Anesthesia
Diunggah oleh
ejikieru03Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Anesthesia
Diunggah oleh
ejikieru03Hak Cipta:
Format Tersedia
Anesthesia
Dr Abdollahi
Anesthesia
From Greek anaisthesis means not sensation
Listed in Baileys English Dictionary 1721.
When the effect of ether was discoveredanesthesia
used as a name for the new phenomenon.
Basic Principles of Anesthesia
Anesthesia defined as the abolition of sensation
Analgesia defined as the abolition of pain
Triad of General Anesthesia
need for unconsciousness
need for analgesia
need for muscle relaxation
History of Anesthesia
History of Anesthesia
Ether synthesized in 1540 by Cordus
Ether used as anesthetic in 1842 by Dr.
Crawford W. Long
Ether publicized as anesthetic in 1846 by
Dr. William Morton
Chloroform used as anesthetic in 1853 by
Dr. John Snow
History of Anesthesia
Endotracheal tube discovered in 1878
Local anesthesia with cocaine in 1885
Thiopental first used in 1934
Curare first used in 1942 - opened the Age
of Anesthesia
Anesthesiologists care for the surgical patient in the
preoperative, intraoperative, and postoperative
period . Important patient care decisions reflect the
preoperative evaluation, creating the anesthesia
plan, preparing the operating room, and managing
the intraoperative anesthetic.
Preoperative Evaluation
The goals of preoperative evaluation include assessing the
risk of coexisting diseases, modifying risks, addressing
patients' concerns, and discussing options for anesthesia
care.
What is the indication for the proposed surgery? It is elective
or an emergency?
The indication for surgery may have particular anesthetic
implications. For example, a patient requiring esophageal
fundoplication will likely have severe gastroesophageal
reflux disease, which may require modification of the
anesthesia plan (e.g., preoperative non particulate antacid,
intraoperative rapid sequence induction of anesthesia).
What are the inherent risk of this surgery?
Surgical procedures have different inherent risks.
For example, a patient undergoing coronary artery
bypass graft has a significant risk of problems
such as death, stroke, or myocardial infarction.
A patient undergoing cataract extraction has a low
risk of major organ damage.
Does the patient have coexisting medical problems?
Does the surgery or anesthesia care plan need to
be modified because of them?
Has the patient had anesthesia before? Were there
Complication such as difficult airway management?
Does the patient have risk factor for difficult
airway management?
Creating the Anesthesia Plan
After the preoperative evaluation, the anesthesia plan can
be completed. The plan should list drug choices and doses
in detail, as well as anticipated problems .Many variations on
a given plan may be acceptable, but the trainee and the
supervising anesthesiologist should agree in advance on
the details.
Preparing the Operating Room
After determining the anesthesia plan, the
trainee must prepare the operating room .
Anesthesia Providers
Anesthesiologist ( aphysician with 4 or more yearsof
speciality training in anesthesiology after medical
school)
Certified registered nurse anesthetist (CRNA),
working under the direction and supervision of an
anesthesiologist or a physician
CRNA must have 2 years of training in anesthesia
Patient Safety
Patient risk and safety are concerns during surgery and
anesthesia .
Data from a number of studies of death caused by
anesthesia indicate a death rate ranging from 1 per 20,000-
35,000.
A fourfoulded decline over the last 30 years even though
surgical procedures are undertaken on increasingly sicker
and much higher risk patients than in the past.
Awareness of potential problems and constant vigilance (the
process of paying close and continuous attention) are crucial
to good patient care.
Preoperative preparation patient
evaluation
Anaesthesiologist:
reviews the patients chart,
evaluate the laboratory data and diagnostic studies such
as electrocardiogram and chest x-ray,
verify the surgical procedure,
examins the patient,
discuss the options for anesthesia and the attendant risks
and
ordered premedication if appropriate
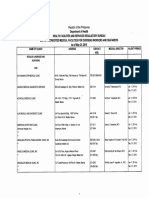
The physical status classification
Developed by the American Society of Anesthesiologist (ASA) to
provide uniform guidelines for anesthesiologists.
It is an evaluation of anesthetic morbidity and mortality related to the
extent of systemic diseases, physiological dysfunction, and anatomic
abnormalities.
Intraoperative difficulties occur more frequently with patients who
have a poor physical status classification.
