Adrenal Crisis
Diunggah oleh
sayednourDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Adrenal Crisis
Diunggah oleh
sayednourHak Cipta:
Format Tersedia
Miss D, 36 year old female was admitted with a sudden collapse following a viral flu.
She had complained of weakness and lethargy over the last few days.
Immediately before collapsing she had complained of severe abdominal pain and had a bout of vomiting. On admission her blood pressure was 60/40mmHg, and the pulse was weak and rapid. CBS was 56mg/dl.
On further questioning it was revealed that the patient had been taking 8 tablets of prednisolone daily without a prescription for joint pains. Recently, she had decided to go off the drugs as she was feeling well. The attending doctor requested an urgent serum electrolyte report.
What do you expect to find in the serum electrolyte report?
Moderate hyperkalaemia, normal or decreased sodium
What is your most likely diagnosis?
Adrenal insufficiency resulting in Addisonian crisis
What are the other possible differential diagnoses?
Anorexia nervosa Acute abdomen Pregnancy related complications
What are your priorities on clinical suspicion of the disease?
It should be treated promptly without waiting for laboratory confirmation. Still, blood can be taken for essential investigations prior to treatment.
What are the problems this patient might have?
Hypoglycaemia Electrolyte imbalance Circulatory collapse Ongoing infection
How will you treat the patient?
Establish IV access with two wide bore cannulae Take blood at time of insertion of cannulae for FBC, BU/SE, blood culture, RBS Take 10ml of blood in a heparinized tube for later analysis of cortisol levels Order urine full report, urine culture, inward CXR and an ECG as other investigations Correct hypoglycaemia with 50% dextrose 50 ml IV and repeat if necessary
Correct fluid deficit by
o Correcting deficit
o Replacing ongoing losses
o Providing maintenance requirement until the patient takes orally
As the blood pressure is below 90mmHg in this patient, she needs one unit of colloids infused fast.
If the blood pressure is still low, 20ml/kg boluses can be given until it picks up.
If facilities are available, fluid replacement is best guided by insertion of a CVP line. When blood pressure is above 90 mmHg further fluids can be given at a rate of 500 ml every 4 to 6 hours judged by the clinical
When blood pressure is above 90 mmHg further fluids can be given at a rate of 500 ml every 4 to 6 hours judged by the clinical signs of overload or deficit. Replace ongoing losses: Ongoing losses as vomiting and diarrhea has to be replaced with normal saline or as oral fluids if the patient is taking orally Maintenance fluid requirement: Maintenance requirement also needs to be supplemented intravenously if the patient is not taking orally.
Replacement of corticosteroids: Hydrocortisone IV is the drug of choice as it has both glucocorticoid and mineralocorticoid activities. It should be given as IV hydrocortisone 100mg stat and as an infusion of 100mg, 8 hourly for 24 48 hours. Then convert to 50mg 8 hourly for 48 hours and later 30mg total dose PO per day. (20mg mane and 10mg vesper). Fludrocortisone can be added 50300 g PO daily
Assess need for antibiotics. The patient may have infection.
Look for features of infection, and start appropriate antibiotics, usually broad spectrum IV antibiotics until culture results are available.
What are the possible causes for adrenal insufficiency in this patient?
The most apparent cause is sudden withdrawal of steroid therapy Other causes to consider are, Autoimmune (polyglandular autoimmune diseases, antibodies against adrenal cortex) Neoplastic conditions (primary, metastatic) Infective conditions (tuberculosis, meningococcal sepsis) Metabolic disorders (amyloidosis) Vascular events (infarction, haemorrhage)
How will you localize the problem in the hypothalamo-pituitaryadrenal axis?
The defect can either be in the adrenal gland (primary) or in pituitary gland (secondary). First establish adrenal insufficiency by doing a morning cortisol level at 9.00 a.m. Values less than 3g/dl confirm the diagnosis while values above 19ug/dl exclude the diagnosis. If it is inconclusive, three tests are used to confirm adrenal insufficiency;
A) Short synacthen test (measuring serum cortisol after synthetic corticotrophin dose, serum cortisol is measured after 30 and 60 minutes and values below 13ug/dl are diagnostic of adrenal insufficiency) B) Metyrapone test (read) C) Insulin tolerance test (read)
Once adrenal insufficiency is established further tests are needed to find the site of malfunction in hypothalamo-- pituitary adrenal axis. A) A serum ACTH level > 100 pg/ml is diagnostic of primary adrenal insufficiencyB) Long synacthen test to confirm primary adrenal insufficiency in inconclusive situations C) CRH test to diagnose secondary (pituitary) from tertiary (hypothalamic) adrenal insufficiency D) CT / MRI, tissue culture and histological diagnosis would be useful in finding an aetiology for adrenal insufficiency.
