Know Your Kidney - Information Booklet
Diunggah oleh
Pushpanjali Crosslay Hospital0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
92 tayangan42 halamanKidneys are one of the five essential organs of the body without which the body cannot survive. As our body ages, various organ systems of the body also age and their work capacity diminishes. Between age 40 and 80, the kidney loses about 20% of its mass and glomerular filtration rate (GFR) reduces by 50%. Serious fluid and electrolyte imbalances and kidney dysfunction can result.
Deskripsi Asli:
Hak Cipta
© Attribution Non-Commercial (BY-NC)
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniKidneys are one of the five essential organs of the body without which the body cannot survive. As our body ages, various organ systems of the body also age and their work capacity diminishes. Between age 40 and 80, the kidney loses about 20% of its mass and glomerular filtration rate (GFR) reduces by 50%. Serious fluid and electrolyte imbalances and kidney dysfunction can result.
Hak Cipta:
Attribution Non-Commercial (BY-NC)
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
92 tayangan42 halamanKnow Your Kidney - Information Booklet
Diunggah oleh
Pushpanjali Crosslay HospitalKidneys are one of the five essential organs of the body without which the body cannot survive. As our body ages, various organ systems of the body also age and their work capacity diminishes. Between age 40 and 80, the kidney loses about 20% of its mass and glomerular filtration rate (GFR) reduces by 50%. Serious fluid and electrolyte imbalances and kidney dysfunction can result.
Hak Cipta:
Attribution Non-Commercial (BY-NC)
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 42
Know your kidney
Information booklet for Public
Edited by:
Dr Neeru P Aggarwal
Dr L K Jha
Dr N P Singh
1
Know Your Kidney
1
Dr N P Singh
The kidneys are one of the five essential organs of the body without
which the body cannot survive. Other such essential organs are the
Brain, Heart, Lungs and Liver. The major function of the kidneys is
to remove waste products and excess fluid from the body, to remove
drugs from the body, to balance the body's fluids, to release hormones
that regulate blood pressure, to produce an active form of vitamin
D that promotes strong, healthy bones and to control the production
of red blood cells.
As our body ages, various organ systems of the body also age and
their work capacity diminishes. The kidneys and urinary system are
no different (Fig. 1). Many 40-year-olds would be surprised to learn
that, as far as their kidneys are concerned, the aging process is already
under way. Between age 40
and 80, the kidney loses about
20% of its mass and
glomerular filtration rate
(GFR) reduces by 50%. This
means that your kidneys are
working 50% of what they
used to. The decreased blood
flow and diminished
regulatory capacity that come
with age are not necessarily
problems. However, when
Fig. 1
Kidneys
Bladder
Ureters
Urethra
2
another factor is added (eg, fluid loss from diarrhea, side effect of
medicines), serious fluid and electrolyte imbalances and kidney
dysfunction can result. Elderly patients, commonly defined as those
aged 65 and older are at increased risk of kidney and urinary problems.
Kidneys can be affected by a number of diseases, which if not treated
early, lead to chronic kidney disease (CKD) and in this situation dialysis
and transplantation are the only treatment options left.
What are the signs of kidney damage?
Swelling of legs
Fatigue and loss of energy
Poor appetite
Difficulty in sleeping
Dry, itchy skin
Muscle cramping at night
The need to urinate more often, especially at night
Unexpected weight loss or gain
How to detect kidney disease?
1. Blood pressure measurement
2. Testing for protein in the urine - an excess of protein in your urine
may mean your kidney's filtering units have been damaged by
disease. At times, an excess of protein detected could be due to
fever or heavy exercise, so your doctor will need to re-evaluate
the levels over several weeks.
3. Testing for blood creatinine.
4. Other investigations prescribed by the doctor as per need.
Factors leading to an Increased risk for kidney disease
Age more than 50 years
Diabetes
Blood pressure
Have a family member who has chronic kidney disease, diabetes
or high blood pressure
3
Hypertension (High Blood Pressure)
Repeated BP measurement of more than 140/90 is taken as high BP.
High BP is an early sign of Kidney disease. Almost all kidney diseases
are associated with high BP. Cardiac diseases are associated with low
BP. It is therefore recommended that on first detection of high BP
all patients should undergo kidney check-up. Surveys done in Delhi
show 1 of 4 adults is hypertensive, and 1 of 2 elderly persons (age
>60 years) have high BP. Uncontrolled high BP is associated with
damage to the eyes, brain, kidneys, heart and other organs of the
body. Uncontrolled blood pressure rapidly damages the kidneys.
Diabetes Mellitus
If fasting blood sugar is more than 125 mg% or any heading (random)
more than 200mg%, you have diabetes. Also, HbA1c levels (a new
test) can detect diabetes much faster. About 40% of patients with
Type II diabetes (those above 30 years of age and obese) develop
kidney failure. Presence of albumin in the urine (microalbumin test/
urine test) is an early indicator of kidney damage due to diabetes.
Nowadays drugs like ACE-inhibitors (Enalapril, Ramipril) or ARBs
(Losartan, Telmisatan) can retard the progression of kidney disease,
while adequate control of weight, Blood sugar and BP can prevent
its complications.
Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia (BPH) is a condition that affects the
prostate gland in men. The prostate is a gland found between the
bladder (where urine is stored) and the urethra (the tube urine passes
through). As men age, the prostate gland slowly grows enlarges). As
the prostate gets bigger, it may press on the urethra and cause the
flow of urine to be slower and less forceful.
4
What are the symptoms of BPH?
Symptoms include the need to get up more often at night to urinate,
increased frequency of urination during the day, difficulty in initiating
urine flow and dribbling after urination ends; and if the stream of
urine is thin.
How will my doctor know if I have BPH?
The doctor will study your medical history, conduct a local rectal
examination, ultrasound, and if needed a biopsy.
Treatment
Drug treatments are available. Finasteride/dutasteride blocks a natural
hormone that makes the prostate enlarge; alpha-blockers also can
help the symptoms of BPH. These medicines may not work in all
men. The side effects of alpha-blockers include dizziness, fatigue
and lightheadedness.
Would I need an operation?
The doctor is the best judge to decide if medications alone will be
effective or if an operation is needed. A very large prostate, repeated
urinary infections and intolerable symptoms are some of the
indications for operations.
Prostatic urethra
narrowed by
enlarged prostate
Direction of urine flow
Urinary bladder
Surgical capsule
True prostate tissue
Prostatic capsule
BPH tissue
5
Prostate Carcinoma
About 6% of males over 50 years of age harbor clinically significant
prostate cancer and the number rises to about 20% for those over
the age of 75 years. Digital rectal examinations and prostate-specific
antigen (PSA) testing has resulted in an 85% increase in the rate of
prostate carcinoma detection. If the cancer is caught at its earliest
stages, most males will not experience any symptoms. Some however,
will experience symptoms that might indicate the presence of prostate
cancer, including:
A need to urinate frequently, especially at night,
Difficulty starting urination or holding back urine,
Weak or interrupted flow of urine,
Painful or burning urination,
Difficulty in having an erection,
Painful ejaculation,
Blood in urine or semen,
Pain or stiffness in the lower back, hips, or upper thighs, or
Weight loss.
Since these symptoms can also indicate the presence of other diseases
or disorders, men who experience any of these symptoms would
need to undergo a thorough work-up to determine the underlying
cause of the symptoms.
The PSA blood test
PSA is a protein produced by the prostate and released in very small
amounts into the bloodstream. When there is a problem with the
prostate, such as when prostate cancer develops and grows, more
and more PSA is released. PSA levels less than 4 ng/mL are usually
considered "normal," those between 4 and 10 ng/mL are usually
considered "intermediate", and results over 10 ng/mL are usually
6
considered "high". The American Cancer Society recommends that
both the PSA and DRE should be offered annually, after the age of
50 years.