Choice of anesthesia
The patients understanding and wishes regarding the type of
anesthesia that could be used
The type and duration of the surgical procedure
The patientss physiologic status and stability
The presence and severity of coexisting disease
The patients mental and psychologic status
The postoperative recovery from various kinds of anesthesia
Options for management of postoperative pain
Any particular requiremets of the surgeon
There is major and minor surgery but only major anesthesia
Types of anesthesia care
General Anesthesia
Reversible, unconscious state is characterised
by amnesia (sleep, hypnosis or basal narcosis),
analgesia (freedom from pain) depression of
reflexes, muscle relaxation
Put to sleep
Types of anesthesia care
Regional Anesthesia
A local anethetic is injected to block or ansthetize a
nerve or nerve fibers
Implies a major nerve block administered by an
anesthesiologist (such as spinal, epidural, caudal, or
major peripheral block)
Types of anesthesia care
monitered anesthesia care
Infiltration of the surgical site with a local
anesthesia is performed by the surgeon
The anasthesiologist may supplement the local
anesthesia with intravenous drugs that provide
systemic analgesia and sedation and depress
the response of the patients autonomic nervous
system
Types of anesthesia care
local anesthesia
Employed for minor procedures in which the
surgical site is infiltrated with a local anesthetic such
as lidocaine or bupivacaine
A perioperative nurse usually monitors the patients
vital signs
May inject intravenous sedatives or analgesic drugs
Premedication
Purpose: to sedate the patient and reduce anxiety
Classified as sedatives and hypnotics, tranquilizers, analgesic or narcotics and
anticholinergics
Antiacid or an H2receptor-blockingdrug such as cimitidine (tagamet) or ranitidine
(Zantac) to decrease gastric acid production and make the gastric contents less acidic
If aspiration occur this premedication decreases the resultant pulmonary damage
Given 60-90 minutes before surgery, or may be given i.v. After the pat. arrives in
the surgical suite
NPO for a minimum of 6 hours before elective surgery
Not given to elderly people or ambulatory patients because residual effects of the
drugs are present long after the pat. have been discharged and gone home
Perioperative monitoring
Undergeneral anesthesia: monitoring
Inspired oxygen analyzer(FiO2) which calibrated to room air and
100% oxygen on a daily basis
Low pressure disconnect alarm, which senses pressure in the
expiratory limb of the patient circuit
Inspiratory pressure
Respirometer (these four devices are an integral part of most modern
anesthesia machine
ECG
BP-automated unit
Heart rate
Precordial or esophagel stethoscope
Temp
Perioperative monitoring
Pulse oximeters
End tidal carbon dioxide (ECO2)
Peripheral nerve stimulator if muscle relaxants are used
Foly catheter
For selected patint with a potential risk of venous air
embolism a doppler probe may placed over the right atrium
Invasive: arterial pressure mesurements, central venous
pressure
Pulmonary artery catheter and continous mixed venous
oxygen saturation measured
Perioperative monitoring
For special conditions other monitors as
transesophageal echocardiography
Electroencephalogram
Cereral or neurological may be used
Inhalational Anesthetic Agents
Inhalational anesthesia refers to the delivery
of gases or vapors from the respiratory
system to produce anesthesia
Pharmacokinetics--uptake, distribution, and
elimination from the body
Pharmacodyamics-- MAC value
Regional Anesthesia
Defined as a reversible loss of sensation in
a specific area of the body
Spinal anesthesia
Epidural anesthesia
IV Regional Blocks
Peripheral Nerve Blocks
Spinal Anesthesia
A local anesthetic agent (lidocaine,
tetracaine or bupivacaine) is injected into
the subarachnoid space
Spinal anesthesia is also known as a
subarachnoid block
Blocks sensory and motor nerves,
producing loss of sensation and temporary
paralysis
Possible Complications of Spinal
Anesthesia
Hypotension
Post-dural puncture headache (Spinal headache) caused by
leakage of spinal fluid through the puncture hole in the dura-
can be treated by blood patch
High Spinal- can cause temporary paralysis of respiratory
muscles. Patient will need ventilator support until block wears
off
Epidural Anesthesia
Local anesthetic agent is injected through
an intervertebral space into the epidural
space.
