Bks
Diunggah oleh
Anonymous 8w9QEG0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
18 tayangan182 halamankoas
Judul Asli
bks
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPT, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Inikoas
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
18 tayangan182 halamanBks
Diunggah oleh
Anonymous 8w9QEGkoas
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 182
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
The infant is lying still and has poor muscle tone.
He is irritable if touched, and his cry is weak. There
are no abnormal airway sounds, retractions, or
flaring. He is pale and mottled. The respiratory rate
is 30 breaths/min, heart rate is 180 beats/min, and
blood pressure is 50 mm Hg/palp. Air movement is
normal and breath sounds are clear to auscultation.
The skin feels cool and capillary refill time is 4
seconds. The brachial pulse is weak. His abdomen
is distended.
A young mother presents to the ED with a 6-
month-old boy who has had vomiting for 24 hours.
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
What are the key
signs of illness in
this infant?
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
General assessment
Initial assessment
Management actions
Severity assessment
Secondary assessment (focused history,
detailed physical exami-nation, pulse oximetry,
and specialized assessment procedures)
Further interventions
Reassessment
Transport
Documentation
Copyright 2007 Seattle/King County EMS
What is a general assessment?
Formerly referred to as a first
impression,
a quick look to establish whether
there are significant life-threatening
problems that require immediate
interventions.
Copyright 2007 Seattle/King County EMS
The initial assessment is a hands-on
examination of the ABCDEs (airway,
breathing, circulation, disability,
exposure).
It builds on information you gathered
during your general assessment.
Initial Assessment
Copyright 2007 Seattle/King County EMS
The first stage of which is quick
screening (triage) to identify
those who need emergency treatment
those who are at special risk and should be
given priority
Or.... those who are non-urgent cases
Copyright 2007 Seattle/King County EMS
Not SICK
SICK
Stable
potential unstable.
UnStable
Level 1 Resuscitative
Level 2 Emergent
Level 3 Urgent
Level 4 Less urgent
Level 5 Non-urgent
Copyright 2007 Seattle/King County EMS
Why treat
children
differently?
Copyright 2007 Seattle/King County EMS
ANAK BUKAN DEWASA KECIL
The key differences to consider in
children are:
1. Weight
2. Anatomical size and shape
3. Physiological cardiovascular,
respiratory, immune function
4. Psychological intellectual ability
and emotional response
Copyright 2007 Seattle/King County EMS
Anatomical Differences
A childs anatomy differs in four significant
ways from an adults. They are:
Smaller airways
Less blood volume
Bigger heads
Vulnerable internal organs
Copyright 2007 Seattle/King County EMS
Anatomical Differences, cont'd
Large tongue in relation to
a small oropharynx
Diameter of the trachea is
smaller
Trachea is not rigid and
will collapse easily
Back of the head is
rounder and requires
careful positioning to keep
airway open
smaller airway
Copyright 2007 Seattle/King County EMS
Anatomical Differences, cont'd
Relatively smaller blood
volume
Approximately 70 cc of
blood for every 1kg (2 lbs)
of body weight
A 10 kg child has about
700cc of bloodabout the
volume of a medium sized
soda cup
smaller airway
less blood volume
Copyright 2007 Seattle/King County EMS
Anatomical Differences, cont'd
Head size is proportionally
larger
Prominent occiput and a
relatively straight cervical
spine
Neck and associated
support structures arent
well developed
Infants and small children
are prone to falling
because they are top
heavy
less blood volume
bigger heads
smaller airway
Copyright 2007 Seattle/King County EMS
Anatomical Differences, cont'd
Internal organs are not
well protected
Soft bones and cartilage
and lack of fat in the rib
cage make internal organs
susceptible to significant
internal injuries
Injury can occur with very
little mechanism or
obvious signs
bigger heads
internal organs
less blood volume
smaller airway
Copyright 2007 Seattle/King County EMS
Infants less than 6 months old
are obligate nasal breathers.
As the narrow nasal passages
are easily obstructed by
mucous secretions
In 3- to 8-year-olds,
adenotonsillar hypertrophy may
be a problem. This not only
tends to cause obstruction, but
also causes difficulty when the
nasal route is used to pass
pharyngeal, gastric or tracheal
tubes.
The anatomy of
the airway itself
changes with age,
and consequently
different problems
affect different
age groups
Copyright 2007 Seattle/King County EMS
The body surface area (BSA) to
weight ratio decreases with
increasing age.
Small children, with a high ratio,
lose heat more rapidly and
consequently are relatively more
prone to hypothermia.
At birth the head accounts for
19% of BSA; this falls to 9% by
the age of 15 years
Copyright 2007 Seattle/King County EMS
The infant has a relatively
greater metabolic rate and
oxygen consumption. This is
one reason for an increased
respiratory rate.
However, the tidal volume
remains relatively constant in
relation to body weight (57
ml/kg) through to adulthood
Copyright 2007 Seattle/King County EMS
Respiratory rate by age at rest
Age(Years) Respiratory rate/ MENIT
< 1 30 -40
1 - 2 25 -35
2 - 5 25 - 30
5 -12 20 - 25
>12 15 -20
Absolute size and relative body
proportions change with age.
Observations on children must be
related to their age.
Therapy in children must be related
to their age and weight.
The special psychological needs of
children must be considered.
