All About CHF
Diunggah oleh
ocsitaocsitulHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
All About CHF
Diunggah oleh
ocsitaocsitulHak Cipta:
Format Tersedia
CHRONIC CONGESTIVE HEART
FAILURE
A Comprehensive Overview on Diagnosis and Treatment
Dr. Cholid Tri Tjahjono, MKes, SpJP
Faculty of Medicine
Brawijaya University Malang
Introduction
Definition : Heart Failure
The situation when the heart is incapable of
maintaining a cardiac output adequate to
accommodate metabolic requirements and the
venous return. E. Braunwald
Pathophysiological state in which an
abnormality of cardiac function is responsible
for the failure of the heart to pump blood at a
rate commensurate with the requirements of
the metabolizing tissues. Euro Heart J ; 2001. 22: 1527-1560
DEFINITION OF HEART FAILURE.
Criteria 1 and 2 should be fulfilled in all cases
1. Symptoms of heart failure
(at rest or during exercise)
And
2. Objective evidence of cardiac dysfunction
(at rest)
And
(in cases where the diagnosis is in doubt)
3. Response to treatment directed towards heart
failure
Task Force Report. Guidelines for the diagnosis and treatment of chronic heart failure.
European Society of Cardiology.2001
EPIDEMIOLOGY
Europe
The prevalence of symptomatic HF range from 0.4-2%.
10 million HF pts in 900 million total population
USA
nearly 5 million HF pts.
500,000 pts are D/ HF for the 1
st
time each year.
Last 10 years number of hospitalizations has increased.
Nearly 300,000 patients die of HF each year.
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
ACC/AHA Guidelines for the
Evaluation and Management of Chronic Heart Failure in the Adult 2001
DESCRIPTIVE TERMS in HEART FAILURE
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1528
Acute vs Chronic Heart Failure
Systolic vs Diastolic Heart Failure
Right vs Left Heart Failure
Mild , Moderate, Severe Heart Failure
New York Heart Association (NYHA)
Classification of Heart Failure
Class I
No limitation : ordinary physical exercise does
not cause undue fatigue, dyspnoea or palpita-
tions.
Class II
Slight limitation of physical activity : comfor-
table at rest but ordinary activity results in
fatigue, dyspnoea, or palpitation.
Class - III
Marked limitation of physical activity : comfor-
table at rest but less than ordinary activity
results in symptoms.
Class - IV
Unable to carry out any physical activity with-
out discomfort : symptoms of heart failure are
present even at rest with increased discomfort
with any physical activity.
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1531
(Adapted from Williams JF et al., Circulation. 1995; 92 : 2764-2784)
ACC/AHA A New Approach To The Classification of HF
Stage Descriptions Examples
A Patient who is at high risk for
developing HF but has no
structural disorder of the heart.
Hypertension; CAD; DM;
rheumatic fever; cardiomyopathy.
B Patient with a structural disorder
of the heart but who has never
developed symptoms of HF.
LV hypertrophy or fibrosis;
LV dilatation; asymptomatic VHD;
MI.
C Patient with past or current
symptoms of HF associated with
underlying structural heart
disease.
Dyspnea or fatigue ec LV systolic
dysfunction; asymptomatic
patients with HF.
D Patient with end-stage disease Frequently hospitalized pts ; pts
awaiting heart transplantation etc
ACC/AHA Guidelines for the
Evaluation and Management of Chronic Heart Failure in the Adult 2001
Stage A Stage B Stage C Stage D
Pts with :
Hypertension
CAD
DM
Cardiotoxins
FHx CM
THERAPY
Treat Hypertension
Stop smoking
Treat lipid disorders
Encourage regular
exercise
Stop alcohol
& drug use
ACE inhibition
Pts with :
Previous MI
LV systolic
dysfunction
Asymptomatic
Valvular disease
THERAPY
All measures under
stage A
ACE inhibitor
Beta-blockers
THERAPY
All measures under
stage A
Drugs for routine use:
diuretic
ACE inhibitor
Beta-blockers
digitalis
THERAPY
All measures under
stage A,B and C
Mechanical assist
device
Heart transplantation
Continuous IV
inotrphic infusions for
palliation
Pts who have
marked symptoms
at rest despite
maximal medical
therapy.
Pts with :
Struct. HD
Shortness of
breath and fatigue,
reduce exercise
tolerance
Struct.
Heart
Disease
Develop
Symp.of
HF
Refract.
Symp.of
HF at rest
Stages in the evolution of HF and recommended therapy by stage
ACC/AHA Guidelines for the
Evaluation and Management of Chronic Heart Failure in the Adult 2001
EVOLUTION OF
CLINICAL STAGES
NORMAL
Asymptomatic
LV Dysfunction
Compensated
CHF
Decompensated
CHF
No symptoms
Normal exercise
Normal LV fxn
No symptoms
Normal exercise
Abnormal LV fxn
No symptoms
Exercise
Abnormal LV fxn
Symptoms
Exercise
Abnormal LV fxn
Refractory
CHF
Symptoms not controlled
with treatment
Evolution of the Concept of Heart Failure
1950 to 2000
1950 2000
Aetiology Hypertension CHD
Valvular heart dis Hypertension
Dilated CMP
Natural Course Slowly progressive Slowly progressive (remodelling)
or unpredictable and rapid
( coronary event )
Understanding Hemodynamic model Neurohormonal model
Common cause Pulmonary infection Sudden death
of death Pump failure
Arrhythmia Atrial Ventricular
Treatment goal Control edema Improve quality of life
Slowing Heart Rate + reduce mortality + reduce
hospitalization
Patophysiology of C H F
g
a b c d e f g a
AO
Aortic
closure
Aortic
pressure
Ventricular
pressure
Cross-
over
Atrial
pressure
MO
Heart
sounds
S
4
M
1
T
1
A
2
P
2 S
3
Cardiologic
systole
a
c
v
JVP
P
T
ECG
P
Q
S
0
800 msec
The Wiggers cycle
O
p
i
e
(
2
0
0
1
)
g
a
b
iso
c
d
iso
e
f
Input
Block diagram of left ventricular pump performance
(Little, 2001)
Output
PULMONARY VENOUS
PRESSURE
CARDIAC OUTPUT
Filling Emptying
ED volume
x
EF
effective
=
Stroke
volume
Heart
rate
x
Diastolic function Systolic function
LV Distensibility
Relaxation
Left atrium
Mitral valve
Pericardium
Contractility
Afterload
Preload
Structure
SYSTOLIC FAILURE
Normal
Normal
diastolic
chamber
distensibility
Left Ventricular Volume
L
e
f
t
V
e
n
t
r
i
c
u
l
a
r
P
r
e
s
s
u
r
e
Left Ventricular Volume
L
e
f
t
V
e
n
t
r
i
c
u
l
a
r
P
r
e
s
s
u
r
e
DIASTOLIC FAILURE
Decreased
diastolic
chamber
distensibility
PRESSURE VOLUME CURVE OF SYSTOLIC AND DIASTOLIC FAILURE
(Zile & Brutsaert 2002)
Abnormal
relaxation
A B
Pericardial
restraint
D
Chamber
dilation
C
Increased
chamber stiffness
L
e
f
t
v
e
n
t
r
i
c
u
l
a
r
p
r
e
s
s
u
r
e
Left ventricular volume
Mechanisms that cause diastolic dysfunction. (Zile, 1990)
DETERMINANTS OF
VENTRICULAR FUNCTION
STROKE
VOLUME
PRELOAD
CONTRACTILITY
CARDIAC OUTPUT
HEART
RATE
- Synergistic LV contraction
- LV wall integrity
- Valvular competence
AFTERLOAD
Frank-Starling Law
Normal
Compensated
CHF
Normal C.O.
LVEDP
C
a
r
d
i
a
c
O
u
t
p
u
t
Ventricular Function Curve:
Frank-Starlings
Congestion
SV
Normal
LVEDV
Factors That Influence Ventricular
Function Curves:
LVEDV
V
e
n
t
r
i
c
u
l
a
r
P
e
r
f
o
r
m
a
n
c
e
Contractile State of
the Myocardium
Cardiac
Glycosides
Catecholamines
Ca Channel
Blockers (?)
