Ectopic Pregnancy MARINO
Diunggah oleh
Michael Angelo SeñaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Ectopic Pregnancy MARINO
Diunggah oleh
Michael Angelo SeñaHak Cipta:
Format Tersedia
Marino M. Abogado Jr.
BSN II - Pure
Objectives of the discussion
To know the definition of ectopic pregnancy
and its manifestation.
To have an idea with its clinical symptoms.
To know the illness etiology and
pathophysiology.
To determine what is the appropriate medical
and nursing management
Definition
Pregnancy in which the fertilized
egg or embryo implants on any
tissue other than the endometrial
lining of the uterus.
Etiology
Pelvic inflammatory disease
History of prior ectopic pregnancy
History of tubal surgery and
conception after tubal ligation
Use of fertility drugs or assisted
reproductive technology
Use of an intrauterine device
Increasing age
Smoking
Salpingitis isthmica nodosum
T-shaped uterus
Prior abdominal surgery, failure with
progestin-only contraception
ruptured appendix.
Common Ectopic Sites
1. Ampullary (mid) portion of the fallopian tube (80-90%),
2. Isthmic (area closer to the uterus) portion of the fallopian
tube (5-10%),
3. Fimbrial (distal end away from the uterus) portion of the
fallopian tube (about 5%),
4. Cornual (within the uterine muscle) portion of the fallopian
tube (1-2%),
5. Abdomen (1-2%),
6. Ovary (less than 1%), or
7. Cervix (less than 1%).
Incidence and Impact
Occurs in 1 in 50 pregnancies
Is becoming increasingly more common
Is the second leading cause of maternal
mortality overall, and primary mortality
factor in first trimester pregnancies
May lead to impairment or loss of fertility
Clinical Signs and
Symptoms
Amenorrhea
Vaginal bleeding(40-50%)
Nausea
Breast fullness
Fatigue
Pain
Low abdominal pain
Heavy cramping
Pelvic tenderness (75%)
Enlarged uterus
Adnexal mass(50%)
Shoulder pain
Recent dyspareunia
Diagnosis
History and physical
any woman presenting with pain and vaginal
bleeding should be considered to have an
ectopic pregnancy until otherwise ruled out
Laboratory markers
Beta-HCG(measured in mIU/mL) --lack of
doubling signals only impending failure, not
indicative of location;absolute value only
helpful in correlation with ultrasound
Progesterone--also only indicates impending
loss, not location
Ultrasound--transvaginal is most
sensitive at this stage of pregnancy.
Correlation with the quantitative serum
hormone levels is suggested to increase
your sensitivity
if intrauterine gestational sac is seen and b-
HCG is 1,000-2,000, normal pregnancy is
virtually certain.
If b-HCG is <1,000 and there is an empty
uterus, ectopic pregnancy is very likely
Culdocentesis
In this test, a needle is inserted into the
space at the very top of the vagina,
behind the uterus and in front of the
rectum. Any blood or fluid found there
likely comes from a ruptured ectopic
pregnancy.
Cullen's sign can indicate a ruptured
ectopic pregnancy.
Medication
Methotrexate 1 mg/kg body weight is
an antimetabolite which inhibits the
reduction of folic acid to tetrahydrofolate.
This interferes with DNA synthesis and
cell multiplication. Ideal for disrupting
trophoblastic tissue proliferation.
Surgery
Tube sparing salpingotomy--used when
gestational sac is <2cm and in distal tube;
lateral incision made and gestational sac
removed.
Tube sacrificing salpingectomy
Effects of Ectopic
Pregnancy
The muscle wall of the tube has not the capacity
of uterine muscles for hypertrophy and
distention and tubal pregnancy nearly always
end in rupture and the death of the ovum.
Tubal abortion usually in ampullary about 8
weeks forming pelvic haematocele
Rupture into the peritoneal cavity
Occur mainly from the narrow isthmus before 8
weeks or later from the interstitial portion of the
tube. Haemorrhage is likely to be severe.
Sometimes rupture is extraperitoneal between the
leaves of the broad ligament Broad ligament
haematoma. Haemorrhage is likely to be controlled
Tubal pregnancy effect on
uterus
The uterus enlarge in first 3 months as if
the implantation were normal, reach the
size of a gravid uterus of the same
maturity.
Uterine decidua grows abundantly and
when the embryo dies bleeding occurs as
the decidua degenerates due to effect of
oestrogen withdrawal.
Nursing Diagnosis: Powerlessness
related to early loss of pregnancy
secondary to ectopic pregnancy
Outcome Evaluation: Client states she
feels sad at pregnancy loss but is able
to deal with situation; has returned to
previous level of activities and has
forward-thinking plans.
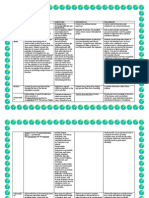
Uterus outlined in red, uterine lining in green, tubal ectopic pregnancy
yellow. Fluid in uterus at blue circle - sometimes called a "pseudosac" -
looks like an early pregnancy sac, but is not (usually a small blood
collection).