May be administered as a one-time dose, or
as a continuous epidural, with a catheter
inserted into the epidural space to
administer anesthetic drug
Dr. Aidah Abu Elsoud Alkaissi
Division of Intensive Care and
Anaesthesiology University of
Linkping Sweden
Complications of Epidural
Anesthesia
Hypotension
Inadvertent dural puncture
Inadvertent injection of anesthetic into the
subarachnoid space
IV Regional Blocks
Also known as a Bier Block
Used on surgery of the upper extremities
Patient must have an IV inserted in the
operative extremity
IV Regional Block
After a pneumatic tourniquet is applied to
extremity, Lidocaine is injected through the
IV.
Anesthesia lasts until the tourniquet is
deflated at the end of the case.
IV Regional Blocks
IMPORTANT- to prevent an overdose of
lidocaine it is important not to deflate the
tourniquet quickly at the end of the
procedure.
Peripheral Nerve Blocks
Injection of local anesthetic around a
peripheral nerve
Can be used for anesthesia during surgery
or for post-op pain relief
Examples: ankle block for foot surgery,
supraclavicular block for post-op pain
control after shoulder surgery
Monitored Anesthesia Care (MAC)
Generally used for short, minor procedures
done under local anesthesia
Anesthesia provider monitors the patient and
may provide supplemental IV sedation if
indicated
Conscious Sedation
Used for short, minor procedures
Used in the OR and outlying areas
(ER, GI Lab, etc)
Patient is monitored by a nurse and receives
sedation sufficient to cause a depressed level of
consciousness, but not enough to interfere with
patients ability to maintain their airway
Inhalation Anesthetics
Nitrous Oxide- can cause expansion of
other gases- use of N
2
0 contraindicated in
patients who have had medical gas instilled
in their eye(s) during retinal detachment
repair surgery
Inhalation Anesthetics
Cause cerebrovascular dilation and increased
cerebral blood flow
Cause systemic vasodilation and decreased blood
pressure
Post-op N&V
All inhalation anesthetics, except N
2
0, can trigger
malignant hyperthermia in susceptible patients
Intravenous
Induction/Maintenance Agents
Propofol (Diprivan)- pain/burning on injection,
can cause bizarre dreams
Pentothal (Sodium Thiopental)- can cause
laryngospasm
General Anesthesia
During induction the room should be as quiet as
possible
The circulator should be available to assist
anesthesia provider during induction & emergence
Never move/reposition an intubated patient
without coordinating the move with anesthesia
first
General Anesthesia
Laryngospasm may happen in a patient having a
procedure with general anesthesia
When laryngospasm occurs, it is usually during
intubation or emergency
Assist anesthesia provider as needed- call for
anesthesia back-up if necessary
Difficult Airway Cart
Anesthesia maintains a Difficult Airway
Cart containing equipment & supplies for
difficult intubations
This cart is stored in one of the anesthesia
supply rooms
Page anesthesia tech if the cart is needed for
your room
Cricoid Pressure or Sellick Maneuver
Used for patients at risk for aspiration
during induction, due to a full stomach or
other factors such as a history of reflux
Pressure on the cricoid cartilage compresses
the esophagus against the cervical vertebrae
and prevents reflux
Sellick Maneuver
Cricoid pressure is maintained, as directed by
anesthesia provider, until the ETT cuff is inflated:
Regional Anesthesia
Circulator may need to assist anesthesia
provider with positioning for spinal or
epidural anesthesia.
Patient usually is positioned laterally for
placement of regional anesthesia, but may
be positioned sitting upright.
