Actual Management
Diunggah oleh
ApOlle Defiesta - DOminguezDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Actual Management
Diunggah oleh
ApOlle Defiesta - DOminguezHak Cipta:
Format Tersedia
ACTUAL MANAGEMENT Do Tracheostomy Care Nursing consideration/ intervention: Do daily skin care around the tube.
be. Use a clean gauze/wash cloth and mild soap and water to cleanse the skin around the tracheostomy tube. Keep the skin clean and dry to avoid skin maceration and potential skin breakdown. Keep a dry, lint-free dressing around the tube. Using a skin barrier after cleansing can help to prevent skin irritation. Remove and clean the inner cannula of the tracheostomy tube once per day or more often, depending upon mucus build up. Wash inner cannulas in hot soapy water, and then disinfect them by boiling in water or soaking in alcohol or in hydrogen peroxide. Suction secretion PRN Nursing consideration/intervention: Auscultate the clients lungs for gurgles with a stethoscope or by listening for signs of excess mucus. Avoid oversuctioning; it can irritate the mocusa. Advice significant others never apply suction when the suction catheter is inserted and must never apply suction for more than 10 seconds to avoid deoxygenating the patient. Teach patient and families that the most important aspect of infection control is frequent hand washing. Keep distance when performing suctioning so that when the patient cough out you will not spill out on you. Suction the airway as needed. Instill 3 to 5 ml of sterile normal saline into the trachea in order to loosen/mobilize thick secretions. Insert Nasogastric Tube for feeding Nursing consideration/ intervention: Assess tube location before administering feeding, ensure that the tube is positioned properly. Perform consistently flushing the tube with water before and after each feeding which enhances the longevity of the tube. Flush all types of feeding with 50 cc syringe; smaller syringes can create pressure high enough to rupture a tube. Teach the client and the family to secure nasogastric tube firmly to the nose and to either side of face or to another position of comfort. Encourage hand washing to eradicate the possible causes of infection. For nasal care: Gently clean and lubricate the clients external nares to prevent build up of crusted secretions and skin breakdown. Use a clean cotton-tipped swab and a water soluble lubricant to clean the clients nostril. Keep patients nose skin clean and dry. Secure the tube with hypoallergenic tape, taking care to avoid pressure on nares. Nebulization Nursing consideration/intervention: Monitor the heart rate before and after the treatment for patients using bronchodilator drugs; bronchodilators may cause tachycardia, palpitations, dizziness nausea or nervousness. Explain the procedure to the patient. This therapy depends on patient effort; proper explanation of the procedure helps to ensure the patients cooperation and effectiveness of the treatment.
Instruct patient to inhale slowly and deeply and hold breathes for 10 seconds; this allows the aerosol to reach deeper airways. Encourage patient to exhale slowly through pursed lips; controlled exhalation helps the small airways open during exhalation. Instruct the patient to wait for 20-30 seconds between inhalations; the first inhalation has the chance to work and subsequent dose reaches deeper into the lungs. Observe expansion of the chest to ascertain that patient is taking deep breaths ; this will ensure that the medication is deposited bewlow the lovel of oropharynx Advice patient to report any adverse reactions such as restlessness, palpitations, nervousness or rash. Perform chest physiotherapy after nebulization to help mobilize secretions. Observe Respiratory Isolation Nursing consideration/intervention; Perform hand washing before and after touching the patient or contaminated articles, and contaminated articles should be discarded. Patient should be encouraged to cough or spit into a paper and then discard. Encourage the use of mask in the patients room Advice family and care provider that if possible stay 6 feet away from the patient and do not share items. Encourage washing hands or use of alcohol hand gel after touching the patient, after taking of your mask and when leaving patients room. Perform Oral Care Nursing intervention/consideration: Clients should know to obtain a toothbrush every 3 months. Lemon-glycerin sponges should not be used. They should not share toothbrushes with family members or drink directly from a