Immunohist Amyloid 2006 Jun - Am J Surg Pathol
Diunggah oleh
esmelloDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Immunohist Amyloid 2006 Jun - Am J Surg Pathol
Diunggah oleh
esmelloHak Cipta:
Format Tersedia
ORIGINAL ARTICLE
Immunohistochemical Classification of Amyloid in Surgical Pathology Revisited
Anja Kebbel, MD* and Christoph Rocken, MD, PhDw
Abstract: We aimed to reassess the suitability of immunohistochemical classication of amyloid in surgical pathology. One hundred sixty-nine biopsies from 121 patients diagnosed with amyloid during the period from 1994 to 2004 were included. Amyloid was classied immunohistochemically, using antibodies directed against amyloid P-component, AA amyloid, apolipoprotein AI, brinogen, keratoepithelin, lactoferrin, lysozyme, b2-microglobulin (b2M), immunoglobulin-derived l-light and k-light chains, and transthyretin. Amyloid was most commonly present in biopsies from the hepatogastrointestinal tract. The deposits were classied immunohistochemically in 156 (92%) biopsies. In 13 biopsies of 12 patients, amyloid remained unclassied. AL amyloidosis was diagnosed in 76 (45%) biopsies and was further categorized into AL amyloid of k-light chain origin [32 (42%) biopsies] or l-light chain origin [20 (26%)]. In 24 (32%) biopsies, the amyloid deposits did not show unequivocal staining for l-light or k-light chain. However, these cases were categorized as probably AL amyloid, not otherwise specied, because no other antibody showed unequivocal staining of the amyloid deposits. AA amyloidosis was diagnosed in 32, ATTR amyloidosis in 21, and AApoAI amyloidosis in 3 biopsies. Other types of amyloid included AKer and ALac amyloids each in 1, and ALys and ACal amyloids each in 2 biopsies. Ab2M amyloid was not diagnosed in any case. Immunohistochemical classication of amyloid still poses problems. Although classication of AA, AApoAI, ALys, ALac, and ATTR amyloids is relatively straightforward, classication of AL amyloid and rare hereditary amyloidoses is a serious obstacle and sometimes even impossible when conclusive clinical information or additional protein biochemical or molecular biologic studies are not available. Key Words: amyloid, immunohistochemistry (Am J Surg Pathol 2006;30:673683)
only be diagnosed morphologically, placing the surgical pathologist into a crucial position. No clinical, serologic, or radiologic procedure has replaced the investigation of a tissue sample to provide denitive diagnostic proof. After the histologic diagnosis of amyloid, it is mandatory to classify the amyloid protein(s) to assess patient prognosis and treatment, which may include chemotherapy or organ transplantation.26,37 Tissue specimens submitted to histology are usually formalin xed and paran embedded, and rst using immunohistochemistry to classify amyloid in these specimens is an obvious step.36,37 The immunohistochemical classication of amyloid has been validated by several studies, most of which were published between 10 and 20 years ago.25,36,46 Within the last 10 years, several new amyloid proteins have been identied. Medical treatment for amyloidcausing diseases has changed, aecting the prevalence of the dierent amyloid types, necessitating a reevaluation of the immunohistochemical classication of amyloid in surgical pathology. In this study, we reviewed all amyloid-containing biopsy specimens submitted to our department within the last 10 years, and assessed the suitability of immunohistochemistry for the classication of amyloid.
MATERIAL AND METHODS Patients
All patients diagnosed with amyloid during the period from 1994 to 2004 at the Department of Pathology of the University of Magdeburg and referred samples from other surgical pathologists and hospitals throughout Germany were included in this retrospective study. Amyloid deposits were studied in 169 biopsies from 121 patients, including 59 women and 62 men (women: men = 1:1.1). The mean age at diagnosis was 62 years (range 21 to 88).
myloid denes a heterogeneous group of diseases of diverse origin characterized by proteinaceous tissue deposits that show green birefringence in polarized light after Congo red staining.30,37 By denition, amyloid can
Histology
All tissue specimens were xed in formalin and embedded in paran. Deparanized sections were stained with hematoxylin and eosin. The presence of amyloid was demonstrated by Congo red staining using polarization and uorescence microscopy.23,30
From the *Department of Pathology, Otto-von-Guericke-University, Magdeburg, Germany; and wDepartment of Pathology, Charite University Hospital, Berlin, Germany. Reprints: Prof Dr med Christoph Rocken, MD, PhD, Department of Pathology, Charite University Hospital, Schumannstr. 20/21, D-10117 Berlin, Germany (e-mail: christoph.roecken@charite.de). Copyright r 2006 by Lippincott Williams & Wilkins
Immunohistochemistry
Commercially available monoclonal antibodies directed against AA amyloid (1:400) and calcitonin (1:100), and polyclonal antibodies directed against
Am J Surg Pathol
Volume 30, Number 6, June 2006
673
Kebbel and Rocken
Am J Surg Pathol
Volume 30, Number 6, June 2006
amyloid P-component (AP) (1:1600), brinogen (1:1000), lactoferrin (1:800), lysozyme (1:3000), transthyretin (TTR) (1:500), l-light chain (1:10.000), k-light chain (1:10.000), and b2-microglobulin (b2M; 1:2000) were purchased from DAKO, Hamburg, Germany. A noncommercially available polyclonal antibody directed against apolipoprotein AI (anti-apoAI; dilution 1:1500) was generated using NH2-DEPPQSPWDRVKDLACCONH2 and NH2-CVLKDSGRDYVSQFEG-CONH2 as immunogen, as described elsewhere.27 A noncommercially available antibody directed against l-light chain (anti-AL1 antibody; dilution 1:1000) was generated by immunizing rabbits with amyloid proteins extracted from amyloid tissue of a patient with systemic AL(l) amyloidosis.3 Immunoglobulin G was obtained by using HiTrap protein G columns (Amersham Pharmacia Biotech, Freiburg, Germany). The specicity of the anti-apoAI antibody was tested by Western blotting, using apolipoproteins puried from human serum, and by immunostaining of tissue sections from atherosclerotic arteries with intimal amyloid deposits. Antibodies directed against keratoepithelin (KE2 and KE15; both dilution 1:10) were kindly provided by Dr Daniel Schorderet.41 Before immunostaining, the specimens were pretreated with 10 mM ethylenediaminetetraacetic acid (2 10 min, 450 W microwave oven; AP, apoAI, and TTR) or with H2O2 (15 min, b2M). The remaining antibodies did not require antigen retrieval or pretreatment with H2O2. Immunoreactions were visualized with the avidin biotin complex method applying a Vectastain ABC alkaline phosphatase kit (Biogene-Alexis GmbH, Grunberg, Germany) or an iVIEW DAB Detec tion kit (Ventana, Illkirch CEDEX, France). Neufuchsin and 3,3-diaminobenzidine-tetrahydrochloride, respectively, served as chromogens. The specimens were counterstained with hematoxylin. The specicity of immunostaining was veried using specimens containing known classes of amyloid showing even immunostaining of the entire amyloid deposits (AA amyloid, apoAI, b2M, TTR, l-light chain), using positive controls recommended by the manufacturers (remaining antibodies) and by omitting the primary antibodies. The specicity of our immunohistochemical classication protocol had been validated in several of our biopsy cases by Western blotting and/or amino acid sequencing of the proteins extracted from amyloidotic tissue, and by molecular biologic studies demonstrating gene mutations.3,11,3133,38,41 Until 2002, amyloid was classied immunohistochemically by using routinely a panel of antibodies directed against AP, AA amyloid, b2M, l-light chain and k-light chain, and TTR. Fat aspiration biopsies were usually stained with a single antibody (anti-AA amyloid antibody), as only 2 to 3 slides were submitted allowing Congo red staining and 1 or 2 additional immunohistochemical stains. Starting in 2003, we classied amyloid by using routinely a panel of antibodies directed against AP, AA amyloid, apoAI, b2M, fribrinogen, lysozyme, l-light chain and k-light chain, and TTR. Antibodies directed
