Materials: Eric Hoben From The Children's Defense Fund
Diunggah oleh
New York State Senate Democratic ConferenceDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Materials: Eric Hoben From The Children's Defense Fund
Diunggah oleh
New York State Senate Democratic ConferenceHak Cipta:
Format Tersedia
Dependent coverage Prohibition on Lifetime Limits Medicaid Expansion Expansion of preventive services without cost-sharing School-Based Health Centers
ters Maintenance of Effort Pre-existing conditions
Adults are allowed to remain on their parents health insurance up to the age of 26 As of June 2011, has benefitted 150,428 young adults in New York
The law bans insurance companies from imposing lifetime dollar limits on health benefits As a result, 1,609,000 children are free from worrying about lifetime limits The law also restricts the use of annual limits and bans them completely in 2014
New York State implemented the Medicaid Expansion in November 2011 This increased income eligibility levels to 138% of the Federal Poverty Level for children ages 0-19 Eliminated stair-step eligibility for families An estimated 70,000 children will enroll onto Medicaid as a result of the expansion
The ACA requires many insurance plans to provide coverage for and eliminate cost-sharing on certain recommended preventive health services Cost-sharing has been shown to be prohibitive for children receiving the care to prevent chronic disease Over 824,000 children in New York State have benefitted from the expansion of preventive services
There are 216 SBHCs in New York, with a total enrollment of nearly 160,000 students Adolescents are more likely to access care at a SBHC, and are more likely to receive screenings for STIs, counseling on birth control and condom use than adolescents who receive care elsewhere Under the ACA, New York has received over $12million to help clinics expand and provide care for more students
Under the ACA, states are not allowed to cut back their Medicaid and CHIP programs beyond the levels they were on March 23, 2010 Must maintain eligibility levels for children in Medicaid and CHIP through 9/30/19 If a state violates MOE, it will lose all Medicaid federal matching funding for its entire Medicaid program until the violation is corrected States will receive two more years of CHP funding
Insurance companies can no longer deny coverage to children who have pre-existing health conditions or offer them a plan that does not cover care for their pre-existing condition In New York, 260,700 children have been protected under this provision
Children will be mandated to have health insurance Foster Care Children Child-specific services Creation of the Center for Medicare and Medicaid Innovation More affordability Childhood obesity demonstration project Child-only coverage option in the Exchange Oral Health
Children in foster care have high rates of acute and chronic illnesses, developmental delays and mental and behavioral health problems In 1999, New York expanded Medicaid eligibility to foster care children up to the age of 21 The ACA allows foster care children to be on Medicaid up to the age of 26
All health plans in the Exchange are required to have an Essential Health Benefits Package The packages must include coverage at no cost for comprehensive screenings and preventative care for children as defined by the Bright Futures standards issued by the American Academy of Pediatrics
These methods are expected to improve the quality of care, and reduce the rate of growth in health care costs for Medicare, Medicaid, and CHIP
In 2014, the law will provide refundable and advanceable premium credits Families with incomes between 133 and 400% of the Federal Poverty Level will be eligible Accessible by purchasing health insurance through the exchange
The ACA gives $25 million to the Centers for Disease Control for a four year project Will build on existing community efforts and will work to identify effective health care and community strategies to support childrens healthy eating and active living and help combat childhood obesity Will target children ages 2-12 enrolled in CHIP