Copyright 2007 Seattle/King County EMS
Development Considerations
Infant: 1 to 12 months
Toddler: 1 to 3 years
Preschool Age: 3 to 5 years
School Age: 6 to 12 years
Adolescent: 12 to 15 years
Copyright 2007 Seattle/King County EMS
PEMERIKSAAN
SULIT DILAKUKAN
KOMINIKASI SULIT
CENDRUNG KETAKUTAN
PENILAIAN KEGAWATAN
SULIT DILAKUKAN
Copyright 2007 Seattle/King County EMS
You must recognize the SICK child within the
first minute of contact.
Much of the information you need to make a
decision can be obtained without touching
the patient.
Copyright 2007 Seattle/King County EMS
PEDIATRIC ASSESSMENT TRIANGLE)
CIRCULATION
a rapid way to determine
physiologic stability
Copyright 2007 Seattle/King County EMS
Pediatric Assessment Triangle
There are three elements that you need to
assess in a pediatric patient in order to
determine SICK or NOT SICK:
Appearance
Work of breathing
Circulation to the skin
These three clinical indicators reflect the
overall status of a childs cardiovascular,
respiratory and neurologic systems.
Copyright 2007 Seattle/King County EMS
PAT, continued
Alertness
Distractibility
Consolability
Eye contact
Speech/cry
Spontaneous motor
activity
Color
airway
Copyright 2007 Seattle/King County EMS
PAT, continued
Abnormal position
Abnormal breath sounds
Retractions
Nasal flaring
airway
work of breathing
Copyright 2007 Seattle/King County EMS
PAT, continued
Color
Temperature
Capillary refill time
Pulse quality
airway
work of breathing
circulation
Copyright 2007 Seattle/King County EMS
PAT,
Alertness
Distractibility
Consolability
Eye contact
Speech/cry
Spontaneous motor
activity
Color
airway
appearance
Muscle tone
Conciousnes
Copyright 2007 Seattle/King County EMS
PAT,
Alertness
Distractibility
Consolability
Eye contact
Speech/cry
Spontaneous motor
activity
Color
airway
appearance
Copyright 2007 Seattle/King County EMS
T I L C S
Element YANG DINILAI
TONE
Extremities movement
move spontaneously or not
Interactivity Alertness: Is the child alert and
attentive to surroundings
Consolability
restless/ AGITATION Does comforting by
the caregiver alleviate agitation and crying?
Look/Gaze
Do the childs eyes follow your movement and maintain
eye contact with objects or people, or is there a vacant
gaze?
Speech/Cry
Are vocalizations strong, or are they weak, muffled, or
hoarse?
Copyright 2007 Seattle/King County EMS
A Child is Alert
V Child responds to Verbal stimulus
P Child responds to Painful stimulus
U Child is Unresponsive to any
stimulus
The AVPU
method
Copyright 2007 Seattle/King County EMS
Visable Movement/Respiratory Effort
REFLEKSI GANGGUAN OKSIGENASI, VENTILASI
Abnormal airway sounds
Abnormal positioning
Retractions
Nasal flaring
Copyright 2007 Seattle/King County EMS
PAT,
Abnormal
Increased excessive (nasal
flaring, retractions or
abdominal muscle use) or
decreased absent
respiratory effort
or noisy breathing.
work of breathing
Copyright 2007 Seattle/King County EMS
PAT,
Normal:
Breathing appears
regular without
excessive respiratory muscle
effort or
audible respiratory sounds
work of breathing
Copyright 2007 Seattle/King County EMS
Element
Explanation
Abnormal
airway sounds
Altered speech, stridor, wheezing
or grunting
Abnormal
positioning
Head bobbing, SNIFFING,
TRIPOTING,
Retractions
Supraclavicular, intercostal or
substernal retractions of the chest
wall
Flaring
Nasal Flaring
Characteristics of Work of Breathing
Copyright 2007 Seattle/King County EMS
PAT,
Color
Temperature
Capillary refill time
Pulse quality
circulation
Inadequate perfusion of
vital organs leads to
compensatory
vasoconstriction in non-
essential anatomic areas,
especially the skin.
Therefore circulation to
skin reflects overall
adequacy of perfusion
Copyright 2007 Seattle/King County EMS
Characteristic of
CIRCULATION TO SKIN
ELEMENT
Explanation
Pallor
White skin coloration from
lack of peripheral blood
Mottling
Patchy skin discoloration, with
patches of cyanosis, due to
vascular instability or
Cyanosis
Bluish discoloration of skin
and mucus
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
SIRKULASI KULIT
N
+
0
+ / 0
0
0
N
N
N
0
N/0
DISTRESS PERNAFSAN
GAGAL NAFAS
SYOK
GANGGUAN METABOLIK
GANGGUAN PRIMER SSP
Copyright 2007 Seattle/King County EMS
Normal
Appearance
Increased
Work of Breathing
MEANS RESPIRATORY DISTRESS
Normal Circulation
Copyright 2007 Seattle/King County EMS
MEANS RESPIRATORY FAILURE
Increased or
Decreased Work
of Breathing
Abnormal
Appearance
Normal circulation
Copyright 2007 Seattle/King County EMS
Abnormal
Appearance
Poor Circulation to Skin
MEANS SHOCK
Copyright 2007 Seattle/King County EMS
Poor Circulation to
Skin
Normal
Appearance
MEANS OBSERVE
Copyright 2007 Seattle/King County EMS
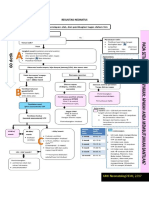
Pediatric Primary Survey
After completing the Triangle, begin a more
complete pediatric primary survey.