against calcitonin, gelsolin, keratoepithelin, or lactoferrin were only applied where appropriate, that is, medullary cancer of the thyroid or corneal specimens with amyloid deposits. For purposes of the current study, missing immunostains for apoAI, fribrinogen, and lysozyme were accomplished where possible, that is, tissue blocks or spare sections were still available. Finally, 92 biopsies were immunostained with antibodies directed against AP, AA amyloid, apoAI, b2M, fribrinogen, lysozyme, l-light chain and k-light chain, and TTR; 51 biopsies were stained with antibodies directed against AP, AA amyloid, b2M, l-light chain and k-light chain, and TTR. Eleven biopsies were stained only with an antibody directed against AA amyloid (mostly fat aspiration biopsies). Six biopsies were stained with antibodies directed against l-light chain and k-light chain only. These were usually patients with multiple biopsies, for example, from the gastrointestinal tract, where at least 1 biopsy was stained with all antibodies. Two biopsies were stained with antibodies directed against AP and AA amyloid and were already histologically shown to suer from AA amyloidosis. All cases were reviewed by 2 observers. The slides were reexamined in light of further clinical information and follow-up biopsies, where available. The quality of the biopsy, immunohistochemical typing of the amyloid bril protein and further clinical information from hospital records and les were recorded. Additional or repeat immunostains were performed by dierent opinions as to the observers. The distribution pattern of amyloid was documented for each biopsy and a correlation was sought between the immunohistochemically classied bril protein and the underlying disease. The nomenclature of amyloid and amyloidosis used in this study follows the recommendations outlined by the International Nomenclature Committee on Amyloidosis.17,47
RESULTS
One hundred sixty-nine biopsies were obtained from 121 patients and 38 dierent organ and tissue sites. A single biopsy was available from 91 patients, more than 1 biopsy (up to 6) was available from 30 patients. A total of 77 (46%) biopsies from 53 patients originated from the hepatobiliary and gastrointestinal tract and these most frequently of the colon [20 biopsies (26%)], followed by stomach [16 (21%)], rectum [18 (23%)], liver [14 (18%)], small intestine [5 (6%)], pharynx [2 (3%)], esophagus [1 (1%)], and gall bladder [1 (1%)]. Ninety-two biopsies (54%) from 81 patients were from nongastrointestinal origin, including respiratory tract [14 (15%)], heart [8 (9%)], kidneys [6 (7%)], fat tissue [11 (12%)], supportive tissue [6 (7%)], and carpal tunnel ligament [5 (5%)] (Table 1).
Patient Age and Sex (Table 2)
Patient age ranged from 21 to 88 years. Amyloid was diagnosed most frequently in the seventh decade of patient life [40 (33%) of 121 patients], followed by the
r
674
2006 Lippincott Williams & Wilkins
Am J Surg Pathol
Volume 30, Number 6, June 2006
Classification of Amyloid in Surgical Pathology
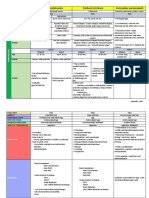
FIGURE 1. Illustration of the immunohistochemical classification of amyloid in 3 biopsy cases. Vascular AL amyloid deposits llight chain origin in a rectal biopsy (left 2 panels). Note weak congophilia, commonly observed in AL amyloidosis, and homogenous staining with an antibody directed against AL amyloid proteins (anti-AL1). Interstitial AA amyloid deposits in a thyroid gland (central 2 panels). Note additional weak and uneven immunostaining with the anti-TTR antibody, which was attributed to contamination of the amyloid deposits by a serum protein. Vascular and interstitial cardiac amyloid deposits in a patient with plasmacytoma (right 2 panels). The amyloid deposits stained with antibodies directed against apoAI, fibrinogen, klight chain and TTR. Although AL amyloidosis of k-light origin was highly likely, amyloid deposits of other origins could not be excluded solely on immunohistochemical grounds. Congo red staining in polarized light (left and central panels) and fluorescence microscopy (right panel). Antibodies directed against AP, AA amyloid (AA), apoAI, fibrinogen, lysozyme, b2M, immunoglobulin derived l-light chain and k-light chain, and TTR. Hematoxylin counterstain. Original magnifications 200.
eighth decade [29 (24%)], and the sixth decade [17 (14%)]. Amyloid was found less frequently in the fth [13 (11%)], nineth [11 (9%)], and fourth decade [9 (7%)]. Only 1 (1%) patient was less than 30 years old at the time of diagnosis (Table 2).
Immunohistochemistry
The amyloid deposits were classied immunohistochemically in 156 (92%) of 169 biopsies obtained from 109 of 121 patients. In 13 (8%) biopsies of 12 patients, amyloid remained unclassied for the following reasons: (a) in 2 biopsies from 2 patients the amount of material obtained was too small to allow immunohistochemical staining, (b) in 5 cases no spare sections were available, (c)
r
and in 6 biopsies from 5 patients, none of the antibodies immunostained the amyloid deposits. AL amyloidosis was diagnosed in 76 (45%) of 169 biopsies and was further categorized into AL amyloid of k-light chain origin [32 (42%) biopsies] or l-light chain origin [20 (26%)] (Fig. 1, left 2 panels). In 24 (32%) biopsies, the amyloid deposits did not show unequivocal staining for k-light chain or l-light chain. However, these cases were categorized as probably AL amyloid, not otherwise specied (n.o.s.) (Table 1), because no other antibody showed unequivocal staining of the amyloid deposits, and the diagnosis was supported by clinical ndings, for example, Bence Jones-proteinuria and monoclonal gammopathy, or additional histopathologic
2006 Lippincott Williams & Wilkins
675
Kebbel and Rocken
Am J Surg Pathol
Volume 30, Number 6, June 2006
TABLE 1. Correlation Between the Origin of the Biopsy Specimens and the Clinicopathologic Classification of the Amyloid Deposits
Amyloid No. Biopsies n (%) Hepatogastro-intestinal tract Colon Rectum Stomach Liver Small intestine Esophagus Gall bladder Respiratory tractw Heart Urogenital tract Kidney Seminal vesicle Urinary bladder Penile glans Portio Renal pelvis and ureter Prostate Other organs/tissues Fat aspiration biopsy Supportive tissuez Lymph node Oral cavityy Thyroid gland Pharynx Mamma Amyloid tumor Cornea Skeletal muscle Brain OthersJ Total n (%) 75 (44) 20 18 16 14 5 1 1 14 (8) 8 (4) 15 (9) 6 3 2 1 1 1 1 57 (34) 11 6 4 5 3 2 2 2 2 2 1 17 169 (100) Probably AL 1 2 1 2 1 7 3 1 1 2 3 24 (14) AL (j) 3 1 3 1 1 4 2 2 1 5 1 1 2 2 3 32 (19) AL (k) 8 2 1 2 2 2 1 1 1 20 (12) AA 6 3 7 5 1 1 1 5 2 1 32 (19) ATTR 2 2 2 3 1 1 1 1 1 7 21 (12) AApoAI 1 1 1 3 (2) Other* 3 4 3 4 2 1 1 2 1 2 1 24 (14) Unclassied 1 1 3 1 5 1 1 13 (8)
*Other types of amyloid included AKer amyloid (1 patient), ALac amyloid (1), ALys amyloid (1), and 10 patients with probably 2 and more types of amyloid (see in detail Table 4). wRespiratory tract included biopsies of the lung (7 patients), bronchus (5) and nasopharynx (3). zSupportive tissue included pelvic bone (4), bone marrow (3), and cyst of the jaw (1). yOral cavity included tongue (3), residual cyst (1), and tonsil (1). JOthers included carpal tunnel ligament (5 patients), synovia (4), skin (3), ligament (2), retroperitoneum (1), parailiacal tumor (1), and residual cyst (1).
