Human Respiratory System and Mechanics
Diunggah oleh
Abdul Qadir100%(1)100% menganggap dokumen ini bermanfaat (1 suara)
237 tayangan105 halaman- conducting portion: transports air. - respiratory portion: carries out gas exchange. Respiratory bronchioles alveolar ducts air sacs called alveoli upper respiratory tract is all conducting lower respiratory tract has both conducting and respiratory portions.
Deskripsi Asli:
Judul Asli
Human Respiratory System and Mechanics.ppt
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPT, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Ini- conducting portion: transports air. - respiratory portion: carries out gas exchange. Respiratory bronchioles alveolar ducts air sacs called alveoli upper respiratory tract is all conducting lower respiratory tract has both conducting and respiratory portions.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
100%(1)100% menganggap dokumen ini bermanfaat (1 suara)
237 tayangan105 halamanHuman Respiratory System and Mechanics
Diunggah oleh
Abdul Qadir- conducting portion: transports air. - respiratory portion: carries out gas exchange. Respiratory bronchioles alveolar ducts air sacs called alveoli upper respiratory tract is all conducting lower respiratory tract has both conducting and respiratory portions.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 105
RESPIRATORY SYSTEM
Organization and Functions of
the Respiratory System
Structural classifications:
upper respiratory tract
lower respiratory tract.
Functional classifications:
Conducting portion: transports air.
1. Nose
2. nasal cavity
3. Pharynx
4. Larynx
5. Trachea
6. progressively smaller airways, from the primary bronchi
to the bronchioles
Organization and Functions of
the Respiratory System
Functional classifications: continued
Conducting portion: transports air.
Respiratory portion: carries out gas exchange.
respiratory bronchioles
alveolar ducts
air sacs called alveoli
Upper respiratory tract is all conducting
Lower respiratory tract has both conducting and
respiratory portions
4
Respiratory System Functions
1. Breathing (pulmonary ventilation):
consists of two cyclic phases:
inhalation, also called inspiration
exhalation, also called expiration
Inhalation draws gases into the lungs.
Exhalation forces gases out of the lungs.
2. Gas exchange: O
2
and CO
2
External respiration
External environment and blood
Internal respiration
Blood and cells
25-6
Respiratory System Functions
3. Gas conditioning:
Warmed
Humidified
Cleaned of particulates
4. Sound production:
Movement of air over true vocal cords
Also involves nose, paranasal sinuses, teeth,
lips and tongue
5. Olfaction (act or process of smelling):
Olfactory epithelium over superior nasal
conchae
6. Defense:
Course hairs, mucus, lymphoid tissue
25-7
Upper Respiratory Tract
Composed of
1. the nose
2. the nasal cavity
3. the paranasal sinuses
4. the pharynx (throat)
5. and associated structures.
All part of the conducting portion of the
respiratory system.
8
Upper Respiratory Tract
Paranasal Sinuses
Paranasal sinuses:
In four skull bones
paired air spaces
decrease skull bone weight
Named for the bones in which they are housed.
frontal
ethmoidal
sphenoidal
maxillary
Communicate with the nasal cavity by ducts.
Covered with the same pseudostratified ciliated
columnar epithelium as the nasal cavity.
10
Pharynx
Common to both the respiratory and
digestive systems.
Commonly called the throat.
Funnel-shaped
slightly wider superiorly and narrower
inferiorly.
Originates posterior to the nasal and oral
cavities
Extends inferiorly near the level of the
bifurcation of the larynx and esophagus.
Common pathway for both air and food.
Pharynx
Walls:
lined by a mucosa
contain skeletal muscles primarily used for
swallowing.
Flexible lateral walls
distensible
to force swallowed food into the esophagus.
Partitioned into three adjoining regions:
nasopharynx
oropharynx
laryngopharynx
Nasopharynx
Superiormost region of the pharynx.
Location:
posterior to the nasal cavity
superior to the soft palate
separates it from the posterior part of the oral cavity.
Normally, only air passes through.
Soft palate
Blocks material from the oral cavity and oropharynx
elevates when we swallow.
Auditory tubes
paired
In the lateral walls of the nasopharynx
connect the nasopharynx to the middle ear.
Pharyngeal tonsil
posterior nasopharynx wall
single
commonly called the adenoids.
25-15
Oropharynx
The middle pharyngeal region.
Location:
Immediately posterior to the oral cavity.
Bounded by the soft palate superiorly,
the hyoid bone inferiorly.
Common respiratory and digestive pathway
both air and swallowed food and drink pass through.
2 pairs of muscular arches
anterior palatoglossal arches
posterior palatopharyngeal arches
form the entrance from the oral cavity.
Lymphatic organs
provide the first line of defense against ingested or inhaled foreign
materials.
Palatine tonsils
on the lateral wall between the arches
Lingual tonsils
At the base of the tongue.
25-16
Laryngopharynx
Inferior, narrowed region of the pharynx.
Location:
Extends inferiorly from the hyoid bone
is continuous with the larynx and esophagus.
Terminates at the superior border of the esophagus
is equivalent to the inferior border of the cricoid cartilage in the
larynx.
