ER Lenght of Stay
Diunggah oleh
Claire EscananDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
ER Lenght of Stay
Diunggah oleh
Claire EscananHak Cipta:
Format Tersedia
Clinical Chemistry / REDUCING LABORATORY TURNAROUND TIME OUTLIERS
Reducing Laboratory Turnaround Time Outliers Can Reduce Emergency Department Patient Length of Stay An 11-Hospital Study
Lorne L. Holland, MD,1 Linda L. Smith,2 and Kenneth E. Blick, PhD1
Key Words: Turnaround time; Length of stay; Emergency department; Quality improvement
DOI: 10.1309/E9QPVQ6G2FBVMJ3B
Abstract
Poor core laboratory performance that causes delays in diagnosis and treatment is an impediment to optimal patient care, particularly in high-volume patient care areas such as the emergency department (ED). To evaluate the impact of laboratory performance on patient care outcomes, we obtained data from 11 hospitals related to laboratory test turnaround time (TAT) parameters and ED patient throughput. We observed that the average length of stay (LOS) in the ED correlated significantly with the percentage of total laboratory outliers (R2 = 0.75; P < .01) and to a lesser extent the TAT means (R2 = 0.66; P < .01). Furthermore, improvements in laboratory performance during the study were associated with concurrent decreases in ED LOS. Although in the past, laboratories have focused on TAT means for performance assessment, our observations suggest that a more appropriate method of benchmarking might be to aggressively set clinically driven TAT targets and assess performance as the percentage of results achieving this goal.
It has been observed that faster interventions generally are associated with better outcomes for patients.1,2 Moreover, the emergency department (ED) length of stay (LOS) correlates with additional inpatient LOS,3,4 suggesting initial delays in diagnosis and management in the ED continue to have repercussions even after the patient has been admitted. Because 60% to 70% of the objective information on the patients chart is laboratory information, it follows that delays in reporting laboratory results would cause a concomitant delay in the diagnosis and management of patients. The influence of rapidly available laboratory data on the efficient diagnosis and management of patients in the ED has been reported for satellite laboratory and point-ofcare testing.5-7 However, these studies focused only on improvements in the ED LOS owing to the addition of ED point-of-care testing with no attention given to potential effects of core laboratory testing on the ED LOS. Therefore, to study the relationship of core laboratory testing performance and ED LOS, we measured turnaround time (TAT) means and percentages of TAT outliers in 11 hospitals for tests commonly used by the ED, including CBC count, electrolytes, cardiac markers, and urinalysis. Previous studies had suggested that TAT means and frequency of outliers were useful tools for assessment of laboratory performance8,9; however, neither of these reports included patient outcome data. Hence, the focus of this study was to address the issues of the direct impact of core laboratory performance on ED LOS and which laboratory TAT metric is the best indicator in terms of ED LOS.
American Society for Clinical Pathology
672 672
Am J Clin Pathol 2005;124:672-674
DOI: 10.1309/E9QPVQ6G2FBVMJ3B
Clinical Chemistry / ORIGINAL ARTICLE
Materials and Methods
Laboratory TAT Data We measured the laboratory received to verified TAT means and TAT outlier percentages (OPs) in 11 community hospitals from November 2003 through July 2004. We measured TATs for basic and comprehensive metabolic panels, troponin I, CBC count, and urinalysis. Outliers were defined as more than 30 minutes for a CBC count, more than 40 minutes for chemistry measurements, more than 60 minutes for troponin I measurement, and more than 30 minutes for a urinalysis. We also measured the ED patient lengths of stay in these hospitals. All 11 hospitals used the same chemistry analyzer (Dade Dimension RxL, Dade, Deerfield, IL) for chemistry and cardiac testing; in hematology, different instruments were used (Abbott Cell-DYN, Abbott, Abbott Park, IL; Coulter, Beckman Coulter, Brea, CA); and for urinalysis, the Roche Criterion (Roche, Indianapolis, IN) strip reader was used. Database Creation For information technology, all hospitals included used the Meditech Version 4.9.1 (Meditech, Westwood, MA) for obtaining laboratory TAT and ED patient LOS data. For database processing, raw data from the Meditech hospital information system were downloaded as text files into Microsoft Excel (Microsoft, Redmond, WA) with subsequent transfer of these data into a Microsoft Access database for analysis. Before transfer to the Access database, data from the different hospitals were standardized by removing obvious inaccuracies such as zero values for TAT and TAT results that were clearly cancellations or add-on tests. Calculations and Statistics Final tabulations of TAT outlier percentages and TAT means were performed in Access with report generation, including charts and graphs, created in Excel. Statistical calculations were performed using Microsoft Excel.
