Peritonitis in PD Patients
Diunggah oleh
Daniel SitungkirJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Peritonitis in PD Patients
Diunggah oleh
Daniel SitungkirHak Cipta:
Format Tersedia
Peritonitis in peritoneal
dialysis patients
Dr Cherelle Fitzclarence
Renal GP
July 2009
Overview
Peritoneal Dialysis - principles
Anatomy
Physiology
Pathology
Presentations
Management
Key points
www.health.com/
Chronic
Kidney
Disease
Diagnosis
End Stage
Kidney
Disease
Diagnosis
DIALYSIS
HAEMODIALYSIS
PERITONEAL DIALYSIS
TRANSPLANTATION
PALLIATIVE CARE
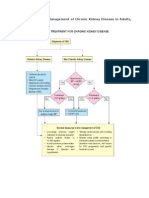
STAGE 1 & 2
Proteinuria plus
eGFR 60+
(to determine eGFR
over 60, hand
calculate GFR using
Cockcroft-Gault
formula)
STAGE 3
eGFR 30-59
ml/min
MODERATE
KIDNEY
DAMAGE
Proteinuria
Care plan
STAGE 5
eGFR <15
ml/min
FAILURE
STAGE 4
eGFR 15-29
ml/min
SEVERE
KIDNEY
DAMAGE
CKD
Care plan
ESKD
Care plan
GFR = (140 - Age) x wt (kg)
se creat (mmol/Lt)
Males = GFR x 1.23
Kidney
Failure
SUPPORTIVE CARE APPROACH
Peritoneal Dialysis
A form of renal replacement therapy for
patients with end stage kidney disease
Endeavours to replace some of the functions
of the kidney such as
Removing waste products
Removing excess fluid
Correcting acid/base imbalances
Correcting electrolyte imbalances
High maintenance form of therapy requiring
meticulous compliance and effort on part of
patient
www.agingdiscodiva.com
IDEAL BODY WEIGHT
IBW
Normotensive (Good BP) 120/70
No signs and symptoms of overload or
dehydration
Set by:
Home Training Staff Royal Perth Hospital
Renal Doctor
Dialysis Staff KSDC
FLUID ASSESSMENT
Blood pressure
Weight
Chest, SaO2, SOB
Oedema
Ankles
Back
Facial
JVP
Skin tugor
Symptoms
Nausea,
vomiting
Diarrhoea
Dizziness
FLUID RESTRICTION
800 1000 mls per day
Weigh patient (will be required daily
SAME SCALES and document
which ones)
In hospital, remove jug
Peritoneal Dialysis
Involves the passage of solutes and water
across a membrane that separates two fluid
containing compartments-blood and dialysate
During dialysis 3 transport processes occur
simultaneously
Diffusion
Ultrafiltration
Absorption
http://www.dialyse-45.net/int/info/techniques.htm
Peritoneal Dialysis
2 types
CAPD continuous ambulatory peritoneal
dialysis
Involves on average 4 dwells per day of 4-8
hours of 2 2.5L each
APD automated peritoneal dialysis
Involves 3-10 exchanges overnight of varying
amounts
Usually but not always a daytime dwell
Peritoneal Dialysis
Anatomy
Serosal membrane lining the gut
Thought to be the same as the body surface
area usually 1-2 m
2
in adult
2 parts visceral peritoneum lining the organs
(80% or the peritoneal surface area and the
parietal peritoneum lining the walls of the
abdominal cavity)
Peritoneal blood flow cant be measured but
indirectly estimated to be between 50-
100mls/min
Peritoneal Dialysis
Horizontal disposition of the peritoneum in the lower part of the abdomen.
www.theodora.com/anatomy/the_abdomen.html
Peritoneal Dialysis
Visceral peritoneum blood supply is from the
superior mesenteric with venous drainage
from the portal system
Parietal peritoneum blood supply is from the
lumbar, intercostal and epigastric arteries
while the venous drainage is via the IVC
Main lymphatic drainage is via stomata in the
diaphragmatic peritoneum which drain into
the right lymphatic duct
Three pore model
Peritoneal capillary is the critical barrier to
peritoneal transport
Movement of solute and water movement
across the capillary is mediated by pores of
three different sizes
Large pores 20-40 nm protein transport
Small pores 4-6nm small solutes eg urea,
creatinine, sodium, potassium, water
Ultrapores (aquaporins) <0.8nm transport of
water
Three pore model of peritoneal
transport
Kidney International
ISSN: 0085-2538
EISSN: 1523-1755
2009 International Society of Nephrology
Peritoneal Transport - Diffusion
Diffusion uraemic solutes and potassium
diffuse from peritoneal capillary blood into the
dialysate. Glucose, lactate, bicarbonate and
calcium diffuse in the opposite direction.