results, for example, histologic evidence of a plasmacytoma. AA amyloidosis was diagnosed in 32 (19%), ATTR amyloidosis in 21 (12%), and AApoAI amyloidosis in 3 (2%) of the 169 biopsies. Other types of amyloid included AKer amyloid in 1 (0.5%),41 ALac amyloid 1 (0.5%), ALys amyloid 2 (1%),31 and ACal amyloid in 2 (1%) of 169 biopsies. Each case was reassessed and the diagnosis, including unclassiable cases, was conrmed in 162 (96%) of 169 biopsies. In 9 of the 162 biopsies, additional immunohistochemical staining allowed the classication. Seven biopsies which were initially categorized as probably AL amyloid n.o.s. were nally subclassied into AL(k) or AL(l) amyloidosis. In 9 (5%) of 169 biopsies, the initial classication could not be conrmed. Reasons for this were (a) AL amyloidoses of l-light chain or k-light chain origin denite could not be conrmed and had to be recategorized into probably AL amyloidosis n.o.s. (4 biopsies); (b) probably AL amyloidosis n.o.s. had to be recategorized into denite
AL amyloidosis k-light chain origin (1 biopsy); (c) denite AL amyloidosis l-light chain origin had to be recategorized into denite AL amyloidosis k-light chain origin (1 biopsy); (d) the immunohistochemical staining had seriously deteriorated over time and prohibited reclassication or the amount of tissue was too small to allow additional immunohistochemical staining (2 biopsies); (e) nally, in 1 patient, hepatic amyloid deposits had been initially classied as AL amyloid, while strong immunostaining with the anti-apoAI antibody was considered as suggestive for AApoAI amyloidosis on reevaluation. However, immunostaining of intestinal amyloid deposits supported the diagnosis of AL amyloidosis and the case was nally classied as probable deposition of multiple amyloid proteins (patient no. 15, Table 4). Amyloid, irrespective of its origin or site of deposition, always stained with the antibody directed against AP (Fig. 1). However, AL amyloid often showed a spotty staining with the anti-AP antibody.
r
676
2006 Lippincott Williams & Wilkins
Am J Surg Pathol
Volume 30, Number 6, June 2006
Classification of Amyloid in Surgical Pathology
TABLE 2. Correlation of Amyloid Proteins With Patient Age and Sex
Age Probably AL amyloid, n.o.s. AL (k) amyloid AL (l) amyloid ATTR amyloid AA amyloid AApoAI amyloid Other types of amyloid Amyloid unclassied Total 23 (41) 21 12 20 18 2 13 (38) (21) (17) (15) (2) (11) 1 (4) 4 (17) 3 1 1 2 1 1 (14) (8) (5) (11) (50) (8) 3 (13) 3 2 2 1 1 4 (14) (17) (10) (6) (50) (31) 6 (26) 7 6 7 5 (33) (50) (35) (28) 8 (35) 6 3 4 4 (29) (25) (20) (22) 1 (4) 1 (5) 6 (30) 1 (5) Gender 11 (48) 10 5 10 9 1 6 (48) (42) (50) (50) (50) (46) 12 (52) 11 7 10 9 1 7 (52) (58) (50) (50) (50) (54) No. Patients n (%) 20 to 29 30 to 39 40 to 49 50 to 59 60 to 69 70 to 79 80 to 89 Unknown Women n (%) Men n (%)
6 (33) 1 (8) 2 (15)
4 (31) 5 (42) 40 (33)
1 (8) 3 (25) 29 (24) 3 (25) 11 (9) 1 (1)
12 (10) 121 (100) 1 (1) 9 (7) 13 (11)
1 (8) 17 (14)
7 (58) 59 (49)
5 (42) 62 (51)
Correlating patient age with the type of amyloid, it was interesting to note that AL amyloid showed a peak in the seventh and eighth decade, whereas ATTR and AA
amyloids each showed 2 peaks: ATTR amyloid in the seventh and nineth decade, and AA amyloid in the fourth and seventh decade (Table 2). No correlation was found
TABLE 3. Correlation Between Amyloid Protein and Clinical Information
Amyloid Clinical Information Plasmacytoma Amyloid Monoclonal gammopathy Abscess Cardiac failure Tumor Nephrotic syndrome Gastritis and hepatosplenomegaly Leucocytosis Squamous cell carcinoma Endocarditis Gastritis Lymphadenopathy Crohn disease Rheumatoid arthritis Systemic lupus erythematodis Tuberculosis Familial mediterranean fever Chronic pneumonia Rosai-Dorfman disease Carpal tunnel syndrome Colon cancer Bone infarction (femur) Mantle cell lymphoma and carpal tunnel syndrome Neuropathy, axonal Renal cell carcinoma Hysterectomy Gastrointestinal bleeding Cardiomyopathia Keratoplasty Breast cancer Medullary thyroid carcinoma and rheumatoid arthritis Prostate cancer Urinary bladder cancer Total n (%) No clinical information n (%) No. Patients n 15 (20) 6 (8) 2 (3) 1 1 2 (3) 2 (3) 1 1 1 1 1 1 1 11(15) 3 (4) 2 (3) 1 1 1 4 (5) 1 1 1 1 1 1 1 1 1 1 1 3 (4) 1 74 (61) 47 (39) Probably AL n.o.s. 3 (20) 3 (50) 1 (50) 1 1 1 (50) AL(j) 7 (47) 2 (33) 1 (50) AL(k) 2 (13) AA ATTR AApoAI Other* 2 (13) Unclassiedw 1 (6) 1 (17)
1 (50) 1 (50) 1 1 1 1 1 (50)
1 1 1 8 (73) 2 (67) 2 1 1 1 4 1 1 1 1 1 1 1 1 1 1 1 3 1 10 (83) 2 (17) 3 (27) 1 (33)
10 (43) 13 (57)
15 (71) 6 (29)
6 (50) 6 (50)
15 (83) 3 (17)
10 (50) 10 (50)
1 (50) 1 (50)
7 (54) 6 (46)
*AKer, ACal amyloid, ALys, AFib, ALac amyloid and two type amyloidoses. wNo classication could be made due to lack of further specimens to support the suspected amyloid classication correlated with the underlying disease.
