A Child With Wheeze
Diunggah oleh
Codillia Cheong0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
71 tayangan53 halamanMedicine
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPTX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniMedicine
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPTX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
71 tayangan53 halamanA Child With Wheeze
Diunggah oleh
Codillia CheongMedicine
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPTX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 53
Presented by,
Tan Yee Mun
Codillia Cheong Kai Shim
Wong Pui Seen
Tutorial Contents
Anatomy, embryology and physiology of the
respiratory and immune systems
Definition of wheeze and the differential diagnoses of
conditions causing it
Definition, pathophysiology, clinical features,
investigations,management and outcome of asthma
including acute exacerbations in children
Epidemiology of asthma in children in Malaysia
Grading of severity of chronic asthma and an acute
exacerbation
Tutorial Contents
Drugs and devices used in asthma
Allergic disorders: allergic rhinitis, allergic
conjunctivitis, atopic
eczema, urticaria, anaphylaxis, food and drug allergy,
insect bite hypersensitivity
Pathophysiology, clinical features, investigations,
management, complications and outcome of foreign
body inhalation in children
The clinical approach to a child with wheeze
Anatomy of Respiratory tract
Respiratory tract are
divided into
Upper respiratory tract
Entrance to larynx
Lower respiratory tract
Larynx to alveoli (trachea
to lungs)
Embryology
What structural aspects must be considered
in the process of respiration?
Trachea
Primary bronchi
Secondary bronchi
Tertiary bronchi
Bronchioles
Terminal bronchioles
Respiratory bronchioles with
start of alveoli outpouches
Alveolar ducts with outpouchings
of alveoli
conductive
portion
exchange
portion
External
Respiration
Internal
Respiration
Anatomy of Immune System
Physiology of Immune System
To discriminate self form non-self and to eliminate the
foreign substance
To protect the host against foreign antigen
Definition of Wheeze
Polyphonic(multiple pitch) noise coming from the
airways believed to represent many airways of different
dimensions vibrating from abnormal narrowing.
Differential Diagnoses of
Conditions that can cause
Wheezing
Transient early wheezing
Atopic asthma
Non-atopic asthma
Recurrent aspiration of feeds
Inhaled foreign body
Cystic fibrosis
Recurrent anaphylaxis in a child with food allergies
Congenital abnormality of lung, airway or heart
Idiopathic
Asthma
Definition of Asthma
Chronic airway inflammation leading to increase
airway responsiveness that leads to recurrent episodes
of wheezing, breathlessness, chest tightness and
coughing particularly at night or early morning.
Often associated with widespread but variable airflow
obstruction that is often reversible either
spontaneously or with treatment.
Reversible and variable airflow limitation as
evidenced by >15% improvement in PEFR (Peak
Expiratory Flow Rate), in response to administration of
a bronchodilator.
Recommendations to define pre-
school wheezing
2 main categories:
Episodic (viral) wheeze.
only wheeze with viral infections and are well between
episodes.
Multiple trigger wheezers
have discrete exacerbations and symptoms in between
these episodes. Triggers are smoke, allergens, crying,
laughing and exercise.
The presence of atopy (eczema, allergic rhinitis and
conjunctivitis) in the child or family supports the diagnosis
of asthma .
However, the absence of these conditions does not
exclude the diagnosis.
Pathophysiology of asthma
Clinical Features of Asthma
Symptoms worse at night and in the early morning
Symptoms that triggers (eg: exercise, pets, dust, cold
air, emotions, laughter)
Intervals symptoms (between acute exacerbation)
Personal or family history of an atopic disease
Positive response to asthma therapy.
Harrisons sulci
Depression at the base of
the thorax with muscular
insertion of the diaphragm
are called Harrisons sulci,
and are associated with
chronic obstructive airways
disease such as asthma
during childhood.
Management
Aim of management-
- To allow the child to lead a normal life by controlling
the symptoms and preventing exacerbations,
optimising pulmonary function, while minimizing
treatment and side effects.
Outcome of Asthma
Majority has a good prognosis.
Those more severe, persistent asthma cases , develop
longitudinal changes in lung function. ( impaired lung
function in childhood and decline in lung function in
adulthood)
Early intervention of anti-inflammatory therapy may
improve the short-term outcome of asthma.
