Arrhythmia Overview: Antonia Anna Lukito
Diunggah oleh
Joshua Obrien0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
48 tayangan45 halamanHeart rhythm disorders (arrhythmias) affect the electrical system, or "wiring," of the heart muscle. Bradycardia describes a heartbeat that is too slow (less than 60 beats a minute) tachycardia (tachy=fast) is a too-rapid heartbeat. Ventricular fibrillation (VF) is the number one cause of sudden cardiac arrest.
Deskripsi Asli:
Judul Asli
Arrhythmia Overview
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPT, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHeart rhythm disorders (arrhythmias) affect the electrical system, or "wiring," of the heart muscle. Bradycardia describes a heartbeat that is too slow (less than 60 beats a minute) tachycardia (tachy=fast) is a too-rapid heartbeat. Ventricular fibrillation (VF) is the number one cause of sudden cardiac arrest.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
48 tayangan45 halamanArrhythmia Overview: Antonia Anna Lukito
Diunggah oleh
Joshua ObrienHeart rhythm disorders (arrhythmias) affect the electrical system, or "wiring," of the heart muscle. Bradycardia describes a heartbeat that is too slow (less than 60 beats a minute) tachycardia (tachy=fast) is a too-rapid heartbeat. Ventricular fibrillation (VF) is the number one cause of sudden cardiac arrest.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 45
Arrhythmia Overview
Antonia Anna Lukito
Arrhythmia
Heart rhythm disorders (arrhythmias) are
problems that affect the electrical system, or
"wiring," of the heart muscle. Heart
arrhythmias are very common and nearly
everyone will experience an abnormal heart
rhythm some time during their lives. Most
are not serious.
Categorization
Arrhythmias can be categorized in three
main ways:
the rate (too slow or too fast);
the location (ventricles-lower chambers
of heart or atria-upper chambers); and
the beat (steady or chaotic and
irregular).
Types of Heart Rhythm Disorders
Bradycardia
Tachycardia
Premature Heart Beat
Fibrillation
Bradycardia
Describes a heartbeat that is too slow (less than 60
beats a minute).
A normal heart contracts about 100,000 times each
day, at a rate of 60 to 100 times a minute.
The weak pace may mean the heart doesn't beat
often enough to ensure blood flow.
Slow heart rates can be the result of certain
medications, congenital heart disease, or the
degenerative processes of aging.
Heart block (or AV Block) and Sick Sinus Syndrome
are forms of bradycardia.
Tachycardia
(tachy=fast) is a too-rapid heartbeat.
There are two predominant types of tachycardia:
supraventricular tachycardia (SVT) and ventricular
tachycardia (VT).
The most common type of SVT is atrial fibrillation, an
irregular and rapid heartbeat in the upper chambers of the
heart (or atria).
At times, ventricular tachycardia (VT) can change without
warning into a deadly arrhythmia called ventricular
fibrillation (VF).
It is the number one cause of sudden cardiac arrest. Within
seconds, an individual loses consciousness and, without
immediate emergency treatment, will die within minutes.
Premature Heart Beat
Occurs when the heart's regular rhythm is
interrupted by early or premature beats.
It may feel as if the heart has skipped a beat.
Usually it is not serious.
If the beat arises from locations in the atria
(upper chambers) it is called premature atrial
beat.
Premature ventricular beats (also called
premature ventricular contractions or PVCs)
arise from the ventricles (lower chambers).
Fibrillation
Describes a heartbeat that is chaotic, or
irregular, and may seem to skip beats or beat
out of rhythm. This occurs when a chamber
of the heart goes into spasm and fails to
pump.
There are two types of fibrillation: atrial
fibrillation and ventricular fibrillation
Treatment Options
Lifestyle Changes
Medications
Cardiac Ablation
Electronic Devices
Implanted Cardioverter Defibrillators (ICDs)
Pacemakers
Devices for Heart Failure
Surgery
Lifestyle Changes
Since other heart disorders increase the risk
of developing arrhythmias, lifestyle changes
often are recommended.