ETOH
Loss of
Myocardium
The Pathophysiology of Heart Failure
Hurst. The Heart. Diagnosis and Management of Heart Failure.10
th
ed. 688
Pathophysiological Sequence of
CHF
Heart Failure
Inadequate Cardiac Output
( ) O
2
Delivery (rest and/or exercise)
Systemic Vasoconstriction
SAS (NE)) RAAS (A-II)
() Flow to Skin, Gut,
and Renal Circulations
Activation of
RAS and ANS
Neurohormonal Activation
Hurst. The Heart. Diagnosis and Management of Heart Failure.10
th
ed. 688
Frank-Starling Effect
Ventricular dilatation
Wall stress
O2 consumption
Coronary
perfusion
SNS
Renin release
Angiotensin II
Vasoconstriction
Growth
factors
Hypertrophy
Apoptosis
ALDO
Fluid
accumulation
Collagen
deposition
Myofibril
necrosis
Preload Afterload
RBF
Renin release
Angiotensin II
Vasoconstriction
Growth
factors
Hypertrophy
Apoptosis
ALDO
Collagen deposition
Myofibril necrosis
Perfusion of Vital Organs
Na filtered
Afterload
Fluid accumulation
Sympathetic nervous system up-regulation
Increased
Norepinephrine levels
Direct
Myocardial toxicity
Myocyte dysfunction
Myocyte
necrosis
Intracellular
Ca
2+
overload/
Energy depletion
Apoptosis
Decreased
Renal blood
flow
Activation of the
RAA system
Increased HR, PVR &
arteriolar vasoconstriction
Increased myocardial
oxygen demand
Increased
Angiotensin II &
Aldosteron
Na
+
& water
retention
Vasoconstriction Cardiac remodeling
Cesario et.al; Reviews in cardiovascular medicine, vol 3, no.1, 2002
Causes of Heart Failure
Myocardial Damage or Disease
Infarction (Acute) / Ischemia
Myocarditis
Hypertrophic Cardiomyopathy
Excess Load on Ventricle
Volume/ Pressure Overload
Resistance to Flow into Ventricle
Cardiac Arrhythmias
Primary Changes in CHF
Site of
Failure
Backward
Failure
Forward
Failure
Right Heart
Failure
(
) Systemic
Venous
Pressure
(
) ejection
into
Pulmonary
Artery
Left Heart
Failure
(
) Pulmonary
Venous
Pressure
(
) ejection
into aorta
MI-INDUCED HEART FAILURE
Myocardial Damage
Contractility
Pump Performance
() SAS Drive
Vasoconstriction
() Systolic Work Load
RAAS SYSTEM
FLUID RETENTION
Diagnosis of C H F
IDENTIFICATIONS OF HF PATIENTS
With a Syndrome of Decrease Exercise
Tolerance
With a Syndrome of Fluid Retention
With No Symptoms or Symptoms of
Another Cardiac or Non Cardiac
Disorder
(MI, Arrythmias, Pulmonary or
Systemic Thromboembolic Events)
SYMPTOMS AND SIGN
Breathlessness, Ankle Swelling, Fatique
Characteristic Symptoms
Peripheral Oedema, JVP , Hepatomegaly
Signs of Congestion of Systemic Veins
S
3
, Pulmonary Rales , Cardiac Murmur
E C G
A low Predictive Value
LAH and LVH May Be Associated wit LV Dysfunction
Anterior Q-wave and LBBB a good predictors of EF
Detecting Arrhytmias as Causative of HF
CHEST X-RAY
A Part of Initial Diagnosis of HF
Cardiomegaly, Pulmonary Congestion
Relationship Between Radiological Signs and
Haemodynamic Findings may Depend on the Duration
and Severity HF
HAEMATOLOGY & BIOCHEMISTRY
A Part of Routine Diagnostic
Hb, Leucocyte, Platelets
Electrolytes, Creatinine, Glucose, Hepatic Enzyme,
Urinalysis
TSH, C-RP, Uric Acid
ECHOCARDIOGRAPHY
The Preferred Methods
Helpful in Determining the Aetiology
Follow Up of Patients Heart Failure
PULMONARY FUNCTIONS
A Little Value in Diagnosis Heart Failure
Usefull in Excluding Respiratory Diseases
EXERCISE TESTING
Focused on Functional, Treatment Assessment and
Prognostic
STRESS ECHOCARDIOGRAPHY
For Detecting Ischaemia
Viability Study
NUCLEAR CARDIOLOGY
Not Recommended as a Routine Use
CMR
( CARDIAC MAGNETIC RESONANCE IMAGING)
Recommenmded if Other Imaging Techniques not
Provided Diagnostic Answer
INVASIVE INVESTIGATION
Elucidating the Cause and Prognostic Informations
Coronary Angiography :
in CADs Patients
Haemodynamic Monitoring :
To Assess Diagnostic and Treatment of HF
Endomyocardial Biopsy :
in Patients with Unexplained HF
NATRIURETIC PEPTIDES
Cardiac Function (LV Function )
Plasma Natriuretic Peptide Concentration
(Diagnostic Blood Use for HF)
Natriuretic Peptide :
Greatest Risk of CV Events
Natriuretic Peptide :
Improve Outcome in Patients with
Treatment
Identify Pts. With Asymptomatic LV
Dysfunction (MI, CAD)
Suspected Heart Failure Because
of symptoms and signs
Assess Presence of Cardiac Disease by ECG, X-Ray
or NatriureticPeptides (Where Available)
Imaging by Echocardiography (Nuclear
Angiography or MRI Where Available)
Assess Etiology, Degree, Precipitating
Factors and Type of Cardiac Dysfunction
Tests Abnormal
Tests Abnormal
Choose Therapy
ALGORITHM FOR THE DIAGNOSIS OF THE HF
If Normal
Heart Failure
Unlikely
Additional Diagnosis Tests
Where Appropriate (e.g.
Coronary Angiography)
If Normal
Heart Failure
Unlikely
(ESC, 2001)
Treatment of C H F
Aims of Treatment
1. Prevention
a) Prevention and/or controlling of diseases leading
to cardiac dysfunction and heart failure
b) Prevention of progression to heart failure once
cardiac dysfunction is established
2. Morbidity
Maintenance or improvement in quality of life
3. Mortality
Increased duration of life
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
ACC/AHA & EUROPE (ESC) 2001
GUIDELINES FOR THE MANAGEMENT
OF HEART FAILURE
ACE-inhibitor
Use as first line therapy
Should be up titrated to the dosages shown in the large
clinical trial, and not titrated based on symptomatic
improvement
DIURETIC to control fluid overload
-BLOCKER
For all patients with stable mild-severe HF on
standard treatment
ACC/AHA & EUROPE (ESC) 2001
GUIDELINES FOR THE MANAGEMENT
OF HEART FAILURE
Aldosteron Receptor Antagonis
in advance HF ( NYHA III-IV )
DIGOXIN
in AF
May be added for symptom relief
ARB
Considered in patients not tolerate ACE
inhibitors and not on - blocker
Management Outline
Establish that the patient has HF.
Ascertain presenting features: pulmonary oedema, exertional
breathlessness, fatigue, peripheral oedema
Assess severity of symptoms
Determine aetiology of heart failure
Identify precipitating and exacerbating factors
Identify concomitant diseases
Estimate prognosis
Anticipate complications
Counsel patient and relatives
Choose appropriate management
Monitor progress and manage accordingly
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
TREATMENT
Correction of aggravating factors
MEDICATIONS
Endocarditis
Obesity
Hypertension
Physical activity
Dietary excess
Pregnancy
Arrhythmias (AF)
Infections
Hyperthyroidism
Thromboembolism
Treatment options
Non-pharmacological management
General advice and measures
Exercise and exercise training
Pharmacological therapy
Angiotensin-converting enzyme (ACE) inhibitors
Diuretics
Beta-adrenoceptor antagonists
Aldosterone receptor antagonists
Angiotensin receptor antagonists
Cardiac glycosides
Vasodilator agents (nitrates/hydralazine)
Positive inotropic agents
Anticoagulation
Antiarrhythmic agents
Oxygen
Devices and surgery
Revascularization (catheter interventions and surgery), other forms of surgery
Pacemakers
Implantable cardioverter defibrillators (ICD)
Heart transplantation, ventricular assist devices, artificial heart
Ultrafiltration, haemodialysis
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
DRUGS
HEMODYNAMIC EFFECTS
A
I
A + V
V
D
Ventricular Filling Pressure
Stroke
Volume
Normal
CHF
PHARMACOLOGIC THERAPY
DIURETICS
Improved
symptoms
Decreased
mortality
Prevention
of CHF
yes ?
?
Vasodil.(Nitrates)
yes yes
?
DIGOXIN
yes =
minimal
INOTROPES
yes mort.
?
Other neurohormonal
control drugs
yes
+ / -
?