Citations
Chambers, H. M., & Chan, F. Y. (2009). Support for women/families after
perinatal death. Cochrane Database of Systematic Reviews, 2009(1),
(CD000452).
Chhabra, S., Dargan, R., & Nasare, M. (2007). Antepartum transabdominal
amnioinfusion. International Journal of Gynaecology and Obstetrics,97(2), 9599.
Chauhan, S. P., et al. (2007). Intrauterine growth restriction and
oligohydramnios among high-risk patients. American Journal of
Perinatology, 24(4), 215221.
Clark, E. A. S., Silver, R. M., & Branch, D. W. (2007). Do antiphospholipid
antibodies cause preeclampsia and HELLP syndrome? Current Rheumatology
Reports, 9(3), 219225.
Crombleholme, W. R. (2009). Obstetrics. In S. J. McPhee & M. A.
Papadakis (Eds.). Current medical diagnosis and treatment. Columbus, OH:
McGraw-Hill.
Yeah!! Natapos din pag
REPORT. HEHE!! relax
Anda mungkin juga menyukai
- Funda 246 Nursing BulletsDokumen20 halamanFunda 246 Nursing BulletsMichael Angelo SeñaBelum ada peringkat
- KitKat OTA Update Now Available For Starmobile PLAYDokumen2 halamanKitKat OTA Update Now Available For Starmobile PLAYMichael Angelo SeñaBelum ada peringkat
- Psyche NotesDokumen18 halamanPsyche NotesIrene Soriano BayubayBelum ada peringkat
- Focus Charting (F-DAR) : How To Do Focus Charting or F-DAR: Notes Fundamentals of NursingDokumen6 halamanFocus Charting (F-DAR) : How To Do Focus Charting or F-DAR: Notes Fundamentals of NursingMichael Angelo SeñaBelum ada peringkat
- 10 Rules of Photo CompositionDokumen10 halaman10 Rules of Photo Compositionxmanws8421Belum ada peringkat
- Celiac Disease-A Not So Uncommon DisorderDokumen28 halamanCeliac Disease-A Not So Uncommon DisorderMichael Angelo SeñaBelum ada peringkat
- 9173Dokumen7 halaman9173kimbsn2014Belum ada peringkat
- Mind Games For Big GainsDokumen3 halamanMind Games For Big GainsMichael Angelo SeñaBelum ada peringkat
- Nursing 106 OB VocabDokumen18 halamanNursing 106 OB VocabMichael Angelo SeñaBelum ada peringkat
- Are You Having ProblemsDokumen5 halamanAre You Having ProblemsMichael Angelo SeñaBelum ada peringkat
- CHN RabeDokumen24 halamanCHN RabeMichael Angelo Seña100% (1)
- Nursing ProceduresDokumen2 halamanNursing ProceduresMichael Angelo SeñaBelum ada peringkat
- Dorothy E. Johnson's Behavioral System ModelDokumen9 halamanDorothy E. Johnson's Behavioral System ModelMichael Angelo SeñaBelum ada peringkat
- BudgetingDokumen4 halamanBudgetingMichael Angelo SeñaBelum ada peringkat
- Sister Callista RoyDokumen4 halamanSister Callista RoyMichael Angelo SeñaBelum ada peringkat
- 1Dokumen1 halaman1Michael Angelo SeñaBelum ada peringkat
- NCP Preeclampsia TissueperfusionDokumen2 halamanNCP Preeclampsia TissueperfusionMichael Angelo Seña100% (2)
- College of Nursing and Midwifery: Mabini Colleges Daet, Camarines NorteDokumen1 halamanCollege of Nursing and Midwifery: Mabini Colleges Daet, Camarines NorteMichael Angelo SeñaBelum ada peringkat
- Kla LallaDokumen1 halamanKla LallaMichael Angelo SeñaBelum ada peringkat
- Disaster NursingDokumen6 halamanDisaster NursingMichael Angelo SeñaBelum ada peringkat
- Theoretical and Conceptual FrameworkDokumen9 halamanTheoretical and Conceptual FrameworkJavea Villagracia100% (2)
- 27 TheoristDokumen6 halaman27 TheoristMichael Angelo SeñaBelum ada peringkat
- Disciplines Disasters and EM BookDokumen39 halamanDisciplines Disasters and EM BookBones S. MrBonesBelum ada peringkat
- StructualDokumen4 halamanStructualMichael Angelo SeñaBelum ada peringkat
- Draft Philippines Report - Institutions and Policies On DRM and CCA - 30june2010Dokumen73 halamanDraft Philippines Report - Institutions and Policies On DRM and CCA - 30june2010Michael Angelo SeñaBelum ada peringkat