In addition, improving health can lesson the
symptoms of arrhythmias and other heart
disorders as well as prove beneficial to
overall patient health
Medications
Medications can control abnormal heart
rhythms or treat related conditions such as
high blood pressure, coronary artery disease,
heart failure, and heart attack.
Drugs also may be administered to reduce
the risk of blood clots in patients with certain
types of arrhythmias
MANAGEMENT OF TACHY-ARRHYTHMIAS
Tachyarrhythmia
Supraventricular
Paroxysmal supraventricular tachycardias
Atrial fibrillation
Atrial flutter
Multifocal atrial tachycardia
Junctional tachycardia
Sinus tachycardia
Ventricular
Ventricular tachycardia ( 5 beats at 120 bpm; non-
sustained <30s, sustained >30s; monomorphic, polymorphic;
with pulse, pulseless)
Ventricular fibrillation
MANAGEMENT OF TACHY-ARRHYTHMIAS
Diagnosis
Obtain a 12-lead ECG
Echo may be necessary to exclude structural heart disease
? invasive electrophysiological study
Acute treatment
If in doubt and patient, treat as VT. If patient haemodynamically unstable,
immediate DC cardioversion/defibrillation
Active seek out and treat causes (acute coronary syndrome, acute
respiratory insufficiency of various aetiologies, sepsis, electrolytes)
Correct electrolytes : keep serum K > 4 mmol/L and Mg > 2 mmol/L
Narrow Complex Tachy-arrhythmias
Haemodynamic unstable
Immediate DC cardioversion (50J for PSVT/A flutter; 200J for AF)
Haemodynamic stable
Vagal maneouvres
Carotid Massage
IV adenosine 6 mg (ATP=10mg)---2 min---6 mg(10)---2 min---12 mg(20)
IV Verapamilm 5mg over 3-5 mins, to maximum 15 mg
IV Amiodarone (loading dose of 150mg over 10 mins, may repeat if failed to rate control;
followed by infusion 30 mg/hour) caution side effects
If failed to rate-control with amiodarone may consider other anti-arrhythmics eg
Diltiazem (0.25 to 0.35 mg/kg loading followed by infusion 5-15 mg/hour) caution
hypotension
IV Beta- blockers (metoprolol titrate 0.5-1mg, esmolol 0.5mg/kg/min for one min followed by
0.05-0.2mg/kg/min) caution hypotension
IV Digoxin (1 mg over 24 hours in increments of 0.25 to 0.5 mg, followed by 0.125 mg to 0.25
mg daily)
Wide Complex Tachy-arrhythmias
Haemodynamic unstable
Immediate DC cardioversion start at 100J, increase if
unsuccessful
Defibrillation according to ACLS protocol for VF and pulseless
VT
Haemodynamic stable
SVT (see above)
VT or uncertain
IV Amiodarone (loading dose of 150mg over 10 mins, may repeat if
failed to rate control; followed by infusion 30 mg/hour)
Bradyarrhythmia
Heart rate < 60 bpm
Sinus node dysfunction (sinus bradycardia, sinus
pause, sick sinus syndrome)
AV node dysfunction (1
st
, 2
nd
, 3
rd
degree AV block)
Actively seek and eliminate causes (ICU mediated,
extrinsic)
ICU vagally mediated causes
Intubation, suctioning, increased intracranial pressure,
urination, defaecation, vomiting , stretching
Extrinsic causes
Drugs (antiarrhythmic agents)
Electrolytes (K, Mg, Ca)
Hypothyroidism
Hypothermia
Sepsis
Specific infection (eg. endocarditis)
AMI (inferior AMI related AV blocks often transient;
Anterior AMI related AV blocks often irreversible)
Bradyarrhythmia
Acute treatment
May not need immediate treatment if haemodynamically stable
Correct electrolytes
Treat if
Symptomatic sinus bradycardia (hypotension, ischaemia, escape ventricular
arrhythmia)
Ventricular asystole
Symptomatic AV block (2nd degree Type I or 3rd degree with narrow-complex
escape rhythm)
Give
Atropine: IV 0.6 mg (max 3 mg)
Isoprenaline: Infusion at 0.5 10 mcg/min (caution in ischaemic heart disease)
Pacing: for symptomatic bradycardia.
