pain is assessed by using the standard pain assessment parameters. Options 1, 2, and 4 may or may not help discriminate the origin of pain. Pain of pleuropulmonary origin usually worsens on inspiration. 3. 2. On transfer from the CCU, the client is allowed self-care activities and bathroom privileges. Supervised ambulation for brief distances are encouraged, with distances gradually increased (50, 100, 200 feet). 4. 1. Edema, the accumulation of excess fluid in the interstitial spaces, can be measured by intake greater than output and by a sudden increase in weight. Diuretics should be given in the morning whenever possible to avoid nocturia. Strict sodium restrictions are reserved for clients with severe symptoms. 5. 1. Sudden loss of electrocardiogram complexes indicates ventricular asystole or possible electrode displacement. Accurate assessment of the client and equipment is necessary to determine the cause and identify the appropriate intervention. 6. 4. BP should be taken with the client seated with the arm bared, positioned with support and at heart level. The client should sit with the legs on the floor, feet uncrossed, and not speak during the recording. The client should not have smoked tobacco or taken in caffeine in the 30 minutes preceding the measurement. The client should rest quietly for 5 minutes before the reading is taken. The cuff bladder should encircle at least 80% of the limb being measured. Gauges other than a mercury sphygmomanometer should be calibrated every 6 months to ensure accuracy. 7. 4. The antidote to heparin is protamine sulfate and should be readily available for use if excessive bleeding or hemorrhage should occur. Vitamin K is an antidote for warfarin. 8. 3. The therapeutic range for prothrombin time is 1.5 to 2 times the control for clients at risk for thrombus. Based on the clients control value, the therapeutic range for this individual would be 16.5 to 22 seconds. Therefore the result is within therapeutic range. 9. 2. Warfarin works in the liver and inhibits synthesis of four vitamin K-dependent clotting factors (X, IX, VII, and II), but it takes 3 to 4 days before the therapeutic effect of warfarin is exhibited. 10. 1. Although obtaining the ECG, chest x-ray, and blood work are all important, the nurses priority action would be to relieve the crushing chest pain. 11. 2. Thrombolytic drugs are administered within the first 6 hours after onset of a MI to lyse clots and reduce the extent of myocardial damage. 12. 1, 3, 5. In a client who has had an ECG, the P wave represents the activation of the electrical impulse in the SA node, which is then transmitted to the AV node. In addition, the P wave represents atrial muscle depolarization, not ventricular depolarization. The normal duration of the P wave is 0.11 seconds or less in duration and 2.5 mm or more in height. 13. 2. Advanced cardiac life support recommends that at least one or two intravenous lines be inserted in one or both of the antecubital spaces. Calling the physician, obtaining a portable chest radiograph, and drawing blood are important but secondary to starting the intravenous line.
14. 4. Detection of myoglobin is one diagnostic tool to determine whether myocardial damage has occurred. Myoglobin is generally detected about one hour after a heart attack is experienced and peaks within 4 to 6 hours after infarction (Remember, less than 90 mg/L is normal). 15. 1. Propranolol hydrochloride is a beta-adrenergic blocking agent. Actions of propranolol hydrochloride include reducing heart rate, decreasing myocardial contractility, and slowing conduction. 16. 3. Compliance is the most critical element of hypertensive therapy. In most cases, hypertensive clients require lifelong treatment and their hypertension cannot be managed successfully without drug therapy. Stress management and weight management are important components of hypertension therapy, but the priority goal is related to compliance. 17. 1. Hypertension is referred to as the silent killer for adults, because until the adult has significant damage to other systems, the hypertension may go undetected. CVAs can be related to long-term hypertension. Liver or pulmonary disease is generally not associated with hypertension. Myocardial infarction is generally related to coronary artery disease. 18. 3. Nitroglycerin may be used prophylactically before stressful physical activities such as stair climbing to help the client remain pain free. Visiting her friend early in the day would have no impact on decreasing pain episodes. Resting before or after an activity is not as likely to help prevent an activity-related pain episode. 19. 1. The client should report a change in the pattern of chest pain. It may indicate increasing severity of CAD. 20. 2. Cardiac catherization is done in clients with angina primarily to assess the extent and severity of the coronary artery blockage, A decision about medical management, angioplasty, or coronary artery bypass surgery will be based on the catherization results. 21. 3. Nitroglycerin produces peripheral vasodilation, which reduces myocardial oxygen consumption and demand. Vasodilation in coronary arteries and collateral vessels may also increase blood flow to the ischemic areas of the heart. Nitroglycerin decreases myocardial oxygen demand. Nitroglycerin does not have an effect on pericardial spasticity or conductivity in the myocardium. 