Copyright 2007 Seattle/King County EMS
A Airway
B Breathing
C Circulation
D Disability
E Exposure
Penilaian fisik
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Evaluation of Respiratory
Performance
Respiratory Rate and Regularity
Level of Consciousness
Color of the Skin and Mucous
Membranes
Respiratory Mechanics
Copyright 2007 Seattle/King County EMS
Respiratory Mechanics
Head Bobbing
Nasal Flaring
Retractions
Grunting
Stridor
Wheezing or Prolonged Exhalation
Copyright 2007 Seattle/King County EMS
LAJU/ FREKUENSI PERNAFASAN
RETRAKSI
STRIDOR INSPIRASI / EKSPIRASI
GRUNTING
PENGGUNAAN OTOT BANTU NAFAS
NAFAS CUPING HIDUNG
Gangguan pernafasan berat
Depresi SSP
Penyakit neuro muskular
Tidak bisa
dinilai pada
USAHA NAFAS/ KINERJA PERNAFASAN
BREATHING
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
FREKUENSI NAFAS
USIA (TAHUN) FREKUENSI/ MENIT
< 1 30 -40
2-5 20 - 30
5-12 15 - 20
>12 12 - 16
DIPENGARUHI DEMAM, NYERI, EMOSI/ TAKUT
FREK > 60 POTENSIAL GAGAL NAFAS
retraksi, kesadaran
Copyright 2007 Seattle/King County EMS
World Health Organization criteria for the
diagnosis of tachypnoea
Age months Respiratory frequency
Breaths/min-1
< 2 month > 60
212 > 50
> 12
> 40
Copyright 2007 Seattle/King County EMS
Respirations
Abnormal respirations are a common
sign of illness or injury.
Count respirations for 30 seconds.
In children less than 3 years, count the
rise and fall of the abdomen.
Note effort of breathing.
Listen for noises.
Copyright 2007 Seattle/King County EMS
INTERPRETATION of BREATH SOUNDS
Sound Cause
Stridor Upper airway obstruction
Wheezing Lower airway obstruction
Expiratory
grunting
Inadequate oxygenation
Inspiratory
crackles
Fluid/mucus/blood in the
Absent breath
sounds despite
increased work of
breathing
Complete airway obstruction
(upper or lower airway)
Pleural fluid, consolidation,
or pneumothorax
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
STATUS KARDIO VASKULAR
EFEK PADA ORGAN LAIN
STATUS MENTAL
CIRCULATION
Copyright 2007 Seattle/King County EMS
STATUS KARDIO VASKULAR
FREKUENSI DENYUT TAKIKARDI:TANDA HIPOKSIA,
PERFUSI BURUK ( demam, sakit,
takut
BRADIKARDI: HIPOKSIA, ISKEMIA
ISI DAN TEKANAN
(VOLUME NADI)
CAPILLARY REFIL NORMAL < 2 DETIK
TEKANAN DARAH
PRODUKSI URIN
HIPOTENSI : PRETERMINAL
1 2 cc/ kgBB/jam
Skin Signs
Feel for
temperature
and moisture.
Estimate
capillary refill.
Copyright 2007 Seattle/King County EMS
FREKUENSI JANTUNG
TEKANAN SISTOLIK MINIMAL
70 + { 2 x umur (tahun) }
USIA FREKUENSI
< 3 bulan 85 - 200
3 bln 2 thn 100 - 190
3 10 tahun 60 -140
Pulse
In infants, feel over the brachial or femoral area.
In older children, use the carotid artery.
Count for at least 1 minute.
Note strength of the pulse.
Copyright 2007 Seattle/King County EMS
STATUS NEUROLOGIK
Copyright 2007 Seattle/King County EMS
A
ALERT
V
RESPONS TO VOICE
P
RESPONS TO PAIN
U
UN RESPONSIVE
A V P U
CARA CEPAT MENILAI KESADARAN
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
SKALA KOMA GLASGOW < 4 tahun
AKTIFITAS RESPONS NILAI
Buka mata Spontan
Karena suara
Karena nyeri
Tidak ada
4
3
2
1
Motorik Menurut perintah/spontan
Lokalisasi nyeri
Menarik karena nyeri
Fleksi karena nyeri
Ekstensi karena nyeri
Tidak ada
6
5
4
3
2
1
Lisan ( Verbal) Terorientasi,tersenyum
Menangis berhubungan
Menangis tdak konsistent
iritabel
Tidak ada
5
4
3
2
1
Copyright 2007 Seattle/King County EMS
SKALA KOMA GLASGOW 4 15 tahun
AKTIFITAS RESPONS NILAI
Buka mata Spontan
Karena suara
Karena nyeri
Tidak ada
4
3
2
1
Motorik Menurut perintah
Lokalisasi nyeri
Menarik karena nyeri
Fleksi karena nyeri
Ekstensi karena nyeri
Tidak ada
6
5
4
3
2
1
Lisan ( Verbal) Terorientasi
Kacau/ bingung
Kata-kata tidak tepat
Suara tidak khas
Tidak ada
5
4
3
2
1
Copyright 2007 Seattle/King County EMS
TINDAKAN LANJUT
MENERUSKAN RESUSITASI
PEMERIKSAAN /PEMANTAUAN
LEBIH LANJUT
MERUJUK
Copyright 2007 Seattle/King County EMS
A young mother presents to the ED with a 6-
month-old boy who has had constant vomiting for
24 hours.