ACEI yes YES
yes
Neurohumoral
Control
NO
yes
no
no
YES
YES
TREATMENT
Normal
Asymptomatic
LV dysfunction
EF <40%
Symptomatic CHF
NYHA II
Inotropes
Specialized therapy
Transplant
Symptomatic CHF
NYHA - IV
Symptomatic CHF
NYHA - III
Secondary prevention
Modification of physical activity
ACEI
Diuretics mild
Neurohormonal
inhibitors
Digoxin?
Loop
Diuretics
Pharmacological therapy
Stage A Stage B Stage C Stage D
Pts with :
Hypertension
CAD
DM
Cardiotoxins
FHx CM
THERAPY
Treat Hypertension
Stop smoking
Treat lipid disorders
Encourage regular
exercise
Stop alcohol
& drug use
ACE inhibition
Pts with :
Previous MI
LV systolic
dysfunction
Asymptomatic
Valvular disease
THERAPY
All measures under
stage A
ACE inhibitor
Beta-blockers
THERAPY
All measures under
stage A
Drugs for routine use:
diuretic
ACE inhibitor
Beta-blockers
digitalis
THERAPY
All measures under
stage A,B and C
Mechanical assist
device
Heart transplantation
Continuous IV
inotrphic infusions for
palliation
Pts who have
marked symptoms
at rest despite
maximal medical
therapy.
Pts with :
Struct. HD
Shortness of
breath and fatigue,
reduce exercise
tolerance
Struct.
Heart
Disease
Develop
Symp.of
HF
Refract.
Symp.of
HF at rest
Stages in the evolution of HF and recommended therapy by stage
ACC/AHA Guidelines for the
Evaluation and Management of Chronic Heart Failure in the Adult 2001
1. ACE INHIBITOR
Angiotensin-converting enzyme inhibitors
Recommended as first-line therapy.
Should be uptitrated to the dosages shown to be
effective in the large, controlled trials, and not
titrated based on symptomatic improvement.
Moderate renal insufficiency and a relatively low blood
pressure (serum creatinine 250 mol.l
-1
and systolic
BP 90 mmHg) are not contraindications.
Absolute contraindications: bilateral renal artery
stenosis and angioedema.
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
CO
PRELOAD AFTERLOAD
Normal Contractility
Diminished
Contractility
Normal Contractility
Diminished
Contractility
VV
AV
VASODILATOR DRUGS
PRINCIPLES
Venous
Vasodilatation
MIXED
Calcium antagonists
a-adrenergic Blockers
ACEI
Angiotensin II inhibitors
K
+
channel activators
Nitroprusside
VENOUS
Nitrates
Molsidomine
ARTERIAL
Minoxidil
Hydralazine
VASODILATORS
CLASSIFICATION
Arterial
Vasodilatation
VASOCONSTRICTION VASODILATATION
Kininogen
Kallikrein
Inactive Fragments
Angiotensinogen
Angiotensin I
RENIN
Kininase II
Inhibitor
ALDOSTERONE
SYMPATHETIC
VASOPRESSIN
PROSTAGLANDINS
tPA
ANGIOTENSIN II
BRADYKININ
ACEI
MECHANISM OF ACTION
A.C.E.
ACEI
HEMODYNAMIC EFFECTS
Arteriovenous Vasodilatation
- PAD, PCWP and LVEDP
- SVR and BP
- CO and exercise tolerance
No change in HR / contractility
MVO
2
Renal, coronary and cerebral flow
Diuresis and natriuresis
75
95
No
Additional
Treatment
Necessary
(%)
Quinapril Heart Failure Trial
J ACC 1993;22:1557
ACEI
FUNCTIONAL CAPACITY
Quinapril
continued
n=114
Quinapril
stopped
Placebo
n=110
p<0.001
100
90
85
80
Weeks
Class II-III
16 12 6 2 10 4 8 18 20 14
ACEI
ADVANTAGES
Inhibit LV remodeling post-MI
Modify the progression of chronic CHF
- Survival
- Hospitalizations
- Improve the quality of life
In contrast to others vasodilators,
do not produce neurohormonal activation
or reflex tachycardia
Tolerance to its effects does not develop
ACEI
UNDESIRABLE EFFECTS
Inherent in their mechanism of action
- Hypotension
- Hyperkalemia
- Angioneurotic edema
Due to their chemical structure
- Cutaneous eruptions
- Neutropenia,
thrombocytopenia
- Digestive upset
- Dry cough
- Renal Insuff.
- Dysgeusia
- Proteinuria
ACEI
CONTRAINDICATIONS
Renal artery stenosis
Renal insufficiency
Hyperkalemia
Arterial hypotension
Intolerance (due to side effects)
ACE-Inhibitors in Asymptomatic Heart Failure
Development of symptomatic HF
Hospitalization of HF
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
SAVE & TRACE Study
ACE-Inhibitors in Symptomatic Heart Failure
All patients symptomatic Heart Failure should receive ACE-I.
A) No fluid retention, ACE-I should be given first.
B) With fluid retention, ACE-I + Diuretic
ACE-I : A) improves survival and symptoms.
B) reduces hospitalization.
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
ACE INHIBITORS USED TO TREAT HEART FAILURE
DOSE RANGE TARGET DOSE FOR
DRUG (mg) FREQUENCY SURVIVAL BENEFIT*
Captopril 6.25 150 Three times daily 50 mg three times daily
Enalapril 2.5 20 Twice daily 10 mg twice daily
Lisinopril 2.5 40 Daily -
Ramipril 2.5 10 Once or twice daily 5 mg twice daily
Quinapril 5 20 Twice daily -
Zofenopril - - 30 mg twice daily
Trandolapril - - 4 mg daily
Imidapril HCl 5 10 Once daily 10 mg daily
* Target doses are those associated with increased survival in clinical trials
This drug is not approved in the United States
Placebo
Enalapril
12 11 10 9 8 7 6 5
PROBABILITY
OF
DEATH
MONTHS
0.1
0.8
0
0.2
0.3
0.7
0.4
0.5
0.6
p< 0.001
p< 0.002
CONSENSUS
N Engl J Med 1987;316:1429
ACEI SURVIVAL
4 3 2 1 0
50
40
30
20
10
0
Months
0 6 12
p = 0.30
24 18 30 36 42 48
Enalapril
n=2111
Placebo
n=2117
SOLVD (Prevention)
N Engl J Med 1992;327:685
%
MORTALITY
ACEI SURVIVAL
n = 4228
No CHF symptoms
EF < 35
50
40
30
20
10
0
Months
0 6 12
p = 0.0036
%
MORTALITY
24 18 30 36 42
48
Enalapril
n=1285
Placebo
n=1284
SOLVD (Treatment)
N Engl J M 1991;325:293
ACEI SURVIVAL
n = 2589
CHF
- NYHA II-III
- EF < 35
Mortality,
%
4
SAVE
N Engl J Med 1992;327:669
Years
30
20
10
0
1 2 3
Placebo
Captopril
0
n=1115
n=1116
p=0.019
-19%
ACEI SURVIVAL
n = 2231
3 - 16 days post AMI
EF < 40
12.5 --- 150 mg / day
Asymptomatic
ventricular
dysfunction post MI
ISIS-4
GISSI-3
SAVE
SMILE
AIRE
ACEI Benefit Pt Selection
Captopril
Lisinopril
Captopril
Zofenopril
Ramipril
0.5 / 5 wk
0.8 / 6 wk
4.2 / 3.5 yr
4.1 / 1 yr
6 / 1 yr
All with AMI
All with AMI
EF < 40
asymptomatic
Ant. AMI, No TRL
Clinical CHF
TRACE
Trandolapril 7.6 / 3 yr
Vent Dysfx / Clinical CHF
EF < 35
ACEI
SURVIVAL POST MI
2. DIURETICS
Diuretics
Essential for symptomatic treatment when
fluid overload is present and manifest.
Always be administered in combination
with ACE inhibitors if possible.
