IndianJPharmacol283143-4034461 111224
Diunggah oleh
mrunaliiDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
IndianJPharmacol283143-4034461 111224
Diunggah oleh
mrunaliiHak Cipta:
Format Tersedia
Indian Journal of Pharmacology 1996; 28: 143-151
EDUCATIONAL FORUM
PROGRESS MADE IN NON-INVASIVE INSULIN DELIVERY
V.P. PATKI, S.H. JAGASIA
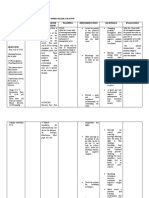
Department of Pharmacology, Grant Medical College, Byculla, Mumbai 400 008. Accepted for publication: December 11, 1995 Summary Insulin is used in the treatment of Diabetes Mellitus. It is a small protein having a molecular weight of 5808. An ideal insulin delivery system should deliver insulin in a pulsatile manner, control the rate of insulin delivery depending on blood glucose concentration, should be delivered into the portal circulation. In addition there should be minimum intraindividual variation, it should be easy to administer and economical. The current insulin treatment does not meet these requirements, hence alternate routes are being developed. The oral delivery though the most convenient and acceptable route however is degraded by intestinal enzymes therefore. insulin was administered with enzyme inhibitors, coated with azoaromatic polymer in the form of nanocapsules, liposomes, microemulsions. But oral delivery showed variable responses and could lead to immunological problems. Increased absorption of insulin by the nasal mucosa was tried by adding various surfactants and by increasing the time of contact. However these surfactants caused irritation and could lead to anti-insulin antibodies. The advantage of pulmonary aerosol is that significant absorption of insulin takes place without the use of absorption promoting agents. The long term effects of this delivery has to be assessed. Besides these the other routes tried are ocular, transdermal. buccal, rectal and vaginal. Insulin delivery buccal rectal oral nasal vaginal pulmonary ocular transdermal
Key words
Diabetes Mellitus is the most common endocrine disease. The frequency of diabetes mellitus in India is 1-2%. Most patients cannot be controlled on oral antidiabetics alone and require insulin. The Indian population, having low socio-economic background can hardly afford to go to the doctor for injections, as well as they are not in a position to face the complications of injection. Therefore, the need for other routes. 1. INDICATIONS FOR INSULIN THERAPY IN DIABETES MELLITUS ARE: (a) Insulin dependent diabetes mellitus (IDDM), (b) diabetic ketoacidosis, (c) non-ketotic hyperglycaemic state, (d) stress of surgery, infection, injury, (e) diabetes during pregnancy, (f) non obese NIDDM unresponsive to oral drugs and (g) NIDDM desirous of preventing long term complications. 2. CHEMISTRY OF INSULIN Insulin IS a small protein and human insulin has a molecular weight of 5808. It is composed of two amino acid chains connected to one another by disulfide linkages. Integrity of insulin molecule must
be maintained for biological activityl,2. Insulin is secreted by the p-cells of the islet of Langerhans. It affects the carbohydrate, protein and fat metabolism. 3. CHARACTERISTICS OF AN IDEAL INSULIN DELIVERY SYSTEM (a) The system should deliver insulin in a pulsatile manner to minimise down regulation of receptors and to reduce the dosage of insulin3. (b) The system should be able to automatically adjust the rate of insulin delivery depending on blood glucose and amino acid concentration i.e. low basal insulin and high prandial insulin level. (c) Since the metabolic processes are centered around the liver, which removes approximately 50% of insulin presented to it. The reactivity of the liver to a given concentration of insulin is much greater than that of peripheral tissues so that delivery of lower dose of insulin in hepatic portal vein can regulate gluconeogenesis and glycogenolysis reducing exposure to peripheral tissues4v5. (d) There should be minimal intraindividual variation. (e) Easy to administer, so as to improve the patient compliance. (f) Economical.
Correspondence: Dr.(Mrs.) V P. Patki
144
V.P. PATKI AND S.H. JAG ASIA
4. SUBCUTANEOUS INSULIN TREATMENT Intensified insulin therapy consists of basal insulin given in the form of either twice-daily injections of delayed action - lente or isoplane (NPH) insulin or once- or twice- daily injections of longer acting ultralente Continuous subcutaneous Insulin infusion (CSII) from a portal pump is used for basal insulin s~pply~~. Prandial insulin is given by injection of short-acting insulin given 30 min before meals, Problems of subcutaneous insulin treatment (a) Insulin is not delivered in a pulsatile manner. (b) Because of the delay in subcutaneous absorption, therefore insulin is administered 30 min before meal&% The other problem is slow return to the baseline after meal-time injection. There is therefore, marked overinsulinization between meals and a consequent risk of hypoglycemia occurring some hours after insulin injection in IDDM. (c) The peripheral delivery of insulin rather than portal, causes high plasma free insulin levels and this may accelerate the development of macrovascular disease9 (d) The intra-individual coefficient of variation for the time until 50% of the dose is absorbed is approximately 25% for all injected insulinlO. (e) Poor patient compliance due to pain on injection. This pain is experienced less by many patients using pens, compared to syringe and needles. Probably the main cause of pain is a blunt needle, needles being blunted by multiple puncture of the rubber diaphragm of insulin vials, now that re-use of disposable syringes is a common practice. The needles of the insulin pens may remain sharper for longer time because withdrawal of insulin from the vials is not needed. Due to these problems there is a need for the alternate insulin delivery systems, which are being developed currently. They are discussed below: 5. ORAL DELIVERY Oral delivery is the most convenient and the most acceptable route. However, insulin by itself is degraded by intestinal enzymes and is not absorbed intact across the gastrointestinal mucosa12-14. 5.1 Studies on oral insulin absorption Experimental Absorption of insulin from the small intestine resulting in lowering of blood glucose has been shown to occur in animals in the first few days after birth15li6 and when the pancreatic enzymes are either absent or inactivated in the gut17-lg.
