Mechanicalventilation 140221055047 Phpapp01
Diunggah oleh
jayr_gabiana24Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Mechanicalventilation 140221055047 Phpapp01
Diunggah oleh
jayr_gabiana24Hak Cipta:
Format Tersedia
Mechanical ventilation
Shilanjan Roy
PGT Medicine
Objectives
Objectives
Discuss indications and techniques for non
invasive positive pressure ventilation.
Describe characteristics of different types of
breath and modes of mechanical ventilation.
Outline basic ventilator settings.
Interactions between ventilatory parameters
and modifications needed to avoid harmful
effects of mechanical ventilation.
Initial ventilator management that apply to
specific clinical situations.
Indications
Indications for Mechanical
Ventilation
The work of breathing usually accounts for 5% of
oxygen consumption (V0
2
).
In the critically ill patient this may rise to 30%.
Invasive mechanical ventilation eliminates the
metabolic cost of breathing.
Indications for Mechanical
Ventilation
Inadequate oxygenation (not corrected by
supplemental O
2
by mask).
Inadequate ventilation (increased PaCO
2
).
Retention of pulmonary secretions (bronchial
toilet).
Airway protection (obtunded patient, depressed
gag reflex).
Indications
Ventilation abnormalities:
Respiratory muscle fatigue
Chest wall abnormalities
Neuromuscular disease
Increased airway resistance and /or obstruction
Decreased ventilatory drive
Oxygenation abnormalities:
Refractory Hypoxaemia
Excessive work of breathing
Need for positive end expiratory pressure
Other indications
Need for sedation and / or neuromuscular
blockade.
Need to decrease systemic / myocardial
oxygen demand.
Use of hyperventilation to reduce Raised
ICP.
Facilitation of alveolar recruitment and
prevention of atelectasis.
NIPPV ( NON INVASIVE
POSITIVE PRESSURE
VENTILATION)
NIV vs. Invasive Mechanical
Ventilation
NIV is defined as ventilatory support
provided via a tight fitting mask or similar
interface as opposed to invasive support,
which is provided via a laryngeal mask,
endotracheal tube or tracheostomy tube.
Tight fitting masks deliver can CPAP,
BIPAP or NIV via the mechanical ventilator.
Advantages of NPPV
Reduced need for sedation
Preservation of airway protective reflexes
Avoidance of upper airway trauma
Decreased incidence of nosocomial sinusitis
and pneumonia
Improved patient comfort
Shorter length of ICU and hospital stay
Improved survival
Disadvantages of NPPV
Claustrophobia
Facial /nasal pressure lesions.
Unprotected airway
Inability to suction deep airway
Gastric distension with use of face mask or
helmet
Possible upper extremity edema, axillary vein
thrombosis, tympanic dysfunction, and
intrahelmet noise with use of helmet
Delay in intubation.
Contraindications of NPPV
Cardiac or respiratory arrest.
Haemodynamic instability
Uncooperative.
Inability to protect the airways.
High risk of aspiration.
Active upper GI bleed.
Severe encephalopathy.
Facial trauma, recent surgery &/or burn
Conditions likely to respond
to NPPV
Hypoxaemic respiratory failure:
Cardiogenic pulmonary edema without
haemodynamic instability
Respiratory failure in IC patients.
(haematologic malignacies and
transplant patients)
Patients not candidates for intubation
Hypercapnic respiratory failure:
AECOPD
AE bronchial asthma
Resp failure in patients with cystic
fibrosis
Patients not candidates for
intubation
Initiation of NPPV
Do not delay intubation if needed.
Ensure appropriate mask or helmet size.
Assess patients tolerance of the mask by
applying it by hands before securing the
harness.
Explain the procedure to the patients
Initial ventilation settings-
Mode: spontaneous
Trigger: maximum sensitivity
EPAP : 4-5 cm H
2
O
IPAP : 10-15 cm H
2
O
Rate: 6/min
Cont
Adjust difference between EPAP & IPAP to
achieve effective tidal vol. & CO
2
clearance.