The larynx (voice box) forms the anterior wall
Lined with a nonkeratinized stratified squamous
epithelium (mucus membrane)
Permits passage of both food and air.
25-17
Lower Respiratory Tract
Conducting portion
Larynx
Trachea
Bronchi
bronchioles and their associated structures
Respiratory portion of the respiratory
system
respiratory bronchioles
alveolar ducts
alveoli
25-18
Larynx
Short, somewhat cylindrical airway
Location:
bounded posteriorly by the laryngopharynx,
inferiorly by the trachea.
Prevents swallowed materials from
entering the lower respiratory tract.
Conducts air into the lower respiratory
tract.
Produces sounds.
25-19
Larynx
Nine pieces of cartilage
three individual pieces
Thyroid cartilage
Cricoid cartilage
Epiglottis
three cartilage pairs
Arytenoids: on cricoid
Corniculates: attach to arytenoids
Cuniforms:in aryepiglottic fold
held in place by ligaments and muscles.
Intrinsic muscles: regulate tension on true vocal
cords
Extrinsic muscles: stabilize the larynx
20
25-21
Trachea
A flexible, slightly rigid tubular organ
often referred to as the windpipe.
Extends through the mediastinum
immediately anterior to the esophagus
inferior to the larynx
superior to the primary bronchi of the lungs.
Anterior and lateral walls of the trachea are supported by
15 to 20 C-shaped tracheal cartilages.
cartilage rings reinforce and provide some rigidity to the
tracheal wall to ensure that the trachea remains open (patent) at
all times
cartilage rings are connected by elastic sheets called anular
ligaments
22
25-23
Trachea
At the level of the sternal angle, the trachea bifurcates into two
smaller tubes, called the right and left primary bronchi.
Each primary bronchus projects laterally toward each lung.
The most inferior tracheal cartilage separates the primary
bronchi at their origin and forms an internal ridge called the
carina.
25-24
Bronchial Tree
A highly branched system
air-conducting passages
originate from the left and right primary bronchi.
Progressively branch into narrower tubes as they diverge
throughout the lungs before terminating in terminal
bronchioles.
Primary bronchi
Incomplete rings of hyaline cartilage ensure that they remain open.
Right primary bronchus
shorter, wider, and more vertically oriented than the left primary
bronchus.
Foreign particles are more likely to lodge in the right primary
bronchus.
25-25
Bronchial Tree
Primary bronchi
enter the hilum of each lung
Also entering hilum:
pulmonary vessels
lymphatic vessels
nerves.
Secondary bronchi (or lobar bronchi)
Branch of primary bronchus
left lung:
two lobes
two secondary bronchi
right lung
three lobes
three secondary bronchi.
Tertiary bronchi (or segmental bronchi)
Branch of secondary bronchi
left lung is supplied by 8 to 10 tertiary bronchi.
right lung is supplied by 10 tertiary bronchi
supply a part of the lung called a bronchopulmonary segment.
26
25-27
Respiratory Bronchioles, Alveolar
Ducts, and Alveoli
Contain small saccular outpocketings called alveoli.
An alveolus is about 0.25 to 0.5 millimeter in diameter.
Its thin wall is specialized to promote diffusion of gases
between the alveolus and the blood in the pulmonary
capillaries.
Gas exchange can take place in the respiratory bronchioles and
alveolar ducts as well as in the lungs, which contain
approximately 300400 million alveoli.
The spongy nature of the lung is due to the packing of millions
of alveoli together.
28
29
30
31
25-32
Lungs: Gross Anatomy
Each lung has a conical shape.
Its wide, concave base rests upon the muscular
diaphragm.
Its relatively blunt superior region, called the apex or
(cupola), projects superiorly to a point that is slightly
superior and posterior to the clavicle.
Both lungs are bordered by the thoracic wall anteriorly,
laterally, and posteriorly, and supported by the rib cage.
Toward the midline, the lungs are separated from each
other by the mediastinum.
The relatively broad, rounded surface in contact with the
thoracic wall is called the costal surface of the lung.
33
34
35
36
37
25-38
Pleura and Pleural Cavities
The outer surface of each lung and the adjacent
internal thoracic wall are lined by a serous
membrane called pleura, which is formed from
simple squamous epithelium.
The outer surface of each lung is tightly
covered by the visceral pleura, while the
internal thoracic walls, the lateral surfaces of
the mediastinum, and the superior surface of
the diaphragm are lined by the parietal pleura.
The parietal and visceral pleural layers are
continuous at the hilum of each lung.
25-39
Pleura and Pleural Cavities
The outer surface of each lung is tightly covered by the visceral pleura,
while the internal thoracic walls, the lateral surfaces of the mediastinum,
and the superior surface of the diaphragm are lined by the parietal pleura.
The potential space between these serous membrane layers is a pleural
cavity.
The pleural membranes produce a thin, serous fluid that circulates in the
pleural cavity and acts as a lubricant, ensuring minimal friction during
breathing.
40
25-41
Lymphatic Drainage
Lymph nodes and vessels are located within the connective
tissue of the lung as well as around the bronchi and pleura.
The lymph nodes collect carbon, dust particles, and pollutants
that were not filtered out by the pseudostratified ciliated
columnar epithelium.