Types including transcutaneous/epicardial/transvenous/permanent
PACING
Indications for urgent transcutaneous pacing
1. Sinus bradycardia with symptoms (SBP <80mmHg) unresponsive to
drug therapy
2. Mobitz type II 2
nd
degree AV block
3. 3
rd
degree heart block
4. Bilateral BBB (alternating BBB or RBBB with alternating
LAFB/LPFB)
5. Newly acquired or age indeterminate bifascicular block (LBBB,
RBBB with LAFB or LPFB) with 1
st
degree AV block
Because transcutaneous pacing may be uncomfortable, especially
when prolonged, it is intended to be prophylactic and temporary.
Refer to cardiologist for transvenous pacing in patients who
require ongoing pacing and in those with a very high probability of
requiring pacing
Indications for temporary transvenous pacing
1. Asystole
2. Symptomatic bradycardia (includes sinus bradycardia with
hypotension and Type I 2
nd
degree AV block with hypotension
not responsive to atropine)
3. Mobitz type II 2
nd
degree AV block
4. 3
rd
degree heart block
5. Bilateral BBB (alternating BBB or RBBB with alternating
LAFB/LPFB)
6. Newly acquired or age indeterminate bifascicular block (LBBB,
RBBB with LAFB or LPFB) with 1
st
degree AV block
Monitor to ensure appropriate pacing and sensing functions and
absence of dislodgment (CXR)
Frequent (at least once per 24 hours) testing of pacing thresholds
(pacing energy is usually set at more than 3 times the threshold)
Pacemakers
Devices that "pace" the heart rate when it is
too slow (bradycardia) can take over for the
heart's natural pacemaker, the sinoatrial
node, when it is functioning improperly.
Pacemakers monitor and regulate the rhythm
of the heart and transmit electrical impulses
to stimulate the heart if it is beating too
slowly.
Oral Anticoagulant in Atrial Fibrillation
Age less than 60, no heart disease, lone atrial fibrillationtreat with aspirin.
Age less than 60, heart disease, but really no risk factorstreat with aspirin.
Age greater than 60, but no risk factorstreat with aspirin.
Add diabetes and coronary artery diseasetreat with warfarin to an INR of 2 to
3.
Age >75treat with warfarin to an INR of 2 to 3.
Other high-risk patients (heart failure, EF <0.35, thyrotoxicosis, hypertension,
rheumatic heart disease)treat with warfarin (INR 2 to 3).
Patients with mitral stenosis, prosthetic heart valvestreat with warfarin (INR 2
to 3).
Prior thromboembolic event and persistent atrial thrombustreat with warfarin
to an INR of 2.5 to 3.5.
Patients undergoing cardioversion (electrical or pharmacological)anticoagulate
patients with atrial fibrillation (of at least 48 hours' duration) for at least 3 to 4
weeks before and 3 to 4 weeks after cardioversion. Even if you do a TEE, show no
thrombus, and cardiovert the patient, you still need to anticoagulate the patient
for 3 to 4 weeks after the procedure
Electronic Devices
By delivering a controlled electric shock to
the heart, defibrillators, or cardioverters
"shock" the heart back into a normal heart
rhythm
Sometimes the devices are external, such as
in an emergency situation. Often, the
electronics are implanted in the patient's
chest
Implanted Cardioverter Defibrillators
(ICDs)
ICDs are 99 percent effective in stopping life-
threatening arrhythmias and are the most
successful therapy to treat ventricular
fibrillation, the major cause of sudden cardiac
arrest.
ICDs continuously monitor the heart rhythm,
automatically function as pacemakers for heart
rates that are too slow, and deliver life-saving
shocks if a dangerously fast heart rhythm is
detected.
Ventricular tachycardia with an ICD
Devices for Heart Failure
The U.S. Food and Drug Administration (FDA)
recently approved a special type of pacemaker
for certain patients with heart failure.
In Cardiac Resynchronization Therapy, an
implanted device paces both the left and right
ventricles (lower chambers) of the heart
simultaneously.