Biopsy
During a biopsy, needles are inserted into the prostate to take small
samples of tissue, often under the guidance of ultrasound imaging.
The biopsy procedure may cause some discomfort or pain, but the
procedure is short, and can usually be performed without an overnight
hospital stay.
Treatment
There is no "one size fits all" treatment for prostate cancer and the
decision will rest on a combination of clinical and psychological factors.
Treatment options for prostate cancer include:
Active surveillance,
Surgical interventions like Prostatectomy,
Radiation therapy for advanced or recurrent Prostate cancer,
Hormone therapy, and
Chemotherapy
Urine Infections
Normally, urine is sterile. It is usually free of bacteria, viruses, and
fungi, but does contain fluids, salts, and waste products. An infection
occurs when tiny organisms, usually bacteria from the digestive tract,
cling to the opening of the urethra and begin to multiply. The urethra
is the tube that carries urine from the bladder to outside the body.
Symptoms include frequent urge to urinate and a painful, burning
feeling in the area of the bladder or urethra during urination. Diagnosis
is made on the bases of urine examination and culture testing. Elderly
females are prone for developing urinary infections because the
7
normal mechanisms that prevent infection become weak in the elderly.
Most infections can be treated with antibiotics, but detailed evaluation
to prevent further infections is also necessary.
Renal Stones
A kidney stone is a hard mass developed from crystals that separate
from the urine within the urinary tract. Normally, urine contains
chemicals that prevent or inhibit the crystals from forming. These
inhibitors do not seem to work for everyone however, so some
people develop stones.
What are the symptoms of kidney stones?
Severe pain
Nausea and vomiting
Fever, chills and weakness
Cloudy or foul-smelling urine
Blood in the urine
Blocked flow of urine
Kidney stones can be diagnosed with the help of investigations like
x-ray, ultrasound and CT scan. CT scan has come up as the most
sensitive investigation to detect kidney stone.
What are the risk factors for kidney stones?
There are several factors that lead to increased risk for the formation
of kidney stones. Some of these maybe due to
Too little fluid intake,
Urinary tract infections,
Misuse of certain medications,
Urinary tract blockage,
Limited activity for several weeks, and
Certain genetic and metabolic diseases.
8
How can stones be prevented from forming?
Adequate intake of fluids.
Avoid excess of tea, coffee, cold drinks and beer. Restrict red
meat
Low salt diet
Avoid pan and gutka
Avoid constipation.
Drug Toxicity
Due to a decreased GFR and heightened sensitivity to nephrotoxins,
the elderly have a higher incidence of nephrotoxicity. Use of certain
medicines and indiscriminate use of over-the-counter compounds
can lead to kidney failure. Agents usually associated with kidney insult
are nonsteroidal anti-inflammatory drugs (painkillers), angiotensin-
converting enzyme inhibitors (BP medicines), aminoglycosides
(antibiotics), and radiocontrast material (used during CT scanning).
These agents should be used only under guidance of a qualified
specialist. Once the kidney fails due to any reason, it becomes very
difficult to treat it and the help of kidney disease experts is essential.
Overall, to maintain good kidney function and to avoid urinary
problems, it is recommended liquid intake of two to three litres per
day must be maintained. Also, an early review with a doctor for any
abnormal symptoms would help in detection of the disease at an
early stage.
9
Are You at Risk of Developing a
Kidney Disease Failure?
2
Dr Neeru P Aggarwal and Dr Sandeep Gupta
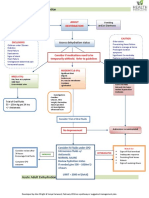
There are known risk factors that predict the development of kidney
disease. While some of them like age and family history are not
modifiable, others like diabetes, high blood pressure can be controlled.
Unfortunately, most people who suffer from chronic kidney disease
(CKD) or early renal failure do not have symptoms and are thus
unaware of the status of their kidneys. Therefore, if you have any of
the following risk factors, work with your doctor in screening for
and preventing kidney damage.
Diabetes
About 40 percent of patients seeking dialysis have diabetes. Type 2
diabetes is the no.1 cause of CKD and End Stage Renal Disease
(ESRD). Uncontrolled disease process damages the renal blood vessels
and the filtering apparatus (nephrons).
Action: Developing renal failure in diabetics is not inevitable. Tight
control of blood sugar can prevent damage to the kidneys. Special
investigations like detection of microalbuminuria in urine can diagnose
CKD at the earliest and when still reversible.
Hypertension (High Blood Pressure)
Hypertension is both a cause and an effect of kidney disease.
Uncontrolled high blood pressure results in maladaptive architectural
damage and puts a higher pressure gradient on the kidneys' filtering
system. The ideal BP in heart diseases, CKD and diabetes is 130/80.
10
Action: Certain antihypertensives like ACE inhibitors, ARB's are of
proven benefit in preventing development of kidney damage. Being
compliant with medication and meticulous control of BP is the best
option.
Obstructive Uropathy
If you happen to have a history of recurrent urinary tract infections,
stone formation, congenital anomaly of the urinary system then the
resulting back flow of urine to the kidneys can cause scarring and
damage to its function.
Action: Some of these factors can be repaired and thereby help
restore function in a blocked kidney. Do seek a doctor's advice in
managing and eradicating them.
Overuse of Medication / Drug Abuse
Heavy use of analgesics like ibuprofen, naproxen, and acetaminophen
are linked to interstitial nephritis, resulting in kidney inflammation
and failure; especially if the kidney functions are already deranged.
Antibiotics use like amino glycosides, vancomycin, penicillin and
cytotoxics also need caution. Use of non prescription drugs like heroin
and cocaine are also toxic to the kidneys.
Action: When being prescribed for any illness, do inform the doctor
of your kidney damage. When on any new medication, report to the
doctor of any new symptom. Be honest about your medical history
and seek support for deaddiction.
History of Non Diabetic Glomerular Disease
Illnesses like glomerulonephritis and nephritic syndrome can damage
the kidneys enough to cause CKD.
Action: Stay alert and consult with your doctor regularly as early
detection and complete treatment decreases the chances of the same.
11
Family History of Kidney Disease
It is prudent to reveal the history of any family member diagnosed
with kidney disease, on dialysis, or has had a kidney transplant. Certain
diseases like Adult Polycystic Kidney Disease are inherited diseases
that gradually damage the kidney as the cysts replace the normal
functioning parenchyma. Diabetes and Hypertension also run in families.
Other risk factors
Smoking and obesity but itself or in patients with high BP and diabetes
may further damage the kidneys. Avoiding smoking and/or maintaining
an ideal body weight is the answer.
Hence, control of risk factors is certainly a more health and
cost effective option than the cost of treatment modalities
available for Chronic Kidney Disease.