EPAP increments of 2 cm H
2
O /step to
improve oxygenation by alveolar
recruitment.
In assist control ventilation begin with V
T
6-8
ml/kg.
Titrate pressure, vol & FiO
2
to achieve
appropriate PaO
2
& PaCO
2
levels.
Ventilator changes can be made
every 15-30 mins.
Invasive mechanical
ventilation
Intubation
Bare Essentials for Intubation
ALSOBLEED
Airway: oral Guedel airway to lift tongue off
posterior pharynx to facilitate mask ventilation
during pre-intubation phase.
2 Liquids: stop feed and aspirate ng tube.
3 Suction: extremely important to avoid pulmonary
aspiration.
4 Oxygen: preoxygenate patient and ensure a
source of O
2
with a delivery mechanism
(ambu-bag and mask) is available
Bare Essentials for Intubation
ALSOBLEED
5 Bougie: to facilitate tube insertion in more difficult
airway.
6 Laryngoscope: have a long and short blade
available.
7 Endotracheal tube: for average adult, cuffed oral
endotracheal tube 7.0 for women and 8.0 for men.
8 End tidal CO
2
: to confirm correct position of tube.
9 Drugs: an induction agent, muscle relaxant,
sedative are usually required.
Principles of Mechanical
Ventilation
Principles of Mechanical
Ventilation
Positive pressure ventilation involves delivering
a mechanically generated breath to get O
2
in and
CO
2
out.
Gas is pumped in during inspiration (Ti) and the
patient passively expires during expiration (Te).
The sum of Ti and Te is the respiratory cycle or
breath.
Basic mechanics
Each mechanical ventilatory cycle can be
divided into 2 phases:
Inspiration is the point at which exhalation
valve closes and fresh gas enters the chest.
The amount of gas delivered during
inspiration is limited by 3 parameters that
can be set in the ventilator:
Volume
Pressure and/or
Flow
Cycling :
Changeover from the end of inspiration to
the second phase , expiration.
Cycling can occur in response to elapsed
time , delivered volume or a decrease in
flow rates.
Expiration begins when the gas flow from
the ventilator is stopped and exhalation
circuit is opened to allow gas to escape from
the lungs.
Triggering :
Changeover from expiration to inspiration.
All ventilators require some signal from the
patient to determine when inspiration should
begin.
Triggering signal results when patients
inspiratory effort produces a drop in airway
pressure or diversion of a constant gas flow
in ventilator circuitry.
CYCLING
TRIGGERING
In the absence of patients interaction with
the ventilator, breaths are delivered based
on elapsed time.
This is called UNASSISTED OR
MANDATORY BREATH.
Based on this definitions two ventilator
breath types are possible:
Mandatory/ UnAssisted breath
Assisted breath
Principles of Mechanical
Ventilation
In the fully ventilated patient, positive pressure
breaths are delivered either as preset volume or
pressure continuous mandatory breaths (CMV)
breaths.
The mechanical ventilator triggers the breath
and switches from inspiration to expiration when
the preset volume, pressure (or time) is
achieved/delivered.
During CMV the patient takes no spontaneous
breaths.
CMV is usually used in theatre and in very unwell
ICU patients.
Types of ventilator breaths
A. volume cycled (control) breath
Ensures delivery of a preset tidal
volume( unless the peak pressure limit is exceeded)
On some ventilators setting of peak
inspiratory flow rate and choice of inspiratory
flow waveform( sine, square, decelerating)
determine length of inspiration.
with volume cycled breaths, worsening
airway resistance or lung compliance results
in increase in peak inspiratory pressure.
B.Time cycled breath
Often called pressure cycled( controlled)
breath, applies a constant pressure over
preset time.
Produces a decelerating inspiratory flow
waveform as the pressure gradient between
the ventilator( constant pressure) patient(
pressure rises as lung fills) falls.
In this setting , changes in the airway
resistance or lung compliance will alter the
tidal volume.