The Awake Patient
Patients undergoing surgery with regional
or local anesthesia, even if sedated, may be
aware of conversation and activity in room
Post sign on door to OR, Patient is Awake
so that staff entering room will be aware
that patient is conscious
When Patient is Awake
Limit any discussion of patients medical
condition and prognosis
Avoid discussion of other patients & limit
unnecessary conversation-- a sedated
patient can easily misinterpret conversation
they overhear
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- RACE TOPICS YEAR WISE-from 2001 To 2019Dokumen25 halamanRACE TOPICS YEAR WISE-from 2001 To 2019DhivaSankarBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Spinal AnesthesiaDokumen4 halamanSpinal AnesthesiaIndah Permata Gaisar100% (2)
- Diabetes Mellitus CPGDokumen157 halamanDiabetes Mellitus CPGejikieru03100% (3)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- 2016 PG Dissertation TopicsDokumen77 halaman2016 PG Dissertation Topicspaidisuri67% (3)
- Our Proforma Invoice Mbli/04/07/M-891: FOR: Our Lady of Mercy General HospitalDokumen3 halamanOur Proforma Invoice Mbli/04/07/M-891: FOR: Our Lady of Mercy General Hospitalejikieru03Belum ada peringkat
- Instilling Purpose in Your ChoirDokumen3 halamanInstilling Purpose in Your Choirejikieru03Belum ada peringkat
- Ofw Clinic May202015Dokumen14 halamanOfw Clinic May202015ejikieru03Belum ada peringkat
- Proforma Invoice 15Dokumen5 halamanProforma Invoice 15ejikieru03Belum ada peringkat
- Proforma Invoice 14Dokumen2 halamanProforma Invoice 14ejikieru03Belum ada peringkat
- Nueva Ecija Doctors Hospital: Our Proforma Invoice Mbli/04/11/M-1445Dokumen3 halamanNueva Ecija Doctors Hospital: Our Proforma Invoice Mbli/04/11/M-1445ejikieru03Belum ada peringkat
- MS Definition and AnatomyDokumen9 halamanMS Definition and Anatomyejikieru03Belum ada peringkat
- Proforma Invoice 7Dokumen3 halamanProforma Invoice 7ejikieru03Belum ada peringkat
- Proforma Invoice 15Dokumen5 halamanProforma Invoice 15ejikieru03Belum ada peringkat
- Proforma Invoice 8Dokumen3 halamanProforma Invoice 8ejikieru03Belum ada peringkat
- FOR: Ospital NG Maynila and Medical Center: Our Proforma Invoice Mbli/04/06/M-797Dokumen4 halamanFOR: Ospital NG Maynila and Medical Center: Our Proforma Invoice Mbli/04/06/M-797ejikieru03Belum ada peringkat
- Proforma Invoice 11Dokumen3 halamanProforma Invoice 11ejikieru03Belum ada peringkat
- Equipment For Ophthalmology: FOR: Amang Rodriguez Medical Center Attention: Roland L. Cortez, M.DDokumen2 halamanEquipment For Ophthalmology: FOR: Amang Rodriguez Medical Center Attention: Roland L. Cortez, M.Dejikieru03Belum ada peringkat
- FOR: Paulino J. Garcia Mem. Medical Center: Our Proforma Invoice Mbli/04/06/M-804Dokumen3 halamanFOR: Paulino J. Garcia Mem. Medical Center: Our Proforma Invoice Mbli/04/06/M-804ejikieru03Belum ada peringkat
- Proforma InvoiceDokumen2 halamanProforma Invoiceejikieru03Belum ada peringkat
- Proforma Invoice 2Dokumen2 halamanProforma Invoice 2ejikieru03Belum ada peringkat
- Proforma Invoice 3Dokumen6 halamanProforma Invoice 3ejikieru03Belum ada peringkat
- Proforma Invoice 4Dokumen3 halamanProforma Invoice 4ejikieru03Belum ada peringkat
- Dermatology CasesDokumen4 halamanDermatology Casesejikieru03Belum ada peringkat
- Treatment of Open Angle GlaucomaDokumen10 halamanTreatment of Open Angle Glaucomaejikieru03Belum ada peringkat
- 5336mah Normal Labor and DeliveryDokumen90 halaman5336mah Normal Labor and DeliveryPencenk AzznewBelum ada peringkat
- Zeiss IOLMaster2Dokumen10 halamanZeiss IOLMaster2ejikieru03Belum ada peringkat
- Diagnosis of GDM: According To The Philippine Practice Guidelines On The Diagnosis and Management of Diabetes MellitusDokumen10 halamanDiagnosis of GDM: According To The Philippine Practice Guidelines On The Diagnosis and Management of Diabetes Mellitusejikieru03Belum ada peringkat