This resynchronizes muscle contractions and
improves the efficiency of the weakened heart
Cardiac Ablation
In this procedure, one or more flexible, thin
tubes (catheters) are guided via x-ray into the
blood vessels and directed to the heart
muscle.
A burst of radiofrequency energy destroys
very small areas of tissue that give rise to
abnormal electrical signals
Catheter Ablation
Surgery
Although surgery is sometimes used to treat
abnormal heart rhythms, it is more
commonly elected to treat other cardiac
problems, such as coronary artery disease
and heart failure.
Correcting these conditions may reduce the
likelihood of arrhythmias
Indications for surgical ablation to treat AF
Patients with symptomatic AF undergoing other
cardiac surgery
Selected patients with asymptomatic AF
undergoing cardiac surgery in whom ablation
can be performed with minimal risk
Stand-alone surgery for AF should be considered
for patients with symptomatic AF who prefer a
surgical approach, have failed one or more
attempts at catheter ablation, or are not
candidates for catheter ablation
Figure 1 The corridor procedure for AF
Lee, R. et al. (2009) Surgery for atrial fibrillation
Nat. Rev. Cardiol. doi:10.1038/nrcardio.2009.106
Figure 2 The surgical maze
Lee, R. et al. (2009) Surgery for atrial fibrillation
Nat. Rev. Cardiol. doi:10.1038/nrcardio.2009.106
Figure 3 Bipolar radiofrequency ablation using Cardioblate
BP2 (Medtronic,
Inc., Minneapolis, MN)
Lee, R. et al. (2009) Surgery for atrial fibrillation
Nat. Rev. Cardiol. doi:10.1038/nrcardio.2009.106
Permission obtained from S. Klein, Medtronic, Inc., Minneapolis, MN
Anda mungkin juga menyukai
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesDari EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesPenilaian: 4 dari 5 bintang4/5 (1)
- 28,29 Management of Cardiac ArrhythmiasDokumen41 halaman28,29 Management of Cardiac ArrhythmiasSL Dr ChEMiSBelum ada peringkat
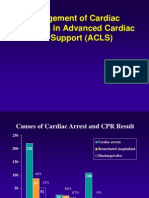
- Management of Cardiac Arrhytmia in Advanced Cardiac Life Support (ACLS)Dokumen34 halamanManagement of Cardiac Arrhytmia in Advanced Cardiac Life Support (ACLS)rhezzaagxxBelum ada peringkat
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideDari EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideBelum ada peringkat
- Medicine Lecture 17,18Dokumen51 halamanMedicine Lecture 17,18Nayela AkramBelum ada peringkat
- Pathophysiology of ArrhythmiasDokumen15 halamanPathophysiology of ArrhythmiasJonathan MontecilloBelum ada peringkat
- Arrhythmia: Zahid Fikri, M.KepDokumen31 halamanArrhythmia: Zahid Fikri, M.KepRahil ZilfahBelum ada peringkat
- 5 ArrhythmiaDokumen44 halaman5 ArrhythmiaDanny DesuBelum ada peringkat
- Management of ArrhythmiasDokumen4 halamanManagement of ArrhythmiasAray Al-AfiqahBelum ada peringkat
- Cardiac Emergencies Cne DelhiDokumen109 halamanCardiac Emergencies Cne DelhiManisha Thakur100% (1)
- Arrhythmia OF THE HEARTDokumen4 halamanArrhythmia OF THE HEARTSellappan MuthusamyBelum ada peringkat
- AntiarrhythmicsDokumen7 halamanAntiarrhythmicszanderBelum ada peringkat
- Arrhythmias: Sing Khien Tiong Gpst1Dokumen34 halamanArrhythmias: Sing Khien Tiong Gpst1preethi preethaBelum ada peringkat
