CPR Lecture
Diunggah oleh
jacnpoyJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CPR Lecture
Diunggah oleh
jacnpoyHak Cipta:
Format Tersedia
Continued Emphasis on High-Quality CPR The 2010 AHA Guidelines for CPR and ECC once again emphasize
e the need for high-quality CPR, including A compression rate of at least 100/min (a change from approximately 100/min) A compression depth of at least 2 inches (5 cm) in adults and a compression depth of at least one third of the anteriorposterior diameter of the chest in infants and children (approximately 1.5 inches [4 cm] in infants and 2 inches [5 cm] in children). Note that the range of 1. to 2 inches is no longer used for adults, and the absolute depth specified for children and infants is deeper than in previous versions of the AHA Guidelines for CPR and ECC.
Allowing for complete chest recoil after each compression Minimizing interruptions in chest compressions Avoiding excessive ventilation There has been no change in the recommendation for a compression-to-ventilation ratio of 30:2 for single rescuers ofadults, children, and infants (excluding newly born infants). The2010 AHA Guidelines for CPR and ECC continue to recommend that rescue breaths be given in approximately 1 second. Once an advanced airway is in place, chest compressions can be continuous (at a rate of at least 100/min) and no longer cycled with ventilations. Rescue breaths can then be provided at about 1 breath every 6 to 8 seconds (about 8 to 10 breaths per minute). Excessive ventilation should be avoided.
A Change From A-B-C to C-A-B The 2010 AHA Guidelines for CPR and ECC recommend a change in the BLS sequence of steps from A-B-C (Airway, Breathing, Chest compressions) to C-A-B (Chest compressions, Airway, Breathing) for adults, children, and infants (excluding the newly born; see Neonatal Resuscitation section). This fundamental change in CPR sequence will require reeducation of everyone who has ever learned CPR, but the consensus of the authors and experts involved in the creation of the 2010 AHA Guidelines for CPR and ECC is that the benefit will justify the effort.
Emphasis on Chest Compressions* 2010 (New): If a bystander is not trained in CPR, the bystander should provide Hands-Only (compression-only) CPR for the adult victim who suddenly collapses, with an emphasis to push hard and fast on the center of the chest, or follow the directions of the EMS dispatcher. The rescuer should continue Hands-Only CPR until an AED arrives and is ready for use or EMS providers or other responders take over care of the victim. All trained lay rescuers should, at a minimum, provide chest compressions for victims of cardiac arrest. In addition, if the trained lay rescuer is able to perform rescue breaths, compressions and breaths should be provided in a ratio of 30 compressions to 2 breaths. The rescuer should continue CPR until an AED arrives and is ready for use or EMS providers take over care of the victim. 2005 (Old): The 2005 AHA Guidelines for CPR and ECC did not provide different recommendations for trained versus untrained rescuers but did recommend that dispatchers provide compression-only CPR instructions to untrained bystanders. The 2005 AHA Guidelines for CPR and ECC did note that if the rescuer was unwilling or unable to provide ventilations, the rescuer should provide chest compressions only.
Change in CPR Sequence: C-A-B Rather Than A-B-C* 2010 (New): Initiate chest compressions before ventilations. 2005 (Old): The sequence of adult CPR began with opening of the airway, checking for normal breathing, and then delivery of 2 rescue breaths followed by cycles of 30 chest compressions and 2 breaths. Why: Although no published human or animal evidence demonstrates that starting CPR with 30 compressions rather than 2 ventilations leads to improved outcome, chest compressions provide vital blood flow to the heart and brain, and studies of out-of-hospital adult cardiac arrest showed that survival was higher when bystanders made some attempt rather than no attempt to provide CPR. Animal data demonstrated that delays or interruptions in chest compressions reduced survival, so such delays or interruptions should be minimized throughout the entire resuscitation. Chest compressions can be started almost immediately, whereas positioning the head and achieving a seal for mouth-to-mouth or bag-mask rescue breathing all take time. The delay in initiation of compressions can be reduced if 2 rescuers are present: the first rescuer begins chest compressions, and the second rescuer opens the airway and is prepared to deliver breaths as soon as the first rescuer has completed the first set of 30 chest compressions. Whether 1 or more rescuers are present, initiation of CPR with chest compressions ensures that the victim receives this critical intervention early, and any delay in rescue breaths should be brief.