42
LUNG MECHANICS
MECHANICS
the branch of physics that deals with the action of
forces on bodies and with motion, comprised of
kinetics, statics, and kinematics.
the theoretical and practical application of this
science to machinery, mechanical appliances, etc.
the technical aspects of working of something;
mechanism; structure.
the science of designing, constructing, and
operating machines
LUNG MECHANICS
Some Terminologies and Facts
LUNG MECHANICS
Some Terminologies and Facts
LUNG MECHANICS
Some Terminologies and Facts
Spirometer
Pulmonary Volumes & Capacities
Spirometry: capacities
Remember: A capacity is always a
sum of certain lung volumes
TLC = IRV + TV + ERV + RV
VC = IRV+ TV + ERV
FRC = ERV + RV
IC = TV + IRV
Spirometry
4 volumes and 4 capacities
Effort dependent
Values vary to height, age, sex &
physical training
IRV = 2.5 L * IC = 3 L
TV = 0.5 L * VC = 4.5 L
ERV = 1.5 L * FRC = 2.5 L
RV = 1 L * TLC = 5.5 L
Spirometry
REMEMBER: Spirometry cannot measure
Residual Volume (RV) thus Functional
Residual Capacity (FRC) and Total Lung
Capacity (TLC) cannot be determined using
spirometry alone.
FRC and TLC can be determined by 1) Helium
dilution, 2) Nitrogen washout, or 3) body
plethysmography
Physiological Lung Structure
Lung weighs 1.5% of body weight
1 kg in 70 kg adult
Alveolar tissue is 60% of lung weight
Alveoli have very large surface area
70 m
2
internal surface area
40 x the external body surface area
Short diffusion pathway for gases
Permits rapid & efficient gas exchange into blood
1.5 m between air & alveolar capillary RBC
Blood volume in lung - 500ml (10% of total blood volume)
Respiratory Mechanics
Multiple factors required to alter
lung volumes
Respiratory muscles generate force to inflate
& deflate the lungs
Tissue elastance & resistance impedes
ventilation
Distribution of air movement within the
lung, resistance within the airway
Overcoming surface tension within alveoli
The Breathing Cycle
Airflow requires a pressure gradient
Air flow from higher to lower pressures
During inspiration alveolar pressure is sub-
atmospheric allowing airflow into lungs
Higher pressure in alveoli during expiration
than atmosphere allows airflow out of lung
Changes in alveolar pressure are generated
by changes in pleural pressure
MUSCLES OF BREATHING
Muscles of Inspiration
MUSCLES OF BREATHING
Muscles of Exspiration
Inspiration
Active Phase Of Breathing Cycle
Motor impulses from brainstem activate muscle
contraction
Phrenic nerve (C 3,4,5) transmits motor stimulation to
diaphragm
Intercostal nerves (T 1-11) send signals to the external
intercostal muscles
Thoracic cavity expands to lower pressure in pleural space
surrounding the lungs
Pressure in alveolar ducts & alveoli decreases
Fresh air flows through conducting airways into terminal
air spaces until pressures are equalized
Lungs expand passively as pleural pressure falls
The act of inhaling is negative-pressure ventilation
Muscles of Inspiration: Diaphragm
Most Important Muscle Of Inspiration
Responsible for 75% of inspiratory effort
Thin dome-shaped muscle attached to the lower ribs, xiphoid process,
lumbar vertebra
Innervated by Phrenic nerve (Cervical segments 3,4,5)
During contraction of diaphragm
Abdominal contents forced downward & forward causing increase in vertical
dimension of chest cavity
Rib margins are lifted & moved outward causing increase in the transverse
diameter of thorax
Diaphragm moves down 1cm during normal inspiration
During forced inspiration diaphragm can move down 10cm
Paradoxical movement of diaphragm when paralyzed
Upward movement with inspiratory drop of intrathoracic pressure
Occurs when the diaphragm muscle is denervated
Diaphragm
Movement of Thorax During
Breathing Cycle
Movement of Diaphragm
67
25-68
Thoracic Wall Dimensional
Changes During Respiration
Lateral dimensional changes occur
with rib movements.
Elevation of the ribs increases the
lateral dimensions of the thoracic
cavity, while depression of the ribs
decreases the lateral dimensions of
the thoracic cavity.
69
Inspiration Expiration
Muscles that Move the Ribs
The scalenes help increase thoracic cavity dimensions
by elevating the first and second ribs during forced
inhalation.
The ribs elevate upon contraction of the external
intercostals, thereby increasing the transverse
dimensions of the thoracic cavity during inhalation.
Contraction of the internal intercostals depresses the
ribs, but this only occurs during forced exhalation.
Normal exhalation requires no active muscular effort.
A small transversus thoracis extends across the inner
surface of the thoracic cage and attaches to ribs 26.
It helps depress the ribs.
Muscles that Move the Ribs
Two posterior thorax muscles also assist with respiration.
These muscles are located deep to the trapezius and
latissimus dorsi, but superficial to the erector spinae
muscles.
The serratus posterior superior elevates ribs 25 during
inhalation, and the serratus posterior inferior depresses ribs
812 during exhalation.