What advice would you give this patient on discharge?
Explain regarding the aetiology of the condition Advice regarding the importance of not stopping steroids suddenly. Give a time plan on tailing off of steroids No dietary restrictions, increase salt intake No activity restrictions Avoid unnecessary medication
Adrenal crisis
Anda mungkin juga menyukai
- Thyroid DrugsDokumen6 halamanThyroid DrugsThe Real UploaderBelum ada peringkat
- Endocrine DisordersDokumen5 halamanEndocrine DisordersBilly Ray VillanuevaBelum ada peringkat
- Endocrine System Study GuideDokumen5 halamanEndocrine System Study GuideClaudia SanchezBelum ada peringkat
- Lifestyle DiseasesDokumen44 halamanLifestyle Diseaseskyro draxBelum ada peringkat
- Physiological Regulation of Arterial Blood PressureDokumen36 halamanPhysiological Regulation of Arterial Blood PressureFrancesBelum ada peringkat
- An Overview Of: Acute Kidney Injury (Aki: Hasan BasriDokumen22 halamanAn Overview Of: Acute Kidney Injury (Aki: Hasan BasriDz PutraBelum ada peringkat
- 4 Hypovolemic ShockDokumen21 halaman4 Hypovolemic Shocksayednour100% (4)
- Hashimoto's Triggers-Advanced Reader Copy-V2Dokumen332 halamanHashimoto's Triggers-Advanced Reader Copy-V2Anonymous XiymFuQdF100% (2)
- Adrenal Insufficiency and Cushing's Disease-1Dokumen34 halamanAdrenal Insufficiency and Cushing's Disease-1Mwanja MosesBelum ada peringkat
- Adrenal Gland OSCEDokumen14 halamanAdrenal Gland OSCEOmar AttaBelum ada peringkat
- Adrenal DisordersDokumen22 halamanAdrenal DisordersRashed ShatnawiBelum ada peringkat
- Essential ThrombocytosisDokumen12 halamanEssential ThrombocytosisGd Padmawijaya100% (1)
- AlcoholDokumen20 halamanAlcoholrecklesspeshal2058100% (1)
- Thyroid Disease: Presentation By: Pimundu Vicent Audo Ritah Tutor: Dr. Fualal JaneDokumen41 halamanThyroid Disease: Presentation By: Pimundu Vicent Audo Ritah Tutor: Dr. Fualal JaneEsther AumaBelum ada peringkat
- Pharmacology of Alcohol Management of Chronic Alcoholism Treatment of Alcoholic Liver DiseasesDokumen41 halamanPharmacology of Alcohol Management of Chronic Alcoholism Treatment of Alcoholic Liver DiseasesVarsha Shende Khobragade100% (2)
- Liver Function Testing PDFDokumen2 halamanLiver Function Testing PDFRajesh KumarBelum ada peringkat
- Cough, Dyspnea and HemoptysisDokumen34 halamanCough, Dyspnea and HemoptysisPooja ShashidharanBelum ada peringkat
- Anticholinergic DrugsDokumen19 halamanAnticholinergic DrugseashshankarBelum ada peringkat
- Pathogenesis of Hashimoto's Thyroiditis (Chronic Autoimmune Thyroiditis) - UpToDateDokumen22 halamanPathogenesis of Hashimoto's Thyroiditis (Chronic Autoimmune Thyroiditis) - UpToDaterazvanBelum ada peringkat
- Cushing'S Syndrome: Roldan, Scorch Dominique Romero, John Reden Sanchez, Tracy JoyDokumen25 halamanCushing'S Syndrome: Roldan, Scorch Dominique Romero, John Reden Sanchez, Tracy JoyGerald John PazBelum ada peringkat
- 8B - Antianginal DrugsDokumen70 halaman8B - Antianginal Drugslalitrajindolia100% (1)
- Evaluation of Liver FunctionDokumen64 halamanEvaluation of Liver FunctionMustafa KhandgawiBelum ada peringkat
- 14 DyslipidemiaDokumen45 halaman14 DyslipidemiaSaniBelum ada peringkat
- PeripheralDokumen25 halamanPeripheralMans FansBelum ada peringkat
- Hormones and Related DrugsDokumen42 halamanHormones and Related DrugsRamya PrabhuBelum ada peringkat