Disease progression to nonreversible airflow
obstrcution may be observed in minority.
Epidemiology
Estimated prevalence of asthma in Malaysia is
4.2%. (The Star, May 2011)
International Studies on Asthma and Allergy
(ISAAC) has shown the prevalence of asthma
among school children is 10%. (Protocol Ed3)
Among children up to 14 yrs old has a
prevalence rate of 4.5% and age 15 years and
above is 4.1%. (The Star, May 2011)
Prevalence of childhood asthma is 24%, particullarly in
Malays and those living in urban areas. (Selangor,
2011)
A study of symptom control and severity of Asians
under 16 years old shows that 2.5% controlled while
53.4% uncontrolled asthma.(MIMS, Jul 2014)
As for severity, 24.5% had moderate to severe
persistent symptoms.
Participants of uncontrolled asthma were the most
frequent users of anti-asthmatic medication and
urgent healthcare services. (MIMS, Jul 2014)
Hospitalization was the most important factor
affecting life quality of Malaysian parents with
asthmatic child.
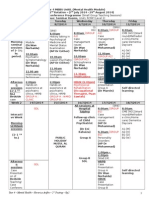
Grading of severity in asthma
1. Intermittent
Daylight symptoms less than once a week
Noctural symptoms less than once a month
No exercise induced symptoms
Brief, infrequent exacerbation not affecting sleep and
activity
Normal lung function
2. Persistent
Criteria Mild Moderate Severe
Daylight
Symptoms
>once a week Daily Daily
Noctural
Symptoms
>2x a month >once a week Daily
Exercise induced
symptom
Present Present Daily
Exacerbation
(affecting sleep
and activity)
> 1x/month >2x/month Frequently,
>2x/month
PERF/FEV1 >80% 60% - 80% <60%
PEFR: Peak Expiratoty Flow Metre FEV1: Forced Expiratory Vol in 1 sec
Acute exacerbation
Assessment of severity:
i. Diagnosis: cough,wheezing, breathless
ii.Triggering factor: food, exercise, drugs
iii.Severity: RR, RE, consious lvl.
Criteria for admission
Failure to respond to standard home treatment.
Failure to respond to nebulised beta 2 agonist.
Relapse with 4 hours of nebulised beta 2 agonists.
Severe acute asthma.
Drugs
Bronchodilators
Beta 2 Agonist (SABA, LABA)
Anticholinergic (Ipratropium bromide)
Inhaled Corticosteroids
Leukotriene receptor agonist (oral)
Theophylline
Prednisolone (Oral steroids)
Anti-IgE injection (Omalizumab)
Mnemonics
A - Adrenergics (Beta 2 Agonist)
- Albuterol
S - Steroids
T - Theophyline
H - Hydration (IV)
M - Mask O2
A - Anticholinergics
- Ipratropium bromide
Inhaler
Nebulizer
Only used in acute asthma where
oxygen is needed in addition to inhaled
drugs.
Allergic Disorders
Allergy - an altered state of reactivity to common
environmental antigens.
Most patients with allergy produce IgE antibodies to the
antigens; familial predisposition to allergic diseases
Allergic rhinitis
Allergic conjuntivitis
Ectopic eczema
Urticaria
Anaphylaxis
Food and drug allergy
Insect bite hypersensitivity
Sudden onset
if the chest does not rise when ventilation is first
attempted.
The most serious complication is complete obstruction
of the airway, recognized as sudden respiratory distress
followed by inability to speak or cough.
Three stages of symptoms:
1. Initial event violent paroxysms of coughing,
choking, gagging, and persistent monophonic wheeze.
2. Asymptomatic interval the foreign body
becomes lodged, reflexes fatigue, and the immediate
irritating symptoms subside.
3. Complications obstruction, erosion, or infection.
Complications include lung abcess, fever, cough,
hemoptysis, pneumonia, and atelectasis.
Most airway foreign bodies lodge in a bronchus (right
bronchus in 58% of cases); laryngeal or tracheal
locations occur in 10% of cases.
