Pe in Raised Icp
Diunggah oleh
lydia_chandraDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Pe in Raised Icp
Diunggah oleh
lydia_chandraHak Cipta:
Format Tersedia
Chapter 189 Papilledema and Raised Intracranial Pressure
ALFREDO A. SADUN
DEFINITION
Optic disc edema, usually bilateral, that results from increased intracranial pressure.
KEY FEATURES
Blurring of the optic disc margins.
Anterior extension of the nerve head.
Venous congestion of arcuate and peripapillary vessels.
Hyperemia of the optic nerve head.
ASSOCIATED FEATURES
Gross elevation of the optic nerve head.
Engorged and dusky veins.
Peripapillary splinter hemorrhages.
Choroidal folds.
Retina striae.
INTRODUCTION
About 1.2 million axons converge at the optic disc to form the optic nerve. The optic nerve follows a 50?mm course as it extends from the back of the eye, travels through the orbit, passes through the optic canal, runs intracranially, and partially decussates along with the contralateral optic nerve to form the optic chiasm. Each axon must maintain active axonal transport in both the orthograde (eye to brain) and retrograde directions. The subarachnoid space of the brain is continuous with the optic nerve sheath. An extensive litany of insults may lead to dysfunction or compression of the optic nerve, which may cause a partial arrest of axoplasmic transport and result in optic disc edema. If the compression is caused by raised intracranial pressure, the condition is termed papilledema. The term, papilledema, carries neurological and neurosurgical connotations. If the cause of the disc edema is not increased intracranial pressure, the term optic disc edema should be used instead of papilledema. Long-standing or severe papilledema, in addition to reflecting intracranial pathology, also may result in bilateral optic nerve dysfunction because of compromise of axonal integrity at the lamina cribrosa.
EPIDEMIOLOGY AND PATHOGENESIS
Tumors of the brain may be benign or malignant, and primary or metastatic. All may cause a rise in intracranial pressure. About 100,000 patients a year in the United States die with intracranial masses (most with metastatic disease). Although tumors of the posterior fossa are very likely to cause obstruction of cerebral spinal fluid flow between the ventricles, most cases of increased intracranial pressure in adults arise from large hemispheric masses.
Patients may suffer from many of the features of intracranial tumors in the absence of any mass lesion. Pseudotumor cerebri (PTC), also termed idiopathic intracranial hypertension, requires that neuroimaging prove negative for mass lesions and obstruction of the ventricular system, and that a lumbar puncture prove positive for high pressure although the fluid is normal in composition.
PTC is a syndrome that is much more likely to be a cause of increased intracranial pressure and hence papilledema among young adults than real tumor. This syndrome has several features that characterize it. The only initial symptom may be a headache, which tends to be worst when recumbent. There is usually an absence of any neurological signs other than visual loss, although a sixth cranial nerve palsy is
not rare. Irreversible visual loss from chronic papilledema is the all-too-common sequela (about 50% of cases) that must be avoided. PTC is usually idiopathic, but it may be seen in association with certain drugs and agents and in particular types of patients. One well understood cause of PTC is from intracranial venous thrombosis which may be subsequent to head trauma. Historically, a common cause of intracranial venous thrombosis was otitis media with mastoiditis.
Drugs such as tetracycline, nalidixic acid, corticosteroids (or more commonly steroid withdrawal), or vitamin A may produce PTC. Patients with hypoparathyroidism and adrenal adenomas are more likely to develop PTC. Chronic respiratory insufficiency, renal syndrome, and iron deficiency anemia also have been associated with PTC.
In the majority of cases, however, no etiological factor can be found for PTC. Most patients are obese young women, and there is a suggestion that there is an endocrine abnormality at the basis of the disorder.
Like glaucoma, increased intracranial pressure can be consequent to an increased production of fluid or to a decrease in outflow facility. Many investigators feel that most causes of PTC involve increased resistance to cerebrospinal fluid drainage.
Most patients (8090%) with PTC seek treatment for a headache. Less often, visual disturbances bring the patient to medical attention. The patient may complain of decreased visual acuity, transient obscuration of visions, an enlarged blind spot, or diplopia (due to sixth cranial nerve palsy).