5.2 Clinical Similar experiment in a patient who underwent total pancreatectomy demonstrated that the human intestine has the capacity to absorb insulin in an active form. However, only 0.5% of the dose given was absorbed*O. This may indicate that capacity of human intestine to absorb insulin is limited but seems more likely due to the proteolytic effect of pepsin and peptidases located on the brush borders of the mucosal cells*o. For insulin to be effective orally it must be protected against proteolysis in the GIT and its absorption should be increased. 5.3 Protection against proteolysis Insulin may be degraded in the gut by pepsin and pancreatic proteolytic enzymes21-25. Administration of enzyme inhibitors with insulin resulted in absorption of insulin and decrease in blood glucose from rat intestine preparation26-28. Insulin along with hexylresorcinol and sodium carbonate when injected into the intestines of normal dogs produced a drop in blood glucose depending on insulin concentration, pH of the solution and surface tension2g,30. The effectiveness in promoting insulin absorption does not depend on the hydrophilic - hydrophobic properties of hyxylresorcinol but is due to inhibition of pepsin and trypsin*s-31. The P-naphthyl-azo-polystyrene-insulin (insulin absorbed physically on P-naphthyl-azo-polystyrene particles / P-NAS-I) was found to interfere with peptic and chymotryptic digestions in vitro and when administered to the stomach, upper jejunum of rabbits produced hypoglycemic response3*. Insulin was coated with polymer cross-linked with azoaromatic group to protect it against attack of digestive enzyme@. This cross-link is broken by microflora present in the colon. The azoaromatic polymer delivery systems when tested in streptozotocin induced diabetic rats showed responses occuring at variable times from l-9 h after administration. This could be due to variations in intestinal transit time among various animals. Gwinup et al 34 encapsulated insulin with a methacrylic acid copolymer and demonstrated an increase in immunoreactive insulin at 4-5 h after per oral insulin ingestion. Results of administration of these preparations in patients with diabetes have yet not been reported. 5.4 Effect of different delivery systems Insulin may be associated with a colloidal delive system, polyalkylcyanoacrylate nanocapsules3 L!
METHODS OF NON-INVASIVE INSULIN DELIVERY
145
These are spherical structures less than 300 nm in diameter surrounded by a biodegradable polymeric wall composed of isobutylcyanoacrylate36. It has been found that nanoparticles less than 200 nm in diameter passed through the intestinal mucosa probably by paracellular pathway3. Damge et aP5 discovered that insulin trapped in nanoparticles remain biologically active after oral administration. Moreover, the duration but not the intensity of the biological response depends on the amount of nanocapsules administered lasting upto 6 or 20 days with a single oral administration of 12.5 or 50 U/kg encapsulated insulin respectively35. The biological effect of insulin nanocapsules depends on the amount of both insulin and polymer38. The intensity and duration also depends on the site of administration (65% ileum, 59% stomach, 52% duodenum and jejunum, 34% colon). This hypoglycemic effect lasted upto 18th day after administration for ileum and jejunum, 15th day for the stomach and duodenum and 13th day for the colon38. The nanoparticles protects insulin against enzymatic degradation in vitro 38. Intestinal absorption of nanocapsules is very rapid3, after intrajejunal administration nanocapsules were recovered in villous blood vessels within 30-60 mins. The transmucosal passage is even more rapid in the ileum through Peyers patches since 10 mins after administration the nanocapsules were found in the underlying lymph ducts. The poor ability of the colon to absorb insulin nanocapsules is due to poor absorptive surface. The presence of surfactants, Poloxamer 188, facilitates the absorption of insulin released from nanocapsules. Whether the repeated administration of nanoparticles can lead to formation of antibodies has to be determined. Patel and Ryman3g showed that oral administration of 5 or 12U of insulin entrapped in liposomes (phosphatidylcholine/cholesterol/diacetyl phosphate in the ratio of 10/2/1) reduced blood glucose levels between 30 and 60% after administration to streptozotocin-induced diabetic rats but not in normal rats. They showed hypoglycemic effect in normal rat by pretreatment with indole-3-acetic acid which probably prevents destruction of insulin40. Dapergolas and Gregoriadis4 observed a 40 and 60% lowering of blood glucose 4 h after delivering 0.3 or 2.9 U insulin trapped in liposome (phosphatidyl-inositol base) to diabetic and normal rats. They also observed that solid liposomes were more effective than fluid liposomes42. Patel etafi3 observed a slight rise in immunoreactive plasma insulin when 80-9OU of insulin per volunteer, liposomes phosphatidyl-
choline/cholesterol in the proportion of 10/2 was administered by the jejunal route. Weingarten ef al 44 demonstrated liposomes which are inactive when administered intragastrically have marked hypoglycemic effect when given by mouth, in the rat. Thus the influence of the administration route is important. Hashimoto and Kawada45 demonstrated liposomes have protective effect against proteolytic digestive enzymes (pepsin and pancreatin) but these effects disappeared in the presence of bile salts. lntragastric administration of insulin trapped in dipalmitoyl phosphatidylcholine/cholesterol/phosphatidic acid (7:2:1) liposomes led to a 5 to 20 fold increase in insulin in lymph obtained from thoracic duct and a two-fold rise in the portal vein46. Since major part of insulin delivered from liposomes enters the lymph there could be immunological problems after repeated administration. Engel et al 47 developed a water in oil in water (w/o/w) emulsion, the emulsion of palmitic acid was prepared using sodium lauryl sulphate as emulsifying agent. There was a decrease in blood glucose by 35% in rats and 57% in gerbils after 60 min. Schichiri et a/48 showed in vitro the w/o/w emulsion of insulin was resistant to the action of pepsin, trypsin and a-chymotrypsin. However, when incubated with pancreatic lipase 33% of insulin activity was retained after 3 h of incubation. They demonstrated a significant decrease in urinary glucose when the preparation was given by an indwelling catheter to alloxan-diabetic rats. Cho and Flynn4g prepared an oil-in-water microemulsion in which the aqueous phase contained insulin and in which the oil phase consisted of cholesterol:lecithin and esterified fatty acids in the proportion of 1:2:14. The insulin was protected by protease inhibitor aprotinin in the aqueous phase. This microemulsion was sprayed on to an inert carried carboxymethylcellulose calcium and placed in hard gelatin capsules. There was a substantial reduction in blood glucose when this formulation was administered orally. This preparation would probably be absorbed via the intestinal lymphatics into the systemic circulation. If the insulin was freed in the systemic circulation before reaching the liver this method of delivery would be convenient but would not contribute significantly to hyperinsulinaemia-dependent complications. Furthermore, if uptake of insulin-rich lipid takes place in the blood vessels, which like the liver, have lipoprotein receptors, the oral preparation might enhance rather than limit insulin related angiopathy50.
146
V.P. PATKI AND S.H. JAGASIA
5.5 Others The presence of sodium-5-methoxysalicylate aids in the absorption of insulin from the upper GIT resulting in significantly elevated insulin levels and reduced glucose levels in the plasma of rats?. Acarbose, an intestinal o-glucosidase inhibitor decreases postprandial glycemia by delaying carbohydrate absorption and also affords some beneficial effects in the diabetic animal. Katovich and Meldrum5* showed that combined insulin and acarbose therapy was more beneficial than individual therapy alone and insulin requirement can be reduced with adjuvant acarbose treatment, Advantages (a) It is the most convenient route. Therefore, improved patient compliance and (b) improved portal levels of insulin. Therefore, it may prevent hyperinsulinaemia associated with other insulin deliveries which may be an important factor in the development of atherosclerosis8n53. Limitations (a) Variable response at variable time due to variations in intestinal transit time, (b) whether insulin administered in the form of nanocapsules, liposomes, microemulsions would lead to immunological problem has to be determined and (c) delivery of insulin is not pulsatile. 6. NASAL DELIVERY lntranasal delivery of insulin will result in improved compliance, however, insulin is subjected to proteolysis in the nasal mucosa14,54,55. 6.1 Studies on nasal insulin absorption Hirai et a/ 56 administered 0.1 ml of insulin preparation to the nasal cavity of male beagle dogs in the form of nebulized spray. A rise in the plasma immunoreactive insulin and concomitantly significant hypoglycemia was observed which was dependent on pH. 6.2 Addition of surfactants to increase absorption When a surfactant such as saponin, sodium glycocholate or BL-9 was added to the preparation, the absorption of insulin from the nasal mucosa was enhanced independent of pH. Gordon et ap7 studied the effects of different bile salts at various concentrations on intranasal insulin absorption in man. Maximum increase in serum insulin was
obtained using deoxycholate followed by chenodeoxy-cholate and cholate at 1% w/v. Blood glucose concentration reduced by approximatly 50% with deoxycholate and peak serum insulin concentration was reached in 10 min after administration of the Spray. Similar results were also obtained by Moses et al 5s. Absorption enhancing effect of different cyclo-dextrins on intranasally administered insulin in rats and rabbits was determined5ssc. Dimethyl-beta-cyclodextrin was found to be most potent5snsc. Nasal absorption is also promoted by medium chain fatty acid salt&, glycyrrhetinic acid derivatives in rat&*, sodium tauro-24,25-dihydrofusidate in sheepss. Etr et al 64 demonstrated that the blood glucose remained low for 3 h after lunch when insulin was used intranasally with 1% deoxycholate in type II diabetics. The relative effectiveness of the nasal and subcutaneous insulin in IDDM was compared65. The intranasal dose administered was 10 times higher than the subcutaneous dose. Upto 90 min the plasma glucose levels were identical by both routes. However, at 120 and 150 min plasma glucose was higher after intranasal insulin in all patients. When Pontiroli eta/66 administered insulin subcutaneously and by the nasal route to four IDDM patients at doses in ratio of 1:9, the intranasal insulin was more effective than SC insulin in lowering fasting blood glucose concentration and in counteracting rises in blood glucose concentration after breakfast. In four other IDDM patients intranasal and SC insulin were about equal in effectiveness in the morning; whereas intranasal insulin was slightly less effective during the afternoon. A 6-month non-randomised crossover outpatient trial, for testing if nasal aerosol spray containing insulin in laureth-9 could be tolerated was conducted All patients (IDDM) were treated first with nasal and ultralente insulin for 3 months and were then switched over to a 3-month regimen of conventional SC insulin. There was no significant difference in overall glycemic control between the regimen of nasal and ultralente insulin and the conventional insulin treatment. Four patients dropped due to nasal irritation. The local irritation varied widely among the subjects tested. Nasal stinging, congestion and rhinorrhoea was predominant due to surfactant and were proportional to its concentration. However, in another study using intranasal spray of insulin with 0.25% laureth-9 for a month instead of preprandil SC bolus in 10 IDDM patients