- Congestive Heart FailureDokumen74 halamanCongestive Heart FailureNiharikaBelum ada peringkat
- Cushing DiseaseDokumen24 halamanCushing DiseaseSuci AlimaBelum ada peringkat
- Cvs PathoDokumen36 halamanCvs PathoISRAELBelum ada peringkat
- Alzheimer's Disease: Causes, Effects, and TreatmentsDokumen21 halamanAlzheimer's Disease: Causes, Effects, and TreatmentsJesshica Navarro AlejandrinoBelum ada peringkat
- Suprarenal (Adrenal) Gland: Dr. R. SanthakumarDokumen33 halamanSuprarenal (Adrenal) Gland: Dr. R. SanthakumardrsubanBelum ada peringkat
- Thyroiddisease 190216062020Dokumen42 halamanThyroiddisease 190216062020Manikandan Vp100% (1)
- Pituitary Gland: The Master GlandDokumen15 halamanPituitary Gland: The Master GlandMohammed ShahanewzBelum ada peringkat
- Assignment: Polycystic Ovary Syndrome (PCOS)Dokumen8 halamanAssignment: Polycystic Ovary Syndrome (PCOS)tehseenullahBelum ada peringkat
- Adverse Drug Reactions (ADRS)Dokumen24 halamanAdverse Drug Reactions (ADRS)ANAM IQBALBelum ada peringkat
- Liver Tests SlidesDokumen65 halamanLiver Tests SlidesDokter MuhammadBelum ada peringkat
- Circulation: Biology: Concepts & ConnectionsDokumen66 halamanCirculation: Biology: Concepts & ConnectionsGlen MangaliBelum ada peringkat
- An AntipsychoticDokumen4 halamanAn AntipsychoticJoMa TuazonBelum ada peringkat
- Endocrine Disorders 1234399857677955 1Dokumen130 halamanEndocrine Disorders 1234399857677955 1api-19824701Belum ada peringkat
- Paratiroid Dan KalsiumDokumen80 halamanParatiroid Dan KalsiumFebrina EvaBelum ada peringkat
- Bioassay of AcetylcholineDokumen1 halamanBioassay of AcetylcholineSangi RajBelum ada peringkat
- Hyporeninemic HypoaldosteronismDokumen12 halamanHyporeninemic HypoaldosteronismCésar Augusto Sánchez SolisBelum ada peringkat
- Hyperprolactine MIA: Prepared By: Daryl S. AbrahamDokumen15 halamanHyperprolactine MIA: Prepared By: Daryl S. AbrahamBiway RegalaBelum ada peringkat
- Pain Pathways IN HUMANSDokumen189 halamanPain Pathways IN HUMANSAshish VyasBelum ada peringkat
- 8.1b. Systole-Diastole & Cardiac CycleDokumen34 halaman8.1b. Systole-Diastole & Cardiac Cycleverysedatedx100% (1)
- Psychiatric Effects of ThyroidDokumen9 halamanPsychiatric Effects of ThyroidJosetta WhitneyBelum ada peringkat
- Clinical HYPERTENSION LecDokumen44 halamanClinical HYPERTENSION LecFarwaBelum ada peringkat
- Amine Autacoids: Histamine & 5-HydroxytryptamineDokumen25 halamanAmine Autacoids: Histamine & 5-HydroxytryptamineJames PerianayagamBelum ada peringkat
- Adrenal GlandDokumen15 halamanAdrenal GlandSivanandan Ramar100% (1)
- Liver DiseasesDokumen29 halamanLiver DiseasesRicaneth TaanBelum ada peringkat
- Secondary Arterial HypertensionDokumen32 halamanSecondary Arterial HypertensionAndi SusiloBelum ada peringkat
- For Best Viewing:: Open in Slide Show Mode Click On IconDokumen32 halamanFor Best Viewing:: Open in Slide Show Mode Click On IconSutapa PawarBelum ada peringkat
- Ischemic Heart DiseaseDokumen4 halamanIschemic Heart DiseaseBanana CakeBelum ada peringkat
- Secondary Amenorrhea Testing AlgorithmDokumen1 halamanSecondary Amenorrhea Testing AlgorithmpolygoneBelum ada peringkat
- HypertensionDokumen85 halamanHypertensionmelkamu AssefaBelum ada peringkat
- Causes of Stroke PDFDokumen16 halamanCauses of Stroke PDFEmmanuel AguilarBelum ada peringkat