In addition, some accessory muscles assist with respiratory
activities.
The pectoralis minor, serratus anterior, and
sternocleidomastoid help with forced inhalation, while the
abdominal muscles (external and internal obliques,
transversus abdominis, and rectus abdominis) assist in active
exhalation.
73
74
Muscles of Inspiration
External Intercostal Muscles
The external intercostal muscles connect to adjacent ribs
Responsible for 25% of inspiratory effort
Motor neurons to the intercostal muscles originate in the respiratory
centers of the brainstem and travel down the spinal cord. The motor
nerves leave the spinal cord via the intercostal nerves. These originate
from the ventral rami of T1 to T11, they then pass to the chest wall
under each rib along with the intercostal veins and arteries.
Contraction of EIM pulls ribs upward & forward
Thorax diameters increase in both lateral & anteroposterior directions
Ribs move outward in bucket-handle fashion
Intercostals nerves from spinal cord roots innervate EIMs
Paralysis of EIM does not seriously alter inspiration because
diaphragm is so effective but sensation of inhalation is decreased
Muscles of respiration
Muscles of Inspiration
Accessory Muscles
These muscles assist with forced inspiration
during periods of stress or exercise
Scalene Muscle
Attach cervical spine to apical rib
Elevate the first two ribs during forced inspiration
Sternocleidomastoid Muscle
Attach base of skull (mastoid process) to top of
sternum and clavicle medially
Raise the sternum during forced inspiration
Boyles Law
The pressure of a gas decreases if the volume of
the container increases, and vice versa.
When the volume of the thoracic cavity increases even
slightly during inhalation, the intrapulmonary pressure
decreases slightly, and air flows into the lungs
through the conducting airways.
Air flows into the lungs from a region of higher
pressure (the atmosphere) into a region of lower
pressure (the intrapulmonary region).
When the volume of the thoracic cavity decreases
during exhalation, the intrapulmonary pressure
increases and forces air out of the lungs into the
atmosphere.
Goals of Respiration
Primary Goals Of The Respiration System
Distribute air & blood flow for gas
exchange
Provide oxygen to cells in body tissues
Remove carbon dioxide from body
Maintain constant homeostasis for
metabolic needs
Functions of Respiration
Respiration divided into four functional events:
1.Mechanics of pulmonary ventilation
2.Diffusion of O
2
& CO
2
between alveoli and
blood
3.Transport of O
2
& CO
2
to and from tissues
4.Regulation of ventilation & respiration
External & Internal Respiration
External Respiration
Mechanics of breathing
The movement of gases
into & out of body
Gas transfer from lungs
to tissues of body
Maintain body &
cellular homeostasis
Internal Respiration
Intracellular oxygen
metabolism
Cellular transformation
Krebs cycle aerobic
ATP generation
Mitochondria & O2
utilization
REGULATION OF
BREATHING
Respiratory Cycle and its control
Respiration rate is the number of
breaths per minute
Human respiration rate is controlled
by a part of the brain called the
medulla
Sends signals to adjust levels of oxygen
present in your body by changing your
breathing rate
Ventilation Control by Respiratory
Centers of the Brain
The trachea, bronchial tree, and lungs are innervated
by the autonomic nervous system.
The autonomic nerve fibers that innervate the heart
also send branches to the respiratory structures.
The involuntary, rhythmic activities that deliver and
remove respiratory gases are regulated in the
brainstem.
Regulatory respiratory centers are located within the
reticular formation through both the medulla
oblongata and pons.
85
CHEMICAL CONTROL OF BREATHING
CHEMICAL CONTROL OF BREATHING
PULMONARY VENTILATION
Pulmonary Ventilation
Pulmonary ventilation is a measure of the rate of ventilation,
referring to the total exchange of air between the lungs and the
ambient or surrounding air.
Pulmonary Ventilation is the total volume of gas per minute
inspired or expired.
The main purpose of ventilation is to maintain an
optimal composition of alveolar gas
Alveolar gas acts as stabilizing buffer compartment between
the environment & pulmonary capillary blood
Oxygen constantly removed from alveolar gas by blood
Carbon dioxide continuously added to alveoli from blood
O
2
replenished & CO
2
removed by process of ventilation, by simple
diffusion.