The sixth cranial nerve palsy is a nonspecific sign of increased intracranial pressure and resolves following a decrease in the intracranial pressure. Permanent impairments produced by PTC are those resulting from chronic papilledema.
Obstruction of the ventricular system, or shunt failure in an individual in whom a ventricular or lumbar peritoneal shunt has been placed previously, may lead to a very rapid rise in intracranial pressure and fulminant papilledema.
The principal pathophysiology of optic disc swelling is blockage of axoplasmic transport. Axoplasmic transport is the movement of materials responsible for maintaining the axon, primarily proteins and
organelles formed in the neuronal soma and transported along the axon. Axonal transport may depend on the microtubules that act as railroad tracks. Orthograde axoplasmic transport can be slow or rapid. The former occurs at 0.53.0?mm per day, and rapid flow at 2001000?mm per day. In addition, retrograde axoplasmic transport also occurs.[1] Mechanical and vascular causes can combine to produce a blockage of optic nerve axoplasmic flow. Such blockage at the level of the lamina choroidalis
1260
and lamina scleralis occurs when optic disc edema is produced experimentally through increased intracranial pressure, ocular hypotony, or increased intraocular pressure. It is felt that local factors produce a stasis of axoplasmic flow. Optic disc edema also may be produced by an event that increases venous pressure at or near the lamina cribrosa,[2] [3] [4] [5] such as occurs secondary to intrinsic tumors or extrinsic orbital masses, or by abnormalities in blood flow such as central retinal vein occlusion (CRVO).
OCULAR MANIFESTATIONS
Papilledema is observed on fundus examination, usually by direct ophthalmoscopy performed both with the standard (white) and red-free light (to better visualize the nerve fiber layer). Indirect ophthalmoscopy with a 20D lens provides a better stereoscopic view, but it is even better with the higher magnification of the 14D. A 90D lens used in conjunction with biomicroscopy is excellent. It is useful to characterize the changes in the optic nerve head that occur in papilledema as being mechanical or vascular in nature. The five mechanical clinical signs of optic disc edema are:
Blurring of the optic disc margins
Filling in of the optic disc cup
Anterior extension of the nerve head (3D = 1?mm of elevation)
Edema of the nerve fiber layer
Retinal or choroidal folds (or both)
The five vascular clinical signs of optic disc edema are venous congestion of arcuate and peripapillary vessels, papillary and retinal peripapillary hemorrhages, nerve fiber layer infarcts (cotton-wool spots), hyperemia of the optic nerve head, and hard exudates of the optic disc.
In addition, elements of optic disc swelling can be used to help characterize the papilledema as early, fully developed, chronic, or late. In early papilledema disc hyperemia, disc swelling, blurring of the disc margins, and blurring of the nerve fiber layer are found ( Fig. 189-1 ). In fully developed papilledema gross elevation of the optic nerve head and engorged and dusky
Figure 189-1 Early papilledema. The optic disc of an 18-year-old man 2 weeks after he had complained of diplopia arising from sixth cranial nerve palsies caused by increased intracranial pressure. Note the minimal evidence of edema.
Figure 189-2 Developed papilledema. The optic disc of a 36-year-old woman who suffered headache and blurred vision for 2 months. Fully developed disc edema presentnote the engorged veins and peripapillary hemorrhages.
veins appear, peripapillary splinter hemorrhages and sometimes choroidal folds arise, and retina striae are seen ( Fig. 189-2 ). In chronic papilledema fewer hemorrhages occur, the optic disc cup is obliterated completely, less disc hyperemia is seen, and hard exudates occur within the nerve head ( Fig. 189-3 ). In late disc edema secondary optic atrophy occurs, disc swelling subsides, retinal arterioles are narrowed or sheathed, and the optic disc appears dirty gray and blurred, secondary to gliosis ( Fig. 189-4 ).
Symptoms of increased intracranial pressure include headache and brief transient obscurations of vision. Less commonly, the patient may describe blurred vision, constriction of visual fields, dyschromatopsia, and diplopia.