Diffusion depends on concentration gradient
(maximal at the start), effective peritoneal
surface area, intrinsic peritoneal membrane
resistance, molecular weight of the solute (eg
small molecules like urea, diffuse more
rapidly than larger molecules such as
creatinine)
Diffusion
www.indiana.edu/.../lecture/lecnotes/diff.html
Peritoneal Transport - Ultrafiltration
Occurs as a consequence of the osmotic gradient between the
hypertonic dialysate and the relatively hypotonic peritoneal
capillary blood
Driven by high concentration of glucose in dialysate
Depends on;
concentration gradient of the osmotic agent (glucose)
peritoneal surface area
hydraulic conductance of the peritoneal membrane
reflection coefficient for the osmotic agent (how effectively
the osmotic agent diffuses out of the dialysate into the
peritoneal capillaries (0-1 is normal the lower the value the
faster the osmotic gradient is lost. Gluc is 0.3 as opposed to
icodextrin which is close to 1)).
Hydrostatic pressure gradient cap press around 20mm
versus intraperitoneal pressure around 7mm Hg which
favours ultrafiltration
Ultrafiltration
http://www.dialysistips.com/principles.html
Peritoneal Transport Ultrafiltration 2
Depends on;
Oncotic pressure gradient which acts to keep fluid in
blood, opposing ultrafiltration (low in
hypoalbuminaemic patients so ultrafiltration tends to
be high)
Sieving occurs when solute moves along with water
across a semipermeable membrane by convection but
some of the solute is held back sieved. The solute
concentration in the ultrafiltrate that has passed
through the membrane is lower than the source
solution. Different solutes sieve differently ranging
from 0 (complete sieving) to 1 (no sieving)
Other osmotic agents such as icodextrin with a large
reflection coefficient so ultrafiltration is sustained
Ultrafiltration
http://www.advancedrenaleducation.com/PeritonealDialysis/Ultrafiltration/HowtoAchieveAdequatePDUF/tabid/229/Default.aspx
Peritoneal Transport Fluid
Absorption
Occurs via the lymphatics at constant rate
Typical values for peritoneal fluid absorption
are 1-2 mls/minute
Affected by intraperitoneal hydrostatic
pressure
Effectiveness of lymphatics
http://www.fmc-ag.com/gb_2006/en/05/glossar.html
Peritonitis
Peritoneal Dialysis is a great form of renal
replacement therapy
Peritonitis is a significant complication
Incidence peritonitis episodes varies from 1/9
patient-months to 1/53 patient-months
(Grunberg 2005; Kawaguchi 1999)
Our figures pending but are likely to be on
the lower end of the scale
Peritonitis in PD pts
Risk Factors
Diabetes
Non caucasian
Obesity
Temperate climate
Depression
Possibly the peritoneal dialysis
modality but not proven
(Huang 2001; Oo 2005).
http://www.diabetesandrelatedhealthissues
.com/
Peritonitis in PD pts
Significant morbidity
Some mortality - It is estimated that PD-
associated peritonitis results in death in 6%
of affected patients (Troidle 2006).
gymsoap.com
Peritonitis in PD pts
Catheter removal may become necessary if
pt is not responding to antibiotics or if
infection is fungal. May be temporary or
permanent
Ultrafiltration failure can occur both acutely
due to increases in capillary permeability
(Ates 2000; Smit 2004) and in the longer
term resulting in technique failure (Coles
2000; Davies 1996).
Pathogenesis
1. Potential routes of infection
Intraluminal improper technique; access to
bacteria via the catheter lumen
Periluminal bacteria present on skin surface
enter the peritoneal cavity via the catheter
tract
Transmural bacteria of intestinal origin
migrate through the bowel wall
Haematogenous peritoneum seeded via the
blood stream
Transvaginal - ??