METHODS OF NON-INVASIVE INSULIN DELIVERY
147
the glycemic control worsened65. Four patients had to be withdrawn from the study because of very inadequate glycemic control. Mean capillary glucose before the evening meal was significantly higher with intranasal insulin. HbAlc increased in all patients. 1 of the IO complained of nasal irritation. Anti-insulin antibodies increased in one patient who received intranasal spray for 12 months (anti-insulin antibodies fell after resumption of SC regimen), the nasal mucosa of this patient was not affected. Another patient, after 17 months, had chronic rhinitis with anosmia65. 6.3 Increased absorption by increasing the time of contact The nasal absorption of insulin can be increased by increasing the time of contact with the nasal mucosa. The clearance half- life can be increased from 15 min with nasal solution to 240 min using starch microspheres (SMS). Insulin administered in combination with SMS resulted in 497% increase in AUC for plasma insulin as compared to insulin solution. The AUC increased by 1657% compared to insulin solution when an enhancer- lysophosphatidylcholine was used with insulin and SMS68. 6.4 Advantages (a ) No pain experienced, therefore improved patient compliance, (b) the intrasubject and intersubject variation in kinetics of nasal insulin absorption are small69 and (c) useful for administering insulin before meals. 6.5 Limitations (a) Irritation due to surfactants, (b) may increase anti-insulin antibodies and (c)effect of allergic rhinitis on the absorption of intra-nasal insulin is not known. 7. PULMONARY DELIVERY The advantage of pulmonary aerosols is that significant absorption of insulin takes place without the use of absorption- promoting agents. Moreover, the metabolism in the lungs may not present a significant barrier to the absorption of bioactive insulln7D. 7.1 Studies on pulmonary insulin absorption A rise in the plasma IRI and decrease in plasma glucose in normal and diabetic patients on administration of aerosolized insulin was reported71. Recently insulin was administered approximated 1 .O U/kg body weight (without promotor) as an aerosol by oral inhalation to 6 non-obese non-smoking
NIDDM patients 72. Gamma camera imaging demonstrated that 7917% of the inhaled dose was deposited in the lungs. Geometric mean fasting plasma insulin level was 71 pmol/L rising t o 2 6 9 PmOl/L after insulin inhalation. Average time to peak insulin level was 4034 min. The mean fasting plasma glucose was reduced to within the normal range in 5 subjects and was almost normal in the sixth subject. Average maximum decrease in plasma glucose from the baseline was 5510% (n= 6) Vs 139% after placebo aerosol inhalation (n=3) containing 0.9% saline indicating that the observed decrease in glucose levels after insulin inhalation was not the result of fasting. No side effects were reported following insulin or placebo aerosol inhalation. This route seems promising however, additional studies are necessary to know the reproducibility of the glucose, the long-term effects of zinc and the preservative and the effective dose of aerosolized insulin required to normalize plasma glucose levels after a mea172. The insulin used was made from purified pork zinc-insulin crystals. A preservative - cresol was added7*. 7.2 Advantages (a) No side effects and (b) no pain experienced while administering. 7.3 Limitations (a) Long term effect has to be assessed and (b) further studies necessary on more patients. 8. OCULAR DELIVERY Very little work has been done in this area. Studies on ocular insulin absorption Nomura et a/ 73 administered insulin solution to upper conjunctival sac in 5 mongrel dogs. They demonstrated that insulin absorption from the conjunctiva was rapid; there was significant and constant increase in plasma IRI levels as early as 5 min after administration causing significant decrease in plasma glucose. The bioavailability of insulin was significantly higher in diabetic dogs (between 1 and 7%) than in normal dogs (less than 0.5%). After 2 months of insulin administration in rabbits there was no significant changes in the ocular tissues. In man, the volume of the conjunctival sac is at the most only 20-30 L so a higher insulin concentration would be needed. Nomura et al however, found the bioavailability decreases when insulin concentration is increased. Others have also investigated this route74-76.
148
V.P. PATKI AND S.H. JAGASIA
9. TRANSDERMAL DELIVERY Attempts have been made to overcome the barrier properties of the skin by iontophoresis or using ultrasonic vibrations. Studies on transdermal insulin absorption A number of investigations are exploring iontophoretic transdermal insulin delivery7717*. The rate of iontophoretic delivery of insulin depends on the properties of the formulation and the electronic variables of the delivery system. Tachibana et al 7g tried delivering insulin to the body by the use of ultrasonic vibration to the skin surface of hairless mice. Exposure to lower energy vibrations (3000-5000 Pa) produced minimum blood sugar at 120 min of 34.111.9% of the initial concentration. The values rose to 53.5 9.3% at 240 min and animal dying of hypoglycemia at 180 min. Exposure to the higher energy vibration produced a minimum at 120 min, 22.43.9% of the control value. The glucose concentration rose to 37.33.2% at 240 min, with two mice dying of hypoglycemia at 150 min and once at 180 min. Limitations Successful studies have been limited to animal models. 10. MISCELLANEOUS Insulin was absorbed from the buccal mucosa in animal studies and caused a decrease in blood glucose*o-82. The percentage of insulin absorbed was 0.5% compared with amount absorbed upon intramuscular injection of insulinso.