The headache of increased intracranial pressure usually is quite distinctive (see Chapter 204 ). Cause for concern exists if the headache is particularly severe or associated with nausea and vomiting or a sense of pressure around the ears. This concern is heightened if the headache becomes worse in a recumbent position or is worst in the early morning, when the patient wakes up, but improves during the day. Even more specific are the transient obscurations of vision, usually described as monocular or binocular blackouts, that last 34 seconds and most often occur as the patient arises from the recumbent position to sitting or standing.[6] Papilledema may produce visual blurring because of enlargement of the blind spot and adjacent retinal folds or edema; this blurring usually is reversible. However, further injury to the optic nerve may be associated with secondary optic atrophy and be permanent, which results in symptoms such as constricted visual fields and poor color vision. Diplopia usually arises from nonlocalizing sixth cranial nerve palsies, and it often resolves after the increased intracranial pressure has been controlled.
DIAGNOSIS AND TESTING
An index of suspicion for papilledema is provided by the history. A careful fundus examination is mandatory. The optic nerve
Figure 189-3 Chronic papilledema. Severe and chronic disc edema in a 27-year-old, very obese woman who has pseudotumor cerebri. Note that the disc cusp is obliterated and hard exudates are present.
Figure 189-4 Secondary optic atrophy from chronic papilledema. The same 27-year-old obese female patient 5 months later. Note the secondary optic atrophy has developed fully. The disc margins appear hazy or dirty.
1261
head is assessed for each of the ten signs of disc edema described above and the papilledema characterized not only as mild, moderate, or severe, but also as early, developed, late, or chronic. A careful procedure is instituted to determine whether the disc edema is, in fact, papilledema; this usually begins with neuroimaging followed by, in most cases, a lumbar puncture with manometry.
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of papilledema is disc edema without increased intracranial pressure and pseudopapilledema. The latter rubric includes all abnormalities of the optic disc that can mimic optic disc edema. The most common of such disc anomalies are optic disc drusen which, especially when deeply buried, may give the disc a lumpy, elevated appearance. However, very few, if any, of the other nine signs of disc edema mentioned above apply. Other causes of optic disc edema without increased intracranial pressure need to be consideredcompressive optic neuropathies, papillitis, anterior ischemic optic neuropathy, CRVO, juvenile diabetic papillopathy, and optic disc vasculitis.[7]
Compressive Optic Neuropathies
Compressive optic neuropathies that may produce disc edema often are located in the anterior orbit. Neoplasms of the optic nerve itself (gliomas) or of its sheaths (meningiomas), or masses from the orbital tissues or paranasal sinuses, may impinge on the anterior optic nerve and result in disc edema. Inflammatory and infiltrative lesions also may manifest as masses. Distal malignancies also may involve the optic nerve and its sheaths by metastasis.
Papillitis
Papillitis often has a component of disc edema and frequently follows a prodromal viral illness. The inflammation may extend beyond the confines of the optic disc and may develop into a neuroretinitis. Cells are found frequently in the vitreous humor; retinal exudates may form a star or a half-star figure between the disc and the macula. Both papillitis and neuroretinitis are seen often in young, healthy adults.
Anterior Ischemic Optic Neuropathy
Anterior ischemic optic neuropathy usually demonstrates sectorial disc edema and peripapillary hemorrhages. An acute loss of vision occurs and the visual field deficit may take on an altitudinal shape. Anterior ischemic optic neuropathy is found most often in patients of age 5075 years and who have hypertension or diabetes.[8]
Central Retinal Vein Occlusion
CRVO or impending CRVO also may result in congestion in the optic nerve heads. However, the extensive hemorrhages found in CRVO usually make the differentiation easy. Generally, CRVOs occur in middle-aged or older individuals who have hypertension or, less often, hyperviscosity syndrome.