The infant is lying still and has poor muscle tone.
He is irritable if touched, and his cry is weak. There
are no abnormal airway sounds, retractions, or
flaring. He is pale and mottled. The respiratory rate
is 30 breaths/min, heart rate is 180 beats/min, and
blood pressure is 50 mm Hg/palp. Air movement is
normal and breath sounds are clear to
auscultation. The skin feels cool and capillary refill
time is 4 seconds. The brachial pulse is weak. His
abdomen is distended.
Copyright 2007 Seattle/King County EMS
Respiratory Emergencies
Respiratory distress is a state where a child is
able to maintain adequate oxygenation of the
blood, but only by increasing his or her work
of breathing.
Respiratory failure occurs when a child
cannot compensate for inadequate
oxygenation and the circulatory and
respiratory systems begin to collapse.
Copyright 2007 Seattle/King County EMS
Seizures
Seizures may be caused by:
Infection
Head trauma
Epilepsy
Electrolyte imbalance
Hypoglycemia
Toxic ingestion or exposure
Birth injury
Copyright 2007 Seattle/King County EMS
Trauma
Use appearance, work of breathing and
circulation to the skin in your assessment.
Mechanism of injury may also play a
factor when deciding whether the child is
SICK or NOT SICK.
Copyright 2007 Seattle/King County EMS
Drowning
The most important factors in drowning
are the duration and severity of hypoxia.
Restoring the ABCs is vital.
Hypothermia can occur in cold water
settings.
Copyright 2007 Seattle/King County EMS
Burns
Check for possible involvement of the
airway.
Make a quick estimate of the burned
body surface area.
Take care to avoid further contamination
of burn injuries by wearing gloves and
carefully dressing the wounds.
Copyright 2007 Seattle/King County EMS
82
Basic Life Support
Slide 83
S A F E approach
Copyright 2007 Seattle/King County EMS
Shout for help
Aprroach with care
Free from danger
Evaluate ABC
Copyright 2007 Seattle/King County EMS
Basic Life Support
Check for DANGER, stop and look
Check RESPONSE, verbal and tactile but
do not shake and shout
If conscious, assess carefully, patient may
still need urgent medical review
Continue to assess and manage
Airway
Breathing
Circulation
Slide 86
D
R
A
B
C
Slide 87
Basic Life Support Flowchart
Check for DANGER
Check for RESPONSE
CONSCIOUS
Make comfortable
Observe ABC
UNCONSCIOUS
Alert assistance
Clear airway
Apply head tilt and jaw support
Check for breathing
NOT BREATHING
2 rescue breaths
Check for pulse
Look for signs of life
BREATHING
Lateral position
Observe ABC
INADEQUATE PULSE
No signs of life
Commence CPR
Copyright 2007 Seattle/King County EMS
Slide 88
Basic Life Support
Airway
Breathing
Circulation
Copyright 2007 Seattle/King County EMS
Is The patient
able to
speak or cry ?
Copyright 2007 Seattle/King County EMS
Airway Assessment
Copyright 2007 Seattle/King County EMS
Slide 91
Observe for secretions and clear (suction)
Do not attempt a blind finger sweep
Open the airway
chin lift / jaw thrust
neutral position in infants
sniffing position in children
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Slide 95
Airway Opening Manoeuvres
Chin lift/head tilt
Infants
Neutral head position
with chin lift
Smaller children
Sniffing position
with chin lift
Copyright 2007 Seattle/King County EMS
Slide 96
Airway Opening Manoeuvres
Chin lift/head tilt
Older children/adults
Backward head tilt
with pistol grip
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Slide 99
Airway Opening Manoeuvres
Jaw thrust
Jaw thrust
Use when concerned re
cervical spine injury
May also facilitate
bag and mask
ventilation
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Slide 101
Foreign Body
Mild airway
obstruction
Effective Cough
Assess Severity
Severe airway
obstruction
Ineffective Cough
Unconscious
Call for
help
Commence
CPR
Conscious
Call for help
Give up to 5 back
blows
If not effective
Give up to 5 chest
thrusts
Encourage
coughing
Continue to check
victim until recovery
or deterioration
Call for help
Copyright 2007 Seattle/King County EMS
Slide 102
Foreign Body
Assess Severity
Effective Cough
Mild airway
obstruction
Encourage coughing
Continue to check
victim until recovery or
deterioration
Call for help
Copyright 2007 Seattle/King County EMS
Slide 103
Foreign Body
If there is an effective cough (mild
obstruction):
Encourage coughing
Continue to check victim until recovery or
deterioration
Call for help
Do not attempt any manoeuvres to remove
unless this is very easily done
Copyright 2007 Seattle/King County EMS
Slide 104
Foreign Body
Assess Severity
Severe airway
obstruction
Ineffective Cough
Unconscious Conscious
Call for help
Commence CPR
Call for help
Give up to 5 back blows
If not effective
Give up to 5 chest
thrusts
Copyright 2007 Seattle/King County EMS
Slide 105
Foreign Body
If there is an ineffective cough (severe
obstruction):
Unconscious
call for help, commence CPR
Conscious
call for help
give up to 5 back blows firm blows
between the shoulder blades using the heel
of the hand
Copyright 2007 Seattle/King County EMS
Slide 106
Back blows infant
Back blows small child
Copyright 2007 Seattle/King County EMS
Slide 107
Foreign Body
If 5 back blows unsuccessful:
Chest thrusts
identify same compression point as for CPR
give up to 5 chest thrusts
similar to compressions but sharper and delivered at a slower
rate
check to see if each thrust has relieved the airway obstruction
Infant
place in a head down supine position across rescuers thigh
Child/ older child / adult
may be placed in sitting or standing position
Note: this is not the same as a Heimlich manouvere this
manouvere is on the chest
Copyright 2007 Seattle/King County EMS
Airway Adjuncts
Copyright 2007 Seattle/King County EMS
Slide 109
Oropharyngeal Airways
Use: to keep the airway open in an unconscious patient
and to facilitate bag and mask ventilation
Use with caution
If airway is able to be maintained
with head positioning and jaw
support dont use an
oropharyngeal airway
Use of oropharyngeal airways:
size is imperative measure
from centre of teeth/mouth to
angle of the jaw layed across
the face
In the infant and small child
insert the concave side over
the tongue under direct vision.