C. Flow cycled breath
usually pressure support breath.
Similar to a time cycled breath.
However, pressure support is terminated
when the flow rate decreases to a
predetermined percentage of initial flow rate
e.g 25%.
F
l
o
w
P
r
e
s
s
u
r
e
Principles of Mechanical Ventilation
Ti Te Ti Te
Volume cycled/ Control
Breath
Pressure cycled/Control
Breath
Why is the peak airway pressure
(PAP) important?
Ventilator Induced Lung Injury (VILI).
Mechanical ventilation is injurious to the lung.
Aim PAP< 35 cm H
2
0.( platue pressure < 30 cm
water)
HIGH PAP may cause barotruma(pneumothorax),
Volutruma( lung parenchymal injury)
Dont forget that the peak airway
pressure will also include the PEEP that
is added
F
l
o
w
P
r
e
s
s
u
r
e
Ti Te Ti Te
Principles of Mechanical Ventilation
Volume Breath Pressure Breath
35 cm H
2
0
Pneumothorax- Example of
ventilator induced barotruma
MODES AND SETTINGS
OF MECHANICAL
VENTILATION
Overview of topics
1. Settings
2. Modes
3. Advantages and disadvantages between
modes
4. Guidelines in the initiation of mechanical
ventilation
5. Common trouble shooting examples with
mechanical ventilation
Settings
1. Trigger mode and sensitivity
2. Respiratory rate
3. Tidal Volume
4. Positive end-expiratory pressure (PEEP)
5. Flow rate
6. Inspiratory time
7. Fraction of inspired oxygen
Trigger
There are two ways to initiate a ventilator-delivered breath:
pressure triggering or flow-by triggering
When pressure triggering is used, a ventilator-
delivered breath is initiated if the demand
valve senses a negative airway pressure
deflection (generated by the patient trying to
initiate a breath) greater than the trigger
sensitivity.
When flow-by triggering is used, a continuous
flow of gas through the ventilator circuit is
monitored. A ventilator-delivered breath is
initiated when the return flow is less than the
delivered flow, a consequence of the patient's
effort to initiate a breath
Tidal Volume
The tidal volume is the amount of air
delivered with each breath. The
appropriate initial tidal volume
depends on numerous factors, most
notably the disease for which the
patient requires mechanical
ventilation.
Respiratory Rate
An optimal method for setting the
respiratory rate has not been
established. For most patients, an
initial respiratory rate between 12 and
16 breaths per minute is reasonable
Positive End-Expiratory
Pressure (PEEP)
Mechanically ventilated patients usually
receive positive end-expiratory pressure
(PEEP), to overcome the loss of
physiological PEEP provided by the
larynx and vocal cords.
Applied PEEP is generally added to mitigate
end-expiratory alveolar collapse.
PEEP
PEEP is delivered throughout the respiratory
cycle and is synonymous to CPAP, but in the
intubated patient.
A typical initial applied PEEP is 5 cmH2O. However, up
to 20 cmH2O may be used in patients undergoing
low tidal volume ventilation for acute respiratory
distress syndrome (ARDS)
Flow Rate
The peak flow rate is the maximum flow
delivered by the ventilator during inspiration.
Peak flow rates of 60 L per minute may be
sufficient, although higher rates are
frequently necessary.
An insufficient peak flow rate is
characterized by dyspnea, spuriously low
peak inspiratory pressures, and scalloping
of the inspiratory pressure tracing
Inspiratory Time: Expiratory
Time Relationship (I:E Ratio)
During spontaneous breathing, the
normal I:E ratio is 1:2, indicating that
for normal patients the exhalation time
is about twice as long as inhalation
time.
If exhalation time is too short breath
stacking occurs resulting in an
increase in end-expiratory pressure
also called auto-PEEP.
Depending on the disease process,
such as in ARDS, the I:E ratio can be
changed to improve ventilation
Fraction of Inspired Oxygen
The lowest possible fraction of inspired
oxygen (FiO2) necessary to meet
oxygenation goals should be used.