- What Are We Talking About?: DR Jane ShooteDokumen46 halamanWhat Are We Talking About?: DR Jane ShooteAndikha100% (1)
- Head Injury 1Dokumen33 halamanHead Injury 1drvishal bhattBelum ada peringkat
- Anatomy of Thyroid GlandDokumen12 halamanAnatomy of Thyroid GlandBinbinbabu BinuBelum ada peringkat
- Pharmacotherapy of Arrythmias For 4th YearDokumen79 halamanPharmacotherapy of Arrythmias For 4th Yeartolcharegasa100% (1)
- ShockDokumen21 halamanShockMin-Joo Esther ParkBelum ada peringkat
- Hyper-coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHyper-coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionDari EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionBelum ada peringkat
- Fluid Electrolytes and Acid Base BalanceDokumen108 halamanFluid Electrolytes and Acid Base BalancesayednourBelum ada peringkat
- General Anesthesia For Cesarean SectionDokumen33 halamanGeneral Anesthesia For Cesarean Sectionsayednour100% (2)
- Assessment of Suitability For Lung Resection: Gerard Gould FRCA Adrian Pearce FRCADokumen4 halamanAssessment of Suitability For Lung Resection: Gerard Gould FRCA Adrian Pearce FRCAsayednourBelum ada peringkat
- Basics of Laser Orthopedic ViewDokumen24 halamanBasics of Laser Orthopedic ViewsayednourBelum ada peringkat
- AnestheticsDokumen34 halamanAnestheticssayednourBelum ada peringkat
- Anesthesia in The FutureDokumen11 halamanAnesthesia in The FuturesayednourBelum ada peringkat
- An Overview of Therapeutic Plasma ExchangeDokumen65 halamanAn Overview of Therapeutic Plasma ExchangesayednourBelum ada peringkat
- Developmental Genetics and Pharmacogeneticsdoc4301Dokumen8 halamanDevelopmental Genetics and Pharmacogeneticsdoc4301sayednourBelum ada peringkat
- Plasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?Dokumen4 halamanPlasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?sayednourBelum ada peringkat
- 1 Plasmapheresis - 1Dokumen61 halaman1 Plasmapheresis - 1sayednour100% (1)
- 166 Serotonin SyndromeDokumen5 halaman166 Serotonin SyndromesayednourBelum ada peringkat
- Nitric Oxide An Overview: Salwa Hassan Teama M.D. NCI. Cairo UniversityDokumen31 halamanNitric Oxide An Overview: Salwa Hassan Teama M.D. NCI. Cairo Universitysayednour100% (1)
- Review Mechanisms of Glucocorticoid-Induced Myopathy: O Schakman, H Gilson and J P ThissenDokumen10 halamanReview Mechanisms of Glucocorticoid-Induced Myopathy: O Schakman, H Gilson and J P ThissensayednourBelum ada peringkat
- Cohort StudyDokumen31 halamanCohort Studysayednour50% (2)
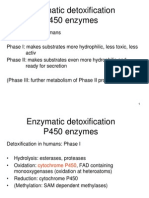
- Enzymatic Detoxification P450 EnzymesDokumen22 halamanEnzymatic Detoxification P450 EnzymessayednourBelum ada peringkat
- Tony Chang, MD Tuesday Conference September 6, 2005Dokumen75 halamanTony Chang, MD Tuesday Conference September 6, 2005sayednourBelum ada peringkat
- 185 Anaesthesia in Pregnancy For Non Obstetric SurgeryDokumen9 halaman185 Anaesthesia in Pregnancy For Non Obstetric SurgeryaangrohmananiaBelum ada peringkat
- 8 Plasma Derivatives ProductsDokumen12 halaman8 Plasma Derivatives ProductssayednourBelum ada peringkat
- Diabetes Book HindiDokumen18 halamanDiabetes Book HindiAdityaBelum ada peringkat