This avoids damage to the
palate
Copyright 2007 Seattle/King County EMS
Slide 110
Oropharyngeal Airways
Potential problems:
Trauma
Obstruction
Illicit a gag reflex
causing aspiration
Laryngospasm
Vagal response
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Nasopharyngeal Airway
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Slide 114
Basic Life Support
Airway
Breathing
Circulation
Copyright 2007 Seattle/King County EMS
Evaluation of
Respiratory
Performance
Copyright 2007 Seattle/King County EMS
Slide 116
Look, Listen & Feel
10 seconds
Copyright 2007 Seattle/King County EMS
Breathing assessment
Respiratory Rate and
Regularity
Level of Consciousness
Color of the Skin and Mucous
Membranes
Respiratory Mechanics
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
The Need for Oxygen
0 1 minute: cardiac irritability
0 4 minutes: brain damage not likely
4 6 minutes: brain damage possible
6 10 minutes: brain damage very likely
> 10 minutes: irreversible brain damage
Within few minutes of
non-breathing, the
patient will suffer
irreversible damage.
The etiology of CPA in
pediatric is asphyxial
rather than
cardiogenic.
Oxygen therapy is the
most important and
initial treatments of
the sick child.
Initial assesment of the sick
child
Breathin
g
No
efective
breathin
g
Airway
Maintain
able
Un
maintain
able
Bag
mask
ventil
ation
NIPP
V
Intub
ation
s
oxyge
n
Airway
adjunc
t
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Simple mask
Copyright 2007 Seattle/King County EMS
partial rebreathing mask
low flow
nasal cannula.
simple oxygen mask.
high flow:
nonrebreathing masks.
Venturi masks.
oxygen hoods
oxygen tents.
Copyright 2007 Seattle/King County EMS
aspirationfsh.swf
Copyright 2007 Seattle/King County EMS
Slide 130
Breathing
If breathing is absent or inadequate:
Give 2 rescue breaths allowing about 1
second per inspiration
Sufficient breath to achieve gentle rise
and fall of chest, this means
puffs for an infant
breaths for a child
full breaths for an older
child/adult
Copyright 2007 Seattle/King County EMS
Slide 131
Bag and Mask
Correct mask size: cover mouth and nose only
Holding the mask: C-grip
C
Slide 132
Bag and Mask
a few technicalities...
Mask size
Bridge of nose to cleft of chin and sufficiently wide to cover
mouth
If too big you may get an air leak and also potential damage
especially with pressure applied to the eyes
Self inflating bag
Connect to oxygen 10L/Min
Once reservoir bag full, delivering 95-100% oxygen
Pressure release valve prevents too high pressure
Self-inflating, so can be used to deliver room air
Slide 133
Self Inflating Bag Sizes
Child (500ml) 2.5 25kg
Preterm
Infant
(240ml)
<2.5kg
Adult
(1600ml)
>25kg
Copyright 2007 Seattle/King County EMS
Slide 134
Checking Self Inflating Bags
Check that the self inflating bag compresses and
reinflates quickly and air is felt from patient outlet
Check the one way valve opens when self inflating
bag is compressed
Occlude patient outlet with hand and compress bag,
listen for the pressure release value to release
Take off oxygen reservoir bag and place over the
patient outlet. Inflate the reservoir bag checking for
holes
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Bag mask ventilation
Copyright 2007 Seattle/King County EMS
Bag to Mask Ventilation
Slide 138
Cricoid pressure:
Place two fingers on the level of the cricoid cartilage and apply
pressure (gently!)
Closes the oesophagus and straightens trachea
Dont release pressure until instructed or if the
patient actively vomits
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Monitor the Effectiveness of
Ventilation
Monitor the Effectiveness of
Ventilation
Visible chest rise with each breath.
Oxygen saturation.
Heart rate.
Blood pressure.
Distal air entry.
Patient response.