The two ventilation phases (inspiration & expiration) provide
this stable alveolar environment
Breathing is the act of creating inflow & outflow of air between
the atmosphere and the lung alveoli
Pulmonary Ventilation
Pulmonary Ventilation
Lung Volume and Capacities
Lung Volume and Capacities
Lung Volumes and Capacities
Intrathoracic Pressure
Intrapulmonary Pressure
Composition of Inspired Air,
Expired Air and Alveolar Air
Carriage of Gases by blood
Compliance of the Lungs
Compliance is a measure of the distensibility of the lungs
Compliance = change in lung volume/ change in lung
pressure
Cpulm = DVpulm / Dppulm
Normal static compliance is 70-100 ml of air/cm of H2O
transpulmonary pressure
Different compliances for inspiration & expiration
based on the elastic forces of lungs
Compliance reduced by higher or lower lung volumes, higher
expansion pressures, venous congestion, alveolar edema,
atelectasis & fibrosis
Compliance increased with age & emphysema secondary to
alterations of elastic fibers
Elastic Forces of the Lung
Elastic Lung Tissue
Elastin & Collagen fibers of
lung parenchyma
Natural state of these fibers
is contracted coils
Elastic force generated by
the return to this coiled state
after being stretched and
elongated
The recoil force assists to
deflate lungs
Surface Air-fluid
Interface
2/3 of total elastic force in
lung
Surface tension of H2O
Complex synergy between air
& fluid holds alveoli open
Without air in the alveoli a
fluid filled lung has only lung
tissue elastic forces to resist
volume changes
Surfactant in the alveoli fluid
reduces surface tension,
keeps alveoli from collapsing
Factors Determining Airway Resistance
Lung Volume
Linear relationship between lung volumes & conductance
of airway resistance
As lung volume is reduced - airway resistance increases
Bronchial Smooth Muscle
Contraction of airways increases resistance
Bronchoconstriction caused by PSN, acetylcholine, low
Pco
2,
direct stimulation, histamine, environmental, cold
Density & Viscosity Of Inspired Gas
Increased resistance to flow with elevated gas density
Changes in density rather than viscosity have more
influence on resistance
Organs in the Respiratory System
STRUCTURE FUNCTION
nose / nasal cavity
warms, moistens, & filters air as it is
inhaled
pharynx (throat) passageway for air, leads to trachea
larynx
the voice box, where vocal chords are
located
trachea (windpipe)
keeps the windpipe "open"
trachea is lined with fine hairs called
cilia which filter air before it reaches the
lungs
bronchi
two branches at the end of the trachea,
each lead to a lung
bronchioles
a network of smaller branches leading from
the bronchi into the lung tissue &
ultimately to air sacs
alveoli
the functional respiratory units in the lung
where gases are exchanged
Malfunctions & Diseases of the Respiratory System
asthma
severe allergic reaction
characterized by the
constriction of bronchioles
bronchitis
inflammation of the lining of
the bronchioles
emphysema
condition in which the alveoli
deteriorate, causing the lungs
to lose their elasticity
pneumonia
condition in which the alveoli
become filled with fluid,
preventing the exchange of
gases
lung cancer
irregular & uncontrolled
growth of tumors in the lung
tissue
Anda mungkin juga menyukai
- Anatomy and Physiology of the Respiratory SystemDokumen43 halamanAnatomy and Physiology of the Respiratory Systemflex gyBelum ada peringkat
- Respiratory System CopDokumen44 halamanRespiratory System CopAsad KHANBelum ada peringkat
- Structure of Digestive SystemDokumen8 halamanStructure of Digestive System32 Mhd RayisBelum ada peringkat
- OxygenationDokumen57 halamanOxygenationassumptaBelum ada peringkat
- Lecture 9 Physiology of BloodDokumen125 halamanLecture 9 Physiology of BloodAhmed MohammedBelum ada peringkat
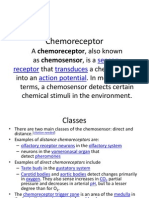
- Chemo ReceptorDokumen8 halamanChemo ReceptorCheryl Lyn SanchezBelum ada peringkat
- Fluid and Electrolyte ConceptDokumen40 halamanFluid and Electrolyte ConceptBarnis Lady Mentari AlamdaniBelum ada peringkat
- PHYSIOLOGY OF BALANCE: A MULTISENSORY INTEGRATION PROCESSDokumen18 halamanPHYSIOLOGY OF BALANCE: A MULTISENSORY INTEGRATION PROCESSKunal ShahBelum ada peringkat
- Mechanism of Urine FormationDokumen5 halamanMechanism of Urine FormationovacuteBelum ada peringkat
- 1.1 Introduction To Human Anatomy - 2018-2019 PDFDokumen11 halaman1.1 Introduction To Human Anatomy - 2018-2019 PDFسيف محمود شاكر حسنBelum ada peringkat