Pathogenesis
2. Bacteria laden plaque the intraperitoneal portion
of the catheter is covered with a bacteria laden
plaque - ? Role in pathogenesis of peritonitis
3. Host defences peritoneal leucocytes critical in
combating bacteria that have entered the
peritoneum. Affected by
A. dialysis solution and ph hypertonic solution
inhibits activity
B. Calcium levels low calcium in dialysate inhibits
activity
Peritoneal IgG levels low levels inhibit activity
HIV little known effect
Aetiology
Staph aureus
Coag neg staph (S.Epidermidis)
E coli
Pseudomonas
Sternotropomonas
Candida
Atypical TB
Diagnosis
2 of the following 3 conditions
Symptoms and signs of peritoneal
inflammation (pain, tenderness, guarding,
rebound)
Cloudy peritoneal fluid with increased white
cell count (specifically neutrophils)
Demonstration of bacteria on gram stain or
culture
Diagnosis symptoms and signs
Abdo pain most common but in a PD pt
suspect peritonitis if general malaise,
nausea, vomiting or diarrhoea
Dont be blinded by the PD
These pts get other pathology
EG. Strangulated hernia, withdrawal from
steroids (if they stop taking meds suddenly
and they happen to be on steroids), ruptured
viscus, ulcers, perforations etc
EXAMINE THE PATIENT
Diagnosis symptoms and signs
Percentage
Symptoms
Abdo pain 95
Nausea and vomiting 30
Fever 30
Chills 20
Constipation or diarrhoea 15
Signs
Cloudy peritoneal fluid 99
Abdo tenderness 80
Rebound tenderness 10-50
Increased temperature 33
Blood leucocytosis 25
CRP 100 but can be delayed
Daugirdas JT et al 2007 p 419
Diagnosis peritoneal fluid
Cloudiness when cell count greater than 100 x 10
6
Normal is around 10x10
6
but always less than 50x10
6
Mostly cloudiness means peritonitis but be aware of other
causes such as fibrin, blood, malignancy, chyle
Dont write peritonitis off as a diagnosis if everything else fits but
the fluid is relatively clear the changes can lag
Must get a WCC (peritoneal fluid) with specific neutrophil count.
Neutrophils required as the total number of white cells can vary
according to whether patient dry or wet etc. Normally
predominant cells are mononuclears and neutrophils are usually
less than 15% of total white cell count
Be aware of mimickers such as PID, ovulation, recent pelvic
examination which may affect the cell counts in the peritoneal
fluid
Peritoneal fluid culture
Send the whole bag
Label it (preferable with texta label can sweat off)
Let the lab know it is coming
Ask for urgent gram stain and cell count and ask this
to be telephoned to you. Be aware that the gram
stain may be negative in 50% of cases of subsequent
culture proven peritonitis
Also ask for M/C/S and fungal cultures
Follow up the culture
Do a full septic workup each time including blood
cultures
Peritonitis
Common things occur commonly and
peritonitis is unfortunately common in our
population of PD patients
BUT
Dont lose sight of the bigger picture and
these patients can suffer from any other
pathology always keep an open mind
Peritonitis Management
Broad spectrum coverage
Vancomycin (2.5g if more than 60kg / 2 g if 60kg or
less)
Gentamicin (200mg if more than 60kg / 140mg if 60kg
or less)
IP is better than IV (confirmed on large Cochrane
review April 2009)
Await culture. If gram positive, then repeat the vanc
dose in 1 week. If gram negative then usually
ceftriaxone 1g intraperitoneally daily for 14 days
Things to note; if pseudomonas tube is very often lost.