bottle of mouth wash. While cleaning the oral cavity, the nurse should never use fingers to hold the clients mouth open. Use gloves and mask are necessary. Perform TSB Nursing consideration/intervention: Assess Vital signs especially Temp. Advice to expose one part of the body at a time, gently sponge with tepid water (lukewarm) for approximately 5 minutes. Begin with face and extremities, then back ; slow ard gently motion are indicated because firm rubbing motion increases heat production cool sponge given rapidly or for a short period of time tend to increase the bodys heat production. Monitor temperature every 10 minutes while sponging resident ; to evaluate effectiveness of the bath. Instruct family to place cool compress on the forehead, axillas, and groin; the axillas ad groin areas contain large blood vessels that are close to the skins surface, which aid the transfer of heat. Application of Calmorptine over the blisters Nursing consideration/intervention: Instruct to cleanse the skin prior to application with mild skin cleanser of water. Pat dry or allow air dry. Apply a thin layer 2-4 times daily to affected area or as necessary to promote comfort or protection. Educate the significant others about the possibility for an allergic reaction due to sensitivity of the ingredient. ( severe itching, increase area of rash)
Instruct the significant others that upon application there will be a slight burning sensation but this is normal and it frequently goes away within 2-3 minutes. Instruct the patient to report if hr/she cannot tolerate the discomfort; the calmorptine will be removed. Moderately high back rest Nursing consideration/intervention; Assess the skin first before doing the positioning. Perform frequent position changes; helps to prevent muscle discomfort, undue pressure resulting to ulcers etc. position changes also maintain muscle tone and stimulate muscular reflexes. Ensure proper alignment and promote client comfort and safety. Place pillow at lower back to support lumbar region thus correcting posterior flexion of lumbar curvature. Instruct the family to place pillow to support head, neck, and upper back to prevent hyperextention of neck. Instruct significant others to place pillow under forearm to eliminate pull on shoulder and assist venous blood flow from hands and lower arms to prevent shoulder muscle strain, possible dislocation of shoulders, edema of hands and arms with flaccid paralysis, flexion contracture of the wrist. Instruct significant others to place small pillow under thighs to flex knees to prevent hyperextention of knees. Instruct significant others to place pillow under lower legs to prevent pressure on heels. Place footboard to provide support for dorsal flexion to prevent plantar flexion of foot (foot drop). Input and output every 4 for temperature of 38C Nursing consideration/intervention: Emphasize the importance of accurate measurement of intake and output to patient and significant others. Instruct the need to use urinary drainage and securing it intact or patent. Instruct the client or significant others the following important input reminders: For tube feedings remember to include the 30-60 ml water flush at the end of intermittent feedings or during continous feedings. For parenteral fluids the exact amount of the intravenous fluid administered is to be recorded. Catheter or tube irrigants fluid used to irrigate urinary catheters, nasogastric tubes must be measured and recorded if not immediately withdrawn. Instruct the client or significant others the following important output reminders: For urinary output empty the drainage bag into a measuring container. Tube drainage. Insert intra-foley catheter then connect to urine bag Nursing consideration/intervention: Perform hand washing or use gloves before and after handling catheters. Instruct the patient and significant others not to pull on the catheter Ensure that there are no kinks or twist in the tubing. Keep the urine drainage bag is below the level of the bladder. Empty the drainage bag regularly. Monitor for signs and symptoms of urinary tract infection including burning, urgency, abdominal pain, cloudy urine and confusion. Ensure adequate intake of fluids. Check that there is no tension on the catheter or tubing, that the catheter is securely taped.
Ensure that the drainage system is well sealed or closed. Check that there are no leaks at the connection sites open system. Observe the flow of urine every 2 -3 hours, and note color, odor, and any abnormal constituents.