12
M k; c V ht , o a f d M u h d h c he kj h
(f u . kZ; y su s d k l g h l e ; )
3
Dr Neeru P Aggarwal, Dr N P Singh and
Dr Azmat Gowher Khan
-ii- r i i-ii i -ri-ii i i ni i ri r| r (i i - i
- ilni i ni ni r| ; ini ii r -i-r i i-ii ni r
(r ; i r| ; - l(( - /// i -i-r ini r
li i (i zozr n i so i ri i ni| iin -
li r/ i ini rin| -- iii - -i-r i -ii ii
-i ini r| ni i iii -i-r i -i l-ni r| r -i;
( -i; z -i-r ilni - lnri; - r l-ni rini r| ;
ii ( nni i(i - - ri ni r il~ ;i ii li i
rini r| ; l-ni ln in i ri nii r l ; i
~i ni i nii ; i (ri ii i| r ; l ii i r
l ; l-ni (li i iii) i iii- i( ri |
Ek/ kqe sg e sa x qn ksZa d h [ kj kc h d ks j ksd saA v Hkh l s b l i j / ; ku n saA
-ii-r ilni - ni i iii ii.ii ni ini r ( -i-r
lnri; i ni ; lii ri n r | n - i n i li -ii ii i si -i
( i i-li ni r| li i i i i i-ni -
ri ini r l i - l(i iii i -i( ri nni r ( i -i ;
i-li l ii - ii i-i ri ini r | r l-ln l in ni
i ni ; li i li ii rii rn r| li i i i
i; i i- iil(n ri li ( ll-l i nni r| l
nn i li i ni i ii i ni r|
13
[ kr j s d s d kj . k
i - i ni, n - i n i li -ii ( l(i -i
- -i-r ni i iii i ;lnri|
f d M u h d ks [ kj kc d j u s e sa e q[ ; Hkwf e d k b u d h g ksr h g S
ni n i- in
-i- r n i ii
d Sl s b l d k i r k y x k l d r s g Sa
ll-n i ii - i-i i i (in ri ilr| ri ; i
ni n ni r ii i l-iln r| --- ,ii l-nii i ii ni
ini r | i l-iln - s -i -i ,ii n i i ii ri ii
i ni r ( l-iln i i-i ii li i ni r|
D ; k d j sa
1. ii - i ii i -i;i~il- l i ( i|
2. ni i i-i i (zo,so)
3. in i li - i| iii - oo ( ii z i- i o
co i i i|
4. i-i |
5. ii - i -i i -ii - , i i, -i irii iri ( i |
; ii i(iili ,ii i ( li i ii ri i n r
l~ i i ; iii i iii i-i l-ln - ii i n r|
n i n ii ri in r ni l(i l iili ii
- ii ili --i ii i rini r|
14
Eating Right to Feel Better
in Kidney Disorder
4
Ms Charu Dua and Dr N P Singh
This chapter will help you know about
I. Diet in kidney stone prevention
II. Nutrition in renal failure (adults)
III. Nutrition during dialysis
I. Diet in Kidney Stone Prevention: General Tips
Diet is one of several factors that can promote or inhibit kidney
stone formation.
Different kinds of kidney stones require different prevention diets.
Drinking water and other fluids is very important in preventing
kidney stones. Try taking lemonade, coconut water, citrus drinks
(avoid Orange juice for oxalate stones). Coffee and tea also adds
to fluid intake. Avoid dark colas as they increase the risk of stone
formation. Moderate intake of beer and wine may also help, but
remember moderation is the key.
People who have had a kidney stone should drink enough water
and other fluids to build at least 2 quarts of urine each day.
Diets high in salt or sodium can increase the excretion of calcium
into the urine and thus increase the risk of calcium containing
kidney stones. Reducing salt intake is preferred to reducing calcium
intake. Avoid or reduce the intake of papads, chutney, salted butter,
ketchups, and table salt in diet. Also avoid the intake of
monosodium glutamate (MSG), canned, tinned, packed,
processed and fast foods as their sodium content is very high.
Read the nutrition information of packed food items to know
their sodium content.
15
Foods rich in animal proteins - such as meat, nuts, urad dal,
rajhma, and other beans contain purines that may increase the
risk of uric acid stones and calcium stones.
Calcium from food can help prevent kidney stone formation
and help maintain bone density. It is a myth that milk and its
products should be avoided if you have calcium stones.
Avoiding foods rich in oxalates, such as spinach, nuts, wheat
bran, and orange juice may help prevent calcium oxalate stones.
After a doctor has completed an evaluation and determined the
cause of the stones, a dietitian can help plan meals that lower the
risk of forming stones.
II. Nutrition in Chronic Kidney Failure (CKD): Adults
Healthy kidneys work to remove waste products and extra minerals
from foods eaten. They also maintain:
Sodium and water balance
Support bone health by balancing calcium and phosphorous.
When kidneys are not working properly, they cannot get rid of
waste products and extra fluids. CKD usually takes a long time to
develop and cannot be cured. In CKD, the kidneys continue to work
- just not as well as they should. Wastes may build up so gradually
that the body becomes used to having those wastes in the blood.
Minerals in food such as potassium, sodium and phosphorous
accumulate and stress the heart, bones, lungs and general health.
Generally people with diabetes, high blood pressure, or both are at
risk for developing CKD.
The goal of diet is to focus on
Preventing the excess accumulation of fluids and wastes, while
allowing the kidney to heal
To control and maintain blood glucose levels
To control blood pressure
To regulate intake of Proteins, Potassium, Phosphorous, Sodium
(salt), Calcium, Fluid intake.
16
Do's and Don'ts of Diet
1. Proteins: Protein is an essential part of any diet. Proteins help
build and maintain muscle, bone, skin, connective tissue, internal organs,
and blood. They help fight disease and heal wounds. However, proteins
also break down into waste products that must be cleaned from the
blood by the kidneys. Eating more protein than required may put an
extra burden on the kidneys and cause kidney function to decline
faster. Doctors have long recommended that patients with CKD eat
moderate or reduced amounts of protein
Some patients, however restrict or totally avoid proteins that leads to
malnutrition. Vegetarian are already on a low protein diet, and hence
before making any changes in protein intake, a dietitian must be
consulted. The recommended amount of protein intake should be
0.8gms/KG/BW. So if you weigh 60 kgs you should consume at
least 48 gms of protein in your diet. Also it is important to have
good quality protein like milk, paneer, egg, soya, chicken and fish.
Though these proteins increase the urea levels, a balance of both
good quality and bad quality protein (dals, rice, wheat etc) is important
to be maintained.
Protein values
Consult a dietician to learn about proteins and balancing intake and
taste, while helping kidneys to heal.
Food Item Protein Content (gms)
Milk (250ml) 8 gms
Curd (100gms) 4.2 gms
Paneer (40gms) 10 gms
Egg White 5 - 6 gms
Chicken/ Fish (50gms) 12 - 13 gms
Dals/ Besan/ Sprouts/Soya 7 gms
(1 Medium size bowl, 30 gms raw)
17
2. Potassium: is primarily present in vegetables and fruits, salads,
fruit juices, soups, lime, coconut water, dried fruits, nuts, tomato
chutney, coconut chutney etc. If potassium levels begin to increase
(check via blood test), consult your dietitian. You may need to
avoid some fruits and vegetables. You can reduce the potassium
content of food by the following:
a. Dialyzing potatoes and other vegetables - you can remove some
of the potassium from potatoes and other vegetables by peeling
them, then soaking them in large amount of water for several
hours before use.
b. Draining and rinsing vegetables well before cooking.
c. Cooking the vegetables helps removing some potassium. Hence,
use tomatoes while cooking, avoid eating them raw.
d. Restrict intake of raw salad.
e. Limit potassium content by portion control (the amount of a
food that you eat at one time). Thus, a high potassium tomato
(1small) provides 273 mg of potassium. Eat a thin slice instead
of the whole tomato, ie, 1/6
th
of 1 small tomato provides 45
mg of potassium.
f. Foods rich in potassium are bananas, oranges, melons, tomatoes,
raw vegetables, lemon, alma, vegetable soups, mushrooms, arbi,
kathal, chutneys, coconut water, fruit and vegetable juices etc.
g. Fruits that are low in potassium are apples, pineapple, papaya,
and guava. However, consumption would need to be limited to
100 gms a day.