Elimination of Look, Listen, and Feel for Breathing* 2010 (New): Look, listen, and feel was removed from the CPR sequence. After delivery of 30 compressions, the lone rescuer opens the victims airway and delivers 2 breaths. 2005 (Old): Look, listen, and feel was used to assess breathing after the airway was opened. Why: With the new chest compressions first sequence, CPR is performed if the adult is unresponsive and not breathing or not breathing normally (as noted above, lay rescuers will be taught to provide CPR if the unresponsive victim is not breathing or only gasping). The CPR sequence begins with compressions (C-A-B sequence). Therefore, breathing is briefly checked as part of a check for cardiac arrest; after the first set of chest compressions, the airway is opened, and the rescuer delivers 2 breaths.
Chest Compression Rate: At Least 100 per Minute* 2010 (New): It is reasonable for lay rescuers and healthcare providers to perform chest compressions at a rate of at least 100/min. 2005 (Old): Compress at a rate of about 100/min. Why: The number of chest compressions delivered per minute during CPR is an important determinant of return of spontaneous circulation (ROSC) and survival with good neurologic function. The actual number of chest compressions delivered per minute is determined by the rate of chest compressions and the number and duration of interruptions in compressions (eg, to open the airway, deliver rescue breaths, or allow AED analysis). In most studies, more compressions are associated with higher survival rates, and fewer compressions are associated with lower survival rates. Provision of adequate chest compressions requires an emphasis not only on an adequate compression rate but also on minimizing interruptions to this critical component of CPR. An inadequate compression rate or frequent interruptions (or both) will reduce the total number of compressions delivered per minute. For further information, see Box 2.
Chest Compression Depth* 2010 (New): The adult sternum should be depressed at least 2 inches (5 cm). 2005 (Old): The adult sternum should be depressed approximately 1. to 2 inches (approximately 4 to 5 cm). Why: Compressions create blood flow primarily by increasing intrathoracic pressure and directly compressing the heart. Compressions generate critical blood flow and oxygen and energy delivery to the heart and brain. Confusion may result when a range of depth is recommended, so 1 compression Number of Compressions Delivered Affected by Compression Rate and by Interruptions The total number of compressions delivered during resuscitation is an important determinant of survival from cardiac arrest. The number of compressions delivered is affected by the compression rate and by the compression fraction (the portion of total CPR time during which compressions are performed); increases in compression rate and fraction increase the total compressions delivered, whereas decreases in compression rate or compression fraction decrease the total compressions delivered. Compression fraction is improved if you reduce the number and length of any interruptions in compressions, and it is reduced by frequent or long interruptions in chest compressions. An analogy can be found in automobile travel. When you travel in an automobile, the number of miles you travel in a day is affected not only by the speed that you drive (your rate of travel) but also by the number and duration of any stops you make (interruptions in travel). During CPR, you want to deliver effective compressions at an appropriate rate (at least 100/min) and depth, while minimizing the number and duration of interruptions in chest compressions. Additional components of high-quality CPR include allowing complete chest recoil after each compression and avoiding excessive ventilation. BOX 2 5 depth is now recommended. Rescuers often do not compress the chest enough despite recommendations to push hard. In addition, the available science suggests that compressions of at least 2 inches are more effective than compressions of 1. inches. For this reason the 2010 AHA Guidelines for CPR and ECC recommend a single minimum depth for compression of the adult chest.