- SplittingDokumen3 halamanSplittingMichael Angelo SeñaBelum ada peringkat
- Chapter 1 UnoffiDokumen1 halamanChapter 1 UnoffiMichael Angelo SeñaBelum ada peringkat
- Multiple Sclerosis Nursing Care PlansDokumen27 halamanMultiple Sclerosis Nursing Care PlansMichael Angelo Seña0% (1)
- Theoretical and Conceptual FrameworkDokumen9 halamanTheoretical and Conceptual FrameworkJavea Villagracia100% (2)
- UNISDR FinalReport (Philippines) - CleanDokumen77 halamanUNISDR FinalReport (Philippines) - CleanMichael Angelo SeñaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Supraspinatus TendonitisDokumen27 halamanSupraspinatus TendonitisnogenaziBelum ada peringkat
- Paediatric PSGDokumen21 halamanPaediatric PSGFayhaa NadeemBelum ada peringkat
- PPDCDokumen13 halamanPPDCGAYATHRI100% (1)
- Case 4-2021: A 70-Year-Old Woman With Dyspnea On Exertion and Abnormal Findings On Chest ImagingDokumen12 halamanCase 4-2021: A 70-Year-Old Woman With Dyspnea On Exertion and Abnormal Findings On Chest ImagingBruno ConteBelum ada peringkat
- Kenny's Boards 2 ReviewsDokumen254 halamanKenny's Boards 2 ReviewsHuguette Marie NseleBelum ada peringkat
- 1 1 4 5 1Dokumen48 halaman1 1 4 5 1bansallove2008Belum ada peringkat
- HTTP Healthmedicinet Com II 2013 10 PDFDokumen314 halamanHTTP Healthmedicinet Com II 2013 10 PDFtuni santeBelum ada peringkat
- InfectiousmeningitisDokumen10 halamanInfectiousmeningitisHow ToBelum ada peringkat
- Oral and Dental HealthDokumen10 halamanOral and Dental HealthannisaramadantiBelum ada peringkat
- Semmelweis' Handwashing & Lister's Antiseptic TechniqueDokumen22 halamanSemmelweis' Handwashing & Lister's Antiseptic TechniqueNewBelum ada peringkat
- Health 10 Q3 Week 2Dokumen8 halamanHealth 10 Q3 Week 2JajaBelum ada peringkat
- Twolevel Wells Score Templates For Deep Vein Thrombosis and Pulmonary Embolism Msword 186721165Dokumen7 halamanTwolevel Wells Score Templates For Deep Vein Thrombosis and Pulmonary Embolism Msword 186721165SaffronMaeBelum ada peringkat
- Uworld DermatDokumen64 halamanUworld DermatRatnam hospitalBelum ada peringkat
- What Is A Hypochondriac?: ENG - B2.0902RDokumen25 halamanWhat Is A Hypochondriac?: ENG - B2.0902RAnelBelum ada peringkat
- Paranoid Personality DisorderDokumen19 halamanParanoid Personality DisorderChucky VergaraBelum ada peringkat
- Action Research BMIDokumen7 halamanAction Research BMIKosaki SmithBelum ada peringkat
- Drugs Used in GI DisordersDokumen35 halamanDrugs Used in GI DisordersSyafi'ie SyukriBelum ada peringkat
- Atarax Pi Ncds06si Approved 17sep19Dokumen11 halamanAtarax Pi Ncds06si Approved 17sep19premkumarhydBelum ada peringkat
- PDFDokumen2 halamanPDFIka Naq BungsuBelum ada peringkat
- A Review On Common Dermatologic ConditionsDokumen16 halamanA Review On Common Dermatologic ConditionsQuality TimbersBelum ada peringkat
- DrugStudy MetoclopramideDokumen2 halamanDrugStudy MetoclopramideAshknee Khainna AlejoBelum ada peringkat
- Chapter VIII Drug StudyDokumen21 halamanChapter VIII Drug StudyDylan Angelo AndresBelum ada peringkat
- Gordon's Functional Health PatternsDokumen2 halamanGordon's Functional Health PatternsKara GloriaBelum ada peringkat
- DiseasesDokumen13 halamanDiseasesJaypee SaturnoBelum ada peringkat
- Gerd Summary1Dokumen2 halamanGerd Summary1api-271278965Belum ada peringkat
- CorticosteroidsDokumen48 halamanCorticosteroidscatherinaywBelum ada peringkat
- SRM04-08 Brothers UnitedDokumen29 halamanSRM04-08 Brothers UnitedBrandon Dempe100% (4)
- Chronic Obstructive Pulmonary DiseaseDokumen40 halamanChronic Obstructive Pulmonary DiseaseIVORY DIANE AMANCIOBelum ada peringkat
- CH 5Dokumen97 halamanCH 5jaraulabelleBelum ada peringkat
- Final TouchDokumen49 halamanFinal TouchmalathiBelum ada peringkat