May need to consider adding a second antibiotic such
as daily ciprofloxacin
Initial symptoms may include;
diarrhoea, vomiting, nausea,
abdominal pain, mental confusion or feeling unwell
PERITONITIS MANAGEMENT
COLLECT DRAINED BAG
*See additional resources (pink section) for drainage instructions
* Send entire bag for urgent MC&S (including WCC differential) and Fungal elements. ****
Must cc KRSS ****
Intraperitoneal (IP) Antibiotics (see Procedures)
Give BOTH
Gentamycin 160mgs if 60kgs or less
(gram ve organisms) 200mg if > 60kgs
AND
Vancomycin - 2gms if 60kgs or less
(gram +ve organisms) 2.5grams if > 60kgs
Give both in a 2L 2.3% bag
Dwell in the abdomen for minimum 6 hours
(Consult microbiologist if Vanc or Gent allergy)
must be able to read newspaper print through the
bag
LOOK FOR OTHER CAUSES
Call PD Coordinator or
Renal GP
ATTENTION:
Vanc and Gent provide some coverage while
awaiting sensitivities.
****Further antibiotics WILL be required ****
If Staph/gram +ve, give IP Vancomicin again on Day 7
If gram negative, refer to sensitivities, but
usually 14 days of IP Ceftriaxone 1gm
YOU MUST follow up the MC & S 48 hours after initial IP treatment.
A WCC > 100 confirms peritonitis.
If the patient is not improving within 24 hrs, or any other concerns, contact PD coordinator
CLEAR BAG
CLOUDY BAG
Peritonitis Mx
CAPD/APD
Drain abdomen and send bag off with path
request as above
Change the transfer set completely following
usual aseptic techniques
Load 2.3% 2 litre dialysate bag (use 1.5% bag
if patient hypotensive) with Vancomycin and
Gentamicin as per above guideline
Infuse bag into peritoneum
6 hour dwell
Peritonitis fungal infection
If fungal organisms are seen on gram stain,
or cultured, it is unlikely you will be able to
save the tube
Once the tube is colonized, the only cure is
removal of tube, peritoneal rest (pt on
Haemodialysis for a few months) and then
start from scratch
Peritonitis
If you think that the patient has peritonitis but you
think they have life threatening sepsis eg
hypotension, tachycardia, fever (or no fever as may
not be able to mount an immune response), altered
conscious state etc, your patient is likely to require IV
broad spectrum antibiotics. Ring the microbiologist
on call. Dont wait to get IP regime in. That can go in
while you are making calls and obtaining results.
Antibiotics must be given within 1 hour of
presentation it is an emergency.
I usually ring SCGH as they maintain a 24 hour
consultant micro roster 93463333 but remember all
our patients who require transfer must go to Royal
Perth Hospital as they are under the RPH consultant
Peritonitis
Patients can have dual pathology
Eg it is not uncommon for patients to have
peritonitis, delay treatment, splint their
abdomen and get pneumonia. This needs to
be treated as per the normal guidelines for
pneumonia
Peritonitis
Additives to bags
Vancomycin, aminoglycosides and
cephalosporins are safe to mix in the same
bag
Aminoglycosides are incompatible with
penicillins
Vancomycin is stable for 28 days in dialysate
(normal room temp)
Cefazolin is stable for 8 days
Gentamicin is stable for 14 days
Heparin added decreases duration of stability
Peritonitis
Often get formation of fibrin clots which
increases risk of catheter block
May need to add 500units of heparin to 1 or 2
bags a day until fibrin clots decrease
Constipation is common you may need to
stop the calcium based phosphate binders
temporarily but better off using aperients
early and preventing the need to alter routine
meds
Peritonitis
Fluid regimes
Depends whether patient is overloaded or
underloaded
Can usually continue normal regime but tailor to
patient
If BP low, use 1.5% bags x 4 a day
If BP high use 2.3% bags, minimum of 4 a day
Aim for BP 120/
APD pts can continue on APD or if needed can
convert temporarily to CAPD in Broome with
resources this should not be necessary
Peritonitis
Can get changes in the permeability of the peritoneal
membrane
Permeability to water, glucose and proteins is
increased
Rapid glucose absorption from the dialysis solution
reduces amount of ultrafiltration and can result in fluid
overload
May need high glucose concentration dialysate with
shorter dwells
Hyperglycaemia is common
Protein loss is increased in peritonitis so patients will
need high protein supplements
Peritonitis
Dont forget secondary causes of peritonitis
Perforated gastric or duodenal ulcer
Pancreatitis
Appendicitis
Diverticulitis
PID
Talk to the surgeon if you are not sure
Peritonitis