Anda mungkin juga menyukai
- 100 Item Exam On Fundamentals of NursingDokumen58 halaman100 Item Exam On Fundamentals of Nursingjacnpoy96% (54)
- CPR LectureDokumen10 halamanCPR LecturejacnpoyBelum ada peringkat
- IMELS New Approach in Basic Life SupportDokumen28 halamanIMELS New Approach in Basic Life SupportAstri Arri FebriantiBelum ada peringkat
- Basic Life SupportDokumen35 halamanBasic Life SupportCitra Kartikasari100% (1)
- Basic Life Support (BLS) Provider HandbookDari EverandBasic Life Support (BLS) Provider HandbookPenilaian: 5 dari 5 bintang5/5 (2)
- Pediatric Advanced Life Support (PALS) Provider HandbookDari EverandPediatric Advanced Life Support (PALS) Provider HandbookBelum ada peringkat
- JohnsonDokumen20 halamanJohnsonjacnpoyBelum ada peringkat
- Assessment of Head and NeckDokumen11 halamanAssessment of Head and Neckjacnpoy100% (2)
- Group 4 Lydia Hall CritiqueDokumen4 halamanGroup 4 Lydia Hall CritiqueMarielle Ann RumbaoaBelum ada peringkat
- Basic Life Support Perubahan Guideline AHA 2005-2010Dokumen22 halamanBasic Life Support Perubahan Guideline AHA 2005-2010Momoh AlkaffBelum ada peringkat
- CPR PFTDokumen19 halamanCPR PFTmusiyamahBelum ada peringkat
- The Main Changes in The Resuscitation GuidelinesDokumen79 halamanThe Main Changes in The Resuscitation GuidelinesFikri AlfarisyiBelum ada peringkat
- 2010 Guidelines For CPR Winner MalangDokumen55 halaman2010 Guidelines For CPR Winner MalangDARA INDAH PRATIWIBelum ada peringkat
- CPR & Electrical TherapiesDokumen67 halamanCPR & Electrical TherapiesRizaldy Yoga67% (3)
- Basic Life SupportDokumen15 halamanBasic Life SupportMizzy Wat EvaBelum ada peringkat
- Departement of Internal Medicine Faculty of Medicine Muhammadiyah University YogyakartaDokumen59 halamanDepartement of Internal Medicine Faculty of Medicine Muhammadiyah University YogyakartaMohammad ArifiantoBelum ada peringkat
- BLS Study Guide PDFDokumen12 halamanBLS Study Guide PDFPingChavez100% (1)
- Basic Cardiac Life Support 2011Dokumen6 halamanBasic Cardiac Life Support 2011Tashfeen Bin NazeerBelum ada peringkat
- Bls Update: (The Following Was Taken From AHA Currents Magazine)Dokumen7 halamanBls Update: (The Following Was Taken From AHA Currents Magazine)Allan DangloseBelum ada peringkat
- Cardiopulmonary Resuscitation (CPR)Dokumen21 halamanCardiopulmonary Resuscitation (CPR)Cristy Guzman100% (1)
- Cardio Pulmonary Resuscitation 2010: Djayanti SariDokumen26 halamanCardio Pulmonary Resuscitation 2010: Djayanti SariAlessandro AlfieriBelum ada peringkat
- Cardio Pulmonary R Ry Resuscitation 2010Dokumen26 halamanCardio Pulmonary R Ry Resuscitation 2010Fatahillah NazarBelum ada peringkat
- Mona Adel, MD, Macc A.Professor of Cardiology Cardiology Consultant Elite Medical CenterDokumen34 halamanMona Adel, MD, Macc A.Professor of Cardiology Cardiology Consultant Elite Medical CenterOnon EssayedBelum ada peringkat
- Basic Life SupportDokumen4 halamanBasic Life Supportraven_claw25Belum ada peringkat
- The Rules and Changes: ACLS Guidelines 2010Dokumen81 halamanThe Rules and Changes: ACLS Guidelines 2010Annisa Rizki Ratih PratiwiBelum ada peringkat
- BLS For Healthcare Providers Student ManualDokumen2 halamanBLS For Healthcare Providers Student ManualdrsmiBelum ada peringkat
- Cardio Pulm ResuscitationDokumen7 halamanCardio Pulm Resuscitationdaniphilip777Belum ada peringkat