Bronchoscopy
x-ray
CT or MRI
Abdominal thrust using
Heimlich maneuver
Back blows and chest thrusts
Infant younger than 1 yr
Conscious child - permits to cough
spontaneously until coughing is not
effective (or aphonic), respiratory
distress and stridor increase
Unconscious - the airway is opened
with the head-tilt/chin-lift maneuver,
and ventilation is attempted.
If there is still no chest rise, a
combination of 5 back blows and 5
chest thrusts is administered.
Child older than 1 yr
A conscious child is administered a series of 5
abdominal thrusts (Heimlich manoeuvre) with the
child standing or sitting.
If the child is unconscious, this is done with the child
lying down.
1. Stand behind the patient
2. Encircle arms around the upper part of the abdomen
just below the patients rib cage
3. Give a sharp, forceful squeeze, forcing the diaphragm
sharply into the thorax.
Obstructive emphysema (air trapping) and shift
of the mediastinum toward the opposite side.
Clinical Approach to a Child with Wheeze
Age
Gradual or sudden onset, duration
Transient early wheezing or persistent and recurrent
wheezing
Preterm, maternal smoking
Allergens (dust mites, pollens, pets etc), other allergic
disorders, family history of allergic disorder, asthma
Feeds
References
European Respiratory Journals [Outcome of asthma :
longitudinal changes in lung function]
Illustrated Textbook of Paediatrics
Paediatrics Protocols
Anda mungkin juga menyukai
- Secrets of Korean MedicineDokumen70 halamanSecrets of Korean Medicineemedronho4550100% (3)
- Normal Labor and DeliveryDokumen10 halamanNormal Labor and Deliverymendato marcabanBelum ada peringkat
- Pedia Platinum (1st Edition)Dokumen546 halamanPedia Platinum (1st Edition)vinb100% (6)
- Health Science Health Profession Pregnancy Childbirth Postpartum Period Newborn MidwifeDokumen21 halamanHealth Science Health Profession Pregnancy Childbirth Postpartum Period Newborn MidwifeRiyaBelum ada peringkat
- Dermatology For The Small Animal PractitionerDokumen145 halamanDermatology For The Small Animal Practitionerсветлана бугаева100% (5)
- OB Chap 22 - Normal LaborDokumen4 halamanOB Chap 22 - Normal LaborChino Paolo SamsonBelum ada peringkat
- Dermatology: Questions & AnswersDokumen26 halamanDermatology: Questions & AnswersDev YadavBelum ada peringkat
- Personality DisorderDokumen87 halamanPersonality DisorderCodillia Cheong100% (2)
- Neonatal BLSDokumen18 halamanNeonatal BLSPatrickNichols0% (1)
- Canine Atopic DermatitisDokumen16 halamanCanine Atopic Dermatitisserbanbogdans536667% (3)
- LalpathlabsDokumen3 halamanLalpathlabsDOMINICBelum ada peringkat
- Syllabus ECCDokumen3 halamanSyllabus ECCLiezel CauilanBelum ada peringkat
- 29 Anti-Viral Drugs PDFDokumen43 halaman29 Anti-Viral Drugs PDFabhishek talokarBelum ada peringkat
- Antenatal Fetal MonitoringDokumen51 halamanAntenatal Fetal MonitoringCodillia Cheong100% (2)
- Paediatric AsthmaDokumen246 halamanPaediatric AsthmaOxana TurcuBelum ada peringkat
- Acute Respiratory Infection in ChildrenDokumen70 halamanAcute Respiratory Infection in Childrenmayadwintas100% (1)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Anatomy SpineDokumen31 halamanAnatomy SpineCodillia CheongBelum ada peringkat
- BLadder Outlet ObstructionDokumen28 halamanBLadder Outlet ObstructionCodillia Cheong100% (1)