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
Cortex
Medulla
Thiazides
Inhibit active exchange of Cl-Na
in the cortical diluting segment of the
ascending loop of Henle
K-sparing
Inhibit reabsorption of Na in the
distal convoluted and collecting tubule
Loop diuretics
Inhibit exchange of Cl-Na-K in
the thick segment of the ascending
loop of Henle
Loop of Henle
Collecting tubule
DIURETICS
THIAZIDES
MECHANISM OF ACTION
Excrete 5 - 10% of filtered Na
+
Elimination of K
Inhibit carbonic anhydrase:
increase elimination of HCO
3
Excretion of uric acid, Ca and Mg
No dose - effect relationship
LOOP DIURETICS
MECHANISM OF ACTION
Excrete 15 - 20% of filtered Na
+
Elimination of K
+
, Ca
+
and Mg
++
Resistance of afferent arterioles
- Cortical flow and GFR
- Release renal PGs
- NSAIDs may antagonize diuresis
K-SPARING DIURETICS
MECHANISM OF ACTION
Eliminate < 5% of filtered Na
+
Inhibit exchange of Na
+
for K
+
or H
+
Spironolactone = competitive
antagonist for the aldosterone receptor
Amiloride and triamterene block
Na
+
channels controlled by aldosterone
Volume and preload
Improve symptoms of congestion
No direct effect on CO, but
excessive preload reduction may
Improves arterial distensibility
Neurohormonal activation
Levels of NA, Ang II and ARP
Exception: with spironolactone
DIURETIC EFFECTS
DIURETICS
ADVERSE REACTIONS
Thiazide and Loop Diuretics
Changes in electrolytes:
Volume
Na
+
, K
+
, Ca
++
, Mg
++
metabolic alkalosis
Metabolic changes:
glycemia, uremia, gout
LDL-C and TG
Cutaneous allergic reactions
DIURETICS
ADVERSE REACTIONS
Thiazide and Loop Diuretics
Idiosyncratic effects:
Blood dyscrasia, cholestatic jaundice and
acute pancreatitis
Gastrointestinal effects
Genitourinary effects:
Impotence and menstrual cramps
Deafness, nephrotoxicity
(Loop diuretics)
DIURETICS
ADVERSE REACTIONS
K-SPARING DIURETICS
Changes in electrolytes:
Na
+
, K
+
, acidosis
Musculoskeletal:
Cramps, weakness
Cutaneous allergic reactions :
Rash, pruritis
3. ALDOSTERONE
INHIBITORS
ALDOSTERONE
Retention Na
+
Retention H
2
O
Excretion K
+
Excretion Mg
2+
Collagen
deposition
Fibrosis
- myocardium
- vessels
Spironolactone
Edema
Arrhythmias
Competitive antagonist of the
aldosterone receptor
(myocardium, arterial walls, kidney)
ALDOSTERONE INHIBITORS
ALDOSTERONE INHIBITORS
INDICATIONS
FOR DIURETIC EFFECT
Pulmonary congestion (dyspnea)
Systemic congestion (edema)
FOR ELECTROLYTE EFFECTS
Hypo K
+
, Hypo Mg
+
Arrhythmias
Better than K
+
supplements
FOR NEUROHORMONAL EFFECTS
Please see RALES results,
N Engl J Med 1999:341:709-717
Recommended in advanced HF (NYHA III-IV),
in addition to ACE inhibition and diuretics to
improve survival and morbidity
Aldosterone receptor antagonists - spironolactone
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
The RALES mortality trial
Low dose spironolactone (12.550 mg) on top
of an ACE inhibitor and a loop diuretic
improved survival of patients in advanced
heart failure (NYHA class III or IV).
Aldosterone receptor antagonists - spironolactone
4. -Blockers
Start Low Go Slow
Activation and Blockade of Neurohumoral
System in CHF
RAA System SNS System
Angiotensin II Noradrenalin
Hypertrophy, apoptosis, ischaemia,
arrhytmia, remodeling, fibrosis
-Blocker ACE-I
ADRENERGIC ACTIVATION
CNS Sympathetic
Outflow
Sympathetic
activity to kidneys
& blood vessels
Cardiac
Sympathetic activity
1-receptors 2-receptors a1-receptors
Mycocyte hypertrophy & death,
dilatation, ischaemia & arrhytmias
Vasoconstriction
Sodium Retention
Packer, AHA 2000
Why add-on -blocker,
if HF patient is already stable
on standard therapy with
ACE-I, diuretics digoxin
?
Carvedilol
(n=696)
Placebo
(n=398)
Survival
Days
0 50 100 150 200 250 300 350 400
1.0
0.9
0.8
0.7
0.6
0.5
Risk reduction = 65%
P<0.001
Packer et al (1996)
Lancet (1999)
0 200 400 600 800
1.0
0.8
0.6
0
Bisoprolol
Placebo
Time after inclusion (days)
P<0.0001
Survival
Risk reduction = 34%
The MERIT-HF Study Group (1999)
Months of follow-up
Mortality %
0 3 6 9 12 15 18 21
20
15
10
5
0
Placebo
Metoprolol CR/XL
P=0.0062
Risk reduction = 34%
US Carvedilol Study
-Blockers in CHF -
All-cause Mortality
CIBIS-II MERIT-HF
Benefits of Add-on -Blocker
Short-term :
1. Improvement of symptoms (LVEF )
2. Improvement of NYHA class
3. Improvement of daily activities
4. Reduction of hospitalization rate & length of
hospital stay (financial & psychological burden)
Long-term :
1. Slowing the progression of CHF
2. Increase of survival rate
A Clear Dose-Effect Relationship
(MOCHA Study)
Plc
0
1
2
3
4
5
6
7
8
LVEF (EF Units)
*
25 6.25 12.5
*
* *
mg bid
P < 0.001
- 30
0
30
60
90
*
*
*
mg bid
Plc
6.25
*
*
*
%
w
o
r
s
e
%
i
m
p
r
o
v
e
d
12.5 25
0
0.1
0.2
0.3
0.4
Hospitalization/Pts
* *
*
* *
P = 0.01
Plc 25 6.25 12.5 mg bid
0
4
8
12
16
Mortality (%)
* * *
* *
P < 0.001
Plc 25 6.25 12.5 mg bid
B
r
i
s
t
o
w
e
t
a
l
(
1
9
9
6
)
Patient Global Assessment
%
S
u
r
v
i
v
a
l
0
0
3 6 9 12 15 18 21
Months
100
90
80
60
70
P=0.00013
Carvedilol
Placebo
COPERNICUS
All-cause mortality
Favors treatment Favors placebo
0.5 0.25 0.75 1.25 1.0
All
patients
Recent or
recurrent
decompensation
Annual placebo mortality rate
(per patient-year)
19.7%
28.5%
0
Effect of carvedilol on mortality
COPERNICUS
Recommended for the treatment of all pts
with stable, mild, moderate and severe heart
failure on standard treatment, unless there is
a contraindication.
Patients with LV systolic dysfunction, with or
without symptomatic HF, following an AMI
long-term betablockade is recommended
in addition to ACE inhibitor.
Beta-adrenoceptor antagonists
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
Beta-adrenoceptor antagonists
CIBIS II, MERIT HF, US CARVEDILOL AND
COPERNICUS study
Reduction in total mortality, cardiovascular
mortality, sudden death and death due to
progression of heart failure in patients in func.
class II-IV.
reduces hospitalizations
improves the functional class and leads to
less worsening of heart failure.
PHARMACOLOGICAL PROPERTIES OF
-BLOCKING AGENT FOR HF
AGENT
1-
BLOKADE
2-
BLOKADE
a-
BLOKADE
ISA
ANCILLARY
EFFECTS
Carvedilol
+ + +
+ + +
+ + +
-
+ + +
Metoprolol
+ + +
-
-
-
-
Bisoprolol
+ + +
-
-
-
-
THE RECOMMENDED PROCEDURE FOR
STARTING -BLOCKER
1. Patient should be on standard therapy
(ACE inhibitor +/- diuretic)
2. Patient in stable conditions
No iv inotropic therapy
Without signs of marked fluid retention
3. Start initial low doses and titrate to maintenance dose
(the dose may be doubled every 1 2 weeks)
(ESC.Guidelines for HF, 2001)
DOSES OF -BLOCKER
BLOCKER FIRST DOSE TARGET DOSE TITRATION
PERIOD
Bisoprolol 1.25 mg 10 mg Weeks Month
Metoprolol
Tartrate
5 mg 150 mg Weeks Month
Metoprolol
Succinate
12.5 mg 200 mg Weeks Month
Carvedilol 2 x 3.125 mg 2 x 25 mg Weeks Month
(European Heart J ournal, vol. 22, Sept. 2001)
CONTRAINDICATIONS OF
-BLOCKER IN PATIENT H F
Asthma Bronchial
Severe Bronchial Desease
Symptomatic Bradycardia and
Hypotension
INTOLERANCE OF -BLOCKER
Symptomatic
Bradycardia
Worsening HF Hypotension
How to Handle Intolerance
SYMPTOMATIC BRADYCARDIA
Check Blood Digoxin and/or reduce
other AV nodus inhibiting drugs
Reduces -Blocker dose
or if necessary stop it
Consider implantation of
peacemaker
How to Handle Intolerance
WORSENING HF
Increase dose of Diuretics
Reduces -Blocker dose
or if necessary stop it
If indicated, give inotropic drugs or
nitroprusside or nitroglycerin
How to Handle Intolerance
HYPOTENSION
Reduces ACE-I or
vasodilator
Take -Blocker :
After meal
At different time than ACE-I
Reduces dose or if necessary stop it
-BLOCKER IN HIGH RISK GROUPS PTS
WITH CHF
Elderly Patient
Type 2 Diabetes Mellitus
Renal Failure
Digitalis / Aldosteron Antagonist /
Amiodaron
(Post-Hoc Analysis of the CIBIS II)
5. Angiotensin II receptor
antagonists
ANGIOTENSIN II INHIBITORS
MECHANISM OF ACTION
RENIN
Angiotensinogen Angiotensin I
ANGIOTENSIN II
ACE
Other paths
Vasoconstriction
Proliferative
Action
Vasodilatation
Antiproliferative
Action
AT1 AT2
AT1
RECEPTOR
BLOCKERS
RECEPTORS
AT1 RECEPTOR BLOCKERS
DRUGS
Losartan
Valsartan
Irbersartan
Candesartan
Competitive and selective
blocking of AT1 receptors
ARBs could be considered in patients who do not
tolerate ACE inhibitors for symptomatic
treatment.