Insulin by itself is not absorbed to an appreciable degree across the rectal mucosa*3~*4. Various adjuvants have been used to promote insulin absorption82-86. Side effects included abdominal discomfort and rectal urgency and are probably due to the surfactants used in supposito@. Insulin can be absorbed across the va inal mucosa when administered as a suppository B8. However, very limited work has been done. 11. CONCLUSION Although the oral route of insulin delivery would be most convenient, however, the intestinal absorption of insulin is low, variable and inconsistent whatever is the added surfactant, enzyme inhibitor, polymer coating used. This variability would expose the patient to wide swings from the peaks of hyperglycemia to life threatening troughs of hypoglycemia. Insulin associated with nanocapsules gives a prolonged hypoglycemia. Microemulsion of insulin also produced a significant decrease in blood glucose. Before being put to clinical use it is necessary to know if insulin is distributed in the systemic circulation or in the lymphatics. If in the latter insulin would lead to the formation of antibodies. Therefore, it cannot be administered repeatedly. Nasal insulin, could be used as a preprandial dose but it may cause an increase in anti-insulin antibodies. Pulmonary route seems to be the most promising route but its efficacy in larger number of patients and long term efficacy and safety has to be established. Transdermal route, though encouraging results have been obtained on animals, its effect on humans has to be determined.
REFERENCES
I. Sanger F. Chemistry of insulin. Br Med Bull 1960;16:183-8. 6. Pickup JC, Keen H, Parsons JA, Alberti KGMM. Continuous subcutaneous insulin infusion: an appeal to achieving normoglycemia. Br Med J 1978;1:204-7. 7. Pickup JC, White MC, Keen H, Kohner EM, Parsons JA. Alberti KGMM. Long term continuous subcutaneous insulin infusion in diabetes at home. Lancet 1979;2:870-3. 8. Kinmonth AL, Baum JD. Timing of pre-breakfast insulin injection and post prandial metabolic control in diabetic children. Br Med J 1980;280:604-6. 9. Stout RW. Insulin and atheroma: 20 years perspective. Diabetes Care 1990;13:631-54. 10. Binder C, Lauritzen T, Faber 0, Pramming S. Insulin pharmacokinetics. Diabetes Care 1984;7:188-99.
2. Nicols DSHW. The biological activity of pure peptides obtamed by enzymatic hydrolysis of insulin. Biochem J 1960;75:395-401. 3. Bratusch-Marrain PR, Komjati M, Waldhausl WK. Efficacy of pulsatile versus continuous insulin administration of hepatic glucose productions and glucose utilisation in type I diabetic humans. Diabetes 1986;35:922-6. 4. Schade DS. Eaton RP. Insulin delivery: how, when, where. N Engl J Med 1985;312:1120-1. 5. Eaton RP, Allen RC, Schade DS, Erickson KN. Standefer J. Prehepatic insulin production in man: kinetic analysis using peripheral connecting peptide behaviour. J Clin Endorcinol Metab 1980;51:520-8.
METHODS OF NON-INVASIVE INSULIN DELIVERY
149
11
Collins BJ, Richarson SG, Spence BK, Hunter J. Nelson JK. Safety of reusing disposable plastic insulin syringes. Lancet 1983;1:559- 60. Murlin JR, Gibbs, CBF, Romansky MJ, et al. Effectiveness of peroral insulin in human diabetes. J Clin Invest 1940;19:709- 22. Earle MP. Experimental use of oral insulin. Israel J Med Sci 1992;8:899-900.
28
Bendayan M, Ziv E, Ben-Sasson R, Bar-On H, Kidron M. Morphocytochemical and biochemical evidence for insulin absorption by the rat ileal epithelium. Diabetologia 1990;33:197-204. Daggs RG, Murlin WR, Murlin JR. The effect of hexylresorcinol upon the absorption of insulin from the gastrointestinal tract of dogs. Am J Physiol 1937;120:744-9. Young LE. Phillip WA, Murlin JR. New results on the absorption of insulin from the alimentary tract. Am J Physiol 1937;128:81-91.
12
29
13
30
14. Amidon GL, Lee HJ. Absorption of peptide and peptidomimetic drugs. Ann Rev Pharmacol Toxicol 1994;34: 321-41. 15. Mosinger B, Placer Z, Koldovsky 0. Passage of insulin through the walls of gastrointestinal tract of the infant rat. Nature 1959;184:1245-6. 16. Pierce AE, Risdall. PC, Shaw B. Absorption of orallv administered insulin by the newly born calf. J Physiol 1964;171:203-15.