- Arrhythmia NewDokumen73 halamanArrhythmia Newlohith saiBelum ada peringkat
- Cardiology Study Guide HandoutDokumen86 halamanCardiology Study Guide Handoutalinida89100% (1)
- Aritmia LetalDokumen53 halamanAritmia LetalMetta SariBelum ada peringkat
- A Fib in 60 Yr Old ManDokumen32 halamanA Fib in 60 Yr Old ManNurul HikmahBelum ada peringkat
- Management of Cardiac ArrestDokumen40 halamanManagement of Cardiac ArrestMark Francis NaniaBelum ada peringkat
- Cardiac Arrhythmia in Children PDFDokumen50 halamanCardiac Arrhythmia in Children PDFNorhafizah AhmadBelum ada peringkat
- ArrhythmiasDokumen47 halamanArrhythmiasJaismi AntonyBelum ada peringkat
- Arrhythmia (Irregular Heartbeats) Symptoms, Types, and TreatmentDokumen5 halamanArrhythmia (Irregular Heartbeats) Symptoms, Types, and TreatmentCyberMeow100% (1)
- Transient Ischemic Attack (TIA) : Heart Attack Peripheral Vascular Disease SmokingDokumen3 halamanTransient Ischemic Attack (TIA) : Heart Attack Peripheral Vascular Disease SmokingPrincessdhay TandangBelum ada peringkat
- Arrhythmia 6 YrDokumen72 halamanArrhythmia 6 YrPiyush MalikBelum ada peringkat
- Life Threatening Arrhythmia and ManagementDokumen40 halamanLife Threatening Arrhythmia and ManagementRuki HartawanBelum ada peringkat
- EmergencyDokumen47 halamanEmergencymedstudy123Belum ada peringkat
- ARRHYTHMIADokumen82 halamanARRHYTHMIAjiluBelum ada peringkat
- 2 - PPT DR Erika Maharani SPJPDokumen42 halaman2 - PPT DR Erika Maharani SPJPAmry YusufBelum ada peringkat
- Arrhythmias: Anurag Patidar Lecturer, Con, DMCHDokumen40 halamanArrhythmias: Anurag Patidar Lecturer, Con, DMCHpreet kaurBelum ada peringkat
- 02.emergency CardiologyDokumen135 halaman02.emergency Cardiologyapi-19916399Belum ada peringkat
- Cardiac ArrythmiasDokumen63 halamanCardiac ArrythmiasSankara SubramanianBelum ada peringkat
- ArrhythmiasDokumen14 halamanArrhythmiasHaribabuBabuBelum ada peringkat
- Cardiovascular Disorders2Dokumen61 halamanCardiovascular Disorders2Lui Andrei AnilaBelum ada peringkat
- 11-Acs2 StemiDokumen33 halaman11-Acs2 Stemiمحمد بن الصادقBelum ada peringkat
- Care of Patients With DysrhythmiasDokumen37 halamanCare of Patients With Dysrhythmiasأم حمدBelum ada peringkat
- Emergency in Medicine 2012Dokumen202 halamanEmergency in Medicine 2012micheal1960Belum ada peringkat
- Atrial Fibrillation: Dr. Roaa AlamoudiDokumen15 halamanAtrial Fibrillation: Dr. Roaa AlamoudiRana AlmimoniBelum ada peringkat
- CardiologyDokumen613 halamanCardiologyyangi dokaBelum ada peringkat
- Heartbeat Disorders: by Aisha Sara Tasnim Physician: Dr. SsebulibaDokumen31 halamanHeartbeat Disorders: by Aisha Sara Tasnim Physician: Dr. SsebulibaNinaBelum ada peringkat
- IC1 - Arrhythmia - 2012 EDITEDDokumen42 halamanIC1 - Arrhythmia - 2012 EDITEDrazorazBelum ada peringkat
- Cardiac ArrythmiaDokumen16 halamanCardiac ArrythmiaHossen AliBelum ada peringkat
- 41 Paediatric ArrhythmiasDokumen4 halaman41 Paediatric ArrhythmiasnasibdinBelum ada peringkat
- Primary Care Arrhythmia FinalDokumen36 halamanPrimary Care Arrhythmia FinalIsmai Eko SaputraBelum ada peringkat
- DR Jess Feltcher - Palpitations in General Practicce - 0Dokumen49 halamanDR Jess Feltcher - Palpitations in General Practicce - 0aim1997Belum ada peringkat