It is unclear whether ARBs are as effective as
ACE inhibitors for mortality reduction.
In combination with ACE inhibition, ARBs may
improve heart failure symptoms and reduce
hospitalizations for worsening heart failure.
Angiotensin II receptor antagonists
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
VAL-H
Patients were randomized to placebo or
valsartan on top of standard therapy.
The results showed no difference in overall
mortality, but a reduction in the combined end-
point all-cause mortality or morbidity
expressed as hospitalization because of
worsening heart failure.
Angiotensin II receptor antagonists
6. Cardiac glycosides
Na
+
K
+
K
+
Na
+
Na
+
Ca
++
Ca
++
Na-K ATPase
Na-Ca Exchange
Myofilaments
DIGOXIN
CONTRACTILITY
DIGOXIN
PHARMACOKINETIC PROPERTIES
Oral absorption (%)
Protein binding (%)
Volume of distribution (l/Kg)
Half life
Elimination
Onset (min)
i.v.
oral
Maximal effect (h)
i.v.
oral
Duration
Therapeutic level (ng/ml)
60 - 75
25
6 (3-9)
36 (26-46) h
Renal
5 - 30
30 - 90
2 - 4
3 - 6
2 - 6 days
0.5 - 2
DIGOXIN
DIGITALIZATION STRATEGIES
(mg)
0.125-0.5 / d
0.25 / d
i.v
0.5 + 0.25 / 4 h
ILD: 0.75-1
oral 12-24 h
0.75 + 0.25 / 6 h
1.25-1.5
oral 2-5 d
0.25 / 6-12 h
1.5-1.75
Loading dose (mg)
Maintenance
Dose
ILD = average INITIAL dose required for
digoxin loading
DIGOXIN
HEMODYNAMIC EFFECTS
Cardiac output
LV ejection fraction
LVEDP
Exercise tolerance
Natriuresis
Neurohormonal activation
DIGOXIN
NEUROHORMONAL EFFECTS
Plasma Noradrenaline
Peripheral nervous system activity
RAAS activity
Vagal tone
Normalizes arterial baroreceptors
%
WORSENING
OF CHF
p = 0.001 DIGOXIN: 0.125 - 0.5 mg /d
(0.7 - 2.0 ng/ml)
EF < 35%
Class I-III (digoxin+diuretic+ACEI)
Also significantly decreased exercise
time and LVEF.
DIGOXIN
EFFECT ON CHF PROGRESSION
RADIANCE
N Engl J Med 1993;329:1
Placebo n=93
DIGOXIN
Withdrawal
DIGOXIN n=85
30
10
0
20
100 80 20 0 40 60
Days
50
40
30
20
10
0
Placebo
n=3403
DIGOXIN
n=3397
48 0 12 24 36
OVERALL MORTALITY
%
DIG
N Engl J Med 1997;336:525
Months
p =0.8
DIGOXIN
LONG TERM EFFECTS
Survival similar to placebo
Fewer hospital admissions
More serious arrhythmias
More myocardial infarctions
DIGOXIN
CLINICAL USES
AF with rapid ventricular response
CHF refractory to other drugs
Other indications?
Can be combined with other drugs
DIGOXIN
CONTRAINDICATIONS
ABSOLUTE:
- Digoxin toxicity
RELATIVE
- Advanced A-V block without pacemaker
- Bradycardia or sick sinus without PM
- PVCs and TV
- Marked hypokalemia
- W-P-W with atrial fibrillation
DIGOXIN TOXICITY
CARDIAC MANIFESTATIONS
ARRHYTHMIAS :
- Ventricular (PVCs, TV, VF)
- Supraventricular (PACs, SVT)
BLOCKS:
- S-A and A-V blocks
CHF EXACERBATION
DIGOXIN TOXICITY
EXTRACARDIAC MANIFESTATIONS
GASTROINTESTINAL:
- Nausea, vomiting, diarrhea
NERVOUS:
- Depression, disorientation, paresthesias
VISUAL:
- Blurred vision, scotomas and yellow-green
vision
HYPERESTROGENISM:
- Gynecomastia, galactorrhea
indicated in atrial fibrillation and any degree of
symptomatic heart failure.
A combination of digoxin and beta-blockade
appears superior than either agent alone.
In sinus rhythm, digoxin is recommended to
improve the clinical status of patients with
persisting heart failure despite ACE inhibitor and
diuretic treatment.
Cardiac glycosides
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
DIG trial
Long-term digoxin did not improve survival.
The primary benefit and indication for digoxin
in heart failure is to reduce symptoms and
improve clinical status decrease the risk of
hospitalization for heart failure without an
impact on survival.
Cardiac glycosides
7. Vasodilator agents
No specific role for vasodilators in the treatment of HF
Used as adjunctive therapy for angina or concomitant
hypertension.
In case of intolerance to ACE inhibitors ARBs are
preferred to the combination hydralazinenitrates.
HYDRALAZINE-ISOSORBIDE DINITRATE
Hydralazine (up to 300 mg) in combination with ISDN (up to 160
mg) without ACE inhibition may have some beneficial effect on
mortality, but not on hospitalization for HF.
Nitrates may be used for the treatment of concomitant angina or
relief of acute dyspnoea.
Vasodilator agents in chronic heart failure
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
8. Positive inotropic therapy
CARDIAC GLYCOSIDES
SYMPATHOMIMETICS
Catecholamines
-adrenergic agonists
PHOSPHODIESTERASE INHIBITORS
Amrinone
Enoximone
Others
Milrinone
Piroximone
POSITIVE INOTROPES
-ADRENERGIC STIMULANTS
CLASSIFICATION
B
1
Stimulants
Increase contractility
Dobutamine Doxaminol Xamoterol
Butopamine Prenalterol Tazolol
B
2
Stimulants
Produce arterial vasodilatation and reduce SVR
Pirbuterol
Carbuterol
Rimiterol
Fenoterol
Tretoquinol
Salbutamol
Terbutaline
Salmefamol
Soterenol
Quinterenol
Mixed
Dopamine
DOPAMINE AND DOBUTAMINE
EFFECTS
Receptors
Contractility
Heart Rate
Arterial Press.
Renal perfusion
Arrhythmia
DA (g / Kg / min) Dobutamine
< 2
DA
1
/ DA
2
++
-
2 - 5
1
++
+
+
+
> 5
1
+ a
++
++
++
++
1
++
++
+
POSITIVE INOTROPES
CONCLUSIONS
May increase mortality
Safer in lower doses
Use only in refractory CHF
NOT for use as chronic therapy
Commonly used to limit severe episodes of
HF or as a bridge to heart transplantation
in end-stage HF.
Repeated or prolonged treatment with oral
inotropic agents increases mortality.
Currently, insuffcient data are available to
recommend dopaminergic agents for heart
failure treatment.
Positive inotropic therapy
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
POSITIVE INOTROPHIC AGENTS
Dobutamin
Milrinone
Levosimendan
DOPAMINERGIC AGENTS
Ibopamine is not recommended for the treatment of
chronic HF due to systolic LV dysfunction.
Intravenous dopamine is used for the sort-term
correction of haemodynamic disturbances of severe
episodes of worsening HF.