- Intravenous FluidsDokumen19 halamanIntravenous Fluidsblack pink in ur area 21100% (1)
- Acidosis and AlkalosisDokumen10 halamanAcidosis and AlkalosisNealeth NanquilBelum ada peringkat
- Physiology of BalanceDokumen27 halamanPhysiology of Balancemulkihakam21Belum ada peringkat
- BSC Nursing - Cardiac OutputDokumen10 halamanBSC Nursing - Cardiac OutputDIKSHA RANI DEKABelum ada peringkat
- Ye Examination: Nabila Kanwal Farah Naz Hina Idrees Saba Mansha Muqadas AshiqDokumen40 halamanYe Examination: Nabila Kanwal Farah Naz Hina Idrees Saba Mansha Muqadas AshiqMisbha AzizBelum ada peringkat
- Anatomy and Physiology of Digestive SystemDokumen34 halamanAnatomy and Physiology of Digestive SystemIan IsidroBelum ada peringkat
- Histology Lower GIT Microscopic Features Small Large IntestineDokumen27 halamanHistology Lower GIT Microscopic Features Small Large IntestineArwa100% (2)
- L - 2 Physiology of Respiration IIDokumen25 halamanL - 2 Physiology of Respiration IIkaukab azimBelum ada peringkat
- Anatomy 2nd-U-2 Lymphatic SystemDokumen52 halamanAnatomy 2nd-U-2 Lymphatic Systemsinte beyuBelum ada peringkat
- Adult BLSDokumen50 halamanAdult BLSdianBelum ada peringkat
- I.V Fluid: PathologyDokumen7 halamanI.V Fluid: PathologyruchikaBelum ada peringkat
- Anatomy Exam 1 Study GuideDokumen3 halamanAnatomy Exam 1 Study Guidefishycocoa1Belum ada peringkat
- Anatomy and Physiology II Course OutcomesDokumen50 halamanAnatomy and Physiology II Course OutcomesShirley LourdesBelum ada peringkat
- Renal SystemDokumen65 halamanRenal Systemxarae23Belum ada peringkat
- BSC Nursing Year 2Dokumen43 halamanBSC Nursing Year 2Kishan PatelBelum ada peringkat
- Evolution of NursingDokumen34 halamanEvolution of NursingUpendra YadavBelum ada peringkat
- LipidsDokumen15 halamanLipidsZam-zamBelum ada peringkat
- Nervous System Structure and FunctionsDokumen46 halamanNervous System Structure and FunctionssureshdassBelum ada peringkat
- Disorders of Potassium Metabolism: Causes, Manifestations and Management (KOMAHS 3rd Year Medicine 9200Dokumen20 halamanDisorders of Potassium Metabolism: Causes, Manifestations and Management (KOMAHS 3rd Year Medicine 9200Solomon Fallah Foa SandyBelum ada peringkat
- Body TissuesDokumen29 halamanBody TissuesPurplesmilezBelum ada peringkat
- Sensory SystemDokumen65 halamanSensory SystemATP_101Belum ada peringkat
- Anatomy and Physiology Musculoskeletal System Chap 6 - 2401Dokumen18 halamanAnatomy and Physiology Musculoskeletal System Chap 6 - 2401slyfoxkittyBelum ada peringkat
- Emergency Nursing ManagementDokumen7 halamanEmergency Nursing Managementyan219Belum ada peringkat
- 16 Sense OrgansDokumen79 halaman16 Sense OrgansvanderphysBelum ada peringkat
- Lymph SystemDokumen7 halamanLymph SystemghaiathBelum ada peringkat
- Overview of GI Tract FunctionsDokumen85 halamanOverview of GI Tract FunctionsDerón Asbery HolmesBelum ada peringkat
- Internal RespirationDokumen9 halamanInternal RespirationRhose ReyesBelum ada peringkat
- Meningitis & EncephalitisDokumen18 halamanMeningitis & EncephalitisZola Ismu ArjunantoBelum ada peringkat
- Hip JointDokumen25 halamanHip JointHashim OmarBelum ada peringkat
- Respiratory SystemDokumen36 halamanRespiratory SystemPritha Bhuwapaksophon100% (1)
- Analyzing and Defining Medical TermsDokumen7 halamanAnalyzing and Defining Medical Termsmarcus colgroveBelum ada peringkat
- Respiratory SystemDokumen56 halamanRespiratory SystemLorenz PasensyosoBelum ada peringkat
- Plasma MembraneDokumen2 halamanPlasma MembraneKerry JiangBelum ada peringkat
- Fluid Therapy in Various ConditionsDokumen62 halamanFluid Therapy in Various ConditionsAndy F MonroeBelum ada peringkat
- Anatomy of Circulatory SystemDokumen56 halamanAnatomy of Circulatory SystemLina Wijaya100% (1)
- Renal System FunctionsDokumen41 halamanRenal System Functionskeerthi krishnaBelum ada peringkat
- Large Intestine.Dokumen15 halamanLarge Intestine.Shimmering MoonBelum ada peringkat
- NCD Prevention & Control StrategiesDokumen80 halamanNCD Prevention & Control Strategiesbiniam yohannesBelum ada peringkat
- Head To Toe ExaminationDokumen6 halamanHead To Toe ExaminationFadillah Raisyah MBelum ada peringkat
- Anatomy and PhysiologyDokumen24 halamanAnatomy and PhysiologyGillarhymesBelum ada peringkat
- Human Anatomy,: First Edition Mckinley & O'LoughlinDokumen40 halamanHuman Anatomy,: First Edition Mckinley & O'LoughlinAgung PurmanaBelum ada peringkat