The ACA allows families to purchase child-only insurance packages in the exchanges Who is in a household for income eligibility purposes will be based on tax households This will enable children that are being cared for by grandparents, children with parents whose employers do not offer dependent coverage, and children in mixed immigrant-status households are able to access coverage
The ACA creates an oral health prevention campaign, dental carries disease management, school-based dental sealant programs and cooperative agreements to improve infrastructure and surveillance systems
www.firstfocus.net www.healthcarereform.ny.gov www.cdc.gov www.hcfany.org http://aspe.hhs.gov/ www.communitycatalyst.org http://innovations.cms.gov/
Erin Hoben ehoben@cdfny.org 212.697.2323x205
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Break EvenAnalysisDokumen24 halamanBreak EvenAnalysisDlsu Amphi-CatBelum ada peringkat
- E WasteDokumen47 halamanE WasteGeorge Dlima67% (9)
- 03.12.19 Senate Majority Budget Resolution ReleaseDokumen6 halaman03.12.19 Senate Majority Budget Resolution ReleaseNew York State Senate Democratic ConferenceBelum ada peringkat
- ERAP Sign-On Letter FinalDokumen2 halamanERAP Sign-On Letter FinalNew York State Senate Democratic ConferenceBelum ada peringkat
- Senate Majority Passes Sweeping Anti-Gun Violence Legislation To Protect New YorkersDokumen7 halamanSenate Majority Passes Sweeping Anti-Gun Violence Legislation To Protect New YorkersNew York State Senate Democratic ConferenceBelum ada peringkat
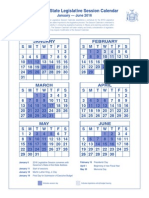
- 2016 Legislative Session CalendarDokumen1 halaman2016 Legislative Session CalendarMatthew HamiltonBelum ada peringkat
- Protecting Long Island: Senate Democrats Fight Against Offshore DrillingDokumen4 halamanProtecting Long Island: Senate Democrats Fight Against Offshore DrillingNew York State Senate Democratic ConferenceBelum ada peringkat
- Senate Majority Passes The Jos Peralta New York State DREAM ActDokumen4 halamanSenate Majority Passes The Jos Peralta New York State DREAM ActNew York State Senate Democratic ConferenceBelum ada peringkat
- Senate Majority Stands Up For Survivors, Passes Child Victims ActDokumen5 halamanSenate Majority Stands Up For Survivors, Passes Child Victims ActNew York State Senate Democratic ConferenceBelum ada peringkat
- Senate Majority Passes Sweeping Anti-Gun Violence Legislation To Protect New YorkersDokumen7 halamanSenate Majority Passes Sweeping Anti-Gun Violence Legislation To Protect New YorkersNew York State Senate Democratic ConferenceBelum ada peringkat
- Standing Up For Women's Rights: Senate Majority Passes Historic Pro-Women LegislationDokumen7 halamanStanding Up For Women's Rights: Senate Majority Passes Historic Pro-Women LegislationNew York State Senate Democratic ConferenceBelum ada peringkat
- Long Island Senate Democrats Stand Up For TaxpayersDokumen3 halamanLong Island Senate Democrats Stand Up For TaxpayersNew York State Senate Democratic Conference100% (1)
- Senate Majority Passes Legislation To Prioritize Students Education Over High-Stakes TestingDokumen4 halamanSenate Majority Passes Legislation To Prioritize Students Education Over High-Stakes TestingNew York State Senate Democratic Conference100% (1)
- 01.23.19 Property Tax Cap ReleaseDokumen3 halaman01.23.19 Property Tax Cap ReleaseNew York State Senate Democratic ConferenceBelum ada peringkat
- History Made: Senate Majority Leader Andrea Stewart-Cousins Opens 2019 Senate Session As First Woman To Ever Lead New York State Legislative ChamberDokumen5 halamanHistory Made: Senate Majority Leader Andrea Stewart-Cousins Opens 2019 Senate Session As First Woman To Ever Lead New York State Legislative ChamberNew York State Senate Democratic ConferenceBelum ada peringkat