Juvenile Diabetic Papillopathy
Juvenile diabetic papillopathy includes unilateral or bilateral disc edema in its manifestations. The loss of vision usually is minimal, and the visual fields may show peripheral constriction or central scotomas. The fundus examination often reveals dilated telangiectatic vessels over the discs, which appears very much like optic disc neovascularization, but these disappear when the disc edema resolves spontaneously 48 weeks later.[8]
Optic Disc Vasculitis
Optic disc vasculitis, or (more globally) uveitis, also may result in optic disc edema. Papillophlebitis, optic disc vasculitis, benign retinal vasculitis, and the big blind-spot syndrome may be considered variations on this theme. These conditions often develop in young, healthy adults who have only minimal visual impairment. The optic disc edema usually occurs in association with engorged retinal veins and occasionally with retinal hemorrhages.
Other Causes
Other causes of disc edema include advanced Graves disease, malignant hypertension, and hypotony. Malignant processes, such as carcinoma, lymphoma, or leukemia,[9] as well as uremia[10] and sarcoid granuloma, also may cause swelling of the optic disc. Nutritional optic neuropathies, such as in tropical epidemics, and toxic optic neuropathies often caused by drugs, such as ethambutol, may result in mild disc edema.[11] Orbital or cranial trauma, radiation, and burns also may cause swelling of the optic discs.
SYSTEMIC ASSOCIATIONS
In addition to papilledema and the potential for visual loss, increased intracranial pressure can cause other signs and symptoms. However, the most serious and irreversible problems associated with increased intracranial pressure, per se, are visual; hence, the ophthalmologist is a critical member of the clinical team for such patients. Palsies of the sixth cranial nerve, hearing loss, and facial nerve palsies also are found, in decreasing order of frequency, in patients who have increased intracranial pressure. However, the cranial nerve palsies are likely to be self-limiting after reduction of the pressure. More often, patients who have increased intracranial pressure complain of headache, pressure in the ears, tinnitus, and fatigue, and sometimes, if severe, nausea and vomiting.
PATHOLOGY
The histopathology of acute optic disc edema reveals axoplasmic stasis, edema, and vascular congestion ( Fig. 189-5 ). Peripapillary hemorrhages are seen primarily in the retinal nerve fiber layer, but they may overlie the optic disc.[12] The increase in tissue mass fills the physiological cup and causes the optic nerve head to protrude anteriorly. The small blood vessels are engorged and tortuous. Vacuoles of extracellular fluid accumulate in and anterior to the retinal lamina cribrosa, and the subarachnoid space is enlarged with stretching of the subarachnoid strands. [12]
The neural retina is displaced away from the optic disc and the outer layer of the retina may be buckled (retinal folds). The rods and cones are displaced away obliquely from their anchor near Bruchs membrane. A shallow retinal detachment may occur in the peripapillary area.
Engorgement of axons in the laminar portion of the optic nerve is best demonstrated by electron microscopy. The swollen axons are filled with mitochondria primarily anterior to the choroidal lamina cribrosa. The mitochondria themselves appear swollen and disrupted, and the fascicles of microtubules also are in disarray. Importantly, the extracellular accumulation is minimal compared with the intracellular and intraaxonal accumulation.[13]
TREATMENT
The treatment of papilledema associated with visual loss depends in large part on the cause, symptoms, signs, and progression of the problem. Attempts must be made to redress the pathophysiology. However, a few comments on the general concepts are given here.
1262
Figure 189-5 Optic disc edema. A and B, Patient has bilateral optic disc edema secondary to grade IV malignant hypertension. B, Note exudates in nasal macula. C, Histological section shows optic disc edema secondary to ocular hypertension caused by phacolytic glaucoma. D, Optic disc edema secondary to ocular hypotony caused by a ruptured globe. Optic disc edema can be caused by increased intracranial pressure or increased or decreased intraocular pressure. The main findings in C and D consist of increased mass of anterior optic nerve caused by axonal swelling, optic nerve head tissue edema and vascular congestion, and lateral displacement of photoreceptors from the end of Bruchs membrane, which terminates in a ring at the optic nerve.