You dont necessarily have to admit the
patient
Admission dictated by symptoms and distress
and often social circumstances up here
blogs.southshorenow.ca/louise/ cms.ich.ucl.ac.uk/website/imagebank/images
Peritonitis - bugs
Staph Vancomycin and repeat in 1 week
Patients should have nasal carriage treated with
mupirocin bd for 5 days and then once a week of bd
for 5 days once a month
Gram Negs IP Ceftriaxone for 2 weeks and
consider repeating the dose of gentamicin after a
week or adding oral ciprofloxacin to the regime
Pseudomonas difficult to treat
Sternotrophomonas usually requires 2 antibiotics
and usually for 4 weeks
Campylobacter not that common responds to
gentamicin
Peritonitis
Multiple organisms
Have a high index of suspicion for secondary
peritonitis
If not secondary peritonitis have 60% chance of curing
with appropriate antibiotics
If one of the organisms is clostridium or bacteroides
likely intra-abdominal abscess or perforated abdominal
viscus but exclude appendicitis, perforated ulcer,
pancreatitis and any other cause of secondary
peritonitis
Occurrence of abdominal catastrophe in PD patient
has a high mortality
Talk to the surgeon
Add metronidazole
Ship south
Peritonitis
Culture negative disease
If cell count less than 50 x 10
6
unlikely to
peritonitis
If higher white cell count, then repeat empiric
therapy
Make sure lab is doing cultures for AFBs and
fungus
If not improving consider legionella,
campylobacter, ureaplama, mycoplasma,
enteroviruses, fungus, histoplasma
capsulatum
Peritonitis
Fungal peritonitis
Predisposing factors
Prior antibiotic use especially if not full treatment
Immunosuppressive therapy
HIV
Malnutrition
Low albumin
Diabetes
Peritonitis
Fungal peritonitis
We tend to try and save the tube by giving
antifungals but guidelines recommend prompt
removal of catheter, conversion to
haemodialysis for a few weeks and then start
from scratch
Penetration of antifungals to peritoneum other
than with IP administration, is poor
Peritonitis
Refractory disease
Defined as disease that is treated with
appropriate antibiotics for 5 days without
improvement
Catheter removal necessary to reduce
morbidity and preserve peritoneum
Increased with gram neg bugs
Peritonitis
Relapsing disease
Peritonitis with the same organism within 4 weeks of stopping
therapy
Usually Staph epidermidis or a gram negative organism
If pseudomonas or gram negatives, remove the catheter
If staph, may be able to rescue with repeat vancomycin weekly
for a month or may be able to remove the tube and
simultaneously insert a new tube (as opposed to any other
organism where a 2 month peritoneal rest is required)
Sometimes can use urokinase to strip the biofilm (bacteria
entrapped in fibrin in the peritoneal membrane) in relapsing
disease last resort but worth a go
Peritonitis
20% of episodes temporally associated with
exit site and tunnel infections (Piraino et al
2005)
Treat exit site infections if red and purulent
Swab it
Start Flucloxacillin empirically and change or
add ciprofloxacin if gram neg
Exit sites are another whole topic
Peritonitis
Prevention
Good technique
Hygiene
Mupirocin
Exit site care
Anchor tape
Cochrane Review 2009
Implications for practice
At the present time broad spectrum antibiotics should be initiated at the
time a diagnosis of peritonitis is made. When choosing antibiotics the
side-effect profile, local drug resistance patterns and previous antibiotic
use and infection history in the individual concerned should be
considered. In cases of recurrent peritonitis dialysis catheters should
be removed rather than using intraperitoneal urokinase.
Currently available evidence from RCTs is inadequate in many areas
of clinical practice important in the management of PD-associated
peritonitis. This is a limiting factor in the provision of definitive
treatment guidelines.
Cochrane Review 2009
Implications for research
Further studies are required to establish the most effective treatment for peritoneal dialysis-
associated peritonitis. An essential feature of such studies is inclusion of enough patients to
ensure adequate power to assess meaningful long and short term outcomes. Short term
outcomes should extend beyond whether cure is achieved without catheter removal, for
example duration of systemic inflammation. Study of long-term outcomes should include
permanent transfer to haemodialysis, development of ultrafiltration failure patient death and
late recurrent episodes of peritonitis beyond four weeks from the original episode.