- Topic:: Unstable AnginaDokumen44 halamanTopic:: Unstable AnginaApurba100% (1)
- KegawatdaruratanDokumen164 halamanKegawatdaruratanmeida astriani gozaziBelum ada peringkat
- Cardiac Rhythm and Related Disorders: Marshell Tendean, MD Department of Internal Medicine UKRIDA JakartaDokumen39 halamanCardiac Rhythm and Related Disorders: Marshell Tendean, MD Department of Internal Medicine UKRIDA JakartaFatimah Hartina FaradillahBelum ada peringkat
- A Patient With PalpitationDokumen43 halamanA Patient With PalpitationChris Jardine LiBelum ada peringkat
- ECG Class ON VT PowerpointDokumen24 halamanECG Class ON VT PowerpointRoshilBelum ada peringkat
- Hippo EM Board Review - Bradycardia - A Simplified Approach Written Summary 2Dokumen10 halamanHippo EM Board Review - Bradycardia - A Simplified Approach Written Summary 2alexandertorresreyBelum ada peringkat
- Er FinalsDokumen63 halamanEr FinalsNaren RaviBelum ada peringkat
- Approach To Patients With Possible Cardiovascular Disease and Physical Examination of The Cardiovascular SystemDokumen79 halamanApproach To Patients With Possible Cardiovascular Disease and Physical Examination of The Cardiovascular SystemLajel S. LachicaBelum ada peringkat
- Chapter 5 HTDokumen56 halamanChapter 5 HTtesfamichael mengistu100% (1)
- Pemicu 6 KGD DeniseDokumen95 halamanPemicu 6 KGD DeniseVincent VandestyoBelum ada peringkat
- Management of Perioperative ArrhythmiasDokumen51 halamanManagement of Perioperative ArrhythmiasAbhishek LonikarBelum ada peringkat
- Cardiology Study Guide Handout PDFDokumen86 halamanCardiology Study Guide Handout PDFStarr Newman100% (1)
- Arrhythmia: King Saud University College of NursingDokumen24 halamanArrhythmia: King Saud University College of Nursinghatem alsrour100% (2)
- Cardiac Arrest1Dokumen27 halamanCardiac Arrest1Muhammad HaekalBelum ada peringkat
- Cardiovascular Diseases and Disorders.Dokumen33 halamanCardiovascular Diseases and Disorders.Hasnat AhmedBelum ada peringkat
- Advanced Cardiovascular Life Support in Adults (ACLS) : SubtitleDokumen30 halamanAdvanced Cardiovascular Life Support in Adults (ACLS) : SubtitleMohamad El SharBelum ada peringkat
- Oxygen Carrying System: Physiology ofDokumen22 halamanOxygen Carrying System: Physiology ofJoshua Obrien100% (1)
- Block EpitGland1Dokumen28 halamanBlock EpitGland1Joshua ObrienBelum ada peringkat
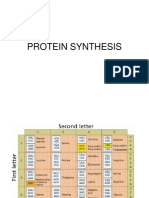
- Protein Synthesis3Dokumen11 halamanProtein Synthesis3Lady KweeBelum ada peringkat
- Budget ProposalDokumen1 halamanBudget ProposalJoshua ObrienBelum ada peringkat
- Sports Injury and Clinical Problem of JointsDokumen25 halamanSports Injury and Clinical Problem of JointsJoshua ObrienBelum ada peringkat
- FMS II DEv of LimbDokumen47 halamanFMS II DEv of LimbJoshua ObrienBelum ada peringkat
- Protein Targetting: Septelia Inawati WanandiDokumen11 halamanProtein Targetting: Septelia Inawati WanandiJoshua ObrienBelum ada peringkat
- Chemistry of Major Compounds in The Body (Full)Dokumen4 halamanChemistry of Major Compounds in The Body (Full)Joshua ObrienBelum ada peringkat
- Acids and BasesDokumen2 halamanAcids and BasesYeniBelum ada peringkat
- Suicide-ICM II 2012Dokumen11 halamanSuicide-ICM II 2012Joshua ObrienBelum ada peringkat