22. 1. Because of the widespread vasodilating effects, nitroglycerin often produces such side effects as headache, hypotension, and dizziness. The client should lie or shit down to avoid fainting. Nitro does not cause shortness of breath or stomach cramps. 23. 3. The correct protocol for nitroglycerin used involves immediate administration, with subsequent doses taken at 5-minute intervals as needed, for a total dose of 3 tablets. Sublingual nitroglycerin appears in the blood stream within 2 to 3 minutes and is metabolized within about 10 minutes. 24. 3. The left anterior descending artery is the primary source of blood flow for the anterior wall of the heart. The circumflex artery supplies the lateral wall, the internal mammary supplies the mammary, and the right coronary artery supplies the inferior wall of the heart. 25. 2. Although the coronary arteries may receive a minute portion of blood during systole, most of the blood flow to coronary arteries is supplied during diastole. Breathing patterns are irrelevant to blood flow. 26. 3. The right coronary artery supplies the right ventricle, or the inferior portion of the heart. Therefore, prolonged occlusion could produce an infarction in that area. The right coronary artery doesnt supply the anterior portion (left ventricle), lateral portion (some of the left ventricle and the left atrium), or the apical portion (left ventricle) of the heart.
27. 3. Abnormalities of the pulmonic valve are auscultated at the second left intercostal space along the left sternal border. Aortic valve abnormalities are heard at the second intercostal space, to the right of the sternum. Mitral valve abnormalities are heard at the fifth intercostal space in the midclavicular line. Tricupsid valve abnormalities are heard at the 3rd and 4th intercostal spaces along the sternal border. 28. 3. Troponin I levels rise rapidly and are detectable within 1 hour of myocardial injury. Troponin levels arent detectable in people without cardiac injury. 29. 4. The ECG is the quickest, most accurate, and most widely used tool to determine the location of myocardial infarction. Cardiac enzymes are used to diagnose MI but cant determine the location. An echocardiogram is used most widely to view myocardial wall function after an MI has been diagnosed. Cardiac catherization is an invasive study for determining coronary artery disease and may also indicate the location of myocardial damage, but the study may not be performed immediately. 30. 4. The pain of angina usually ranges from a vague feeling of tightness to heavy, intense pain. Pain impulses originate in the most visceral muscles and may move to such areas as the chest, neck, and arms. 31. 4. Vascular resistance is the impedance of blood flow by the arterioles that most predominantly affects the diastolic pressure. Cardiac output determines systolic blood pressure. 32. 3. The kidneys respond to a rise in blood pressure by excreting sodium and excess water. This response ultimately affects systolic pressure by regulating blood volume. 33. 1. Baroreceptors located in the carotid arteries and aorta sense pulsatile pressure. Decreases in pulsatile pressure cause a reflex increase in heart rate. Chemoreceptors in the medulla are primarily stimulated by carbon dioxide. Peripheral chemoreceptors in the aorta and carotid arteries are primarily stimulated by oxygen. 34. 1. Afterload refers to the resistance normally maintained by the aortic and pulmonic valves, the condition and tone of the aorta, and the resistance offered by the systemic and pulmonary arterioles. Cardiac output is the amount of blood expelled from the heart per minute. Overload refers to an abundance of circulating volume. Preload is the volume of blood in the ventricle at the end of diastole. 35. 4. Preload is the amount of stretch of the cardiac muscle fibers at the end of diastole. The volume of blood in the ventricle at the end of diastole determines the preload. Afterload is the force against which the ventricle must expel blood. Cardiac index is the individualized measurement of cardiac output, based on the clients body surface area. Cardiac output is the amount of blood the heart is expelling per minute. 36. 3. Propranolol and other beta-adrenergic blockers are contraindicated in a client with asthma, so the nurse should question the physician before giving the dose. The other responses are appropriate actions for a client receiving propranolol, but questioning the physician takes priority. The clients apical pulse should always be checked before giving propranolol; if the pulse rate is extremely low, the nurse should withhold the drug and notify the physician. 37. 3. Furosemide is a potassium-depleting diuretic than can cause hypokalemia. In turn, hypokalemia increases myocardial excitability, leading to ventricular tachycardia. 38. 4. Because spironolactone is a potassium-sparing diuretic, the client should avoid salt substitutes because of their high potassium content. The client should also avoid potassiumrich foods and potassium supplements. To reduce fluid-volume overload, sodium restrictions should continue.