3. Sodium: Sodium is found in ordinary table salt and many salty
seasonings like soy sauce. Canned foods, some frozen foods, and
most processed foods have large amounts of table salt. Snack foods
like chips and namkeens are also high in salt. Too much sodium
intake can be harmful as it leads to fluid retention. The extra fluid
raises blood pressure thereby straining the heart and kidneys.
18
Examine the sodium content on the nutrition labels of the foods
you buy. Choose "sodium-free" or "low-sodium" food products.
Aim to keep your daily sodium intake to less than 1,500 milligrams.
Try alternative seasonings like tamarind juice, salt-free seasoning
mixes, or herbs like (oregano, basil, thyme, roasted zeera, black
pepper)
Avoid the salt shaker on the table, chat masala, metha soda, Aji-
no-moto (MSG).
4. Phosphorus: is a mineral found in many foods. Too much
phosphorus in blood pulls calcium from your bones. Losing calcium
will make your bones weak and more likely to fracture. Too much
phosphorus may make your skin itch. Foods like milk and cheese,
dried beans, peas, colas, canned iced teas and lemonade, nuts,
chocolates and peanut butter are high in phosphorus. Talk with your
dietitian about how much phosphorus you should have in your diet.
As your kidney disease progresses, you may need to take a phosphate
binder. These medications act like sponges to soak up, or bind,
phosphorus while it is in the stomach. Since it is bound, the
phosphorus does enter the blood, and is excreted in the stool.
5. Water: As kidney disease progresses, fluid intake would need to
be restricted to avoid build up in the body. Inform your doctor if
you notice an increase or decrease the amount of urine your body
generates; or if you have any swelling around your eyes or in your
legs, arms, or abdomen. In addition:
Drink water as per thirst, sip it, do not gulp
Drink in small cups or glasses
Freeze juices in an ice cube tray and eat it like a candy or a bar.
Plan your fluid serving at every meal.
Any food that is liquid at room temperature also contains water.
These foods include tea, coffee, soups, melons, grapes, oranges,
tomatoes, dal, curd, milk, lassi, jelly, lettuce and celery. All such
foods add to your daily fluid intake.
19
6. Remember: in Diabetes and Kidney disease
To eat 5 -6 small but frequent meals
To eat regular meals: Keep day to day intake consistent so that
the medication regime matches the food intake. Eat meals and
snacks at the same time each day to prevent high/low blood
sugar levels.
Use snacks to prevent severe hypoglycemia. Be sure to have a
bedtime snack containing protein, starch, fat to provide the body
with an energy source that will last through the night.
Manage carbohydrate intake carefully since the amount of
carbohydrate eaten, the time it is eaten and what is eaten determines
the blood sugar level.
Avoid over-treating low blood sugar by eating enough
carbohydrates to raise blood sugar; and checking blood sugar
every 10 mins will help determine quantity of intake.
Reduce cholesterol and saturated fat intake
Maintain appropriate weight for height
Increase fiber intake (salads, sprouts, vegetables, fruits, brown
bread, oats etc)
Avoid foods high in salt (processed food, canned food, market
butter, ketchups, sauces, salt etc)
Avoid excessive protein intake by reducing consumption of red
meat.
Avoid eating sugar and its products
Avoid eating fruits with main Meals, eat them in between. Avoid
fruits like mango, banana, cheeku and grapes if your sugars are
high. Avoid fruit juices (fresh or tetra pack)
Avoid eating vegetables like potatoes, arbi, and sweet potato.
7. Hypertension and Kidney Disease:
High Blood Pressure (hypertension) is a strong risk factor for heart
disease, stroke and kidney failure. Most patients with established
hypertension do not make sufficient lifestyle changes, do not take
20
medicines and neglect their disease. Therefore, to prevent and control
hypertension lifestyle modification is imperative. Lifestyle modification
not only improves control but also helps reduce medication doses in
hypertension. Moreover, it helps prevent high blood pressure.
Lifestyle Modifications for Hypertension Prevention and
Management
Here are some tips on healthy living and lifestyle modifications that
would be helpful to everyone in the family along with the person
with high blood pressure. So these should be adopted by all and no
separate cooking for the patient.
Lose weight if overweight - Eat to live, do not live to Eat.
Regular physical activity - The wise depend on exercise for fitness.
Reduce intake of dietary saturated fat - Clean up the oily mess.
Reduce salt (sodium) intake - Excess salt is harmful.
Maintain adequate intake of dietary potassium - Diet rich in fruits
and vegetables.
Limit intake of alcohol - There is a devil in every berry of grape.
High dietary fiber intake - He who follows nature is never out
of the way.
Avoid smoking and intake of excess caffeine - Do not get reduced
to ashes.
III: Nutrition during Dialysis
When you start dialysis, you must make many changes in your life.
Watching the foods you eat will make you healthier. Food gives you
energy and helps your body repair itself. Food is broken down in
your stomach and intestines. Your blood picks up nutrients from the
digested food and carries them to all your body cells. These cells take
nutrients from your blood and put waste products back into the
bloodstream. When your kidneys were healthy, they work round-
the-clock to remove wastes from your blood. The wastes leave your
body when you urinate. Other wastes are removed in bowel
movements.
21
Now that your kidneys have stopped working, dialysis removes the
wastes from your blood. However, in-between dialysis sessions,
wastes can build up in your blood and make you sick. You can reduce
the amount of wastes by watching what you eat and drink. A good
meal plan can improve your dialysis and your health.
1. Fluids: You must continue to restrict fluid as advised by your
doctor/ dietitian. Fluid can build up between dialysis sessions,
causing swelling and weight gain. The extra fluid affects your
blood pressure and can make your heart work harder. You could
have serious heart trouble from overloading your system with
fluid.
Control your thirst
The best way to reduce fluid intake is to reduce thirst caused
by the salt you eat. So, avoid salty foods like chips etc. Choose
low-sodium products.
You can keep your fluids down by drinking from smaller
cups or glasses. The dietitian will be able to give you other
tips for managing your thirst.
Your dry weight is your weight after a dialysis session when all
of the extra fluid in your body has been removed. If you let too
much fluid build up between sessions, it is harder to get down to
your proper dry weight. Your dry weight may change over a
period of 3 to 6 weeks. Talk with your doctor regularly about
what your dry weight should be.
2. Continue to restrict Potassium/Phosphorous. Only one fruit
during dialysis is acceptable. Try not to take fruits with high water
content (melons, oranges etc).
3. Protein: Before when you on dialysis, your doctor may have
told you to follow a low-protein diet. Being on dialysis changes
this. Most people on dialysis are encouraged to eat as much high-
quality protein as they can. Protein helps muscle and repair tissue.
22
The better nourished you are, the healthier you will be. You will
also have greater resistance to infection and recover from surgery
more quickly. Your body breaks protein down into a waste product
called urea. If urea builds up in your blood, it is a dangerous
sign. Eating mostly high-quality proteins is important because
they produce less waste than others. High-quality proteins come
from meat, fish, milk, poultry, and eggs (especially egg whites).
4. Sodium: Sodium is found in salt and other foods. Most canned
foods and frozen foods contain large amounts of sodium. Too
much sodium makes you thirsty. However, if you drink more
fluid, your heart has to work harder to pump the fluid through
your body. Over time, this can cause high blood pressure and
congestive heart failure.
Try to eat fresh foods that are naturally low in sodium. Look for
products labeled low sodium.
Talk with a dietitian about spices you can use to flavor your food.
The dietitian can help you find spice blends without sodium.
23
Chronic Kindney Diseases:
Hemodialysis as Treatment Option
5
Dr L K Jha and Dr N P Singh
In India with a population base of above one billion, approximately
1.5 lakh patients develop chronic renal failure every year. Diabetes
Mellitus, hypertension, chronic glomerulonephritis, chronic interstitial
nephritis, and stone diseases are the leading causes of kidney failure
in India. Dialysis is needed when the body loses about 85 to 90
percent of its kidney function. A majority of these patients choose
hemodialysis as the initial treatment option as it is cheaper and easily
available. Only a few patients choose peritoneal dialysis (PD) as an
option for home dialysis.