Specific interventions that would be of value include early versus late catheter removal.
Studies designed to study infections due to specific organisms would also be valuable. An
example is a study of glycopeptide versus cephalosporin therapy in peritonitis due to
coagulase negative Staphylococcal species. The majority of studies have included patients
on CAPD rather than APD hence studies designed to test the efficacy of antibiotics in APD
are required. This is particularly applicable to studies of intermittent versus continuous
dosing when cycler dwell times may well influence pharmacokinetics.
Future research should be conducted using standard definitions, with inclusion of
information about factors that may influence the response to therapy such as prophylaxis
regimens and dialysis solutions used. Current ISPD guidelines provide a comprehensive list
of requirements for future studies that should be referred to when designing studies.
Take home points
Have a high index of suspicion
Use the remote area manual
Always let KRSS know of episode
Copy all results to KRSS
Dont hesitate to ask if you are not sure KRSS team, KRSS GP, Renal GP,
Nephrologist
www.learningradiology.com
Acknowledgements
Thanks to Daugirdas et al 2007 Handbook
of dialysis
http://mrw.interscience.wiley.com/cochrane/cl
sysrev/articles/CD005284/frame.html
Thank you
Questions
renalgp@kamsc.org.au
Anda mungkin juga menyukai
- Swollen Kidney, (Hydronephrosis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandSwollen Kidney, (Hydronephrosis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Disseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandDisseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- Hereditary Spherocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHereditary Spherocytosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Diabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandDiabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- Atelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesDari EverandAtelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesBelum ada peringkat
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Infective Endocarditis: A Multidisciplinary ApproachDari EverandInfective Endocarditis: A Multidisciplinary ApproachArman KilicBelum ada peringkat
- Unstable Angina, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandUnstable Angina, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Diabetic Retinopathy: Causes, Tests, and Treatment OptionsDari EverandDiabetic Retinopathy: Causes, Tests, and Treatment OptionsBelum ada peringkat
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- A Simple Guide to Thyrotoxicosis, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Thyrotoxicosis, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- Cyanosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCyanosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPenilaian: 5 dari 5 bintang5/5 (1)
- Cardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Cardiovascular Diseases: Genetic Susceptibility, Environmental Factors and their InteractionDari EverandCardiovascular Diseases: Genetic Susceptibility, Environmental Factors and their InteractionBelum ada peringkat
- Kidney Development, Disease, Repair and RegenerationDari EverandKidney Development, Disease, Repair and RegenerationMelissa Helen LittlePenilaian: 3.5 dari 5 bintang3.5/5 (2)
- Renal Disease in Cancer PatientsDari EverandRenal Disease in Cancer PatientsKevin W. FinkelBelum ada peringkat
- Gastrointestinal Bleeding, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandGastrointestinal Bleeding, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Pancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandPancytopenia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Overview of The Management of Acute Kidney Injury in Adults - UpToDateDokumen13 halamanOverview of The Management of Acute Kidney Injury in Adults - UpToDateDaniely FreitasBelum ada peringkat