- Triage and Disaster ManagementDokumen19 halamanTriage and Disaster ManagementCodillia CheongBelum ada peringkat
- HEPA B and PIDDokumen40 halamanHEPA B and PIDNica PinedaBelum ada peringkat
- CWU Psychiatry 1.1Dokumen8 halamanCWU Psychiatry 1.1Codillia CheongBelum ada peringkat
- PnemoniaDokumen38 halamanPnemoniaArjumand AliBelum ada peringkat
- System Disorder: Dermatitis and Acne: Atopic Dermatitis 57Dokumen1 halamanSystem Disorder: Dermatitis and Acne: Atopic Dermatitis 57Kassandra MerrillBelum ada peringkat
- Degenerative Diseases of SpineDokumen115 halamanDegenerative Diseases of SpineCodillia CheongBelum ada peringkat
- Community Psychiatry Gp5Dokumen34 halamanCommunity Psychiatry Gp5Codillia CheongBelum ada peringkat
- Maternal Sepsis and Sepsis ShockDokumen17 halamanMaternal Sepsis and Sepsis ShockAlvaro Andres Flores JimenezBelum ada peringkat
- MCNDokumen12 halamanMCNIan CarodanBelum ada peringkat
- Abnormal Menstruations AUB and Dysmenorrhea: Abebe C (MD)Dokumen34 halamanAbnormal Menstruations AUB and Dysmenorrhea: Abebe C (MD)adam0% (1)
- Febrile Seizure Case FileDokumen4 halamanFebrile Seizure Case Filehttps://medical-phd.blogspot.comBelum ada peringkat
- Prenatal Care by Connie Sussan AustenDokumen31 halamanPrenatal Care by Connie Sussan AustenNoraBelum ada peringkat
- Diagnosis of PregnancyDokumen22 halamanDiagnosis of PregnancyvrutipatelBelum ada peringkat
- Leopold's Maneuver ResearchDokumen4 halamanLeopold's Maneuver ResearchCarl Andre ReyesBelum ada peringkat
- MeaslesDokumen23 halamanMeaslesadwait marhattaBelum ada peringkat
- MANUAL OF PLACENTAL PATHOLOGY FinaleDokumen24 halamanMANUAL OF PLACENTAL PATHOLOGY FinaleAnonymous wE02eRBelum ada peringkat
- 6-Health Problems Common in PreschoolerDokumen36 halaman6-Health Problems Common in PreschoolerPam Lala100% (2)
- DystociaDokumen3 halamanDystociaRiajoy AsisBelum ada peringkat
- Essential Update: Pediatric Pneumonia May Be Effectively Treated With Twice-Daily AmoxicillinDokumen54 halamanEssential Update: Pediatric Pneumonia May Be Effectively Treated With Twice-Daily AmoxicillinYostesara Maurena SantosaBelum ada peringkat
- Complications in Third and Fourth Stage of LaborDokumen35 halamanComplications in Third and Fourth Stage of LaborHui Chen100% (2)
- Passenger: (Fetus and Placenta)Dokumen24 halamanPassenger: (Fetus and Placenta)Toni DomingoBelum ada peringkat
- Profile of A NewbornDokumen2 halamanProfile of A NewbornM.N MesaBelum ada peringkat
- Leprosy MsDokumen78 halamanLeprosy MsAmit Kochhar67% (3)
- Ps of LaborDokumen28 halamanPs of LaborErvina Luisa Delias CampusBelum ada peringkat
- Vaginal SeptumDokumen10 halamanVaginal SeptumLily YuriBelum ada peringkat
- Breastfeeding and HivDokumen30 halamanBreastfeeding and HivbxrbxrBelum ada peringkat
- Osh State UniversityDokumen14 halamanOsh State Universitykhuzaima9Belum ada peringkat
- Diagnosis of PregnancyDokumen26 halamanDiagnosis of PregnancyMounikaBelum ada peringkat
- Normal Conduct of LaborDokumen62 halamanNormal Conduct of LaborFaye Cabotaje LinganBelum ada peringkat
- Intrauterine Fetal Death: Prepared By: Roshni Adhikari Roshani Sunar Sabina Ranabhat Sadhana DevkotaDokumen15 halamanIntrauterine Fetal Death: Prepared By: Roshni Adhikari Roshani Sunar Sabina Ranabhat Sadhana DevkotaRoshni SunarBelum ada peringkat