Positive inotropic therapy
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
9. Antiarrhythmics
ANTIARRHYTHMICS
Sustained VT, with/without symptoms
- Blockers
- Amiodarone
Sudden death from VF
- Consider
implantable
defibrillator
ANTIARRHYTHMICS
MORTALITY
EMIAT
Am Coll Cardiol 1996
13.6
13.7
Placebo Amiodarone
0
5
10
15
101 / 743
102 / 743
MORTALITY
AT 2 YEARS
%
n=1486
5-21d post MI
Amiodarone
200 mg/d
Follow up 1 - 4 years
ns
No indication for the use of antiarrhythmic agents in HF
Indications for antiarrhythmic drug therapy include AF
(rarely flutter), non-sustained or sustained VT.
CLASS I ANTIARRHYTHMICS
should be avoided
CLASS II ANTIARRHYTHMICS
Beta-blockers reduce sudden death in heart failure
CLASS III ANTIARRHYTHMICS
Amiodarone is the only antiarrhythmic drug without
clinically relevant negative inotropic effects.
Antiarrhythmics
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
10. Anticoagulation
11. Antiplatelet Drugs
ANTICOAGULANTS
PREVIOUS EMBOLIC EPISODE
ATRIAL FIBRILLATION
Identified thrombus
LV Aneurysm (3-6 mo post MI)
Class III-IV in the presence of:
- EF < 30
- Aneurysm or very dilated LV
Phlebitis
Prolonged bed rest
Recommendation
1. All pts with HF and AF should be treated with
warfarin unless contraindicated.
2. Patients with LVEF 35% or less.
Anticoagulation
HFSA Guidelines for Management of Patients With Heart Failure Caused by Left
Ventricular Systolic Dysfunction - Pharmacological Approaches 2000
Antiplatelet Drugs
Recommendation
There is insufficient evidence concerning the
potential negative therapeutic interaction
between ASA and ACE inhibitors.
Antiplatelet agent for pts with HF who have
underlying CAD.
HFSA Guidelines for Management of Patients With Heart Failure Caused by Left
Ventricular Systolic Dysfunction - Pharmacological Approaches 2000
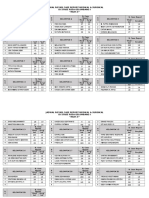
Chronic heart failure choice of
pharmacological therapy
LV systolic dysfunction ACE inhibitor Diuretic Beta-blocker
Aldosterone
Antagonist
Asymptomatic LV
dysfunction
Indicated Not indicated Post MI Not indicated
Symptomatic HF (NYHA II) Indicated
Indicated if
Fluid retention
Indicated Not indicated
Worsening HF (NYHA III-IV) Indicated
Indicated
comb. diuretic
Indicated
Indicated
End-stage HF (NYHA IV) Indicated
Indicated
comb. diuretic
Indicated
Indicated
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
A
Chronic heart failure choice of
pharmacological therapy
LV systolic dysfunction
Angiotensin
II receptor
antagonists
Cardiac glycosides
Vasodilator
(hydralazine/
isosorbide
dinitrate)
Potassium -sparing
diuretic
Asymptomatic LV
dysfunction
Not indicated With AF Not indicated Not indicated
Symptomatic HF (NYHA II)
If ACE inhibitors
are not tolerated
and not on beta-
blockade
(a) when AF
(b) when improved
from more severe
HF in sinus
rhythm
If ACE inhibitors
and angiotensin
II antagonists
are not
tolerated
If persisting
hypokalaemia
Worsening HF (NYHA III-IV)
If ACE inhibitors
are not tolerated
and not on beta-
blockade
indicated
If ACE inhibitors
and angiotensin
II antagonists
are not
tolerated
If persisting
hypokalaemia
End-stage HF (NYHA IV)
If ACE inhibitors
are not tolerated
and not on beta-
blockade
indicated
If ACE inhibitors
and angiotensin
II antagonists
are not
tolerated
If persisting
hypokalaemia
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
B
Intervention
Pts with heart failure of ischaemic origin revascularization
symtomatic improvement.
A strong negative correlation of operative mortality and LVEF,
a low LVEF (<25%) was associated with increased
operative mortality. Advance HF symptoms (NYHA IV)
resulted in a greater mortality rate.
Off pump coronary revascularization may lower the surgical
risk for HF.
Heart Transplantation is an accepted mode of treatment for
end-stage HF.
Revascularization
Surgical
Non Surgical
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
Care and Follow-up
Recommended components of programs
use a team approach
vigilant follow-up, first follow-up within 10 days of
discharge
discharge planning
increased access to health care
optimizing medical therapy with guidelines
intense education and counselling inpatient and
outpatient
strategies address barriers to compliance
early attention to signs and symptoms
flexible diuretic regimen
Guidelines for the diagnosis and treatment of chronic heart failure
European Heart Journal (2001) 22, 1527-1560
Future treatment
1. Sympathetic nervous system
2. The RAA system
3. Atrial and brain natriuretic peptides
4. Arginin vasopressin
5. Endothelin
6. Growth hormone
7. Calcitonin gene related peptide
Neurohormonal modulation
Cardiac reparation: fixing the heart
with cells, new vessels and genes (1)
1. Multiplication of residual myocytes
(forcing the cells to enter mytotic cycle)
2. Transforming fibrablasts in the scar
3. Implanting exogenous contractiles cells
(foetal cardiomyocites, skeletal
myoblasts, stem cells)
Aims: to repopulate fibrous scars with new
contractile cells
Cell based
interventions
Eur Heart J 2002;4: D73-81
CONT (2)
1. Administration of angiogenic growth factors
VEGF, basic FGF
2. Problems: nature of compound , dose,
route, and adverse events (abnormal blood
vessels, proliferative retinopathy, etc)
Angiogenesis
Aims: to provides new blood supply to
the diseased heart
Eur Heart J 2002;4: D73-81
CONT(3)
1. Gene manipulation of 3 majors areas: Ca
handling, beta-adenergic signalling and
apoptosis
2. Inducing expression of silent genes
Gene therapy
Aims: to improve the function of the failing
heart
Safety problems: control of targeted protein
expression, inflammation, autoimmunity
and oncogenesis (basically irreversible)
Eur Heart J 2002;4: D73-81
Dual-chamber pacemakers are
beneficial
Drug-resistant CHF
Intact sinus rhythm
Absence of chronic atrial dysrhythmias
EF <20%
Viable myocardium
No or stable angina
DMC and PR >, MR and TR, QRS >, QRS
PR + QRS > 350 ms.
QRS >140 ms, MR > 450 ms, and LV filling
time <200 ms
HOCM
Cardiac resynchronization
therapy
Reason:
Patients with CHF frequently exhibited
QRS prolongation with disease
progression. The delayed ventricular
activation leads to asynchronous
ventricular contraction with negative
effects on LV performance
Aim:
To normalize AV activation sequence
and disturbed ventricular contraction
patterns
Cardiac resynchronization
therapy
Study
NYHA QRS (ms) EF (%)
0 mo 3 mo 0 mo 3 mo 0 mo 3 mo
Path-CHF
(n=42)
3.0 2.0 - - - -
In Sync
(n=81)
3.4 2.2 179 143 21 24
Alouco
(n=26)
3.3 2.0 179 159 - -
MUSTIC
(n=67)
- - 176 - 23 -
J Inv Cardiol 2002; 14: 48-53
Resume
Pharmacological Treatment :
I. Asymptomatic Systolic LV dysfunction :
ACE Inhibitor
-Blocker (in CAD)
II. Symptomatic Systolic LV dysfunction
A. No fluid retention
ACE Inhibitor
-Blocker
If ischaemia (+) nitrate / revascularization
B. Fluid retention
Diuretic
ACE Inhibitor (ARBs if not tolerated)
-Blocker
Digitalis
Resume
III. Worsening HF
Standard treatment : ACE Inhibitor, -Blocker
Diuretic : doses + loop diuretic
Low dose spironolactone
Digitalis
Consider :
Revascularization
Valve surgery
Heart transplant
IV. End-stage HF
Intermittent inotrophic support
Circulatory support (IABP, Ventr.Assist Devices)
Haemofiltration on dialysis
briddging to heart transplantation
Conclusion
Management of HF must be starting from
the earlier stage (AHA/ACC stage A).
Treatment at each stage can reduce
morbidity and mortality.
Before initiating therapy :
Established the correct diagnose.
Consider management outline.
Conclusion
Non pharmacolgical intervention are helpfull in :
improving quality of life
reducing readmission
lowering cost.
Organize multi-disciplinary care :
HF clinic, HF nurse specialist, pts telemonitoring.
Health care system.
To optimize HF management
Treatment should be according to the Guidelines,
intensive education, and behavioral change efforts.
Thank YoU
DIASTOLIC HEART
FAILURE
SCOPE OF THE PROBLEM
Epidemiological studies of HF have
suggested that 30-50% of cases of HF
have preserved LV systolic function.