Medical treatment usually consists of repeated lumbar punctures and diuretics, especially carbonic anhydrase inhibitors and, in cases of pseudotumor, weight reduction.[14]
If medical treatment is not sufficient, optic nerve sheath decompression [15] [16] or a lumboperitoneal shunt[17] may need to be carried out. It is very important to understand that the decision to treat, or to
alter treatment modality, usually is based on the ophthalmologists descriptions of the extent of both optic disc edema and visual loss, as measured by such parameters as color vision or visual fields. Hence, the ophthalmologist is a crucial member of the clinical team that makes management decisions.
COURSE AND OUTCOMES
The prognosis for papilledema is largely dependent on the cause. Most patients who have metastatic brain tumors do very badly; those who have ventricular obstructive disease may be shunted successfully; patients who have pseudotumor usually can be managed quite well. Two general points warrant emphasis. The diagnosis of papilledema requires a prompt work-up until the most serious pathologies are ruled out. Here, neurological, neurosurgical, or neuroradiological consultation is required usually. However, once the problem has been reduced to that of papilledema only, the ophthalmologist can best determine how aggressive the course of management needs to be. All too often, permanent visual loss occurs in relatively benign diseases such as PTC for lack of appropriate ophthalmologic involvement.[14]
REFERENCES
1. Brady ST, Lasek RJ, Allen RD. Video microscopy for fast axonal transport of extruded axoplasm: a new model for study of molecular mechanisms. Cell Motil. 1985;5:81101.
2. Minckler DS, Bunt AH. Axoplasmic transport in ocular hypotony and papilledema in the monkey. Arch Ophthalmol. 1977;95:14306.
3. Hayreh MS, Hayreh SS. Optic disc edema in raised intracranial pressure. I. Evolution and resolution. Arch Ophthalmol. 1977;95:123744.
4. Tso MOM, Hayreh SS. Optic disc edema in raised intracranial pressure. III. A pathologic study of experimental papilledema. Arch Ophthalmol. 1977; 95:144857.
5. Hayreh SS. Optic disc edema in raised intracranial pressure. V. Pathogenesis. Arch Ophthalmol. 1977;95:155365.
6. Sadun AA, Currie JN, Lessell S. Transient visual obscurations with elevated optic discs. Ann Neurol. 1984;16:48994.
7. Sanders MD, Sennhenn RH. Differential diagnosis of unilateral optic disc edema. Trans Ophthalmol Soc U K. 1980;100:12331.
8. Glaser J. Neuro-ophthalmology, ed 2. Phila
Anda mungkin juga menyukai
- Differential Diagnosis of Papilledema - UpToDateDokumen28 halamanDifferential Diagnosis of Papilledema - UpToDateDaniel PadillaBelum ada peringkat
- Pa Pill EdemaDokumen13 halamanPa Pill Edemarutuparna383Belum ada peringkat
- Papiledema & Neuritis OpticDokumen42 halamanPapiledema & Neuritis OpticNadine Wang0% (1)
- The Optic NerveDokumen7 halamanThe Optic NerveEdwin DarmawanBelum ada peringkat
- Papilledema: Jump To Navigationjump To SearchDokumen4 halamanPapilledema: Jump To Navigationjump To SearchEri DooBelum ada peringkat
- General physical exam of neuro systemDokumen112 halamanGeneral physical exam of neuro systemSuganya BalachandranBelum ada peringkat