Like healthy kidneys, dialysis keeps the body in balance to:
Removes waste, salt and extra water to prevent them from
building up in the body
Keeps a safe level of certain chemicals in the blood, such as
potassium, sodium and bicarbonate
Control blood pressure.
Hemodialysis (HD) works by circulating the blood through special
filters outside the body. The blood flows across a semi-permeable
membrane (the dialyzer or filter), along with solutions that help remove
toxins. Dialysis quickly removes drugs or poisons in acute situations.
This technique can be life saving in people with acute or chronic
kidney failure.
Dialysis uses special ways of accessing the blood in the blood vessels.
The access can be temporary or permanent. Temporary access takes
24
the form of dialysis catheters - hollow tubes placed in large veins
that can support acceptable blood flow. Permanent access is created
by surgically joining an artery to a vein. This allows the vein to receive
blood at high pressure, leading to a thickening of the vein's wall. This
vein can handle repeated puncture and also provides excellent blood
flow rates. The connection between an artery and a vein can be made
using blood vessels (an arteriovenous fistula, or AVF) or a synthetic
bridge (AVF) or a synthetic bridge (arteriovenous graft, or AVG):
Blood is diverted from the access point in the body to a dialysis
machine. Here, the blood flows counter-current to a special solution
called the dialysate. The chemical imbalances and impurities of the
blood are corrected and the blood is then returned to the body.
Schematic representation of a Dialyzer
Hemodialysis
Just before the hemodialysis the following assessments are made:
Blood pressure Breathing rate
Chest assessment Heart rate
Temperature Weight
Examination of venous access
25
Hemodialysis can be performed at the patient's home or at a dialysis
centre, where hemodialysis is provided by trained nurses and
technicians. Typically, most patients undergo hemodialysis for three
sessions every week. Each session lasts from 3 to 4 hours.
Advantages of hemodialysis
It does not require admission
Dialysis unit staff conducts the procedure
No equipments or supplies required at home
No external excess required.
Risks
Blood pressure changes associated with hemodialysis may pose a
risk for patients with heart problems. Apart from this there are some
other immediate risks involved, these are
A small bubble of air in the blood that travels to a blood vessel
in another part of the body (air embolism)
Bleeding from the access site
Cramps
Dialyzer reaction
Electrolyte imbalance
Infection
Irregular
Low blood pressure (hypotension)
Nausea and vomiting
Long-term risks include:
Autonomic neuropathy
Blood loss leading to iron deficiency
Cardiovascular disease
Dialysis-associated amyloidosis
Dialysis dementia
26
Peritoneal Dialysis
6
Dr L K Jha and Dr Neeru P Aggarwal
Peritoneal dialysis (PD) is a procedure that removes wastes, chemicals,
and extra water from your body. This type of dialysis uses the lining
of abdomen to filter blood. This lining is called the peritoneal
membrane and acts as the artificial kidney.
How Peritoneal Dialysis Works
A mixture of minerals and sugar dissolved in water (the dialysis
solution), travels through a catheter (soft plastic tube) into the patients'
abdomen. The sugar (dextrose) draws wastes, chemicals, and extra
water from the tiny blood vessels in the peritoneal membrane into
the dialysis solution. After several hours, the used solution is drained
from the abdomen along with the waste. The abdomen is then refilled
with fresh dialysis solution, and the cycle is repeated. The process of
draining and refilling is called an exchange. Each exchange takes about
30 to 40 minutes. The length of time the dialysis solution stays in the
patients' abdomen is called the dwell time. A typical schedule calls
for four exchanges a day, each with a dwell time of 4 to 6 hours.
Different types of PD have different schedules of daily exchanges;
and provides the patient with some measure of control during the
process of treatment, thus they can schedule their sessions at home,
at work, or on trips. However, this independence also requires the
patient to work closely with patients' health care team - the
Nephrologist, dialysis nurse, dialysis technician, dietitian, social worker
and most importantly, the family members.
27
Getting Ready for PD
Whether patient chooses an ambulatory or automated form of PD,
Patient will need to have a soft catheter placed in patients abdomen.
The catheter is the tube that carries the dialysis solution into and out
of patients abdomen. The standard catheter for PD is made of soft
tubing for comfort. It has cuffs made of a polyester material, called
Dacron, that merge with patients scar tissue to keep it in place. The
end of the tubing that is inside patients abdomen has many holes to
allow the free flow of solution in and out. It requires an open surgery
to insert CAPD catheter, under local or rarely general anesthesia.
After catheter insertion the patient usually begins a full schedule of
exchanges for 2 to 3 weeks. This break-in period lets patient build up
scar tissue that will hold the catheter in place.
Types of PD
There are two forms of PD. In Continuous ambulatory peritoneal
dialysis (CAPD), no machine is required. As the word ambulatory
suggests, the patient can walk around with the dialysis solution in
their abdomen. In Continuous cycler-assisted peritoneal dialysis
(CCPD), a machine called a cycler is used to fill and drain the abdomen,
usually while the patient is asleep. CCPD is also sometimes called
Automated peritoneal dialysis (APD).
The type of PD patient chooses will depend on the schedule of
exchanges patient would like to follow, as well as other factors. A
patient may start with one type of PD and switch to another; or the
patient may find that a combination of automated and nonautomated
exchanges suits them the best - in any case, the patient would need to
work with the health care team to find the best schedule and techniques
to meet their lifestyle and health needs.
Continuous Ambulatory Peritoneal Dialysis (CAPD)
If the patient chooses CAPD, they would have to introduce the dialysis
solution into their abdomen. After 4 to 6 or more hours of dwell
28
time, the solution, now containing wastes, would need to be drained
into the bag. The cycle would need to be repeated with a fresh bag
of solution. No machine is required for this procedure, as the filling
and drainage is done by gravity. The doctor will prescribe the number
of exchanges needed, which is typically three or four exchanges during
the day and one evening exchange with a long overnight dwell time
while the patient is asleep.
Continuous Cycler-Assisted Peritoneal Dialysis (CCPD)
CCPD uses an automated cycler to perform three to five exchanges
during the night while the patient is asleep. In the morning, the patient
would require one exchange with a dwell time that lasts the entire
day.
Pros and Cons
All the treatment options for treatment of Kidney failure have their
pros and cons.
CAPD
Pros
Can be done alone
Can be done at self determined times provided the required
number of exchanges are done daily
Can be done anywhere
No machine is required
Traveling to a center three times a week is not required.
Cons
Daily schedule may be disrupted
Since it is a continuous treatment, all exchanges must be performed
7 days a week.
CCPD
Pros
Can be done at night while sleeping
Exchanges must done during the day
29
Cons
A machine is required
Night movement is limited as you will be connected to the cycler
The high recurring cost is a major hurdle in CAPD, which on a monthly
average is about Rs 15,000 to 18,000.
Possible Complications
The most common problem with peritoneal dialysis is peritonitis, a
serious abdominal infection. This infection can occur if the opening
where the catheter enters the body becomes infected or if
contamination occurs when the catheter is connected or disconnected
from the bags. Peritonitis requires antibiotic treatment by your doctor.
To avoid peritonitis, you must be careful to follow procedures exactly
and learn to recognize the early signs of peritonitis, which include
fever, unusual color or cloudiness of the used fluid, and redness or
pain around the catheter. Report these signs to your doctor or nurse
immediately so that peritonitis can be treated quickly to avoid additional
problems.