Results
The hospitals included in this study ranged in size from 90 to 380 beds with annual ED volumes of 23,000 to 45,000 patients and 35,000 to 74,000 annual ED laboratory test orders. The mean TAT and percentage of TAT outliers for these hospitals are shown in Figure 1 and Figure 2, respectively. The community hospitals as a group showed a correlation of ED LOS with the TAT OP and, to a lesser extent, the mean TAT Table 1. Figure 3 depicts trends observed at 1 hospital for the ED LOS when improvements were made in the percentage of TAT outliers.
Discussion
For years, clinical laboratories have judged overall quality of services using mean TATs measured in minutes. However, TAT means vary greatly based on individual hospitals and the type of test under consideration, as shown in Figure 1 (ie, 6 minutes for the best hospitals mean CBC count and 41 minutes for the worst hospitals mean cardiac TAT). At the same time, the TAT OP varied even more between hospitals (Figure 2). To complicate matters further, Figure 4 shows that TAT means are not related consistently to the TAT OP among the 11 hospitals studied. For example, hospitals 6 through 9 show comparable TAT means but vary markedly in terms of the TAT OP. We observed a significant relationship between the TAT OP and ED LOS (Table 1). The regression equation suggests that for each 1-point increase in the TAT OP, the additional patient wait time in the ED is approximately 7 minutes. Extrapolation revealed that as the TAT OP approaches zero, the ED LOS should approximate 160 minutes. These assumptions will hold true only when the laboratory is the rate-limiting factor in the ED LOS. Although this typically is
45 Best Average Worst 30 29 25 28 37
41
20 Top Average Worst Percent TAT Outliers 15 17.3
Turnaround Time (min)
10 4.8 5 2.5 0.9 1.1
8.2 3.6 2.4
8.3 5
8.1
15 6
12 10 8 10
13
13
0.8 BMP/CMP Cardiac
0 CBC Count Urinalysis BMP/CMP Cardiac
CBC Count
Urinalysis
Figure 1 Mean laboratory turnaround times (TATs). BMP/CMP basic and comprehensive metabolic panels. ,
Figure 2 Laboratory turnaround time (TAT) outliers. BMP/CMP basic and comprehensive metabolic panels. ,
American Society for Clinical Pathology 673
Am J Clin Pathol 2005;124:672-674
DOI: 10.1309/E9QPVQ6G2FBVMJ3B
673 673
Holland et al / REDUCING LABORATORY TURNAROUND TIME OUTLIERS
Table 1 Relationship Between Laboratory TAT Outliers and ED Length of Stay in Community Hospitals
Percent TAT Outliers Regression Equation ED LOS = 7 .1[TAT OP] + 159.8 ED LOS = 5.7[Mean TAT] 51.9 R2 0.75 0.66 P <.01 <.01
20 TAT outlier percentage Average ED LOS
4 15 3 10 2 5 ED LOS (h) Percent TAT Outliers
ED, emergency department; LOS, length of stay; OP, outlier percentage; TAT, turnaround time.