Copyright 2000 American Heart Association
Circulation 2000;102:253I--290I-
Bag-mask
ventilation
for child
victim
Contraindicated if
gag-reflex is intact
Higher success rate
Does NOT protect
from aspiration
Difficult to maintain
during transport
Copyright 2007 Seattle/King County EMS
Slide 147
Basic Life Support
Airway
Breathing
Circulation
Color of skin and capillary
refill
Strength of peripheral
and central pulses
Skin temperature
Obtain vascular access
(set IV lines)
Initiate volume
replacement
Perform chest
compressions
Defibrillate or provide
synchronized cardioversion
Initiate drug therapy
PULSE Check
Take no more than 10
seconds
Cardiac output in infancy and childhood largely
depends on heart rate.
No scientific data has identified an absolute heart
rate at which chest compressions should be
initiated;
the recommendation to provide cardiac
compression for a heart rate <60 bpm with
signs of poor perfusion
Copyright 2007 Seattle/King County EMS
Slide 151
Pulse Check
the smallprint
Do not check the pulse for longer than 10 seconds
If the patient shows no sign of life and a pulse cannot be
palpated in 10 seconds presume it to be absent!
Brachial is recommended in the infant as carotid pulse is
difficult to find and extension of the neck may compromise
the airway
Carotid pulse locate thyroid cartilage and feel to side, dont
feel too high due to the risk of inadvertently massaging the
carotid sinus, inducing bradycardia and hypotension
Locating and palpating carotid artery pulse
( > 1 year)
Locating and palpating brachial pulse
( < 1 year)
152
Copyright 2007 Seattle/King County EMS
Slide 153
Look for signs of life
No signs of life =
unconscious
unresponsive
not moving
not breathing normally
No signs of life commence external cardiac
compressions
Copyright 2007 Seattle/King County EMS
Slide 154
Circulation
Assess for pulse and
signs of life
If no pulse,
inadequate pulse or no
signs of life
commence ECC
CPR of the pediatric patient
155
PIJAT JANTUNG LUAR
Copyright 2007 Seattle/King County EMS
If no pulse palpated,
begin
chest compression
157
Copyright 2007 Seattle/King County EMS
Slide 158
Patient should be on a hard
surface eg. cardiac board
Rhythmic action, equal time for
compression and relaxation
Aim for a rate of 100
compressions per minute
Copyright 2007 Seattle/King County EMS
Slide 159
CPR Ratio
CIRCULATION
Hand Position
Depth of
Compression
INFANT
1/3 depth of chest
OLDER
CHILD
30 compressions: 2 breaths
5 cycles / 2 min
SMALL
CHILD
Lower half of sternum
Ratio and Rate
1 rescuer
The ratio describes the number of
compressions in relation to breaths,
the rate is the number of
compressions/breaths given per
minute.
Ratio and Rate
2 rescuers
15: 2
5 cycles/min
30: 2
5 cycles/2 min
Copyright 2007 Seattle/King County EMS
Slide 160
CPR Infant
Infant
Locate the lower half of the sternum
Two fingers one operator CPR
Two thumbs / two fingers if two operators
Ratio
Lone health care provider/ lay rescuer
30 compressions : 2 breaths (5 cycles per 2 minute)
Two health care providers
15 compressions : 2 breaths (5 cycles per 1
minute)
Aim for a rate of 100 compressions per
minute
Copyright 2007 Seattle/King County EMS
Slide 161
CPR Infant
Finger/Thumb
position:
lower 1/2 of the sternum
Compression depth:
1/3 of the depth of the chest
Copyright 2007 Seattle/King County EMS
Slide 162
CPR Ratio
CIRCULATION
Hand Position
Depth of
Compression
INFANT
1/3 depth of chest
OLDER
CHILD
30 compressions: 2 breaths
5 cycles / 2 min
SMALL
CHILD
Lower half of sternum
Ratio and Rate
1 rescuer
Ratio and Rate
2 rescuers
15: 2
5 cycles/min
30: 2
5 cycles/2 min
Copyright 2007 Seattle/King County EMS
Slide 163
CPR Small Child
Child: Up to 8 years
Use the heel of one hand
Locate lower half of sternum
Ratio
Lone health care provider/ lay rescuer
30 compressions : 2 breaths (5 cycles per 2 minute)
Two health care providers
15 compressions : 2 breaths (5 cycles per 1 minute)
Aim for a rate of 100 compressions per minute
Copyright 2007 Seattle/King County EMS
Slide 164
CPR Ratio
CIRCULATION
Hand Position
Depth of
Compression
INFANT
1/3 depth of chest
OLDER
CHILD
30 compressions: 2 breaths
5 cycles / 2 min
SMALL
CHILD
Lower half of sternum
Ratio and Rate
1 rescuer
Ratio and Rate
2 rescuers
15: 2
5 cycles/min
30: 2
5 cycles/2 min
Copyright 2007 Seattle/King County EMS
Slide 165
CPR Older Child/Adult
Older child/adult i.e.>9years
Use two hands
Locate lower half of sternum
Ratio:
Lone health care provider/ lay rescuer or
two health care providers
30 compressions : 2 breaths (5 cycles per 2
minute)
Aim for a rate of 100 compressions per minute
Pressure is exerted through the heel of the hand,
with arm/s straight, using body weight as the
compression force
Copyright 2007 Seattle/King County EMS
Slide 166
CPR
(Small and older child)
Compression depth: 1/3 of chest
CPR older child/ adult
1/3
CPR small child
Copyright 2007 Seattle/King County EMS
Slide 167
CPR
ARC recommend minimum interruptions of
ECC and CPR should not be interrupted to
check for signs of life
Ineffective CPR:
too gentle
too slow
incorrect hand position
too many interruptions
Copyright 2007 Seattle/King County EMS
Locating finger position for chest compressions in
infant (< 1 year)
Imagine a line drawn between the nipples
Place 2 fingers on sternum 1 fingers width below line.