This will decrease the likelihood that
adverse consequences of supplemental
oxygen will develop, such as absorption
atelectasis, accentuation of hypercapnia,
airway injury, and parenchymal injury
Modes of Ventilation: The
Basics
Assist-Control Ventilation :Volume Control
Assist-Control Ventilation: Pressure Control
Pressure Support Ventilation
Synchronized Intermittent Mandatory
Ventilation :Volume Control
Synchronized Intermittent Mandatory
Ventilation :Pressure Control
Assist Control Ventilation
A set tidal volume (if set to volume control)
or a set pressure and time (if set to pressure
control) is delivered at a minimum rate
Additional ventilator breaths are given if
triggered by the patient.
Once stabilised on CMV, the level of ventilatory
support may be reduced (weaning).
This can be done by providing a mixture of
synchronised intermittent mandatory breaths
(SIMV) and spontaneously triggered pressure
supported breaths (PSV).
Synchronized Intermittent
Mandatory Ventilation
Breaths are given are given at a set minimal rate,
however if the patient chooses to breath over the
set rate no additional support is given
One advantage of SIMV is that it allows patients to
assume a portion of their ventilatory drive
SIMV is usually associated with greater work of
breathing than AC ventilation and therefore is less
frequently used as the initial ventilator mode
Like AC, SIMV can deliver set tidal volumes
(volume control) or a set pressure and time
(pressure control)
Negative inspiratory pressure generated by
spontaneous breathing leads to increased venous
return, which theoretically may help cardiac output
and function
SIMV and Pressure Support
Ventilation
In SIMV mode the ventilator allows two kinds of
breath.
The first is delivered according to the preset
waveform and is the mandatory breath. The timing
of the start of this breath may be triggered by the
patients respiratory effort but, if the patient is not
making sufficient respiratory effort, is determined by
the ventilator. The second is a spontaneous breath. If
SIMV is combined with pressure support then the
ventilator facilitates this second breath by providing
pressure support. This second type of breath is
entirely dependent on patient effort.
The graphs illustrate the changes in pressure and
flow that occur with first a mandatory breath and then
a pressure-supported breath
SIMV and Pressure Support Ventilation
Ventilator Patient
SIMV and Pressure Support
Ventilation
Ventilator assisted breaths are synchronized with
the patients breathing to prevent the possibility
of a mechanical breath on top of a spontaneous
breath.
However, the patients attempt at a breath would
not be enough to generate an adequate tidal
volume on its own, hence the term pressure
support.
Pressure Support
Ventilation
The patient controls the respiratory rate
and exerts a major influence on the
duration of inspiration, inspiratory flow rate
and tidal volume
The model provides pressure support to
overcome the increased work of breathing
imposed by the disease process, the
endotracheal tube, the inspiratory valves
and other mechanical aspects of
ventilatory support.
PSV
As patients improve, mandatory breaths are
withdrawn and receive pressure-supported breaths
alone.
Finally, as tidal volumes improve, the level of
pressure support is reduced and then withdrawn
so patients breathe spontaneously with PEEP
alone.
Extubation can now be contemplated.
Spontaneous modes of breathing should always
be encouraged as respiratory muscle function is
maintained
Pressure Support Ventilation
Patient Patient
PSV augments the patients own
respiratory effort and best adjusted by
observing changes in patients resp
rate, v
t
and comfort.
Pressure support is only delivered during
inspiration and the patients attempt at breathing
triggers the breath rather than the ventilator.