31. Sealock RR, Murlin JR, Driver RL. A comparative study of the effect of alkylresorcinols and related compounds upon the absorption of insulin from isolated intestinal loops of anaesthetized dogs. Am J Physiol 1939;128:92-6. 32. Shigeta Y, Shichiri M, Okada A, Karasaki K. Plasma immunoreactive insulin after intestinal administration of I;naphthyl-azo-polystyrene-insulin to the rabbit. Endocrinology 1972;91:320-2. 33. Saffran M, Kumar GS. Savariar C, Burnham JC, Williams F, Neckers DC. A new approach to the oral administration of insulin and other peptide drugs. Science 1986;233:1081-4 34. Gwinup G, Elias AN, Domurat ES. Insulin and C-peptide levels following oral administration of insulin in testinal enzyme protected capsules. Gen Pharmacol 1991:22, 243-6. 35. Damge C, Michel C, Aprahamian M, Couvreur P. New approach for oral administration on insulin with polyalkylcyanoacrylate nanocapsules as drug carriers. Diabetes 1988;37:246-51. 36. Al-Khouri FN, Robbot-Trevpel L, Fessi H, Devissaguet JP, Puisieux F. Development of a new process for manufacture of polyiso-butylcyanoacrylate nanocapsules. lntl J Pharmaceut 1986:28:125- 32. 37 Aprahamian M, Michel C. Humbert W. Devissaguet JP, Damge C. Transmucosal passage of polyalkylcyanoacry late nanocapsules as a new drug carrier in the small intestine. Biology Cell 1987;61:69-76. Michel C, Aprahamian M, Defontaine L, Couvreur P, Damge C. The effect of site of administrtion in the gastrointestinal tract on the absorption of insulin from nanocapsules in diabetic rats. J Pharmacy Pharmacol 1991;43:1-5. Patel HM, Ryman BE. Oral administration of insulin by encapsulation within lioosomes FEBS Letters 1976;62 60-3. Patel HM, Ryman BE. Orally administered liposomally trapped insulin in normal man. Biochem Soc Transact 1977;6:784-5. Dapergolas G, Gregoriadis G. Hypoglycemic effect of liposome entrapped insulin administered intragastrically into rats. Lancet 1976;2:824-7.
17. Fisher NF. The absorption of insulin from the intestine, vagina and scrotal sac. Am J Physiol 1923;67:65-71. 18. Murlin JR, Hawley EE. Absorption of insulin from the alimentary tract of depancreatized dogs when protected by blood serum Am J Physiol 1927;83:147-61. 19. Danforth E, Moore RO. Intestinalabsorption of insulin in rats, Endocrinology 1959;65:118-23. 20. Crane CW, Path MC, George RWN Luntz. Absorption of insulin from the human small intestine. Diabetes 1968;17:625-7. Banting FG, Best CH. The internal secretion of the pancreas. J Lab Clin Med 1922;7:251-66. Dudley HW. The purification of insulin and some of its properties. Biochem J 1923;17:376-90. Scott DA. The action of trypsin on insulin J Biol Chem 1925;63.641-51. Harned BK, Nash TP. The protection of insulin by antiproteases and its absorption from the intestine. J Biol Chem 1932;97:443-5. Blotner H. The effect of gastric juice, bile trypsin and pancreatin on insulin: the prevention of the digestion on insulin with alcohol. Am J Med Sci 1936:192:263-72. Laskowski M. Jr, Haessler HA, Miech RP, Peansky RJ, Laskowski M. Effects of trypsin inhibitor on passage of insulin across the intestinal barrier. Science 1958;127: 1115-6 Kidron M, Bar-On H, Berry EM, Ziv E. The absorption of insulin from various regions of rat intestine. Life Sciences 1982;31-2837-41.
21.
22
23
24
38
25
39
26
40
27
41
150
V.P. PATKI AND S.H. JAGASIA
42. Dapergolas G, Gregoriadis G. The effect of liposomal lipid composition on the fate and effect of liposome entrapped insulin and tubocurarine. Biochem Soc Transact 1977;5: 1383-6. 43. Patel HM. Harding NGL, Logue F, et al. lntrajejunal absorption of liposomally entrapped insulin in normal man. Biochem Soc Transact 1978;6:784-5. Weingarten C, Moufti A, Desjeux JP, et al Oral ingestion of insulin liposomes effects of the administration route. Life Sci 1981;28:2747-52.
administered intranasally as an insulin-bile salt aerosol. Diabetes 1983;32: 1040-7. 59. Merkus FEW, Verhoef JC, Romeijn SG. Schipper NG. Absorption enhancing effect of cyclodextrins on intranasally administered insulin in rats. Pharm Res 1991;8:588-92. 60. Watanabe Y, Matsumoto Y, Kawamoto K. Yazawa S. Matsumoto M. Enhacing effect of cyclodextrins on nasal absorption of insulin and its duration in rabbits. Chem Pharm Bull, Tokyo 1992;40:3100- 4. 61. Mishima M, Wakita Y, Nakano M. Studies on the promoting effects of medium chain fatty acid salts on the nasal absorption insulin in rats. J Pharmacobiodvn 1987:10:624-31 62. Mishima M, Okada S, Wakita Y, Nakano M. Promotion of nasal absorption of insulin by glycyrrhetinicacid derivatives. J Pharmacobiodyn 1989;12:31-6. 63. Lee WA, Narog BA, Patapoff TW, Wang YJ. lntranasal bioavailability of insulin powder formulations Effect of permeation enhancer-to-protein ratio. J Pharm Sci 1991;80: 725-9. 64. Etr ME, Slama G, Desplanque N. Preprandial intranasal insulin as adjuvant therapy. in type II diabetes. Lancet 1987;2:1085-6. 65. Lassmann-Vague V, Thiers D, Vialettes B, Vague P Preprandial intranasal insulin. Lancet 1988;1:367-8. 66. Pontiroli AE, Alberetto M. Secchi A, Dossi G, Bosi I, Pozza G. Insulin given intranasally induces hypoglycemia in normal and diabetic subjects. Br Med J 1982;284:303-6 67. Salzman R, Manson J, Grifting G, eta/. lntranasal aerosolized insulin: mixed-meal studies and long term use in type I diabetics. New Engl J Med 1985;312:1078-84. 68. Farraj NF, lllum L, Davis SS. Johansen BR. Nasal administration of insulin using microsphere enhancer delivery system. Diabetologia 1989;32:486A. 69. Nolte MS, Taboga C, Salamon E, et al. Biological activity of nasally administered insulin in normal subjects. Horm Metab Res 1990;22:170-4. 70. Liu F, Kildsig DO, Mitra AK. Pulmonary biotransformation of insulin in rat and rabbit. Life Sci 1992;51:1683-9. 71. Wigley FM, Londono JH, Wood SH, Shipp HC, Waldman RH. Insulin across respiratory mucosae by aerosol delivery. Diabetes 1971;20:552-6. 72. Laube BL, Georgopoulos A, Adams GK. Preliminary study of the efficacy of insulin aerosol delivered by oral inhalation in diabetic patients. JAMA 1993;269:2106-9.