- Senate Democratic Leader Andrea Stewart-Cousins Earns High Score From New York League of Conservation VotersDokumen1 halamanSenate Democratic Leader Andrea Stewart-Cousins Earns High Score From New York League of Conservation VotersNew York State Senate Democratic ConferenceBelum ada peringkat
- Statement From Senate Democratic Leader Andrea Stewart-Cousins On The Passing of Dr. Olivia HookerDokumen2 halamanStatement From Senate Democratic Leader Andrea Stewart-Cousins On The Passing of Dr. Olivia HookerNew York State Senate Democratic ConferenceBelum ada peringkat
- 08.24.18 ASC Trump Tax StatementDokumen1 halaman08.24.18 ASC Trump Tax StatementNew York State Senate Democratic Conference100% (1)
- Pricey Predicament: Access To Affordable Emergency ContraceptionDokumen9 halamanPricey Predicament: Access To Affordable Emergency ContraceptionNew York State Senate Democratic ConferenceBelum ada peringkat
- Statement From Senate Democratic Leader Andrea Stewart-Cousins On Legislative Pay IncreasesDokumen1 halamanStatement From Senate Democratic Leader Andrea Stewart-Cousins On Legislative Pay IncreasesNew York State Senate Democratic ConferenceBelum ada peringkat
- 06.27.18 ASC Statement On Janus DecisionDokumen1 halaman06.27.18 ASC Statement On Janus DecisionNew York State Senate Democratic ConferenceBelum ada peringkat
- ICYMI: Senate Democratic Leader Andrea Stewart-Cousins Op-Ed: Want To Protect Women's Reproductive Health in New York? Elect Democrats To SenateDokumen2 halamanICYMI: Senate Democratic Leader Andrea Stewart-Cousins Op-Ed: Want To Protect Women's Reproductive Health in New York? Elect Democrats To SenateNew York State Senate Democratic ConferenceBelum ada peringkat
- Statement From Senate Democratic Leader Andrea Stewart-Cousins Regarding Speed CamerasDokumen1 halamanStatement From Senate Democratic Leader Andrea Stewart-Cousins Regarding Speed CamerasNew York State Senate Democratic ConferenceBelum ada peringkat
- Standing Up For Women's Health and Rights: Senate Democrats Force Vote On Comprehensive Contraception Coverage Act and Reproductive Health ActDokumen4 halamanStanding Up For Women's Health and Rights: Senate Democrats Force Vote On Comprehensive Contraception Coverage Act and Reproductive Health ActNew York State Senate Democratic ConferenceBelum ada peringkat
- Don't Put A Cap On Justice: Why The Child Victims Act Is Worth ItDokumen8 halamanDon't Put A Cap On Justice: Why The Child Victims Act Is Worth ItNew York State Senate Democratic ConferenceBelum ada peringkat
- Senate Democrats & Governor Cuomo Call For Roe v. Wade CodificationDokumen4 halamanSenate Democrats & Governor Cuomo Call For Roe v. Wade CodificationNew York State Senate Democratic ConferenceBelum ada peringkat
- Statement From Senate Democratic Leader Andrea Stewart-Cousins On Republican Member Items ResolutionsDokumen1 halamanStatement From Senate Democratic Leader Andrea Stewart-Cousins On Republican Member Items ResolutionsNew York State Senate Democratic ConferenceBelum ada peringkat
- 06.18.18 SenDem Property Tax Relief Plan ReleaseDokumen3 halaman06.18.18 SenDem Property Tax Relief Plan ReleaseNew York State Senate Democratic ConferenceBelum ada peringkat
- Statement From Senate Democratic Leader Andrea Stewart-Cousins On The Confirmation of Justice Paul FeinmanDokumen1 halamanStatement From Senate Democratic Leader Andrea Stewart-Cousins On The Confirmation of Justice Paul FeinmanNew York State Senate Democratic ConferenceBelum ada peringkat
- 05.03.18 Senate Democratic Leader Andrea Stewart-Cousins' Statement On Senator Larkin's RetirementDokumen1 halaman05.03.18 Senate Democratic Leader Andrea Stewart-Cousins' Statement On Senator Larkin's RetirementNew York State Senate Democratic ConferenceBelum ada peringkat
- 05.01.18 Why Don't More New Yorkers Vote?: A Statewide Snapshot Identifying Low Voter TurnoutDokumen12 halaman05.01.18 Why Don't More New Yorkers Vote?: A Statewide Snapshot Identifying Low Voter TurnoutNew York State Senate Democratic ConferenceBelum ada peringkat