- Minor Discomforts of Pregnancy - FlatulenceDokumen11 halamanMinor Discomforts of Pregnancy - FlatulenceAimee LynnBelum ada peringkat
- Pregnancy Induced HypertensionDokumen7 halamanPregnancy Induced HypertensionRalph Emerson RatonBelum ada peringkat
- Chiken PoxDokumen7 halamanChiken PoxShahzada KhurramBelum ada peringkat
- Seminar 2 (Paeds)Dokumen31 halamanSeminar 2 (Paeds)Jonathan YeohBelum ada peringkat
- The Neonatal Period (N2)Dokumen25 halamanThe Neonatal Period (N2)api-3721542100% (1)
- QuestionDokumen10 halamanQuestionserviceBelum ada peringkat
- Maternal and ChildDokumen33 halamanMaternal and Childjosephine100% (1)
- Contraceptive Options For Women and Couples With HIV: Intrauterine Device (Iud or Iucd)Dokumen23 halamanContraceptive Options For Women and Couples With HIV: Intrauterine Device (Iud or Iucd)Claudio UdjajaBelum ada peringkat
- Congenital AnomaliesDokumen22 halamanCongenital Anomaliesjessy100% (1)
- Pregnancy ChangesDokumen20 halamanPregnancy ChangesMj BrionesBelum ada peringkat
- 1st Cwu OngDokumen18 halaman1st Cwu Ongdila_ayubBelum ada peringkat
- Hypothyroidism in PregnancyDokumen29 halamanHypothyroidism in PregnancyhanaddulBelum ada peringkat
- Risk of Post Partum Infections-1Dokumen29 halamanRisk of Post Partum Infections-1gerryneutron100% (1)
- Placenta CirculationDokumen11 halamanPlacenta CirculationJason Jimmy Lee PillayBelum ada peringkat
- InfluenzaDokumen2 halamanInfluenzajohnndoeeBelum ada peringkat
- Nursing Care of Family During Labor and BirthhhDokumen6 halamanNursing Care of Family During Labor and BirthhhAudreySalvadorBelum ada peringkat
- Cerebral PalsyDokumen14 halamanCerebral PalsyWaode SittrisnawatiBelum ada peringkat
- Type B (Hib) Vaccine: Haemophilus InfluenzaeDokumen2 halamanType B (Hib) Vaccine: Haemophilus InfluenzaeEnce MalatambanBelum ada peringkat
- RubellaDokumen10 halamanRubellaKiran Kumar100% (1)
- Obg Icd-10 Pregnancy, Childbirth, PuerperiumDokumen11 halamanObg Icd-10 Pregnancy, Childbirth, PuerperiumarifianjuariBelum ada peringkat
- Anaemia in Pregnancy: By-Dr. Soumya.p (2nd Yr PG) Mod - Dr. Rita. D (Professor and Hod)Dokumen98 halamanAnaemia in Pregnancy: By-Dr. Soumya.p (2nd Yr PG) Mod - Dr. Rita. D (Professor and Hod)SoumyaBelum ada peringkat
- Abnormal Vaginal BleedingDokumen41 halamanAbnormal Vaginal BleedingmarkkerwinBelum ada peringkat
- (MMUNISATIONDokumen54 halaman(MMUNISATIONatharva sawantBelum ada peringkat
- Diarrhea: ChildrenDokumen16 halamanDiarrhea: ChildrenEmmi Valentina PardedeBelum ada peringkat
- Pediatric Respiratory EmergencyDokumen35 halamanPediatric Respiratory EmergencyImran FaisalBelum ada peringkat
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Surgical Problems in PregnancyDokumen37 halamanSurgical Problems in PregnancyCodillia CheongBelum ada peringkat
- MenorrhagiaDokumen36 halamanMenorrhagiaCodillia CheongBelum ada peringkat
- Asthma Devices: Taken From DR - Padmini's Elms (CSL Video) Hazirah's NotesDokumen7 halamanAsthma Devices: Taken From DR - Padmini's Elms (CSL Video) Hazirah's NotesCodillia CheongBelum ada peringkat
- AnaesthesiologyDokumen6 halamanAnaesthesiologyCodillia CheongBelum ada peringkat
- Final Pro 2015Dokumen3 halamanFinal Pro 2015Codillia CheongBelum ada peringkat
- Fever Case MXDokumen10 halamanFever Case MXCodillia CheongBelum ada peringkat