Depress - 1 in.
At least 100 per min
1 breath to every 5 compressions
168
Copyright 2007 Seattle/King County EMS
Locating hand position for chest compressions in
child (> 1 year)
Use 2-3 fingers to locate lower margin of rib cage.
Follow rib margin to base of sternum (xiphoid process)
Over 8 yr
Place other hand on top of hand on sternum
Depress 1 - 2 in
80-100 per min
2 breaths to every 15 compressions
169
Copyright 2007 Seattle/King County EMS
1 ~ 8 yr
Use heel of one hand
Depress 1 1 in
100 per min
One-rescuer
1 breath to every 5 compressions
Two-rescuer
2 breaths to every 15 compressions
170
Copyright 2007 Seattle/King County EMS
Copyright 2000 American Heart Association
Circulation 2000;102:253I--290I-
Brachial pulse check in infant
Copyright 2007 Seattle/King County EMS
Copyright 2000 American Heart Association
Circulation 2000;102:253I--290I-
Carotid pulse check in child
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Circulation 2000;102:253I--290I-
One-hand chest compression
technique in child
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
Copyright 2007 Seattle/King County EMS
After each compression
allow the chest to recoil
fully
because complete chest
reexpansion improves
blood flow into the heart
Copyright 2007 Seattle/King County EMS
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Fullsize SBAR Report SheetDokumen1 halamanFullsize SBAR Report SheetShane LambertBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Diabetic KetoacidosisDokumen16 halamanDiabetic Ketoacidosisdrtpk100% (2)
- OB - Normal Labor and DeliveryDokumen51 halamanOB - Normal Labor and DeliveryJosh Matthew Rosales33% (3)
- Letting Go by Atul GawandeDokumen18 halamanLetting Go by Atul Gawandetakoyakilovers100% (2)
- Case Presentation: - Vuppu BhavaniDokumen53 halamanCase Presentation: - Vuppu BhavaniLohith Kumar MenchuBelum ada peringkat
- Kdigo 2012 CKD GLDokumen163 halamanKdigo 2012 CKD GLOkky Sari Rahayu100% (1)
- Monitoring AnesthesiaDokumen39 halamanMonitoring AnesthesiaAnonymous 8w9QEGBelum ada peringkat
- Test Bank For Physical Examination and Health Assessment 1st Canadian Edition by JarvisDokumen10 halamanTest Bank For Physical Examination and Health Assessment 1st Canadian Edition by JarvisThomas White100% (22)
- User Manual Buble Cpap PDFDokumen7 halamanUser Manual Buble Cpap PDFmamahosieleBelum ada peringkat
- 2016 Sep RECALLDokumen49 halaman2016 Sep RECALLkyahuaBelum ada peringkat
- Final PPT SiDokumen38 halamanFinal PPT SiSaad IqbalBelum ada peringkat
- Lesson 3. Physiological Basis of BehaviorDokumen46 halamanLesson 3. Physiological Basis of BehaviorMary Ann DimayugaBelum ada peringkat
- Gagal Ginjal Akut Dan KronikDokumen29 halamanGagal Ginjal Akut Dan Kronikaironi_irsyahmaBelum ada peringkat
- Ferritin and Vitamin D Levels and Its Relation To Bone Diseases in Thalassemic Adults: A Hospital-Based Retrospective Cohort StudyDokumen8 halamanFerritin and Vitamin D Levels and Its Relation To Bone Diseases in Thalassemic Adults: A Hospital-Based Retrospective Cohort StudyAnonymous 8w9QEGBelum ada peringkat
- International Journal of Gerontology: Hidetoshi Aihara, Masaki Tago, Toru Oishi, Naoko E. Katsuki, Shu-Ichi YamashitaDokumen5 halamanInternational Journal of Gerontology: Hidetoshi Aihara, Masaki Tago, Toru Oishi, Naoko E. Katsuki, Shu-Ichi YamashitaAnonymous 8w9QEGBelum ada peringkat
- PsDokumen6 halamanPsAnonymous 8w9QEGBelum ada peringkat
- Jact03i2p107 PDFDokumen5 halamanJact03i2p107 PDFJonathan WelchBelum ada peringkat
- Hepatology 04Dokumen7 halamanHepatology 04Fedhi As'adi THearthiefBelum ada peringkat
- 327overviewonthalassemias AreviewDokumen14 halaman327overviewonthalassemias AreviewAnonymous 8w9QEGBelum ada peringkat
- Nej Mo A 1306801Dokumen11 halamanNej Mo A 1306801Anonymous 8w9QEGBelum ada peringkat
- 10 11648 J Ajim 20190701 13Dokumen3 halaman10 11648 J Ajim 20190701 13Anonymous 8w9QEGBelum ada peringkat
- NIH Public Access: Vitamin D Metabolism, Mechanism of Action, and Clinical ApplicationsDokumen21 halamanNIH Public Access: Vitamin D Metabolism, Mechanism of Action, and Clinical ApplicationsAndreas HadinataBelum ada peringkat