- Diseases of The Optic Nerve 09Dokumen25 halamanDiseases of The Optic Nerve 09somebody_maBelum ada peringkat
- Papilloedema 71Dokumen23 halamanPapilloedema 71Shivani NairBelum ada peringkat
- Cerebrovascular Diseases Risk Factors:: o o o o oDokumen4 halamanCerebrovascular Diseases Risk Factors:: o o o o otrinaBelum ada peringkat
- Optic Nerve: Applied AnatomyDokumen10 halamanOptic Nerve: Applied AnatomyMariam QaisBelum ada peringkat
- Proiect Nerv OpticDokumen7 halamanProiect Nerv Opticiuliabucur92Belum ada peringkat
- Cerebral Venous Thrombosis: Review ArticleDokumen6 halamanCerebral Venous Thrombosis: Review ArticlefabioBelum ada peringkat
- HYDROCEPHALUSDokumen17 halamanHYDROCEPHALUSSalim FatmaBelum ada peringkat
- Essential Ophthalmology NotesDokumen31 halamanEssential Ophthalmology NotesHashim Ahmad50% (2)
- Birth Traumas 1Dokumen34 halamanBirth Traumas 1PrernaSharmaBelum ada peringkat
- Stroke in ChildrenDokumen20 halamanStroke in ChildrenDiksha CheetooBelum ada peringkat
- Exophthalmos Is Defined in DorlandDokumen15 halamanExophthalmos Is Defined in DorlandAmin Kamaril Wahyudi ArrdianBelum ada peringkat
- Ward ClassDokumen4 halamanWard ClassJeyb BravoBelum ada peringkat
- Optic AtrophyDokumen40 halamanOptic Atrophypriya0% (1)
- RvoDokumen43 halamanRvoOrchlon LkBelum ada peringkat
- Birth Trauma TypesDokumen34 halamanBirth Trauma TypesIr Van NBelum ada peringkat
- Severe Hydrocephalus in an InfantDokumen22 halamanSevere Hydrocephalus in an InfantNina100% (2)
- Causes and Presentation of Peripheral Anterior SynechiaeDokumen11 halamanCauses and Presentation of Peripheral Anterior SynechiaeMarisa SukoBelum ada peringkat
- Retinopathy, Diabetic, BackgroundDokumen12 halamanRetinopathy, Diabetic, BackgroundmyusuffrBelum ada peringkat
- UWorld Notes Neurology: Spontaneous cerebellar hemorrhageDokumen6 halamanUWorld Notes Neurology: Spontaneous cerebellar hemorrhagesarahBelum ada peringkat
- Subdural HematomaDokumen7 halamanSubdural Hematomamiss RN50% (2)
- Neuro Bar Topics 1-68-1Dokumen122 halamanNeuro Bar Topics 1-68-1ahmedaznjadatBelum ada peringkat
- WHNODokumen96 halamanWHNOani3990Belum ada peringkat
- Food and CyanideDokumen2 halamanFood and CyanideeugeniarBelum ada peringkat
- NCP Rheum 0268Dokumen9 halamanNCP Rheum 0268drheriBelum ada peringkat
- Anesthesia For NeurosurgeryDokumen37 halamanAnesthesia For Neurosurgeryfauzybius35Belum ada peringkat
- Hydrocephalus2 Thumb Hydrocephalus: DefinitionDokumen7 halamanHydrocephalus2 Thumb Hydrocephalus: DefinitionVeulah TijamBelum ada peringkat
- Kabwe Central Hospital: "Hydrocephalus"Dokumen39 halamanKabwe Central Hospital: "Hydrocephalus"Emmanuel MukukaBelum ada peringkat
- Differential Diagnosis and StrokeDokumen38 halamanDifferential Diagnosis and StrokeAin AmanyBelum ada peringkat
- Birth Injuries 170507205454Dokumen60 halamanBirth Injuries 170507205454Vyshak KrishnanBelum ada peringkat
- Chapter 14. The Dizzy Patient The Dizzy Patient: IntroductionDokumen9 halamanChapter 14. The Dizzy Patient The Dizzy Patient: IntroductionjumabarrientosBelum ada peringkat
- Hydrocephalus: An Abnormal Buildup of Cerebrospinal Fluid in the BrainDokumen82 halamanHydrocephalus: An Abnormal Buildup of Cerebrospinal Fluid in the Brainmohd asadBelum ada peringkat