- Chemistry of Major Compounds in The Body (Full)Dokumen4 halamanChemistry of Major Compounds in The Body (Full)Joshua ObrienBelum ada peringkat
- Cell CycleDokumen28 halamanCell CycleJoshua ObrienBelum ada peringkat
- Cell CycleDokumen28 halamanCell CycleJoshua ObrienBelum ada peringkat
- Fisio Log I Jan TungDokumen32 halamanFisio Log I Jan TungJoshua ObrienBelum ada peringkat
- Joint Instability: Hendradi Khumarga SPOT. FICSDokumen48 halamanJoint Instability: Hendradi Khumarga SPOT. FICSJoshua ObrienBelum ada peringkat
- Myocardial Ischemia and Myocardial Infarction 2009Dokumen71 halamanMyocardial Ischemia and Myocardial Infarction 2009Joshua ObrienBelum ada peringkat
- Cardiac EnzymeDokumen2 halamanCardiac EnzymeJoshua ObrienBelum ada peringkat
- Bloods VesselDokumen34 halamanBloods VesselJoshua ObrienBelum ada peringkat
- Antiaritmia: Frans D. Suyatna Modified by Sulistia 1010 Departemen Farmakologi & Terapeutik FKUIDokumen56 halamanAntiaritmia: Frans D. Suyatna Modified by Sulistia 1010 Departemen Farmakologi & Terapeutik FKUIJoshua ObrienBelum ada peringkat
- CardiovascularDokumen21 halamanCardiovascularJoshua ObrienBelum ada peringkat
- Excitable Tissue (Muscle) : V. Sutarmo SetiadjiDokumen40 halamanExcitable Tissue (Muscle) : V. Sutarmo SetiadjiJoshua ObrienBelum ada peringkat
- Connective Tissue: Dr. Jan Tambayong, PHK Histologi FK-UPHDokumen51 halamanConnective Tissue: Dr. Jan Tambayong, PHK Histologi FK-UPHJoshua ObrienBelum ada peringkat
- The Upper Limb: Musculoskeletal System BlockDokumen50 halamanThe Upper Limb: Musculoskeletal System BlockJoshua ObrienBelum ada peringkat
- Skill Lab Cath & EchoDokumen81 halamanSkill Lab Cath & EchoJoshua ObrienBelum ada peringkat
- #1 Kuliah Basic Principle and Lab Test For Thrombosis and FibrinolysisDokumen22 halaman#1 Kuliah Basic Principle and Lab Test For Thrombosis and FibrinolysisJoshua ObrienBelum ada peringkat
- AntiaritmiaDokumen56 halamanAntiaritmiaYeniBelum ada peringkat
- Electrical Activity of The Heart: V. Sutarmo SetiadjiDokumen16 halamanElectrical Activity of The Heart: V. Sutarmo SetiadjiJoshua ObrienBelum ada peringkat
- Aritmia 1Dokumen83 halamanAritmia 1YeniBelum ada peringkat
- Thalassemia Dr. DinaDokumen21 halamanThalassemia Dr. DinaYeniBelum ada peringkat
- Methods of Nutrient DeliveryDokumen3 halamanMethods of Nutrient DeliveryFarmisa MannanBelum ada peringkat
- Annotated BibliographyDokumen4 halamanAnnotated Bibliographyapi-284834629Belum ada peringkat
- Hypertensive Disorders of Pregnancy and AssociatedDokumen10 halamanHypertensive Disorders of Pregnancy and AssociatedMedrechEditorialBelum ada peringkat
- Acu-Stim For RecoveryDokumen4 halamanAcu-Stim For Recoverycare_e_genBelum ada peringkat
- Feeding Device Shaju V Cherian and Dipu KCDokumen20 halamanFeeding Device Shaju V Cherian and Dipu KCShaju V CherianBelum ada peringkat
- The Diagnosis and Management ofDokumen3 halamanThe Diagnosis and Management ofPreetam PatnalaBelum ada peringkat
- GuideDokumen52 halamanGuidemihaelklajner100% (1)
- ICE DrugsDokumen2 halamanICE DrugsRichelle FrondaBelum ada peringkat
- Comparison of Health-Related Quality of Life of Elderly With Hypertension Living in Long-Term Facility vs. CommunityDokumen82 halamanComparison of Health-Related Quality of Life of Elderly With Hypertension Living in Long-Term Facility vs. CommunityEllah ChristineBelum ada peringkat