DHF has mortality rate equal as
systolic heart failure
No guideline yet regarding the
treatment of DHF
Greenberg & Hermann 2004
Defining Diastolic Heart Failure
Diastolic dysfunction refers to a condition in which
abnormalities in mechanical function are presenting
during diastole.
Diastolic dysfunction is a condition in which higher
than normal LV filling pressure are needed to maintain
a normal cardiac output.
Diastolic heart failure is a clinical syndrome
characterized by the symptoms and signs of heart
failure, a preserved EF and abnormal diastolic
function.
(Vasan & Levy 2000)
Normal diastolic
function
Mild diastolic
dysfunction
Pseudonormal
stage
Restrictive-
filling stage
Left ventricular relaxation Normal
Left ventricular stiffness Normal
Left atrial contractility Normal Normal
Preload Normal Normal
Electrocardiogram
Mitral flow
Pulmonary venous
flow
E wave
A wave
QRS
T
P
Diastole
Systole
Atrial reversal
Echo-Doppler and Diastolic Dysfunction
( Garcia, 2000 )
Diastolic Heart Failure : Effects of
Age on Prevalence and Prognosis
Age, y
<50 50-70 >70
Prevalence 15 33 50
Mortality 15 33 50
Morbidity 25 50 50
( Zile & Brutsaert, 2002 )
CHARACTERISTICS
Age
Sex
Left ventricle EF
Left ventricle cavity size
LVH on echo
Chest radiography
Gallop rhythm present
Coexisting conditions
Hypertension
Diabetes mellitus
Previous MCI
Obesity
Chronic lung disease
Sleep apnea
Long term dialysis
Atrial fibrillation
DIASTOLIC HEART
FAIURE
Frequently elderly
Frequently female
Preserved or normal (+ > 40%)
Usually normal,often LVH
concentric
Usually present
Congestion with/out cardiomegali
Fourth heart sound
+++
+++
+
+++
++
++
++
+
Usually paroxismal
SYSTOLIC HEART
FAILURE
All ages,typically 50-70 yr
More often male
Depressed,+ < 40%
Usually dilated
Sometimes present
Congestion & cardiomegali
Third heart sound
++
++
+++
+
0
++
0
+
Usually persistent
(NEJM 2003)
Conditions Associated with Diastolic
Dysfunction
Condition
Coronary artery disease
Hypertensive heart disease
Valvular heart disease
Normal aging
Hypertrophic cardiomyopathy
Infiltrative disease of the
myocardium
(amyloid,sarcoid,haemocromatosis,
lympoma)
Possible Contributory Mechanism :
Asynchronous myocardial relaxation
secondary,to ischemia or scar and
altered mechanical loading
LVH
AS leading to LVH , MS leading to reduced
filling
Impaired early filling due to reduced
compliance with associated increase in late
filling
Hypertrophy,fibrosis, and asynchronous
regional lengthening, hence impaired
relaxation.
Reduced LVED distensibility (increased
LVEDP)
(Vasan & Levy 1998)
(Mandinov,Eberli,Seiler,Hess.Cardiosvasc Res 2000)
Diagnostic Criteria for Diastolic Heart Failure
( European Study Group on DHF, 1998 )
Signs or symptoms of congestive heart failure
Exertional dyspnoea [eventually objective evidence by reduced peak exercise oxygen consumption
(<25 ml.kg
-1
.min
-1
)], orthopnea, gallop sounds, lung crepitations, pulmonary oedema
and
Normal or mildly reduced left ventricular systolic function:
LVEF45% and LVEDIDI<3.2 cm.m
-2
or LVEDVI<102 ml.m
-2
and
Evidence of abnormal left ventricular relaxation, filling, diastolic distensibility and diastolic stiffness:
Slow isovolumic left ventricular relaxation:
LVdP/dt
min
<1100 mmHg.s
-1
and/or IVRT
<30y
>92 ms, IVRT
30-50y
>100 ms, IVRT
>50y
>105 ms
and/or >48 ms
and/or slow early left ventricular filling:
PFR<160 ml.s
-1
.m
-2
and/or PFR
<30y
<2.0 EDV.s
-1
, PFR
30-50y
<1.8 EDV.s
-1
, PFR
>50y
<1.6 EDV.s
-1
and/or E/A
<50y
<1.0 and DT
<50y
>220 ms, E/A
>50y
<0.5 and DT
>50y
>280 ms
and/or S/D
<50y
>1.5, S/D
>50y
>2.5
and/or reduced left ventricular diastolic distensibility:
LVEDP>16 mmHg or mean PCW>12 mmHg
and/or PV A Flow > 35 cm.s
-1
and/or PV A t>MV A t+ 30 ms
and/or A/H>0.20
and/or increased left ventricular chamber or muscle stiffness:
b>0.27
and/or b>16
Criteria for Definite DHF
Criterion Objective Evidence
Definite evidence of CHF
AND
Objective evidence of normal LV
systolic function in proximity to
the CHF event
AND
Objective evidence of LV diastolic
dysfunction
Includes clinical symptoms and signs, supporting
laboratory tests (such as chest X-ray), and a typical
clinical response to treatment with diuretics, with or
without documentation of elevated LV filling pressure
(at rest, on exercise, or in response to a volume load)
or a low cardiac index
Abnormal LV relaxation /filling/distensibility indices on
cardiac catheterization
LV EF > 0.50 within 72 h of event
( Vasan & Levy, 2000 )
Criteria for Probable DHF
Criterion Objective Evidence
Definitive evidence of CHF
Objective evidence of normal LV systolic
function in proximity to the CHF event
Objective evidence of LV diastolic
dysfunction is lacking
AND
BUT
Includes clinical symptoms and signs, supporting laboratory tests
(such as chest X-ray), and a typical clinical response to treatment
with diuretics, with or without documentation of elevated LV filling
pressure (at rest, on exercise, or in response to a volume load) or a
low cardiac index
LV EF > 0.50 within 72 h of CHF event
No conclusive information on LV diastolic function
Criteria for Possible DHF
Criterion Objective Evidence
Definitive evidence of CHF
Objective evidence of normal LV systolic
function, but not at the time of the CHF event
Objective evidence of LV diastolic dysfunction
is lacking
Includes clinical symptoms and signs, supporting laboratory test (such
as chest X-ray), and a typical clinical response to treatment with
diuretics, with or without documentation of elevated LV filling pressure
(at rest, on exercise, or in response to a volume load) or a low cardiac index
LV EF > 0.50
No conclusive information on LV diastolic function
AND
AND
( Vasan & Levy, 2000 )
Other Methods in diagnosing DHF
Plasma Brain Natriuretic Peptide
Doppler tissue imaging
Magnetic resonance imaging
Radionuclide angiography
Cardiac catheterization
Greenberg & Hermann 2004
Treatment of Diastolic Heart Failure
Clinical investigations in relatively small
groups of patients
Clinical experience
Concepts based on pathophysiology
mechanisms
The guidelines are based on :
Treatment of Diastolic Heart failure
symptom targeted treatment
disease / pathological targeted treatment
the underlying mechanism targeted
treatment
( Zile & Brutsaert, 2002 )
Diastolic Heart Failure: Treatment
Symptom targeted treatment
Decrease pulmonary venous pressure
Reduce LV volume
Maintain atrial contraction
Prevent tachycardia
Improve exercise tolerance
Use positive inotropic agents with caution
( Zile & Brutsaert, 2002 )
Diastolic Heart Failure: Treatment
Nonpharmacological treatment
Restrict sodium to prevent volume overload
Restrict fluid to prevent volume overload
Perform moderate aerobic exercise to improve cardiovascular
conditioning, decrease heart rate and maintain skeletal muscle
function
Pharmacological treatment
Diuretics including loop diuretics thiazides, spironolactone
Long-acting nitrates, -Adrenergic blockers
Calcium channel blockers
Renin angiotensin-aldosterone antagonists including ACE
inhibitors, angiotensin II receptor blockers and aldosterone
antagonists
Symptom targeted treatment
( Zile & Brutsaert, 2002 )
Disease-targeted treatment
Prevent/treat myocardial ischemia
Prevent/regress ventricular hypertrophy
Mechanisms targeted treatment
Modify myocardial and extramyocardial mechanisms
Modify intracellular and extracellular mechanisms
An ideal therapeutic agent.