2006 Lippincott Williams & Wilkins
677
Kebbel and Rocken
Am J Surg Pathol
Volume 30, Number 6, June 2006
between the type of amyloid protein and patient gender (Table 2).
Correlation of Amyloid Fibril Proteins With Clinical Information (Table 3)
Clinical information was documented in 74 (61%) of 121 patients. AL amyloidosis (either of l-light chain or k-light chain origin) was commonly associated with plasmacytoma, AA amyloidosis with a chronic inammatory disease, and ATTR amyloidosis was commonly associated with carpal tunnel syndrome (Table 3). In the minority of our biopsy cases (39%), no clinical information was provided. However, the diagnosis of amyloid was only rarely suspected clinically.
Immunostaining by More Than a Single Antibody (Table 4)
Immunostaining by more than a single antibody, excluding AP, was apparent in 51 of 169 biopsies and could be divided into 4 groups. Group 1 was the second largest group and consisted of 18 biopsies. Two or more antibodies immunostained the amyloid deposits, but only one of these antibodies demonstrated even or homogeneous staining of the entire deposit, which was interpreted as evidence of the amyloid protein (Fig. 1, central 2 panels). The remaining antibodies, most commonly the antil-light chain, antik-light chain, or anti-TTR antibody showed uneven and scattered staining of some deposits, while other amyloid deposits in the same specimen were immunonegative. In these cases, the uneven immunoreaction of amyloid was not interpreted as an identication of an amyloid protein. Group 2 comprised the largest group and consisted of 19 biopsies in which the immunoreaction was inhomogeneous for 2 or more antibodies. In 10 biopsies, antil-light chain and antik-light chain antibodies, in addition with 1 or 2 other antibodies showed uneven, scattered, and sometimes weak staining of some deposits. As none of the antibodies showed strong and even staining, these cases were classied as probably AL amyloid n.o.s. The other 9 cases showed staining with either the anti-l or the antik-light chain antibody, in addition with 1 or 2 other antibodies. Diagnosis of AL amyloidosis was reached on the basis of light chain restriction, that is, amyloid stained only with antil-light chain or antik-light chain antibodies. Group 3 included 10 biopsies from 8 patients in which immunohistochemical classication led us to suspect the presence of 2 dierent types of amyloid within the same deposit. In 6 of these biopsies, 2 antibodies demonstrated even, homogeneous staining of the amyloid deposits. In the remaining 4 biopsies, only 1 antibody demonstrated an even or homogeneous staining, but either anti-l or anti-k additionally showed a weak staining as well (Fig. 1, right 2 panels). Group 4 consisted of 4 biopsies from 3 patients in whom irregular immunostaining by 1 antibody was evident, but classication was impossible. However, in 2 of these cases, a tentative diagnosis could be made. The
underlying disease of plasmacytoma suggested that, in 1 case, the diagnosis of probably AL amyloidosis n.o.s. was most likely. The other biopsy was obtained from a seminal vesicle and showed a characteristic subepithelial deposition of amyloid typical for localized seminal vesicle amyloid, which is known to originate from semenogelin.24 Although AApoAI and ATTR amyloidosis were characterized by a strong and even immunostaining of the entire amyloid deposits with the antibodies directed against apoAI and TTR, respectively, other types of amyloid also often showed some staining with these antibodies, which, however, was spotty and often only focal: focal or spotty immunostaining with the antiapoAI antibody was found in 17 (23%) of 73 biopsies and with the anti-TTR antibody in 17 (16%) of 109 biopsies. Similarly, focal or spotty immunostaining of some amyloid deposits was observed with antibodies directed against l-light chain [9 (11%) of 85 biopsies], k-light chain [8 (10%) of 79], brinogen [9 (11%) of 79], and b2M [6 (5%) of 120]. In contrast, antibodies directed against AA amyloid and lysozyme stained only AA and ALys amyloids, respectively.
Multiple Types of Amyloid
Case Descriptions Ten (8%) of 121 patients showed immunohistochemical staining patterns (corresponding to groups 1 to 3) suggestive for the presence of multiple types of amyloid. The mean age was 57.9 years with a range of 34 to 72. Female to male ratio was 0.8. In 5 cases (patient nos. 34, 35, 37, 38, 39) there was only 1 single biopsy (colon, heart, liver, retroperitoneum, or rectum) available from each patient. An even and strong immunostaining of intestinal amyloid was found with antibodies directed against AA amyloid and TTR in patient no. 34 compatible with AA and ATTR amyloids. Patient no. 35 showed homogeneous immunostaining of hepatic amyloid with antillight chain, antik-light chain and anti-TTR antibodies, compatible with AL and ATTR amyloids. Patient no. 37 suered from a plasmacytoma of k-light chain type but showed homogeneous immunostaining of heart amyloid with antik-light chain, anti-TTR, anti-apoAI, and antibrinogen antibodies (Fig. 1, right 2 panels). Patient nos. 38 and 39 showed strong immunostaining of rectal and retroperitoneal amyloid deposits with anti-apoAI and antik-light chain antibodies, compatible with AApoAI and AL(k) amyloids. Two or more biopsies from dierent organs (stomach, bone marrow, and heart; colon and stomach; liver and rectum; twice liver, colon, rectum, and fat tissue) were available in another set of 4 patients (Patient nos. 8, 15, 26, 36). The diagnosis of more than 1 amyloid disease was conrmed by the concomitant biopsies, that is, staining of amyloid deposits with more than 1 antibody was found in 2 dierent biopsies (Table 4). One patient suered from rheumatoid arthritis with AA amyloid in the fat tissue sample and from a medullary thyroid carcinoma with calcitonin-immunoreactive amyloid deposits in a lymph node metastasis.