- Faktor-Faktor Yang Berhubungan Dengan Kejadian Dermatitis Atopik Di Puskesmas Bangkinang KotaDokumen10 halamanFaktor-Faktor Yang Berhubungan Dengan Kejadian Dermatitis Atopik Di Puskesmas Bangkinang KotaAsha NopatiBelum ada peringkat
- CHAPTER 17 - Overview of Human Infectious DiseasesDokumen3 halamanCHAPTER 17 - Overview of Human Infectious DiseasesJacob PallorinaBelum ada peringkat
- Paces Guide 2012 From Online NotesDokumen228 halamanPaces Guide 2012 From Online NotesThistell ThistleBelum ada peringkat
- What Is A Medical Technologist?: History of Medical Technology ProfessionDokumen7 halamanWhat Is A Medical Technologist?: History of Medical Technology ProfessionRey Ann ConcepcionBelum ada peringkat
- Activity Intolerance YAp ER NCPDokumen2 halamanActivity Intolerance YAp ER NCPmecz26100% (2)
- ATT Induced Hepatotoxicity: Dr. K. K. SharmaDokumen36 halamanATT Induced Hepatotoxicity: Dr. K. K. SharmaSucharita Ray100% (1)
- Insulin Resistance and PCOS-dr. Hilma Final 11 Juli 2021 FIXDokumen48 halamanInsulin Resistance and PCOS-dr. Hilma Final 11 Juli 2021 FIXputrihealthirezaBelum ada peringkat
- Aerobic Lab ReportDokumen19 halamanAerobic Lab Reportapi-427151706Belum ada peringkat
- Optijuice BenefitsDokumen134 halamanOptijuice BenefitsIdeza SabadoBelum ada peringkat
- Fraser Health: Health Authority Redesign AccomplishmentsDokumen13 halamanFraser Health: Health Authority Redesign AccomplishmentsStephen OlsonBelum ada peringkat
- Focus Diagnosis Action Response Subjective: "I Hate Water and I Don't Drink It Much " DXDokumen2 halamanFocus Diagnosis Action Response Subjective: "I Hate Water and I Don't Drink It Much " DXGrape Juice100% (1)
- For Demo in Teaching Strategies by Mike ReyesDokumen10 halamanFor Demo in Teaching Strategies by Mike ReyesPaulo Sandino GaliciaBelum ada peringkat
- Nursing Care Plan Using This Format: Prioritization of Nursing DiagnosisDokumen2 halamanNursing Care Plan Using This Format: Prioritization of Nursing DiagnosisERIKA ANNE CADAWANBelum ada peringkat
- Postmortem Biochemistry of Vitreous Humor and Glucose MetabolismDokumen7 halamanPostmortem Biochemistry of Vitreous Humor and Glucose MetabolismsbeyeforhireBelum ada peringkat
- Chapter 6-Family Nursing Care PlanDokumen3 halamanChapter 6-Family Nursing Care PlanBi B BelleBelum ada peringkat
- The Effect of Iron (Fe) Tablets To The Anemia Status of Adolescent WomenDokumen5 halamanThe Effect of Iron (Fe) Tablets To The Anemia Status of Adolescent WomenNani MulyatiBelum ada peringkat
- Orthopedic NursingDokumen201 halamanOrthopedic NursingMitch Hellgirl Almonte100% (2)
- Antuñano 2000 PDFDokumen10 halamanAntuñano 2000 PDFAlonso FlBelum ada peringkat
- Writing Nurses12 PDFDokumen3 halamanWriting Nurses12 PDFnjBelum ada peringkat
- Papers: Fetal Nuchal Translucency: Ultrasound Screening For Chromosomal Defects in First Trimester ofDokumen3 halamanPapers: Fetal Nuchal Translucency: Ultrasound Screening For Chromosomal Defects in First Trimester ofHao Keat HoeBelum ada peringkat
- Exam Labor ProcessDokumen4 halamanExam Labor ProcessAileen A. Monares0% (1)