A standard level of pressure support delivered in
inspiration is 20 cm H
2
0
Airway pressure & flow tracings for commonly used modes of mechanical
ventilation
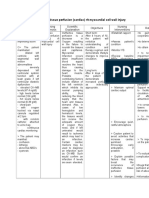
Advantages of Each Mode
Mode Advantages
Assist Control Ventilation (AC) Reduced work of breathing compared
to spontaneous breathing
AC Volume Ventilation Guarantees delivery of set tidal
volume
AC Pressure Control Ventilation Allows limitation of peak inspiratory
pressures
Pressure Support Ventilation (PSV) Patient comfort, improved patient
ventilator interaction
Synchronized Intermittent Mandatory
Ventilation (SIMV)
Less interference with normal
cardiovascular function
Disadvantages of Each
Mode
Mode Disadvantages
Assist Control Ventilation (AC) Potential adverse hemodynamic
effects, may lead to inappropriate
hyperventilation
AC Volume Ventilation May lead to excessive inspiratory
pressures
AC Pressure Control Ventilation Potential hyper- or hypoventilation with
lung resistance/compliance changes
Pressure Support Ventilation (PSV) Apnea alarm is only back-up, variable
patient tolerance
Synchronized Intermittent Mandatory
Ventilation (SIMV)
Increased work of breathing compared
to AC
To succeed, the initiating cause of respiratory failure,
sepsis, fluid and electrolyte imbalance and nutritional
status should all be treated or optimised.
Failure to wean is associated with:
Ongoing high V0
2
.
Muscle fatigue.
Inadequate drive.
Inadequate cardiac reserve.
Successful Weaning and Extubation
Successful Weaning and
Extubation
Weaning screens exist to help select patients for
extubation.
In the unsupported patient, if f/Vt is >100,
extubation is likely to be unsuccessful.
There is some evidence to support extubation to
NIV, particularly in patients with COPD.
Guidelines in the Initiation of
Mechanical Ventilation
Primary goals of mechanical ventilation are
adequate oxygenation/ventilation, reduced
work of breathing, synchrony of vent and
patient, and avoidance of high peak
pressures
Set initial FIO2 on the high side, you can
always titrate down
Initial tidal volumes should be 8-10ml/kg,
depending on patients body habitus. If
patient is in ARDS consider tidal volumes
between 5-8ml/kg with increase in PEEP
Guidelines in the Initiation of
Mechanical Ventilation
Use PEEP in diffuse lung injury and ARDS
to support oxygenation and reduce FIO2
Avoid choosing ventilator settings that limit
expiratory time and cause or worsen auto
PEEP(espl in obstructive airway disease)
When facing poor oxygenation, inadequate
ventilation, or high peak pressures due to
intolerance of ventilator settings consider
sedation, analgesia or neuromuscular
blockage
SPECIFIC CASE
SCENARIOS
Trouble Shooting the Vent
If we have a patient with history of COPD/asthma
with worsening oxygen saturation and increasing
hypercapnia differential includes:
Given the nature of the disease process, patients
have difficultly with expiration (blowing off all the
tidal volume)
Must be concern with breath stacking or auto-
PEEP
Management options include:
Decrease respiratory rate Decrease tidal volume
Adjust flow rate for quicker
inspiratory rate
Increase sedation
Adjust I:E ratio
Trouble Shooting the Vent
Increase in patient agitation and dis-synchrony on the
ventilator:
Could be secondary to overall
discomfort
Increase sedation
Could be secondary to feelings of
air hunger
Options include increasing tidal volume,
increasing flow rate, adjusting I:E ratio,
increasing sedation
Trouble shooting the vent
If you are concern for acute respiratory distress
syndrome (ARDS)
Correlate clinically and radiologic
findings of diffuse patchy infiltrate on
CXR
Obtain a PaO2/FiO2 ratio (if < 200 likely
ARDS)
Begin ARDS net protocol:
Low tidal volumes
Increase PEEP rather than FiO2
Consider increasing sedation to promote
synchrony with ventilator
ARDS Protocol
Start with a PEEP of 5 and uptitrate..optimal PEEP is
usually 8-15 cm H2O.
Start with a Vt of 8 ml/kg then gradually decrease till
Vt of 6 ml/kg is reached.
P plat should be < 30.
Ph> 7.15 is acceptable.