- Guidelines EctDokumen10 halamanGuidelines EctCodillia CheongBelum ada peringkat
- Schizophrenia: Group 2A (2014)Dokumen50 halamanSchizophrenia: Group 2A (2014)Codillia CheongBelum ada peringkat
- 1.mental Health - Gp2 NewDokumen6 halaman1.mental Health - Gp2 NewCodillia CheongBelum ada peringkat
- Environmental EmergencyDokumen4 halamanEnvironmental EmergencyJUDE MARIANO JR. ALBANCES CARLOSBelum ada peringkat
- Infant Formulas. Pediatr Rev 2011Dokumen13 halamanInfant Formulas. Pediatr Rev 2011Zeniff ArciveBelum ada peringkat
- Dermatitis Atopica Niños - Ingles PDFDokumen10 halamanDermatitis Atopica Niños - Ingles PDFESTEPHANY PAMELA GAMBINI ACOSTABelum ada peringkat
- Atopic Eczema and XerosisDokumen8 halamanAtopic Eczema and XerosisMirandaBelum ada peringkat
- Atopic Dermatitis and Skin Microbiome Ne PDFDokumen6 halamanAtopic Dermatitis and Skin Microbiome Ne PDFSmaranda ADBelum ada peringkat
- Look At, See or Watch - English Grammar Today - Cambridge Dictionary PDFDokumen220 halamanLook At, See or Watch - English Grammar Today - Cambridge Dictionary PDFMadhur BhutraBelum ada peringkat
- WAO 2019 Food Allergy Information SheetDokumen8 halamanWAO 2019 Food Allergy Information SheetNatasya Nuraini FajriBelum ada peringkat
- Nickel Allergy and Orthodontic Treatment: Lilian Staerkjaer and Torkil MenneDokumen6 halamanNickel Allergy and Orthodontic Treatment: Lilian Staerkjaer and Torkil MenneRockey ShrivastavaBelum ada peringkat
- Hamza DissertDokumen108 halamanHamza DissertMobin Ur Rehman KhanBelum ada peringkat
- Pityriasis Alba: Are You Confident of The Diagnosis?Dokumen3 halamanPityriasis Alba: Are You Confident of The Diagnosis?freska ayu wardhaniBelum ada peringkat
- Chapter 19 - Immunotoxicology of Meta - 2015 - Handbook On The Toxicology of MetDokumen20 halamanChapter 19 - Immunotoxicology of Meta - 2015 - Handbook On The Toxicology of MetChanWingSanBelum ada peringkat
- Top 5 Dermatologic Indications For Pentoxifylline in Dogs - NewDokumen8 halamanTop 5 Dermatologic Indications For Pentoxifylline in Dogs - NewdpcamposhBelum ada peringkat
- AsthmaDokumen4 halamanAsthmaIsabel CastilloBelum ada peringkat
- 15 Methodical Instruction CheilitesDokumen17 halaman15 Methodical Instruction CheilitesKarlina Dwi PutriBelum ada peringkat
- Asthma Small Group DiscussionDokumen12 halamanAsthma Small Group DiscussionLyca Mae AurelioBelum ada peringkat
- Allergic Contact DermatitisDokumen6 halamanAllergic Contact DermatitisCrysnaBelum ada peringkat
- Journal-ATOPIC DERMATITISDokumen16 halamanJournal-ATOPIC DERMATITISFourta LasoctoBelum ada peringkat
- Derma MCQ Ch01 PDFDokumen20 halamanDerma MCQ Ch01 PDFShah NawazBelum ada peringkat
- Effect of Oral Vitamin E On Atopic DermatitisDokumen4 halamanEffect of Oral Vitamin E On Atopic DermatitisYusufTaqwaMuladiBelum ada peringkat
- Alterations With Infectious, Inflammatory and Immunologic ResponsesDokumen8 halamanAlterations With Infectious, Inflammatory and Immunologic ResponsesPATRIZJA YSABEL REYESBelum ada peringkat
- Pak International Nursing College Hayatabad Peshawar Paper: Microbiology MCQS: 70Dokumen8 halamanPak International Nursing College Hayatabad Peshawar Paper: Microbiology MCQS: 70anon_675257473Belum ada peringkat
- Hypersensitivity ReactionsDokumen11 halamanHypersensitivity ReactionsMenly SusadaBelum ada peringkat