Diet for Peritoneal Dialysis
A peritoneal dialysis diet is slightly different from an in-center
hemodialysis diet.
Salt and liquids would have to be restricted as compared with in-
center hemodialysis, though more of each can be consumed each
day.
Protein intake must be increased.
There may be need to eat high-potassium foods.
Total calories may need to be restricted as the dialysis fluid contains
calories.
Your doctor and a dietitian who specializes in helping people
with kidney failure will be able to help you plan your meals.
30
Kidney Transplantation
7
Mr Shishir Kumar and Dr N P Singh
The kidney is an organ that along with its primary functions plays a
crucial role in filtering undesirable toxic wastes, regulates blood
pressure and volume of fluids and electrolytes in our body.
In recent years, we have witnessed a disturbing increase in the patients
suffering from diabetes, hypertension, severe infections and a trend
of vehement use of painkillers. These are the major causes of the
alarming increase in the number of patients suffering from Chronic
Kidney Disease, which when left untreated or undiagnosed leads to
End-stage Kidney Disease. Thus, it is awareness, prevention and
understanding that is very important.
The question that frequently arises is about possible treatment (a curative
measure) when diagnosis is confirmed. Once the patient has been
diagnosed of ESKD, there are two options:
1. Kidney Transplantation.
2. Dialysis (HD, CAPD, CRRT, SLED).
Kidney Transplantation is considered a boon for the patient since it is
curative with numerous advantages (though there are some minor
disadvantages in a few cases) and helps bring back smiles in the ailing
lives of innumerous patients worldwide.
To understand Kidney Transplantation, we need to be aware of its
outcome:
The patient leads an almost normal, healthier, longer and better
quality of life with more energy, zeal and independence.
Complications that arise during dialysis (retardation of health,
31
deterioration in quality of life, pain, time-consumption) is not
applicable to the transplant patient.
Cost effective: Initially it seems that Kidney Transplantation
expenses are high but it reduces over time as the patient recovers
and is usually less than that of prolonged dialysis therapy.
Procedure
For a patient suffering from ESKD (End-stage Kidney Disease) who
has been advised by the treating Nephrologist to undergo Kidney
Transplantation, the first step is finding a potential Kidney Donor,
whose kidney would be transplanted in the patient. Donors have
been categorized into these by the THOA (Transplant of Human
Organ Act) 1994 (legal enactment to stop organ-trafficking and
donation of organ/tissues for financial gain).
1. Live related donors (parents/grandparents/siblings/son/
daughter).
2. Live un-related donors (spouse and family friend).
3. Deceased (cadaver) donors (retrieval of kidney from the victim
of Brain death).
Willingness for any of above itself does not encompass the criteria
of having a suitable donor. It is recommended that the prospective
donor be in the age group of 18 to 65 years and must be of the
same Blood Group as the patient or of a compatible one. Blood
group mapping remains the same as that in blood donation (Fig. 1.1)
Patient blood group Donor blood group
A A OR O
B B OR O
AB A OR B OR AB OR O
O O
32
The prospective donor with matched or compatible blood group
has to undergo a series of investigations and medical examination to
rule out Diabetes Mellitus, Hypertension, and Cancer, HIV, kidney
disease or other medical and psychiatric illness. The prospective donor
can be accepted as a suitable kidney donor only after the above
clearances.
In instances where two patients do not have either matched blood
group or compatible blood group donors; swapping or exchanging
their willing donor with another patient's donor facing the same
predicament is possible and is known as "Paired Donors" (fig. 1.2).
Case 1
Case 2
A
B
B A
Patient 1 Patient 2
Donor 1 Donor 2
q
q
After the pre-transplant work-up of the patient, suitability of the
donor and the legal clearances (as laid by THOA-1994), the Transplant
team (Transplant surgeon, Nephrologists, Anesthetists, Nursing staff)
initiates the surgery (under General Anesthesia) in which the healthy
Kidney is harvested from the donor and is grafted (usually on the
right lower abdomen) into the body of the patient.
The Transplant protocol from deceased (cadaver) donor is different
from that of the live related or un-related donors. This difference lies
in the "Brain Stem Death" declaration (by the team of doctors
33
including treating consultant, Neurosurgeon, Neurologists who
minutely examine the patient on ventilator support and affirms that
the patient is in complete and irreversible cessation of all brain functions
that lead to death) and willingness of the relatives to permit retrieval
and transplantation of the kidney for therapeutic purposes. Brain
death must not be confused unconsciousness as the former is an
irreversible process while the later is a reversible one.
The patient may be on short term dialysis even after Transplant from
a deceased donor because during preservation (post retrieval) the
kidney is damaged due to lack of oxygen and blood supply. In cadaver
transplant programs, the donor's (deceased) relatives are not financially
benefited as it is considered to be an auspicious deed by the relatives.
In Post Kidney Transplantation there are certain precautions that must
be taken care of meticulously by the patient (recipient) and their
attendants:
All medications prescribed must be takes regularly and as
prescribed as altering the medication or its dosage, discontinuation
or skipping of doses leads to severe rejections or transplant
failures.
Follow-up with the doctor and laboratory investigations as advised
must be regular.
Weight, blood pressure, urine volume, blood sugar (as advised)
must be monitored.
In emergency situations, the consulting doctor must be informed
of the transplant and the medications prescribed.
All over-the-counter drugs or herbals must be strictly avoided.
The consulting doctor must be immediately informed about any
abnormality (fever, chills, tendency of vomiting).
Proper hygiene, a well balanced diet (canned food must not
consumed) and drinking more than 3 liters of water a day must
be maintained.
34
Regular exercise (excluding vigorous sports like football, boxing)
must be done.
Since transplant patients are more prone to infections due to
immunosuppressants, they must avoid going in crowds, contacts
with pets and should use disposable sterile mask for first three
months in public places.
As for the Donor, lifelong medication will not be needed and post-
discharge from the transplant centre will require two weeks rest with
some medications including antibiotics and painkillers. In case the
donor is an office-goer, duties can be resumed from the 20th day
post discharge from hospital but should avoid strenuous tasks. By
two to three months, a normal life can be led as earlier without any
further medication.
In India, there are an increasing number of patients waiting for kidney
transplantation. Each year, there are 1,50,000 new patients being added
to the previous existing number while only a few actually receive the
transplantation (around 4000 to 4500 per year). Amongst these, many
do not reach Hemodialysis initiation due to lack of optimum
infrastructural support and trained personnel in their region. Further,
the high treatment costs and shortage of organ (particularly deceased
or cadaver donor) plays a crucial role in depriving them with this
curative measure.
It is the need of the hour to spread awareness amongst all about the
relevance of cadaver transplantation and imbibe the cultural and
spiritual urge to Pledge Organs while alive. Such a step will lower the
waiting list of such patients. To quote Rabindranath Tagore: "Death
is not extinguishing the light; it is only putting out the lamp
because the dawn has come."
.
35
Urinary Stone Disease
8
Dr Shailesh Chandra Sahay and Dr Raheel Hasan
Kidney stone can cause most unbearable pain. Stone disease is
common urological disease. But some time kidney stones can exist
silently without any symptom. Stone disease can cause urinary tract
infection and damage to kidney, if not treated timely. Once stone
occurs, its recurrence is common. So understanding, prevention and
care of stone disease is essential.
What is a kidney stone?
A kidney stone is a hard crystal mass formed within the kidney or
urinary tract. Increased concentration of crystals or small particles of
calcium, oxalate, urate, phosphate etc in urine is responsible for the
stone formation.
What are the size, shape and location of urinary stones?