- History Taking: DR - Kamaran HassanDokumen41 halamanHistory Taking: DR - Kamaran HassanSrush AliBelum ada peringkat
- Composition and Function of Blood ComponentsDokumen17 halamanComposition and Function of Blood ComponentsPrakash Kumar Nayak100% (1)
- Large IntestineDokumen50 halamanLarge Intestinemex Gbrekorkos100% (1)
- 8.2 Mechanisms of BreathingDokumen44 halaman8.2 Mechanisms of Breathingwickedbiology101Belum ada peringkat
- Esophagus: - Development ofDokumen14 halamanEsophagus: - Development ofJonathan00711Belum ada peringkat
- Introduction To Physiology: General Physiology The Cell HomeostasisDokumen38 halamanIntroduction To Physiology: General Physiology The Cell HomeostasisAnanta Subedi100% (1)
- 7th-The Alimentary SystemDokumen25 halaman7th-The Alimentary Systemprasun_v100% (1)
- UntitledDokumen62 halamanUntitledManaye MamuyeBelum ada peringkat
- Respiratory SystemDokumen49 halamanRespiratory SystemVishal SharmaBelum ada peringkat
- Improving Communication Skills of Pharmacy StudentDokumen13 halamanImproving Communication Skills of Pharmacy StudentAbdul QadirBelum ada peringkat
- Bio-Sheet A 1Dokumen15 halamanBio-Sheet A 1Abdul QadirBelum ada peringkat
- 7 - Air Ticket - Ameer Baksh-1Dokumen1 halaman7 - Air Ticket - Ameer Baksh-1Abdul QadirBelum ada peringkat
- CreditCardStatement4495051 - 2087 - 18-Jun-21Dokumen1 halamanCreditCardStatement4495051 - 2087 - 18-Jun-21Abdul QadirBelum ada peringkat
- The Sky, The Road, The Glass of Wine: On Translating FaizDokumen15 halamanThe Sky, The Road, The Glass of Wine: On Translating FaizAbdul QadirBelum ada peringkat
- Ay2022 2023 Humphrey Fellowship Essay Questions Section of The Online ApplicationDokumen5 halamanAy2022 2023 Humphrey Fellowship Essay Questions Section of The Online ApplicationAbdul QadirBelum ada peringkat
- Professional Development Training For Researchers: New CourseDokumen20 halamanProfessional Development Training For Researchers: New CourseAbdul QadirBelum ada peringkat
- 8th Extended Notification B.A B.SC (S) Exam 2019Dokumen1 halaman8th Extended Notification B.A B.SC (S) Exam 2019Abdul QadirBelum ada peringkat
- Us 5866157Dokumen11 halamanUs 5866157Abdul QadirBelum ada peringkat
- Regulating Tourist Guides and Drug ImportsDokumen23 halamanRegulating Tourist Guides and Drug ImportsM TofeeqBelum ada peringkat
- Unit 3 Text 1 Reading Sample Cover LetterDokumen2 halamanUnit 3 Text 1 Reading Sample Cover LetterAbdul QadirBelum ada peringkat
- 2013 Investigation of Swelling Behavior of Dome Matrix® Drug Delivery Module by X Ray TomographyDokumen6 halaman2013 Investigation of Swelling Behavior of Dome Matrix® Drug Delivery Module by X Ray TomographyAbdul QadirBelum ada peringkat
- Hypromellose - A Choice of Polymer in Extended Release Tablet FormulationDokumen16 halamanHypromellose - A Choice of Polymer in Extended Release Tablet FormulationAbdul QadirBelum ada peringkat
- Caring CNA Seeks New OpportunityDokumen3 halamanCaring CNA Seeks New OpportunityVallejosFernandoMartinBelum ada peringkat
- 1 s2.0 0378517388902694 Main PDFDokumen8 halaman1 s2.0 0378517388902694 Main PDFAbdul QadirBelum ada peringkat
- Role of MediaDokumen2 halamanRole of MediaAbdul QadirBelum ada peringkat
- First Fortynine ST 030256 MBPDokumen8 halamanFirst Fortynine ST 030256 MBPAbdul QadirBelum ada peringkat
- Physicochemical Properties of Drug SubstancesDokumen12 halamanPhysicochemical Properties of Drug SubstancesAbdul QadirBelum ada peringkat
- Extreme Living After Humans A PDFDokumen3 halamanExtreme Living After Humans A PDFAbdul QadirBelum ada peringkat
- Physicochemical Properties of Drug Substances PDFDokumen17 halamanPhysicochemical Properties of Drug Substances PDFAbdul Qadir100% (1)
- Complete HolmesDokumen989 halamanComplete HolmesDeepeshKediaBelum ada peringkat
- Udas Naslain by Abdullah Hussain PDFDokumen502 halamanUdas Naslain by Abdullah Hussain PDFNadeem Ahmed Zafar72% (29)
- Anatomy/physiology BookDokumen428 halamanAnatomy/physiology BookTushant100% (4)
- Opiod Detoxification PDFDokumen8 halamanOpiod Detoxification PDFAbdul QadirBelum ada peringkat
- HEC Recognized Curriculum For DOctor of Physdiotherapy 2010Dokumen196 halamanHEC Recognized Curriculum For DOctor of Physdiotherapy 2010Faisal QureshiBelum ada peringkat
- The Drugs Act, 1976Dokumen32 halamanThe Drugs Act, 1976Dr-Usman KhanBelum ada peringkat