IDEAL MANAGEMENT Diagnostic Evaluation Complete blood count (CBC) with differential - detect an elevated leukocyte count in bacterial and viral meningitis. - Rising WBC indicates bodys efforts to combat pathogens; normal values: 4000 to 11,000 mm3. Very low WBC (neutropenia <1000 mm3) indicates severe risk for infection because patient does not have sufficient WBCs to fight infection. NOTE: In elderly patients, infection may be present without an increased WBC. Lumbar puncture - (elevated CSF pressure, cloudy or milky white CSF, high protein level, positive Gram stain and culture that usually identifies the infecting organism unless it's a virus, and depressed CSF glucose concentration) CSF evaluation for pressure, leukocytes, protein, glucose Nursing intervention/consideration; Explain the procedure to the patient Instruct the patient to empty the bladder and bowels prior to the procedure to prevent unnecessary discomfort During the procedure: o Instruct the patient to lie still with you supporting the back of the neck and knees. o Reassure the patient throughout the procedure by explaining what is happening. o Encourage normal breathing and relaxation. o Observe the clients respiration and pulse during the procedure. o Ask the client to report headache or persistent pain at the insertion site. o Place a small dressing at the puncture site. After the procedure: o Ensure clients comfort and safety. o Assist the client in a dorsal recumbent position with only one head pillow. The patient remains in this position for 1-2 hours depending on the doctors order. o Offer oral fluids frequently, unless contraindicated, to help restore the volume of CSF. o Observe for swelling and bleeding at the puncture site. o Monitor changes in the neurologic status of the patient. o Determine whether the patient is experiencing numbness, tingling or pain radiating down the legs. MRI/CT scan - With and without contrast rules out cerebral hematoma, hemorrhage, or tumor Nursing consideration/intervention: o Instruct the patient and family the purpose of the MRI o Educate the client about the sounds and sensations she/he will hear and feel during the examination. o Instruct client to lie very still which can take from 60-69 minutes. o Instruct client to remove all metallic accessories.
o If the use of contrast agent is planned, ask whether the patient tends to become nauseated easily, and adjust the intake of food and fluids accordingly. o Use of earplugs should be initiated. o Assure client that it is possible to communicate with the technician during the scan for the claustrophobic patients. o Instruct the client that after examination he may resume previous activities and diet. o Tell the patient to expect to experience diuresis if a contrast agents is used for the MRI.
CT scan with contrast - to detect abscesses. Low CD4+ counts indicate immunosuppression in HIV-positive patients and other patients with immunosuppressive disorders. - Latex agglutination may be positive for antigens in meningitis. Nursing consideration/intervention: o Check whether the client already signed the inform consent. o Explain that fasting is not usually required for a CT scan of the head but ask whether or not the client becomes nauseated easily; if so, adjust food and fluid intake accordingly. o Instruct client that is commonly given, ask if the client has an allergy to iodine or contrast dyes. o Instruct the client that the hair should be smoothly combed. o Position the client supine and the body body part to be scanned is placed on a doughnut shaped ring of the scanner. o Instruct the patient to expect to hear mechanical noises coming from the scanner. o If sedation is needed instruct the patient to avoid: (1) alcohol and caffeine on the day of the scan, (2) avoid eating for 2 hours before the scan, (3) avoid driving for atleast 12 hours. Chest X-rays - may reveal pneumonitis or lung abscess, tubercular lesions, or granulomas secondary to fungal infection Nursing consideration/intervention: o Ask the client to remove any radiopaque objects and to wear a gown. o Instruct the client that he may be asked to move into various position. o Monitor unstable patient during the procedure. Treatment - team effort with nursing, infectious diseases specialists, neurology, internal medicine, and otolaryngology specialists, and laboratory and diagnostic staff - Antibiotic therapy and vigorous supportive care - Usually, I.V. antibiotics are given for at least 2 weeks, followed by oral antibiotics, o ampicillin, cefotaxime, ceftriaxone, and nafcillin Dexamethasone (Decadron) - as adjunctive therapy o Mannitol - to decrease cerebral edema o Anticonvulsant (usually given I.V.) or a sedative - to reduce restlessness o Aspirin or acetaminophen - to relieve headache and fever Supportive measures consist of bed rest, hypothermia, and fluid therapy to prevent dehydration o Isolation - if nasal cultures are positive o Therapy for any coexisting conditions, such as endocarditis or pneumonia o Temozolomide (Temodar) - neoplastic meningitis