- Opioid-Induced Androgen Deficiency in Males (OPIAD Syndrome) : Medicinski Casopis January 2015Dokumen7 halamanOpioid-Induced Androgen Deficiency in Males (OPIAD Syndrome) : Medicinski Casopis January 2015Lilamala LilavelikaBelum ada peringkat
- Cortisol, Fixing ImbalancesDokumen21 halamanCortisol, Fixing ImbalancesTheresa Dale100% (2)
- Polycystic Ovarian Syndrome: Anna Lissa J. Bernadas, M.D., F.P.O.G.SDokumen39 halamanPolycystic Ovarian Syndrome: Anna Lissa J. Bernadas, M.D., F.P.O.G.SJerahmeel Sombilon GenillaBelum ada peringkat
- Relationship Between Levels of Fasting Blood Glucose and Hba1C in Prediabetes PatientsDokumen4 halamanRelationship Between Levels of Fasting Blood Glucose and Hba1C in Prediabetes Patientsمحمد رحيم حسن محمودBelum ada peringkat
- Hiperandrogenismo ArtigoDokumen11 halamanHiperandrogenismo ArtigoFernando RibeiroBelum ada peringkat
- Aromatase Inhibitors For Breast Cancer I PDFDokumen11 halamanAromatase Inhibitors For Breast Cancer I PDFGaro ArslanianBelum ada peringkat
- CH 27 CaseStudy With WorksheetDokumen3 halamanCH 27 CaseStudy With WorksheetBelinda LapsitBelum ada peringkat
- 2013 ENDOCRINE PHARMACOLOGY Word Notes PDFDokumen52 halaman2013 ENDOCRINE PHARMACOLOGY Word Notes PDFNicole Opao100% (4)
- D V Bhaskar - 2019 - 12 - 18Dokumen5 halamanD V Bhaskar - 2019 - 12 - 18asdfBelum ada peringkat
- BoltonDokumen1 halamanBoltonapi-384478473Belum ada peringkat
- DSL - Thyroid Function TestDokumen7 halamanDSL - Thyroid Function TestUmar AzlanBelum ada peringkat
- Veterinary Physiology BiochemistryDokumen22 halamanVeterinary Physiology BiochemistryHnin ThazinBelum ada peringkat
- Basaria 2005 DDDokumen9 halamanBasaria 2005 DDCosmin GabrielBelum ada peringkat
- HipertiroidDokumen37 halamanHipertiroidTaysqy swftBelum ada peringkat
- 46 - Abdullah Al Sabahi - Thyroid Disease - Subacute Thyroiditis PosterDokumen1 halaman46 - Abdullah Al Sabahi - Thyroid Disease - Subacute Thyroiditis Postermohammed makkiBelum ada peringkat
- Results Endocrinology Test.Dokumen9 halamanResults Endocrinology Test.jaikishan marathe 69Belum ada peringkat
- HypothalamusDokumen5 halamanHypothalamusBoneGrissleBelum ada peringkat
- Pharmacology II - Exam 3 Review (Katzung) Flashcards - QuizletDokumen16 halamanPharmacology II - Exam 3 Review (Katzung) Flashcards - Quizletyeshuavelando13Belum ada peringkat
- Endocrine System: MSN 4006 Advanced PsychopathophysiologyDokumen15 halamanEndocrine System: MSN 4006 Advanced Psychopathophysiologybane1925Belum ada peringkat
- Case Study Cushing Syndrome 1Dokumen5 halamanCase Study Cushing Syndrome 1Selena Marie100% (1)
- TSH LiaisonDokumen6 halamanTSH Liaisonsorayafathi90Belum ada peringkat
- DetailedapproaDokumen65 halamanDetailedapproaMuhammed BarznjiBelum ada peringkat
- Data Diabetes Kota MakassarDokumen7 halamanData Diabetes Kota MakassarKabul BudionoBelum ada peringkat
- Hormone NotesDokumen2 halamanHormone Notesapi-188978784100% (1)
- Endocrin E Diseases: by Group 3Dokumen53 halamanEndocrin E Diseases: by Group 3Ash AshBelum ada peringkat
- Science 10 - PPTX (3rd Quarter)Dokumen54 halamanScience 10 - PPTX (3rd Quarter)Gian BaliloBelum ada peringkat
- Phase 2a Endocrinology - Sba Saq Session 2Dokumen54 halamanPhase 2a Endocrinology - Sba Saq Session 2Zeyad AmrBelum ada peringkat
- IAL Biology SB2 Assessment 7CDokumen4 halamanIAL Biology SB2 Assessment 7CsalmaBelum ada peringkat