39. 4. The P-R interval is measured on the ECG strip from the beginning of the P wave to the beginning of the QRS complex. It is the time it takes for the impulse to travel to the ventricle. 40. 1. Such a response does not have false hope to the client but is positive and realistic. The answer tells the client what cardiac rehabilitation is and does not dwell upon his negativity about it. 41. 3. Palpating pulses distal to the insertion site is important to evaluate for thrombophlebitis and vessel occlusion. They should be bilateral and strong. 42. 4. This scan detects myocardial damage and perfusion, an acute or chronic MI. It is a more specific answer than (1) or (2). Specific ventricular function is tested by a gated cardiac blood pool scan. 43. 3. Even though initial tests seem to be within normal range, it takes at least 3 hours for the cardiac enzyme studies to register. In the meantime, the client needs to be watched for bradycardia, heart block, ventricular irritability, and other arrhythmias. Other activities can be accomplished around the MI monitoring. 44. 3. The arterial oxygen supply is lowered and the demand for oxygen is increased, which results in the hearts having to beat faster to meet the bodys needs for oxygen. 45. 1. Creatine kinase (CK, formally known as CPK) rises in 3-8 hours if an MI is present. When the myocardium is damaged, CPK leaks out of the cell membranes and into the blood stream. Lactic dehydrogenase rises in 24-48 hours, and LDH-1 and LDH-2 rises in 8-24 hours. 46. 1. Decreased arterial flow is a result of vasospasm. The etiology is unknown. It is more problematic in colder climates or when the person is under stress. Hyperemia occurs when the vasospasm is relieved. 47. 1. A nitroglycerin patch should be applied to a nonhairy, nonfatty area for the best and most consistent absorption rates. Sites should be rotated to prevent skin irritation, and the drug should be continued if headache occurs because tolerance will develop. Sublingual nitroglycerin should be used to treat chest pain. 48. 3. Tolerance can be prevented by maintaining an 8- to 12-hour nitrate-free period each day. 49. 3. Heart rate increases in response to decreased blood pressure caused by vasodilation. 50. 2. Spironolactone is a potassium-sparing diuretic; furosemide is a potassium-loosing diuretic. Giving these together minimizes electrolyte imbalance.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- U.S. Food & Drug Administration: 10903 New Hampshire Avenue Silver Spring, MD 20993Dokumen19 halamanU.S. Food & Drug Administration: 10903 New Hampshire Avenue Silver Spring, MD 20993Aagam ShahBelum ada peringkat
- Bci-Cat-9200 Advisor Vital Signs MonitorDokumen2 halamanBci-Cat-9200 Advisor Vital Signs MonitorAbraham AlmirudisBelum ada peringkat
- Cardiac MonitoringDokumen138 halamanCardiac Monitoringanjanar26Belum ada peringkat
- Physical Activity and Exercise During Pregnancy and The Postpartum PeriodDokumen11 halamanPhysical Activity and Exercise During Pregnancy and The Postpartum Periodfariska amanizataBelum ada peringkat
- Anesthesia Hub - QuestionsDokumen15 halamanAnesthesia Hub - QuestionsMedicine Agency100% (3)
- Overview of Hypertension in Acute and Chronic Kidney Disease - UpToDateDokumen8 halamanOverview of Hypertension in Acute and Chronic Kidney Disease - UpToDateNiñoTanBelum ada peringkat
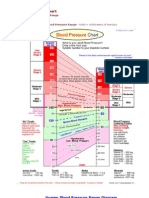