o Cochlear implantation rehabilitation - deafness caused by meningitis therapy for S. aureus and gram-negative bacilli . o If meningitis is suspected after neurosurgical procedures, potential I.V. line bacteremia, CSF leak, or immunosuppression o Antifungal agents - for cryptococcal meningitis o Empiric antituberculosis drugs must be initiated if infection by Mycobacterium tuberculosis is suspected Ideal Nursing Management o Nursing Assessment o Obtain a history of recent infections such as upper respiratory infection, and exposure to causative agents o Assess neurologic status and vital signs o Evaluate for signs of meningeal irritation o Assess sensorineural hearing loss (vision and hearing), cranial nerve damage (eg, facial nerve palsy), and diminished cognitive function. Reducing Fever o Perform TSB starting from the face down. o Administer antimicrobial agents on time to maintain optimal blood levels. o Monitor temperature frequently or continuously, and administer antipyretics as ordered. o Institute other cooling measures, such as a hypothermia blanket, as indicated. o Maintaining Fluid Balance o Prevent I.V. fluid overload, which may worsen cerebral edema. o Monitor intake and output closely. o Monitor CVP frequently. For Enhancing Cerebral Perfusion o Assess LOC, vital signs, and neurologic parameters frequently. o Observe for signs and symptoms of ICP (eg, decreased LOC, dilated pupils, widening pulse pressure). o Maintain a quiet, calm environment to prevent agitation, which may cause an increased ICP. o Prepare patient for a lumbar puncture for CSF evaluation, and repeat spinal tap, if indicated. Lumbar puncture typically precedes neuroimaging o Notify the health care provider of signs of deterioration: increasing temperature, decreasing LOC, seizure activity, or altered respirations. o Reducing Pain - Administer analgesics as ordered; monitor for response and adverse reactions. Avoid opioids, which may mask a decreasing LOC. o Darken the room if photophobia is present. o Assist with position of comfort for neck stiffness, and turn patient slowly and carefully with head and neck in alignment. o Elevate the head of the bed to decrease ICP and reduce pain. For Promoting Return to Optimal Level of Functioning o Implement rehabilitation interventions after admission (eg, turning, positioning). o Progress from passive to active exercises based on the patient's neurologic status. For Patient Education and Health Maintenance o Advice close contacts of the patient with meningitis that prophylactic treatment may be indicated; they should check with their health care providers or the local public health department. o To help prevent the development of meningitis, teach patients with chronic sinusitis or other chronic infections the importance of proper medical treatment.
o Encourage the patient to follow medication regimen as directed to fully eradicate the infectious agent. o Encourage follow-up and prompt attention to infections in future. o Inform patients who have children about the importance of vaccination with measles, mumps, rubella vaccine, H. influenzae type B vaccine, and pneumococcal vaccine as a preventive measure. Vaccination is recommended for children younger than school age.
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Peds Charts Book NotesDokumen37 halamanPeds Charts Book NotesVin Lorenzo CampbellBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Airway ManagementDokumen42 halamanAirway ManagementOwy100% (4)
- Childhood DisordersDokumen7 halamanChildhood DisordersApOlle Defiesta - DOminguezBelum ada peringkat
- Sample Only Nso - Tracheostomy CareDokumen5 halamanSample Only Nso - Tracheostomy CareNader Abdurasad100% (1)
- Difficult Airway Guidelines 2022 06-2021Dokumen88 halamanDifficult Airway Guidelines 2022 06-2021luisfernandoamaya89Belum ada peringkat