- Wolff-Parkinson- White-Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandWolff-Parkinson- White-Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- End-Stage Renal Disease: An Integrated ApproachDari EverandEnd-Stage Renal Disease: An Integrated ApproachWilliam J. StoneBelum ada peringkat
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- HYPOKALEMIA) ReportDokumen72 halamanHYPOKALEMIA) ReportFairoz Macud AdapBelum ada peringkat
- Acute Renal Failure: Dr. Bobi Ahmad S, S.KPDokumen62 halamanAcute Renal Failure: Dr. Bobi Ahmad S, S.KPdr.Bobi Ahmad Sahid, S.KepBelum ada peringkat
- Appendicitis: The Etiology, Hygenic and Dietetic TreatmentDari EverandAppendicitis: The Etiology, Hygenic and Dietetic TreatmentPenilaian: 3 dari 5 bintang3/5 (2)
- Hypokalemic Periodic Paralysis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHypokalemic Periodic Paralysis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Idiopathic Thrombocytopenic Purpura, A Simple Guide to The Condition, Treatment And Related ConditionsDari EverandIdiopathic Thrombocytopenic Purpura, A Simple Guide to The Condition, Treatment And Related ConditionsBelum ada peringkat
- I Got the Flu! What is Influenza? - Biology Book for Kids | Children's Diseases BooksDari EverandI Got the Flu! What is Influenza? - Biology Book for Kids | Children's Diseases BooksBelum ada peringkat
- Kidney TransplantDokumen11 halamanKidney TransplantPrincess Xzmae RamirezBelum ada peringkat
- Hemodialysis in ChildrenDokumen28 halamanHemodialysis in ChildrenKarna Yuli sitanggangBelum ada peringkat
- Problem-based Approach to Gastroenterology and HepatologyDari EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisBelum ada peringkat
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutDari EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutPenilaian: 5 dari 5 bintang5/5 (1)
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDokumen4 halamanRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniBelum ada peringkat
- Acute and Chronic Pancreatitis ShirleyDokumen6 halamanAcute and Chronic Pancreatitis ShirleyVictor AladejanaBelum ada peringkat
- Nephrotic Syndrome in Children: January 2013Dokumen7 halamanNephrotic Syndrome in Children: January 2013molenBelum ada peringkat
- Renal Failure PresentationDokumen65 halamanRenal Failure PresentationBhawna JoshiBelum ada peringkat
- Australian Diabetes Society Guidelines For Routine Glucose Control in HospitalDokumen70 halamanAustralian Diabetes Society Guidelines For Routine Glucose Control in HospitalYovan PrakosaBelum ada peringkat
- Hemolytic Uremic SyndromeDokumen1 halamanHemolytic Uremic SyndromeAndrea TeranBelum ada peringkat
- Atrial Fibrillation HandoutDokumen5 halamanAtrial Fibrillation HandoutAlfa AlfinBelum ada peringkat
- Chronic Kidney DiseaseDokumen40 halamanChronic Kidney DiseaseSarah Benjamin0% (1)
- Anticoagulants, Thrombolytics and AntiplateletDokumen57 halamanAnticoagulants, Thrombolytics and AntiplateletEsther Agustin100% (1)
- Aortic RegurgitationDokumen12 halamanAortic RegurgitationSanjeet SahBelum ada peringkat
- Case Study For Chronic Renal FailureDokumen6 halamanCase Study For Chronic Renal FailureGabbii CincoBelum ada peringkat
- HyponatremiaDokumen26 halamanHyponatremiapreethi.rayan455Belum ada peringkat
- Nursing Management: Nursing Management: Acute Kidney Injury and Chronic Kidney DiseaseDokumen22 halamanNursing Management: Nursing Management: Acute Kidney Injury and Chronic Kidney Diseasedian rachmat saputroBelum ada peringkat
- Hypo Album inDokumen11 halamanHypo Album inAndi Agung RiatmojoBelum ada peringkat
- Stem Cell TransplantationDokumen13 halamanStem Cell TransplantationMylls MondejarBelum ada peringkat
- Algo Bradycardia DikonversiDokumen5 halamanAlgo Bradycardia DikonversiDaniel SitungkirBelum ada peringkat
- Algoritma BradikardiaDokumen2 halamanAlgoritma BradikardiaDaniel SitungkirBelum ada peringkat