- SerialDokumen1 halamanSerialHendri Cuplizk NamaquBelum ada peringkat
- SerialDokumen1 halamanSerialHendri Cuplizk NamaquBelum ada peringkat
- Bahan Kuliah. Semester - 7.Dokumen32 halamanBahan Kuliah. Semester - 7.Anonymous 8w9QEGBelum ada peringkat
- Health Promotion Presentation: Ibrahim Saruvaan Faculty of Health Science Maldives National UniversityDokumen28 halamanHealth Promotion Presentation: Ibrahim Saruvaan Faculty of Health Science Maldives National UniversityAnonymous 8w9QEGBelum ada peringkat
- SerialDokumen1 halamanSerialHendri Cuplizk NamaquBelum ada peringkat
- KDIGO AKI Guideline DownloadDokumen141 halamanKDIGO AKI Guideline DownloadSandi AuliaBelum ada peringkat
- SerialDokumen1 halamanSerialHendri Cuplizk NamaquBelum ada peringkat
- Data AwalDokumen1.798 halamanData AwalAnonymous 8w9QEGBelum ada peringkat
- Data AwalDokumen1.798 halamanData AwalAnonymous 8w9QEGBelum ada peringkat
- Hospital Palembang: Silvia Triratna Pediatric Critical Care Division Dept of Child Health RSUP Mohammad HusinDokumen170 halamanHospital Palembang: Silvia Triratna Pediatric Critical Care Division Dept of Child Health RSUP Mohammad HusinAnonymous 8w9QEGBelum ada peringkat
- BLSBLOKSDokumen116 halamanBLSBLOKSAnonymous 8w9QEGBelum ada peringkat
- Bahan Kuliah Gagal JantungDokumen14 halamanBahan Kuliah Gagal JantungAnonymous 8w9QEGBelum ada peringkat
- Concise Anatomy For AnesthesiaDokumen149 halamanConcise Anatomy For AnesthesiaAnonymous 8w9QEGBelum ada peringkat
- AnestesiDokumen11 halamanAnestesiAnonymous 8w9QEGBelum ada peringkat
- MonitoringDokumen18 halamanMonitoringAnonymous 8w9QEGBelum ada peringkat
- Abtahi 2020Dokumen9 halamanAbtahi 2020Rati Ramayani AbidinBelum ada peringkat
- D Dimer Test in VTEDokumen35 halamanD Dimer Test in VTEscribmedBelum ada peringkat
- Pathology Review BookDokumen5 halamanPathology Review BookAnas AliagaBelum ada peringkat
- Shedding Light: On Depressive, Anxiety and Sleep Disorders in Parkinson'S DiseaseDokumen246 halamanShedding Light: On Depressive, Anxiety and Sleep Disorders in Parkinson'S DiseaseTeguh priambodoBelum ada peringkat
- Nicolas, Krizha-Drug StudyDokumen12 halamanNicolas, Krizha-Drug StudyKrizha Angela NicolasBelum ada peringkat
- Topical Finasteride Consent Form April 2017Dokumen6 halamanTopical Finasteride Consent Form April 2017Krsmanovic ZoranBelum ada peringkat
- World No-Tobacco DayDokumen2 halamanWorld No-Tobacco DayAkankshaBelum ada peringkat
- 50 Studies Questioning Vaccine SafetyDokumen5 halaman50 Studies Questioning Vaccine SafetyshifanahmedBelum ada peringkat
- Resusitasi NeonatusDokumen7 halamanResusitasi NeonatusIqbal Miftahul HudaBelum ada peringkat
- EMS Airflow BrochureDokumen2 halamanEMS Airflow BrochureMELHEM_J8008Belum ada peringkat
- Bird Mark 7A Respirator BrochureDokumen2 halamanBird Mark 7A Respirator BrochureLos Infantes Ska Jazz100% (4)
- 9650-0301-01 Rev. MDokumen48 halaman9650-0301-01 Rev. MCarlos AndresBelum ada peringkat
- Hirschsprung's Disease, PDFDokumen1 halamanHirschsprung's Disease, PDFMr. LBelum ada peringkat
- Burn Management by Tajuu Seid: Surgical WardDokumen33 halamanBurn Management by Tajuu Seid: Surgical Wardelias adugnaBelum ada peringkat
- BIOLOGYDokumen5 halamanBIOLOGYDiana NurulBelum ada peringkat
- Spinal SurgeryDokumen19 halamanSpinal SurgerySalomeSibashviliBelum ada peringkat
- Sas 39Dokumen2 halamanSas 39Sistine Rose LabajoBelum ada peringkat
- TALLY 79 Respondents FinalDokumen7 halamanTALLY 79 Respondents FinalMarissa AsimBelum ada peringkat
- Philippine College of Science and Technology College of NursingDokumen21 halamanPhilippine College of Science and Technology College of NursingAijem RyanBelum ada peringkat
- Nama: Khoirus Viestaria NIM: 135130101111035 Kelas: 2013/CDokumen2 halamanNama: Khoirus Viestaria NIM: 135130101111035 Kelas: 2013/CDina SahmirandaBelum ada peringkat
- Intramedullary Spinal Cord Tumors: Part II - Management Options and OutcomesDokumen10 halamanIntramedullary Spinal Cord Tumors: Part II - Management Options and OutcomeszixzaxoffBelum ada peringkat