- Part 5: Adult Basic Life SupportDokumen15 halamanPart 5: Adult Basic Life SupportSurya ArhBelum ada peringkat
- Practice: Adult and Paediatric Basic Life Support: An Update For The Dental TeamDokumen4 halamanPractice: Adult and Paediatric Basic Life Support: An Update For The Dental TeamsmilekkmBelum ada peringkat
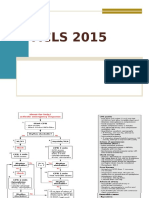
- Acls 2015Dokumen13 halamanAcls 2015I Gede Aditya100% (5)
- UP DA TE CP R 20 15: Prof. Dr. Achsanuddin Hanafie, SP - An, KIC, KAO Dept. Anestesiologi Dan Terapi Intensif FK-USUDokumen37 halamanUP DA TE CP R 20 15: Prof. Dr. Achsanuddin Hanafie, SP - An, KIC, KAO Dept. Anestesiologi Dan Terapi Intensif FK-USUAndrias OzBelum ada peringkat
- AHA Guidelines For CPR and ECC Comparison Chart of Key Changes (2010)Dokumen8 halamanAHA Guidelines For CPR and ECC Comparison Chart of Key Changes (2010)PhilippineNursingDirectory.comBelum ada peringkat
- Bls 2015 GuidelinesDokumen51 halamanBls 2015 GuidelinesifyBelum ada peringkat
- Cardio-Pulmonary Resuscitation (CPR)Dokumen18 halamanCardio-Pulmonary Resuscitation (CPR)Savita HanamsagarBelum ada peringkat
- AHA Defibrilation: Ventricular FibrilationDokumen4 halamanAHA Defibrilation: Ventricular FibrilationStacia StefaniBelum ada peringkat
- IntroductionDokumen4 halamanIntroductiondyah ayuBelum ada peringkat
- Basic Life SupportDokumen10 halamanBasic Life SupportAlvin M AlcaynoBelum ada peringkat
- Bab Ii Tinjauan TeoriDokumen11 halamanBab Ii Tinjauan TeoriLiana DaniellaBelum ada peringkat
- UntitledDokumen11 halamanUntitledAnkita BramheBelum ada peringkat
- BLS AlgorithmDokumen9 halamanBLS AlgorithmDr VJ GeorgeBelum ada peringkat
- Cardiopulmonary Resuscitation 2015Dokumen31 halamanCardiopulmonary Resuscitation 2015Clarissa Maya TjahjosarwonoBelum ada peringkat
- Basic Life SupportDokumen6 halamanBasic Life SupportRyan Mathew ScottBelum ada peringkat
- Civic Welfare Training ServiceDokumen13 halamanCivic Welfare Training ServiceVanessa Rose RofloBelum ada peringkat
- Cardiopulmonary Resuscitation: ReferenceDokumen42 halamanCardiopulmonary Resuscitation: ReferenceKristine Castillo100% (1)
- Basic Life Support: BY Himanshu Rathore M.Sc. Nursing 1 YearDokumen30 halamanBasic Life Support: BY Himanshu Rathore M.Sc. Nursing 1 YearHimanshu RathoreBelum ada peringkat
- ACLSDokumen61 halamanACLSmgthida935100% (1)
- Basic Life Support: Submitted By: Kennedy V. Velasco Bscrim 1-AlphaDokumen7 halamanBasic Life Support: Submitted By: Kennedy V. Velasco Bscrim 1-AlphaProsperJuan BelieversBelum ada peringkat
- Basic Life Support (BLS) : Prepared by DR Melaku M (ECCM R-1) Moderator:dr Yonas (Assistant Professor of ECCM)Dokumen42 halamanBasic Life Support (BLS) : Prepared by DR Melaku M (ECCM R-1) Moderator:dr Yonas (Assistant Professor of ECCM)Balemlay HailuBelum ada peringkat
- CPR - Cardiopulmonary ResuscitationDokumen31 halamanCPR - Cardiopulmonary ResuscitationPanji HerlambangBelum ada peringkat
- Sir BrandonDokumen14 halamanSir Brandonjoshuagadingan6Belum ada peringkat
- CPR Guidelines. W. WieczorekDokumen61 halamanCPR Guidelines. W. WieczorekMarga KouryBelum ada peringkat
- From MedscapeCME Clinical BriefsDokumen4 halamanFrom MedscapeCME Clinical Briefssraji64Belum ada peringkat
- Cardiopulmonary ResuscitationDokumen3 halamanCardiopulmonary ResuscitationLee Liang Lee LiangBelum ada peringkat