- Hydrocephalus and Spina Bifida GuideDokumen61 halamanHydrocephalus and Spina Bifida GuideAbdirahman Abdillahi FarahBelum ada peringkat
- Hypertension & End Organ DamageDokumen41 halamanHypertension & End Organ DamageTrushank PathakBelum ada peringkat
- Disorders of Optic Nerve and Visual Pathways: Ipek MidiDokumen24 halamanDisorders of Optic Nerve and Visual Pathways: Ipek MidiEcaterina ChiriacBelum ada peringkat
- Open Angle Glaucoma GuideDokumen24 halamanOpen Angle Glaucoma GuideJessica McCroryBelum ada peringkat
- OTITIC HYDROCEPHAlusDokumen7 halamanOTITIC HYDROCEPHAlusKuchh BhiiBelum ada peringkat
- Glaucoma Optic NerveDokumen8 halamanGlaucoma Optic NerveernawatiBelum ada peringkat
- CSF Imbalance Causes HydrocephalusDokumen32 halamanCSF Imbalance Causes HydrocephalusElvisBelum ada peringkat
- Case Pres - HydrocephalusDokumen26 halamanCase Pres - HydrocephalusJack Bisarra Sanchez100% (1)
- Pathology of CNS: Eric M. Mirandilla MD, DPSPDokumen71 halamanPathology of CNS: Eric M. Mirandilla MD, DPSPDhruva PatelBelum ada peringkat
- Epidural Hematom FersiDokumen11 halamanEpidural Hematom FersiMuhammad SolehBelum ada peringkat
- Hydrocephalus Could Attack Everyone in All AgeDokumen9 halamanHydrocephalus Could Attack Everyone in All AgeimildaBelum ada peringkat
- Anatomy and Physiology of EyeDokumen19 halamanAnatomy and Physiology of Eyeashwini priyaBelum ada peringkat
- Hydrocephalus: Dr. Deepa Khanal 3 Year Resident Pediatrics KMCTHDokumen36 halamanHydrocephalus: Dr. Deepa Khanal 3 Year Resident Pediatrics KMCTHar bindraBelum ada peringkat
- Sofia Margarita M. NicolasDokumen11 halamanSofia Margarita M. NicolasSofia MandacBelum ada peringkat
- Hydro Cep Hal UsDokumen11 halamanHydro Cep Hal UsEmmanuel MukukaBelum ada peringkat
- HYDROCEPHALOUSDokumen25 halamanHYDROCEPHALOUSSuman PoudelBelum ada peringkat
- Hydrocephalus UpdatesDokumen65 halamanHydrocephalus Updatescddinchimm100% (1)
- Neuro-Ophthalmology Review Authr Daniah AlshowaeirDokumen50 halamanNeuro-Ophthalmology Review Authr Daniah AlshowaeirRAJBelum ada peringkat
- Normal Eye With Sudden Decreased VisionDokumen38 halamanNormal Eye With Sudden Decreased VisionAnjar NuryantoBelum ada peringkat
- Topic - Neurosurgery From Medicine SimplifiedDokumen7 halamanTopic - Neurosurgery From Medicine SimplifiedDebzz PradhanBelum ada peringkat
- Traumatic Brain InJuryDokumen21 halamanTraumatic Brain InJuryShara SampangBelum ada peringkat
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtDari EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtPenilaian: 5 dari 5 bintang5/5 (1)
- Neurology Equations Made Simple: Differential Diagnosis and NeuroemergenciesDari EverandNeurology Equations Made Simple: Differential Diagnosis and NeuroemergenciesBelum ada peringkat
- GBS Edu Tool V3Dokumen43 halamanGBS Edu Tool V3lydia_chandraBelum ada peringkat
- DermaDokumen30 halamanDermalydia_chandraBelum ada peringkat
- Fluid ImbalanceDokumen5 halamanFluid Imbalancelydia_chandraBelum ada peringkat
- Dopa MinDokumen39 halamanDopa Minlydia_chandraBelum ada peringkat
- The Steriotypes: Cultural StereotypeDokumen8 halamanThe Steriotypes: Cultural StereotypeRosbeyli Mazara ReyesBelum ada peringkat
- Megha Rakheja Project ReportDokumen40 halamanMegha Rakheja Project ReportMehak SharmaBelum ada peringkat