- Blood Pressure ChartDokumen5 halamanBlood Pressure Chartmahajan1963100% (1)
- Running Head: The Effects of Earthing/Grounding On Sleep 1Dokumen16 halamanRunning Head: The Effects of Earthing/Grounding On Sleep 1api-529971768Belum ada peringkat
- Surrogate Endpoints in Clinical ResearchDokumen14 halamanSurrogate Endpoints in Clinical ResearchSIRO Clinical Research InstituteBelum ada peringkat
- Shock HypovolemicDokumen16 halamanShock HypovolemicTitinBelum ada peringkat
- Seminar - Heart FailuerDokumen19 halamanSeminar - Heart Failuermustafalotfy01Belum ada peringkat
- Inadvertent Overinfusion of Norepinephrine Using Infusion Pump Loading Dose 2015 Intensive and Critical Care NursingDokumen5 halamanInadvertent Overinfusion of Norepinephrine Using Infusion Pump Loading Dose 2015 Intensive and Critical Care NursingJose J.Belum ada peringkat
- Management of Intradialytic Hypertension: The Ongoing ChallengeDokumen6 halamanManagement of Intradialytic Hypertension: The Ongoing ChallengeSari ChaerunisahBelum ada peringkat
- Validation of A New Tool For The Assessment of Study Quality and Reporting in Exercise Training Studies: TestexDokumen10 halamanValidation of A New Tool For The Assessment of Study Quality and Reporting in Exercise Training Studies: TestexMatias Santis OlivaresBelum ada peringkat
- Vedavaani-A Gurukulam ProjectDokumen98 halamanVedavaani-A Gurukulam ProjectDr Suvarna NalapatBelum ada peringkat
- Cor PulmonaleDokumen62 halamanCor PulmonaleAlbert NixonBelum ada peringkat
- QynetiQ Enterprise - User Manual 1.5 (EN) PDFDokumen122 halamanQynetiQ Enterprise - User Manual 1.5 (EN) PDFUlly Rochaya PrabandariBelum ada peringkat
- MCN CH 17Dokumen14 halamanMCN CH 17Kristine KrisBelum ada peringkat
- Ecg Short Rapid ReviewDokumen54 halamanEcg Short Rapid ReviewSilviaSumintoBelum ada peringkat
- NCP Preeclampsia and EclampsiaDokumen16 halamanNCP Preeclampsia and EclampsiaBiway Regala100% (1)
- Peel 1996 - Cardiopulmonary System and Movement DysfunctionDokumen8 halamanPeel 1996 - Cardiopulmonary System and Movement DysfunctionBeto ZamunérBelum ada peringkat
- Risk Factors Pathophysiology and Management of HypertensionDokumen13 halamanRisk Factors Pathophysiology and Management of HypertensionDominggas RusunwullyBelum ada peringkat
- Cardiovascular Responses To Static ExerciseDokumen7 halamanCardiovascular Responses To Static Exercisesilvio da costa guerreiroBelum ada peringkat
- Pet Ownership and Cardiovascular Risk (2013) PDFDokumen11 halamanPet Ownership and Cardiovascular Risk (2013) PDFMario Salgado ChávezBelum ada peringkat
- Pediatrics 2004 555 76Dokumen24 halamanPediatrics 2004 555 76utarinuBelum ada peringkat
- Journal Pre-Proof: Clinical Epidemiology and Global HealthDokumen17 halamanJournal Pre-Proof: Clinical Epidemiology and Global HealthYurisma KhoerulBelum ada peringkat
- Post-Mortem Care NotesDokumen3 halamanPost-Mortem Care NotesAleah JayaganBelum ada peringkat
- NCD High-Risk Assessment (Community Case Finding Form) NCD High-Risk Assessment (Community Case Finding Form)Dokumen1 halamanNCD High-Risk Assessment (Community Case Finding Form) NCD High-Risk Assessment (Community Case Finding Form)Claribel Domingo BayaniBelum ada peringkat
- Chpater 8 Pension & WelfareDokumen54 halamanChpater 8 Pension & WelfareSami Ur RehmanBelum ada peringkat
- DR - Mangala Gowri S R PDFDokumen107 halamanDR - Mangala Gowri S R PDFNepoo ChiBelum ada peringkat