44
45. Hashimoto A, Kawada J. Effects of oral administration of positively charged insulin liposomes on alloxan-diabetic rats; preliminary study. Endocrinol Jap 1979;26:337-44. 46. Arrieta-Molero JE, Aleck K, Sinha ML, Brownscheidle CM, Shapiro LJ, Sperling MA. Orally administered liposome entrapped insulin in diabetic animals. Hormone Res 1982;16:249-56. 47. Engel RH, Riggi SJ. Fahrenbach MJ. Insulin: intestinal absorption as water-in-oil-in-water emulsion. Nature 1968;219:856-7. 48. Schichiri M, Kawamori R, Yoshida M, et al. Short treatment of alloxan-diabetic rats with intrajejunal administration of water-in-oil-in-water emulsion. Diabetes 1975;24:971-6. 49 Cho YW, Flynn M. Oral delivery of insulin. Lancet 1989;2:1518-9. 50. Elias AN, Gwinup G. Oral insulin. Lancet 1990;335-55.
51. Nishikata T, Rytting JH, Kamada A, Higuchi T. Enhanced intestinal absorption of insulin in rats in the presence of sodium-5- methoxysalicylate. Diabetes 1981;30:1065-7. 52. Katovich MJ, Meldrum MJ. Effect of insulin and acarbose alone and in combination with the female streptozotcin-induced diabetic rat. J Pharm Sci 1993;82:1209-13. 53. Gwinup G, Elias AN, Vaziri ND. A case of oral insulin therapy in the prevention of diabetic mico and macro angiopathy. lntl J Artifical Organs 1990;13:393-5.
54. Yamamoto A, Hayakawa, Lee VH. Insulin and proinsulin proteolysis in mucosal homogenates of the albino rabbit. implication in peptide delivery from nonoral routes. Life Sci 1990;47:2465-74. 55. Sarkar MA Drug metabolism in the nasal mucosa. Pharm Res 1992;9.1-9. 56. Hirai S, lkenaga T, Matsuzawa T. Nasal absorption of insulin in dogs. Diabetes 1978;27:296-9.
57 Gordon GS, Moses AC, Silver RD. Flier JC, Carey MC. Nasal absorption of insulin. enhancement by hydrophobic bile salts Proc National Acad Sci, USA 1985;82:7419-23. 58. Moses AC, Gordon GS, Carey MC, Flier JS. Insulin
73. Nomura M. Kubota MA, Sekiya M, et a/. Insulin absorption from conjuctiva studied in normal and diabetic dogs. J Pharmacy Pharmacol 1990;42:292-4.
METHODS OF NON-INVASIVE INSULIN DELIVERY
151
74.
Chiou CGY, Chuang CY, Chang MS. Systemic delivery of Insulin through eyes to lower the glucose concentration. J Ocular Pharmacol 1989;5:81-91.
82. Aungst BJ, Rogers NJ, Shefter E. Comparison of nasal, rectal, buccal, sublingual and intramuscular insulin efficacy and the effects of a bile salt absorption promotor. J Pharmac o l Exp Ther 1988;244:23-7. 83. Nishihata T, Rytting JH, Kamada A, Higuchi T, Routh M, Caldwell L. Enhancement of rectal absorption of insulin using salicylates in dogs. J Pharm Pharmacol 1983;35: 148-51. Hauss DJ, Ando HY. The influence of concentration of two salicylate derivatives on rectal insulin absorption enhancement. J Pharm Pharmacol 1988;40:659-61
75. Yamamoto A, Luo AM, Dodd-Kashi S, Lee VHL. The ocular route for systemic insulin delivery in the albino rabbit. J Pharmacol Exptl Therap 1989;249:249-55. 76. Hopper PE, Murphy CJ, Feldman EC, Nelson RW, Bottoms GD, Franti CE. Serum glucose and insulin responses to an insulin containing opthalmic solution administered topically In clinically normal cats. Am J Vet Res 1991;52:903-7. 77. Kri B. Control of blood glucose levels in alloxan-diabetic rabbits by iontophoresis of insulin. Diabetes 1985;35: 217-21. 78. Siddiqui 0, Sun Y, Liu J, Chien Y. Facilitated transdermal transport of insulin. J Pharmaceut Sci 1987;76:341-5.
84.
85. Kim S, Kamada A, Higuchi T, Nishihata T Effect of enamine derivatives on rectal absorption of insulin in dogs and rabbits. J Pharm Pharmacol 1983;35:100-3. 86. van-Hoogdalem EJ, Heijligers Feijen CD, Verhoef JC, de Boer AG, Breimer DD. Absorption enhancement of rectally infused insulin by sodium tauro-24.25-dihydrofusidate (STDHF) in rats. Pharm Res 1990;7:180-3. 87. Kennedy FP. Recent advances in insulin delivery techniques current status and future potential. Drugs 1991;42:213-27. 88. Fisher NF. The absorption of insulin from the intestine, vagina and scrotal sac. Am J Physiol 1923;67:65-71.