- A Brief History of Herbalism - Lesson 1Dokumen41 halamanA Brief History of Herbalism - Lesson 1btopacioBelum ada peringkat
- DNA Damage Induced - Differen PDFDokumen14 halamanDNA Damage Induced - Differen PDFAbdul QadirBelum ada peringkat
- Ebola Therapy Protects Severel PDFDokumen2 halamanEbola Therapy Protects Severel PDFAbdul QadirBelum ada peringkat
- Isl201 PDFDokumen62 halamanIsl201 PDFAbdul Qadir100% (2)
- List of Doctors by SpecialtyDokumen6 halamanList of Doctors by Specialtykaushal shahBelum ada peringkat
- FEVER Approach (Paeds)Dokumen3 halamanFEVER Approach (Paeds)NorFarah Fatin AnuarBelum ada peringkat
- Complications-Colostomy: Rectal Discharge, Hernias, Blockages & MoreDokumen4 halamanComplications-Colostomy: Rectal Discharge, Hernias, Blockages & MorehaithamBelum ada peringkat
- What Type of Resistance Training Program Can Help Increase Muscle MassDokumen75 halamanWhat Type of Resistance Training Program Can Help Increase Muscle Massyokimura dimaunahanBelum ada peringkat
- Sexually Transmitted InfectionsDokumen110 halamanSexually Transmitted Infectionstummalapalli venkateswara raoBelum ada peringkat
- Complex Regional Pain Syndrome in Adults - Second Edition - 0 PDFDokumen97 halamanComplex Regional Pain Syndrome in Adults - Second Edition - 0 PDFLotteDomineBelum ada peringkat
- Hyperthermia and Risk For AspirationDokumen3 halamanHyperthermia and Risk For AspirationAlmyr RimandoBelum ada peringkat
- 00-30juni 2023 Data Stok FLDokumen98 halaman00-30juni 2023 Data Stok FLSunaryo AryandaBelum ada peringkat
- PDFDokumen2 halamanPDFMohammed FasilBelum ada peringkat
- Pre Conference Final ProgDokumen2 halamanPre Conference Final ProgkeithlyndBelum ada peringkat
- Giant Skin TagDokumen2 halamanGiant Skin Tagshf.mxlikBelum ada peringkat
- Keeler Ophthalmoscope Bulb and Retinoscope Bulb ModelsDokumen1 halamanKeeler Ophthalmoscope Bulb and Retinoscope Bulb ModelsEDRAES17Belum ada peringkat
- Anticoagulant and Antiplatelet Medications and Dental Procedures ADADokumen8 halamanAnticoagulant and Antiplatelet Medications and Dental Procedures ADADeeBelum ada peringkat
- Dissertation Topics 2Dokumen21 halamanDissertation Topics 2Apollo Institute of Hospital Administration100% (1)
- Penelitian Pengembangan Minyak Atsiri Sebagai Aromaterapi Dan Potensinya Sebagai Produk Sediaan Farmasi MuchtaridiDokumen9 halamanPenelitian Pengembangan Minyak Atsiri Sebagai Aromaterapi Dan Potensinya Sebagai Produk Sediaan Farmasi MuchtaridiFitria Dewi 'uthie'Belum ada peringkat
- FORMAT Discharge PlanDokumen5 halamanFORMAT Discharge PlanButchay LumbabBelum ada peringkat
- DR Wong Teck WeeipadDokumen2 halamanDR Wong Teck Weeipadtwwong68Belum ada peringkat
- Hand Hygiene: Protocol For UWS ClinicsDokumen8 halamanHand Hygiene: Protocol For UWS ClinicsOliaBelum ada peringkat
- Hemorragic Post PartumDokumen10 halamanHemorragic Post PartumJihan NurlailaBelum ada peringkat
- Child Development Mannualfinal-SinhalaDokumen250 halamanChild Development Mannualfinal-SinhalaAshhara FazalBelum ada peringkat
- Grievously: News Item 9: EARTHQUAKE 2Dokumen2 halamanGrievously: News Item 9: EARTHQUAKE 2roxana_boraBelum ada peringkat
- Permission To Attend Hockey DayDokumen4 halamanPermission To Attend Hockey Dayapi-244287783Belum ada peringkat
- Curriculum Vita1Dokumen2 halamanCurriculum Vita1rajalashmiBelum ada peringkat
- Vitamins Are Organic Compounds Required in The Diet in Small Quantities To Perform Biological FunctionsDokumen70 halamanVitamins Are Organic Compounds Required in The Diet in Small Quantities To Perform Biological FunctionsRose LiteBelum ada peringkat
- Thyroid and Antithyroid Drugs - PPTX - 20231126 - 103419 - 0000Dokumen11 halamanThyroid and Antithyroid Drugs - PPTX - 20231126 - 103419 - 0000Vaishnavi SheteBelum ada peringkat
- Drug Study AdalatDokumen4 halamanDrug Study AdalatLea CelestialBelum ada peringkat
- Pathology - List - 89.8.20Dokumen25 halamanPathology - List - 89.8.20Mamula RiazBelum ada peringkat
- Case Study of Mrs. WalkerDokumen4 halamanCase Study of Mrs. WalkerPreet ChahalBelum ada peringkat
- IRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)Dokumen4 halamanIRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)analyn123Belum ada peringkat
- A Mindfulness Intervention For Children With Autism Spectrum DisorderDokumen155 halamanA Mindfulness Intervention For Children With Autism Spectrum Disorderclaughlinsr4721Belum ada peringkat