- Outer Ear: Anatomy Physiology DisordersDokumen21 halamanOuter Ear: Anatomy Physiology DisordersDaniel SitungkirBelum ada peringkat
- GlaucomaDokumen12 halamanGlaucomaDaniel SitungkirBelum ada peringkat
- Anatomy Review Part 1Dokumen54 halamanAnatomy Review Part 1Daniel SitungkirBelum ada peringkat
- Anatomy of The Abdomen: Dr. Ahmad Kamil Shahwan Ph.D. General SurgeryDokumen87 halamanAnatomy of The Abdomen: Dr. Ahmad Kamil Shahwan Ph.D. General SurgeryDaniel SitungkirBelum ada peringkat
- Inguinal HerniaDokumen33 halamanInguinal Herniatianally100% (2)
- Antibiotika PDFDokumen101 halamanAntibiotika PDFDaniel SitungkirBelum ada peringkat
- HypospadiasDokumen20 halamanHypospadiasDaniel SitungkirBelum ada peringkat
- Artículo MédicoDokumen17 halamanArtículo MédicoOncología CdsBelum ada peringkat
- Polycystic Kidney DiseaseDokumen6 halamanPolycystic Kidney DiseaseRimsha Khan100% (1)
- 1.acute Kidney InjuryDokumen3 halaman1.acute Kidney InjuryIan CruzBelum ada peringkat
- 4creatine and Diabetes - Supplements and NutritionDokumen4 halaman4creatine and Diabetes - Supplements and NutritionjesseBelum ada peringkat
- Chronic Kidney Disease BookletDokumen8 halamanChronic Kidney Disease BookletRina SoniaBelum ada peringkat
- Genito Urinary SystemDokumen106 halamanGenito Urinary Systemnursereview88% (8)
- Jurnal Pico KMBDokumen7 halamanJurnal Pico KMBOktaviani Putri PratiwiBelum ada peringkat
- 5.0 Sessions of Interest: Wednesday, November 16Dokumen17 halaman5.0 Sessions of Interest: Wednesday, November 16api-340273587Belum ada peringkat
- Dialysis Treatment - A Comprehensive DescriptionDokumen13 halamanDialysis Treatment - A Comprehensive Descriptionrmprskgwk5Belum ada peringkat
- Normal GFR in ChildDokumen8 halamanNormal GFR in ChildbobbypambudimdBelum ada peringkat
- GenitourinaryDokumen16 halamanGenitourinaryAnonymous iG0DCOfBelum ada peringkat
- 2012 Cath Lab Consensus DocumentDokumen85 halaman2012 Cath Lab Consensus DocumentDorin DocBelum ada peringkat
- Summary of CPG Management of CKD in AdultsDokumen12 halamanSummary of CPG Management of CKD in AdultsAhmad Zhafri Md NoorBelum ada peringkat
- European Best Practice Guidelines On Vascular Access 2007Dokumen30 halamanEuropean Best Practice Guidelines On Vascular Access 2007Jim Dominguez RosalesBelum ada peringkat
- Definition and Staging of Chronic Kidney Disease in Adults - UpToDateDokumen1 halamanDefinition and Staging of Chronic Kidney Disease in Adults - UpToDateLauraBelum ada peringkat
- CKD History TakingDokumen2 halamanCKD History TakingNadia Salwani80% (5)
- TW Case StudyDokumen27 halamanTW Case Studyapi-346311171Belum ada peringkat
- ACCP 2018 NephrologyDokumen31 halamanACCP 2018 NephrologyMonica Febri Andari100% (1)
- IRIS-DOG-Treatment Recommendations 2023Dokumen17 halamanIRIS-DOG-Treatment Recommendations 2023jhumira perez de la oBelum ada peringkat
- ReninDokumen4 halamanReninSarah AndrianiBelum ada peringkat
- 2 Tietz 2012 Kidney Function TestsDokumen39 halaman2 Tietz 2012 Kidney Function TestsIvana BajunovicBelum ada peringkat
- Jurnal Intadialitic ExerciseDokumen9 halamanJurnal Intadialitic Exercisedwi nurdianingtyasBelum ada peringkat
- Arteriovenous Access For HemodialysisDokumen11 halamanArteriovenous Access For Hemodialysislakshminivas PingaliBelum ada peringkat
- Pembahasan To Online 5Dokumen522 halamanPembahasan To Online 5vanadiel4Belum ada peringkat
- Curs 02 Renal Vascular DiseasesDokumen56 halamanCurs 02 Renal Vascular DiseasesMadalina SercaianuBelum ada peringkat
- NCM 109 Maternal Lecture Lesson: CausesDokumen2 halamanNCM 109 Maternal Lecture Lesson: CausesJanelle ArcillaBelum ada peringkat
- Nepharites Lesson PlanDokumen21 halamanNepharites Lesson Plansaritha Oruganti100% (1)
- HypertensionDokumen14 halamanHypertensionChucky Vergara100% (2)
- Rational Use of Diawdawduretic and Patofisiologi EdemaDokumen10 halamanRational Use of Diawdawduretic and Patofisiologi EdemaWendy WiharjaBelum ada peringkat
- Evidence Based MedicineDokumen22 halamanEvidence Based MedicineLastry WardaniBelum ada peringkat