Average TAT (min)
the case, in certain situations, the laboratory test TAT conceivably would not be a bottleneck for ED throughput. Adding further strength to observed correlation between the ED LOS and TAT OP is the dynamic relationship demonstrated in Figure 3; workflow improvements in 1 community hospital improved the TAT OP with concomitant decreases in the ED LOS. As shown, the ED LOS was reduced from 4.1 to 3.2 hours as the laboratory TAT OP decreased from 14.4% to 4.9%. By using the preceding regression formula, the projected decrease in the ED LOS for this amount of improvement in the TAT OP is 67 minutes, which compares favorably with the observed decrease of 55 minutes.
0 Nov Dec Jan Feb Mar Apr May Jun Jul
Figure 3 Changes in the emergency department (ED) length of stay (LOS) in relation to the percentage of laboratory turnaround time (TAT) outliers at 1 hospital.
60 50 40 30 20 10 0 Mean TAT TAT outliers 10 9 8 7 6 5 4 3 2 1 0 1 2 3 4 5 6 7 8 9 10 11
Conclusions
The TAT OP has a direct and significant relationship with patient wait times in the ED. Moreover, our findings indicate that improvement in core laboratory TAT OP will reduce ED patient LOS substantially. In addition, we found that the older methods for monitoring laboratory performance using test TAT means are not particularly useful in assessing the laboratorys impact on patient care. We conclude that the laboratory has a clear and significant role in the effective practice of realtime, evidence-based medicine in the critical care setting.
From the 1Department of Pathology, OU Medical Center and University of Oklahoma Health Sciences Center, Oklahoma City; and 2Premier Inc, Charlotte, NC. Address reprint requests to Dr Blick: Dept of Pathology, Box 26307, University of Oklahoma Health Sciences Center, Oklahoma City, OK 73190.
Figure 4 Turnaround times (TATs) and outliers in 11 community hospitals. 3. Richardson DB. The access-block effect: relationship between delay in reaching an inpatient bed and inpatient length of stay. Med J Aust. 2002;177:492-495. 4. Liew D, Liew D, Kennedy MP. Emergency department length of stay independently predicts excess inpatient length of stay. Med J Aust. 2003;179:524-526. 5. Murray RP, Leroux M, Sabga E, et al. Effect of point-of-care testing on the length of stay in an adult emergency department. J Emerg Med. 1999;17:811-814. 6. Lee-Lewandrowski E, Corboy D, Lewandrowski K, et al. Implementation of a point-of-care satellite laboratory in the emergency department of an academic medical center. Arch Pathol Lab Med. 2003;127:456-460. 7. Leman P, Guthrie D, Simpson R, et al. Improving access to diagnostics: an evaluation of a satellite laboratory service in the emergency department. Emerg Med J. 2004;21:452-456. 8. Valenstein, PN, Emancipator K. Sensitivity, specificity, and reproducibility of four measures of laboratory turnaround. Am J Clin Pathol. 1989;91:452-457. 9. Valenstein P. Laboratory turnaround time. Am J Clin Pathol. 1995;105:676-688.
References
1. Vacek JL. Classic Q wave myocardial infarction: aggressive, early intervention has dramatic results. Postgrad Med. 2002;112:71-77. 2. Montalescot G, Borentain M, Payot L, et al. Early vs late administration of glycoprotein IIb/IIIa inhibitors in primary percutaneous coronary intervention of acute ST-segment elevation myocardial infarction: a meta-analysis. JAMA. 2004;292:362-366.