79. Tachibana K, Tachibana S. Transdermal delivery of insulin by ultrasonicvibrations. J Pharm Pharmacol 1991;43:270-I.
80.
lshida M. Machida Y. Nambu N, Nagai T. New mucosal dosage form of insulin. Chem Pharm Bull 1981;29:810-6.
81. Nagai T. Adhesive topical drug delivery systems. J Control Rel 1985;2:121-34.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Slide Paparan - Dicky - Potensi Genomik DM BGSIDokumen27 halamanSlide Paparan - Dicky - Potensi Genomik DM BGSIFebrian DewiBelum ada peringkat
- Tensimeter - Erkameter EDokumen8 halamanTensimeter - Erkameter EeryBelum ada peringkat
- European University of Lefke: Eczacılık Fakültesi / Faculty of PharmacyDokumen3 halamanEuropean University of Lefke: Eczacılık Fakültesi / Faculty of PharmacyMariem Ben HediaBelum ada peringkat
- Slow Contact Tracing' Blamed For Spread of New CoronavirusDokumen6 halamanSlow Contact Tracing' Blamed For Spread of New CoronavirusProdigal RanBelum ada peringkat
- 3 NURSING-CARE-PLAN FinaaalDokumen7 halaman3 NURSING-CARE-PLAN FinaaalSam PothBelum ada peringkat
- Agger NasiDokumen3 halamanAgger NasiDr Saikat SahaBelum ada peringkat
- Application For Disabled Parking Placard/Plate: A. Disabled Applicant InformationDokumen2 halamanApplication For Disabled Parking Placard/Plate: A. Disabled Applicant InformationBen ChaimBelum ada peringkat
- Stylohyoid LigamentDokumen4 halamanStylohyoid LigamentArindom ChangmaiBelum ada peringkat
- General Tonic Monograph and Pharmacology Shi Quan Da Bu WanDokumen8 halamanGeneral Tonic Monograph and Pharmacology Shi Quan Da Bu WanrikiBelum ada peringkat
- General Examination For CVSDokumen29 halamanGeneral Examination For CVSstudymedic100% (1)
- Laboratory Investigation ReportDokumen7 halamanLaboratory Investigation ReportAmarjeetBelum ada peringkat
- HSG Maxessential Brochure W ForeignersDokumen18 halamanHSG Maxessential Brochure W Foreignersswapnil.pandeyBelum ada peringkat
- OTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Dokumen10 halamanOTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Ladyfair TanticoBelum ada peringkat
- Structure and Neural Mechanisms of CatatoniaDokumen10 halamanStructure and Neural Mechanisms of CatatoniaAlejandra ToralBelum ada peringkat
- Ati #3Dokumen8 halamanAti #3Leah Elizabeth100% (8)
- Complications of Brain Tumors and Their TreatmentDokumen18 halamanComplications of Brain Tumors and Their TreatmentBenedictus Yudha BaskaraBelum ada peringkat
- How Do I Know If My Activities Are of Moderate To Vigorous Intensity?Dokumen2 halamanHow Do I Know If My Activities Are of Moderate To Vigorous Intensity?Balsc Bals BalscBelum ada peringkat
- Argumentative EssayDokumen7 halamanArgumentative EssayHuy BuiBelum ada peringkat
- Test Bank For Phlebotomy 4th Edition by Warekois DownloadDokumen9 halamanTest Bank For Phlebotomy 4th Edition by Warekois Downloadryanparker18011988fno100% (23)
- Homoeopathy in Breast Cancer: AbstractsDokumen5 halamanHomoeopathy in Breast Cancer: Abstractskathir_cBelum ada peringkat
- Tabel Severitas BPJS Tindakan JantungDokumen9 halamanTabel Severitas BPJS Tindakan JantungTeduh ParamadinaBelum ada peringkat
- How To Manage Cortisol Levels With Maca RootDokumen19 halamanHow To Manage Cortisol Levels With Maca RootCalvin McDuffieBelum ada peringkat
- 307-Article Text-578-1-10-20210309 PDFDokumen13 halaman307-Article Text-578-1-10-20210309 PDFPUTRI LISTIANIBelum ada peringkat
- Corticosteroids 24613Dokumen33 halamanCorticosteroids 24613NOorulain HyderBelum ada peringkat
- Lecture 3 PsychopharmacologyDokumen99 halamanLecture 3 PsychopharmacologyPavan chowdaryBelum ada peringkat
- FC Continuous Education Microcredentials July 2021 (3354)Dokumen9 halamanFC Continuous Education Microcredentials July 2021 (3354)Luis Peralta GuzmanBelum ada peringkat
- Activity Journal Mobile Blood Donation Advocacy 1Dokumen3 halamanActivity Journal Mobile Blood Donation Advocacy 1Cherrymae BenzonBelum ada peringkat
- Ethnomedicine and Drug Discovery PDFDokumen2 halamanEthnomedicine and Drug Discovery PDFJohn0% (1)
- Inion Freedom Brochure v2 12-2014Dokumen11 halamanInion Freedom Brochure v2 12-2014Ivo van de KampBelum ada peringkat
- Basic Medical Sign LanguageDokumen8 halamanBasic Medical Sign LanguageRohan Kurade100% (1)