r
678
2006 Lippincott Williams & Wilkins
Am J Surg Pathol
Volume 30, Number 6, June 2006
Classification of Amyloid in Surgical Pathology
TABLE 4. Immunostaining With More Than One Single Antibody
Patient No. Material Group1 1 2 3 4 5 6 7 8 9 10 11 11 12 13 14 15 15 16 Group 2 17 15 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 32 33 Group 3 34 35 36 37 26 26 38 39 8 36 Group 4 40 41 42 42 Stomach Stomach Stomach Thyroid gland Penile glans Skin Bone Stomach Rectum Colon Colon Lung Carpal tunnel Colon Small intestine Liver Liver Pharynx Underlying Disease Rosai-Dorfman disease Rheumatoid arthritis Tuberculosis Familial mediterranean fever Nephrotic syndrome Plasmacytoma Monoclonal gammopathy Crohn disease Carpal tunnel syndrome Colon cancer Renal cell carcinoma Tumor AA Aj Ak ATTR A2M ApoAI AFib x x x x x (x) (x) x x x x x (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) x x x x x (x) (x) (x) (x) (x) (x) (x) (x) x x x (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) (x) x (x) (x) (x) (x) (x) (x) x x x (x) (x) (x) (x) (x) (x) (x) (x) (x) x x x x x x (x) (x) (x) (x) (x) (x) (x) n.s.a. (x) n.s.a. n.s.a. (x) n.s.a. (x) n.s.a. n.s.a. n.s.a. (x) (x) x x x (x) (x) (x) (x) (x) n.s.a. n.s.a. (x) (x) (x) n.s.a. (x) n.s.a. n.s.a. (x) (x) n.s.a. x x x n.s.a. (x) (x) n.s.a. n.s.a. n.s.a. n.s.a. (x) (x) (x) Diagnosis AA AA AA AA AL(k) AL(k) AL(k) AL(k) (+ATTR s.c.b.) AL(k) AL(l) AL(l) AL(l) ATTR ATTR ATTR AApoAI (+AL s.c.b.) AApoAI (+AL s.c.b.) AApoAI
Bronchus Colon Small intestine Lung Lung Nasopharynx Tumor Kidney Kidney Renal pelvis and ureter Rectum Heart Mamma Amyloid tumor Kidney Endocarditis Pharynx Plasmacytoma Lung Lymph node Lymphadenopathy Lymph node Plasmacytoma Rectum Plasmacytoma Rectum Colon Liver Liver Heart Stomach Bone marrow Rectum Retroperitoneum Colon Rectum Tonsil Seminal vesicle Skin Muscle
Probably AL Probably AL (+AApoAI s.c.b.) Probably AL (x) Probably AL Probably AL Probably AL n.s.a. Probably AL n.s.a. Probably AL Probably AL (x) Probably AL (x) AL(k) (+AFib s.c.b.) n.s.a. AL(k) (x) AL(k) (x) AL(k) n.s.a. AL(l) n.s.a. AL(l) AL(l) AL(l) AL(l) AA + ATTR AL + ATTR AL(k) + ATTR x AL(k) (AApoAI, ATTR, AFib) x AL(k) +AFib x AL(k)+AFib AApoAI + AL(k) AApoAI + AL(k) n.s.a. ATTR + AL(k) (x) ATTR + AL(k) Probably AL Unclassied Unclassied Unclassied
Plasmacytoma
Cardiomyopathy Plasmacytoma Plasmacytoma Prostate cancer
(x)
s.c.b. indicates see concomitant biopsy. x indicates even and homogenous and (x) indicates uneven, inhomogeneous or irregular immunostaining.
DISCUSSION
The surgical pathologist has various obligations after amyloid had been found in a biopsy or resection specimen. The clinical signicance has to be assessed, as not all amyloid deposits found in surgical pathology specimens are related to a systemic disease or are
r
clinically relevant. A large number of dierent amyloid diseases have to be considered, including local and systemic varieties. The amyloid deposits have to be classied and the specic amyloid type found has to be related to the specic amyloid disease. The immunohistochemical classication of amyloid was validated
2006 Lippincott Williams & Wilkins
679
Kebbel and Rocken
Am J Surg Pathol
Volume 30, Number 6, June 2006
between 8 and 20 years ago.1,2,4,7,8,10,12,13,25,36,43,46 Within the last 10 years, several new amyloid proteins had been identied, and medical treatment of amyloid-causing diseases has changed, which putatively aects the prevalence of individual amyloid types and necessitates a reevaluation of the immunohistochemical classication of amyloid in surgical pathology. Noncommercially available antibodies were used by several previous investigations,25,36,43,46 which has limited a broader application in surgical pathology, although this study also applied several commercially available antibodies. Similar to our previous investigation, amyloidcontaining biopsy specimens were obtained from various dierent anatomical sites (Table 1) including gastrointestinal tract, respiratory tract, heart, urogenital tract, head and neck region, and many others. Among these, biopsies from the hepatogastrointestinal tract were still the most common.36 This is partly due to the fact that the gastrointestinal tract, in general, is a common biopsy site, leading to the detection of amyloid without prior clinical suspicion. Symptomatic hepatogastrointestinal amyloidosis also leads to a histologic investigation. This mainly relates to liver biopsies for the investigation of hepatosplenomegaly and pathologic liver function tests. A few biopsies obtained from the stomach and colorectum were taken to investigate gastrointestinal bleeding related to amyloid deposition. Finally, rectal biopsies are commonly used to search for amyloid in suspected cases. The rectal biopsy was introduced by Joseph Gafni and Ezra Sohar9 in 1960 and has become a standard procedure for biopsy conrmation of amyloid. Biopsies from the upper gastrointestinal tract became favorable with the advent of more sophisticated endoscopic tools. Amyloid has been found in gastric and duodenal biopsies of approximately 7% to 13.3% of the patients suering from rheumatoid arthritis.18,19 In our series, several other amyloid-containing tissue samples were obtained for reasons related to symptomatic amyloidosis, for example, carpal tunnel syndrome, cardiomyopathy and cardiac failure, lattice corneal dystrophy, nephrotic syndrome, neuropathy, local amyloid-related tumorous lesions among others. All these are symptoms known to occur in patients suering from amyloidosis. Although fat aspiration biopsies were obtained to specically search for amyloid in patients suering from rheumatoid arthritis, in the majority of our biopsy cases, no specic inquiry for amyloid analysis was placed, which leads to the conjecture that amyloid, despite being symptomatic, is still rarely suspected clinically, even in patients suering from a disease known to cause amyloidosis, that is, rheumatoid arthritis or plasmacytoma. For the immunohistochemical classication of the amyloid deposits, we applied a broad set of commercially (antibodies directed against AA amyloid, AP, b2M, calcitonin, brinogen, l-light chain and k-light chain, lactoferrin, lysozyme) and a few noncommercially (directed against apoAI and l-light chain-derived amyloid proteins) available antibodies. Only 1 antibody did not
lead to the denite or probable classication of the respective amyloid type, that is, the anti-b2M antibody. This antibody always shows intensive staining of corpora amylacea of the prostate, which is used as a positive control in our department. Corpora amylacea have previously been shown to be of b2M origin and also intensely immunoreacted with a specic antibody raised against b2M-derived amyloid brils.5,34 Thus, it is highly unlikely that the missing classication of any biopsy case as Ab2M amyloid is related to missing immunoreactivity of the antibody, but rather that Ab2M amyloidosis has disappeared. Ten years ago we had 7 (5%) biopsy specimens with Ab2M amyloid.36 However, improvements made in the treatment of patients on dialysis have led to the disappearance of Ab2M amyloid.40 Although AA, AApoAI, ALac, AKer, ALys and ATTR amyloids always showed a strong and even immunostaining with the respective antibody, this was not a common nding for AL amyloid. Immunohistochemical classication of AL amyloid and dierentiation from rare hereditary amyloidoses is still a major problem in surgical pathology using both commercially available and noncommercially available antibodies. Cases diagnosed as denite or probable AL amyloid showed (1) unequivocal positive homogeneous