- Optimal Management of Hypotension During Cesarean Delivery Under Spinal AnesthesiaDokumen22 halamanOptimal Management of Hypotension During Cesarean Delivery Under Spinal AnesthesiaJosé Alberto LozanoBelum ada peringkat
- Perioperative Pre-Class Mini-Lecture - CH 17-19Dokumen22 halamanPerioperative Pre-Class Mini-Lecture - CH 17-19Marcel YoungBelum ada peringkat
- Ch. 18. Intra-Operative Nursing CareDokumen49 halamanCh. 18. Intra-Operative Nursing Careمحمد الحواجرةBelum ada peringkat
- Local Anesthesia Exam TipsDokumen9 halamanLocal Anesthesia Exam TipsshadapaaakBelum ada peringkat
- Eop AnaesDokumen26 halamanEop AnaesSheera EiyraaBelum ada peringkat
- Theatre Nursing: By: Gachuhi WangariDokumen130 halamanTheatre Nursing: By: Gachuhi WangariJonah nyachae100% (1)
- Final THESIS 1-116 To PrintDokumen116 halamanFinal THESIS 1-116 To PrintMahesh RajwalBelum ada peringkat
- Shivering and Neuraxial AnesthesiaDokumen12 halamanShivering and Neuraxial AnesthesiaKarla Albert ReyesBelum ada peringkat
- Local Anesthetics Used For Spinal Anesthesia: Abdirahman Dahir Wais (BSN, Anesthetist)Dokumen39 halamanLocal Anesthetics Used For Spinal Anesthesia: Abdirahman Dahir Wais (BSN, Anesthetist)Abdi MohamedBelum ada peringkat
- Principles of AnesthesiaDokumen60 halamanPrinciples of AnesthesiaTakale BuloBelum ada peringkat
- OB1 Lec - AnalgesiaDokumen3 halamanOB1 Lec - Analgesiaapi-3700579Belum ada peringkat
- Case Study Presentation KPJ JohorDokumen131 halamanCase Study Presentation KPJ JohorAmar Nur Arif ZazuliBelum ada peringkat
- Laporan Kasus - Dendy Dwi Ramadhani - PPDS Anestesi BrawijayaDokumen1 halamanLaporan Kasus - Dendy Dwi Ramadhani - PPDS Anestesi BrawijayaDendyBelum ada peringkat
- Charles D Giordano CRNA, MSN (Major USAFR)Dokumen51 halamanCharles D Giordano CRNA, MSN (Major USAFR)saritha OrugantiBelum ada peringkat
- American Society of Anesthesiologists: A B C D E F GDokumen40 halamanAmerican Society of Anesthesiologists: A B C D E F Gmarina_shawkyBelum ada peringkat
- Anesthesia: Mr. Renato D. Lacanilao, RN, MAN LecturerDokumen25 halamanAnesthesia: Mr. Renato D. Lacanilao, RN, MAN LecturerJmarie Brillantes Popioco100% (1)
- Segmental Spinal Anesthesia A Systematic ReviewDokumen6 halamanSegmental Spinal Anesthesia A Systematic Reviewجعفر محمدBelum ada peringkat
- Laporan Kasus: Gagal Spinal Pada Pasien Operasi Amputasi Transfemoral Dengan Debridemen Dan PenatalaksanaannyaDokumen10 halamanLaporan Kasus: Gagal Spinal Pada Pasien Operasi Amputasi Transfemoral Dengan Debridemen Dan PenatalaksanaannyaRibut sriwahyuniBelum ada peringkat
- B20M05L07 Regional AnesthesiaDokumen15 halamanB20M05L07 Regional AnesthesiaLeodel Tolentino BarrioBelum ada peringkat
- Persistent Paralysis After Spinal Paresthesia PDFDokumen6 halamanPersistent Paralysis After Spinal Paresthesia PDFNadia Gina AnggrainiBelum ada peringkat
- MyelographyDokumen5 halamanMyelographyYamikaze MinatoBelum ada peringkat
- Update in AnaesthesiaDokumen56 halamanUpdate in AnaesthesiaRoy ABelum ada peringkat
- Original Article: Ayesha Goyal, P. Shankaranarayan, P. GanapathiDokumen6 halamanOriginal Article: Ayesha Goyal, P. Shankaranarayan, P. GanapathiAnonymous S0H8cqgnfiBelum ada peringkat
- Pain and Its Control in R 2018 Veterinary Clinics of North America Exotic ADokumen16 halamanPain and Its Control in R 2018 Veterinary Clinics of North America Exotic AYaiza Garcia CasadoBelum ada peringkat
- Davinci Medical AcademyDokumen10 halamanDavinci Medical Academysk100% (2)
- Combined Spinal Epidural Anesthesia and Analgesia: March 2012Dokumen21 halamanCombined Spinal Epidural Anesthesia and Analgesia: March 2012Elaine LaizaBelum ada peringkat
- Regional Anesthetic Blocks - StatPearls - NCBI BookshelfDokumen7 halamanRegional Anesthetic Blocks - StatPearls - NCBI BookshelfCarolina SidabutarBelum ada peringkat