Kidney stones vary in size and shape. It can be smaller than a grain of
sand or can be as large as a tennis ball. The shape of the stone may be
round or oval with smooth surface, such stones cause less pain and
chances of natural removal is high.
What are the types of kidney stones?
There are four types of kidney stones.
1. Calcium stone: This is the most common type of kidney stone,
which occurs in about 70 - 80% cases. Calcium oxalate stones
tend to form when the urine is acidic.
2. Struvite stones: Struvite (Magnesium ammonium phosphate)
stones are less common (about 10 - 15%) and result from
infections in the kidney.
36
3. Uric acid stones: Uric acid stones are not very common (about
5 - 10%) and more likely to form when there is too much uric
acid in the urine and urine is persistently acidic. Uric acid stones
can form in people with gout.
4. Cystine stones: Cystine stones are rare and occur in an inherited
condition called cystinuria.
Factors Contribute to the Formation of Urinary Stone
Factors that increase risk of developing kidney stones are:
Reduced fluid - especially water intake and dehydration.
Family history of kidney stones.
Diet- Consuming a diet high in animal protein, sodium and
oxalate, but low in fiber and potassium rich citrus fruits.
75 % of kidney stones and 95% of bladder stones occur in men.
A person who is bed-ridden or immobile for a long period.
A person living in hot humid atmosphere.
Recurrent urinary tract infections and blockage to the flow of
urine.
Metabolic diseases- Hyperparathyroidism, cystinuria, gout etc.
Use of certain medications: Diuretics and antacids.
What are the symptoms of a urinary stone?
The symptoms of urinary stone may vary with size, shape, and location
of the urinary stone. Common symptoms of urinary stone are:
Abdominal pain.
Frequency of urination and persistent urge to urinate.
Nausea or vomiting.
Passage of blood in urine (haematuria).
Pain and/or burning while passing urine.
If the bladder stone gets stuck at entrance to the urethra, urine
flow suddenly stops during urination.
Passing of stone in urine.
37
Can kidney stones damage the kidney?
Yes. Stones in the kidney or ureter can block or obstruct the flow of
urine within the urinary tract. Such obstruction can cause dilatation
of kidney. Persistent severe dilatation due to blockage can cause kidney
damage in a long term in a few patients.
Diagnosis of urinary stones
Radiological investigations
Ultrasound
X- ray KUB
CT Scan
Intravenous urography (IVU) :IVU test is very reliable at detecting
stones and obstruction. Major benefit of IVU is that it provides
information about the function of the kidney.
Laboratory investigations
Urine tests
Blood tests
Stone analysis
Chemical analysis of stones can establish their composition, which
helps to decide preventive measures and therapeutic plan.
Prevention of urinary stones
All patients who suffered from kidney stone should follow preventive
measures.
General measures
1. Drink lots of fluid: A simple and most important measure to
prevent formation of stone is to drink plenty of water, drink plenty
of water and drink plenty of water. Drink - 12 - 14 glasses (more
than 3 liters) of water per day. To ensure adequate water intake
throughout the day, carry a water bottle with you.
38
Which fluids are preferred to prevent urinary stone?
Intake of fluids such as coconut water, barley or rice water and
citrate-rich fluids such as lemonade, or pineapple fruit juices helps in
the prevention of stone.
Which fluids should be avoided by a person with urinary stone?
Avoid grapefruit, canberry and apple juice; strong tea, coffee, chocolate
and sugar sweetened soft drinks such as colas; and all alcoholic
beverages, including beer.
2. Salt restriction: Avoid excessive salt intake in diet. So avoid pickles,
papad, salty snacks etc. Restrict sodium intake to less than 100 mEq
or 6 gram table salt per day to prevent formation of stone.
3. Decrease intake of animal protein: Avoid non vegetarian food
such as mutton, chicken, fish and egg. These animal containing foods
contain high uric acid and purines and can increase the risk of uric
acid stones and calcium stones.
4. Balanced diet: Eat fruits such as banana, pineapple, blueberries,
cherries, and oranges. Eat vegetables such as carrots and bitter gourd
(karela); squash and bell peppers. Eat high fiber containing foods
such as barely, beans, oats, and psyllium seed. Avoid or restrict refined
foods such as white bread, pastas, and sugar. Kidney stones are
associated with high sugar intake.
5. Other advice: Restrict intake of vitamin C to less than 1000 mg
per day. Avoid large meals late at night. Obesity is an independent
risk factor for stone. So avoid obesity with consumption of balanced
diet.
Restriction of salt intake in diet is very important for prevention of
calcium stones.
39
Treatment of urinary stones
Two major treatment options are:
A. Conservative treatment
B. Surgical treatment
A. Conservative treatment: Large number of kidney stones are
small (less than 5 mm in diameter) enough to pass on its own within
3 to 6 weeks of the onset of symptoms. The aim of conservative
treatment is to relieve symptoms and to help stone removal without
surgical operation.
Immediate treatment of kidney stones: To treat unbearable pain
a patient may requires intra muscular or intravenous administration
of NSAIDs or opioids.
Plenty of fluid intake
Other measures
Maintaining urine pH is essential. Drugs like calcium channel
blockers and alpha-blockers inhibit spasms of ureter and help the
patient to pass the stone in ureter on its own.
B. Surgical treatment: Frequently used surgical methods are
Percutaneous nephrolithotripsy (PCNL), extracorporeal shock wave
lithotripsy (ESWL), ureteroscopy and in rare cases open surgery.
Which patient needs for surgical treatment?
Most patients with small stone can be effectively treated conservatively.
But surgery may be needed to remove kidney stone if:
It causes recurrent or severe pain and does not pass after a
reasonable period of time.
It is too large to pass on its own
It blocks the flow of urine significantly and causes damage to
kidney.
It causes recurrent urinary tract infection or bleeding.
40
1. ESWL - Extra-corporeal shockwave lithotripsy
Lithotripsy is ideal for kidney stones less than 1.5 cm in size or
upper ureteric stones.
In lithotripsy- highly concentrated shock waves or ultra sonic
waves produced by lithotriptor machine break up the stones.
After lithotripsy the patient is advised to drink liberally to tently
used surgical flush out stone fragments.
Lithotripsy is less effective for large stones and in obese patients.
Lithotripsy is not advisable during pregnancy, severe infection,
uncontrolled hypertension, distal obstruction in urinary tract and
bleeding disorders.
2. Percutaneous nephrolithotomy (PCNL)
Percutaneous nephrolithotomy, or PCNL, is an effective method for
removing medium-sized or large (bigger than 1.5 cm) kidney or
ureteral stones.
3. Ureteroscopy (URS)
Ureteroscopy is a highly successful modality for treating stones located
in the mid - and lower ureter. Under anaesthesia, the thin lighted
flexible tube (ureteroscope) equipped with a camera is inserted via
the urethra into the bladder and up the ureter.
Stone is seen through the ureteroscope and depending on the size of
the stone and the diameter of the ureter the stone may be fragmented
and/or removed.
4. Open surgery
Open surgery is most invasive and painful treatment modality for
stone disease requiring five to seven days hospitalization.
With the availability of new technologies, the need for open surgery
has been reduced drastically.
41
When should a patient with kidney stone contact doctor?
Patient with kidney stone should immediately contact doctor if:
Severe pain in abdomen, not relieved with medication.
Severe nausea or vomiting which prevents intake of fluid and
medication.
Fever, chills and burning urination with pain in abdomen.
Blood in urine.