or spotty immunostaining of amyloid deposits with antibodies directed against either l-light chain or k-light chain (Fig. 1), (2) spotty or uneven staining with antibodies directed against either l-light chain or k-light chain and 1 or 2 other antibodies (Table 4), (3) no staining with any antibody, except anti-AP antibody, or (4) no immunostaining with antibodies directed against l-light chain or k-light chain, but spotty or uneven staining with other antibodies. This variety is related to the intrinsic nature of AL amyloid. The amyloid protein(s) are derived from the variable region of l-light chains or k-light chains and each patient with AL amyloid has a unique amyloid protein, reducing the chance that a single antibody will ever be able to stain all dierent types of AL amyloid. In addition, even nonimmunoglobulin-derived amyloid deposits may show staining with antibodies directed against l-light chain or k-light chain. This can be related to contamination of amyloid by serum proteins. Indeed many dierent types of proteins have been found immunohistochemically in amyloid deposits. However, because contamination of amyloid with serum proteins is nonselective, we considered staining of the same amyloid deposit with both antil-light chain and antik-light chain antibodies to be indicative of contamination by immunoglobulins. A similar approach is used in surgical pathology to separate reactive from neoplastic plasmacell inltrates. Thus, light chain restriction, that is, detection of only l-light chain or k-light chain immunoreactivity was considered as evidence of amyloid protein. Matters become more complicated with the regular staining of amyloid deposits with more than 1 antibody (Table 4). We observed staining with more than one antibody in 51 (30%) of 169 biopsies, anti-apoAI and anti-TTR being the most prevalent. This might be related
r
680
2006 Lippincott Williams & Wilkins
Am J Surg Pathol
Volume 30, Number 6, June 2006
Classification of Amyloid in Surgical Pathology
to contamination of amyloid deposits by serum proteins, or to the presence of a second or third amyloid protein in the same amyloid deposit. Recently, Sakata et al demonstrated that apoAI frequently colocalizes with amyloid deposits in various forms of human systemic amyloidosis of dierent origin.39 In addition, both TTR and apoAI are precursors of amyloid proteins and one might suggest that, once an amyloid deposit has formed, for example, of immunoglobulin origin, this forms a nidus where other amyloidogenic precursor proteins start to aggregate. In 10 patients, immunostaining was suggestive for codeposition of 2 or more amyloid proteins (Table 4). The coexistence of 2 or more amyloid bril proteins in the same patient and even in the same amyloid deposit has been described previously and further complicate the immunohistochemical classication of amyloid.6,14,15,22,35,42,44 Thus, in case of staining of amyloid with more than 1 antibody, the surgical pathologist has to decide which staining is related to the detection of the amyloid protein(s) and which is related to contaminating proteins. In this respect, further clinical information and histologic nding may aid in reaching a denite or probable diagnosis. In our series, detection of a light chain restriction in surrounding plasmacells or presence of a frank plasmacytoma in a bone marrow biopsy was a valuable adjunct in reaching the correct or at least most likely diagnosis. We also commonly observed that dierent from other types of amyloid, AL amyloid more frequently showed a weak congophilia (Fig. 1) and usually a spotty and less intense immunostaining with the anti-AP antibody. We also observed that it is often helpful to investigate another amyloid containing tissue site, where insudation of the tissue by serum proteins was less prominent. Thus, denitive and unequivocal classication of immunoglobulin light chain-derived amyloid (AL amyloid) is a dicult task. The diagnosis probably AL amyloid n.o.s. was made in 46% of all biopsy cases with the diagnosis of AL amyloid (Table 3). Diagnostic accuracy increased by using a panel of dierent antibodies directed against l-light chains. Amyloid deposits formed by more than 1 amyloid protein do occur, but are very dicult to specify as such by immunohistochemistry alone. Microextraction of amyloid proteins from formalin-xed and paran-embedded biopsy specimens and subsequent biochemical characterization of the amyloid protein may help to reach the correct diagnosis.16,21,28,45 Our current review of the immunohistochemical classication of amyloid shows that AL amyloidosis is most prevalent, accounting for almost 45% of all cases with amyloid, followed by AA (19%) and ATTR amyloids (12%; Table 1). Comparing these gures with our previous study, it is interesting to note that AA amyloid is now less prevalent in a series of surgical pathology specimens than 10 years ago, decreasing from 35% to 19%.36 This is most likely related to improvements in the treatment of rheumatoid arthritis, which was then and is now the most common cause of AA amyloidosis.36 Interestingly, the relative prevalence of ATTR amyloid in surgical pathology specimens has
r
increased. Formerly, only 7 (5%) biopsies enclosed ATTR amyloid, whereas now 21 (13%) biopsies had ATTR amyloid. The prevalence of AL amyloid increased slightly from 36% to 45%. These changes could be related to the diminution of Ab2M amyloid and the decreased prevalence of AA amyloid, raising the relative frequency of other amyloid types. Our current review may also assist practicing surgical pathologists. In times of cost-cutting it is often impossible to always apply or even keep on stock a panel of more than 10 dierent antibodies for the immunohistochemical classication of amyloid. The immunohistochemcial classication should always cover at least AL, ATTR, and AA amyloids. AFib, AApoAI, and ALys amyloids, and other rare hereditary amyloid diseases should be considered depending on whether amyloid is found locally or represents a systemic disease. Searching for Ab2M amyloid may only be justied in rare circumstances, for example, longstanding dialysis and after all other common types of systemic amyloid have been excluded. The age distribution showed that 57% of our patients were in their seventh and eighth decade of life at the time of diagnosis. Although AL amyloid peaked in the seventh and eighth decade, AA and ATTR amyloids showed each 2 age peaks, probably reecting the dierent etiologies. Patients suering from juvenile rheumatoid arthritis develop AA amyloidosis earlier in their life than patients with disease onset during adulthood. In the seventh and even in the nineth decade, ATTR amyloid could be hereditary in origin or the manifestation of the senile-cardiovascular type. In the senile-cardiovascular type of ATTR amyloidosis the apparent protein precursor is not altered by a mutation, that is the nonvariant TTR. However, patient age per se does not exclude heredity. Similar observations have been made by comparing patients suering from hereditary ATTR amyloidosis in Portugal and France.29 In France, the vast majority of patients with hereditary ATTR amyloidosis were diagnosed above the age of 60 years.29 In one of our patients, follow-up information was available and sequencing of the TTR-gene detected a Met30-mutation. In summary, our study shows that the prevalence of dierent amyloid types has changed during the last decade. Ab2M amyloid has vanished and the relative prevalence of AA amyloid has decreased, probably due to improved treatment of the underlying diseases. AL amyloid, ATTR amyloid and previously unknown amyloid types, for example, AApoAI, ALac, and AKer amyloids become more prevalent in surgical pathology series. Although lack of immunostaining with antibodies directed against AA, AApoAI, AKer, ALac, ALys, and ATTR amyloids always excluded these amyloid types, missing immunostaining with antibodies directed against immunoglobulin-derived l-light chain and k-light chain or AL amyloid proteins does not exclude AL amyloidosis. With an increasing number of dierent systemic amyloid diseases identied, an increasing number of dierential diagnoses have to be considered. Despite signicant