- MinePlan Release NotesDokumen14 halamanMinePlan Release NotesJuanJo RoblesBelum ada peringkat
- Prac Research Module 2Dokumen12 halamanPrac Research Module 2Dennis Jade Gascon NumeronBelum ada peringkat
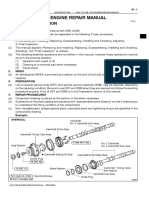
- How To Use This Engine Repair Manual: General InformationDokumen3 halamanHow To Use This Engine Repair Manual: General InformationHenry SilvaBelum ada peringkat
- 2010 Economics Syllabus For SHSDokumen133 halaman2010 Economics Syllabus For SHSfrimpongbenardghBelum ada peringkat
- IB Theatre: The Ilussion of InclusionDokumen15 halamanIB Theatre: The Ilussion of InclusionLazar LukacBelum ada peringkat
- Bpoc Creation Ex-OrderDokumen4 halamanBpoc Creation Ex-OrderGalileo Tampus Roma Jr.100% (7)
- Commuter Cleaning - Group 10Dokumen6 halamanCommuter Cleaning - Group 10AMAL ARAVIND100% (1)
- FPR 10 1.lectDokumen638 halamanFPR 10 1.lectshishuBelum ada peringkat
- Aladdin and the magical lampDokumen4 halamanAladdin and the magical lampMargie Roselle Opay0% (1)
- Mayflower Compact - WikipediaDokumen4 halamanMayflower Compact - WikipediaHeaven2012Belum ada peringkat
- 11th AccountancyDokumen13 halaman11th AccountancyNarendar KumarBelum ada peringkat
- Education: Address: Mansoura, EL Dakhelia, Egypt EmailDokumen3 halamanEducation: Address: Mansoura, EL Dakhelia, Egypt Emailmohammed sallemBelum ada peringkat
- 1120 Assessment 1A - Self-Assessment and Life GoalDokumen3 halaman1120 Assessment 1A - Self-Assessment and Life GoalLia LeBelum ada peringkat
- Maternity and Newborn MedicationsDokumen38 halamanMaternity and Newborn MedicationsJaypee Fabros EdraBelum ada peringkat
- Equity Inv HW 2 BHDokumen3 halamanEquity Inv HW 2 BHBen HolthusBelum ada peringkat
- ILO and Social Security (GROUP B)Dokumen13 halamanILO and Social Security (GROUP B)Dhiren VairagadeBelum ada peringkat
- 00.arkana ValveDokumen40 halaman00.arkana ValveTrần ThànhBelum ada peringkat
- Heidegger - Nietzsches Word God Is DeadDokumen31 halamanHeidegger - Nietzsches Word God Is DeadSoumyadeepBelum ada peringkat
- Topic 4: Mental AccountingDokumen13 halamanTopic 4: Mental AccountingHimanshi AryaBelum ada peringkat
- P.E 4 Midterm Exam 2 9Dokumen5 halamanP.E 4 Midterm Exam 2 9Xena IngalBelum ada peringkat
- EAPP Q2 Module 2Dokumen24 halamanEAPP Q2 Module 2archiviansfilesBelum ada peringkat
- 2020 Book WorkshopOnFrontiersInHighEnerg PDFDokumen456 halaman2020 Book WorkshopOnFrontiersInHighEnerg PDFSouravDeyBelum ada peringkat
- Detailed Lesson PlanDokumen5 halamanDetailed Lesson PlanHazel Mae HerreraBelum ada peringkat
- BCIC General Holiday List 2011Dokumen4 halamanBCIC General Holiday List 2011Srikanth DLBelum ada peringkat
- Tax Invoice/Bill of Supply/Cash Memo: (Original For Recipient)Dokumen1 halamanTax Invoice/Bill of Supply/Cash Memo: (Original For Recipient)Pravin AwalkondeBelum ada peringkat
- Marlissa - After School SpecialDokumen28 halamanMarlissa - After School SpecialDeepak Ratha50% (2)
- Legal validity of minor's contracts under Indian lawDokumen8 halamanLegal validity of minor's contracts under Indian lawLakshmi Narayan RBelum ada peringkat
- Red Orchid - Best PracticesDokumen80 halamanRed Orchid - Best PracticeslabiaernestoBelum ada peringkat