- Speech & Language Therapy in Practice, Autumn 1998Dokumen32 halamanSpeech & Language Therapy in Practice, Autumn 1998Speech & Language Therapy in PracticeBelum ada peringkat
- OPT Plus Form 1Dokumen1 halamanOPT Plus Form 1ApOlle Defiesta - DOminguezBelum ada peringkat
- OPT Plus Form 1Dokumen1 halamanOPT Plus Form 1ApOlle Defiesta - DOminguezBelum ada peringkat
- Procedural Checklist For Care of TracheostomyDokumen2 halamanProcedural Checklist For Care of TracheostomyAbegail TabuniagBelum ada peringkat
- Nursing Reviewer Part 3Dokumen10 halamanNursing Reviewer Part 3Johny VillanuevaBelum ada peringkat
- Surgical Finals Passing The Clinical PDFDokumen40 halamanSurgical Finals Passing The Clinical PDFnetradeep67% (3)
- John Jameson, Danny Bryden - Care of The Critically Ill Surgical Patient Student Handbook-The Royal College of Surgeons of England (2017)Dokumen355 halamanJohn Jameson, Danny Bryden - Care of The Critically Ill Surgical Patient Student Handbook-The Royal College of Surgeons of England (2017)osamaeBelum ada peringkat
- NP1Dokumen43 halamanNP1Edward Nicko GarciaBelum ada peringkat
- Thoracic SurgeryDokumen28 halamanThoracic Surgeryapi-3840195100% (5)
- Atlas Instruments Ent Head NeckDokumen317 halamanAtlas Instruments Ent Head NeckDr-Firas Nayf Al-Thawabia100% (1)
- Infection Control ManualDokumen51 halamanInfection Control ManualIka C Purnomo100% (2)
- CS Form No. 212 Revised Personal Data Sheet 2Dokumen13 halamanCS Form No. 212 Revised Personal Data Sheet 2ferosiacBelum ada peringkat
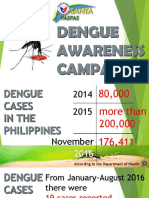
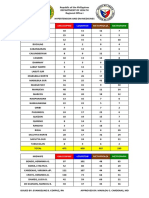
- DengueDokumen20 halamanDengueApOlle Defiesta - DOminguezBelum ada peringkat
- HPN DM MedsDokumen1 halamanHPN DM MedsApOlle Defiesta - DOminguezBelum ada peringkat
- ChemDokumen1 halamanChemApOlle Defiesta - DOminguezBelum ada peringkat
- Rev. Fr. Cirilo O. Ortega, SVDDokumen2 halamanRev. Fr. Cirilo O. Ortega, SVDApOlle Defiesta - DOminguezBelum ada peringkat
- Drug StudyDokumen6 halamanDrug StudySa Dei100% (1)
- Laboratory Studies: o o o o o o o oDokumen4 halamanLaboratory Studies: o o o o o o o oApOlle Defiesta - DOminguezBelum ada peringkat
- Tracheostomy 4Dokumen5 halamanTracheostomy 4rizwanBelum ada peringkat
- Care of Tracheostomy TubesDokumen10 halamanCare of Tracheostomy TubesMj BrionesBelum ada peringkat
- APPLIANCE 3e (Instruments) - 1Dokumen174 halamanAPPLIANCE 3e (Instruments) - 1Fahad2036100% (2)
- Tracheostomy Management: 1. Overview and AnatomyDokumen16 halamanTracheostomy Management: 1. Overview and AnatomymochkurniawanBelum ada peringkat
- Maksimoski CVDokumen7 halamanMaksimoski CVapi-513347575Belum ada peringkat
- N116-Skills Performance Checklist: Tracheostomy SuctioningDokumen3 halamanN116-Skills Performance Checklist: Tracheostomy SuctioningAlessandra Dominique MarianoBelum ada peringkat
- Week 3 - MS1 COURSE TASK - CU 3Dokumen2 halamanWeek 3 - MS1 COURSE TASK - CU 302 - DIMAYUGA, BRYANBelum ada peringkat
- TracheostomyDokumen32 halamanTracheostomydr MohammedBelum ada peringkat
- Chapter 22 - Management of Patients With Upper Respiratory Tract Disorders (INCOMPLETEon 13)Dokumen16 halamanChapter 22 - Management of Patients With Upper Respiratory Tract Disorders (INCOMPLETEon 13)Mary Singleton100% (1)
- What Is A Tracheostomy? Why Is A Tracheostomy Performed?Dokumen5 halamanWhat Is A Tracheostomy? Why Is A Tracheostomy Performed?Mara JnelleBelum ada peringkat
- Assessment of Adult Patients With TracheostomyDokumen15 halamanAssessment of Adult Patients With TracheostomyARTHUR CHRISTION CRUZBelum ada peringkat
- Inhalation Injury From Heat, Smoke, or Chemical IrritantsDokumen29 halamanInhalation Injury From Heat, Smoke, or Chemical IrritantsJulian SalazarBelum ada peringkat
- American Journal of Respiratory and Critical Care MedicineDokumen12 halamanAmerican Journal of Respiratory and Critical Care MedicineChanya ChomchoeyBelum ada peringkat
- Nur422-Airway Suctioning 1Dokumen28 halamanNur422-Airway Suctioning 1MJ DacerBelum ada peringkat
- Tracheal Intubation in Critical Ill Patient PDFDokumen8 halamanTracheal Intubation in Critical Ill Patient PDFArdi FkuiBelum ada peringkat
- Ca of The Respiratory System NCM 112 Cell Ab Final TopicsDokumen95 halamanCa of The Respiratory System NCM 112 Cell Ab Final TopicsA. Lizette PabloBelum ada peringkat
- ENT by Rajiv Dhawan 2023Dokumen165 halamanENT by Rajiv Dhawan 2023CastleKG100% (1)