2006 Lippincott Williams & Wilkins
681
Kebbel and Rocken
Am J Surg Pathol
Volume 30, Number 6, June 2006
technical and methodologic improvements, immunohistochemical classication of amyloid proteins still poses problems.36,37 It can produce ambiguous or misleading results and correct classication of immunoglobulin light chain-derived amyloid (AL amyloid) and hereditary amyloidoses is a serious obstacle, and sometimes even impossible when conclusive clinical information or additional protein biochemical or molecular biologic studies are not available.20,38 ACKNOWLEDGMENTS The authors thank all the surgical pathologists from Germany and across Europe, who referred many interesting biopsy cases to our department for immunohistochemical classication of the amyloid deposits. REFERENCES
1. Arbustini E, Morbini P, Verga L, et al. Light and electron microscopy immunohistochemical characterization of amyloid deposits. Amyloid. 1997;4:157170. 2. Baretton G, Linke RP, Lohrs U. Systemic amyloidoses. Immuno histochemical typing at the time of autopsy using a series of specic antibodies. Pathologe. 1990;11:7179. 3. Bohne S, Sletten K, Menard R, et al. Cleavage of AL amyloid proteins and AL amyloid deposits by cathepsins B, K, and L. J Pathol. 2004;203:528537. 4. Chastonay P, Hurlimann J. Characterization of dierent amyloids with immunological techniques. Path Res Pract. 1986;181: 657663. 5. Cross PA, Bartley CJ, McClure J. Amyloid in prostatic corpora amylacea. J Clin Pathol. 1992;45:894897. 6. Fernandez-Alonso J, Rios-Camacho C, Valenzuela-Castano A, et al. Mixed systemic amyloidosis in a patient receiving long term haemodialysis. J Clin Pathol. 1994;47:560561. 7. Fischer JL, Cyran J, Linke RP. Typing of amyloidoses intra vitam by tissue biopsy using antibodies. Report on 2 patients. Internist. 1986;27:113117. 8. Fujihara S, Balow JE, Costa JC, et al. Identication and classication of amyloid in formalin-xed, paran-embedded tissue sections by the unlabeled immunoperoxidase method. Lab Invest. 1980;43:358365. 9. Gafni J, Sohar E. Rectal biopsy for the diagnosis of amyloidosis. Amer J Med Sci. 1960;240:102/332106/336. 10. Gallo G, Kaakour M, Kumar A, et al. Immunohistologic classication of systemic amyloidosis by fat aspiration biopsy. Amyloid. 1994;1:9499. 11. Gregorini G, Izzi C, Obici L, et al. Renal Apolipoprotein A-I Amyloidosis: a rare cause of hereditary tubulo-interstitial nephritis. J Am Soc Nephrol. 2005. In press 12. Hoshii Y, Iwata T, Kawano H, et al. Immunohistochemical classication of 109 autopsy cases of systemic amyloidosis in Japan. Patologia. 1992;25:212213. 13. Ii K, Kyle RA, Dyck PJ. Immunohistochemical characterization of amyloid proteins in sural nerves and clinical associations in amyloid neuropathy. Am J Pathol. 1992;141:217226. 14. Isobe T, Matsushita T, Minakata T, et al. Coexistence of AL and Ab2M amyloid in tissues of a patient with myeloma on hemodialysis. Amyloid. 1996;3:4143. 15. Jones CH, Kanagasundaram NS, Coral AP, et al. Combined Waldenstroms macroglobulinaemia associated AL and beta-2microglobulin amyloidosis. Nephrol Dial Transplant. 1997;12: 27082712. 16. Kaplan B, Hrncic R, Murphy CL, et al. Microextraction and purication techniques applicable to chemical characterization of amyloid proteins in minute amounts of tissue. Methods Enzymol. 1999;309:6781.
17. Kazatchkine MD, Husby G, Araki S, et al. Nomenclature of amyloid and amyloidosisWHO-IUIS nomenclature sub-committee. Bull Who. 1993;71:105108. 18. Kobayashi H, Tada S, Fuchigami T, et al. Secondary amyloidosis in patients with rheumatoid arthritis: diagnostic and prognostic value of gastroduodenal biopsy. Brit J Rheumatol. 1996;35:4449. 19. Kuroda T, Tanabe N, Sakatsume M, et al. Comparison of gastroduodenal, renal and abdominal fat biopsies for diagnosing amyloidosis in rheumatoid arthritis. Clin Rheumatol. 2002; 21:123128. 20. Lachmann HJ, Booth DR, Booth SE, et al. Misdiagnosis of hereditary amyloidosis as AL (primary) amyloidosis. N Engl J Med. 2002;346:17861791. 21. Layeld R, Bailey K, Lowe J, et al. Extraction and protein sequencing of immunoglobulin light chain from formalin-xed cerebrovascular amyloid deposits. J Pathol. 1996;180:455459. 22. Liepnieks JJ, Benson MD. Codeposition of transthyretin and immunoglobulin lambda light chain in senile cardiac (ATTR) amyloidosis. In: Grateau G, Kyle R, Skinner M, eds. Amyloid and Amyloidosis. London, NewYork: CRC Press; 2005: 332333. 23. Linke RP. Highly sensitive diagnosis of amyloid and various amyloid syndromes using Congo red uorescence. Virchows Arch. 2000;436:439448. 24. Linke RP, Joswig R, Murphy CL, et al. Senile seminal vesicle amyloid is derived from semenogelin I. J Lab Clin Med. 2005; 145:187193. 25. Linke RP, Nathrath WBJ, Eulitz M. Classication of amyloid syndromes from tissue sections using antibodies against various amyloid bril proteins: report of 142 cases. In: Glenner GG, Osserman EF, Benditt EP, et al, eds. Amyloidosis. New York, London: Plenum Publishing Corporation; 1986:599605. 26. Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349:583596. 27. Mucchiano GI, Haggqvist B, Sletten K, et al. Apolipoprotein A-1derived amyloid in atherosclerotic plaques of the human aorta. J Pathol. 2001;193:270275. 28. Murphy CL, Eulitz M, Hrncic R, et al. Chemical typing of amyloid protein contained in formalin-xed paran-embedded biopsy specimens. Am J Clin Pathol. 2001;116:135142. 29. Plante-Bordeneuve V, Carayol J, Ferreira A, et al. Genetic study of transthyretin amyloid neuropathies: carrier risks among French and Portuguese families. J Med Genet. 2003;40:e120. 30. Puchtler H, Sweat F, Levine M. On the binding of Congo red by amyloid. J Histochem Cytochem. 1962;10:355364. 31. Rocken C, Becker K, Fandrich M, et al. ALys amyloidosis caused by compound heterozygosity in exon 2 (Thr70Asn) and exon 4 (Trp112Arg) of the lysozyme gene. Human Mutat. 2006;27: 119120. 32. Rocken C, Hegenbarth V, Schmitz M, et al. Plasmacytoma of the tonsil with AL amyloidosis: evidence of post-brillogenic proteolysis of the bril protein. Virchows Arch. 2000;436:336344. 33. Rocken C, Kronsbein H, Sletten K, et al. Amyloidosis of the breast. Virchows Arch. 2002;440:527535. 34. Rocken C, Linke RP, Saeger W. Corpora amylacea in the lung, prostate and uterus: a comparitive immunohistochemical study. Path Res Pract. 1996;192:9981006. 35. Rocken C, Saeger W, Linke RP. Several dierent types of amyloid in a 93-year-old female patient: case report of an autopsy case. Pathologe. 1993;14:4246. 36. Rocken C, Schwotzer E, Linke RP, et al. The classication of amyloid deposits in clinicopathological practice. Histopathology. 1996;29:325335. 37. Rocken C, Sletten K. Amyloid in surgical pathology. Virchows Arch. 2003;443:316. 38. Rocken C, Wilhelm S. Inuence of tissue xation on the extraction and identication of amyloid proteins. J Lab Clin Med. 2005; 146:244250 39. Sakata N, Hoshii Y, Nakamura T, et al. Colocalization of apolipoprotein AI in various kinds of systemic amyloidosis. J Histochem Cytochem. 2005;53:237242.