- What Is BLS?: Respiratory ArrestDokumen2 halamanWhat Is BLS?: Respiratory ArrestStephanie Joy EscalaBelum ada peringkat
- Anzcor Guideline 13 6 Apr 2021Dokumen6 halamanAnzcor Guideline 13 6 Apr 2021Essam HassanBelum ada peringkat
- ACLSDokumen39 halamanACLSJason LiandoBelum ada peringkat
- CPR & ECC: 2015 Aha Guideline FORDokumen36 halamanCPR & ECC: 2015 Aha Guideline FORRush32Belum ada peringkat
- AHA CPR Guidelines 2010Dokumen2 halamanAHA CPR Guidelines 2010Alvin Roel NiervaBelum ada peringkat
- Cardio Pulmonary Resuscitation 2010Dokumen26 halamanCardio Pulmonary Resuscitation 2010Raa RiulBelum ada peringkat
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesDari EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesPenilaian: 4 dari 5 bintang4/5 (6)
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesDari EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesPenilaian: 5 dari 5 bintang5/5 (2)
- Healthcare Provider Basic Life Support CPR Quick Study Guide 2015 Updated GuidelinesDari EverandHealthcare Provider Basic Life Support CPR Quick Study Guide 2015 Updated GuidelinesBelum ada peringkat
- Bootle Top JyuwanDokumen1 halamanBootle Top JyuwanjacnpoyBelum ada peringkat
- Cardiopulmonary Resuscitation 2013Dokumen6 halamanCardiopulmonary Resuscitation 2013Amiel Francisco ReyesBelum ada peringkat
- Bottle TopDokumen1 halamanBottle TopjacnpoyBelum ada peringkat
- Assessment of The Musclo-Skletal SystemDokumen25 halamanAssessment of The Musclo-Skletal SystemjacnpoyBelum ada peringkat
- TFN SemiDokumen47 halamanTFN SemijacnpoyBelum ada peringkat
- Aggravating Circumstances-PrintDokumen2 halamanAggravating Circumstances-PrintjacnpoyBelum ada peringkat
- EmergenciesDokumen38 halamanEmergenciesjacnpoyBelum ada peringkat
- TracheostomyDokumen36 halamanTracheostomyjacnpoyBelum ada peringkat
- CPR Lecture FinalDokumen45 halamanCPR Lecture FinaljacnpoyBelum ada peringkat
- Dorothy JonhsonDokumen19 halamanDorothy JonhsonjacnpoyBelum ada peringkat
- Ana-Map For NICEDokumen1 halamanAna-Map For NICEjacnpoyBelum ada peringkat
- TracheostomyDokumen36 halamanTracheostomyjacnpoyBelum ada peringkat
- Oncologic Disorders of The BrainDokumen12 halamanOncologic Disorders of The BrainjacnpoyBelum ada peringkat
- Abuse and Violence: Abuse Is The Wrongful Use and Maltreatment of Another PersonDokumen10 halamanAbuse and Violence: Abuse Is The Wrongful Use and Maltreatment of Another PersonjacnpoyBelum ada peringkat
- Ana-Map For NICEDokumen1 halamanAna-Map For NICEjacnpoyBelum ada peringkat
- Dying and DeathDokumen21 halamanDying and DeathjacnpoyBelum ada peringkat
- Geriatrics Addition To Health HistoryDokumen2 halamanGeriatrics Addition To Health HistoryjacnpoyBelum ada peringkat
- Family TasksDokumen2 halamanFamily Tasksjacnpoy100% (3)
- Overview of Nephrotic SyndromeDokumen19 halamanOverview of Nephrotic Syndromefarmasi_hm100% (1)
- Effects of Cuscuta Chinensis Lam. Versus Fluoxetine For Treatment of Major Depression: A Double-Blind, Randomized Controlled TrialDokumen10 halamanEffects of Cuscuta Chinensis Lam. Versus Fluoxetine For Treatment of Major Depression: A Double-Blind, Randomized Controlled TrialBaru Chandrasekhar RaoBelum ada peringkat
- Lbbbi18 Long Exam 1Dokumen71 halamanLbbbi18 Long Exam 1namkimseoBelum ada peringkat