- Should target the underlying mechanisms
- Improve calcium homeostasis and energetics
- Blunt neurohumoral activation
- Prevent and regress fibrosis
Diastolic Heart Failure
( Zile & Brutsaert, 2002 )
Trials of Diastolic Heart Failure
Trial
Comparison
Follow-up (n)
Diagnostic Criteria
for DHF
Other Important
Inclusion/ Exclusion
Criteria
Main Outcomes
PEP-CHF
CHARM-2
I-PRESERVE
SENIORS
(diastolic subset)
Hong Kong
SWEDIC
Placebo
Perindopril
Placebo
Candesartan
Placebo
Irbesartan
Placebo
Nebivolol
Placebo
Ramipril
Irbesartan
Placebo
Carvedilol
1.000
Minimum 18 months
2.500
Minimum 24 months
3.600
Approx 48 months
2.000
(% DHF uncertain)
450
Minimum 12 months
140
9 months
3 of 9 clinical and
2 of 4 echocardiographic
criteria
EF > 40%
EF > 45%
EF > 35% and a cardiac
abnormality
Doppler criteria
Doppler criteria
Age > 70 years
Diuretics
Hospital admission in last
3 months
None
Clinical diagnosis of HF
Aged > 70 years
Hospital admission within
last 12 months
Diuretics
AF excluded
Death or HF-related
hospitalization
Death or hospitalization
for HF
Death and hospitalization
cardiovascular disease
Death or hospitalization
for HF
Quality of life 6-minute
walk test
Regression of diastolic
dysfunction
( Banerjee, et.al, 2002)
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Cardiovascular Physiology Concepts Klabu PDFDokumen257 halamanCardiovascular Physiology Concepts Klabu PDFJer100% (4)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Physiology Summary Chapter 20Dokumen9 halamanPhysiology Summary Chapter 20gail01850% (2)
- Heart Failure Pathophysiology GuideDokumen74 halamanHeart Failure Pathophysiology GuidetoobstudyingBelum ada peringkat
- Pathophysiology of Heart Failure With Reduced Ejection Fraction - Hemodynamic Alterations and Remodeling - UpToDateDokumen29 halamanPathophysiology of Heart Failure With Reduced Ejection Fraction - Hemodynamic Alterations and Remodeling - UpToDatesamBelum ada peringkat
- Pathways CKDDokumen2 halamanPathways CKDlianBelum ada peringkat
- Pathway CKDDokumen1 halamanPathway CKDocsitaocsitulBelum ada peringkat
- PathwayDokumen4 halamanPathwayocsitaocsitulBelum ada peringkat
- Management and Prevention of Upper GI BleedingDokumen0 halamanManagement and Prevention of Upper GI Bleedingbasinang_jangil100% (1)
- Pocketbook FarmakoDokumen106 halamanPocketbook FarmakoocsitaocsitulBelum ada peringkat
- Anak Leukemia 5985 17627 1 SMDokumen4 halamanAnak Leukemia 5985 17627 1 SMocsitaocsitulBelum ada peringkat
- Effect of Toys and Preoperative Visit On Reducing Children's Anxiety and Their Parents Before Surgery and Satisfaction With The Treatment ProcessDokumen8 halamanEffect of Toys and Preoperative Visit On Reducing Children's Anxiety and Their Parents Before Surgery and Satisfaction With The Treatment ProcessocsitaocsitulBelum ada peringkat
- JADWAL Case Report Part ADokumen6 halamanJADWAL Case Report Part AocsitaocsitulBelum ada peringkat
- GINA Pocket 2014 Jun11Dokumen32 halamanGINA Pocket 2014 Jun11Gilbert Petrus Richard SamsBelum ada peringkat
- HIPERTENSI & Hipertesni KrisisDokumen64 halamanHIPERTENSI & Hipertesni KrisisocsitaocsitulBelum ada peringkat
- Naskah Soal UN Fisika SMA 2012 Paket E35Dokumen13 halamanNaskah Soal UN Fisika SMA 2012 Paket E35Agus MuhtarBelum ada peringkat
- Celery Seeds Lower Blood Glucose in Diabetic RatsDokumen4 halamanCelery Seeds Lower Blood Glucose in Diabetic RatsocsitaocsitulBelum ada peringkat
- Pengkajian Luka Bates JensenDokumen6 halamanPengkajian Luka Bates JensenocsitaocsitulBelum ada peringkat
- Standardised Inotrope and Vasopressor Guidelines - Learning Package FINALDokumen30 halamanStandardised Inotrope and Vasopressor Guidelines - Learning Package FINALInês MendonçaBelum ada peringkat
- Cardiac OutputDokumen31 halamanCardiac OutputDylan BhuriBelum ada peringkat
- Fluid Responsiveness in Mechanically Ventilated Patients A Review of Indices Used in Intensive CADokumen9 halamanFluid Responsiveness in Mechanically Ventilated Patients A Review of Indices Used in Intensive CAerwanBelum ada peringkat
- 9279 BSM6000 en S 0Dokumen12 halaman9279 BSM6000 en S 0Jose L GuzCamBelum ada peringkat
- Ebook Egans Fundamentals of Respiratory Care 11Th Edition Kacmarek Test Bank Full Chapter PDFDokumen40 halamanEbook Egans Fundamentals of Respiratory Care 11Th Edition Kacmarek Test Bank Full Chapter PDFalexandercampbelldkcnzafgtw100% (10)
- Conceito de Pré Carga e Pós Carga em CardiologiaDokumen9 halamanConceito de Pré Carga e Pós Carga em CardiologiarmesquitajrBelum ada peringkat
- 3 - Cardiac Contractility - Ass. Prof. Doaa Abou-Bakr - 2020Dokumen8 halaman3 - Cardiac Contractility - Ass. Prof. Doaa Abou-Bakr - 2020Hossam BaniisBelum ada peringkat
- Basic & Advanced Hemodynamic Monitoring Part 1 PDFDokumen142 halamanBasic & Advanced Hemodynamic Monitoring Part 1 PDFUlfah UulBelum ada peringkat
- Cardiovascular SystemDokumen37 halamanCardiovascular SystemHira KhanBelum ada peringkat
- Noninvasive Hemodynamic Monitoring in The Intensive Care UnitDokumen18 halamanNoninvasive Hemodynamic Monitoring in The Intensive Care UnitmegaBelum ada peringkat
- 18 TH Course SyllabusDokumen1.744 halaman18 TH Course SyllabusxtineBelum ada peringkat
- Cardiac Output: Ejection Fraction (EF%)Dokumen5 halamanCardiac Output: Ejection Fraction (EF%)JockerBelum ada peringkat
- Dynamic Hemodynamic Monitoring Assesses Cardiovascular SufficiencyDokumen23 halamanDynamic Hemodynamic Monitoring Assesses Cardiovascular SufficiencyJuan CarrascoBelum ada peringkat
- Tutor Notes Wk1&2 Blood On The RoadDokumen17 halamanTutor Notes Wk1&2 Blood On The RoadThomaldo Perkonivic100% (1)
- Preload and AfterloadDokumen4 halamanPreload and AfterloadNeranga SamaratungeBelum ada peringkat
- Cardiovascular System Physiology, Lecture 2 (Cardiodynamics)Dokumen15 halamanCardiovascular System Physiology, Lecture 2 (Cardiodynamics)Sherwan R Shal100% (5)
- Hemodynamic Parameters To Guide Fluid Therapy: Review Open AccessDokumen9 halamanHemodynamic Parameters To Guide Fluid Therapy: Review Open AccessClaudioValdiviaBelum ada peringkat
- Quiz Cardiovascular Part 1 of 3Dokumen30 halamanQuiz Cardiovascular Part 1 of 3MedShare90% (10)
- Hemodynamics For The Bedside Nurse 1CEUDokumen7 halamanHemodynamics For The Bedside Nurse 1CEURN333100% (1)
- Heart FailureDokumen118 halamanHeart FailureAli Murtaza AbbasBelum ada peringkat
- Cardiac Contractility: Factors Affecting Strength of Heart Muscle ContractionDokumen4 halamanCardiac Contractility: Factors Affecting Strength of Heart Muscle ContractionzaidBelum ada peringkat
- Congestive Heart Failure, Pulmonary Edema, and CPAPDokumen35 halamanCongestive Heart Failure, Pulmonary Edema, and CPAPSherwan R Shal100% (1)
- Preload and AfterloadDokumen28 halamanPreload and Afterloadapi-19916399100% (1)
- FloTrac Sensor Clinical UtilityDokumen21 halamanFloTrac Sensor Clinical UtilityAnestesia 2017 UDECBelum ada peringkat
- Chapter 9 CARDIOVASCULAR SYSTEMDokumen21 halamanChapter 9 CARDIOVASCULAR SYSTEMAlexander Santiago ParelBelum ada peringkat
- 2021 ASO Biology Exam Part 1Dokumen20 halaman2021 ASO Biology Exam Part 1Joshua DeathBelum ada peringkat