r
682
2006 Lippincott Williams & Wilkins
Am J Surg Pathol
Volume 30, Number 6, June 2006
Classification of Amyloid in Surgical Pathology
40. Schwalbe S, Holzhauer M, Schaeer J, et al. beta(2)-microglobulin associated amyloidosis: a vanishing complication of long-term hemodialysis?. Kidney Int. 1997;52:10771083. 41. Stix B, Leber M, Bingemer P, et al. Hereditary lattice corneal dystrophy is associated with corneal amyloid deposits enclosing Cterminal fragments of kerato-epithelin. Invest Ophthalmol Vis Sci. 2005;46:11331139. 42. Storkel S, Sturer A. Combined amyloidosis of the AA and AB type following chronic hemodialysis. Pathologe. 1989;10: 107113. 43. Strege RJ, Saeger W, Linke RP. Diagnosis and immunohistochemical classication of systemic amyloidoses. Report of 43 cases in an unselected autopsy series. Virchows Arch. 1998;433:1927.
44. Takahashi M, Hoshii Y, Kawano H, et al. Ultrastructural evidence for colocalization of K light chain- and beta(2)-microglobulinderived amyloids using double labelling immunogold electron microscopy. Virchows Arch. 1996;429:383388. 45. Tennent GA. Isolation and characterization of amyloid brils from tissue. Methods Enzymol. 1999;309:2647. 46. Kaa CA, Hol PR, Huber J, et al. Diagnosis of the type of amyloid in paran wax embedded tissue sections using antisera against human and animal amyloid proteins. Virchows Archiv [A]. 1986; 408:649664. 47. Westermark P, Araki S, Benson MD, et al. Nomenclature of amyloid bril proteins, Report from the meeting of the International Nomenclature Committee on Amyloidosis. August 89, 1998. Part 1. Amyloid. 1999;6:6366.
2006 Lippincott Williams & Wilkins
683
Anda mungkin juga menyukai
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- CH 11Dokumen18 halamanCH 11dazaikun22032003Belum ada peringkat
- HFMDDokumen9 halamanHFMDAnindita PramadyasiwiBelum ada peringkat
- Oral Patho Q AnswerDokumen10 halamanOral Patho Q AnswerAnȜ'am Abu Ȝ'leonBelum ada peringkat
- Urine Culture Test: Tests and ProceduresDokumen2 halamanUrine Culture Test: Tests and ProceduresVikashKumarBelum ada peringkat
- Statement From Maine Veterinary Medical CenterDokumen3 halamanStatement From Maine Veterinary Medical CenterWGMEBelum ada peringkat
- Endurence TrainingDokumen33 halamanEndurence TrainingSaxena AbhilashBelum ada peringkat
- Anatomy and Physiology of the Respiratory SystemDokumen2 halamanAnatomy and Physiology of the Respiratory SystemRam Pgdt50% (4)
- The Hall of Fire 05Dokumen29 halamanThe Hall of Fire 05maldreidor100% (1)
- Principles of Spine Trauma and Spinal Deformities PDFDokumen34 halamanPrinciples of Spine Trauma and Spinal Deformities PDFVirlan Vasile CatalinBelum ada peringkat
- Sharks of The World Volume 4 Part 2Dokumen414 halamanSharks of The World Volume 4 Part 2cavrisBelum ada peringkat
- African Lion (Panthera Leo) With Dark Mane. Photo Credit: Dr. Michelle StevensDokumen45 halamanAfrican Lion (Panthera Leo) With Dark Mane. Photo Credit: Dr. Michelle StevensWaqar IbrahimBelum ada peringkat
- Urine Analysis PracticalDokumen53 halamanUrine Analysis PracticalMubasharAbrar100% (2)
- Reproductive SystemDokumen7 halamanReproductive SystemRiaz siddiquiBelum ada peringkat
- TABLE (Ascaris, Trichuris, and Enterobius)Dokumen3 halamanTABLE (Ascaris, Trichuris, and Enterobius)TRISHA MAE ORDONABelum ada peringkat
- Annotated Reading Dengue FeverDokumen1 halamanAnnotated Reading Dengue FeverGoRbz SarmientoBelum ada peringkat
- OSCE Mock ExamDokumen52 halamanOSCE Mock Examanas100% (2)
- Lessons Learned From The Dog GenomeDokumen11 halamanLessons Learned From The Dog GenomebellonicoBelum ada peringkat
- Cancer Tongue Cured With HomoeopathyDokumen6 halamanCancer Tongue Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD HomBelum ada peringkat
- Exercise 7.2 - ElectrocardiogramDokumen2 halamanExercise 7.2 - ElectrocardiogramKevin F. CortesBelum ada peringkat
- Toshihiko Yayama - Qi Healing - The Way To A New Mind and BodyDokumen159 halamanToshihiko Yayama - Qi Healing - The Way To A New Mind and BodyFernando Iglesias100% (2)
- Normal Puerperium PDFDokumen22 halamanNormal Puerperium PDFwawa3385100% (1)
- Thoracic WallDokumen12 halamanThoracic WallZainab NaffeeBelum ada peringkat
- Balancing The Risk of Your Puppy Contracting Parvovirus Against TheDokumen4 halamanBalancing The Risk of Your Puppy Contracting Parvovirus Against Theapi-255712054Belum ada peringkat
- Ambahan: Ambahans Inscribed On Plants in A Bamboo Grove (Source: Antoon Postma)Dokumen10 halamanAmbahan: Ambahans Inscribed On Plants in A Bamboo Grove (Source: Antoon Postma)Mernie Grace DionesioBelum ada peringkat
- Upper Midline CorrectionDokumen5 halamanUpper Midline CorrectionmutansBelum ada peringkat
- Body Fluid Electrolytes Acid Base BalanceDokumen2 halamanBody Fluid Electrolytes Acid Base BalanceMarzanul Islam AnikBelum ada peringkat
- FE ImbalanceDokumen6 halamanFE ImbalanceDonna CortezBelum ada peringkat
- Factors That Damage the Stomach LiningDokumen8 halamanFactors That Damage the Stomach LiningTania Louise Pioquinto AbuanBelum ada peringkat
- CannulaDokumen4 halamanCannulaAnonymous m0vrFqAsBelum ada peringkat
- Rat Catchers PDFDokumen8 halamanRat Catchers PDFDavid FrostBelum ada peringkat