- 2017 Journal Citation Reports by Thomson Reuters: July 2017Dokumen251 halaman2017 Journal Citation Reports by Thomson Reuters: July 2017vlad lupasteanuBelum ada peringkat
- Effects of Vernonia Amygdalina (Bitter Leaf) On The Bio-Marker of Oxidative Stress in Accetaminophen Induced Liver Damage of Albino RatsDokumen12 halamanEffects of Vernonia Amygdalina (Bitter Leaf) On The Bio-Marker of Oxidative Stress in Accetaminophen Induced Liver Damage of Albino Ratsiaset123Belum ada peringkat
- Acute Limb Ischemia SiteDokumen23 halamanAcute Limb Ischemia Sitedokteraan100% (2)
- Chromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Dokumen5 halamanChromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Jun JoniBelum ada peringkat
- Physical Fitness Test Body Composition/Cardiovascular Tests: Lesson 2 For 1 Hour Day 2 Week 2 Quarter 1Dokumen36 halamanPhysical Fitness Test Body Composition/Cardiovascular Tests: Lesson 2 For 1 Hour Day 2 Week 2 Quarter 1Elmar MariñasBelum ada peringkat
- My Trip To The Hospital - A Coloring BookDokumen0 halamanMy Trip To The Hospital - A Coloring Bookili_thBelum ada peringkat
- Hyper Calc Emi ADokumen31 halamanHyper Calc Emi AFatima SajidBelum ada peringkat
- Advanced Life Support (Training Manual)Dokumen74 halamanAdvanced Life Support (Training Manual)Matt100% (25)
- SimMan 3G BrochureDokumen8 halamanSimMan 3G BrochureDemuel Dee L. BertoBelum ada peringkat
- Arabic Clerking Etc-3Dokumen26 halamanArabic Clerking Etc-3walefamousBelum ada peringkat
- Part 2 Lecture 2Dokumen53 halamanPart 2 Lecture 2Shella SilvestreBelum ada peringkat
- Small PDFDokumen589 halamanSmall PDFskilmagBelum ada peringkat
- Monthly Wellness Tip Heat StressDokumen1 halamanMonthly Wellness Tip Heat StressbharathaninBelum ada peringkat
- Nursing Care Plan - Constipation (Antepartum)Dokumen2 halamanNursing Care Plan - Constipation (Antepartum)kaimimiyaBelum ada peringkat
- Exercise No. 26 The Blood GroupsDokumen8 halamanExercise No. 26 The Blood GroupsPATRICIA ROSE SORIANOBelum ada peringkat
- Uterine CancerDokumen20 halamanUterine Cancerzyrine jhen100% (4)
- Antimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaDokumen9 halamanAntimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaBima RizkiBelum ada peringkat
- RL2 CCR Book March-2021-P117-118Dokumen2 halamanRL2 CCR Book March-2021-P117-118Judah ObengBelum ada peringkat
- Booklet Bcu Revisi 5Dokumen8 halamanBooklet Bcu Revisi 5irza nasutionBelum ada peringkat
- Cardiac Changes Associated With Vascular Aging: Narayana Sarma V. Singam - Christopher Fine - Jerome L. FlegDokumen7 halamanCardiac Changes Associated With Vascular Aging: Narayana Sarma V. Singam - Christopher Fine - Jerome L. Flegabraham rumayaraBelum ada peringkat
- Pulmonary Rehabilitation - UpToDateDokumen37 halamanPulmonary Rehabilitation - UpToDateAlejandro CadarsoBelum ada peringkat
- Miron Zhang i-PRF Drug DeliveryDokumen17 halamanMiron Zhang i-PRF Drug Deliverygary manningBelum ada peringkat
- Description:: Dance Therapy "In The Mood of Dancing"Dokumen2 halamanDescription:: Dance Therapy "In The Mood of Dancing"kristine_silangBelum ada peringkat
- ParkinsonDokumen12 halamanParkinsonStephanie NieBelum ada peringkat
- Above Knee AmputationDokumen8 halamanAbove Knee AmputationAbdul Ghafoor SajjadBelum ada peringkat
- Vibrio CholeraeDokumen20 halamanVibrio CholeraeChockalingam MeenakshisundaramBelum ada peringkat