PSV
PEEP
SIMV
PSV
CMV
Mandatory Spontaneous Overlap
PSV
PEEP
SIMV
PSV
CMV PSV
PEEP
SIMV
PSV
CMV
Mandatory Spontaneous Overlap
Standard Ventilator Settings
MORITE
Mode CMV, Volume Control
O
2
0.5 (50% 0
2
)
Respiratory Rate 12/minute
Inspiratory Action Set Vt at 500 mls
Inspiratory Time Set I:E ratio 1:2
Expiratory Action Set PEEP at 5 cm H
2
0
Be Aware PAP 35 cm H
2
O
HYPOTENSION ASSOC WITH
MECHANICAL VENTILATION
1)TENSION PNEUMOTHORAX
2)CONVERSION FROM NEGATIVE TO POSITIVE
INTRATHORASIC PRESSURES.
3)Auto PEEP.
4)AMI./ MYOCARDIAL ISCHAEMIA.
TAKE HOME MESSAGE
1) Goals of NIV and IPPV are to suppport
ventilation and oxygenation, reduce work of
breathing and patient comfort.
2)NPPV is best utilized in C/A/C patients
whose resp condition is expected to improve
in 48-72 hrs.
3)Guidelines for initiating mechanical
ventilation should be carefully followed.
4)Inspiratory plateue pressures should be
maintained <30 cm H
2
o.
TAKE HOME MESSAGE
5) During mech ventilation, patient must be carefully
monitored using vent alarm systems, rintermittant
ABG analysis, pulse oximetry , physical assessment,
and chest radiograph as needed.
6) Hypotension in ventilated pt should be prompt
evaluated for pneumothorax, auto PEEP, AMI.
7)The primary determinants of oxygenation are Fi02
and Mean airway pressure whereas alveolar
ventilation affects CO
2
exchange.
8) THE Complex interaction of inspiratory pressures,
I:E Ratio, Fio2, and PEEP must be evaluated.
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Dubai Professional License ApplicationDokumen8 halamanDubai Professional License Applicationjayr_gabiana24Belum ada peringkat
- Procedure and Application Form For Nursing and Midwifery Registration in DubaiDokumen1 halamanProcedure and Application Form For Nursing and Midwifery Registration in DubaiSiva PrakashBelum ada peringkat
- HAAD Coomonly Asked Questions Sibika at KulturaDokumen3 halamanHAAD Coomonly Asked Questions Sibika at Kulturajayr_gabiana2450% (2)
- Haad Dataflow GuideDokumen16 halamanHaad Dataflow Guidehady920100% (4)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Semi-Detailed Lesson Plan in Science 9Dokumen3 halamanSemi-Detailed Lesson Plan in Science 9justine100% (1)
- DLP 12-14 M Hope 1Dokumen7 halamanDLP 12-14 M Hope 1KaiA.SermenoBelum ada peringkat
- BLS & AclsDokumen112 halamanBLS & AclsPriya SharmaBelum ada peringkat
- CIRRHOSIS - Albumin in Decompensated Cirrhosis New Concepts and PerspectivesDokumen12 halamanCIRRHOSIS - Albumin in Decompensated Cirrhosis New Concepts and PerspectivesntnquynhproBelum ada peringkat
- Meta Control 3000 Brochure ENGLISHDokumen2 halamanMeta Control 3000 Brochure ENGLISHNguyễn Thu ThủyBelum ada peringkat
- Secondary Growth of PlantsDokumen13 halamanSecondary Growth of PlantsAngie Kong Su Mei50% (2)
- Primary and Secondary Lymphoid OrgansDokumen7 halamanPrimary and Secondary Lymphoid OrgansAfeef AshrafBelum ada peringkat
- Action Potential: ConcentrationDokumen8 halamanAction Potential: ConcentrationAhmad HaBelum ada peringkat
- Fitt Principle SubmissionDokumen2 halamanFitt Principle Submissionapi-469731439Belum ada peringkat