Urine stops totally.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Pushpanjali Life Saver ProgramDokumen2 halamanPushpanjali Life Saver ProgramPushpanjali Crosslay HospitalBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- What Is A Stroke/ Brain Attack?Dokumen6 halamanWhat Is A Stroke/ Brain Attack?Pushpanjali Crosslay HospitalBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Pushpanjali Institute of Cardiac SciencesDokumen2 halamanPushpanjali Institute of Cardiac SciencesPushpanjali Crosslay HospitalBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Connect March 2013Dokumen8 halamanConnect March 2013Pushpanjali Crosslay HospitalBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Connect June 2012Dokumen8 halamanConnect June 2012Pushpanjali Crosslay HospitalBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Medifocus Dec 2012Dokumen67 halamanMedifocus Dec 2012Pushpanjali Crosslay HospitalBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Connect November 2012Dokumen8 halamanConnect November 2012Pushpanjali Crosslay HospitalBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Crosslay Welness ProgrammesDokumen2 halamanCrosslay Welness ProgrammesPushpanjali Crosslay HospitalBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Radiology September 2010Dokumen33 halamanRadiology September 2010Pushpanjali Crosslay HospitalBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Connect October 2011Dokumen8 halamanConnect October 2011Pushpanjali Crosslay HospitalBelum ada peringkat
- Medifocus Diabetes Issue-September 2011Dokumen26 halamanMedifocus Diabetes Issue-September 2011Pushpanjali Crosslay HospitalBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- What Is IVF? A GuideDokumen21 halamanWhat Is IVF? A GuidePushpanjali Crosslay HospitalBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Pediatrics March 2009Dokumen41 halamanPediatrics March 2009Pushpanjali Crosslay HospitalBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Pregnancy October 2009Dokumen38 halamanPregnancy October 2009Pushpanjali Crosslay HospitalBelum ada peringkat
- Medifocus January 2008Dokumen61 halamanMedifocus January 2008Pushpanjali Crosslay HospitalBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Connect October 2010Dokumen8 halamanConnect October 2010Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect March 2011Dokumen8 halamanConnect March 2011Pushpanjali Crosslay HospitalBelum ada peringkat
- ENT October 2007Dokumen50 halamanENT October 2007Pushpanjali Crosslay HospitalBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Cancer April 2008Dokumen33 halamanCancer April 2008Pushpanjali Crosslay HospitalBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Medifocus April 2007Dokumen61 halamanMedifocus April 2007Pushpanjali Crosslay HospitalBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Connect Dec 08Dokumen12 halamanConnect Dec 08Pushpanjali Crosslay HospitalBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Connect Sep 09Dokumen8 halamanConnect Sep 09Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect July 2010Dokumen8 halamanConnect July 2010Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect May 08Dokumen11 halamanConnect May 08Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect Dec 07Dokumen12 halamanConnect Dec 07Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect Sep 08Dokumen11 halamanConnect Sep 08Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect Jan 08Dokumen12 halamanConnect Jan 08Pushpanjali Crosslay HospitalBelum ada peringkat
- Connect March 07Dokumen12 halamanConnect March 07Pushpanjali Crosslay HospitalBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Wonder Drugs On The Horizon: Dr. Malay NandyDokumen19 halamanWonder Drugs On The Horizon: Dr. Malay NandyPushpanjali Crosslay HospitalBelum ada peringkat
- Brain Kidney Interactions in Post Traumatic Brain Death PDFDokumen6 halamanBrain Kidney Interactions in Post Traumatic Brain Death PDFspeed_09Belum ada peringkat
- Michael Goss Death CertificateDokumen1 halamanMichael Goss Death Certificateapi-239096088Belum ada peringkat
- NCM 105 Lec: Nutriton and Diet Therapy Project On Therapeutic DietsDokumen15 halamanNCM 105 Lec: Nutriton and Diet Therapy Project On Therapeutic DietsVinz OñoBelum ada peringkat
- Chronic Kidney DiseaseDokumen6 halamanChronic Kidney Diseaseashi leginBelum ada peringkat
- Drug Name Gemcitabine: Synonym (S) : Common Trade Name (S) : ClassificationDokumen8 halamanDrug Name Gemcitabine: Synonym (S) : Common Trade Name (S) : ClassificationOka Robi MuhammadBelum ada peringkat
- ThooeoeDokumen1.142 halamanThooeoelapyem thomasBelum ada peringkat
- NCM 118 ReviewerDokumen14 halamanNCM 118 ReviewerMarceil MortelBelum ada peringkat
- Managing Hyperglycaemia in People With DKD - Final DraftDokumen90 halamanManaging Hyperglycaemia in People With DKD - Final DraftRiched LhyneBelum ada peringkat
- Chronic Kidney DiseaseDokumen54 halamanChronic Kidney DiseaseJosh Matthew RosalesBelum ada peringkat
- Approach To The Adult With Metabolic Acidosis PDFDokumen19 halamanApproach To The Adult With Metabolic Acidosis PDFAdi CărbunaruBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Bonello 2018Dokumen15 halamanBonello 2018Илија РадосављевићBelum ada peringkat
- Diabetic Kidney DiseaseDokumen69 halamanDiabetic Kidney DiseaseLavina JainBelum ada peringkat
- Grand Coaching: Medical Surgical NursingDokumen22 halamanGrand Coaching: Medical Surgical NursingEsarpy (Nana)Belum ada peringkat
- Internal 8.2022Dokumen15 halamanInternal 8.2022Nimer Abdelhadi AliBelum ada peringkat
- Chronic Kidney DiseaseDokumen11 halamanChronic Kidney DiseaseSalma Mohamed RezkBelum ada peringkat
- NURSING CARE PLAN - DialysisExpoDokumen2 halamanNURSING CARE PLAN - DialysisExpoDANIELLA MALARANG MELBelum ada peringkat
- Dehydration Pathway 2016Dokumen3 halamanDehydration Pathway 2016rochmandrg dokter gigiBelum ada peringkat
- Unleash Benefit of Metoprolol in CCS Applying Evidence Into PracticeDokumen35 halamanUnleash Benefit of Metoprolol in CCS Applying Evidence Into PracticeEdelweisscynaBelum ada peringkat
- Acute Renal FailureDokumen28 halamanAcute Renal FailureAs SyarifBelum ada peringkat
- 25F AXA HealthMax 20P 1.2M (Trad)Dokumen19 halaman25F AXA HealthMax 20P 1.2M (Trad)Aljes ReyesBelum ada peringkat
- 7 Ways To Lower Creatinine Level NaturallyDokumen20 halaman7 Ways To Lower Creatinine Level NaturallyAmjad Pathan100% (1)
- Healing Siddha Medicine PDFDokumen4 halamanHealing Siddha Medicine PDFPugazhendi ManiBelum ada peringkat
- Nursing Practice IVDokumen16 halamanNursing Practice IVJohn wewBelum ada peringkat
- Genitourinary 2010 (Rationale)Dokumen13 halamanGenitourinary 2010 (Rationale)Wenzy CruzBelum ada peringkat
- Ketorolac (Systemic) - Drug Information - UpToDateDokumen42 halamanKetorolac (Systemic) - Drug Information - UpToDateJosué Pablo Chicaiza AbadBelum ada peringkat
- Pathophysiology of Burns - 1Dokumen32 halamanPathophysiology of Burns - 1Y. Beatrice Abigail50% (2)
- 2013 NICE Guideline HyperphosphatemiaDokumen264 halaman2013 NICE Guideline HyperphosphatemiaSilvana M MendonçaBelum ada peringkat
- Case AKIDokumen5 halamanCase AKIVivi DeviyanaBelum ada peringkat
- MTRH I.Med ProtocolsDokumen42 halamanMTRH I.Med ProtocolsRoberto Maina100% (3)
- 1 - 6 Managing Feline Renal Disease PDFDokumen7 halaman1 - 6 Managing Feline Renal Disease PDFIme PrezimeBelum ada peringkat
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (27)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (81)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)