674 674
Am J Clin Pathol 2005;124:672-674
DOI: 10.1309/E9QPVQ6G2FBVMJ3B
American Society for Clinical Pathology
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Folk 1957Dokumen24 halamanFolk 1957Wilev Jesus Julio DonadoBelum ada peringkat
- Biostatistics 6 ÖzetVeGüzel PDFDokumen177 halamanBiostatistics 6 ÖzetVeGüzel PDFAtilla GÖKTAŞBelum ada peringkat
- Chapter 5: Statistical Inference: EstimationDokumen8 halamanChapter 5: Statistical Inference: EstimationŞterbeţ RuxandraBelum ada peringkat
- Worksheet Ch5-6 MuleDokumen4 halamanWorksheet Ch5-6 MuleAmanuel MandefrowBelum ada peringkat
- Highway Construction Production Rates and Estimated Contracct TimesDokumen95 halamanHighway Construction Production Rates and Estimated Contracct TimesLTE002Belum ada peringkat
- Business Statistics: Fourth Canadian EditionDokumen41 halamanBusiness Statistics: Fourth Canadian EditionTaron AhsanBelum ada peringkat
- Thera Bank-ProjectDokumen26 halamanThera Bank-Projectpratik zanke100% (12)
- Backtesting RSI Trading RulesDokumen31 halamanBacktesting RSI Trading RulesTungPhamBelum ada peringkat
- ch10 cHuXDokumen52 halamanch10 cHuXNaeem UllahBelum ada peringkat
- CE 415 Highway and Traffic EngineeringDokumen24 halamanCE 415 Highway and Traffic EngineeringIhtesham HussainBelum ada peringkat
- Algebra All Answers PercDokumen73 halamanAlgebra All Answers PercEm Mendoza100% (2)
- Normally Distributed Kruskal-Wallis Test: MedianDokumen42 halamanNormally Distributed Kruskal-Wallis Test: MedianRe-Jhay Garcia LingahanBelum ada peringkat
- Measure of Central TendencyDokumen20 halamanMeasure of Central TendencySarah KhanBelum ada peringkat
- Week 4-6 - Ruin TheoryDokumen76 halamanWeek 4-6 - Ruin TheoryParita PanchalBelum ada peringkat
- Math 101 SyllabusDokumen9 halamanMath 101 SyllabusBea Garcia AspuriaBelum ada peringkat
- CH 16 Data HandlingDokumen9 halamanCH 16 Data HandlingKomal TagraBelum ada peringkat
- Math10 Module Q1 Wk4Dokumen13 halamanMath10 Module Q1 Wk4Geraldine RamosBelum ada peringkat
- Statdisk User ManualDokumen20 halamanStatdisk User Manualmspandey20000% (1)
- Statistical Analysis With Software Application: Module No. 4Dokumen13 halamanStatistical Analysis With Software Application: Module No. 4Vanessa UbaBelum ada peringkat
- QPAMBSC17Dokumen789 halamanQPAMBSC17jonnaBelum ada peringkat
- Chapter 10Dokumen13 halamanChapter 10Khay OngBelum ada peringkat
- BALANGUE ALLEN JOHN Lesson 7Dokumen12 halamanBALANGUE ALLEN JOHN Lesson 7James ScoldBelum ada peringkat
- Quantitative Techniques For Management (DBB2102)Dokumen10 halamanQuantitative Techniques For Management (DBB2102)2004singhalvasuBelum ada peringkat
- Quality Assurance in The Clinical Chemistry Laboratory Quality ControlDokumen8 halamanQuality Assurance in The Clinical Chemistry Laboratory Quality Controlさあ ああさBelum ada peringkat
- DocxDokumen16 halamanDocxDeepika PadukoneBelum ada peringkat
- Computer College Calamba Campus: Bachelor of Science in Business AdministrationDokumen5 halamanComputer College Calamba Campus: Bachelor of Science in Business AdministrationAnti VirusBelum ada peringkat
- Module 5 (The Normal Curve)Dokumen12 halamanModule 5 (The Normal Curve)Gabino Pacayo PetilosBelum ada peringkat
- Sampling and Sample SurveyDokumen15 halamanSampling and Sample SurveySUFIAUN FERDOUS100% (1)
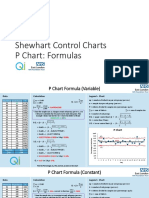
- P Chart FormulasDokumen3 halamanP Chart FormulasエンシラBelum ada peringkat
- CH 05 Probability An Introduction To Modeling UncertaintyDokumen31 halamanCH 05 Probability An Introduction To Modeling Uncertainty唐嘉玥Belum ada peringkat