- Drenergic AND Anti Adrenergic Drugs: Shabib AkhtarDokumen21 halamanDrenergic AND Anti Adrenergic Drugs: Shabib AkhtarDeepa ShaiekhBelum ada peringkat
- Inotropic and Vasoactive Drugs in Pediatric ICUDokumen6 halamanInotropic and Vasoactive Drugs in Pediatric ICUCandy RevolloBelum ada peringkat
- Pathophysiology of Ischemic Stroke FinalDokumen3 halamanPathophysiology of Ischemic Stroke FinalAcohCChao75% (4)
- Respiratory and Circulatory SystemsDokumen58 halamanRespiratory and Circulatory SystemsmiomodgBelum ada peringkat
- Phyp211 - Week 2Dokumen2 halamanPhyp211 - Week 2KHRIZZA PAULETTE ANTIFORDA VEGABelum ada peringkat
- Procedure On Basic Life Support: General ConceptsDokumen4 halamanProcedure On Basic Life Support: General Conceptsmalleshwari athramBelum ada peringkat
- Thoracic Trauma in Small AnimalsDokumen5 halamanThoracic Trauma in Small AnimalsCabinet VeterinarBelum ada peringkat
- Acute Coronary Syndrome NCP 02Dokumen6 halamanAcute Coronary Syndrome NCP 02AgronaSlaughterBelum ada peringkat
- Histology The Respiratory System: Prof. Dr. Sabah N. AlwachiDokumen15 halamanHistology The Respiratory System: Prof. Dr. Sabah N. AlwachilaithjnbBelum ada peringkat
- PhysioEx Exercise 9 Activity 2Dokumen3 halamanPhysioEx Exercise 9 Activity 2MARILYN MARIANA HERNANDEZ MENDOZABelum ada peringkat
- Chapter 21 Intro To CNS PharmaDokumen8 halamanChapter 21 Intro To CNS PharmaChristine Annmarie TapawanBelum ada peringkat
- The Radial Path of Ion Movement Through RootsDokumen2 halamanThe Radial Path of Ion Movement Through RootsAtika AnggrainiBelum ada peringkat
- Pathophysiology Final Exam ReviewDokumen38 halamanPathophysiology Final Exam ReviewBheru Lal100% (2)
- Circulation and Blood 1B.1Dokumen17 halamanCirculation and Blood 1B.1tas xoBelum ada peringkat
- Intrinsic Frequencies of Carotid Pressure Waveforms Predict Heart Failure EventsDokumen9 halamanIntrinsic Frequencies of Carotid Pressure Waveforms Predict Heart Failure EventsSaionara FranciscoBelum ada peringkat
- Praktikum 3Dokumen16 halamanPraktikum 3Samuel Manalu100% (1)
- Public Knowledge of The Symptoms of Myocardial Infarction: A Street Survey in Birmingham, EnglandDokumen6 halamanPublic Knowledge of The Symptoms of Myocardial Infarction: A Street Survey in Birmingham, Englandpanji satryo utomoBelum ada peringkat
- 2013 ESH/ESC Practice Guidelines For The Management of Arterial HypertensionDokumen14 halaman2013 ESH/ESC Practice Guidelines For The Management of Arterial HypertensionReski Melinia PatinggiBelum ada peringkat
- Pathophysiology The Biologic Basis For Disease in Adults and Children 7th Edition Mccance Test BankDokumen13 halamanPathophysiology The Biologic Basis For Disease in Adults and Children 7th Edition Mccance Test BankMargaretGreenjadpw100% (18)
- VII. Course in Ward / Treatments / Intervention Medical Management 1. Doctor's Progress Notes Date Physician's Order RationaleDokumen7 halamanVII. Course in Ward / Treatments / Intervention Medical Management 1. Doctor's Progress Notes Date Physician's Order RationaleDaniela Claire FranciscoBelum ada peringkat
- Effect of Local Insulin Injection On Wound VasculaDokumen6 halamanEffect of Local Insulin Injection On Wound Vasculaeva yustianaBelum ada peringkat