- Protecting New York's Democracy: Senate Democrats Issue Report, Sponsor Bills To Fix Election LawsDokumen5 halamanProtecting New York's Democracy: Senate Democrats Issue Report, Sponsor Bills To Fix Election LawsNew York State Senate Democratic ConferenceBelum ada peringkat
- What is Economics? - The study of production, distribution and consumption /TITLEDokumen37 halamanWhat is Economics? - The study of production, distribution and consumption /TITLEparthBelum ada peringkat
- The Impact of Rapid Population Growth On Economic Development in Ethiopia - 045539Dokumen51 halamanThe Impact of Rapid Population Growth On Economic Development in Ethiopia - 045539ABAYNEGETAHUN getahunBelum ada peringkat
- Chairing A Meeting British English TeacherDokumen7 halamanChairing A Meeting British English TeacherJimena AbdoBelum ada peringkat
- Schmitt NF JumpDokumen1 halamanSchmitt NF JumpKim PalmieroBelum ada peringkat
- Microeconomics Chapter 1 IntroDokumen28 halamanMicroeconomics Chapter 1 IntroMc NierraBelum ada peringkat
- Name and Address: No. Name of Contact and Phone / Fax NumbersDokumen1 halamanName and Address: No. Name of Contact and Phone / Fax NumbersmohammedBelum ada peringkat
- Vietnam Trade MissionDokumen2 halamanVietnam Trade MissionXuân NguyễnBelum ada peringkat
- DR Winston McCalla, Lessons From The Caribbean Region Experience, Presentation, 2-2012Dokumen21 halamanDR Winston McCalla, Lessons From The Caribbean Region Experience, Presentation, 2-2012Detlef LoyBelum ada peringkat
- López Quispe Alejandro MagnoDokumen91 halamanLópez Quispe Alejandro MagnoAssasin WildBelum ada peringkat
- Stock DividendsDokumen7 halamanStock DividendsShaan HashmiBelum ada peringkat
- Foregin Policy IndiaDokumen21 halamanForegin Policy IndiaJeevandeep Singh DulehBelum ada peringkat
- OCI DiscussionDokumen6 halamanOCI DiscussionMichelle VinoyaBelum ada peringkat
- Understanding Consumer Equilibrium with Indifference CurvesDokumen6 halamanUnderstanding Consumer Equilibrium with Indifference CurvesJK CloudTechBelum ada peringkat
- Tata Motors Suv Segment ProjectDokumen57 halamanTata Motors Suv Segment ProjectmonikaBelum ada peringkat
- SAARC - Successes and Challenges PDFDokumen6 halamanSAARC - Successes and Challenges PDFalam amarBelum ada peringkat
- Array 5x2 On Concrete Block Ballast-01Dokumen2 halamanArray 5x2 On Concrete Block Ballast-01Wisnu WicaksonoBelum ada peringkat
- Elasticity of SupplyDokumen11 halamanElasticity of Supply201222070% (1)
- Microeconomia: Preferenze Lessicografiche (Dimostrazioni Delle Proprietà)Dokumen3 halamanMicroeconomia: Preferenze Lessicografiche (Dimostrazioni Delle Proprietà)maslsl daimondBelum ada peringkat
- Tony Tan Caktiong – Jollibee founderDokumen6 halamanTony Tan Caktiong – Jollibee founderRose Ann0% (1)
- Jonathan Timm ResumeDokumen2 halamanJonathan Timm ResumeJonathan TimmBelum ada peringkat
- Davaney Progressive Faith and Social Justice Final 3-19-2014 PDFDokumen124 halamanDavaney Progressive Faith and Social Justice Final 3-19-2014 PDFAnne Santos100% (1)
- Project Study Template - Ver2.0Dokumen14 halamanProject Study Template - Ver2.0Ronielle MercadoBelum ada peringkat
- Cleared OTC Interest Rate Swaps: Security. Neutrality. TransparencyDokumen22 halamanCleared OTC Interest Rate Swaps: Security. Neutrality. TransparencyAbhijit SenapatiBelum ada peringkat
- The Illinois QTIP Election To The RescueDokumen5 halamanThe Illinois QTIP Election To The RescuerobertkolasaBelum ada peringkat
- Revised approval for 132/33kV substation in ElchuruDokumen2 halamanRevised approval for 132/33kV substation in ElchuruHareesh KumarBelum ada peringkat
- HUDCO BRIEF - Nasa - Brief276Dokumen4 halamanHUDCO BRIEF - Nasa - Brief276GS MohanBelum ada peringkat
- Foreign Investment Act SummaryDokumen3 halamanForeign Investment Act SummaryPrisiclla C CarfelBelum ada peringkat
- Money and Monetary StandardsDokumen40 halamanMoney and Monetary StandardsZenedel De JesusBelum ada peringkat